Abstract
Objective
To investigate the effect of internal fixation on postoperative ankle function in patients with supination‐external rotation type IV ankle fractures, including medial malleolus fractures and deltoid ligament injury.
Methods
Between January 2012 and June 2014, patients with medial structure injuries were enrolled in this study and assigned to the medial malleolus fracture group or the deltoid ligament group. The surgical procedures for the two groups were documented. The follow‐up endpoint was the time point when the steel plate or screw was removed from the lateral ankle. The Olerud–Molander ankle scoring system was used to assess ankle function.
Results
A total of 84 patients with supination‐external rotation type IV ankle fractures had complete medical records and were included in this study. The average age of the patients was 44.16 years (range, 15–75). The patient sample included 39 males and 45 females. Overall, 49 patients (19 males and 30 females) suffered a medial malleolus fracture. The average age of these patients was 40.20 years (range, 15–75). Patients with a posterior malleolar fracture fragment >25% of the articular surface accounted for 81.6% (40 patients) of these patients. Overall, 35 patients (20 males and 15 females) experienced a deltoid ligament injury. The average age of these patients was 44.21 years (range, 17–73). Patients with a posterior malleolar fracture fragment >25% of the articular surface accounted for 11.5% (four patients) of these patients. Open reduction was performed in patients with medial malleolus fractures, and two 4.0‐mm cannulated screws were used to fixate the posterior malleolus and the medial malleolus. The suture‐anchor technique was used to repair the ligaments in patients with deltoid ligament injuries. The follow‐up endpoint was the time point when the steel plate and screws were removed from the lateral ankle in patients. The average follow‐up period was 13.4 months (range, 11–17). The Olerud–Molander ankle scoring system was used to assess postoperative ankle function. The average score for the patients in the medial malleolus fracture group was 90.3 points (range, 85–95). The average score for the patients in the deltoid ligament injury group was 87.7 points (range, 80–95). No significant differences were found in the scores between the two groups.
Conclusion
Medial malleolus fracture and deltoid ligament injury are two different presentations of supination‐external rotation type IV ankle fractures. Anatomic reduction of the articular surface concurrent with restoration of ankle stability can achieve favorable results for these two injuries.
Keywords: Ankle, Deltoid ligament, Fracture, Medial malleolus
Introduction
The incidence of ankle fractures is approximately 187/100,000 persons, which is reported to be the fourth most common bone fracture that requires surgical management1. The two most commonly used classification systems are the Danis–Weber and Lauge–Hansen systems. The former is based on the level of the fracture, while the latter is based on the suspected injury mechanism. According to the Lauge–Hansen classification, supination‐external rotation fractures are the most common clinical ankle fractures, accounting for 40%–75% of the total. It is almost identical to a type B fracture in the Danis–Weber classification system, and can be further classified into the following four subtypes: type I, anterior tibiofibular ligament sprain; type II, anterior tibiofibular ligament sprain or avulsion fracture of the lateral malleolus tip combined with spiral fracture of the fibula below the level of the ankle joint; type III, type II plus posterior tibiofibular ligament rupture or posterior malleolus fracture; and type IV, type III plus medial malleolus fracture or deltoid ligament injury2. Type IV injuries are the most unstable ankle fractures and have poor outcomes after conservative treatment; therefore, this kind of fracture requires surgical treatment.
However, the surgical outcome of type IV supination‐external rotation ankle fractures is difficult to verify, and varies in different studies. This is because type IV supination‐external rotation fractures often involve two kinds of medial structure injury: a deltoid ligament injury and/or medial malleolus fractures. Both injuries are considered to be unstable fractures for which surgical treatment is superior to conservative treatment3.
