Abstract
Lumbar spinal stenosis is typically a degenerative condition that leads to compression of the spinal canal and lateral recess, resulting in leg pain and walking disability. Surgical management is indicated after failure of non‐surgical management or rapidly worsening neurological impairment. The traditional approach is a laminectomy with foraminotomy and partial facetectomy but a newer minimally invasive option, unilateral laminectomy for bilateral decompression (ULBD), seems to demonstrate the better postoperative outcomes due to its unilateral exposure. ULBD involves a midline incision, opening the thoracolumbar fascia, retracting the paravertebral muscles unilaterally, then a hemilaminectomy, flavectomy, and decompression of the spinal canal with foraminotomy or partial facetectomy. The clinical decision on which side to approach spinal stenosis with ULBD has not been discussed in the literature. We have come up with an algorithm to decide which side to approach for ULBD based on position of spinous process and angulation, side of maximal compression, and surgeon handedness.
Keywords: Decompression, Lumbar spinal stenosis, Surgical technique, Unilateral laminectomy
Introduction
Lumbar spinal stenosis (LSS) is typically caused by degenerative facet‐joint arthrosis, ligamentum hypertrophy, and broad‐based disc bulging, leading to compression of the spinal canal and lateral recess, resulting in walking disability and leg pain. LSS is a progressive degenerative condition most common in patients over the age of 60 years and can significantly impact quality of life and daily activities, and lead to progressive disability1, 2. Patients may present with neurogenic claudication, which can be exacerbated by standing and relieved by flexion at the waist, such as when in the seated position. Patients may also experience tingling, numbness, and weakness of the lower extremities3, 4. Non‐surgical management is the first‐line therapy for most patients with LSS and may include physiotherapy, hydrotherapy, pain medication, and epidural injections of corticosteroids or anesthetics5, 6, 7. Surgery is indicated in the acute setting for patients with rapidly progressive neurological impairment or sphincteric dysfunction. Surgical decompression is also a viable treatment option for patients with chronic disability who fail to respond to conservative management. Surgical decompression in the setting of failed conservative therapy has been shown to have similar outcomes to patients who are treated initially with surgical decompression8. LSS is a chronic condition in which many patients fail to achieve relief of symptoms with non‐surgical management. Ciol et al. found that in a conservatively managed cohort only 15% experienced an improvement in symptoms after 4 years, with 70% describing similar symptoms and 15% reporting worsened symptoms2.
The traditional surgical approach to LSS generally involves a laminectomy with foraminotomy and partial facetectomy (Fig. 1), which can be performed with lumbar fusion in the case of spondylolisthesis9. Recent literature, however, supports simple decompression alone, without instrumentation, in the setting of listhesis in selected patients10, 11. Surgery is more commonly elective, with the intention to improve quality of life rather than to prevent neurological impairment. There is limited high quality evidence for the efficacy of surgical management of spinal stenosis, with most studies focusing on patient‐centered outcomes, with a lack of occupational outcomes, and few studies including follow‐up past 3 years12.
Figure 1.
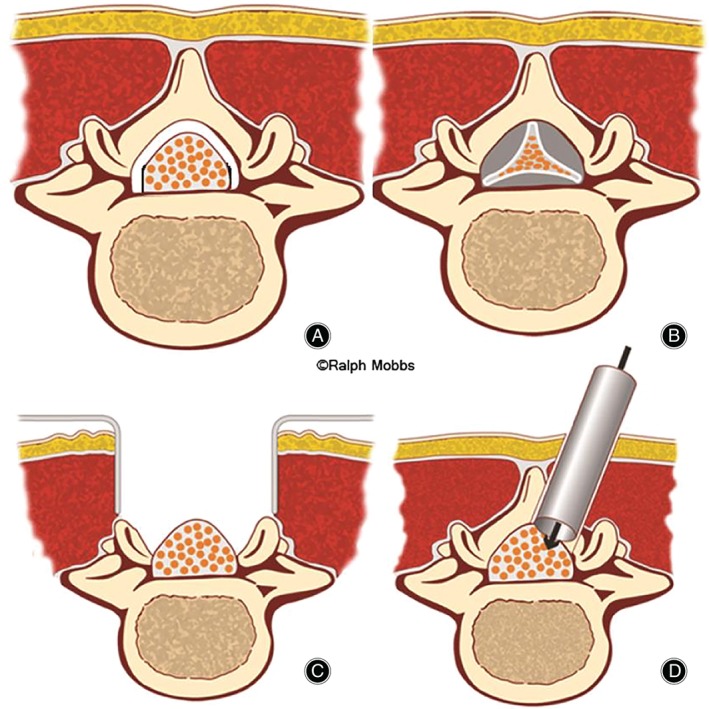
Schematic options for lumbar spinal stenosis. (A) Normal lumbar spinal canal. (B) Central stenosis due to flavum and facet hypertrophy and disc encroachment. (C) “Standard” laminectomy with removal of muscular attachments and midline structures. (D) Unilateral laminectomy with preservation of midline structures.
