Abstract
Walking is a common activity among older adults. Fallers were discovered to have a higher propensity to conscious motor processing (reinvestment) than age-matched non-fallers, leading to movement disruption, possibly by constraining or interfering with automatic motor control mechanisms. However, gait rehabilitation programs by implicit motor learning methodologies may ameliorate reinvestment propensity while improving gait ability in older adults. One hundred and five older adults, with moderate to high risk of falling, will be recruited from different community centres in Hong Kong to investigate the effect of single-task, dual-task and analogy training (implicit motor learning methodologies) on walking during rehabilitation in the context of reinvestment propensity, balance, walking ability and fear of falling. Participants will be randomly allocated and received 12 training sessions in either a Single-task Walking Group (STWG), a Dual-task Walking Group (DTWG) or an Analogy Walking Group (AGWG). Reinvestment propensity, walking ability, balance and fear of falling will be assessed by the Chinese version Movement Specific Reinvestment Scale (MSRS-C), 10-meter Walk Test, Tinetti Balance Assessment Tool, Timed ‘Up & Go’ Test (TU&G), Berg Balance Scale (BBS) and 13-item Falls Efficacy Scale (FES-13), respectively at baseline before training (T0), just after completion of all training sessions (T1), and 6 months after completion of all training sessions (T2). Participants' number of falls between T1 and T2 will also be recorded. The results could establish a solid foundation for further development and implementation of a novel and effective gait rehabilitation program in fall prevention for older adults at risk of falling.
Keywords: Single-task training, Dual-task training, Analogy training, Gait rehabilitation, Older adults
1. Introduction
Walking is one of the commonest daily activities among older adults [1]. Healthy individuals are mostly capable of walking automatically, however, may use conscious motor processing when encountering movement difficulties or under stress [2]. Conscious motor processing involves the explicit processing of movement-related knowledge using working memory [3]. The process of switching from automatic motor processing to conscious explicit motor processing has been called ‘reinvestment’ [3,4]. “Reinvestment” was defined as “an inward focus of attention in which an attempt is made to perform the skill by consciously processing explicit knowledge of how it works” [4]. Previous evidence suggests that individuals, who are highly motivated to make successful movements or who are self-aware about the way in which they move (e.g., individual with movement difficulties), demonstrate an elevated propensity for conscious motor processing (reinvestment) in different populations with movement disorders, such as Parkinson diseases and Stroke [[5], [6], [7], [8], [9], [10]]. It was discovered that older fallers have a higher propensity to reinvest (conscious motor control) than age-matched non-fallers [11]. More importantly, conscious motor processing (reinvestment) may lead to movement disruption, possibly by constraining or interfering with automatic motor control mechanisms [12,13]. Focusing internally may also interfere with the allocation of attention for navigation of the environment and/or multitasking, further increasing the risk of falling of older adults [14]. These difficulties may be exacerbated in demanding situations in which attentional capacity is further overloaded. Previous studies discovered that older fallers have a higher tendency to divide their attention between the internal mechanisms of their movements and external environment, whereas older non-fallers mainly focus externally during walking [14]. Efforts to attend both internal and external information by older fallers may overload resources in the working memory [15], which may affect the movement control during walking.
However, no research has investigated a potential intervention to ameliorate the propensity for conscious motor processing (reinvestment) in older adults. Such intervention is expected to yield better rehabilitation outcomes during gait rehabilitation programs by Physiotherapists. Indeed, methods to minimize the predisposition to reinvest during gait re-education could be derived from previous implicit motor learning literature. Implicit learning is the process of acquiring knowledge largely independently of awareness of both the process and the products of acquisition, whereas explicit learning requires consciousness and learning of explicit rules [16]. Motor skills can be learned implicitly or explicitly [4,17]. Implicit motor learning via a concurrent cognitive secondary task (dual-task training) or by a biomechanical metaphor (analogy training) may decrease the propensity for conscious motor processing (reinvestment) in older adults at risk of falling by distracting/preventing them from reinvestment (e.g., dual-task training) or by minimizing the accumulation of explicit rules that may overload the working memory during motor learning or relearning (e.g., analogy training), respectively [4,18].
The current study represents the first attempt to investigate the effect of single-task, dual-task and analogy training (implicit motor learning methodologies) during gait rehabilitation in the context of conscious motor processing (reinvestment) propensity, balance, walking ability and fear of falling by older adults at risk of falling. It is hypothesized that older adults who completed the dual-task or analogy training will have lower conscious motor processing (reinvestment) propensity and demonstrate better rehabilitation outcomes than older adults who completed the single-task training (active control group). The rehabilitation outcomes of, for example, conscious motor processing (reinvestment) propensity, walking ability, gait & balance, fear of falling, and numbers of recurrent falls will be investigated.
