Abstract
Purpose of Review
The purpose of this chapter is to highlight current recommendations regarding colorectal cancer (CRC) screening and post-polypectomy surveillance colonoscopy in older adults and to review the available literature in order to help inform decision-making in this age group.
Recent Findings
Age is a risk factor for CRC, however, older adults with a history of prior screening are at lower risk for CRC compared to those who have never been screened. Decision-making for CRC screening and post-polypectomy surveillance colonoscopy in older adults is complex and several factors including age, screening history, comorbidities, functional status, bowel preparation, prior experiences, preferences, and barriers need to be considered when weighing risks and benefits. Recent guidelines have started to incorporate life expectancy and prior screening history into their recommendations; however, how to incorporate these factors into actual clinical practice is less clear.
Summary
There are limited data on the relative benefits of screening and surveillance in older adults and therefore, at this time, decision-making should be individualized and incorporate patient preferences in addition to medical factors.
Keywords: colon cancer, screening, surveillance
Introduction
Colorectal cancer (CRC) is the third leading cause of cancer and the second leading cause of cancer-related death for men and women in the U.S. [1]. The primary goal of CRC screening is to reduce the incidence of CRC by removal of pre-malignant polyps (including adenomas and serrated lesions) and to reduce morbidity and mortality by early detection of cancer. If during screening colonoscopy polyps are detected and removed, subsequent colonoscopies are recommended at more frequent intervals to evaluate for metachronous polyps, due to a presumed higher risk for future CRC in these patients. These colonoscopies are termed “post-polypectomy surveillance.” With increasing uptake of CRC screening and technologic advances that have improved detection of polyps, there has been a substantial rise in the number of surveillance colonoscopies performed annually over time [2]. Provided that the initial colonoscopy consists of an optimal bowel preparation and reaches the cecum, the U.S. Multi-Society Task Force (USMSTF) recommends surveillance at a 3-year interval for those with high-risk polyps (3 or more adenomas or serrated lesions, or any polyp that is ≥10mm in size, has tubulovillous features or high grade dysplasia, or a traditional serrated polyp) and 5–10 years for those with low-risk polyps (1–2 adenomas or serrated lesions, each <10mm in size) [3]. In current practice, CRC screening and post-polypectomy surveillance continues as long as benefits outweigh risks, a decision commonly made based on clinical gestalt by providers.
By 2035, the U.S. Census Bureau projects a large demographic shift in the U.S. The aging baby boomer generation will lead to a rise in the number of adults over the age of 65, reaching 78 million or accounting for 1 in every 5 adults [4]. This demographic shift presents several challenges for overall CRC screening and surveillance. Age is certainly a risk for factor for CRC, with peak incidence at 65–69 years [5]; however, prior to performing screening or surveillance in older adults, it is important to take into consideration both the benefits and harms of preventive colonoscopy. The purpose of this chapter is to review the currently available CRC screening and post-polypectomy surveillance in older adults, review the potential benefits and harms of colonoscopy, and discuss important considerations for decision-making. In this chapter, we consider older adults to be individuals over the age of 60 as per standard definition [6]. In addition, we will use the term “surveillance” to indicate post-polypectomy surveillance colonoscopy in adults without inflammatory bowel disease or genetic CRC or polyposis syndromes.
Epidemiology
Age is a known risk factor for colon polyps and CRC [5]. The median age at CRC diagnosis in the U.S. is 68 for men and 72 for women [7]. As of 2016, 63% of adults between the ages of 50 and 75 were up-to-date with CRC screening nationally, with some variation by state [5]. The rise in screening rates with removal of polyps has led to a steady decline in CRC incidence and mortality, particularly among those over the age of 65 [7]. Despite the increased incidence of polyps with high-risk features such as advanced histology or location in the proximal colon among older adults, once polyps have been removed, age has not been shown to be associated with recurrence of polyps or CRC [8–10]. These findings support that age alone should not be used in decision-making and also calls for the need for further guidance around CRC screening and surveillance among older adults.
