Abstract
The mammalian circadian and sleep-wake systems are closely aligned through their coordinated regulation of daily activity patterns. Although they differ in their anatomical organization and physiological processes, they utilize overlapping regulatory mechanisms that include an assortment of proteins and molecules interacting within the extracellular space. These extracellular factors include proteases that interact with soluble proteins, membrane-attached receptors and the extracellular matrix; and cell adhesion molecules that can form complex scaffolds connecting adjacent neurons, astrocytes and their respective intracellular cytoskeletal elements. Astrocytes also participate in the dynamic regulation of both systems through modulating neuronal appositions, the extracellular space and/or through release of gliotransmitters that can further contribute to the extracellular signaling processes. Together, these extracellular elements create a system that integrates rapid neurotransmitter signaling across longer time scales and thereby adjust neuronal signaling to reflect the daily fluctuations fundamental to both systems. Here we review what is known about these extracellular processes, focusing specifically on areas of overlap between the two systems. We also highlight questions that still need to be addressed. Although we know many of the extracellular players, far more research is needed to understand the mechanisms through which they modulate the circadian and sleep-wake systems.
Abbreviations: ADAM, A disintegrin and metalloproteinase; AMPAR, AMPA receptor; BDNF, brain-derived neurotrophic factor; Bmal1, Brain and muscle Arnt-like-1 gene; BMAL1, Brain and muscle Arnt-like-1 protein; CAM, cell adhesion molecules; Cry, cryptochrome gene; CRY, cryptochrome protein; DD, dark-dark; dNlg4, drosophila neuroligin-4 gene; ECM, extracellular matrix; ECS, extracellular space; EEG, electroencephalogram; Endo N, endoneuraminidase N; GFAP, glial fibrillary acidic protein; Ig, immunoglobulin; IL, interleukin; LC, locus coeruleus; LD, light-dark; LH, lateral hypothalamus; LRP-1, low density lipoprotein receptor-related protein 1; LTP, long-term potentiation; MMP, matrix metalloproteinases; Ncam, neural cell adhesion molecule gene; NCAM, neural cell adhesion molecule protein; NMDAR, NMDA receptor; nNOS, neuronal nitric oxide synthase gene; nNOS, neuronal nitric oxide synthase protein; NO, nitric oxide; Nrl, neuroligin gene; Nrx, neurexin gene; NST, nucleus of the solitary tract; P2, purine type 2 receptor; PAI-1, plasminogen activator inhibitor-1; Per, period gene; PER, period protein; PPT, peduculopontine tegmental nucleus; PSA, polysialic acid; REMS, rapid eye movement sleep; RSD, REM sleep disruption; SCN, suprachiasmatic nucleus; SWS, slow wave sleep; TNF, tumor necrosis factor; tPA, tissue-type plasminogen activator; TTFL, transcriptional-translational negative feedback loop; uPA, urokinase-type plasminogen activator; uPAR, uPA receptor; VIP, vasoactive intestinal polypeptide; VLPO, ventrolateral preoptic; VTA, ventral tegmental area; VP, vasopressin
Keywords: Circadian rhythms, Sleep-wake system, Suprachiasmatic nucleus, Extracellular proteases, Cell adhesion molecules, Astrocytes
Highlights
-
•
Extracellular interactions modulate circadian rhythm and sleep-wake processes.
-
•
Participating molecules and proteins include proteases and cell adhesion molecules.
-
•
Astrocytes and the extracellular matrix also likely play key regulatory roles.
-
•
The degree of overlap in these system’s extracellular mechanisms is not known.
-
•
More research focused on these dynamic extracellular processes is needed.
1. Introduction
The fields of circadian biology and sleep-wake regulation have been closely intertwined for decades, with many studies investigating how the circadian clock regulates daily rhythms in sleep and wakefulness, and in turn how arousal levels in animals affect their circadian clocks. However, research investigating the cellular mechanisms underlying circadian rhythms and sleep-wake regulation has rarely been conducted in a coordinated fashion. Thus, it is noteworthy that many of the same molecular mechanisms are critical elements of both systems. For example, circadian and sleep-wake systems involve overlapping intracellular synaptic plasticity mechanisms (e.g., Caverzasio et al., 2018; Taishi et al., 2001; Iyer et al., 2014; Antle et al., 2009). More recently, accumulating evidence supports both systems utilizing mechanisms that involve proteins (inter)acting within the extracellular synaptic space. This scenario parallels the well-documented involvement of both intracellular and extracellular protein interactions in learning- and addiction-associated synaptic plasticity (e.g., Thalhammer and Cingolani, 2014; Wojtowicz et al., 2015; Panja and Bramham, 2014; Abrahao et al., 2017; Wright and Harding, 2009; Dityatev and Rusakov, 2011). Based on these similarities, a unified review of the dynamic extracellular protein interactions involved in circadian rhythm and sleep-wake regulation seems warranted.
There is a rich literature on the neuroanatomy of the circadian and sleep-wake systems, as well as the neurotransmitters regulating both systems. There is also a great deal known about the intracellular signaling pathways and genetic underpinnings of the circadian system, while these aspects of the sleep-wake system are somewhat less clear. The extensive research focused on these critical aspects of both systems has greatly enhanced our understanding of the systems and their interactions, and there are many excellent reviews of these topics, some of which we reference in this review. Our goal here is to highlight extracellular mechanisms that complement the better-known intracellular processes underlying both regulatory systems, with a specific focus on those interacting with the extracellular matrix. With that goal in mind, we acknowledge that this review will skip over many elements central to the functioning of the two systems, and in so doing we do not mean to downplay their importance. Indeed, we believe that a complete understanding of both the circadian and sleep-wake systems and their interactions ultimately will depend on fully connecting the intracellular and the extracellular mechanisms to create a unified picture.
2. Background on the circadian rhythm and sleep-wake systems
2.1. Circadian rhythms
Endogenous circadian oscillators precisely orchestrate the daily behavioral and physiological rhythms of most organisms, while simultaneously maintaining proper phase and synchrony with the external environment. The preeminent circadian clock in mammals is located in the suprachiasmatic nucleus (SCN), a bilateral structure immediately above the optic chiasm that straddles the third ventricle. The SCN is not homogeneous; it can be divided into dorsal/shell vs. ventral/core regions based on differential expression of neuropeptides, ion channels, transporters, and receptors; amplitude and phase of clock gene expression rhythms; and afferent and efferent projections (Moore, 1983, van den Pol et al., 1996, Miller and Spear, 2006, Hastings et al., 2014), although this is likely a dramatic oversimplification of SCN organization (Morin, 2007). Lesions of the SCN eliminate daily rhythms such as the sleep-wake rhythm, body temperature rhythm, and daily hormonal rhythms, while not affecting their overall expression level (Moore, 1983, Miller, 1993, Moore, 1995). Conversely, transplanting fetal SCN tissue back into the brain after SCN lesions can restore circadian rhythms (DeCoursey and Buggy, 1986, Lehman et al., 1986, Ralph, 1996). The SCN continues to generate 24 h rhythms in neuronal activity, neuropeptide secretion, and metabolism when isolated in vitro (Gillette and Reppert, 1987, Shibata and Moore, 1988, Prosser and Gillette, 1989, Herzog, 2007, Gillette and Wang, 2014). Together with many other lines of data, these results support the SCN’s role as the master circadian clock.
The SCN circadian oscillator consists of a transcriptional-translational negative feedback loop (TTFL) involving a group of clock genes that includes Period (Per) 1 and 2; Cryptochrome (Cry) 1 and 2, Brain and muscle Arnt-like-1 (Bmal1), and Clock. BMAL1 and CLOCK proteins are transcriptional regulators that increase transcription of Per and Cry genes, the mRNAs for which are then translated into proteins that slowly accumulate in the cytoplasm. Once their levels increase sufficiently, PER and CRY proteins enter the nucleus, dimerize, and inhibit the activity of BMAL1/CLOCK, thus decreasing their own transcription. For more information on the complex inter-workings of the TTFL, see detailed reviews (Gallego and Virshup, 2007, Hastings et al., 2014, Buhr and Takahashi, 2013). The TTFL is coupled to additional circadian oscillator gears, including a redox oscillator and a cell membrane oscillator that are thought to strengthen and stabilize the SCN circadian clock (Gillette and Wang, 2014, Milev et al., 2015, Hastings et al., 2014). Although the individual cellular circadian oscillators are autonomous, intercellular coupling mechanisms within the SCN further strengthen the circadian clock, creating the dominant synchronizing signals for the rest of the organism (Herzog, 2007, Evans, 2016).
SCN clock phase is modulated by many inputs. However, the primary environmental synchronizer of the clock is light stimulation of the retina, which communicates with the SCN via the retinohypothalamic tract (Rusak, 1979, Moore and Lenn, 1972). Photic stimulation triggers glutamate release from retinal ganglion cell synaptic terminals within the SCN. Glutamate activation of postsynaptic AMPA receptors (AMPARs) and NMDA receptors (NMDARs) depolarizes the neurons, increases intracellular Ca2+ levels, and activates intracellular signaling cascades (Ding et al., 1997, Mikkelsen et al., 1995, Meijer and Schwartz, 2003). When these events occur during the subjective nighttime, they trigger increases in the transcription and translation of circadian clock genes that result in a phase delay or phase advance of the clock depending on whether they occur during the early or late night, respectively. Conversely, if these events occur during the subjective day they have no effect on clock phase. Thus, the circadian clock exhibits time-dependent responses (Meijer and Schwartz, 2003, Cheng and Obrietan, 2006, Colwell, 2011). The initial phase-shifting events are thought to occur primarily in neurons in the ventral/core region of the SCN [e.g., vasoactive intestinal polypeptide (VIP)-containing neurons], which process and transmit the information to neurons in the dorsal/shell region of the SCN [e.g. vasopressin (VP)-containing neurons]. Cells in the dorsal/shell SCN subsequently generate signals to coordinate rhythmicity within the SCN and distribute rhythmic signals to the rest of the organism (Nakaya et al., 2003, Antle et al., 2007, Schwartz et al., 2010).
While we know quite a bit about the intracellular gears of the circadian clock and the pathways mediating photic phase resetting, several pressing questions remain unanswered regarding SCN clock function. It is not fully understood how SCN cells couple and synchronize, and what regulates changes in these coupling and synchronizing processes. The full diversity of cell types within the SCN and their specific functions within the circadian clock are still being defined. Also, the mechanisms restricting photic phase-resetting responses to the night are also unclear. Extracellular mechanisms may provide answers to some of these questions.
2.2. Sleep-wake system
Unlike the SCN circadian clock, the sleep-wake system is distributed across many brain regions, including the brainstem, midbrain, hypothalamus, thalamus, and cortex. Moreover, sleep is not a single phenomenon, but a complex mixture of different brain states. Sleep can be divided into distinct stages based on electroencephalogram (EEG) and electromyogram recordings, including slow wave sleep (SWS), characterized by high amplitude, low frequency brain waves, and rapid eye movement sleep (REMS), characterized by low amplitude, higher frequency EEG activity. Animals, including humans, cycle through the different sleep states in a species- and age-dependent frequency throughout the sleeping period (Scammell et al., 2017).
Although rapid cycling between sleep- and wake-like states can be observed within small regions such as cortical columns (e.g., Rector et al., 2005; discussed in Kanda et al., 2017), the global brain circuitry and neurotransmitters contributing to regulating sleep is complex, and a thorough review is beyond the scope of this paper. Broadly speaking, the system can be divided into “wake-promoting” and “sleep-promoting” areas (keeping in mind that most of these areas are heterogeneous in their cellular composition, e.g., Yu et al., 2018).
