Abstract
BACKGROUND:
Food insecurity is believed to affect the quality and quantity of foods consumed; however, studies examining food insecurity and diet quality have been inconclusive and few studies have explored variability in these associations by sex and race/ethnicity.
OBJECTIVE:
This study examined associations between food insecurity and diet quality, and variations by sex and race/ethnicity.
DESIGN:
Cross-sectional analysis of data from the 2011–14 National Health and Nutrition Examination Surveys (NHANES).
PARTICIPANTS:
The study population was comprised of 4,393 adults (20–65 years) with family incomes ≤300% of the federal poverty level with complete data on household food security and dietary intake via two 24-hour dietary recalls.
MAIN OUTCOME MEASURES:
Diet quality was assessed using the Healthy Eating Index (HEI)-2015.
STATISTICAL ANALYSIS PERFORMED:
Associations between food security and HEI-2015 total and component scores were examined using linear regression models and generalized linear models. Models adjusted for sociodemographic and health covariates.
RESULTS:
Compared to food secure adults, food insecure adults reported a 2.22-unit lower HEI-2015 score (95% CI −3.35, −1.08). This association was most pronounced among Non-Hispanic (NH) Whites and adults of Asian or “Other” races/ethnicities. There were no associations among NH Black or Hispanic adults, and no differences by sex. Among NH Whites, food insecurity was associated with lower scores for total protein foods, seafood and plant proteins, and added sugar. Among Asians, food insecurity was associated with lower scores for whole fruit.
CONCLUSION:
Food insecurity was associated with lower diet quality primarily among NH Whites, Asians, and “Other” adults, a group compris ed of American Indian or Alaska Natives, Native Hawaiian or Other Pacific Islanders and multi-racial adults. Further research is needed to better understand the nature of this association among understudied racial/ethnic groups.
Keywords: food insecurity, diet quality, race/ethnicity, National Health and Nutrition Examination Surveys
INTRODUCTION
Food insecurity, the household-level condition of limited or uncertain access to adequate and nutritious food, has persisted in the United States since the first national report was released in 1995.1 Over the past decade, food insecurity levels have increased to 14% in response to the Great Recession, recovering only in recent years to pre-recession levels.2 In 2017, the national prevalence of food insecurity was estimated at 11.8%, affecting 40 million people.2 Food insecurity disproportionately affects households with children, adults living alone, and individuals of minority race/ethnicity.2
Although food insecurity has been shown to affect numerous health behaviors and health conditions, at the core of the understanding of food insecurity is its impact on disrupted eating patterns and nutritional inadequacy. It is captured in the USDA definition of food insecurity that the “quality, variety, or desirability” of foods co nsumed is reduced.3 Despite this conceptualization, the evidence of food insecurity and diet quality has been inconclusive. In a systematic review published in 2014, Hanson and Connor found 170 tested associations between food insecurity and dietary intake – of these, 50 s uggested an adverse association, while 97 showed no association.4 Many of the tested associations focused on macronutrients and micronutrients, and some examined individual foods or food groups. Only four studies included measures of overall diet quality, of which the results were evenly split between an adverse association and no association.5–8 Since then, few studies have continued to investigate the association between food insecurity and diet quality at the population level, even though there have been recent shifts in national levels of food insecurity and changes to the dietary guidelines that drive the measurement of overall diet quality.9, 10 Furthermore, no study has investigated how the food insecurity and diet quality association varies by demographic characteristics in a heterogeneous sample of adults.
The objective of this present study was to examine the association between household food insecurity and dietary quality using a recent and nationally representative sample of US adults. Differences in these associations were examined by sex, as many studies have found stronger associations with physical health outcomes among females compared to males.5, 11, 12 Differences by race/ethnicity were also examined, as national reports have highlighted disparities in levels of food insecurity and poor dietary quality in minority racial/ethnic households.2, 13, 14 It was hypothesized that household food insecurity would be inversely associated with diet quality and that this association would be stronger for minority racial/ethnic households.
MATERIALS AND METHODS
Study Population
The National Health and Nutrition Examination Surveys (NHANES) is an ongoing, multistage survey designed to be representative of the civilian, noninstitutionalized US population.15 Administered by the National Center for Health Statistics, NHANES collects information on demographics, health behaviors, dietary intake, weight, and biomarkers related to major chronic disease using interviews, examinations, and laboratory tests. Data from 2011–12 and 2013–14 were combined in the present study. The analytic population was restricted to 4,393 adults (ages 20–65 years) and family incomes ≤300% of the federal poverty level (FPL).16 The present analysis focused on non-elderly adults as children and older adults have different nutritional needs and may have different experiences of household food insecurity. The analysis was also restricted to adults with family incomes at ≤300% FPL to be inclusive of the individuals at risk for food insecurity who are known to be in relatively higher income thresholds,2 and to reduce potential confounding by family income on the association between household food insecurity and dietary quality. Secondary analysis of publicly available NHANES data was considered exempt from further IRB review by the University of Michigan Institutional Review Board – Health Sciences and Behavioral Sciences.
