Abstract
Background
Irritation of the sinuvertebral nerve by a posterior or posterolateral disk desiccation can cause somatic referred pain that can mimic a lumbar radiculopathy. We present a case of a patient presenting with this condition and the positive result in pain improvement after endoscopic radiofrequency ablation of the sinuvertebral nerve.
Case Description
An 18-year-old Olympic runner presented to our clinic with back pain and left leg pain in a clear L5 distribution. He did not have a history of trauma. His imaging did not demonstrate any lesion causing compression of the left L5 nerve root as expected. He was found to have a left healing L5 pedicle fracture and ipsilateral chronic L5 pars interarticularis fracture. He was also found to have an ipsilateral minor left L5-S1 disk desiccation. His visual analog scale (VAS) score was 7. After a positive provocative diskogram, the patient underwent percutaneous transforaminal endoscopic radiofrequency ablation of the left L5 sinuvertebral nerve, which was irritated by the left L5-S1 disk desiccation. At his 6-month follow-up visit, the patient's VAS score was 1.
Conclusions
It is important for clinicians to remember that back-associated leg pain can be caused by somatic referred pain because of irritation of the sinuvertebral nerve. Endoscopic radiofrequency of this nerve can be beneficial in pain control, but further randomized prospective trials are needed to study these techniques further.
Key words: Back pain, Endoscopic spine surgery, Pars interarticularis fracture, Radiofrequency ablation, Sinuvertebral nerve
Introduction
Back pain associated with leg pain typically points toward a lumbar radiculopathy as an etiology of the symptoms. However, similar complaints can be caused by somatic referred pain from musculoskeletal structures such as the intervertebral disks or facet joints.1 Specifically, this mechanism can explain back-associated leg pain in the setting of posterior or posterolateral disk desiccation without any clear compression of nerve roots on imaging studies.2, 3 In those situations, the leg pain can be explained by irritation of the sinuvertebral nerve, a structure that is formed in the intervertebral foramen at each level by fibers from the ventral primary ramus and ramus communicans coming from the sympathetic trunk.4 This nerve innervates the posterior and posterolateral disk at the level of the intervertebral foramen it enters and the level above.2 Previously, we have demonstrated that endoscopic laser ablation of this nerve improves somatic referred pain from the sinuvertebral nerve.3, 4 In this case report, we describe a high-level athlete with somatic referred left L5 leg pain in the setting of a pedicle/pars interarticularis fracture–associated L5-S1 left disk desiccation. We also discuss his drastic symptomatic improvement after percutaneous transforaminal endoscopic radiofrequency ablation of the left L5 sinuvertebral nerve affected by the disk desiccation.
Patient and Results
Patient History
The patient was an 18-year-old high-level Olympic runner with no history of trauma, who presented with 3 months of severe back pain with left leg pain in a clear L5 distribution. He did not have any right-sided leg symptoms. He had no urinary or bowel symptoms. He did not note any saddle anesthesia. He had a visual analog scale score of 7. On examination, he was neurologically intact. He did have a positive straight leg raise test on the left at 45°. His magnetic resonance imaging demonstrated a minor left L5-S1 disk desiccation on the left with no clear compression of any nerve roots. His disk height was well maintained (Figure 1). A computed tomography scan demonstrated a left healing pedicle fracture with a more chronic vertical left pars interarticularis fracture (Figure 2). After months of exhaustion of conservative measures, including epidural steroid injections, the patient was offered a L5-S1 provocative diskogram and, if positive, a left L5-S1 percutaneous transforaminal endoscopic radiofrequency ablation of the sinuvertebral nerve. Informed patient consent was obtained at that time.
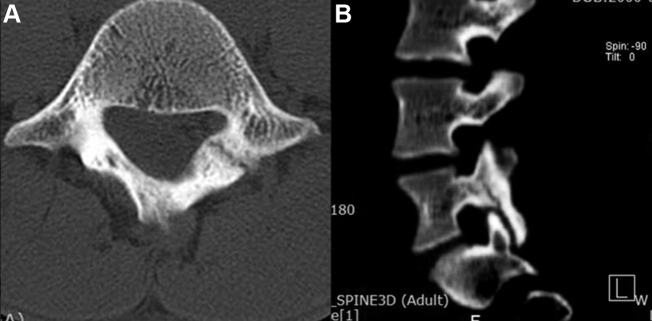
Figure 1.
(A) Preoperative axial T2 magnetic resonance image (MRI) of the L5-S1 disk space demonstrating minor disk desiccation on the left but no significant central canal, lateral recess, or neuroforaminal stenosis that could explain a left L5 radiculopathy. (B and C) Preoperative left parasagittal T2 and STIR MRIs demonstrating the left pedicle fracture with surrounding STIR signal. STIR, short T1 inversion recovery.