Monoaminergic wake-promoting areas include the locus coeruleus (LC), raphe nuclei, ventral tegmental area (VTA), tuberomammillary nucleus, parabrachial nucleus, pedunculopontine tegmental nucleus (PPT) and laterodorsal tegmental nucleus. Neurons in these areas, especially the cholinergic parabrachial nucleus and PPT neurons, project to the cholinergic basal forebrain, which in turn sends projections throughout the cortex. These neurons generate much of the alerting signals for the brain (Scammell et al., 2017). Another set of neurons critical for arousal are orexin-containing neurons in the lateral hypothalamus (LH). These LH neurons project to the thalamus as well as to sleep-promoting regions discussed below (Chemelli et al., 1999, Lin et al., 1999, Nambu et al., 1999). SWS-promoting areas include the ventrolateral preoptic (VLPO) and medial preoptic areas, the parafacial zone, and GABAergic neurons in the basal forebrain. Neurons in all of these areas promote sleep at least in part by inhibiting the activity of wake-promoting neurons (Krystal et al., 2013, Fisher et al., 2013, Benington and Heller, 1995a).
In addition to sleep-promoting neurons inhibiting the wake-promoting neurons mentioned above, REMS regulation involves the sublaterodorsal nucleus, which is activated by PPT/laterodorsal tegmental nucleus cholinergic signals as well as by the decrease in LC- and raphe-induced inhibition that occurs during SWS. The sublaterodorsal nucleus, along with two reticular nuclei, acts on the medulla to inhibit motor activity and on the ventrolateral periaqueductal gray to promote REMS (Broese et al., 2012). For more detailed information on the neuroanatomy and neurochemistry of sleep, see several excellent reviews (Scammell et al., 2017, Fraigne et al., 2015, Eban-Rothschild et al., 2018).
As with the circadian system, there are still many outstanding questions regarding the sleep-wake system. Included among them are the distinct functions and mechanisms underlying SWS vs. REMS. Other questions include why regular cycling between different sleep states is important, and what are the mechanisms controlling these state changes. A possibility explored in this review is that mechanisms regulating sleep-wake and sleep state transitions, as well as the functional properties of sleep may involve extracellular processes. It will be important going forward to gain a better understanding of what triggers the different state transitions at both local and global levels, and how the regular cycling between sleep states enhances the restorative actions of sleep.
2.3. Circadian-sleep connection
A conceptual model of how the daily sleep-wake cycle is generated invokes two distinct processes: a homeostatic “Process S” and a circadian clock-generated “Process C”. Process S accumulates while an animal is awake, slowly increasing the drive to fall asleep. Process C, an alerting signal, waxes and wanes with the activity of the circadian clock. During the animal’s active phase Process S and Process C increase in parallel, keeping the animal alert and active. However, as the day progresses Process C reaches its peak and starts to decline, while Process S continues to increase. Eventually, the sleep-promoting Process S overcomes the diminished alerting signal of Process C and the animal falls asleep. While the animal sleeps, Process S dissipates, and Process C, having reached is nadir, begins to increase. Once Process C reaches and surpasses Process S the animal awakens to begin a new cycle (Borbely, 1982, Borbely et al., 2016). Although simplistic, this model succinctly illustrates the interactive nature of the two systems.
The circadian signal regulating sleep includes SCN efferents to the subparaventricular zone, which sends excitatory projections to the medial preoptic and dorsomedial hypothalamus, the latter of which sends additional excitatory projections to LH orexin neurons and to the LC (Deurveilher et al., 2002, Borbely et al., 2016). Because SCN neuronal activity is higher in the day, the initial output from the SCN is thought to be inhibitory in nocturnal animals and excitatory in diurnal animals. Distinct from the circadian signals emanating from the SCN, there are distributed circadian influences on sleep. For example, the circadian clock gene Bmal1 regulates the rhythmic production of histamine in wake-promoting tuberomammillary neurons. Selective Bmal1 deletion in these neurons, rendering them arrhythmic, disrupts circadian sleep-wake rhythms without disrupting circadian rhythms overall (Yu et al., 2014). Another circadian clock gene, Rev-erbα, regulates circadian dopamine production in the VTA (Chung et al., 2014). There are also interesting data pointing to Bmal1-supported circadian rhythmicity specifically in muscle cells being important for normal sleep regulation (Ehlen et al., 2017).
The nature of the homeostatic “Process S” is less clear, and likely encompasses multiple factors. Examples of postulated molecules include extracellular adenosine, which has been shown to increase during wake in parallel with higher metabolic activity and to decrease during sleep as metabolism wanes (Benington and Heller, 1995b, Holst and Landolt, 2015); prostaglandin D2, which also accumulates during wake, activates DP1 receptors and increases extracellular adenosine levels (Huang et al., 2014); and cytokines such as interleukin (IL)-1β and tumor necrosis factor (TNF)α (Clinton et al., 2011). Central to the concept of “Process S” is that sleep serves a restorative function that allows the brain to consolidate synaptic changes generated by previous events, replenish energy stores, and eliminate accumulated metabolic byproducts (Kuhn et al., 2016, Cirelli and Tononi, 2017).
While the interactions between Process C and S provide an elegant conceptual model of the interplay between these two systems, it provides little insight into the cellular mechanisms that regulate the cycling between different sleep states, between sleep and wakefulness, and between different phases of the circadian clock. Although the circadian and sleep-wake systems are quite distinct, it is noteworthy that they share many cellular processes. Relevant to this review, accumulating evidence supports both systems utilizing extracellular processes that overlap the synaptic mechanisms associated with learning, memory, and drug addiction. These extracellular mechanisms include changes in enzymatic activity, protein-protein interactions, cellular morphology involving the extracellular matrix (ECM), ECM-associated proteins, cell-adhesion molecules, cell-attached proteins, extracellular proteases, and astrocyte-associated processes (e.g., Panja and Bramham, 2014; Abrahao et al., 2017; Wright and Harding, 2009; Ota et al., 2013; Slaker et al., 2016). One thought is that these shared extracellular mechanisms serve in part to integrate phasic signaling processes across longer timeframes to broadly regulate the excitatory-inhibitory balance of the brain. Here we review some of the evidence that these extracellular processes play critical regulatory roles in both the circadian and sleep-wake systems.
3. Extracellular dynamics modulate circadian clock and sleep-wake systems
3.1. Extracellular matrix (ECM)
The extracellular landscape contains structural and enzymatic components that are as diverse in their composition as they are in their interactions. The neural ECM consists of molecules secreted by both neurons and astrocytes that become interlocked through covalent protein-protein and protein-carbohydrate interactions. Its composition varies regionally, developmentally, and activity-dependently. The ECM can serve as a structural scaffold, restrict diffusion of soluble factors, and has even been hypothesized to serve as a form of memory storage (Tsien, 2013). The importance of the ECM to neuronal signaling has led some researchers to designate it as the fourth “essential element” of a tetrapartite synapse, together with pre- and post-synaptic neurons and surrounding astrocytes (Smith et al., 2015).
ECM molecules include chondroitin sulfate proteoglycans, heparin sulfate proteoglycans, collagen, elastin, laminin, fibronectin and hyaluronic acid. The ECM binds additional proteins, including growth factors, proteases, thrombospondins, tenascin C and R, reelin, vitronectin, plasminogen activator inhibitor-1 (PAI-1) and chemokines (Jayakumar et al., 2017, Senkov et al., 2014). The ECM also binds to cell surface proteins/receptors, creating one avenue for modulating intracellular signaling (Kerrisk et al., 2014). Depending on its composition and interacting partners, the ECM can promote or deter cell growth and movement, and can enhance or inhibit cell-cell interactions (Senkov et al., 2014). We direct readers interested in more details concerning the composition and development of the ECM to several excellent reviews (Wojtowicz et al., 2015, Senkov et al., 2014, Dityatev and Rusakov, 2011, Levy et al., 2014, O'Callaghan et al., 2017). Although, to our knowledge, the ECM composition in the SCN and in sleep-wake regulating areas have not been investigated, evidence demonstrates that a variety of extracellular factors that interact with the ECM and/or are modulated by changes in the ECM, including neighboring astrocytes, regulate both systems. We explore these factors in more detail below.
3.2. Cell adhesion molecules (CAMs)
CAMs (including the immunoglobulin super family, integrins, neurexins, neuroligins, ephrins, Eph receptors, and cadherins) are a diverse group of cell-attached proteins that interact with each other and with the ECM. They can connect adjacent neurons as well as form neuron-astrocyte connections through interactions with the ECM and other cell attached proteins, often concurrently linking with intracellular scaffolding and cytoskeletal elements (Thalhammer and Cingolani, 2014). Through these interactions CAMs can create a syncytium that functionally integrates the activities of neighboring cells by uniting their intracellular and extracellular components. Here we focus primarily on the extracellular interactions of these molecules, while acknowledging that a comprehensive picture of their actions in these systems requires connecting the extracellular processes to those inside the cells.
3.2.1. Immunoglobulin super family: NCAMs and L1-CAMS
The immunoglobulin (Ig) super family of CAMs, which includes the neural cell adhesion molecules (NCAMs) and L1-CAMs, typically bind via their Ig domains to partners on neighboring cells rather than binding to the ECM (Rudenko, 2017, Colombo and Meldolesi, 2015). In the intracellular compartment they modulate Ca2+ signaling, interact with cytoskeletal proteins, and alter the activity of multiple intracellular kinases (Colombo and Meldolesi, 2015, Sheng et al., 2013). A unique feature of NCAMs is that their interactions are sterically inhibited when they are expressed with a polysialic acid (PSA) carbohydrate chain covalently attached to their fifth Ig domain. This chain must be cleaved by an endopeptidase before transynaptic NCAM binding can occur (Bruses and Rutishauser, 2001, Varbanov and Dityatev, 2016). PSA-NCAM is primarily expressed during neurodevelopment, while NCAM in the adult brain usually lacks PSA. However, PSA-NCAM is expressed in a few regions in the adult brain (e.g., hippocampus, amygdala, and supraoptic nucleus,) and its expression in these areas increases in response to glutamate stimulation (Bruses and Rutishauser, 2001, Theodosis et al., 2004, Varbanov and Dityatev, 2016). The switch to PSA-NCAM is thought to allow long-term potentiation (LTP)- and learning-associated changes in synaptic structure (Bruses and Rutishauser, 2001, Theodosis et al., 2004, Varbanov and Dityatev, 2016, Sytnyk et al., 2017). Additionally, changes in NCAM expression have been linked to self-administration of drugs of abuse (Rudenko, 2017), and changes in stress vulnerability in mice (Sytnyk et al., 2017). L1-CAM deficient mice do not exhibit deficits in LTP, but they show changes in hippocampal synaptic transmission, learning deficits, and increased stress vulnerability (Sytnyk et al., 2017). Similar to NCAM, changes in L1-CAM are seen with animal models of drug addiction (Rudenko, 2017).
The SCN is one of the brain regions in which PSA-NCAM levels remain high in adulthood, and evidence indicates that PSA-NCAM is required for normal circadian function. Genetic deletion of NCAM or enzymatic removal of PSA with endoneuraminidase N (endo N) disrupts the period and stability of free-running locomotor activity in mice (Shen et al., 1999), and inhibits light induced phase shifts of behavioral activity rhythms (Glass et al., 2000). Endo N injections into the SCN in vivo reduce the number of light-induced c-Fos immunoreactive cells, particularly in the ventrolateral SCN (Glass et al., 2000). Importantly, in vitro endo N administration prevents phase delays induced by either glutamate administration or electrical stimulation of the optic chiasm in rat SCN brain slices, indicating that PSA-NCAM's role is intrinsic to the SCN (Prosser et al., 2003). Endo N removal of PSA in the SCN also potentiates non-photic circadian phase resetting (Fedorkova et al., 2002). These studies demonstrate the importance of PSA-NCAM for normal circadian clock entrainment.