Measures
The primary exposure of interest was household food insecurity, measured using the 18-item US Food Security Survey Module. The module assesses individual and household-level experiences and behaviors related to food purchasing, food availability, and diet over the past 12 months. A score of 0–18 was created by summing the affirmative responses of the 18 questions, with higher scores indicating worse food insecurity. Food insecurity categories were assigned according to USDA guidelines: 0, food secure, 1–2, marginally food secure, and 3 or more, food insecure.17
The outcome of interest was overall diet quality, measured by the Healthy Eating Index (HEI)-2015. Among NHANES participants, dietary intake was assessed using one or two 24-hour dietary recalls using the Automated Multiple Pass Method, the first of which was conducted in the Mobile Examination Center and the second over the phone.18 To reduce the potential for misreporting in dietary intake, recalls with total energy intakes <500 or >5000 kcal were excluded from the analyses (n=288). The application of this approach in studies of diet and health outcomes has been shown to be identical to other methods of accounting for implausible energy intake;19 however, the criteria applied in the present study were expanded to account for the increased variability that could arise from 24-hour dietary recalls.20, 21 The HEI-2015 was developed through a collaboration between USDA and the National Cancer Institute to measure adherence to the 2015–2020 Dietary Guidelines for Americans.22 Scored out of 100 points, the HEI-2015 is comprised of 13 individual components: total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and saturated fats. With the exception of the last four components which are reverse scored, higher points are awarded for higher consumption of all individual components. Maximum scores for total fruits, whole fruits, total vegetables, greens and beans, total protein foods, and seafood and plant proteins are 5 points; maximum scores for all other components are 10 points. HEI-2015 total and component scores were calculated according to the simple HEI scoring algorithm using publicly-available SAS macros from the National Cancer Institute.23
Covariates included in the analysis to adjust for potential confounding included age (in 5-year categories), sex, race/ethnicity (non-Hispanic (NH) White, NH Black, Mexican American or other Hispanic, Asian, or NH other/multi-race), birthplace (US born, foreign born), educational attainment (<12 years, high school diploma or equivalent, some college, college graduate), marital status (married or living with partner, never married, or separated/ widowed/ divorced), family income as a ratio to the federal poverty level (FPL) (in 50% FPL increments), and smoking status (never smoker, former smoker, current smoker). All covariates were self-reported and were selected as potential confounders of the association between food insecurity and dietary quality. Individuals with missing data for family income (n=746) were represented with missing indicators. Individuals with missing data for educational attainment (n=10), marital status (n=4) and smoking (n=3) were excluded from the analysis due to the small number of cases.
Statistical analysis
Complex sampling weights for the dietary subsample were used to account for different sampling probabilities and participation rates across the four-year period. Sociodemographic characteristics by household food insecurity status were compared using χ2 tests for categorical variables and univariate regression for continuous variables. Multivariable linear regression models were used to examine absolute differences in HEI-2015 total scores by household food insecurity, adjusting for all covariates. Generalized linear models with a gamma distribution and log-link function were used to estimate relative differences of HEI-2015 component scores by food insecurity categories. A gamma distribution was used to accommodate the fact that the dietary component data were non-negative and highly skewed to the right.24 Relative differences can be interpreted as the percentage difference between groups. All analyses were further stratified by sex and race/ethnicity. Race/ethnicity categories included NH White, NH Black, Mexican American or other Hispanic, Asian, and NH “Other.” Heterogeneity by sex and race/ethnicity was determined using Wald tests of the cross-product terms between sex and race/ethnicity with household food insecurity.
Statistical tests were 2-sided and significance was considered at P <0.05. Statistical analyses were performed with SAS 9.325 and Stata/ SE 12.126.
RESULTS
Of the 4,393 adults with family incomes ≤300% of the federal poverty level, using weighted proportions from NHANES, 55.7% were food-secure, 14.6% were marginally food-secure, and 29.6% were food-insecure over the past 12 months. Compared to food-secure adults, marginally food-secure and food-insecure adults were younger, were more likely to be NH Black or Hispanic, had lower educational attainment and family incomes, and more likely to be a current smoker (Table 1).
Table 1:
Sociodemographic and health characteristics of 4,393 adults with family incomes ≤300% of the federal poverty level - NHANES 2011–14
| Food secure (n=2292) | Marginally food secure (n=697) | Food insecure (n=1404) | P-valuea | ||||
|---|---|---|---|---|---|---|---|
| n | Weighted %b | n | Weighted %b | n | Weighted %b | ||
| Age in years, mean (SE) | 40.7 (0.8) | 39.6 (0.8) | 39.3 (0.7) | 0.007 | |||
| Sex | 0.87 | ||||||
| Men | 1097 | 47.8 | 312 | 46.8 | 640 | 46.6 | |
| Women | 1195 | 52.2 | 385 | 53.2 | 764 | 53.4 | |
| Race/ethnicity | <0.001 | ||||||
| Non-Hispanic White | 849 | 58.8 | 205 | 45.6 | 490 | 47.5 | |
| Non-Hispanic Black | 570 | 14.6 | 189 | 16.5 | 381 | 18.1 | |
| Hispanic | 542 | 18.2 | 214 | 27.7 | 426 | 28.4 | |
| Asian | 263 | 5.8 | 56 | 4.6 | 49 | 2.0 | |
| Otherc | 68 | 2.6 | 33 | 5.8 | 58 | 3.9 | |
| Birthplace | 0.58 | ||||||
| US born | 1579 | 78.2 | 468 | 75.3 | 1006 | 76.5 | |
| Foreign born | 713 | 21.8 | 229 | 24.7 | 398 | 23.5 | |
| Educational attainment | <0.001 | ||||||
| <12 years | 528 | 17.6 | 195 | 23.9 | 447 | 29.8 | |
| High school diploma or equivalent | 546 | 26.3 | 186 | 27.6 | 391 | 29.3 | |
| Some college | 796 | 35.3 | 240 | 36.5 | 460 | 33.6 | |
| College graduate | 422 | 20.9 | 76 | 12.0 | 106 | 7.3 | |
| Marital status | 0.14 | ||||||
| Married or living with partner | 1254 | 56.5 | 368 | 51.0 | 706 | 51.2 | |
| Never married | 611 | 26.8 | 176 | 28.6 | 393 | 27.4 | |
| Separated, divorced, or widowed | 427 | 16.7 | 153 | 20.4 | 305 | 21.4 | |
| Poverty income ratio | <0.001 | ||||||
| 0–50% federal poverty level | 186 | 7.5 | 95 | 12.9 | 257 | 16.2 | |
| 50.1–100% federal poverty level | 403 | 15.6 | 188 | 25.1 | 435 | 29.6 | |
| 100.1–150% federal poverty level | 477 | 19.4 | 167 | 22.4 | 350 | 24.4 | |
| 150.1–200% federal poverty level | 340 | 14.5 | 96 | 17.0 | 132 | 11.2 | |
| 200.1–250% federal poverty level | 282 | 15.4 | 52 | 7.6 | 89 | 7.7 | |
| 250.1–300% federal poverty level | 285 | 15.7 | 54 | 9.9 | 62 | 4.9 | |
| Smoking status | <0.001 | ||||||
| Never smoker | 1306 | 56.2 | 377 | 52.6 | 694 | 47.5 | |
| Former smoker | 442 | 19.2 | 131 | 19.0 | 217 | 13.6 | |
| Current smoker | 544 | 24.6 | 189 | 28.3 | 493 | 38.9 | |
P-values derived from χ2 tests for categorical variables and univariate regression for continuous variables
Indicates weighted proportion
“Other” race/ethnicity refers to Non-Hispanic indi viduals identifying as American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander, and adults who identify as multi-racial.