The problem is, based on current clinical data, a consensus has not yet been reached regarding the management and postoperative outcomes of these two kinds of injury pattern. Tejwani et al. concluded that the extent of medial malleolus fractures was more severe than that of deltoid ligament injury and that the postoperative prognosis of patients with medial malleolus fractures was similarly poor4. Kennedy et al. conducted a retrospective study of 88 cases and found that the outcomes of bimalleolar fractures were poorer than those of lateral malleolus fractures with deltoid ligament injury5. Stufkens et al. performed a study in 36 patients with supination‐external rotation type IV fractures and found that the treatment outcomes were better in patients with deltoid ligament injuries than in patients with medial malleolus fractures6. In contrast, Berkes et al. found that treatment outcomes were similar between patients with deltoid ligament injury and patients with medial malleolus fractures in a follow‐up study of 108 patients with supination‐external rotation fractures7. Similarly, Donken et al. performed a 21‐year follow‐up study of 148 patients and found no significant differences in the subjective and objective radiographic scores between patients with medial malleolus fractures and those with deltoid ligament injury8. However, all these previous studies did not propose strategies for managing deltoid ligament injuries, which may have affected patient prognoses.
To sum up, the purpose of the present study is not only to investigate the effect of internal fixation on postoperative ankle function in patients with supination‐external rotation type IV ankle fractures, including both medial malleolus fractures and deltoid ligament injury, but also try to compare the postoperative clinical outcomes of these two different kinds of medial structure injury, so as to better understand the characteristics of supination‐external rotation type IV ankle fractures.
Materials and Methods
Inclusion and Exclusion Criteria
The inclusion criteria are: (i) ankle fracture of IV supination‐external rotation; and (ii) close fracture. The exclusion criterion is an open fracture.
General Information
Between January 2012 and June 2014, a total of 84 patients with supination‐external rotation type IV ankle fractures who were treated at our hospital and had complete medical records were included in this study. The patients were assigned to the medial malleolus fracture group or the deltoid ligament injury group based on the medial structure injury. Routine X‐ray and computed tomography (CT) scans were performed before surgery in all patients to confirm the diagnosis of posterior malleolar fractures. In addition, these tests were used to determine the proportion of the articular surface of the posterior malleolar fracture fragment to the entire articular surface of the distal articular surface of the tibia. A posterolateral incision to the fibula was used for fixation of the fibula and posterior malleolus in cases with a posterior malleolar fracture fragment >25% of the articular surface. Posterior malleolar fractures can remain untreated when the fracture fragment surface is <25%. The follow‐up endpoint was the time point when the steel plate or screw was removed from the lateral ankle after surgery. The Olerud–Molander ankle scoring system was used to assess ankle function in the two groups of patients.
Surgical Procedure
Indication for Fixation of the Posterior Malleolus
Fixation of the posterior malleolus here was indicated when the articular surface of the posterior malleolar fracture fragment was more than 25% of the entire articular surface of the distal articular surface of the tibia.
Medial Malleolus Fracture Group
After successful anesthesia was achieved, patients were positioned in the floating position. A tourniquet was placed on the proximal thigh, and the affected extremity was routinely prepped from toe to knee in a sterile fashion and draped. Initially, the affected lower extremity was rotated medially. A longitudinal incision posterolateral to the fibula was made. The sural nerve was identified and protected. A blunt dissection was performed between the flexor hallucis longus muscle and the peroneal tendons to expose the fracture sites of the fibula and the posterior malleolus and to remove scar tissue from the fracture sites. Anatomic reduction was performed to restore fibular rotation and length and posterior malleolus integrity. A reconstruction bone plate of appropriate length was attached to the posterior side of the fibula with screws. In patients with a posterior malleolar fracture fragment size >25% of the articular surface, two cannulated screws (4.0 mm in diameter and 32.0 mm in length; Johnson & Johnson [China] Medical Equipment) were used to fixate the posterior malleolus. Anatomical reduction of the fractures and good internal fixation were confirmed by X‐ray examination. Next, the affected lower extremity was rotated laterally. A curved incision anteroinferior to the medial malleolus was made, and the great saphenous vein and the saphenous nerve were dissected and protected. The anterior part of the tibionavicular ligament that was located in the superficial layer of the deltoid ligament and the anteromedial ankle capsule were incised to expose the fracture sites of the medial malleolus and to determine whether the medial talar dome cartilage was injured. After clearing hematomas in the medial interval, cartilage fragments, and periosteum trapped in the fracture line, anatomic reduction of the medial ankle fracture was performed using two cannulated screws (4.0 mm in diameter and 36.0 mm in length; Johnson & Johnson [China] Medical Equipment) for fixation. Good internal fixation and positioning were confirmed by X‐ray examination. The ankle external rotation test (at dorsiflexion of the foot) was performed to confirm ankle stability. The incision was closed in layers (Fig. 1).