Current Guidelines
In 2008, the U.S. Preventive Services Task Force (USPSTF) recommended CRC screening for average-risk individuals 50–75 years of age and against screening beyond the age of 75 [11]. The recommendation against screening beyond age 75 was based on microsimulation modeling and the assumption that these individuals have had prior adequate screening [12]. However, there were no clear guidelines for whether to recommend for or against screening individuals over the age of 75 who have not undergone prior screening. Van Hees and colleagues performed a cost-effective analysis of individuals over the age of 75 undergoing screening, with consideration of comorbidities in addition to age. They found that screening was in fact cost-effective up to the age of 86 in those without comorbidities, up to the age of 83 in those with moderate comorbidities, and up to the age of 80 in those with severe comorbidities [13].
To reflect the growing body of literature to support that age alone should not be used to determine whether to pursue screening in older adults, the USMSTF on CRC revised their CRC screening guidelines in 2016. These 2016 recommendations state that individuals who are up to date with CRC screening or have had prior negative screening, should discontinue screening at the age of 75 or when life expectancy is estimated to be less than 10 years. However, they also recommended that those who have not had prior screening should be considered for screening up to the age of 85 and that this decision should be individualized [14].
In contrast to the updates to CRC screening guidelines that incorporate age and prior screening into recommendations, there are no clear guidelines for surveillance for older adults. Existing documents provide guidance of intervals for surveillance colonoscopy based on polyp number, size and histology, but provide limited to no direction on when to consider stopping surveillance in older adults. The USMSTF on CRC suggests that surveillance “should be individualized, based on an assessment of benefit, risk, and comorbidities,” yet offers no practical tools for its implementation [3]. Experts have acknowledged the need for personalization of surveillance, in addition to screening, in older adults [15]. Table 1 summarizes the currently available guidance around screening and surveillance colonoscopy by age in the US. In addition, this table includes guidelines from other countries if age of cessation for screening or surveillance was considered.
Table 1.
Available Colorectal Cancer Screening and Post-Polypectomy Surveillance Guidelines for Older Adults
| Society | Year | Screening | Surveillance |
|---|---|---|---|
| United States | |||
| U.S. Preventive Services Task Force [39] | 2016 | Adults 76–85 years of age: • The decision to screen for CRC is an individual one. • The net benefit of screening for individuals who have previously been screened is small • Those who have never been screened are more likely to benefit • Screening is most appropriate for those healthy enough to undergo treatment and those without comorbid conditions that significantly limit their life expectancy |
No recommendations provided |
| U.S. Multi-Society Task Force on Colorectal Cancer [14] | 2017 | Individuals who are up to date with screening, who have prior negative screening, reach age 75 or have <10 years of life expectancy: • Discontinuation of screening should be considered • Individuals without prior screening: • Should be considered for screening up to age 85, depending on age and comorbidities |
The decision to continue surveillance should be individualized with consideration of benefit, risk, and comorbidities |
| American Cancer Society [45] | 2018 | Adults 76–85 years of age: • Should make a decision with their medical provider about whether to be screened, based on their own preferences, life expectancy, overall health, and prior screening history Adults over the age of 85: • Should not undergo CRC screening |
No recommendations provided |
| Other | |||
| British Society of Gastroenter-ology and Association of Colproctology for Great Britain and Ireland [43] | 2010 | No recommendations for screening individuals over the age of 74 years | After 75 years of age: • The decision to continue surveillance should be based on relative cancer risk and comorbidity • Colonoscopy is likely to be less successful and more risky at older ages • Most will not benefit from surveillance due to the average lead time for progression of an adenoma to cancer (10 years) which is the same as the average life expectancy of an individual aged 75 years or older |