2. Method
2.1. Design
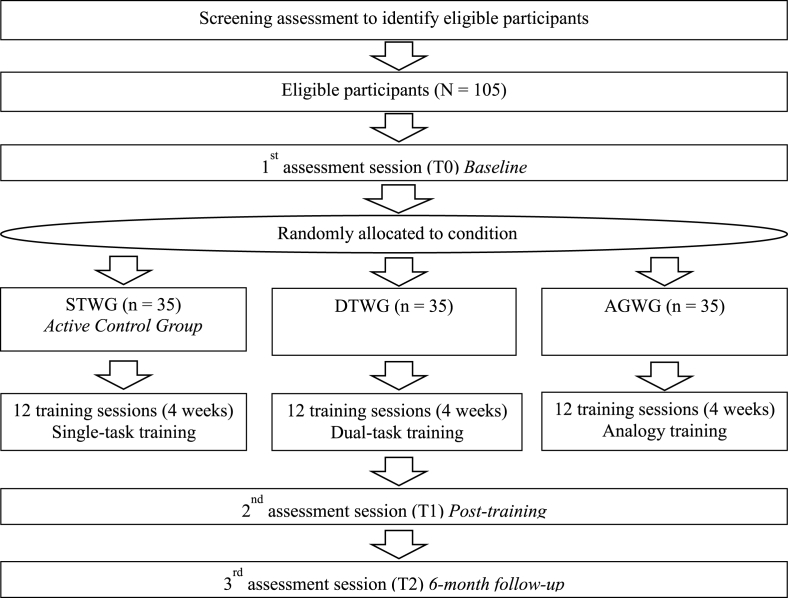
A three-arm, parallel group, and randomized trial will be conducted in Hong Kong. Participants will be randomly allocated into either: 1, Single-task Walking Group (STWG) – an active control group; 2, Dual-task Walking Group (DTWG) or 3, Analogy Walking Group (AGWG). Assessments will be conducted at baseline before training (T0), just after completion of all training sessions (T1), and 6 months after completion of all training sessions (T2) (Fig. 1).
Fig. 1.
Schematic diagram of the study design (randomized controlled trial).
2.2. Participants
One-hundred and five older adults will be recruited from elderly community centres in Hong Kong by convenience sampling. The inclusion criteria are: (1) Age 65 or above; (2) No history of cerebral vascular disease, Parkinson's disease or other neurological deficit; (3) Chinese version of the Mini–Mental State Examination (MMSE-C) [19,20] total score of equal or more than 24; (4) Able to walk independently indoor for at least 10 m; (5) Older adults with moderate to high risk of falling, as indicated by the score of less than 24 out of 28 in the Tinetti Balance Assessment Tool [21].
2.3. Randomisation and intervention conditions
An independent person will randomly assign the participants (N = 105), who meet the inclusion criteria, by concealed block randomization with a sealed and opaque envelope system to either a Single-task Walking Group (STWG, n = 35), a Dual-task Walking Group (DTWG, n = 35) or an Analogy Walking Group (AGWG, n = 35). A computerized random-number generator will be used to formulate an allocation schedule. The independent person will also be responsible for arranging the exercise training schedules for all participants.
Participants in the STWG, DTWG and AGWG will receive different instructions during walking training. The instructions were developed by an expert group of Physiotherapists who are experienced in geriatric exercise training. Before the start of the 12 training sessions, participants in different groups will be invited to participate in their own group's pre-training session in which they will be clearly explained about the walking instruction in their own specific group. All participants can therefore be able to learn the specific walking instruction in an earlier session, aiming to ensure their comprehensive understanding.
2.3.1. Single-task walking group
In the STWG, expertly-designed explicit instruction will be used to instruct the participants during walking (i.e., the comprehensive explicit therapeutic instructions). As usual practice, the explicit instruction depends on the walking ability of our participants (e.g., “please walk with bigger steps and more even weight-bearing on both feet”).
2.3.2. Dual-task walking group
In the DTWG, expertly-designed dual-task instruction will be utilized (i.e., walk with a concurrent cognitive dual-task of counting backward by 3's from different randomized 2-digit numbers).