Unilateral laminectomy for bilateral decompression (ULBD) is a recently developed minimally invasive surgical technique for decompression of the spinal canal, which only requires unilateral exposure, therefore minimizing iatrogenic injury to the paraspinal muscles. Broadly speaking, ULBD requires a posterior midline incision followed by opening of the thoracolumbar fascia and retraction of the paravertebral muscles ipsilaterally (Figs 1, 2). An appropriate retractor of surgeon choice is inserted and a hemilaminectomy is performed to expose the ligamentum flavum. This is followed by a flavectomy and decompression of the spinal canal, which may involve foraminotomy and partial facetectomy13.
Figure 2.
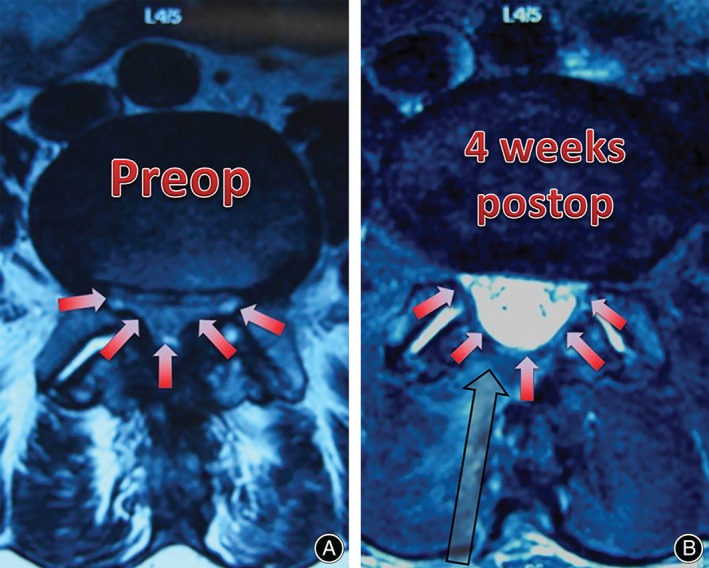
(A, B) Preoperative and postoperative MRI scan. The red arrows demonstrate the severity of the preoperative stenosis, and the degree of postoperative decompression. The surgery was performed from a right‐sided approach (grey arrow) based on surgeon handedness and preference; the spinous process was midline with symmetrical canal and lateral recess compression.
Den Boogert et al. retrospectively compared postoperative functional disability, pain, and patient satisfaction among 175 patients with LSS who underwent either a ULBD or a traditional laminectomy14. Patients in the ULBD group reported better overall satisfaction with the procedure and a reduction in visual analogue score (VAS) leg symptoms. However, no difference in postoperative functional disability was observed and the authors suggest that the differences in leg symptoms and overall satisfaction may not be related to surgical technique. Mobbs et al. conducted a similar study comparing ULBD to open laminectomy for LSS15. They looked at the same outcomes (the Oswestry disability index [ODI] and the VAS leg and patient satisfaction), but the study design was a prospective, randomized trial instead. Mobbs et al. observed significant improvements in ODI and VAS leg scores for both open and ULBD interventions. Comparing open and ULBD, however, they found that patients receiving ULBD experienced significantly higher improvement in VAS leg scores. Patients who underwent ULBD also experienced faster time to mobilization and were more likely to not require opioids to control postoperative pain. Morgalla et al. reported on 108 patients with LSS who were managed surgically through a unilateral partial hemilaminectomy, a hemilaminectomy, or a laminectomy approach16. Patients who underwent unilateral partial hemilaminectomies demonstrated significantly improved outcomes at 12 month follow‐up; however, there were no statistically significant differences in outcomes between the techniques.