| European Union [44] | 2010 | No recommendations for screening individuals over the age of 74 years | The cutoff age for stopping surveillance is usually 75 years, but this should also depend on patient wishes and comorbidity |
CRC, colorectal cancer
Current Practice
Despite the available practice guidelines, substantial inappropriate use of preventive colonoscopy continues among older adults. Inappropriate use can be characterized as both potential overuse (too soon based on recommend intervals or performance where benefits are limited by life expectancy) or potential underuse (too late or not at all for high risk lesions). Saini and colleagues found that adults between the ages of 70 and 75 with limited life expectancy were more likely to undergo screening than those over the age of 75 in good health [16]. Mittal and colleagues also found that nearly 25% of Medicare beneficiaries who underwent screening colonoscopy had a limited life expectancy (<10 years from time of screening) [17]. Although this study pre-dated the 2016 USMSTF CRC screening guidelines, its main findings would likely persist using current data. In addition, nearly half of patients who had negative screening exams underwent repeat colonoscopies within 7 years (e.g., earlier than the recommended 10-year screening interval) [18]. In contrast, among older adults with a positive fecal occult blood test warranting a diagnostic colonoscopy, only 56% had a follow up colonoscopy [19]. Similarly, surveillance literature also shows underuse of colonoscopy for high-risk lesions and overuse for low-risk lesions among older adults [20–22].
Inappropriate use of cancer screening and surveillance has been attributed to patient, provider, and system level factors. Where benefits of cancer screening and surveillance are uncertain, one proposed solution is to engage patients through shared decision-making. However, prior data show that physicians are more likely to engage their healthy patients and less likely to engage their older adults with poor health status in decision-making surrounding cancer screening, despite the heightened need for eliciting values and preferences among the latter [23]. One would assume that patients who are in poor health status would agree with their providers about cessation of cancer screening and surveillance. However, patients’ perceived health differs from their actual, calculated life expectancy [24]. In addition, a significant proportion of adults, even in the setting of poor health, are opposed to cessation of screening and surveillance. This reluctance to stop CRC screening and surveillance may be due to overall enthusiasm for cancer screening in the U.S. [25]. This enthusiasm for cancer screening was also noted in a recent survey-based study. Despite receiving education about benefits and harms of colonoscopy, nearly half of patients with low-risk adenomas (1–2 adenomas, each less than 1 cm without any advanced histology), were uncomfortable with cessation of surveillance even in the setting of poor health. Factors associated with discomfort with stopping surveillance included fear of CRC and increased perceived effectiveness of colonoscopy. Trust in physicians was associated with increased comfort [26]. As previously discussed, physicians are also drivers of inappropriate CRC screening and surveillance. Despite understanding that older adults may gain minimal benefit from future endoscopy, physicians often do not recommend cessation in such cases [27].
Yield of Colonoscopy
Prior data suggest that CRC risk doubles with each decade of life between 40 and 80 years [28]. The estimated combined risk of colon polyps and CRC in adults between the ages of 75 and 79 is estimated at 26% whereas the risk in adults ages 50–54 is estimated at 14% [29]. Tran and colleagues also found that among individuals ≥75 years of age who were undergoing surveillance, the CRC incidence was 0.24 per 1000 person-years as compared to 3.61 per 1000 person-years in the reference population of individuals 50–74 years of age [9]. However, individuals with a history of polyps who undergo serial, subsequent surveillance colonoscopy, are often actually at lower risk for CRC than those who have not yet undergone CRC screening due to the protection offered by colonoscopy [9, 30].