Figure 1.
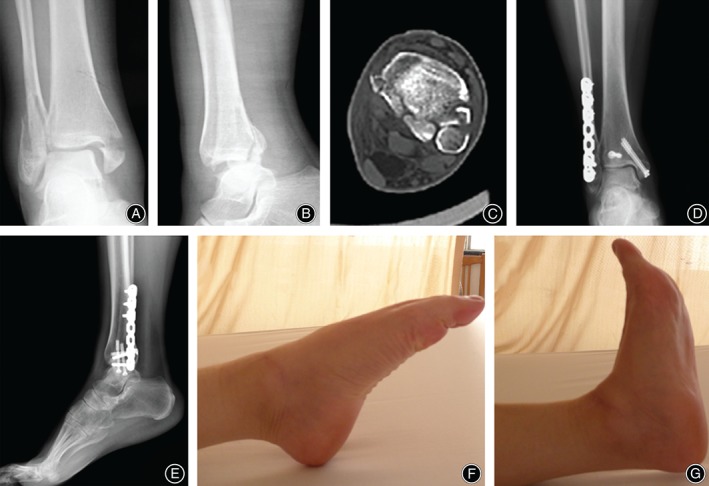
Supination‐external rotation type IV ankle fracture with medial malleolus fracture. (A–C) Preoperative X‐rays and computed tomography scan indicated trimalleolar fracture. (D,E) Postoperative X‐rays demonstrated that anatomical reduction was obtained, and lateral malleolus was fixated by a plate, while posterior and medial malleolus were fixated with cannulated screws. (F,G) Good ankle function was confirmed after surgery.
Deltoid Ligament Injury Group
After successful anesthesia was achieved, patients were positioned in the supine position. A tourniquet was placed on the proximal thigh. In patients without medial malleolus fractures, the ankle external rotation stress test (at dorsiflexion of the foot) was performed under C‐arm fluoroscopy to reconfirm that the deltoid ligament was injured. When the medial interval of the ankle was greater than 4 or 1 mm greater than the interval of the tibiotalar joint, a diagnosis of deltoid ligament injury was made9.
A curved incision anteroinferior to the medial malleolus was made. The great saphenous vein and the saphenous nerve were dissected and protected. The ruptured deltoid ligament may be seen, in which both superficial and deep components of the ligament may be disrupted. Next, the medial malleolus was inspected to determine whether the medial talar dome cartilage was injured. After clearing the ligament stump, hematomas, cartilage fragments, and periosteum from the medial interval, a 3.5‐mm TwinFix anchor (Shilehui Medical Product Int'l Trade [Shanghai]) was placed 10 mm from the tip of the anterior colliculus portion of the medial malleolus for next‐step use. A longitudinal incision lateral to the fibula was made to expose the fracture site and to remove hematomas and scar tissue from the fracture site. Anatomic reduction was performed to restore fibular rotation and length. A reconstruction bone plate of proper length was attached to the lateral side of the fibula with screws. Soft tissue was retracted in the medial incision to perform overlapping suture‐anchor fixation of the distal part of the superficial component of the ruptured deltoid ligament and the periosteum in the anterior colliculus portion of the medial malleolus. Good internal fixation and positioning were confirmed by X‐ray examination. The ankle external rotation test (at dorsiflexion of the foot) was performed to confirm ankle stability. The incision was closed in layers (Fig. 2).
Figure 2.