The clinical decision on which side to approach spinal stenosis with ULBD has not been discussed in the literature. We have devised a simple algorithm that provides a guide for this decision, and discuss the decision‐making surrounding how to approach a ULBD.
Technique Note
Following appropriate patient workup, including a period of conservative management, and exclusion of other causes of claudication such as vascular arterial insufficiency, the spinal surgeon should consider approach‐related issues, including efficiency of unilateral retractor angle and exposure, and approach from the side that is most symptomatic.
Our algorithm for direction of approach and side of retractor placement is as follows (Figs 3, 4, 5, 6):
Figure 3.

Direction of approach. (A) The red arrow demonstrates the most efficient approach angle for decompression as the spinous process deviates to the left side, (B) providing a wide “window” for the surgeon to perform the decompression.
Figure 4.
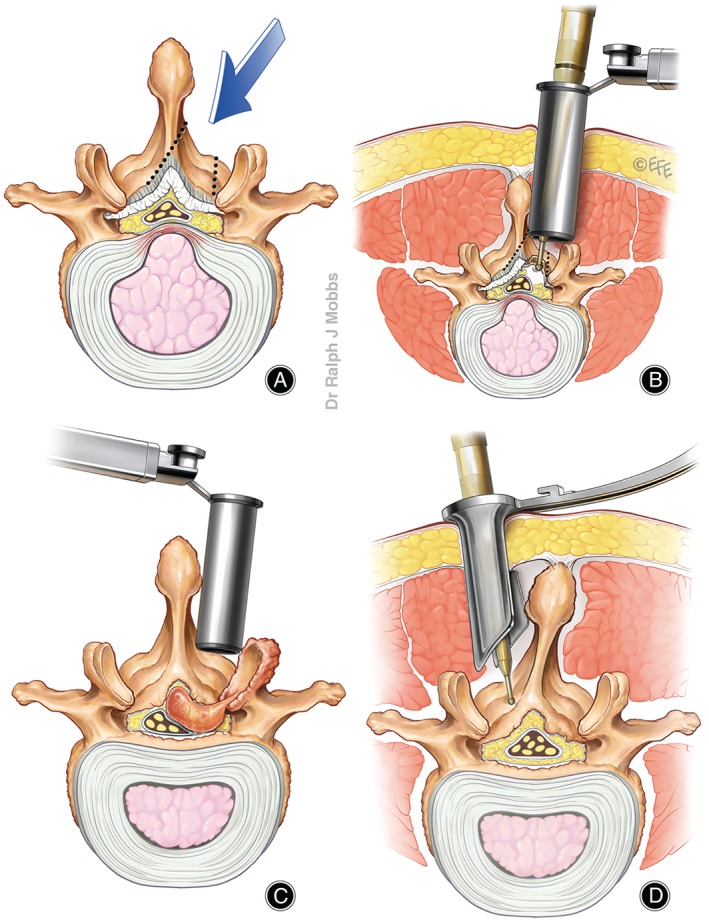
Unilateral laminectomy for bilateral decompression (ULBD) for lumbar canal stenosis. (A) Central canal stenosis can be managed by a unilateral approach with undercutting of the spinous process to access the contralateral lateral recess (dotted arrows). (B) The use of a tubular or blade‐retractor system can be used for ULBD. (C) Spinous process anatomy may assist the surgeon with the most appropriate angle of approach. (D) Canal stenosis due to unilateral pathology, such as a facet cyst, can be accessed through the ULBD approach.
Figure 5.