Factors to Consider
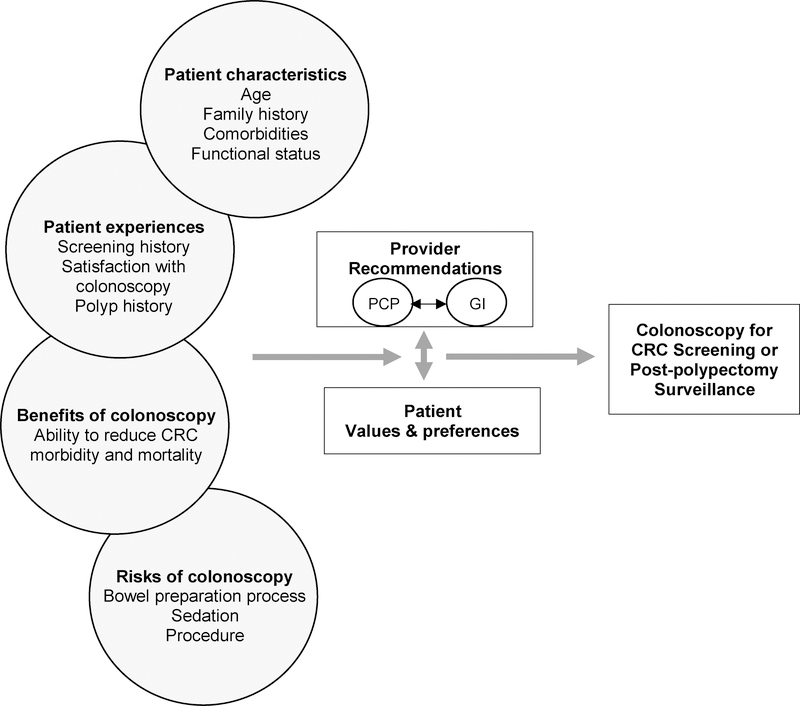
There are several practical considerations when thinking about CRC screening and surveillance in older adults. These factors include patient characteristics, patient experiences, benefits of colonoscopy, risks or colonoscopy, patient values and preferences, and provider recommendations (Figure 1). The following section focuses on the risks of colonoscopy and provider recommendations and communication.
Figure 1:
Factors to Consider for CRC Screening and Surveillance Decision-Making for Older Adults
Older adults are more likely to have complications related to the bowel preparation process. For example, in preparation for a colonoscopy, certain medications, such as hypoglycemics, anticoagulants, and antithrombotics, are often recommended to be held. Older adults are more likely to have comorbidities requiring such agents and interruption of these medications may increase the risk of associated complications (e.g., risk of recurrent venous thromboembolism or cerebral vascular accident when holding anticoagulation). In addition, older adults may have impaired mobility and limited functional status, increasing the risk of falls while prepping [31]. Bedside commodes and admission to the hospital for assistance with bowel preparation have been suggested, though further studies are needed to assess whether these strategies decrease rates of falls and evaluate costs of this from a public health perspective. In terms of bowel purgative regimens, polyethylene glycol (PEG) based preparations are recommended over sodium phosphate-based preparations due to lower risk of electrolyte imbalances and kidney injury [32, 33]. However, even when PEG-based preparations are used in older adults, they have been shown to cause electrolyte imbalances such as hypokalemia or hypo- and hypernatremia. Also, non-compliance rates as high as 32% have been reported with PEG-based bowel preparations among older adults. This is likely due to a combination of factors including poor tolerance of the volume of bowel preparation, dehydration, and symptoms such as nausea, vomiting, and abdominal pain. Overall, given these limitations, older adults are more likely to have inadequate bowel preparations [34].
Older adults are also more likely to experience cardiovascular and pulmonary complications related to sedation, such as arrhythmias, myocardial infarction, and aspiration pneumonia [35, 36]. In addition, they are at increased risk for procedure-related complications including post-polypectomy bleeding and perforation, with higher associated morbidity and mortality. In fact, despite the very low overall risk of perforation during routine colonoscopy (0.5 per 1,000 colonoscopies), data show that older adults are 30% more likely than younger patients to suffer a perforation [28].