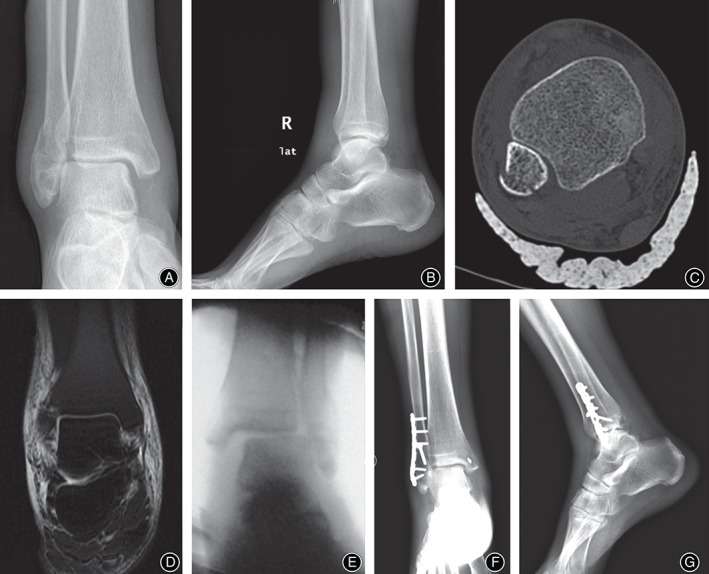
Supination‐external rotation type IV ankle fracture with deltoid ligament injury. (A–C) Medial malleolar fracture was not found in both preoperative X‐rays and computed tomography scan. (D) Preoperative magnetic resonance imaging scan indicated deltoid ligament injury; (E) Ankle valgus stress test was positive during surgery. (F, G) Suture‐anchor fixation of the deltoid ligament in postoperative X‐rays.
In 4 patients with a posterior malleolar fracture, the fragment size was >25% of the articular surface. These patients were positioned in the floating position. A tourniquet was placed on the proximal thigh. The affected extremity was routinely prepped from toe to knee in a sterile fashion and draped. Initially, the affected lower extremity was rotated laterally. A curved incision anteroinferior to the medial malleolus was made to explore the deltoid ligament and to place a 3.5‐mm TwinFix anchor (Shilehui Medical Product Int'l Trade [Shanghai]) for the next step. Then, the affected lower extremity was rotated medially. A longitudinal incision lateral to the fibula was made. The sural nerve was identified and protected. A blunt dissection was performed between the flexor hallucis longus muscle and the peroneal tendons to expose the fracture sites of the fibula and the posterior malleolus and to remove scar tissue from the fracture sites. Anatomic reduction was performed to restore the fibular rotation and length and posterior malleolus integrity. A reconstruction bone plate of proper length was attached to the posterior side of the fibula with screws. The posterior malleolus fracture was fixated using two cannulated screws (4.0 mm in diameter and 36.0 mm in length, Johnson & Johnson [China] Medical Equipment). The affected lower extremity was rotated laterally. Soft tissue was retracted from the medial incision to perform overlapping suture‐anchor fixation of the distal part of the superficial component of the ruptured deltoid ligament and the periosteum in the anterior colliculus portion of the medial malleolus. Good internal fixation and positioning were confirmed by X‐ray examination. The ankle external rotation test (at dorsiflexion of the foot) was performed to confirm ankle stability. The incision was closed in layers.
Postoperative Management
A short leg cast was used to fixate the lower extremity for 6 weeks after surgery. The cast was removed after 6 weeks, and partial weight‐bearing exercise was started. The affected extremity could bear full weight 10 weeks after surgery.
Results
General Outcome
A total of 84 patients with supination‐external rotation type IV ankle fractures had complete medical records and were included in this study. The average age of the patients was 44.16 years (range, 15–75). The patient sample included 39 males and 45 females. Overall, 49 patients were included in the medial malleolus fracture group. The average age of these patients was 40.20 years (range, 15–75). This patient group included 19 males and 30 females. Patients with a posterior malleolar fracture fragment >25% of the articular surface accounted for 81.6% (40 patients) of these patients. Overall, 35 patients were included in the deltoid ligament injury group. The average age of these patients was 44.21 years (range, 17–73). This patient group included 20 males and 15 females. Patients with a posterior malleolar fracture fragment >25% of the articular surface accounted for 11.5% (four patients) of these patients.