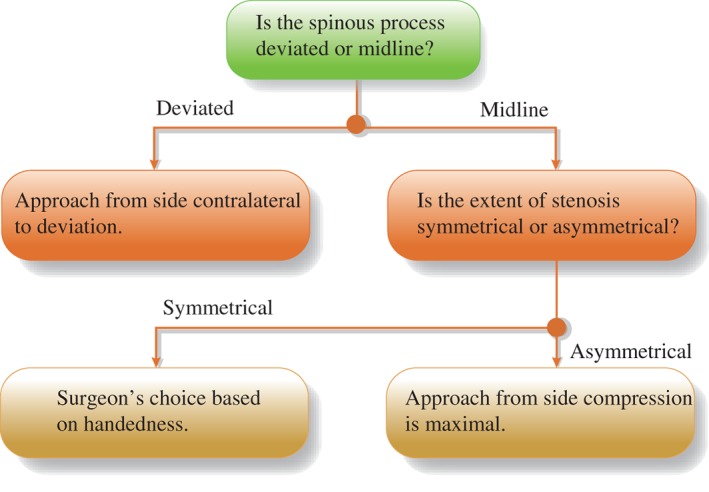
Algorithm for direction of approach and side of retractor placement.
Figure 6.
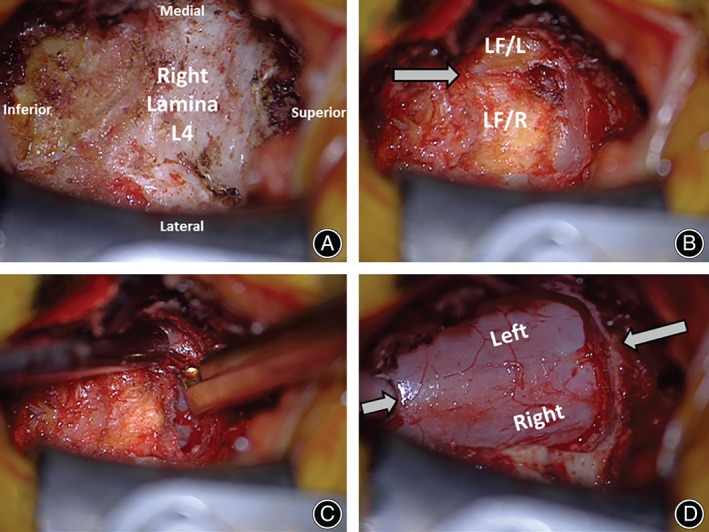
Intraoperative pictures for unilateral laminectomy for bilateral decompression (ULBD). (A) Initial unilateral exposure for a right‐sided approach. (B) The inferior half of the L 4 lamina has been drilled and the base of the spinous process to expose the ligamentum flavum bilateral to the insertion point deep to the L 4 lamina. (C) Decompression of the contralateral (left) side. (D) Completion of case demonstrating bilateral decompression from a unilateral (right) approach.
Position of Spinous Process and Angulation
If the spinous process is deviated to one direction, the approach should be from the contralateral side to the deviation to maximize the window of approach at the spinous process/lamina junction, to provide the surgeon the maximal anatomic window (Figs 3, 4C).
Side of Maximal Compression
If the spinous process is midline, the approach should be from the side where the compression is maximal: for example, if there is an additional facet joint cyst or disc bulge on a particular side, then the unilateral retractor placement should be on that side (Fig. 4D).
Symmetrical Stenosis and Midline Spinous Process
If there is symmetrical stenosis and a midline spinous process, it is the surgeons' choice based on handedness (Fig. 2). For instance, the senior author prefers a right‐sided approach as the use of the right hand is more dexterous to decompress the more technically demanding remaining spinous process.
Discussion
With an aging population, demand for surgical management of degenerative conditions affecting mobility, such as LSS, will significantly increase. This requires careful evaluation of current best practice and new surgical techniques in order to provide the best available care for these patients to reduce pain and disability, and to improve mobility. Several studies have shown good outcomes for a ULBD approach for the management of LSS; however, it is not clear whether this approach is superior, as high quality evidence is lacking in the literature13, 14, 15, 16. That said, these studies do provide evidence suggesting that the ULBD may be associated with better outcomes than with traditional laminectomy, and reduce hospital stay and the overall cost of the intervention (REF).