Figure 2.
(A) Preoperative axial computed tomography (CT) image demonstrating the left L5 pars interarticularis fracture with surrounding pseudarthrosis. (B) Preoperative parasagittal CT image demonstrating the left pedicle fracture with surrounding pseudarthrosis and bony sclerosis in addition to a more posterior pars interarticularis fracture.
Operative Technique
The first stage of the operation involved performing a provocative diskogram. Because this patient had a low iliac crest, it was possible to perform both the diskogram and the ablation through a transforaminal approach (Figure 3A). In the setting of a high-riding iliac crest, performing a transforaminal approach would not be possible. Under local anesthesia with the patient awake, the patient was positioned prone on a Wilson frame (Wilson Radiolucent Frame 5319 G, Mizuho, Union City, California, USA). After infiltration of the entry point and presumed trajectory with 7–10 cc of 1% lidocaine, anteroposterior and lateral fluoroscopy was used to advance a spinal needle into the L5 suprapedicular notch at Kambin's triangle (Figure 3B and C). This was performed through a 1-cm incision 14 cm left of the vertebral midline. A series of anteroposterior and lateral radiographs were performed throughout the approach to ensure the correct trajectory. At the suprapedicular notch, a mixture of lidocaine and epinephrine was injected into the foraminal space as previously described.5 Afterward, the spinal needle was advanced further into the disk space. In the disk space, a contrast mixture of 6 mL iohexol dye (Taejoon Pharm, Seoul, Republic of Korea) and 1 mL indigo carmine (Korea United Pharmaceutical, Yoenki, Republic of Korea) was injected (Figure 4). This provoked significant back pain with associated leg pain similar to the patient's usual symptoms. At this point, the decision was made to proceed with ablation of the sinuvertebral nerve. A guidewire was inserted through the spinal needle and the needle was removed. As previously described, an obturator was then placed in the same trajectory as the guidewire but was stopped at Kambin's triangle and not introduced further into the L5-S1 disk space.6 After sequential dilation, a beveled working cannula was placed; next, the obturator and guidewire were removed. An endoscope (Joimax GmbH, Karlsruhe, Germany) was introduced. A Trigger-Flex radiofrequency probe (Elliquence, Baldwin, New York, USA) was used to improve visualization by dissecting soft tissue and epidural fat. The endoscope was then introduced further into the epidural space (Figure 5). At this point, as is the case in most instances, the sinuvertebral nerve was not visualized. Therefore, different points across the area surrounding the disk desiccation were palpated with the radiofrequency probe, and all areas that provoked a pain response in the patient similar to his usual symptoms were ablated with the radiofrequency probe using quick millisecond pulse treatment. After meticulous hemostasis was obtained, the working cannula and endoscope were removed. The patient's incision was closed with absorbable dermal suture and skin glue. The patient was taken to the postoperative recovery area with no new neurologic deficits and no intraoperative complications (Video 1).
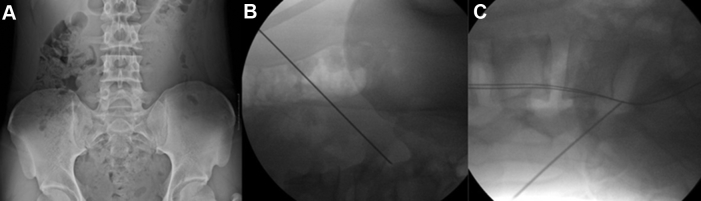
Figure 3.
(A) Preoperative anteroposterior (AP) radiograph showing the low iliac crest making a transforaminal approach feasible in this patient. (B and C) Intraoperative AP and lateral radiographs demonstrating the approach through Kambin's triangle to the suprapedicular notch prior to entering the disk space and performing a provocative diskogram.
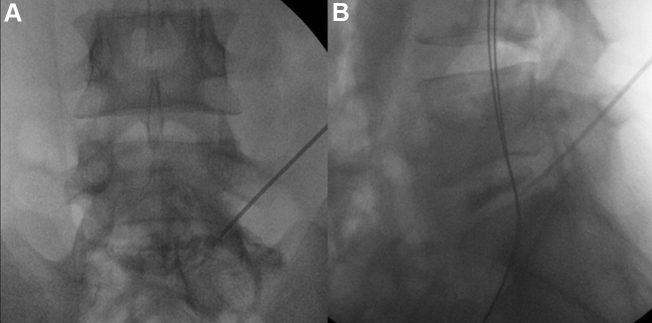
Figure 4.