Follow‐up
The follow‐up endpoint was the time point when the steel plate and screws were removed from the lateral ankle in patients. The average follow‐up period was 13.4 months (range, 11–17). The Olerud–Molander ankle scoring system was used to assess postoperative ankle function. The average score for patients with medial malleolus fractures was 90.3 points (range, 85–95). In addition, the average score was 87.7 points (range, 80–95) in patients with deltoid ligament injuries. No significant differences were found in the scores between the two groups.
Discussion
Supination‐external rotation fractures are the most common type of ankle fracture according to the Lauge–Hansen classification and account for approximately 40%–70% of all ankle fractures3, 9. This type of ankle fracture is equivalent to the Weber B or type B fracture in the Danis–Weber classification and the AO/OTA fracture classification. Supination‐external rotation fractures can be classified into the following four types: type I, anterior tibiofibular ligament sprain; type II, anterior tibiofibular ligament sprain or avulsion fracture of the lateral malleolus tip combined with spiral fracture of the fibula below the level of the ankle joint; type III, type II plus posterior tibiofibular ligament rupture or posterior malleolus fracture; and type IV, type III plus medial malleolus fracture or deltoid ligament injury2.
Type IV injuries are unstable ankle fractures and have poor outcomes after conservative treatment; therefore, these fractures require surgical treatment. However, the clinical outcomes of medial structure injuries vary according to the type of injury. Tejwani et al. investigated 266 cases of supination‐external rotation type IV ankle fractures in a follow‐up study between 2000 and 20054. Of these cases, 163 were bilateral ankle fractures and 103 were lateral malleolus fractures with deltoid ligament injuries. The authors found that ankle function after surgery was poorer in patients with bilateral ankle fractures than those with lateral malleolus fractures with deltoid ligament injuries. The overall incidence of complications, including those resulting from the subsequent surgery to remove the internal fixation implants, was higher in patients with bilateral ankle fractures than in patients with lateral malleolus fractures plus deltoid ligament injuries. These results were consistent with those in the 3‐year follow‐up study by Kennedy et al.5. In addition, Stufkens et al. performed a 13‐year (average time) follow‐up study in 36 patients with supination‐external rotation type IV fractures and found that the treatment outcomes were better in patients with deltoid ligament injuries (regardless of partial or full injuries) than in patients with medial malleolus fractures6. In contrast, Berkes et al. found that treatment outcomes were similar between patients with deltoid ligament injury and patients with medial malleolus fractures in a follow‐up study of 108 patients with supination‐external rotation fractures7. A possible reason for the discrepancy may be that mini‐plates were used to fixate the posterior malleolus fractures regardless of the fracture fragment size in the study by Berkes et al.; therefore, the significance of predicting a prognosis based on the medial structure injury was limited. Donken et al. performed a 21‐year follow‐up study in 148 patients and found that the subjective and objective imaging scores were not significantly different between patients with medial malleolus fractures and patients with deltoid ligament injuries8. However, none of these studies proposed strategies for managing medial deltoid ligament injuries.
Management of Acute Deltoid Ligament Injury
The need for open reduction in the treatment of medial malleolus fractures remains controversial. In addition, the need for primary sutures and the selection of suture technique during the management of acute deltoid ligament injuries continues to be debated. Previous surgery has included fixation of the lateral malleolus and distal tibiofibular syndesmosis without management of the deltoid ligament. However, the ruptured deltoid ligament, which is curled in the medial ankle interval, may prevent ankle reduction. The non‐anatomical healing of the ligament may cause pain in the medial interval and ankle instability. The medial interval pain that patients with bilateral malleolus fractures experience may be caused by untreated deltoid ligament injuries. In the setting of lateral malleolus fracture, a 1956 experiment by Close revealed that the talus could be laterally shifted a distance of 3.7 mm only after the complete rupture of the superficial and deep components of the deltoid ligament10. In 1976, Harper showed that even in the setting of an intact lateral malleolus, the talus could tilt 11° and become unstable with deltoid ligament disruption11. Therefore, suturing the deltoid ligament may help to restore ankle stability. In recent years, greater attention has been paid to the management of acute deltoid ligament injury. In 1987, Baird and Jackson found that treatment of the deltoid ligament with suturing could achieve good results in patients with supination‐external rotation type IV injuries12. Boden et al. concluded that the medial deltoid ligament was the primary structure for ankle stability13. Thus, Maynou et al. suggested that exploration and ligament repair in the medial interval should be performed in patients with a medial interval greater than 3 mm14. Similarly, Jelinek and Porter suggested that repair of the deltoid ligament in the acute phase prevented late medial ankle instability and that medial ankle cartilage injuries could be detected during deltoid ligament repair15.