Associations between household food insecurity and HEI-2015 total scores adjusted for sociodemographic and health covariates are shown in Table 2. Among all adults, food insecurity was associated with a 2.22-point lower HEI-2015 score (95% CI −3.35, −1.08). The adjusted mean HEI-2015 score among food-secure adults was 54.6 (SE 0.6); the adjusted mean HEI-2015 score among food-insecure adults was 52.4 (SE 0.8). Adjusted mean HEI-2015 scores by sex and race/ethnicity are shown in Figure 1. By sex, females had higher mean HEI-2015 scores than males at all levels of food security. However, there were no significant differences in these associations by sex (P=0.27).
Table 2:
Associations between household food insecurity and Healthy Eating Index (HEI)-2015 total scores – NHANES 2011–2014
| All adultsa | Non-Hispanic White | Non-Hispanic Black | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SE) | βc | 95% CI | Mean (SE) | βc | 95% CI | Mean (SE) | βc | 95% CI | |
| Food secure | 54.6 (0.6) | Ref. | 53.1 (1.5) | Ref. | 54.0 (0.7) | Ref. | |||
| Marginally food secure | 53.4 (0.7) | −1.19 | −2.87, 0.50 | 50.1 (2.0) | −2.95 | −5.58, −0.33 | 54.0 (1.7) | −0.02 | −3.15, 3.11 |
| Food insecure | 52.4 (0.8) | −2.22 | −3.35, −1.08 | 50.2 (1.6) | −2.92 | −4.49, −1.35 | 53.6 (1.0) | −0.34 | −1.76, 1.09 |
| P-trend | 0.0002 | 0.0002 | 0.64 | ||||||
| Hispanic | Non-Hispanic Asian | “Other” Race/Ethnicity b | |||||||
| Mean (SE) | βc | 95% CI | Mean (SE) | βc | 95% CI | Mean (SE) | βc | 95% CI | |
| Food secure | 54.6 (1.2) | Ref. | 55.6 (1.5) | Ref. | 60.6 (2.7) | Ref. | |||
| Marginally food secure | 56.1 (1.8) | 1.45 | −1.69, 4.59 | 57.4 (2.2) | 1.80 | −3.75, 7.35 | 60.2 (2.2) | −0.44 | −5.31, 4.42 |
| Food insecure | 53.9 (1.0) | −0.68 | −2.73, 1.36 | 50.0 (2.3) | −5.64 | −10.84, −0.44 | 55.2 (2.7) | −5.37 | −10.60, −0.14 |
| P-trend | 0.54 | 0.15 | 0.048 | ||||||
P value from Wald test for heterogeneity of β were: 0.36 for sex and 0.002 for race/ethnicity
“Other” race/ethnicity refers to Non-Hispanic indi viduals identifying as American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander, and adults who identify as multi-racial
β coefficient estimated using linear regression models adjusted for age, sex, race/ethnicity (except for stratified models), birthplace, educational attainment, marital status, poverty income ratio, and smoking status
Figure 1a:
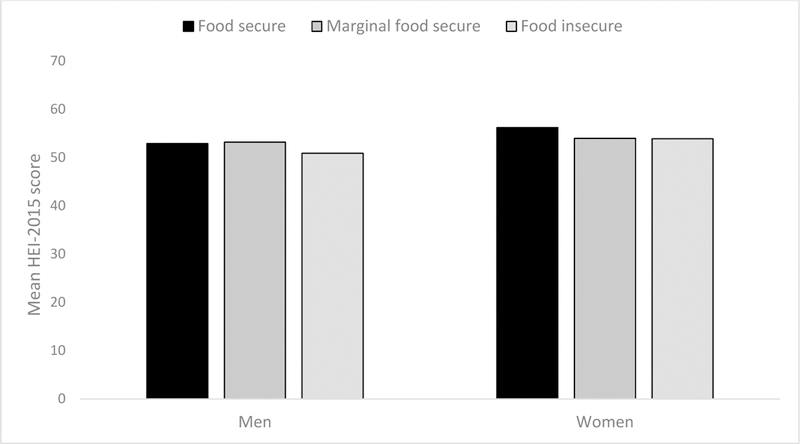
Adjusted mean Healthy Eating Index (HEI)-2015 total scores by sex of 4,393 adults – NHANES 2011–2014.