(A and B) Intraoperative anteroposterior and lateral radiographs showing provocative L5-S1 diskogram with injection of dye into the disk space.
Figure 5.
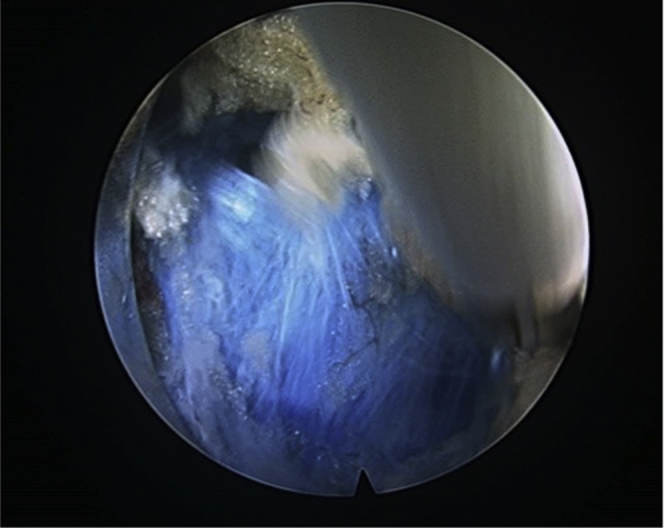
Intraoperative picture taken with endoscope demonstrating blue dye at the surface of the left L5-S1 annulus pointing to significant annular degeneration at the site of the desiccation seen on the preoperative magnetic resonance imaging. Also seen is the radiofrequency probe that also serves as a tissue dissector.
Postoperative Course
The patient's leg pain improved immediately after surgery. At his 6-month follow-up appointment, he continued to be pain-free with a visual analog scale score of 1. He had a negative straight leg raise test, and 10 months later the patient was able to return to his sports and win a bronze medal at a national level event.
Discussion
In this paper, we describe our experience in performing percutaneous transforaminal endoscopic radiofrequency ablation of the left L5 sinuvertebral nerve in a young high-level Olympic runner with somatic referred back and left leg pain. This pain was presumed to localize to a slight left L5-S1 disk desiccation causing irritation of the left sinuvertebral nerve. The disk desiccation, which also was associated with a left L5 pedicle and a pars interarticularis fracture, likely occurred because of repetitive microinjuries caused by the patient's athletic endeavors. Irritation of the sinuvertebral nerve was confirmed to be the cause of the symptoms in this patient by the following findings: a positive result on provocative diskography, intraoperative pain during palpation of the area of the L5-S1 disk desiccation, and complete resolution of pain after radiofrequency ablation. There have been published cases of pedicle fractures occurring in high-level athletes presenting with longstanding back pain, but to our knowledge the patient we describe is the first reported case of a high-level athlete presenting with a concomitant, ipsilateral pedicle and pars interarticularis fracture.7 Interestingly, the neural arch has been found to be the most vulnerable region to the typical cyclic loading forces encountered in many athletic activities, with the weakest area being the pars interarticularis followed by the pedicle.7, 8, 9 Taking these factors into consideration, it is not overly surprising that the presented patient sustained fractures to both of those areas. In the presented patient, these fractures were also associated with a disk desiccation that caused pressure on the sinuvertebral nerve causing significant somatic referred pain. After exhaustion of conservative measures, the standard treatment of nonhealing pedicle or pars fractures is fusion. The case presented suggests the use of a minimally invasive nonfusion procedure as an alternative to the more aggressive fusion option. Previously, we presented our experience with transforaminal endoscopic ablation of the basivertebral nerve, which is a terminal branch of the sinuvertebral nerve that enters the vertebral body itself and innervates the end plates, for chronic low back pain associated with Modic changes.10 Our positive findings were strengthened by a randomized controlled trial showing a statistically significant benefit to radiofrequency ablation of the basivertebral nerve complex via intraosseous means in patients with chronic low back pain with concomitant Modic changes.11 In this case report, we similarly show that endoscopic radiofrequency ablation of the sinuvertebral nerve irritated by a disk desiccation can provide for adequate, sustained pain relief. This positive result is congruent with our previous findings showing 96.1% excellent to good outcome in 52 patients whom we performed endoscopic laser ablation of the sinuvertebral nerve with a side-firing Nd-YAG laser (Lutronic, Seoul, Republic of Korea) in doses of energy between 500 and 1000 J and a 5- to 7.5-W calibration setup.4 The success of endoscopic ablative procedures is promising for patients and surgeons alike because it provides for options for pain relief with minimal associated risk in conditions that previously were either unable to be treated adequately or were aggressively treated with fusion operations with questionable results, and awake radiofrequency ablation allows to confirm the pain point during procedure (e.g., by stimulating a diskal tear the patient can confirm the nature of pain as the original pain he/she is suffering from). However, prior to advocating for these endoscopic ablative procedures to be offered as standard of care, randomized controlled trials are needed to prove in an unbiased manner that endoscopic ablation of the sinuvertebral nerve does improve outcomes when compared with placebo and the natural progression of the disease.