2.3.3. Analogy walking group
In the AGWG, participants will walk with an analogy instruction (i.e., imagine you are kicking a ball in front of you).
2.4. Procedures
In a prior pilot study of expert focus group with experienced Physiotherapists in Hong Kong, the research team has developed the culturally appropriate single-task, dual-task and analogy instructions, together with training protocols during the rehabilitation program. Our pilot randomized controlled study also ascertained the training feasibility, effectiveness and safety. The current proposed study is the imperative step to further investigate a novel and potentially influential fall rehabilitation method.
At the first meeting with participants, the study protocol and informed consent form will be described in detail, where all participants will be offered the opportunity to review and ask questions. Ethical approval and written consent will be obtained prior to the research procedure.
All participants will participate in three training sessions (about 45 min each) per week for 4 weeks, in small groups of 5 participants. A total of 12 sessions will be completed. In each training session, all groups will have warm-up (5 min), balance training (5 min), body transport training (5 min), body transport with hand manipulation training (5 min), walking training with various difficulties (e.g., different walking surfaces) in a 10-meter walkway with different instructions according to their allocated walking groups (20 min) and cool down (5 min). The training protocols have been proved to be safe and feasible by our pilot study. All training sessions will be conducted by experienced Hong Kong registered Physiotherapists with experience in exercise training for older adults.
2.5. Assessments
Each participant will undergo assessment sessions (total 3 assessment sessions) at baseline before training (T0), just after completion of all training sessions (T1) and 6 months after completion of all training sessions (T2). During the baseline assessment (T0), a structural questionnaire will be used to ask for demographics, detailed history of fall incident, detailed medical history, social history and social-economic status of the participants. A battery of assessments will be conducted to assess physical and cognitive abilities of the participants in all assessment sessions (T0, T1 & T2).
2.6. Primary outcome
2.6.1. Conscious motor processing (reinvestment) propensity
The primary outcome of the study is conscious motor processing (reinvestment) propensity. The Chinese version Movement Specific Reinvestment Scale (MSRS-C) will be administered to assess the propensity for conscious processing of movements (reinvestment). MSRS-C is a valid and reliable measurement of the conscious motor processing (reinvestment) propensity in Chinese older population in Hong Kong, which was found to be a potential risk factor of falls [22]. The Scale contains 10 items and comprises two separate factors (i) movement self-consciousness and (ii) conscious motor processing. Examples of items from the MSRS-C include, “I am self-conscious about the way I look when I am moving” and “I am aware of the way my body works when I am carrying out a movement”, which aim to assess movement self-consciousness and conscious motor processing, respectively.
2.7. Secondary outcomes
2.7.1. Walking ability
Single-task and dual-task walking abilities will be measured. Single-task walking ability will be assessed by 10 m comfortable and fast walking speed [23]. Dual-task walking ability will be determined by 10 m comfortable and fast walking speed with concurrent verbal or visual-spatial dual-tasks of auditory stroop task [24] or clock test [25], respectively. The dual-task effect on gait speed will be calculated from the difference between single-task and dual-task walking speed.
2.7.2. Gait & balance
Functional gait and balance will be assessed by the Tinetti Balance Assessment Tool [21], Timed ‘Up & Go’ Tests (TU&G) [26] and the Berg Balance Scale (BBS) [27]. The Tinetti Balance Assessment tool is a valid, reliable and easy administered test that can measure gait (12 points) and balance (16 points) components (i.e., total score of 28 points) at the same time [21]. The TU&G requires participants to stand up from a chair, walk 3 m at a comfortable pace, turn around, walk back for 3 m, turn around and then sit down on the chair. The time taken to complete the whole procedure will be recorded. The TU&G demonstrates good reliability and validity with discriminative and predictive properties [26,28]. The BBS is a highly valid and reliable scale to assess balance [27]. It consists of 14 items of tasks in which participants need to maintain balance in performing the tasks. Each item can be scored 0 to 4 marks giving a maximum total score of 56.
2.7.3. Fear of falling
The Falls Efficacy Scale (FES-13) [[29], [30], [31]] will be completed to assess the fear of falling. The FES-13 is a valid and reliable subjective evaluation scale, which measures self-efficacy of the respondent at avoiding a fall in performing each of the 13 non-hazardous daily activities in the scale. Each item can be scored from 0 to 10 points with a higher score representing higher efficacy or confidence [31].