The use of surgical decompression alone to treat lumbar spinal stenosis declined slightly in the United States between 2002 and 2007, whereas the use of a combined procedure of decompression and fusion increased by a factor of 15 during this period. However, evidence showing a benefit of adding fusion to decompression surgery is lacking17. In addition, recent studies have provided further evidence that decompression without instrumentation should be considered in the setting of spondylolisthesis, despite the findings of the SPORT trial10, 11. This adds weight to the concept that minimizing approach‐related trauma with a unilateral exposure, and, therefore, reducing iatrogenic instability, is of potential benefit, and that the unilateral approach for bilateral decompression could be a primary tool in the spine surgeon's armamentarium. The authors are confident that given the evolution of surgical options and the management of LSS based on recent data that the approach of ULBD will grow in popularity. Hence, technical considerations should be thought out and considered.
As our algorithm is based entirely on anatomical considerations, careful evaluation of the preoperative MRI is required for the algorithm's implementation (Figs 2, 3). Our algorithm does not account for complicating anatomical factors such as scoliosis and spondylolisthesis, and the discretion of the surgeon will be necessary for such cases. Handedness of the surgeon plays an important role in deciding which side to approach, as surgeon comfort and dexterity is an important factor for efficient workflow during the procedure. The authors prefer a right‐sided approach when there is equivalence of approach direction, because for a right‐handed surgeon, approaching from the right side will make clearance of the contralateral recess and foramen easier as the right hand will be in an ergonomically superior position for approach angle to achieve the decompression.
Disclosure: All authors have no conflict of interest to declare.
References
- 1. Katz JN, Harris MB. Clinical practice. Lumbar spinal stenosis. N Engl J Med, 2008, 358: 818–825. [DOI] [PubMed] [Google Scholar]
- 2. Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc, 1996, 44: 285–290. [DOI] [PubMed] [Google Scholar]
- 3. Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O'Duffy JD. Lumbar spinal stenosis: clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med, 1985, 103: 271–275. [DOI] [PubMed] [Google Scholar]
- 4. Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis?. JAMA, 2010, 304: 2628–2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bodack MP, Monteiro M. Therapeutic exercise in the treatment of patients with lumbar spinal stenosis. Clin Orthop Relat Res, 2001, 384: 144–152. [DOI] [PubMed] [Google Scholar]
- 6. Mazanec DJ, Podichetty VK, Hsia A. Lumbar canal stenosis: start with nonsurgical therapy. Cleve Clin J Med, 2002, 69: 909–917. [DOI] [PubMed] [Google Scholar]
- 7. Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res, 2006, 443: 198–207. [DOI] [PubMed] [Google Scholar]
- 8. Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleâs F. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10‐year study. Spine (Phila Pa 1976), 2000, 25: 1424–1435, discussion 1435–1436. [DOI] [PubMed] [Google Scholar]
- 9. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA, 2006, 296: 2451–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med, 2016, 374: 1424–1434. [DOI] [PubMed] [Google Scholar]
- 11. Försth P, Ólafsson G, Carlsson T, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med, 2016, 374: 1413–1423. [DOI] [PubMed] [Google Scholar]
- 12. Gibson J, Waddell G. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev, 2005, (4): CD001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Storzer B, Schnake KJ. Microscopic bilateral decompression by unilateral approach in spinal stenosis. Eur Spine J, 2016, 25 (Suppl. 2): S270–S271. [DOI] [PubMed] [Google Scholar]
- 14. den Boogert HF, Keers JC, Marinus Oterdoom D, Kuijlen JM. Bilateral versus unilateral interlaminar approach for bilateral decompression in patients with single‐level degenerative lumbar spinal stenosis: a multicenter retrospective study of 175 patients on postoperative pain, functional disability, and patient satisfaction. J Neurosurg Spine, 2015, 23: 326–335. [DOI] [PubMed] [Google Scholar]
- 15. Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine, 2014, 21: 179–186. [DOI] [PubMed] [Google Scholar]
- 16. Morgalla MH, Noak N, Merkle M, Tatagiba MS. Lumbar spinal stenosis in elderly patients: is a unilateral microsurgical approach sufficient for decompression?. J Neurosurg Spine, 2011, 14: 305–312. [DOI] [PubMed] [Google Scholar]
- 17. Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976), 2013, 38: 916–926. [DOI] [PubMed] [Google Scholar]