Figure 1b:
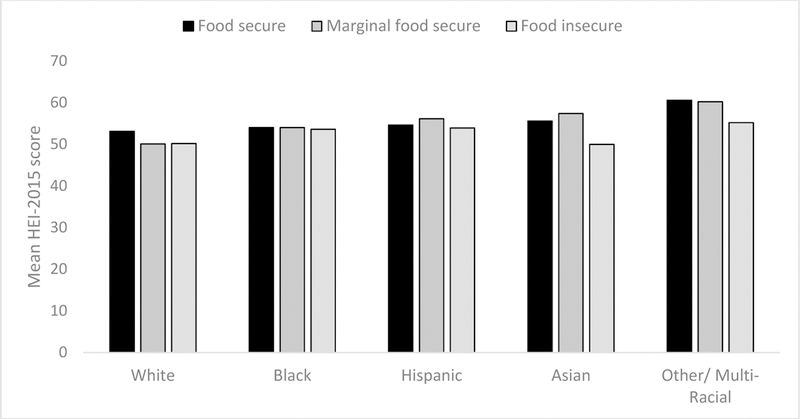
Adjusted mean Healthy Eating Index (HEI)-2015 total scores by race/ethnicity of 4,393 adults – NHANES 2011–2014
Associations between household food insecurity and HEI-2015 total scores varied significantly by race/ethnicity (P<0.001). Among NH Whites, the adjusted mean HEI-2015 scores ranged from 50.1 to 53.1. Marginal food security was associated with a 2.95-point lower HEI-2015 score (95% CI −5.58, −0.33) and food insecurity was associated with a 2.92-point lower HEI-2015 score (95% CI −4.49, −1.35). Among NH Asians, the adjusted mean HEI-2015 scores among food-secure adults and food-insecure adults were 55.6 and 50.0, respectively – a difference of 5.64 points (95% CI −10.84, −0.44). Among NH “Other” adults, the adjusted mean HEI-2015 scores among food-secure and food-insecure adults were 60.6 and 55.2, respectively – a difference of 5.37 points (95% CI −10.60, −0.14).
Associations between food insecurity and individual HEI-2015 components were examined further (Table 3). Among NH Whites, food insecurity was associated with a lower score on total protein foods (RD 0.94, 95% CI 0.89, 0.99), seafood and plant proteins (RD 0.83, 95% C 0.70, 0.98), and added sugar (denoting higher intake) (RD 0.88, 95% CI 0.81, 0.95). Among NH Black adults, marginal food security was associated with a lower score on whole grains (RD 0.66, 95% CI 0.52, 0.85). Among Hispanic adults, marginal food security was associated with a higher score on sodium (RD 1.19, 95% CI 1.01, 1.41). Among NH Asian adults, food insecurity was associated with a lower score on whole fruits (RD 0.68, 95% CI 0.50, 0.93). Among NH “Other” adults, marginal food secur ity was associated with a lower score on total fruits (RD 0.31, 95% CI 0.17, 0.56) and whole fruits (RD 0.41, 95% CI 0.19, 0.84). No other associations were observed between food insecurity and individual HEI-2015 components across these racial/ethnic groups.
Table 3:
Associations between household food insecurity and Healthy Eating Index (HEI)-2015 component scores – NHANES 2011–2014
| Non-Hispanic White | Non-Hispanic Black | Hispanic | Asian | “Other” Race/Ethnicitya | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RDb | 95% CI | RDb | 95% CI | RDb | 95% CI | RDb | 95% CI | RDb | 95% CI | ||
| Total vegetablesc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 1.01 | 0.91, 1.12 | 1.01 | 0.90, 1.12 | 1.12 | 1.03, 1.22 | 1.03 | 0.85, 1.25 | 0.93 | 0.56, 1.52 | |
| Food insecure | 0.99 | 0.91, 1.07 | 0.97 | 0.90, 1.05 | 1.05 | 0.97, 1.14 | 0.94 | 0.78, 1.15 | 0.98 | 0.77, 1.23 | |
| P-trend | 0.76 | 0.46 | 0.18 | 0.66 | 0.82 | ||||||
| Greens and beansc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.97 | 0.72, 1.32 | 0.92 | 0.64, 1.33 | 0.98 | 0.78, 1.23 | 0.87 | 0.64, 1.19 | 0.59 | 0.19, 1.80 | |
| Food insecure | 1.13 | 0.88, 1.44 | 1.06 | 0.84, 1.34 | 1.01 | 0.83, 1.23 | 0.90 | 0.67, 1.20 | 1.03 | 0.44, 2.43 | |
| P-trend | 0.37 | 0.66 | 0.90 | 0.36 | 0.79 | ||||||
| Total fruitsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.80 | 0.63, 1.01 | 1.02 | 0.80, 1.32 | 1.21 | 1.04, 1.41 | 1.31 | 0.96, 1.79 | 0.31 | 0.17, 0.56 | |
| Food insecure | 0.81 | 0.64, 1.04 | 1.03 | 0.84, 1.25 | 1.06 | 0.89, 1.26 | 0.75 | 0.53, 1.06 | 0.64 | 0.35, 1.19 | |
| P-trend | 0.07 | 0.78 | 0.46 | 0.41 | 0.08 | ||||||
| Whole fruitsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.92 | 0.70, 1.21 | 1.24 | 0.92, 1.67 | 1.19 | 0.98, 1.43 | 1.31 | 0.92, 1.86 | 0.41 | 0.19, 0.84 | |
| Food insecure | 0.78 | 0.60, 1.01 | 1.03 | 0.80, 1.33 | 1.05 | 0.87, 1.26 | 0.68 | 0.50, 0.93 | 0.51 | 0.24, 1.09 | |
| P-trend | 0.06 | 0.77 | 0.58 | 0.22 | 0.05 | ||||||