2.7.4. Recurrent falls
All participants will be asked to record their number of falls prospectively at the time between T1 (completion of all training sessions) and T2 (6 months after completion of all training sessions) using a calendar. Once they have any fall incident, participants will record it at his/her individual calendar prospectively. The number of falls within the 6-month follow-up period will then be collected retrospectively.
2.8. Ethics approval and clinical trial registration
Ethical approval was obtained from the Institutional Review Board of the University of Hong Kong/ Hospital Authority Hong Kong West Cluster (IRB no.: UW17-049). The informed consent will be obtained for eligible participants. At the first meeting with all participants, the study protocol and informed consent form will be described in detail, where all participants will be offered the opportunity to review and ask questions. The trial was prospectively registered in the ClinicalTrials.gov (NCT03811782).
2.9. Statistical analysis
Analysis of variance with repeated measures and follow-up tests, for example correlation analysis, will be employed to investigate the between group differences (STWG, DTWG and AGWG) and within group differences (T0, T1 and T2) in the primary outcome variable (i.e., propensity for conscious motor processing (reinvestment)) and all the other secondary outcome variables that related to older adult falls (i.e., single- and dual-task walking abilities, scores of the functional gait and balance assessments and fear of falling). Fall rate at the 6-month follow-up period will be examined using the survival analysis. For example, we may analyse the expected duration of time one or more fall incidents happen.
2.10. Sample size
An effect size of 0.31 was calculated from the pilot study for the primary outcome of conscious motor processing (reinvestment) propensity, as measured by the MSRS-C [22,32,33], which suggests that a sample size of n = 28 participants per group would provide sufficient power for the study to detect groups’ differences. To be conservative, the study plans to recruit n = 35 participants per group given that the drop-out rate might be around 20 to 30% for a similar type of randomized controlled trial.
3. Discussion
Walking is an essential activity in daily life, older adults with fall history may be more prone to recurrent falls due to their higher propensity in conscious motor processing (reinvestment) [11,34]. Hence, gait rehabilitation strategies should not only aim to re-educate older adults’ gait functioning, but also reduce their propensity to reinvest while walking. The current study aims to examine the effect of single-task, dual-task and analogy training during gait rehabilitation on conscious motor processing (reinvestment) propensity, balance, walking ability and fear of falling in older adults at risk of falling in Hong Kong. The study design was formulated based on two prior pilot studies (a focus group study and a pilot randomized controlled trial). However, one potential limitation of this study is that we cannot be able to quantify the potential effect of body balance and transport trainings without dual-tasking as we focus on examining the manipulation of single-task, dual-task and analogy instructions during walking training only.
The current study aims to compare the group differences (STWG, DTWG and AGWG) and within group differences (T0, T1 and T2) in the primary outcome variable (i.e., conscious motor processing (reinvestment) propensity) and all the other secondary outcome variables related to older adult falls (i.e., single- and dual-task walking abilities, scores of the functional gait and balance assessments and fear of falling). Previous meta-analysis has shown that appropriate group-based exercise could improve balance. Therefore, it is believed that participants of all groups will show improvement in single- and dual-task walking abilities, scores of the functional gait and balance assessments and fear of falling upon the completion of the gait rehabilitation program [34]. However, since explicit learning by single-task walking training (i.e., STWG) could possibly increase conscious motor processing (reinvestment) propensity, which may lead to constraining or interfering with automatic motor control mechanisms [13]. Participants in the STWG are expected to demonstrate smaller improvements in different rehabilitation outcomes (e.g., conscious motor processing (reinvestment) propensity, walking ability, gait & balance, fear of falling, and numbers of recurrent falls) than that of the DTWG and AGWG. Furthermore, as the potential effect of the dual-task and analogy training is to reduce conscious motor processing (reinvestment) propensity, participants of the two groups are predicted to display long-term reduction in conscious motor processing (reinvestment) propensity 6 months after the end of the gait rehabilitation program (T2). Further correlational analysis may also show that conscious motor processing (reinvestment) propensity correlates with different fall risk outcomes (e.g., single- and dual-task walking abilities, scores of the functional gait and balance assessments and fear of falling) as previous studies indicated that older fallers had a higher tendency to reinvest than non-fallers [11].