Hintermann classified acute deltoid ligament injury into the following three types according to the site of injury: type I, proximal insertion rupture, 72% of injuries; type II, middle ligament rupture, 9% of injuries; and type III, distal ligament insertion rupture, 19% of injuries16. Suture‐anchor fixation is recommended for deltoid ligament injuries and has been widely used in recent years16, 17. Between 2004 and 2014, Hsu et al. used suture‐anchor fixation for acute deltoid ligament repair in 14 National Football League (NFL) players18. All players had good outcomes without any complications; medial ankle pain and instability was not present. Similarly, in the current study, a curved incision anteroinferior to the medial malleolus was used to inspect the medial interval of the ankle, remove possible talar cartilage fragments and intra‐articular hematomas, and release the part of the deltoid ligament that was trapped in the medial interval. In addition, we performed overlapping suture‐anchor fixation of the superficial component of the deltoid ligament and the periosteum of the anterior colliculus portion of the medial malleolus. The anatomy of the superficial components of the deltoid ligament and the medial ankle interval returned to normal, which ensured healing of the deep deltoid ligament components at a reasonable tension and restoration of ankle stability.
Management of Posterior Malleolus Fractures
Supination‐external rotation type IV injuries are commonly accompanied by distal tibiofibular syndesmosis injury and posterior malleolus fractures. In 1960, over a period of more than 20 years, McLaughlin retrospectively analyzed a large number of patients with posterior malleolus fractures who underwent closed reduction and found that all patients with posterior malleolus fractures that involved more than 25% of the articular surface experienced posterior dislocation of the talus, which resulted in traumatic arthritis19. This phenomenon was observed regardless of the accuracy of the initial manual reduction or the type of external fixation used to maintain reduction. Therefore, McLaughlin proposed that involvement of 25% of the articular surface was a cut‐off point for performing internal fixation of posterior malleolus fractures. In 1977, McDaniel and Wilson found that the incidence of ankle subluxation increased and treatment efficacy decreased when the ankle fracture fragment size was >25% of the articular surface20. Therefore, the authors suggested that anatomic reduction and internal fixation should be used when the posterior malleolus fracture fragment size is >25% of the articular surface. In a previous study, Drijfhout van Hooff et al. divided 131 patients into three groups depending on the fragment size: <5%, 5%–25%, or >25%21. The average follow‐up period was 6.9 years (range, 2.5–15.9). Functional outcome measures recommended by the American Orthopaedic Foot and Ankle Society (AOFAS) and the American Academy of Orthopaedic Surgeons (AAOS), a visual analog scale (VAS), dorsiflexion restriction compared with the contralateral ankle, and the incidence of osteoarthritis on X‐ray were studied. The results revealed that the incidence of osteoarthritis was associated with the size of the posterior fracture fragment, which suggests that fixation for posterior fracture fragments >25% of the articular surface is effective. Therefore, in the current study, a CT scan was used to determine the proportion of the posterior malleolus fragment size to the distal tibial articular surface. Fixation with screws should be performed in patients with a proportion >25%. In addition, we found that patients with a posterior malleolus fracture fragment size >25% of the articular surface accounted for 81.6% of all patients in the medial malleolus fracture group, whereas only 4 patients had a posterior malleolus fracture fragment size >25% of the articular surface, which accounted for 11.5% of all 35 patients in the deltoid ligament injury group. Further statistical data are needed to confirm whether these results demonstrate that the force‐causing injury was more severe in the medial malleolus fracture group than in the deltoid ligament injury group.