Finally, due to potentially limited functional status (i.e. ability to ambulate assisted), bowel preparation quality, and sedation-related complications, older adults are more likely to have incomplete procedures [34]. Given these increased risks of colonoscopy, older adults should be counseled prior to undergoing screening or surveillance colonoscopy. Qualitative work has shown that older adults are often not aware of the risks of colonoscopy nor do they remember being counseled about them [24].
The specific role of providers involved in decision-making around screening and surveillance is not well defined. While primary care physicians (PCPs) are often the referring physicians for screening and surveillance, gastroenterologists perform the procedure and make recommendations for future intervals of colonoscopy based on currently available information, including age and health status at the time. Interestingly, in a recent survey, PCPs and gastroenterologists differed on which provider should be responsible for decision-making for surveillance in older adults. PCPs felt that decisions regarding surveillance should be made between PCPs and patients, while gastroenterologists felt that decisions regarding surveillance should be made between gastroenterologists and patients [37]. As most patients have long-standing relationships with their PCPs, they prefer that their PCPs remain engaged in decision-making after screening and surveillance [24].
Furthermore, communication between PCPs and gastroenterologists may be limited and there is currently no standardized structure for communication regarding colonoscopy results and recommendations. Communication is further complicated by the lag between the drafting of the colonoscopy procedure report and the final recommendations, which often can only be made after pathology has been reviewed (days to weeks later). Effective communication between gastroenterologist, referring providers, and their patients is essential [38]. Using plain language, avoiding medical jargon, incorporating absolute risks (as opposed to relative risks), and displaying risk through the use of pictographs, are all ways to effectively present information about benefits and harms to patients [39].
When to Stop CRC Screening and Surveillance
Decisions about cancer screening and surveillance cessation in older adults are complex. While on the one hand, older adults are at increased risk for CRC, older adults are also at greater risk for procedure-related harms as previously discussed. Using data based on modeling studies, the USPSTF recommended CRC screening for adults between the ages of 50 and 75, but that decisions for screening for individuals between the ages of 76 and 85 should be individualized [40]. While data support weighing benefits and harms in older adults and using a personalized approach [15], patients are resistant to screening cessation. Fear of cancer, hope for early detection and treatment, family history, obligation, and reassurance are all factors patients that report for their desire to continue CRC screening [26, 41].
Ultimately, approaches to stopping CRC screening and surveillance must engage patients. Preferences and values need to be considered, especially when the decisions about benefits and harms are uncertain. Life expectancy tools, several of which have been developed for cancer screening specifically, may be incorporated into shared decision-making. One such tool is ePrognosis (http://cancerscreening.eprognosis.org/screening/), which incorporates not just age, but also comorbidities and functional status to determine overall life expectancy. However, there are several limitations to prognostic tools including the lack of consideration of prior screening history and overall cancer risk. In addition, some patients are simply not receptive to risk calculators or have poor numeracy skills limiting their ability to engage in any quantitative data presented [38, 42].
Finding the balance between incorporating patients’ preferences and values, especially for those who wish to continue screening and surveillance despite overall poor health status, and preventing harms is challenging. Future studies should focus on older adults’ conceptualization of CRC screening and surveillance and also investigate optimal ways to enhance patient-provider and provider-provider communication.
Future areas of research
In order to improve management of and decision-making around CRC screening and surveillance in older adults, several areas of research are needed, including optimal ways to discuss benefits and harms, personalize decisions, optimize bowel preparation, effectively communicate risk, and how to approach screening and surveillance cessation in a practical way (Table 2).