| Whole grainsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.99 | 0.71, 1.39 | 0.66 | 0.52, 0.85 | 1.22 | 0.84, 1.76 | 0.94 | 0.51 1.76 | 0.51 | 0.14, 1.83 | |
| Food insecure | 1.02 | 0.81, 1.27 | 1.07 | 0.88, 1.31 | 0.92 | 0.71, 1.21 | 0.53 | 0.26, 1.11 | 0.87 | 0.42, 1.83 | |
| P-trend | 0.88 | 0.64 | 0.56 | 0.17 | 0.69 | ||||||
| Dairyc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.99 | 0.82, 1.21 | 1.09 | 0.92, 1.29 | 0.95 | 0.82, 1.09 | 0.88 | 0.65, 1.19 | 1.12 | 0.82, 1.53 | |
| Food insecure | 1.00 | 0.93, 1.09 | 1.05 | 0.93, 1.18 | 0.96 | 0.86, 1.08 | 0.92 | 0.64, 1.34 | 1.01 | 0.69, 1.48 | |
| P-trend | 0.93 | 0.39 | 0.51 | 0.55 | 0.92 | ||||||
| Total protein foodsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.97 | 0.89, 1.05 | 0.99 | 0.95, 1.02 | 0.99 | 0.96, 1.02 | 1.03 | 0.98, 1.08 | 1.06 | 0.88, 1.28 | |
| Food insecure | 0.94 | 0.89, 0.99 | 0.98 | 0.96, 1.01 | 0.97 | 0.93, 1.02 | 0.93 | 0.80, 1.07 | 1.13 | 0.90, 1.41 | |
| P-trend | 0.02 | 0.27 | 0.21 | 0.39 | 0.29 | ||||||
| Seafood and plant proteinsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.82 | 0.66, 1.01 | 1.03 | 0.85, 1.24 | 1.00 | 0.89, 1.12 | 0.99 | 0.80, 1.22 | 0.80 | 0.28, 2.26 | |
| Food insecure | 0.83 | 0.70, 0.98 | 0.99 | 0.83, 1.17 | 0.95 | 0.84, 1.07 | 0.79 | 0.56, 1.12 | 0.74 | 0.41, 1.36 | |
| P-trend | 0.02 | 0.89 | 0.39 | 0.22 | 0.30 | ||||||
| Fatty acidsc | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.92 | 0.75, 1.12 | 0.99 | 0.82, 1.18 | 1.03 | 0.89, 1.19 | 1.12 | 0.94, 1.34 | 0.81 | 0.58, 1.15 | |
| Food insecure | 1.01 | 0.90, 1.14 | 0.93 | 0.83, 1.05 | 1.06 | 0.93, 1.21 | 0.92 | 0.73, 1.16 | 0.93 | 0.65, 1.32 | |
| P-trend | 0.99 | 0.24 | 0.34 | 0.75 | 0.66 | ||||||
| Sodiumd | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.91 | 0.77, 1.09 | 1.14 | 0.95, 1.35 | 1.19 | 1.01, 1.41 | 1.09 | 0.54, 2.21 | 1.05 | 0.67, 1.65 | |
| Food insecure | 1.05 | 0.93, 1.18 | 0.98 | 0.84, 1.15 | 1.06 | 0.93, 1.20 | 0.89 | 0.42, 1.90 | 0.80 | 0.49, 1.29 | |
| P-trend | 0.50 | 0.83 | 0.34 | 0.86 | 0.34 | ||||||
| Refined grainsd | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.94 | 0.80, 1.12 | 1.10 | 0.98, 1.23 | 0.98 | 0.83, 1.17 | 1.06 | 0.78, 1.43 | 1.07 | 0.72, 1.58 | |
| Food insecure | 0.92 | 0.84, 1.01 | 1.02 | 0.93, 1.11 | 0.94 | 0.79, 1.12 | 0.81 | 0.46, 1.42 | 1.14 | 0.80, 1.61 | |
| P-trend | 0.08 | 0.67 | 0.45 | 0.54 | 0.46 | ||||||
| Saturated fatd | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.93 | 0.78, 1.11 | 0.99 | 0.90, 1.09 | 1.01 | 0.92, 1.11 | 0.94 | 0.83, 1.05 | 1.00 | 0.81, 1.23 | |
| Food insecure | 0.95 | 0.87, 1.05 | 0.95 | 0.87, 1.04 | 1.03 | 0.93, 1.13 | 1.07 | 0.99, 1.16 | 0.84 | 0.61, 1.15 | |
| P-trend | 0.31 | 0.25 | 0.56 | 0.31 | 0.27 | ||||||
| Added sugard | |||||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Marginally food secure | 0.95 | 0.84, 1.08 | 0.90 | 0.74, 1.10 | 0.99 | 0.87, 1.11 | 1.08 | 0.94, 1.24 | 0.82 | 0.37, 1.85 | |
| Food insecure | 0.88 | 0.81, 0.95 | 1.01 | 0.87, 1.17 | 0.96 | 0.89, 1.02 | 0.95 | 0.77, 1.17 | 0.90 | 0.53, 1.52 | |
| P-trend | 0.002 | 0.93 | 0.19 | 0.82 | 0.68 | ||||||
“Other” race/ethnicity refers to Non-Hispanic individuals identifying as American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander, and adults who identify as multi-racial.
Relative difference (RD) estimated using generalized linear models adjusted for age, sex, birthplace, educational attainment, marital status, poverty income ratio, and smoking status. RDs are interpreted as the percentage difference between groups (e.g. a RD of 0.90 is 10% difference between the food security category and the reference group).