Management of the Distal Tibiofibular Syndesmosis
The management of the distal tibiofibular syndesmosis in supination‐external type IV rotation injury remains controversial. Jones and Nunley demonstrated that subjective, functional, and radiologic outcomes were not different between screw fixation for the distal tibiofibular syndesmosis and suture‐anchor fixation for deltoid ligament injury in supination‐external rotation type IV fractures22. However, suture‐anchor fixation is cost‐effective and leads to fewer surgical risks during subsequent surgery to remove internal fixation implants. Hunt performed a 12‐month follow‐up study in 347 patients between 2000 and 2006 and found that postoperative ankle function was poorer in patients with screw fixation of the distal tibiofibular syndesmosis than in patients without fixation23. In addition, Miller et al. showed that postoperative ankle function improved slightly after the removal of screws for fixation of a distal tibiofibular syndesmosis24. In addition, clinical data have shown that screw position in 22%–52% of patients who undergo distal tibiofibular syndesmosis fixation is not accurate, which may lead to decreased range of motion in the ankle25, 26, 27. In 2015, a study by Schottel et al. revealed that deltoid ligament repair may be an alternative approach for screw fixation of the distal tibiofibular syndesmosis28. Therefore, screw fixation of the distal tibiofibular syndesmosis was not performed in the current study because the intraoperative stress test demonstrated ankle stability. This type of management ensured operative homogeneity between the two groups of patients and avoided costs due to subsequent surgery to remove implants and possible complications.
The follow‐up results in this study demonstrated no significant differences between the two groups of patients, regardless of the subjective, objective, and imaging outcomes. These results indicate that both surgical management of medial malleolus fractures and deltoid ligament injuries can achieve good results in terms of regaining ankle stability and anatomic reduction of the articular surface. The suture‐anchor technique for deltoid ligament fixation is helpful in the management of supination‐external rotation type IV fractures.
This study has limitations, such as the limited number of cases and the short follow‐up period. Large, multi‐center, high‐quality, randomized, controlled trials are needed to confirm the results of this study.
Disclosure: This study was supported by Project Supported by Xinjiang Autonomous Region Science and Technology Assistance Project (No. 201491190) and Project Supported by Natural Science Foundation of Shanghai (No. 15ZR1405500).
References
- 1. Switaj PJ, Weatherford B, Fuchs D, Rosenthal B, Pang E, Kadakia AR. Evaluation of posterior malleolar fractures and the posterior pilon variant in operatively treated ankle fractures. Foot Ankle Int, 2014, 35: 886–895. [DOI] [PubMed] [Google Scholar]
- 2. Lauge‐Hansen N. Fractures of the ankle IV. Clinical use of genetic roentgen diagnosis and genetic reduction. Arch Surg, 1952, 64: 488–500. [PubMed] [Google Scholar]
- 3. Van den Bekerom MP, Mutsaerts EL, van Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg, 2009, 129: 227–235. [DOI] [PubMed] [Google Scholar]
- 4. Tejwani N, McLaurin TM, Bhadsavle S, Koval K, Egol K. Are outcomes of bimalleolar fractures poorer than those of lateral malleolar fractures with medial ligamentous injury?. J Bone Joint Surg Am, 2007, 89: 1438–1441. [DOI] [PubMed] [Google Scholar]
- 5. Kennedy JG, Johnson SM, Collins AL, et al. An evaluation of the Weber classification of ankle fractures. Injury, 1998, 29: 577–580. [DOI] [PubMed] [Google Scholar]
- 6. Stufkens SA, Knupp M, Lampert C, van Dijk CN, Hintermann B. Long‐term outcome after supination‐external rotation type‐4 fractures of the ankle. J Bone Joint Surg Br, 2009, 91: 1607–1611. [DOI] [PubMed] [Google Scholar]