PSA-NCAM mediates synaptic cell-cell interactions in other brain regions, and its localization pattern in the SCN suggests it may play a similar role there. In the adult mouse SCN, PSA-NCAM is localized on neuronal somas in the central SCN and adjacent to synaptic junctions, but very little is seen in the ventral SCN (Shen et al., 1999). PSA often is associated with cells expressing light-induced c-Fos, which are generally cells that receive retinal input (Glass et al., 2003). In SCN astrocytes, PSA-NCAM is predominately located along fine processes between opposing neuronal somas and associated with synaptic junctions and small blood vessels, but not on larger processes or cell bodies (Shen et al., 1999).
There are striking circadian changes in PSA-NCAM expression in the SCN. In hamster SCN, PSA expression is rhythmic in both light-dark (LD) and constant dark (DD) conditions, with higher levels during the day than at night (Glass et al., 2003). Similar rhythms are found in rat SCN maintained in vitro (Prosser et al., 2003). The in vivo PSA rhythms are slightly blunted in DD conditions, suggesting regulation by both the circadian clock and photic input (Glass et al., 2003). Consistent with this conclusion, PSA expression in the SCN is induced in vivo by light stimulation at CT19, and in vitro by glutamate treatment (Glass et al., 2003, Prosser et al., 2003). The exact nature of PSA’s role in phase shifting is still not known, but the induction of PSA by light together with the effects seen in response to PSA removal suggests a role in photic signaling (Glass et al., 2003). Interestingly, while glutamate does not generate phase shifts during the daytime, it still induces PSA expression at this time, indicating that while PSA induction may be involved in the phase shifting process, PSA induction by itself is not sufficient to generate phase shifts (Prosser et al., 2003).
Coordinating and synchronizing cells within the SCN could involve NCAM acting through both PSA-dependent and –independent mechanisms. Initial assessments of NCAM in the SCN utilized a transgenic NCAM knockout that completely lacks the Ncam gene (Shen et al., 1999). However, Ncam encodes three NCAM isoforms (180,140, and 120 kDa) that have distinct structures and functions. NCAM 180 is the isoform that is glycosylated with PSA; NCAM 180 and NCAM 140 are transmembrane proteins with intracellular regions; and NCAM 120 is membrane-attached with no intracellular region. A comparison of the entrainment and phase-resetting phenotypes of different NCAM isoform knockouts supports the hypothesis that NCAM, but not PSA, is needed for synchronization to LD cycles, while PSA and its NCAM carrier are important for free-running periods in DD (Shen et al., 2001). However, the molecular mechanisms through which PSA-NCAM gates phase shifting are still unclear. One possibility is that PSA interacts with secreted factors such as brain-derived neurotrophic factor (BDNF). To this end, it has been shown that endo N removal of PSA from NCAM in the SCN abolishes the sensitizing effect of BDNF on mouse photic phase resetting (Glass et al., 2004). Interactions with L1–CAM may also be important for PSA-NCAM's role in the SCN. L1-CAM protein is expressed at high levels in the SCN, and appears to be associated with retinal inputs (Yamada et al., 2003). Continuous infusion of anti-L1-CAM antibody into the 3rd ventricle disrupts circadian rhythms during the infusion period and results in a phase shift in the free running rhythm of locomotor activity for several days after infusion (Yamada et al., 1999). In summary, although the detailed mechanisms remain unclear, PSA-NCAM appears critical for photic phase resetting in the SCN.
Research suggests that PSA-NCAM is also important in the sleep system. For example, PSA-NCAM is found surrounding wake-promoting neurons in the adult hypothalamus and brainstem, and to a lesser extent around neurons in sleep-promoting brain regions like the VLPO and the ventrolateral periaqueductal gray (Black et al., 2009). PSA is also expressed at high levels in the nucleus of the solitary tract (NST), a brainstem area associated with sympathetic nerve activity and arousal state (Bokiniec et al., 2017). These authors found that endo N alters astrocyte morphology and neuronal activity in the NST. Regarding sleep regulation more directly, another study found that six hours of sleep deprivation increases PSA-NCAM immunoreactivity in the median eminence of the hypothalamus, while removing PSA with endo N decreases REMS during the latter part of the sleep period, decreases the number of REMS episodes, and shortens the mean duration of REMS in rats (Black et al., 2009). These data suggest that PSA-NCAM-dependent synaptic restructuring is necessary for REMS production. As with the circadian system, much more work is needed to understand the extent and mechanisms of its involvement in sleep regulation.
3.2.2. Neurexins and Neuroligins
Another set of CAMs includes the neurexins, which are located on presynaptic neurons, and their neuroligin binding partners, which are located postsynaptically or on astrocytes (Reissner et al., 2013, Rudenko, 2017). Although they have not been investigated extensively in the adult brain, evidence suggests that changes in neurexin expression accompany changes in synaptic signaling that occur after repeated cocaine exposure (Kelai et al., 2008). Neuroligins can signal in both anterograde and retrograde directions to alter synaptic signaling properties (Futai et al., 2007, Liu et al., 2016, Jiang et al., 2017). Importantly, neuroligin-neurexin interactions are modulated by extracellular proteases (Smith et al., 2015).
Neurexins and neuroligins may play a role in mediating the diurnal variations in neuronal activity in the SCN. Cell autonomous, diurnal rhythms have been found in the expression and splicing of neurexin genes in the SCN of mice (Shapiro-Reznik et al., 2012). Neurexin genes (Nrx1/2/3) encode two families (α and β) each with multiple splice variants (Reissner et al., 2013). Diurnal rhythms are found in the transcription of some but not all variants (Shapiro-Reznik et al., 2012). Consistent with these data, a separate report indicates that expression of the neurexin binding partner, Nlg1, is higher in the day than the night in mouse forebrain. Moreover, several E-boxes were found upstream of Nlg1, and the binding of BMAL1 and CLOCK to one E-box varies with the time of day (El Helou et al., 2013).
Since neurexins can influence the excitatory/inhibitory synaptic balance, their expression in relation to post-synaptic scaffolding proteins (PSD-95 and gephryn) was assessed in the SCN. Protein levels of PSD-95, gephyrin, and neurexin-2α exhibit diurnal variations in the mouse SCN in vivo. Gephryin levels are elevated in the dark period and minimal in the day, while PSD-95 levels are high during the day and low at night (Shapiro-Reznik et al., 2012). Similar rhythms in these mRNA transcripts and proteins are seen in immortalized rat SCN2.2 cells (Shapiro-Reznik et al., 2012). Importantly, siRNA mediated suppression of neurexin transcripts in SCN2.2 cells affects the levels of gephyrin and PSD-95, supporting a role for neurexin transcripts in maintaining circadian rhythms in these synaptic scaffold proteins (Shapiro-Reznik et al., 2012). These data raise the exciting possibility that circadian rhythms in neurexin expression influence the excitatory-inhibitory synaptic balance in the SCN and/or daily rhythms in synaptic remodeling.
Neuroligins also influence sleep processes. Sleep deprivation decreases expression of Nlg1 in mouse forebrain, with results indicating that increased sleep pressure decreases the expression of Nlg1 containing an insert in splice site B (El Helou et al., 2013). These changes are correlated with decreases in synaptic NLG1 levels in the anterior forebrain of mice. Additionally, Nlg1 knockout mice have decreased wakefulness and increased SWS. Sleep deprivation also decreases binding of transcription factors to the Nlg1 E-box (mentioned above), suggesting a possible connection between circadian and sleep homeostatic modulation of Nlg1 expression (El Helou et al., 2013).
A second study found similar changes in sleep-wake regulation in Nlg1 knockout mice, with evidence for enhanced neuronal synchrony in these mice during sleep (Massart et al., 2014). Interestingly, using transcriptomics, they found that sleep deprivation induces similar changes in gene expression in both Nlg1 knockout and wildtype mice, suggesting the synaptic changes in Nlg1 expression may be downstream of the molecular pathways driving the transcriptional response to sleep (Massart et al., 2014). They also found differentially methylated and hydroxymethylated genomic regions following sleep deprivation that implicate molecular pathways involved in neurotransmission, cellular assembly, and metabolism (Massart et al., 2014). In particular, members of the Nrx-Nlg family were differentially hydroxymethylated following sleep deprivation (Massart et al., 2014).
Interestingly, transgenic mice expressing a form of Nlg3 with a missense mutation exhibit altered EEG spectral profiles even though they exhibit a normal duration and distribution of sleep-wake states (Liu et al., 2017). These changes are different from those seen in Nlg1 knockout mice, suggesting distinct roles for different neuroligin family members (Liu et al., 2017). The idea of differential neuroligin involvement in sleep regulation is further supported by data showing that immunohistochemical expression of neuroligin 2 increases in wakefulness-promoting orexin neurons in the LH of mice subjected to 6 hours of sleep deprivation (Matsuki et al., 2015). The authors also found that in these same orexin neurons the expression of α1 subunit-containing GABAA receptors increases after 6 hours of sleep deprivation (Matsuki et al., 2015). Because GABA release by VLPO neurons promotes sleep in part by inhibiting orexin neurons (Krystal et al., 2013), further investigation of the mechanism behind neuroligin 2 regulation of the α1-GABA A-receptors could clarify the role(s) of cellular adhesion molecules in sleep.
The involvement of neuroligins in sleep is further corroborated by research in Drosophila, in which null mutant dNlg4 flies exhibit abnormal sleep behavior, sleeping significantly less each night with longer sleep onset latency than wildtype flies (Li et al., 2013). They also exhibit more sleep episodes and shorter sleep-bout duration, suggesting disrupted sleep consolidation (Li et al., 2013). DNlg4 is expressed in large ventrolateral clock neurons, and whole-cell current-clamp recordings of these neurons indicate that dNlg4 flies have impaired GABA transmission. Collectively, their results demonstrate that dNlg4 regulates sleep in Drosophila by modulating inhibitory synapse function (Li et al., 2013).
Neurexins have not been studied as extensively with respect to sleep regulation. However, in Drosophila, dNrx1 gene inactivation decreases the total amount of daytime sleep (Larkin et al., 2015). Moreover, deletion of neurexin using two null mutant Drosophila strains (nrx273 and nrxΔ83) reduces nighttime sleep, decreases sleep episode length, and increases the number of sleep episodes (Tong et al., 2016). Data demonstrating that a trans-heterozygote strain with a partial reduction in neurexin expression exhibits a corresponding decrease in sleep suggests that the amount of sleep loss is correlated with the amount of neurexin reduction. Mechanistically, the effect on sleep in response to neurexin knockout or reduction appears to be due to decreased Ca2+ signaling (Tong et al., 2016).
In summary, there is growing evidence supporting neurexin/neuroligin involvement in both the circadian and sleep-wake systems. Moreover, the Drosophila results along with data showing CLOCK/BMAL regulation of sleep-associated neuroligin expression suggests an enticing regulatory link between the two systems involving CAMs. Nevertheless, there are critical gaps in our understanding of the mechanisms through which they participate in circadian and sleep-wake processes. In particular, how changes in their expression and/or interactions within the extracellular space translate into changes in intracellular signaling has yet to be elucidated. With respect to the sleep-wake system in particular, more information on regionally specific roles of neurexin and neuroligin is also needed.