Table 2:
Areas for Future Research Regarding CRC Screening and Post-polypectomy Surveillance in Older Adults
| • Determine the applicability of CRC screening risk calculators to surveillance patients |
| • Identify effective ways to communicate risks around CRC after polyp removal to patients |
| • Determine the role of family history in determining when to stop screening and surveillance |
| • Integrate history of colonoscopy and number, size, type of polyps into need for ongoing surveillance |
| • Determine optimal bowel preparation strategies for older adults in terms of tolerability and safety |
| • Optimize communication of screening and surveillance colonoscopy results to patients |
| • Identify how and when to stop screening and surveillance in older adults |
Conclusions
With the rapidly aging population, there will be an increasing need for thoughtful decision-making around CRC screening and surveillance in older adults. While there are ample evidence-based guidelines for screening, surveillance recommendations for older adults are lacking and we do not have data to support when or how to stop surveillance. Therefore, we are left to extrapolate existing data on screening in older adults and apply similar principles to surveillance, recognizing the likelihood of lower risk of CRC in older adults with a history of polyps who have undergo serial colonoscopies over their lifetime compared to average-risk younger adults.
References
Papers of particular interest, published recently, have been highlighted below (**):
- 1.Noone AM, Howlader N, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2015, National Cancer Institute; Bethesda, MD, https://seer.cancer.gov/csr/1975_2015/. Accessed 25 Oct 2018. [Google Scholar]
- 2.Lieberman DA, Holub J, Eisen G, et al. Utilization of colonoscopy in the United States: results from a national consortium. Gastrointestinal Endoscopy 2005;62:875–883. [DOI] [PubMed] [Google Scholar]
- 3.Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for Colonoscopy Surveillance After Screening and Polypectomy: A Consensus Update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844–857. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Census Bureau. Older People Projected to Outnumber Children for First Time in U.S. History. https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html. Accessed 25 Oct 2018.
- 5.Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA A Cancer Journal for Clinicians 2017;67:177–193. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. World Report on Ageing And Health. 2015; 1–246. [Google Scholar]
- 7.American Cancer Society. Colorectal Cancer Facts & Figures 2017–2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2017-2019.pdf. Accessed 25 Oct 2018.
- 8.Day LW, Velayos F. Colorectal Cancer Screening and Surveillance in the Elderly: Updates and Controversies. Gut Liver 2015;9:143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran AH, Man Ngor EW, Wu BU. Surveillance Colonoscopy in Elderly Patients. JAMA Intern Med 2014;174:1675–1682.**Large retrospective cohort of adults 50 years of age or greater undergoing surveillance colonoscopy for history of CRC or polyps showing a low incidence of CRC and a high rate of post procedure hospitalization among older adults (>75 years).
- 10.Martínez ME, Baron JA, Lieberman DA, et al. A Pooled Analysis of Advanced Colorectal Neoplasia Diagnoses After Colonoscopic Polypectomy. Gastroenterology 2009;136:832–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United States Preventive Services Task Force. Screening for Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2008:627–637. [DOI] [PubMed] [Google Scholar]
- 12.Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, et al. Evaluating Test Strategies for Colorectal Cancer Screening: A Decision Analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2018:659–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Hees F, Habbema JDF, Meester RG, et al. Should Colorectal Cancer Screening Be Considered in Elderly Persons Without Previous Screening? Ann Intern Med 2014;160:750–32.** Microsimulation modeling study to determine age up to which to consider CRC screening. In unscreened older adults, screening found to be cost-effective up to age 86 in those without comorbidities, up to 83 in those with moderate comorbidities, up to 80 in those with severe comorbidities.
- 14.Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterology 2017;112:1016–1030.**The U.S. Multi-Society Task Force recently updated guidelines to include that discontinuation of screening should be considered in individuals who are up to date with screening, who have prior negative screening, reach age 75 or have <10 years of life expectancy. Also, individuals without prior screening should be considered for screening up to age 85, depending on their age and comorbidities. Finally, they concluded that the decision to continue surveillance should be individualized with consideration of benefit, risk, and comorbidities.