Adequacy components indicates higher points for greater consumption. Maximum points and standards for maximum score per 1,000 kcal are as follows: total fruits, 5 points for ≥0.8 C equiv.; whole fruits, 5 points for ≥0.4 C equiv.; total vegetables, 5 points for ≥1.1 C equiv.; greens and beans, 5 points for ≥0.2 C equiv.; whole grains, 10 points for ≥1.5 oz equiv.; dairy, 10 points for ≥1.3 C equiv.; total protein foods, 5 points for ≥2.5 oz equiv.; seafood and plant proteins, 5 points for ≥0.8 oz equiv.; fatty acids, 10 points for (polyunsaturated fat + monounsaturated fat)/ saturated fat ≥2.5
Moderation components indicates higher points for lower consumption. Maximum points and standards for maximum score per 1,000 kcal are as follows: refined grains, 10 points for ≤1.8 oz equiv.; sodium, 10 points for ≤1.1 g; added sugars, 10 points for ≤6.5% of energy; saturated fats, 10 points for ≤8% of energy
DISCUSSION
In this nationally representative sample, food insecurity was significantly associated with lower diet quality. These associations were most pronounced among NH Whites, Asians, and adults of “other” race/ethnicity. The primary assoc iation of food insecurity and lower diet quality is similar to previous studies using varied measures. In early studies using the original Healthy Eating Index, Basiotis and colleagues found that women in food-insufficient households scored 3.9 points less than women in food-sufficient households.5 Bhattarchya and colleagues found that food insecurity was associated with a 2.4 point lower HEI among non-elderly adults, independent of poverty.6 An analysis of NHANES 1988–1994 and 2001–2002 data by Montoya and colleagues found that food-insecure adults had lower HEI scores than food-secure adults.7 A prior analysis of 1999–2008 NHANES data showed a 2.2-point mean difference in HEI-2005 scores between fully food-secure and very low food-secure adults.10 Finally, in a recent study by Sanjeevi and colleagues, food-insecure women scored 0.9 points lower on the Dietary Guidelines Adherence Index 2015 than food-secure women.9 This study builds on the current literature by highlighting racial/ethnic differences in these associations, and by demonstrating that the inverse association between food insecurity and diet quality is robust to the changing measurements of food insecurity and overall diet quality over time.
Although the results confirmed the initial study hypothesis that food insecurity would be inversely associated with diet quality, predominantly in minority racial/ethnic groups, the observed inverse associations among NH Asian and “Other” adults were still unexpected, partly due to the heterogeneity of individuals comprising this latter group. “Other” is a category within NHANES that is given to anyone who does not self-identify as NH White, NH Black, Hispanic, or NH Asian. This includes adults of American Indian or Alaska Native (AIAN), and Native Hawaiian or Other Pacific Islander (NHOPI) descent as well as multi-racial adults.27 Among AIAN households, a few studies using convenience samples have documented the significantly high rates of food insecurity, ranging from 44% to 77%.28, 29 One of these studies also documented how food-insecure American Indian adults had lower intakes of vegetables and higher intakes of fruit juices, sugar-sweetened beverages, and fried potatoes compared to food-secure American Indian adults, consistent with the results in the present study.30 Among NHOPI adults, data from the Hawai’i Health Survey found that food insecurity was associated with poorer mental and physical health, higher BMI, and higher prevalence of chronic conditions.31 Among Asian adults, there have been a few studies of food insecurity and dietary outcomes among Korean adults from the Korea NHANES,32–34 but there have been no systematic studies of food insecurity among any Asian American groups.
As the results of the current study showed, the associations between food insecurity and diet quality were driven by different components among different racial/ethnic groups. Among NH Whites, the association between food insecurity and diet quality was driven by lower intakes of total protein foods, seafood and plant proteins, and higher intakes of added sugars. Among NH Asians and “Other” adults, food insecurity was only associated with the fruit component of the HEI-2015 score. This suggests there may be synergistic effects of other dietary components among food-insecure adults driving the inverse association with diet quality. At this time, more research is needed to understand the experiences of food insecurity among Asian, AIAN, NHOPI, and multi-racial individuals, in addition to risk factors, health consequences, and psychosocial factors that could buffer these effects. In addition, large economic and health surveys should adopt the racial/ethnic categories proposed by the Office of Management and Budget (OMB) in order to better understand the heterogeneous needs of the “Other” group.35
It was also of interest that no associations were observed between food insecurity and diet quality among NH Black and Hispanic adults. Although for both racial/ethnic groups, the effect estimates were negative, suggesting lower overall diet quality related to food insecurity, they did not reach statistical significance. In this study, NH Black adults demonstrated the lowest mean diet quality compared to other racial/ethnic groups, corroborating previous research showing that NH Black adults generally lag behind NH White and Hispanic adults with respect to diet quality.36. Qualitative studies have identified multiple barriers to healthy eating among NH Black adults, including personal preferences, limited household resources, inability to access to healthful grocery stores, and poor communication with health care providers.37–39 These factors may overshadow the association of food insecurity and diet quality among NH Black adults.
Among Hispanic adults, some studies have examined the role of acculturation status as a modifier of the association between food insecurity and diet-related health outcomes. In two studies with body mass index (BMI) as the outcome, greater acculturation among food-insecure children and adults were associated with higher BMI, but lower acculturation among food-insecure children and adults had no association.40, 41 Greater acculturation may be associated with higher total energy intake and increased consumption of junk foods with little nutritional value.42–44 Although acculturation was not measured in the present study, ignoring the modifying role of acculturation may have led to nonsignificant results between food insecurity and diet quality among Hispanic adults.