3.2.3. Shank3
Shank3 is a postsynaptic scaffolding protein that interacts with neuroligins and glutamate receptors, and can regulate synaptic plasticity in part through changing the structural organization of dendritic spines (Iasevoli et al., 2013, O'Connor et al., 2014). Thus, while not technically a CAM, evidence supporting its involvement in circadian rhythms and sleep-wake regulation makes it worth mentioning in this context. Time-of-day dependent differences in Shank3α expression are seen in the hippocampus and striatum of mice housed in LD conditions that correlate with rhythms in serum melatonin levels (Sarowar et al., 2016). Eight weeks after reversal of the LD cycle the rhythms of Shank3 in the hippocampus are reversed, while the rhythms in the striatum remain unchanged (Sarowar et al., 2016). The authors interpreted this to mean that Shank3 expression is modulated by both circadian and non-circadian mechanisms. They also found that physical activity increases Shank3 in the thalamus and cortex, while it decreases Shank3 in the striatum (Sarowar et al., 2016). While Shank3 levels have not been assessed in the SCN or in DD conditions, the diurnal variations across multiple brain regions combined with the evidence pointing to dynamic synaptic structure in the SCN (discussed below) suggest that an investigation of Shank3 proteins in the SCN is warranted.
Shank3 may also participate in sleep regulation. Genomic analysis of patients with clinical conditions that include experiencing epileptic seizures during SWS (e.g., Landau-Kleffner syndrome) revealed that a number of genes associated with cellular adhesion molecules, including Shank3, contain variations in copy number (Lesca et al., 2012). Although the pathology of these syndromes is likely multifactorial, the rhythms in Shank3 expression mentioned above raise the possibility that it may be important for sleep state transitions.
3.2.4. Eph-ephrins
Another group of CAMs that has been implicated in both the circadian and sleep-wake systems includes the Eph receptors and their ephrin ligands. Eph receptors, which are tyrosine kinase receptors, are categorized as A-type or B-type, with A-type primarily binding ephrinA's and B-type binding ephrinB's (Dines and Lamprecht, 2016). Eph receptors and their ligands are both membrane-bound, can connect neighboring neurons and astrocytes, and can signal in both anterograde and retrograde directions (Papouin et al., 2017, Thalhammer and Cingolani, 2014, Dines and Lamprecht, 2016). Eph-ephrin signaling is important during neurodevelopment, where it participates in cell-cell attraction and repulsion, as well as modulating dendritic spine morphology and synapse formation (Dines and Lamprecht, 2016). In the adult brain Ephs and their ligands are important for modulating memory formation and synaptic plasticity events in the hippocampus and other limbic areas (Dines and Lamprecht, 2016, Wiera and Mozrzymas, 2015).
Eph-ephrin interactions have not been studied extensively in the SCN, but there are a couple of studies that point to their involvement in circadian clock mechanisms. The EphA4 receptor is expressed in the SCN and its expression is decreased in Clock mutant mice (Freyburger et al., 2016). Additionally, the number of PER1 immunoreactive cells is reduced in the SCN of EphA4-/- mice when compared to wildtype mice (Kiessling et al., 2017). EphA4-/- mice exhibit reduced wheel-running activity, longer endogenous periods under DD, and shorter periods under constant light compared to their wildtype counterparts (Kiessling et al., 2017). EphA4-/- mice also exhibit smaller phase delays in response to light pulses during the early subjective night, and a corresponding reduction in light-induced c-FOS expression (Kiessling et al., 2017). Thus, EphA4 is required for the normal maintenance and entrainment of circadian rhythms, but the molecular mechanisms through which EphA4 acts are not clear. In the adult hippocampus, EphA4 promotes the retraction of dendritic spines and down regulation of AMPARs (Murai et al., 2003). It is possible that EphA4 plays a similar role in the SCN, where daily rearrangements in astrocytic processes have been extensively characterized (see below).
Eph-ephrin interactions are also implicated in sleep regulation. For example, EphA4 knockout mice exhibit reduced levels of REMS (Freyburger et al., 2016). They also have reduced SWS, both at baseline and after 6 hr sleep deprivation, with data suggesting a role for Eph4a in shaping cortical oscillations but not necessarily in the response to elevated sleep pressure (Freyburger et al., 2016). Conversely, two microarray studies found decreases in the expression of Ephrin B3 in the forebrain [(Mongrain et al., 2010) discussed in O'Callaghan et al. (2017)] and cortex (Mackiewicz et al., 2009) of wildtype mice undergoing sleep deprivation. Together with the previously reviewed data on NCAM and neurexin/neuroligin involvement in the sleep-wake system, the molecular response to sleep deprivation may include changing the mixture of CAMs and other extracellular-interacting receptors in order to alter synaptic signaling parameters. Further, these extracellular molecules appear to be necessary for maintaining normal sleep architecture. Future research examining the differential expression and regulation of these molecules and elucidating their interactions with intracellular signaling processes will clarify their role in maintaining both circadian and sleep homeostasis.
3.2.5. Integrins
Integrins are CAM heterodimers composed of α and β subunits, where the α subunit confers ligand specificity and the β subunit interacts with intracellular factors to initiate signaling cascades. Activation of integrins can be “inside-out”, where an initial intracellular ligand binds to the β subunit thereby altering interactions of the α subunit with its extracellular ligands, or “outside-in”, where the initial stimulus is an extracellular ligand binding to the α subunit, which in turn affects β subunit intracellular actions (Park and Goda, 2016). Integrins are important for synaptic plasticity. During hippocampal LTP, β1- and β3-integrins participate in altering dendritic morphology, glycine receptor expression, and glutamate receptor signaling (Park and Goda, 2016). Likewise, cocaine addiction-associated synaptic plasticity the nucleus accumbens involves β3-integrin-induced changes in AMPAR and BDNF levels (Zhang et al., 2015).
The involvement of integrins in the SCN circadian clock has, to our knowledge, not been investigated. However, there is evidence for integrins participating in sleep regulation. For example, in an investigation that screened human saliva for markers of sleep deprivation, individuals who experienced 30 hours of sleep loss have higher Integrin αM levels. They also found that sleep deprivation increases the expression of a homologous protein, Integrin α5, in Drosophila (Thimgan et al., 2013). A separate study found that sleep deprived mice exhibit decreases in Integrin α4 and increases in Integrin α10 in the forebrain [(Mongrain et al., 2010), discussed in O'Callaghan et al. (2017)]. Finally, a microarray study found sleep-induced changes in mRNA expression for several integrins in the cortex (Mackiewicz et al., 2007). Although these data provide no mechanistic details, they support functional roles for integrins in sleep. Given the known parallels between synaptic plasticity mechanisms and those involved in the circadian and sleep-wake systems, we believe that additional research exploring integrin actions within both systems would be informative.
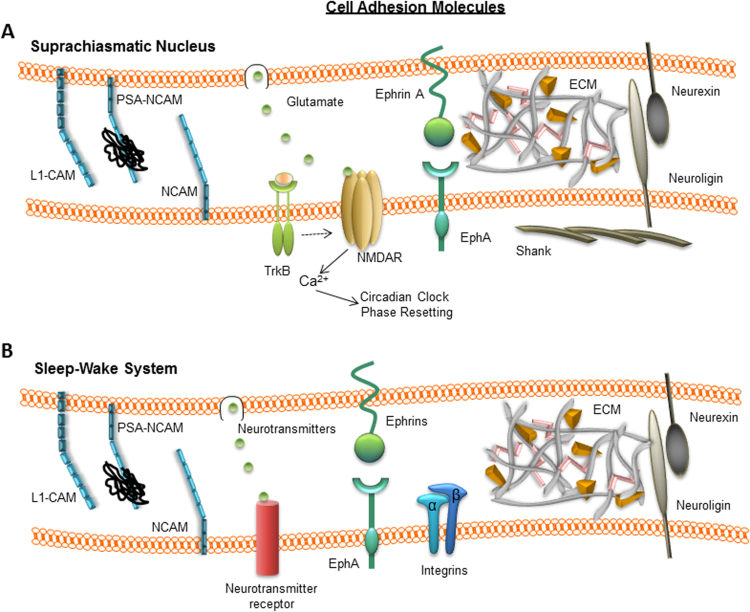
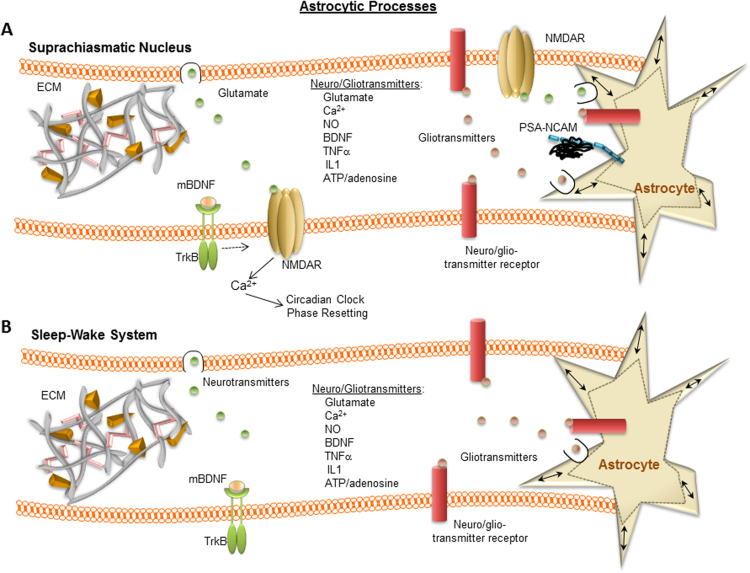
In summary, there is broad evidence for CAMs participating in both the circadian and sleep-wake systems (Fig. 1, Table 1). The degree of support varies between the two systems and on the specific type of CAM. In many cases the data are just correlational, while in some cases the evidence includes more functional detail. Nevertheless, one could postulate that through their ability to structurally connect neurons and astrocytes to each other and to the ECM, CAMs may dynamically modulate cell coupling within both the circadian clock and sleep-wake systems in ways that broadly shift the neuronal excitatory/inhibitory signaling balance. However, much more research is needed to clarify the mechanisms involved, and how much they are the same or different between the two systems.
Fig. 1.
Cell adhesion molecules implicated in SCN circadian system (A) and sleep-wake system (B) modulation. For the sleep-wake system, note that the figure collates data from a variety of brain regions. The strength of the data in both systems varies, from simple mRNA or protein expression through extensive functional evidence. The figure does not attempt to represent all of the cell adhesion molecules, transmitters, or interactions that are known or theorized to participate in each system, but rather aims to illustrate the potential commonalities and differences between the systems.
Table 1.