- 7. Berkes MB, Little MT, Lazaro LE, et al. Malleolar fractures and their ligamentous injury equivalents have similar outcomes in supination‐external rotation type IV fractures of the ankle treated by anatomical internal fixation. J Bone Joint Surg Br, 2012, 94: 1567–1572. [DOI] [PubMed] [Google Scholar]
- 8. Donken CC, Verhofstad MH, Edwards MJ, van Laarhoven CJ. Twenty‐one‐year follow‐up of supination‐external rotation type II‐IV (OTA type B) ankle fractures: a retrospective cohort study. J Orthop Trauma, 2012, 26: e108–e114. [DOI] [PubMed] [Google Scholar]
- 9. Pankovich AM. Applications to ankle trauma and areas of future clinical research In: Stiehl JB, ed. Inman's Joints of the Ankle. 2nd edn. Baltimore: Williams and Wilkins, 1991; 85–97. [Google Scholar]
- 10. Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am, 1956, 38: 761–781. [PubMed] [Google Scholar]
- 11. Harper MC. Deltoid ligament: an anatomical evaluation of function. Foot Ankle, 1987, 8: 19–22. [DOI] [PubMed] [Google Scholar]
- 12. Baird RA, Jackson ST. Fractures of the distal part of the fibula with associated disruption of the deltoid ligament. Treatment without repair of the deltoid ligament. J Bone Joint Surg Am, 1987, 69: 1346–1352. [PubMed] [Google Scholar]
- 13. Boden SD, Labropoulos PA, McCowin P, et al. Mechanical considerations for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am, 1989, 71: 1548–1555. [PubMed] [Google Scholar]
- 14. Maynou C, Lesage P, Mestdagh H, Butruille Y. Is surgical treatment of deltoid ligament rupture necessary in ankle fractures?. Rev Chir Orthop Reparatrice Appar Mot, 1997, 83: 652–657. [PubMed] [Google Scholar]
- 15. Jelinek JA, Porter DA. Management of unstable ankle fractures and syndesmosis injuries in athletes. Foot Ankle Clin, 2009, 14: 277–298. [DOI] [PubMed] [Google Scholar]
- 16. Hintermann B. Medial ankle instability. Foot Ankle Clin, 2003, 8: 723–738. [DOI] [PubMed] [Google Scholar]
- 17. Wang X, Ma X, Zhang C, Wang C, Huang JZ. Treatment of chronic deltoid ligament injury using suture anchors. Orthop Surg, 2014, 6: 223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int, 2015, 36: 1272–1278. [DOI] [PubMed] [Google Scholar]
- 19. McLaughlin HL. Trauma. Philadelphia: Saunders, 1960. [Google Scholar]
- 20. McDaniel WJ, Wilson FC. Trimalleolar fractures of the ankle. An end result study. Clin Orthop Relat Res, 1977, 122: 37–45. [PubMed] [Google Scholar]
- 21. Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. Influence of fragment size and postoperative joint congruency on long‐term outcome of posterior malleolar fractures. Foot Ankle Int, 2015, 36: 673–678. [DOI] [PubMed] [Google Scholar]
- 22. Jones CR, Nunley JA. Deltoid ligament repair versus syndesmotic fixation in bimalleolar equivalent ankle fractures. J Orthop Trauma, 2015, 29: 245–249. [DOI] [PubMed] [Google Scholar]
- 23. Hunt KJ. Syndesmosis injuries. Curr Rev Musculoskelet Med, 2013, 6: 304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miller AN, Paul O, Boraiah S, et al. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma, 2010, 24: 12–16. [DOI] [PubMed] [Google Scholar]
- 25. Tucker A, Street J, Kealey D, McDonald S, Stevenson M. Functional outcomes following syndesmotic fixation: a comparison of screws retained in situ versus routine removal – is it really necessary?. Injury, 2013, 44: 1880–1884. [DOI] [PubMed] [Google Scholar]
- 26. van den Bekerom MP, Lamme B, Hogervorst M, et al. Which ankle fractures require syndesmotic stabilization?. J Foot Ankle Surg, 2007, 46: 456–463. [DOI] [PubMed] [Google Scholar]
- 27. Manjoo A, Sanders DW, Tieszer C, Bolhuis HW. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma, 2010, 24: 2–6. [DOI] [PubMed] [Google Scholar]
- 28. Schottel PC, Baxter J, Gilbert S, Garner MR, Lorich DG. Anatomic ligament repair restores ankle and syndesmotic rotational stability as much as syndesmotic screw fixation. J Orthop Trauma, 2016, 30: e36–e40. [DOI] [PubMed] [Google Scholar]