This research highlights the continued need for research to identify and evaluate potential strategies to promote food security and healthful eating behaviors across all racial/ethnic groups. At the federal level, the Supplemental Nutrition Assistance Program (SNAP) is the primary safety net that serves to reduce food insecurity and improve access to nutritious foods for low-income families. Because SNAP allows individuals to choose the foods they buy for their households, SNAP is able to serve individuals across diverse cultural backgrounds, preferences, and dietary needs.45 Despite this strength, minority racial/ethnic groups and immigrant populations, particularly Hispanic and Asian families, have the lowest participation rates in SNAP and this may contribute to disparities in diet quality and eating behaviors.45–47
This study is primarily limited by the cross-sectional nature of the data, which doesn’t allow us to examine duration of food insecurity and its impact on diet quality, or concurrent changes in food insecurity and diet quality over time. Household food insecurity was assessed over the past 12 months, while dietary intake was assessed at the time of the survey. This may have resulted in misclassification, as food insecurity is a transient condition and can vary over the course of the season, month, or even week. Future studies may want to consider using a measure that captures food insecurity over the past 30 days, to better understand associations with dietary intake. Finally, HEI-2015 scores were also calculated using the simple scoring method, which uses the average of two 24-hour dietary recalls. This method may not approximate usual dietary intakes of the individual. However, this analytic method is currently recommended by the National Cancer Institute for analyses relating HEI components to a health outcome.48
CONCLUSION
In this national sample of adults with family incomes ≤300% of the federal poverty level, food insecurity was associated with lower diet quality primarily among NH Whites and Asian, NHOPI, AIAN, and multi-racial adults. No differences were observed between males and females. Future food insecurity research should focus on understudied racial groups, including Asian, NHOPI, AIAN, and multi-racial adults, to better understand how food insecurity adversely affects health outcomes. This research will useful in informing interventions to improve diet quality among groups most vulnerable to food insecurity.
RESEARCH SNAPSHOT.
RESEARCH QUESTION:
How is food insecurity associated with overall diet quality, and do these associations vary by individual’s sex or race/ethnicity?
KEY FINDINGS:
In the study population of 4,393 adults, food insecurity was associated with a 2.2-lower Healthy Eating Index (HEI)-2015 score (95% CI −3.35, −1.08), after adjusting for sociodemographic and health characteristics. Further investigation by race/ethnicity demonstrated that this association was most pronounced among Non-Hispanic White, Non-Hispanic Asian, and adults of “Other” races/ethnici ties. No association was observed among Non-Hispanic Black or Hispanic adults, nor did the association vary by sex.
Acknowledgments
Funding disclosures: The authors were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (4R00HD084758 to Dr. Leung and 5K23HD07582 to Dr. Tester)
Footnotes
Conflicts of interest: No conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hamilton WL, Cook JT, Thompson WW, et al. Household Food Security in the United States in 1995: Technical Report of the Food Security Measurement Project: Food and Consumer Service, U.S. Department of Agriculture; 1997.
- 2.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2017, ERR-256: U.S. Department of Agriculture, Economic Research Service; 2018. 290 [Google Scholar]
- 3.USDA ERS - Definitions of Food Security. Food Security in the U.S. Vol 2018: 291 Economic Research Service, U.S. Department of Agriculture; 2017. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-293us/definitions-of-food-security.aspx. Published 2017. Revised September 5, 2018. Accessed February 10, 2018.
- 4.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 2014;100:684–692. [DOI] [PubMed] [Google Scholar]
- 5.Basiotis PP, Lino M. Food Insufficiency and Prevalence of Overweight among Adult Women. Fam Econ Rev 2003;15:55–57. [Google Scholar]
- 6.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ 2004;23:839–862. [DOI] [PubMed] [Google Scholar]
- 7.Montoya MF, Hite AW, Rohrbeck P, et al. Quality of diet related to food insecurity and food stamps use among older people. Ageing Res 2011;2:e3. [Google Scholar]
- 8.Champagne CM, Casey PH, Connell CL, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. J Am Diet Assoc 2007;107:1886–1894. [DOI] [PubMed] [Google Scholar]
- 9.Sanjeevi N, Freeland-Graves J, Hersh M. Food insecurity, diet quality and body mass index of women participating in the Supplemental Nutrition Assistance Program: The role of intrapersonal, home environment, community and social factors. Appetite 2018;125:109–117. 311 [DOI] [PubMed] [Google Scholar]
- 10.Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet 2014;114:1943–313 1953 e1942. [DOI] [PubMed] [Google Scholar]
- 11.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr 2001;131:1738–1745. [DOI] [PubMed] [Google Scholar]
- 12.Jones SJ, Frongillo EA. The modifying effects of Food Stamp Program participation on the relation between food insecurity and weight change in women. J Nutr 2006;136:1091–1094. [DOI] [PubMed] [Google Scholar]
- 13.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet 2013;113:297–321 306. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y, Chen X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among US adults? J Am Diet Assoc 2011;111:1904–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NHANES - National Health and Nutrition Examination Surveys: National Center for Health Statistics, Centers for Disease Control and Prevention
- 16.ASPE Poverty Guidelines. Vol 2017: US Department of Health and Human Services https://aspe.hhs.gov/poverty-guidelines. Accessed November 14, 2017.
- 17.U.S. Household Food Security Survey Module: Three-Stage Design, With Screeners: Economic Research Service, U.S. Department of Agriculture; 2012https://www.ers.usda.gov/media/8271/hh2012.pdf. Accessed November 14, 2017. [Google Scholar]
- 18.MEC In-person dietary interviews procedure manual. National Health and Nutrition Examination Survey: Centers for Disease Control and Prevention; 2002. https://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/DIETARY_MEC.pdf. Published 336 January 2002. Accessed November 15, 2017.