Summary of evidence supporting involvement of extracellular interacting proteins and molecules in the SCN circadian system and sleep-wake system.
| Protein | General function | Circadian Rhythm Effects in SCN | Sleep Effects Across Brain Regions | Citations |
|---|---|---|---|---|
| CAMs & related | ||||
| EphA4 | Cell adhesion molecule | Disrupted circadian function in EphA4-/- mice; necessary for maintenance and entrainment of circadian clocks, expressed in SCN and expression decreases in Clock mutant mice | EphA4-/- mice display reduced REMS, and reduced NREMS. | Kiessling et al., 2017; Freyburger et al., 2016 |
| Ephrin B3 | Cell adhesion molecule | Unknown | Sleep deprivation decreases expression of Ephrin B3 in forebrain and cortex. | Mongrain et al., 2010; Mackiewicz et al., 2007; O'Callaghan et al., 2017 |
| Integrins | Cell adhesion molecule | Unknown | Increased levels of αM integrin in human saliva after 30 h sleep loss; sleep deprivation decreases Integrin α4 and increases Integrin α10; sleep deprivation in Drosophila increases α5-integrin expression; sleep induces changes in integrin mRNA expression in cortex | Thimgan et al., 2013; O'Callaghan et al., 2017; Mackiewicz et al., 2007; Mongrain et al., 2010 |
| L1-CAM | Cell adhesion molecule | Infusion disrupts circadian phase shifts and SCN architecture | unknown | Yamada et al., 1999; Yamada et al., 2003 |
| (PSA)-NCAM | Cell adhesion molecule | Induced by light and involved in circadian clock entrainment; removal of PSA disrupts circadian rhythms; protein expression high during day, low at night; localized to neuronal somas and astrocytic fine processes in SCN | Expressed in hypothalamus, brainstem, VLPO, ventrolateral periaqueductal grey; increased immunoreactivity in median eminence after sleep deprivation; removal of PSA in brain decreases REMS, decreases REMS episodes and shortens mean duration of REMS | Shen et al., 1999; Glass et al., 2000; Prosser et al., 2003; Fedorkova et al., 2002; Glass et al., 2003; Shen et al., 2001; Glass et al., 2004; Black et al., 2009; Bokiniec et al., 2017 |
| Neurexins | Presynaptic CAM | Circadian rhythm in neurexin 2α gene transcription | dNrx1 gene inactivation and neurexin deletion decreases sleep in Drosophila | Shapiro-Reznik et al., 2012; Tong et al 2016; Larkin et al., 2015 |
| Neuroligins | Postsynaptic CAM | Binding of BMAL1 and CLOCK exhibits diurnal rhythm in forebrain | Sleep deprivation influences expression levels of Nlg1and Nlg2; Nlg1 knockout mice have decreased wakefullness/increased SWS; Missense mutation in Nlg3 alters EEG spectral profiles; dNlg4 regulates sleep in Drosophila | Matsuki et al 2015; El Helou et al., 2013; Massart et al. 2014; Liu et al 2017; Li et al., 2013 |
| Shank3 | Postsynaptic scaffolding protein | Time-of-day dependent rhythms in expression | Patients with epileptic seizures during SWS have variations in copy number of Shank3 gene | Sarowar et al., 2016; Lesca et al., 2012 |
| Extracellular protease-related | ||||
| BDNF | Growth factor | Heterozygous knockout mice have reduced photic phase shifts; needed for glutamate-induced phase shifting; allows photic phase shifts during the day; mRNA and protein are high at night, low during the day | Cortical mRNA levels increase after sleep deprivation; injections of BDNF increase SWS in mice; in PPT and subcoeruleus nucleus, protein expression increases after REMS disruption | Mou et al., 2009; Liang et al., 1998; Liang et al., 2000; Michel et al., 2006; Taishi et al., 2001; Datta et al. 2015; Barnes et al., 2017; Faraguna et al., 2008; Mou et al., 2009 |
| LRP-1 | Membrane bound receptor | Expressed in the SCN; required for glutamate-induced phase shifts in vitro; heavy chain portion expression is high at night, low in day | Sleep deprivation decreases soluble LRP-1 levels in blood plasma; LRP-1 mRNA increases in cortex during sleep | Cooper & Prosser, 2014; Wei et al. 2017; Mackiewicz et al., 2007 |
| MMP-2/9 | Proteases | Expressed in the SCN; inhibiting induces phase shifts; protein expression not rhythmic; decreased MMP9 activity at ZT23 | Cortical/hippocampal mRNA levels decrease after sleep deprivation | Halter and Prosser, submitted for publication; Taishi et al., 2001 |
| Neuroserpin | Inhibits tPA/uPA | Protein expression is high in day, low at night; neuroserpin antibody allows glutamate phase shifts in the day in vitro | Unknown | Prosser & Conner, unpublished data |
| PAI-1 | Inhibitor of tPA | Expressed in the SCN; blocks glutamate induced phase shifts in vitro | Increased expression in blood of female shift workers with poor sleep quality | Mou et al., 2009; Nadir et al. 2015 |
| Plasmin | Cleave BDNF | Expressed in the SCN; inhibiting blocks glutamate-induced phase shift | Unknown | Mou et al., 2009 |
| tPA | Cleave plasminogen | Involved in glutamate-induced phase shifting; influences food anticipatory behavior; rhythmic protein expression in vitro with higher levels at night | In mice, cortical mRNA levels increase after sleep deprivation | Taishi et al., 2001; Mou et al., 2009; Cooper et al., 2017; Krizo et al., 2018 |
| TrkB | Membrane bound receptor of BDNF | Important for glutamate-induced phase resetting | Inhibiting PPT reduces REM sleep, suggesting TrkB activation is necessary for increase in REMS homeostatic drive; truncated TrkB, lacking kinase domain, increases total REMS and decreases latency to REMS | Mou et al., 2009; Barnes et al. 2017; Liang et al., 2000; Michel et al., 2006; Watson et al., 2015 |
| uPA | Cleave plasminogen | Supports phase shift in absence of tPA; no circadian rhythm detected in vitro | Unknown | Cooper et al., 2017 |
| Vitronectin | ECM Molecule | Regulation of tPA by PAI-1 requires VN | Unknown | Mou et al., 2009 |
| Gliotransmitters | ||||
| Adenosine | Nucleoside | Adenosine acting on A1 receptors can phase-shift the SCN clock and block photic phase shifts; at least some actions involve inhibiting glutamate release | Inhibits wake-promoting neurons via A2a receptors; lack of adenosine increases SWS time and enhances SWS after sleep deprivation; astrocyte-derived adenosine modulates sleep; glucose stimulates astrocytic release of adenosine in VLPO | Huang et al., 2014; Womac et al., 2009; Antle et al., 2001; Watanabe et al., 1996; Elliott et al., 2001; Sigworth and Rea, 2003; Hallworth et al., 2002; Halassa et al., 2009; Blutstein and Haydon, 2013; Scharbarg et al., 2017 |
| ATP | Nucleotide | Genes involved in ATP regulation exhibit circadian rhythms; circadian variation in production and accumulation of extracellular ATP in SCN2.2 cells and rat in vivo | Mice lacking pannexin-1 channel have inverted wake/SWS ratio and increased activity in light and dark. ATP agonists increase SWS in mice. ATP PX27 receptor expression varies with sleep state. ATP increases astrocytic release of IL1β and TNFα. | Menger et al., 2005; Womac et al., 2009; Kovalzon et al., 2017; Krueger et al, 2010; Krueger et al., 2011; Jewett and Krueger, 2012. |
| Interleukins | Cytokines | IL1β and IL-6 exhibit circadian patterns of expression in human plasma. Decreased Per and Cry expression in liver, fibroblasts and neuronal cell cultures and decrease behavioral activity in mice. Peak mRNA expression during light phase. Hippocampal microglia exhibit diurnal expression of IL1β. | IL1β protein and mRNA levels increase during wakefulness and decrease during sleep.Low doses of IL1β increase SWS while high doses suppress SWS and REMS. Mice lacking IL1β receptors have less SWS and REMS during active period. Sleep regulatory regions in the brain (cortex, brainstem and hypothalamus) contain glia expressing IL1β. Selective expression of IL1β receptor to neurons or astrocytes prevents IL1β-induced increases in sleep. Astrocytic IL1β receptors required for proper REM, NREM sleep, and production of IL-6 protein in the hypothalamus. IL-6 increases in mice that experienced sleep fragmentation. | Bauer et al., 1994; Vgontzas et al., 1997, Vgontzas et al., 2005; Cearley et al., 2013; Taishi et al., 1997; Vacas et al., 2017; Fonken et al., 2015; Fonken et al., 2015; Imeri and Opp, 2009; Del Gallo and Opp, 2014. Ingiosi et al., 2015; Ingiosi and Opp, 2016. Krueger et al., 2011. |
| TNFα | Cytokine | Plasma expression of TNFα exhibits circadian rhythms; regulates LPS-induced phase shifts of locomotor activity rhythms in mice; decreases Per and Cry expression in liver, fibroblasts and neuronal cell cultures and behavioral activity in mice. Peak mRNA expression during light phase. TNFα decreases expression of Dpb mRNA in SCN tissue. TNFα shifts PER2 rhythms in SCN astrocyte cultures. Hippocampal microglia exhibit diurnal expression of TNFα. | Wakefulness increases mRNA and protein expression of TNFα while inhibiting its activity can decrease sleep. Increases in TNFα accompany sleep fragmentation and decreased sleep quality in mice and humans. TNFα is expressed by glia in sleep regulatory regions of the brain (cortex, brainstem, and hypothalamus). TNFα receptor knockouts exhibit decreased SWS and REMS late in their active period and entire sleep period. Increases and fragments NREM sleep, inhibits REM sleep. TNFα enhances sleep like states (i.e. burstiness, synchronization and slow wave power) of cultured cortical astrocytes. | Born et al. 1997; Bredow et al. 1997; Cearley et al., 2013; Cavadini et al., 2007; Gast et al., 2012; Vacas et al., 2017; Duhart et al., 2013; Fonken et al., 2015; Fonken et al., 2015; Imeri and Opp, 2009; Jewett et al., 2015. Krueger et al., 2011. |
| Nitric oxide | Secreted gaseous molecule | Found in SCN astrocytes; modulates photic transduction; hemoglobin scavenging of NO blocks some but not all circadian effects | Wakefullness and sleep deprivation increase NO production by NOS; Nos3 expression in cerebral cortex increases during sleep; nNOS-/- mice have decreased SWS; in sleep deprived mice nNOS inhibition in basal forebrain decreases REM sleep recovery while iNOS inhibition prevents SWS recovery | Ding et al., 1994; Golombek et al., 2004; Plano et al., 2010; Artinian et al., 2001; Caillol et al., 2000; Brown et al., 2012; Mackiewicz et al., 2007; Morairty et al. 2013; Kalinchuk et al., 2006 |
3.3. Extracellular proteases
The ECM is a dynamic structure constantly being remodeled in response to extracellular proteases secreted by the surrounding cells. Extracellular proteases in the brain include thrombin, neurotrypsin, neuropsin, plasminogen, tissue-type plasminogen activator (tPA), urokinase-type plasminogen activator (uPA), and matrix metalloproteinases (MMPs). Several of these proteases have been implicated in both circadian clock and sleep-wake regulation. Although we focus primarily on their actions within the extracellular space, we provide information on their effects on intracellular signaling associated with the circadian and sleep-wake systems when it is available.
3.3.1. tPA and uPA
tPA and uPA are extracellular serine proteases produced and secreted by neurons and astrocytes in many regions of the brain, including the cortex, limbic system, hypothalamus, and cerebellum (Kalderon et al., 1990, Presta et al., 1990, Masos and Miskin, 1997, Lee et al., 2017, Medcalf, 2017). tPA and uPA share their plasminogen activating function (cleaving plasminogen to form active plasmin), upstream inhibitors (including PAI-1 and neuroserpin), downstream targets (including ECM molecules, MMPs, CAMs, and plasminogen) (Al-Horani, 2014), and some membrane-localized receptors, including low density lipoprotein receptor-related protein 1 (LRP-1) and annexin II (Archinti et al., 2011, Chevilley et al., 2015). However, the two proteases also diverge in various ways, including their mechanisms of activation and cell signaling actions.
tPA’s well established role as a neuromodulator is elegantly described in a recent review (Medcalf, 2017). Some tPA-induced effects on hippocampal learning, LTP, and LTP-associated synapse formation involve proteolytic formation of plasmin from plasminogen, followed by proteolytic activation of proBDNF to form mature BDNF (mBDNF) (Fiumelli et al., 1999, Pang et al., 2004, Pang and Lu, 2004). tPA has also been shown to modulate amygdala- and hippocampus-based synaptic plasticity through both direct and indirect interactions with NMDAR subunits (Norris and Strickland, 2007, Pawlak et al., 2005a, Pawlak et al., 2005b, Pawlak et al., 2003, Yuan et al., 2009, Obiang et al., 2012, Ng et al., 2012, Norris and Strickland, 2007, Pawlak et al., 2005a, Pawlak et al., 2005b). tPA can bind to cell-surface receptors, including LRP-1, annexin II, and epidermal growth factor receptor (Chevilley et al., 2015, Zhuo et al., 2000, Miles and Parmer, 2013), which can stimulate receptor-mediated signaling, restrict its sphere of activity, and modify its proteolytic activity (Miles and Parmer, 2013, Chevilley et al., 2015).
uPA also participates in synaptic remodeling, with the majority of uPA research in this area focused on its role in neural repair following stroke or spinal cord damage (Merino et al., 2017, Seeds et al., 2009, Wu et al., 2014). Many of uPA’s actions require binding to its uPA receptor (uPAR). Ligand-bound uPAR interacts with other cell-surface proteins, including LRP-1, integrins, and receptor tyrosine kinases. In most cases, these interactions result in internalization of the receptor-protein-ligand complex (Miles and Parmer, 2013, van Gool et al., 2015, Madsen et al., 2007).