The findings of the current study will have extremely high practical implications for fall rehabilitation. Through better understanding of the single-task, dual-task and analogy training in gait rehabilitation, we can design novel interventions for fall rehabilitation aiming to reduce risk of falling in older adults, by means of different implicit learning methods (e.g., analogy and dual-task training), to ameliorate the predisposition for conscious motor processing (reinvestment). The current study therefore has manifest potential to further enhance the rehabilitation outcome of fall rehabilitation programs implemented in Hong Kong. One of the main strengths of the current study is that the sample size is large for the similar type of study in psychomotor rehabilitation and such a randomized control trial could provide strong evidence for implementing effective gait rehabilitation program to older adults with moderate to high risk of fall in clinical settings. Although this study may demonstrate the change in conscious motor processing (reinvestment) propensity after the gait rehabilitation program, one potential limitation of this study is that the real-time conscious motor processing (real-time reinvestment) will not be measured during and after the training as we will follow the feasible protocol of our pilot study. Therefore, it may not be able to provide comprehensive evidence to demonstrate how dual-task and analogy training could affect real-time conscious motor processing (reinvestment) after the training sessions. Future studies could examine and compare the level of real-time conscious motor processing (reinvestment) of older adults while completing the training in the different gait rehabilitation programs (i.e. single-task walking, dual-task walking and analogy walking training).
4. Conclusion
The current proposed study will possibly provide solid evidence demonstrating the potential effects of single-task, dual-task and analogy training during gait rehabilitation on conscious motor processing (reinvestment) propensity, balance, walking ability and fear of falling by older adults at risk of falling in Hong Kong. It may suggest that implicit motor learning could be a feasible and effective intervention in daily rehabilitation, by a novel and simple method of modifying instructions to patients during training, through implementating gait re-education with a concurrent cognitive secondary task or by analogy learning.
Funding source
This research is funded by the General Research Fund, Hong Kong Research Grants Council (Grant Number: 17603318) of the Hong Kong Special Administrative Region, China.
Clinical trial registration
ClinicalTrials.gov Identifier: NCT03811782.
Conflicit of interest
The authors declare no competing interests.
Acknowledgements
The author gratefully thanks our collaborators Ms. Ng Ada Fong Ting, Professor Rich Masters and Dr. Catherine Capio for their support and advice during writing of the proposal for funding application.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100398.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lai P.C., Low C.T., Wong M., Wong W., Chan M.H. Spatial analysis of falls in an urban community of Hong Kong. Int. J. Health Geogr. 2009;8:14. doi: 10.1186/1476-072X-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hauer N., Specht N., Schuler M., Bärtsch P., Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Aging. 2002;31:49–57. doi: 10.1093/ageing/31.1.49. [DOI] [PubMed] [Google Scholar]
- 3.Masters R.S.W., Maxwell J. The theory of reinvestment. Int. Rev. Sport Exerc. Psychol. 2008;1:160–183. [Google Scholar]
- 4.Masters R.S.W. Knowledge, nerves and know-how: the role of explicit versus implicit knowledge in the breakdown of a complex motor skill under pressure. Br. J. Psychol. 1992;83:343–358. [Google Scholar]
- 5.Masters R.S.W., Polman R.C.J., Hammond N.V. ‘Reinvestment’: a dimension of personality implicated in skill breakdown under pressure. Pers. Indiv. Differ. 1993;14:655–666. [Google Scholar]
- 6.Orrell A., Masters R.S.W., Eves F.F. 'Reinvestment': a dimension of the stroke personality? Neurorehabilitation Neural Repair. 2002;16:S108. [Google Scholar]
- 7.Fasotti L., Kovacs F. Slow information processing and the use of compensatory mechanisms. In: Chamberlain M.A., Neumann V., Tennant A., editors. Traumatic Brain Injury Rehabilitation Service, Treatments and Outcomes. Chapman & Hall; London: 1995. pp. 141–152. [Google Scholar]
- 8.Stapleton T., Asburn A., Stack E. A pilot study of attention deficits, balance control and falls in the subacute stage following stroke. Clin. Rehabil. 2001;15:437–444. doi: 10.1191/026921501678310243. [DOI] [PubMed] [Google Scholar]