Conclusions
The case presented is the first, to our knowledge, of a high-level athlete presenting with a concomitant, ipsilateral pedicle and pars interarticularis fracture without a history of trauma. It also demonstrates the successful treatment of back pain and associated leg pain without any nerve root compression on imaging modalities via percutaneous transforaminal endoscopic radiofrequency ablation of a sinuvertebral nerve. We also conclude that the pedicle and facet fractures might be associated with the onside instability and chronic irritation of the sinuvertebral nerve, which were treated by this method, leading to the recovery of the patient. Further randomized controlled trials studying the efficacy and long-term outcomes of this procedure are needed.
Acknowledgments
The authors thank scientific team members Ms. Jae Eun Park, Mr. Kyeong-rae Kim, and Mr. Sang Hyuck Yoon for providing assistance in acquiring full-text articles and managing digital works.
Footnotes
Supplementary digital content available online.
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Data
Intraoperative video of the endoscopic procedure.
References
- 1.Schafer A., Hall T., Briffa K. Classification of low back-related leg pain - a proposed patho-mechanism-based approach. Man Ther. 2009;14:222–230. doi: 10.1016/j.math.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Bogduk N., Tynan W., Wilson A.S. The nerve supply to the human lumbar intervertebral discs. J Anat. 1981;132:39–56. [PMC free article] [PubMed] [Google Scholar]
- 3.Choi S.H., Adsul N., Kim H.S., Jang J.S., Jang I.T., Oh S.H. Magnetic resonance imaging undetectable epiduroscopic hotspot in chronic discogenic back pain - does sinuvertebral neuropathy actually exist? World Neurosurg. 2018;110:354–358. doi: 10.1016/j.wneu.2017.11.151. [DOI] [PubMed] [Google Scholar]
- 4.Kim H.S., Paudel B., Chung S.K., Jang J.S., Oh S.H., Jang I.T. Transforaminal epiduroscopic laser ablation of sinuvertebral nerve in patients with chronic diskogenic back pain: technical note and preliminary result. J Neurol Surg A Cent Eur Neurosurg. 2017;78:529–534. doi: 10.1055/s-0037-1604361. [DOI] [PubMed] [Google Scholar]
- 5.Kim H.S., Yudoyono F., Paudel B. Suprapedicular circumferential opening technique of percutaneous endoscopic transforaminal lumbar discectomy for high grade inferiorly migrated lumbar disc herniation. Biomed Res Int. 2018;2018 doi: 10.1155/2018/5349680. 5349680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim H.S., Yudoyono F., Paudel B. Analysis of clinical results of three different routes of endoscopic transforaminal lumbar discectomy for lumbar herniated disk. World Neurosurg. 2017;103:442–448. doi: 10.1016/j.wneu.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Parvataneni H.K., Nicholas S., McCance S.E. Bilateral pedicle stress fractures in a female athlete: case report and review of the literature. Spine (Phila Pa 1976) 2004;29:E19–E21. doi: 10.1097/01.BRS.0000105988.43472.2B. [DOI] [PubMed] [Google Scholar]
- 8.Sadiq M.Z. Bilateral pedicle stress fracture in the lumbar spine of a sedentary office worker. Eur Spine J. 2006;15:S653–S655. doi: 10.1007/s00586-006-0184-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cyron B.M., Hutton W.C., Troup J.D. Spondylolytic fractures. J Bone Joint Surg Br. 1976;58:462–466. doi: 10.1302/0301-620X.58B4.1018032. [DOI] [PubMed] [Google Scholar]
- 10.Kim H.S., Adsul N., Yudoyono F. Transforaminal epiduroscopic basivertebral nerve laser ablation for chronic low back pain associated with Modic changes: a preliminary open-label study. Pain Res Manag. 2018;2018 doi: 10.1155/2018/6857983. 6857983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischgrund J.S., Rhyne A., Franke J., Sasso R., Kitchel S., Bae H. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2018;27:1146–1156. doi: 10.1007/s00586-018-5496-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative video of the endoscopic procedure.