Many uPA and tPA inhibitors, including PAI-1, PAI-2, neuroserpin, and proteinase nexin 1, are expressed in the brain (Gettins and Olson, 2016, Van De Craen et al., 2012). Of these, PAI-1 is unique in having to bind vitronectin to remain active (Declerck and Gils, 2013). Because vitronectin typically binds to the ECM, this can serve to restrict the location and activity of PAI-1 (Minor and Peterson, 2002, Podor et al., 2000). Neuroserpin, thought to be expressed solely within the central nervous system (Hastings et al., 1997, Miranda and Lomas, 2006), can also modulate cell adhesion through a tPA-independent mechanism that may involve cleavage of the CAM, N-cadherin (Lee et al., 2008).
One of the first indications that extracellular proteases influence the SCN circadian clock was data showing that the plasminogen activating cascade regulates SCN clock phase resetting. Proteins within this enzymatic cascade, including tPA, uPA, PAI-1, vitronectin, plasminogen, and plasmin are all expressed in the SCN (Mou et al., 2009, Cooper et al., 2017). tPA expression in the SCN is rhythmic, with high levels at night and low levels during the day (Cooper et al., 2017). Inhibiting tPA or plasmin (with PAI-1 or α2-antiplasmin, respectively) prevents glutamate-induced phase delays and phase advances of the SCN circadian clock in vitro (Mou et al., 2009).
Exactly how tPA modulates photic phase resetting is not clear, but one strong possibility is that it enhances BDNF signaling. As mentioned earlier, plasmin can cleave proBDNF to generate mBDNF. mBDNF activation of its receptor, TrkB, may contribute to restricting photic phase shifting to the night. Similar to tPA, BDNF levels are higher in the SCN at night and lower during the day (Liang et al., 1998). Moreover, tPA-/- mice have less mBDNF in the SCN than wildtype mice (Cooper et al., 2017, Krizo et al., 2018). Blocking TrkB receptors inhibits light- and glutamate-induced phase shifts (Liang et al., 2000, Michel et al., 2006), and light-induced phase shifts are attenuated in BDNF heterozygous mice (Liang et al., 2000). Also, administration of exogenous BDNF during the subjective day allows light and glutamate-induced shifts to occur when they normally would not (Liang et al., 2000, Michel et al., 2006, Mou et al., 2009). Importantly, inhibition of glutamate-induced phase shifts by blocking tPA activity is reversed by co-administration of plasmin or mBDNF, but not plasminogen or proBDNF (Mou et al., 2009). Together, these data support a scenario where tPA acts upstream of mBDNF as part of a gating mechanism that restricts photic/glutamate phase shifts to the night: at night, when tPA levels are high, tPA cleaves plasminogen into plasmin, which then cleaves proBDNF to mBDNF. TrkB receptor activation by mBDNF enhances the ability of glutamate signals to induce phase shifts.
Mou et al. (2009) further demonstrated that endogenous regulation of tPA activity in the SCN by PAI-1 requires vitronectin, since PAI-1 does not block phase shifts in brain slices prepared from vitronectin knockout mice (Mou et al., 2009). Interestingly, tPA activity in the SCN may also be regulated by neuroserpin. Preliminary data indicates that neuroserpin is expressed at higher levels in the day than the night in the SCN, and co-application of a neuroserpin antibody (to inhibit neuroserpin activity) with glutamate to SCN brain slices during the daytime induces a 3 h phase advance that is not seen with glutamate application alone (Prosser and Conner, unpublished data). Together, these data support tPA regulation of circadian clock phase control. However, more research on tPA’s downstream actions and upstream regulators is needed to fully elucidate the mechanisms through which the plasminogen pathway influences circadian clock function and how the circadian clock in turn feeds back on these processes.
Given the data presented above, it is somewhat surprising that tPA-/- mice entrain normally to LD cycles and exhibit minimal changes in sensitivity to light-induced phase-shifts in vivo or glutamate-induced phase shifts in vitro. The only discernable deficiency in light entrainment is that tPA knockout mice re-entrain to either an inverted light cycle or to a 6 h advance in the light cycle more slowly than wildtype litter mates (Cooper et al., 2017, Krizo et al., 2018). It is also interesting to note that tPA modulates food anticipatory behavior driven by a food-entrainable circadian oscillator that functions independently of the SCN clock (Krizo et al., 2018). This study found that tPA knockout mice have reduced wheel running activity compared to wildtype mice and altered behavioral activity patterns in response to fasting and temporally restricted food availability. The mechanisms underlying these effects remain unclear, but tPA’s involvement in food-entrained circadian behavior together with the effects of tPA seen in vitro underscores the diverse roles extracellular proteases can play in circadian oscillators.
While exploring these findings, it was determined that uPA also regulates glutamate-induced phase shifts in the SCN. The initial evidence that uPA functions in the SCN was the finding that PAI-1, which is only known to inhibit tPA and uPA, continues to block glutamate-induced phase delays in brain slices from tPA-/- mice (Cooper et al., 2017). Further, selective inhibition of uPA prevents glutamate induced phase shifts in tPA-/- but not wildtype SCN tissue, suggesting that in tPA-/- mice, uPA can compensate for the lack of tPA. Thus, it appears that either plasminogen activator is sufficient but neither is necessary for phase shifting to occur (Cooper et al., 2017).
Although the data suggest that tPA and uPA function in parallel to support glutamate-induced phase shifts, their regulation and mechanisms of action appear to be distinct. First, tPA and uPA differ in both their expression and activity patterns in the SCN in vitro. tPA expression exhibits a circadian rhythm, with higher levels at night than day, while uPA expression is not rhythmic. Additionally, using casein-plasminogen zymography as a preliminary measure of proteolytic activity in the SCN, no circadian rhythm is seen in either tPA or uPA activity (Cooper et al., 2017). Finally, unlike with tPA (Cooper et al., 2017, Krizo et al., 2018), inhibiting uPA does not change mBDNF levels in the SCN, suggesting that uPA in the SCN acts independently of mBDNF generation (Cooper et al., 2017). Taken together, these data demonstrate that tPA and uPA play functionally redundant roles regarding glutamate-induced phase resetting, but they are modulated separately and act through divergent pathways that need further investigation.
3.3.2. Matrix metalloproteinases (MMPs)
MMPs are a well-studied family of ECM-targeting proteases that can be categorized based on their substrates, e.g., whether they degrade collagen (collagenases; MMP-1, -8, and -13), or gelatin (gelatinases, MMP-2 and -9), or by their localization, e.g., whether they are membrane-bound (MT-MMPs) or soluble. There are also MMP-related proteases, including the membrane-bound a disintegrin and metalloproteinases (ADAMs) and secreted ADAMTs (ADAMs with thrombospondin motifs) (Smith et al., 2015). MMPs can be activated by other MMPs and by serine proteases, and are inhibited by tissue inhibitor of metalloproteases (TIMPs) (Malemud, 2006; Yang et al., 2011, Saftig and Reiss, 2011, Wiera and Mozrzymas, 2015). Substantial attention has been given to the actions of MMP-9 in the brain. Both increasing and decreasing MMP-9 expression can disrupt hippocampal LTP (Wiera and Mozrzymas, 2015). Increases in MMP-9 are seen in the nucleus accumbens and amygdala during withdrawal from drugs of abuse, and MMP-9-induced changes in dendritic structure in these regions enhance the propensity for relapse (Song and Dityatev, 2017). MMP-9 has been shown to modulate NMDAR membrane localization (Barrow et al., 2009), possibly through cleavage of cell-surface β-dystroglycan, Eph-ephrin proteins, or neuroligin 1 (Michaluk et al., 2007, Georgakopoulos et al., 2006, Peixoto et al., 2012), which in turn can affect intracellular scaffolding proteins such as PSD-95. MMP-9 can also cleave proBDNF to generate mBDNF, allowing it to activate its TrkB receptor and enhance NMDAR signaling (Wiera and Mozrzymas, 2015). MMP-9 enhancement of LTP could also involve cleaving cell-surface integrins and thereby disrupting cell attachments (Wiera and Mozrzymas, 2015).
MMPs also influence SCN timekeeping. Inhibiting MMP-2 and 9 in vitro in the SCN induces phase shifts that are time-of-day dependent: MMP-2/9 inhibition induces phase advances when treatments are applied during mid-subjective day and early subjective night, but not when applied during late night (Halter and Prosser, submitted for publication). These phase shifts appear to involve distinct signaling mechanisms. Although both daytime and nighttime phase-shifts induced by MMP-2/9 inhibition require activation of NMDARs, activation of plasmin and the TrkB receptor are required for daytime phase advances but not early night phase delays. Neither MMP-2 nor MMP-9 exhibit circadian rhythms in protein expression in the SCN. However, MMP-9 proteolytic activity is lowest during late night, corresponding with the time when MMP-2/9 inhibition does not phase-shift the clock. Additional research into whether MMP-2 and MMP-9 modulate the circadian clock through other known substrates, including glutamate receptors and CAMs, are on-going.
Much less attention has been paid to the involvement of extracellular proteases in sleep-wake regulation. However, Taishi et al. (2001) investigated mRNA expression of tPA and MMP-9, together with BDNF and the synaptic scaffolding protein Arc, before and after mice were sleep-deprived for 8 hours. They found that mRNA for tPA, BDNF, and Arc all increase in the cortex following sleep deprivation, while Arc mRNA levels increase in the hippocampus. Conversely, MMP-9 mRNA expression decreases in both the cortex and hippocampus after sleep deprivation (Taishi et al., 2001). They also found that increasing the ambient temperature, which increases REMS and SWS, decreases tPA, BDNF and Arc mRNA in the cortex and increases MMP-9 mRNA in the cortex and hippocampus. A microarray study (Mackiewicz et al., 2007) also found increases in mRNAs for several MMP-interacting proteins in the cortex during sleep. Together, these results suggest a connection between sleep-wake state and these genes. It would be worthwhile to investigate how these changes in mRNA translate into changes in protein expression and proteolytic activity, and further, if any of these changes contribute to the increase in sleep propensity after sleep deprivation. In this context, however, it is interesting to note that female shift workers with poor sleep quality have higher levels of PAI-1, the primary inhibitor of tPA, in their blood compared to daytime shift workers (Nadir et al., 2015). Whether the increase in circulating PAI-1 is a negative feedback response to increased transcription of tPA mRNA after sleep deprivation is still yet to be determined.