- 9.Grattan L.M., Ghahramanlou M., Aronoff J., Wozniak M.A., Kittner S.J., Price T.R. An empirical study of personality change after stroke. Stroke. 2001;32:318. [Google Scholar]
- 10.Masters R.S.W., Pall H.S., MacMahon K.M.A., Eves F.F. Duration of Parkinson's disease is associated with an increased propensity for ‘reinvestment’. Neurorehabilitation Neural Repair. 2007;21:123–126. doi: 10.1177/1545968306290728. [DOI] [PubMed] [Google Scholar]
- 11.Wong W.L., Masters R.S.W., Maxwell J.P., Abernethy A.B. Reinvestment and falls in community-dwelling older adults. Neurorehabilitation Neural Repair. 2008;22:410–414. doi: 10.1177/1545968307313510. [DOI] [PubMed] [Google Scholar]
- 12.Wulf G., Shea C.H., Park J.H. Attention in motor learning: Preferences for and advantages of an external focus. Res. Q. Exerc. Sport. 2001;72:335–344. doi: 10.1080/02701367.2001.10608970. [DOI] [PubMed] [Google Scholar]
- 13.McNevin N.H., Shea C.H., Wulf G. Increasing the distance of an external focus of attention enhances learning. Psychol. Res. 2003;67:22–29. doi: 10.1007/s00426-002-0093-6. [DOI] [PubMed] [Google Scholar]
- 14.Wong W.L., Masters R.S.W., Maxwell J.P., Abernethy B. The role of reinvestment in walking and falling in community-dwelling older adults. J. Am. Geriatr. Soc. 2009;57:920–922. doi: 10.1111/j.1532-5415.2009.02228.x. [DOI] [PubMed] [Google Scholar]
- 15.Baddeley A.D. Psychology Press; UK: 1994. Essentials of Human Memory. [Google Scholar]
- 16.Sternberg R.J. MIT Press; Cambridge: 1999. The Nature of Cognition. [Google Scholar]
- 17.Berry D.C., Broadbent D.E. Interactive tasks and the implicit-explicit distinction. Br. J. Psychol. 1988;79:251–272. [Google Scholar]
- 18.Masters R.S.W. Theoretical aspects of implicit learning in sports. Int. J. Sport Psychol. 2000;31:530–541. [Google Scholar]
- 19.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-Mental State” A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Chiu H.F.K., Lee H.C., Chung W.S., Kwong P.K. Reliability and validity of the Cantonese version of mini-mental state examination – a preliminary study. J. Hong Kong Coll. Psychiatrists. 1994;4(Suppl 2):25–28. [Google Scholar]
- 21.Tinetti M.E. Performance-Oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986;34:119–126. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- 22.Masters R.S.W., Eves F.F., Maxwell J. ISSP 11th World Congress of Sport Psychology, Sydney, Australia. 2005. Development of a movement specific reinvestment scale. [Google Scholar]
- 23.Bohannon R.W. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age. Ageing. 1997;26:15–19. doi: 10.1093/ageing/26.1.15. [DOI] [PubMed] [Google Scholar]
- 24.Siu K.C., Catena R., Chou L.S., van Donkelaar P., Woollacott M. Effects of a secondary task on Obstacle avoidance in healthy young adults. Exp. Brain Res. 2008;184:115–120. doi: 10.1007/s00221-007-1087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plummer-D’Amato P., Altmann L.J.P., Saracino D., Fox E., Behrman A.L., Marsiske M. Interactions between cognitive tasks and gait after stroke: a dual task study. Gait Posture. 2008;27:683–688. doi: 10.1016/j.gaitpost.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Podsiadlo D., Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 27.Berg K., Wood-Dauphinee S., Williams J.I., Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother. Can. 1989;41:304. [Google Scholar]
- 28.Shumway-Cook A., Brauer S., Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed up & Go test. Phys. Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 29.Tinetti M.E., Leon C.F.M., Doucette J.T., Baker D.I. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J. Gerontol. 1994;49(3):M140–M147. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 30.Tinetti M.E., Richman D., Powell L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990;45(6):239–243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 31.Hellström K., Lindmark B. Fear of falling in patients with stroke: a reliability study. Clin. Rehabil. 1999;13:509–517. doi: 10.1191/026921599677784567. [DOI] [PubMed] [Google Scholar]
- 32.Wong T.W.L., Abernethy A.B., Masters R.S.W. Enhancement of the movement. Specific reinvestment scale in older adults. J.Gerontopsychology Geriatr. Psychiatry. 2015;28(3):137–141. [Google Scholar]
- 33.Wong T.W.L., Abernethy A.B., Masters R.S.W. Instructions influence response to the Chinese version movement specific reinvestment scale (MSRS-C) in community- dwelling older adults. Geriatr.Gerontol. Int. 2015;4 doi: 10.1111/ggi.12644. [DOI] [PubMed] [Google Scholar]
- 34.Sherrington C., Whitney J.C., Lord S.R., Herbert R.D., Cumming R.G., Close J.C. Effective exercise for the prevention of falls: a systematic review and meta‐analysis. J. Am. Geriatr. Soc. 2008;56(12):2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.