- 19.Rhee JJ, Sampson L, Cho E, Hughes MD, Hu FB, Willett WC. Comparison of methods to account for implausible reporting of energy intake in epidemiologic studies. Am J Epidemiol 2015;181:225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berkey CS, Rockett HR, Field AE, et al. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics 2000;105:E56. [DOI] [PubMed] [Google Scholar]
- 21.Rockett HR, Breitenbach M, Frazier AL, et al. Validation of a youth/adolescent food frequency questionnaire. Prev Med 1997;26:808–816. [DOI] [PubMed] [Google Scholar]
- 22.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet 2018;118:1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.SAS Code. The Healthy Eating Index Vol 2018: Division of Cancer Control and 348 Population Sciences, National Cancer Institute; 2018. https://epi.grants.cancer.gov/hei/sas-code.html. Revised January 26, 2018. Accessed January 30, 2018. [Google Scholar]
- 24.McCullagh P, Nelder JA. Generalized Linear Models, Second Edition. Boca Raton, Florida: Chapman & Hall/CRC; 1989. [Google Scholar]
- 25.SAS version 9.3 Cary, NC: SAS Institute Inc.; 2011. [Google Scholar]
- 26.Stata/ SE version 12.1 College Station, TX: StataCorp LLC; 2012. [Google Scholar]
- 27.Race - Census Bureau Vol 2018: United States Census Bureau; 2018https://www.census.gov/topics/population/race/about.html. Revised January 23, 2018. Accessed February 16, 2018. [Google Scholar]
- 28.Brown B, Noonan C, Nord M. Prevalence of Food Insecurity and Health-Associated Outcomes and Food Characteristics of Northern Plain Indian Households. J Hunger 360 Environ Nutr 2007;1:37–53. [Google Scholar]
- 29.Pardilla M, Prasad D, Suratkar S, Gittelsohn J. High levels of household food insecurity on the Navajo Nation. Public Health Nutr 2014;17:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tomayko EJ, Mosso KL, Cronin KA, et al. Household food insecurity and dietary patterns in rural and urban American Indian families with young children. BMC public health 2017;17:611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baker Kromer K, Derrickson JP, Derrickson SAK, et al. Hunger and Food Insecurity in Hawai’i: Baseline Estimates 1999–2000, Hawai’i Health Survey (HHS). Honolulu, Hawai’i: Hawai’i State Department of Health, Office of Health Status Monitoring; 2001.
- 32.Yang YJ. Socio-demographic Characteristics, Nutrient Intakes and Mental Health Status of Older Korean Adults depending on Household Food Security: Based on the 2008–2010 Korea National Health and Nutrition Examination Surveys. Korean J Community Nutr 2015;20:30–40. [Google Scholar]
- 33.Kim K, Kim MK, Shin YJ, Lee SS. Factors related to household food insecurity in the Republic of Korea. Public Health Nutr 2011;14:1080–1087. [DOI] [PubMed] [Google Scholar]
- 34.Chun IA, Ryu SY, Park J, Ro HK, Han MA. Associations between food insecurity and healthy behaviors among Korean adults. Nutr Res Pract 2015;9:425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity: Federal Register Notice October 30, 1997 Vol 2018: Office of Management and Budget; https://obamawhitehouse.archives.gov/omb/fedreg_1997standards. Accessed September 12, 2018. [Google Scholar]
- 36.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Int Med 2014;174:1587–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee LT, Willig AL, Agne AA, Locher JL, Cherrington AL. Challenges to Healthy Eating Practices: A Qualitative Study of Non-Hispanic Black Men Living With Diabetes. Diabetes Educ 2016;42:325–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doldren MA, Webb FJ. Facilitators of and barriers to healthy eating and physical activity for Black women: a focus group study in Florida, USA. Crit Public Health 2012;23:32–38. [Google Scholar]
- 39.Nolan SE, Tucker CM, Flenar DJ, Arthur TM, Smith TM. Motivators of and Barriers to Engagement in Healthy Eating Behaviors among non-Hispanic Black Adults. J Racial Ethn Health Disparities 2016;3:473–483. [DOI] [PubMed] [Google Scholar]
- 40.Ryan-Ibarra S, Sanchez-Vaznaugh EV, Leung C, Induni M. The relationship between food insecurity and overweight/obesity differs by birthplace and length of US residence. Public Health Nutr 2017;20:671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buscemi J, Beech BM, Relyea G. Predictors of obesity in Latino children: acculturation as a moderator of the relationship between food insecurity and body mass index percentile. J Immigr Minor Health 2011;13:149–154. [DOI] [PubMed] [Google Scholar]
- 42.Mazur RE, Marquis GS, Jensen HH. Diet and food insufficiency among Hispanic youths: acculturation and socioeconomic factors in the third National Health and Nutrition Examination Survey. Am J Clin Nutr 2003;78:1120–1127. [DOI] [PubMed] [Google Scholar]
- 43.Dave JM, Evans AE, Saunders RP, Watkins KW, Pfeiffer KA. Associations among food insecurity, acculturation, demographic factors, and fruit and vegetable intake at home in Hispanic children. J Am Diet Assoc 2009;109:697–701. [DOI] [PubMed] [Google Scholar]
- 44.Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and Non-Hispanic Whites. J Nutr 2011;141:1898–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lauffer S Characteristics of Supplemental Nutrition Assistance Program Households: Fiscal Year 2016 Alexandria, VA: Office of Policy Support, Food and Nutrition Service, US Department of Agriculture; 2017. [Google Scholar]
- 46.Kaiser L Why do low-income women not use food stamps? Findings from the California Women’s Health Survey. Public Health Nutr 2008;11:1288–1295. [DOI] [PubMed] [Google Scholar]
- 47.Pinard CA, Bertmann FMW, Byker Shanks C, et al. What Factors Influence SNAP Participation? LIterature Reflecting Enrollment in Food Assistance Programs from a Social and Behavioral Science Perspective. J Hunger Environ Nutr 2017;12:151–168. [Google Scholar]
- 48.The Healthy Eating Index - Research Uses: Choosing a Method Vol 2018: National Cancer Institute, Division of Cancer Control & Population Sciences; 2018. https://epi.grants.cancer.gov/hei/tools.html. Revised February 12, 2018. Accessed February 16, 2018.