One downstream product of both tPA and MMP-9 activity that is implicated in sleep regulation is BDNF. Previous work in rats shows that cortical injections of BDNF during sleep increase SWS, while injections of a polyclonal anti-BDNF antibody or the tyrosine kinase inhibitor K252a during wakefulness decrease SWS (Faraguna et al., 2008). Also, increases in REM episodes induced by selective REMS disruption (RSD) positively correlate with increases in BDNF expression in the PPT and the subcoeruleus nucleus (Datta et al., 2015). In a recent study (Barnes et al., 2017) two TrkB antagonists (K-252a and ANA-12) were injected into the PPT of rats prior to unrestricted sleep or RSD. The results show that RSD increases BDNF expression in the PPT, which is reduced when rats are pretreated with either K252a or ANA-12. Moreover, K252a injections in RSD animals reduce REMS episodes without changing the time spent in wakefulness. This implies that TrkB activation is necessary for the increase in REMS homeostatic drive. Along these lines, knockout of the truncated form of the TrkB receptor, which lacks a kinase domain, in mice leads to increased total REMS and decreased latency to REMS while SWS architecture is unaffected (Watson et al., 2015). Interestingly, this form of the TrkB receptor is more highly expressed in astrocytes than neurons (Fenner, 2012).
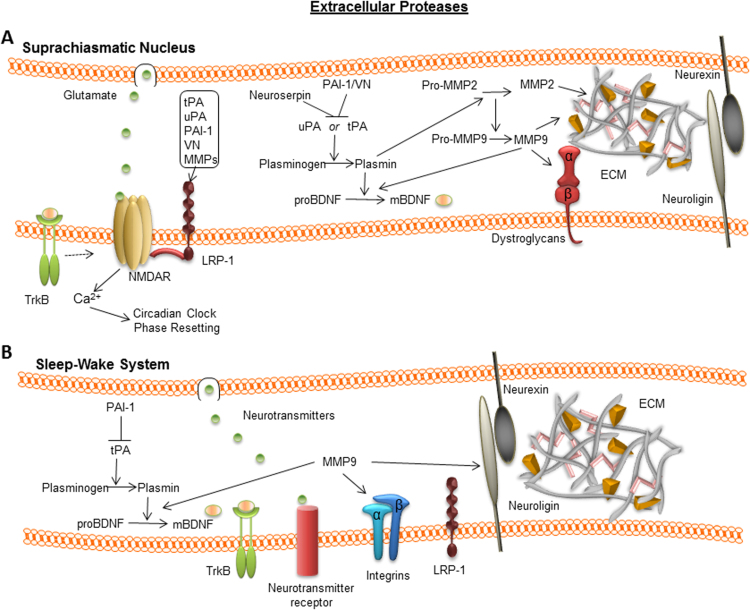
Overall, these studies support the hypothesis that extracellular proteases play important roles within both the circadian and sleep-wake systems (Fig. 2, Table 1). There is a paucity of information regarding the plasminogen pathway in the sleep-wake system relative to the circadian system, while both systems appear to be modulated by MMPs. The data suggest that one mechanism through which these proteases may act in both systems is through modulating BDNF signaling via TrkB receptors, although many other possibilities also exist. Given BDNF’s importance in synaptic plasticity generally, and circadian rhythms and sleep-wake more specifically, it will be important for future studies to explore whether BDNF and/or other proteolytic targets serve as a link between these systems, what the role(s) of these downstream targets are in each system, and to what extent they are regulated by specific extracellular proteases in each of these systems.
Fig. 2.
Extracellular proteases implicated in SCN circadian system (A) and sleep-wake system (B) modulation. For the sleep-wake system, note that the figure collates data from a variety of brain regions. The strength of the data in both systems varies, from simple mRNA or protein expression through extensive functional evidence. The figure does not attempt to represent all of the cell adhesion molecules, transmitters, or interactions that are known or theorized to participate in each system, but rather aims to illustrate the potential commonalities and differences between the systems.
3.4. Extracellular protease interacting proteins
As discussed earlier, the extracellular proteases tPA, uPA and MMP can modulate cell signaling non-proteolytically by binding to membrane-localized receptors, including LRP-1 and annexin II (Archinti et al., 2011, Chevilley et al., 2015; van Gool et al., 2015). MMP-9 has also been shown to modulate cell signaling through cleaving cell-attached receptors, including β-dystroglycan, integrins, Eph-ephrin proteins, and neuroligin 1 (Wiera and Mozrzymas, 2015, Peixoto et al., 2012). Although most of these targets and subsequent intracellular signaling processes have not been investigated in the context of either circadian rhythm or sleep-wake regulation, our lab has explored the involvement of LRP-1 in circadian clock phase resetting.
3.4.1. LRP-1
LRP-1 is a large protein that includes a 515 kDa extracellular α subunit that is non-covalently attached to an 85 kDa transmembrane β subunit (Kerrisk et al., 2014, Ramanathan et al., 2015). LRP-1 has a diverse set of ligands, including apoE, tumor growth factor-β, MMPs, PAI-1, neuroserpin, tPA, uPA, and amyloid-β. Ligand binding can trigger endocytosis or activation of multiple protein kinases (Kerrisk et al., 2014, Ramanathan et al., 2015, van Gool et al., 2015). “Shedding” of the extracellular subunit generates a soluble protein that can continue to bind ligands, which can serve a sequestration/inactivation function (van Gool et al., 2015). This shedding can be mediated by a variety of extracellular proteases, including tPA, a variety of MMPs, ADAMs, and β-secretase 1 (van Gool et al., 2015), and the resulting soluble protein can interact with other receptors, including uPARs, NMDARs and platelet-derived growth factor receptors (Ramanathan et al., 2015, van Gool et al., 2015). These receptor-LRP-1 interactions can generate functional changes linked to alterations in receptor localization. LRP-1 participates in LTP and learning and memory processes through mechanisms that involve tPA (Kerrisk et al., 2014, Zhuo et al., 2000). Evidence also suggests that, through its interaction with PSD-95, LRP-1 can regulate the surface expression of NR2B subunit containing NMDARs (Maier et al., 2013).
LRP-1 could serve as a point of convergence for tPA, uPA, MMPs, and other regulators of the circadian clock, including NMDARs and BDNF/TrkB signaling. LRP-1 can both regulate and respond to the extracellular environment: via its endocytic activity it is able to control the levels of a variety of extracellular proteins, including tPA, uPA, vitronectin, PAI-1, and MMPs. Our lab has found that LRP-1 influences circadian clock phase shifting, as inhibiting LRP-1 abolishes glutamate-induced phase shifts of SCN neuronal activity rhythms in vitro (Cooper and Prosser, 2014). While the mechanisms underlying these actions remain unclear, the data suggest that tPA is not required for LRP-1 to modulate circadian clock phase. However, because LRP-1 inhibits glutamate-induced phase shifts, we hypothesize that LRP-1’s actions involve interactions with NMDARs and/or mechanisms downstream of NMDAR activation.
In summary, there has been minimal attention given to the potential involvement of receptors (and their intracellular signaling cascades) that interact with extracellular proteases in either the circadian or sleep-wake systems (Fig. 2, Table 1). To the best of our knowledge, ours is the only investigation of LRP-1 in the SCN, and we are not aware of research investigating the function of LRP-1 in the sleep-wake system. Nevertheless, the microarray study by Mackiewicz (2007) found that LRP-1 mRNA expression increases in the cortex during sleep. In light of LRP-1’s ability to endocytose numerous extracellular molecules and to modulate glutamatergic signaling, we believe continued exploration of LRP-1 in the circadian system, as well as an investigation of LRP-1 in the sleep-wake system, is warranted. We also believe investigating other extracellular protease-interacting receptors within the context of both systems would be worthwhile.
3.5. Astrocytes
Another critical facet of the extracellular environment is changes in astrocytic structure and signaling properties. Astrocytes exhibit structural dynamics that can involve interactions with the ECM, which result in volumetric and spatial changes in the extracellular space (ECS) and changes in the extent of neuronal appositions. Astrocytic morphological changes and how they modulate neuronal activity in the neuroendocrine system have been extensively investigated in the supraoptic nucleus, as recently reviewed (Clasadonte and Prevot, 2017). However, similar changes have also been shown to occur in the hippocampus (Pannasch et al., 2014), raising the possibility that they participate in learning and memory processes. Changes in astrocyte morphology have also been shown in the olfactory bulb in response to fasting and satiety signals (Daumas-Meyer et al., 2017). Astrocytes also modulate brain processes, including those linked to learning and memory and to drug addiction, through releasing and responding to signaling molecules (Ben Achour and Pascual, 2012, Rose et al., 2018, Maurer and Williams, 2017, Lacagnina et al., 2017). Their critical involvement in brain signaling through multiple mechanisms led to their inclusion within a ‘tripartate synapse’ functional unit together with pre- and post-synaptic neurons (Perea and Araque, 2002, Fields et al., 2013).
Astrocytes contribute to the regulation of both the circadian and sleep-wake systems (Areal et al., 2017, Ruben and Hogenesch, 2017). The mechanisms through which astrocytes participate in the two systems, however, are not fully understood. Some studies have focused on changes in astrocyte morphology, while others have investigated whether astrocytes interact with neuronal signals by actively secreting gliotransmitters. Regardless of the detailed mechanisms, these astrocytic processes are closely tied to changes in ECM, ECS and extracellular molecules. Here, we discuss the data linking astrocytes and the ECS in both systems.
3.5.1. Astrocyte morphology
Astrocytic morphology adjusts to changing physiological conditions by extending and retracting processes into and out of synaptic regions, which can dramatically alter the physical parameters of synaptic signaling, including synaptic cleft volume, the extent of neuron-neuron contact, the rate of astrocytic clearance of neurotransmitters and other substances from the synaptic cleft, and the degree to which substances can diffuse in and out of the synaptic active zone (Papouin et al., 2017). These structural changes involve interactions with the ECM and associated molecules (Muir et al., 2002, Song and Dityatev, 2017). In some cases, protein-protein interactions directly connect neurons and astrocytes. For example, EphA4-EphrinA3 connections have been identified between dendritic spines and astrocytic processes in the hippocampus (Thalhammer and Cingolani, 2014). Therefore, changes in astrocytic morphology may be both a consequence and a regulator of changes in ECM molecules.
Circadian rhythms in astrocytic morphology in the SCN have been studied for many years. The first demonstration of astrocyte circadian rhythms was in 1993, when daily changes in glial fibrillary acidic protein (GFAP) were found in the SCN of Syrian hamsters (Lavialle and Serviere, 1993). The distribution of GFAP immunoreactivity exhibits diurnal rhythms in both constant light and DD, moving from a distributed network pattern during the day to a condensed and isolated staining pattern at night. Together with several subsequent studies (Shen et al., 1999, Elliott and Nunez, 1994, Moriya et al., 1996) there is broad support for the existence of GFAP rhythms in the SCN, and because GFAP is essential for astrocytic cytoskeletal organization, they point to structural plastic changes in SCN cell networks (Becquet et al., 2008).