- 15.Eckstrom E, Feeny DH, Walter LC, et al. Individualizing Cancer Screening in Older Adults: A Narrative Review and Framework for Future Research. J Gen Intern Med 2012;28:292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saini SD, Vijan S, Schoenfeld P, et al. Role of quality measurement in inappropriate use of screening for colorectal cancer: retrospective cohort study. BMJ 2014;348:g1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mittal S, Lin YL, Tan A, et al. Limited Life Expectancy Among a Subgroup of Medicare Beneficiaries Receiving Screening Colonoscopies. Clinical Gastroenterology and Hepatology 2014;12:443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodwin JS. Overuse of Screening Colonoscopy in the Medicare Population. Arch Intern Med 2011;171:1335–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kistler CE. Long-term Outcomes Following Positive Fecal Occult Blood Test Results in Older Adults. Arch Intern Med 2011;171:1344–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper GS, Kou TD, Barnholtz Sloan JS, et al. Use of colonoscopy for polyp surveillance in Medicare beneficiaries. Cancer 2013;119:1800–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy CC, Lewis CL, Golin CE, et al. Underuse of Surveillance Colonoscopy in Patients at Increased Risk of Colorectal Cancer. Am J Gastroenterology 2014;110:633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahn B, Freeland Z, Gopal P, et al. Predictors of guideline concordance for surveillance colonoscopy recommendations in patients at a safety-net health system. Cancer Causes & Control 2015;26:1653–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis CL, Esserman D, DeLeon C, et al. Physician Decision Making for Colorectal Cancer Screening in the Elderly. J Gen Intern Med 2013;28:1202–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cazares K, OConnor S, Calderwood AH. Older Adults Perspectives Toward Surveillance Colonoscopy: A Qualitative Study. Am J Gastroenterology 2018:S145. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz LM, Woloshin S, Fowler FJ, et al. Enthusiasm for Cancer Screening in the United States. JAMA 2004;291:71–78. [DOI] [PubMed] [Google Scholar]
- 26.Maratt JK, Lewis CL, Saffar D, et al. Veterans’ Attitudes Towards De-Intensification of Surveillance Colonoscopy for Low-Risk Adenomas. Clinical Gastroenterology and Hepatology 2018; doi.org/ 10.1016/j.cgh.2018.09.029. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Calderwood AH, Anderson JC, Robinson CM, et al. Endoscopist Specialty Predicts the Likelihood of Recommending Cessation of Colorectal Cancer Screening in Older Adults. Am J Gastroenterol. 2018. November 2. doi: 10.1038/s41395-018-0406-z. [Epub ahead of print]** Using the New Hampshire Colonoscopy Registry, 85% of adults 70–74 years of age with a normal screening colonoscopy were found to have a recommendation to return for screening (when they would be 80–84 years of age). Advanced age and absence of family history of CRC were associated with recommended to stop screening. Gastroenterologists were more likely to recommend screening cessation for patients of advanced age as compared to non-gastroenterology endoscopists.
- 28.Day LW, Walter LC, Velayos F. Colorectal Cancer Screening and Surveillance in the Elderly Patient. Am J Gastroenterology 2011;106:1197–1206. [DOI] [PubMed] [Google Scholar]
- 29.Lin OS, Kozarek RA, Schembre DB, et al. Screening Colonoscopy in Very Elderly Patients: Prevalence of Neoplasia and Estimated Impact on Life Expectancy. JAMA 2006;295:2357–2365. [DOI] [PubMed] [Google Scholar]
- 30.Calderwood AH, Holub JL, Robertson DJ, Greenwald DA (2018) Practice patterns and yield of surveillance colonoscopy among older adults: an analysis of the GI Quality Improvement Consortium (GIQUIC). Gastrointestinal Endoscopy 2018;87:AB100. [DOI] [PubMed] [Google Scholar]
- 31.Kumar A, Lin L, Bernheim O, et al. Effect of Functional Status on the Quality of Bowel Preparation in Elderly Patients Undergoing Screening and Surveillance Colonoscopy. Gut Liver 2016;10:569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ho JM-W, Juurlink DN, Cavalcanti RB. Hypokalemia Following Polyethylene Glycol-Based Bowel Preparation for Colonoscopy in Older Hospitalized Patients with Significant Comorbidities. The Annals of Pharmacotherapy 2010:466–470. [DOI] [PubMed] [Google Scholar]
- 33.Rex DK. Dosing Considerations in the Use of Sodium Phosphate Bowel Preparations for Colonoscopy. The Annals of Pharmacotherapy 2007:1466–1475. [DOI] [PubMed] [Google Scholar]
- 34.Lukens FJ. Colonoscopy in Octogenarians: A Prospective Outpatient Study. Am J Gastroenterol 2002;97:1722–1725. [DOI] [PubMed] [Google Scholar]
- 35.Cha JM, Kozarek RA, La Selva D, et al. Risks and Benefits of Colonoscopy in Patients 90 Years or Older, Compared With Younger Patients. Clinical Gastroenterology and Hepatology 2016;14:80–86.e1. [DOI] [PubMed] [Google Scholar]
- 36.Reumkens A, Rondagh EJA, Bakker CM, et al. Post-Colonoscopy Complications: A Systematic Review, Time Trends, and Meta-Analysis of Population-Based Studies. Am J Gastroenterology 2016;111:1092–1101. [DOI] [PubMed] [Google Scholar]
- 37.Le ST, Lash BR, Schroy PC III, et al. Physician Perceptions of Surveillance Follow-up Colonoscopy in Older Adults. The Journal of the American Board of Family Medicine 2017;30:371–373.** Survey-based study of primary care physicians (PCPs) and gastroenterologists that evaluated factors related to decision-making in surveillance for older adults. Factors that PCPs considered life expectancy (40%), gastroenterologists’ recommendations (28%), and patient preferences (12%) as the most important factors while gastroenterologists considered comorbidities (57%), findings on prior colonoscopies (27%), and risks of the procedure (10%) as the most important factors for decision-making.
- 38.Maratt JK, Calderwood AH, Saini SD. When and How to Stop Surveillance Colonoscopy in Older Adults: Five Rules of Thumb for Practitioners. Am J Gastroenterol 2017;113:5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping Patients Decide: Ten Steps to Better Risk Communication. JNCI J Natl Cancer Inst 2011;103:1436–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.U.S. Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2016;315:2564–2575.** The U.S. Preventive Services Task Force provides revised guidelines for older adults to include that the decision to screen those who are 76–85 years of age should be individualized. Overall, they concluded that the net benefit of screening individuals in this age group, who have previously been screened, is small and that those who have not been screened are more likely to benefit. They also concluded that screening is most appropriate for those who are healthy enough to undergo treatment and those without comorbid conditions that limit their life expectancy.
- 41.Torke AM, Schwartz PH, Holtz LR, et al. Older Adults and Forgoing Cancer Screening. JAMA Intern Med 2013;173:526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.May FP, Gupta S. When Should Screening Stop for Elderly Individuals at Average and Increased Risk for Colorectal Cancer? Clinical Gastroenterology and Hepatology 2018;16:178–180.e1. [DOI] [PubMed] [Google Scholar]
- 43.Cairns SR, Scholefield JH, Steele RJ, Dunlop MG, Thomas HJW, Evans GD, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010. April 28;59(5):666–89. [DOI] [PubMed] [Google Scholar]
- 44.European Colorectal Cancer Screening Guidelines Working Group. European guidelines for quality assurance in colorectal cancer screening and diagnosis. 2010. November 17;:1–1426. [Google Scholar]
- 45.American Cancer Society. Updates on Colorectal Cancer Screening Guideline. https://www.cancer.org/latest-news/american-cancer-society-updates-colorectal-cancer-screening-guideline.html. Accessed 12 Nov 2018.** The American Cancer Society states that adults between the ages of 76–85 should make decisions about pursuing screening with their medical provider, with consideration of their own preferences, life expectancy, overall health, and prior screening history. The also recommended against screening for those over the age of 85.