Astrocytes in the SCN undergo rhythmic structural rearrangements in addition to rhythms in GFAP. For example, there are day/night variations in glial and axonal terminal coverage on VIP neurons (Becquet et al., 2008). The data support a model where glial coverage of dendrites changes in a circadian manner: during the night glia tightly surround VIP dendrites and are retracted from VP dendrites, while in the day-time they move to cover VP dendrites more closely and retract from VIP dendrites. These rhythms in dendritic spine ensheathment may be important for gating photic signals (Becquet et al., 2008, Girardet et al., 2010b). Along these lines, it has been shown that changes in lighting conditions alters the ultrastructure of synapses formed by retinal ganglion cells in the SCN, primarily onto VIP neurons in the retinorecipient region (Guldner et al., 1997). VIP neurons have a greater number of synapses during the day than at night, and this includes both glutamatergic and non-glutamatergic synapses. For a more detailed review of the data supporting structural rearrangements of SCN synapses see (Girardet et al., 2010a). Going forward, it will be important to determine to what extent these changes are driven by the circadian clock and/or external signals. Additional research is also needed to determine how these astrocytic morphological changes affect the signaling properties of the neurons.
Differences in astrocytic morphology are also seen between sleep and wake states. Sleep deprivation induces morphological changes in cortical astrocytes, most notably an extension of their filipodial appositions into the synaptic space (Bellesi et al., 2015, Areal et al., 2017). As with the circadian system, the effects of changing astrocytic morphology on sleep may include changes in neuronal ensheathment. Mice exposed to acute or chronic sleep deprivation display increases in perisynaptic astrocytic processes that surround spine heads, axons, and dendrites (Bellesi et al., 2015). These processes exhibit signs of enhanced astrocytic phagocytosis, and the astrocytes contain more endosomes, a canonical indication that cells are participating in cellular or metabolic recycling (Bellesi et al., 2017). Functionally, these astrocytic dynamics may contribute to the reduction or “scaling down” of synaptic size and connections during sleep that has been seen by other research groups (de Vivo et al., 2017, Diering et al., 2017). Thus, similar to the circadian system, astrocytic morphological changes are seen with changes in sleep-wake state, but the functional role(s) of these changes remain obscure.
Although the precise mechanisms through which these rearrangements are propagated and what role they play remains unclear, these daily iterative structural changes are reminiscent of ECM-associated events seen during development, which suggests that these processes could involve ECM remodeling. Changes in cell-attached proteins also likely participate in regulating these changes. For example, astrocyte morphology changes in the hippocampus have been shown to involve connexin proteins (Pannasch et al., 2014) and a protease-activated receptor (Sweeney et al., 2017), while in the hypothalamic neuroendocrine system they involve local neuromodulators and changes in the cell adhesion protein SynCAM (reviewed in Clasadonte and Prevot, 2017). Many questions remain regarding how changes in astrocyte morphology modulate the circadian and sleep-wake systems, including: What cellular and molecular processes drive these changes, and what are the mechanisms through which changes in astrocyte morphology influence circadian and sleep functions? For example, changes in astrocyte morphology could affect synaptic signaling through altering the buffering capacity and/or tortuosity of the ECS. In some brain regions, astrocytes can control the concentration of extracellular glutamate through a variety of mechanisms (Malarkey and Parpura, 2008).
Astrocytic regulation of the ECS has not been investigated in the circadian system, but it has become a focus in the sleep-wake system. In the cortex, the transition from wakefulness to sleep is correlated with an increase in ECS volume that appears to alter the diffusion properties of molecules in the ECS (Xie et al., 2013). Sleeping mice or mice that are anesthetized exhibit a 60% increase in interstitial space in the cortex, which is associated with a higher clearance rate of molecules and metabolites from the brain, possibly due to a higher exchange rate of cerebrospinal fluid. In support of this idea, the clearance of radio-labeled amyloid-β is faster in sleeping vs. awake mice (Xie et al., 2013). Similarly, sleep deprivation increases morning amyloid-β levels in blood plasma of humans, and this increase is correlated with a decrease in expression of soluble LRP-1 (Wei et al., 2017). Because LRP-1 mediates the internalization of amyloid-β, this finding suggests that LRP-1 dependent regulation of extracellular molecules may be closely tied to the processes regulating sleep (Kanekiyo and Bu, 2009). Given the evidence of an interaction between amyloid-β accumulation and sleep disruptions (reviewed in Ju et al., 2014), it is possible that one critical function of sleep is to increase ECS and allow enhanced clearance of toxic metabolites.
Other research found that application of the β-adrenergic agonist isoproterenol to cortical brain slices decreases ECS volume and increases the volume of distal astrocytic processes (Sherpa et al., 2016). Functionally, the authors concluded that β-adrenergic activation during wakefulness increases astrocyte extensions into the synaptic space, decreasing ECS and increasing the concentration of extracellular substances. A recent review (Puentes-Mestril and Aton, 2017) highlights evidence that changes in astrocytic structure during sleep can alter neuronal communication through changing the ECS, possibly involving a glial-lymphatic, or ‘glymphatic’, system and its ability to change the ionic and/or small molecule synaptic composition. It is important to note, however, that the theory of a ‘glymphatic’ system for clearing toxic metabolites is not universally accepted (e.g., Smith and Verkman, 2018). Moreover, a recent study (Gakuba et al., 2018) found that anesthesia decreases the rate of CSF clearance in mice relative to that seen during wakefulness. Importantly, this study did not investigate CSF clearance rates during sleep, which is a critical next step.
Taken together, these studies support astrocytic regulation of ECS clearance being an important aspect of sleep processes. It will be interesting for future research to determine whether astrocytic modulation of the ECS functionally regulates sleep-wake state transitions or whether it is a result of those transitions. It will also be important to investigate the role of other mechanisms in regulating ECS clearance. For example, (Godin et al., 2017) recently showed that enzymatic degradation of the ECM can dramatically alter the shape and diffusion dynamics of the ECS.
3.5.2. Gliotransmission
Another mechanism through which glia can influence neuronal plasticity is by releasing signaling molecules (e.g., Gundersen et al., 2015; Guerra-Gomes et al., 2018; Rose et al., 2018), and these gliotransmitters appear to affect both circadian and sleep-wake systems. In reviewing the evidence for gliotransmission, it is important to note that gliotransmitter (and neurotransmitter) signaling efficacy can vary dramatically with changes in astrocyte morphology and its interactions with the ECM (Ben Achour and Pascual, 2012), and the interplay between these variables has received little attention in either system.
Recent evidence that astrocyte-derived signals are important for circadian rhythms comes from three studies. One group used astrocyte-specific Bmal1 knockout mice and casein kinase-1ε mutant mice to show that astrocytes regulate the free-running period of clock gene expression rhythms in the SCN and behavioral locomotor activity rhythms (Tso et al., 2017). Similarly, a second group showed that selective ablation of Bmal1 in astrocytes alters behavioral rhythms that can be rescued through pharmacological manipulation of GABA signaling (Barca-Mayo et al., 2017). Addressing the question of how astrocytes communicate with neurons, a third group used live cell imaging to demonstrate that neurons and astrocytes have rhythms in intracellular calcium that are in antiphase to one another, with neurons being metabolically more active during the circadian day and astrocytes more active during the night. Additionally, they demonstrated that glutamate functions as a gliotransmitter in this system: night-active astrocytes release glutamate, which activates presynaptic NR2C subunit-containing NMDARs. This stimulates GABA release, leading to decreased neuronal activity in the SCN at night (Brancaccio et al., 2017). In light of previous work showing that astrocytes in the SCN exhibit periodic (7-20 second) oscillations in intracellular Ca2+ that are inhibited by glutamate (van den Pol et al., 1992), it will be interesting to investigate potential mechanistic connections between astrocytic Ca2+ rhythms and glutamate release in the SCN. The research by Brancaccio et al., (2017) highlighting the importance of gliotransmission in the SCN is consistent with evidence that a variety of astrocytic signals, including nitric oxide (NO), ATP, adenosine, and the cytokines TNFα and IL1, influence both circadian and sleep-wake systems. Although many of these molecules have intracellular functions, we wish to focus here on their potential extracellular actions.
3.5.2.1. Nitric oxide
NO has been implicated as an extracellular modulator of photic transduction in the SCN (Ding et al., 1994, Golombek et al., 2004, Plano et al., 2010). Nitric oxide synthase (NOS) is found in SCN astrocytes (Caillol et al., 2000), supporting astrocytes as one source of NO in the SCN. Notably, treating SCN brain slices with hemoglobin, an extracellular NO scavenger, disrupts some but not all actions of NO in the SCN (Artinian et al., 2001), suggesting that NO participates in both intracellular and transcellular signaling in the SCN.
Signaling by NO also modulates the sleep-wake system. Generally, during wakefulness and early stages of sleep deprivation, the activity of NOS increases, resulting in NO production and sleep promotion (Wisor et al., 2011b). Importantly, NO affects both REMS and SWS processes (summarized in Brown et al., 2012) and the effects vary by cell type. The cell type differences could be due in part to production of NO by distinct isoforms of NOS, neuronal NOS (nNOS) vs. inducible NOS (iNOS), the latter of which being predominantly expressed by microglia and astrocytes (Murphy et al., 1993, Wong et al., 1996).
In their genetic screen, Mackiewicz et al., (2007) identified Nos3 as one of the genes that increases in the cerebral cortex during sleep. Consistent with this finding, another study found that cortical interneurons co-expressing nNOS and the substance P receptor NK1 exhibit increased c-Fos expression during sleep (Morairty et al., 2013). Also, nNOS knockout mice display a decrease in slow wave activity during sleep, indicating a decrease in sleep homeostatic drive, but they also have a shorter latency to sleep, which implies that sleep homeostatic drive increases (Morairty et al., 2013). A commentary on this report suggested that nNOS regulates sleep through two distinct pathways; one in response to arousal and the other associated with sleep homeostasis (Greene, 2013). Exploring this relationship further, the same group found that the amount of time spent in SWS does not alter the minimal amount of c-Fos activity in one population of nNOS/NK1 neurons, while another population of nNOS/NK1 neurons exhibits increased c-Fos expression after sleep deprivation (Dittrich et al., 2015). Together, these findings reinforce the idea that the role of NO in sleep regulation is cell-type dependent, and that there are at least two distinct roles of nNOS neurons in sleep. Although these studies focused on neuronal actions of NO, the NO can diffuse to and communicate with nearby astrocytes to regulate sleep processes in a manner that would be affected by changes in the ECS (Krueger et al., 2013). Moreover, as mentioned above, NO synthesized by glial cells may also modulate sleep. In support of this, injecting a specific inhibitor of nNOS into the basal forebrain decreases REMS recovery in sleep-deprived mice, while injecting a specific inhibitor of iNOS prevents SWS recovery (Kalinchuk et al., 2006).
3.5.2.2. Purines
ATP and adenosine are other potential gliotransmitters modulating the circadian and sleep-wake systems. Although ATP released into the extracellular space can be rapidly degraded to adenosine, it is a signaling molecule in its own right, particularly with respect to signaling between astrocytes and neurons (Scemes and Giaume, 2006, Wang et al., 2000). ATP activates purinergic receptors, generally enhancing cellular (neuronal and astrocytic) activity. Conversely, adenosine (either released from cells or after extracellular degradation from ATP) activates distinct adenosine receptors that can either increase or decrease neuronal activity (Parpura et al., 2017, Stockwell et al., 2017, Holst and Landolt, 2015). Astrocytes and neurons both release ATP and adenosine (Pascual et al., 2005, Fellin et al., 2017, Holst and Landolt, 2015), although astrocytes may be the primary source for released adenosine (Blutstein and Haydon, 2013).
Genes involved in ATP regulation exhibit circadian oscillations in the SCN (Menger et al., 2005). Circadian oscillations in ATP production and extracellular accumulation have been observed in vitro in SCN2.2 cell cultures (which may be comprised largely of astrocytes), and daily variations in extracellular ATP occur in rat SCN in vivo. Interestingly, these oscillations are also seen in cortical astrocyte cultures, indicating that ATP extracellular accumulation may be a pervasive physiological output of circadian oscillating cells (Womac et al., 2009). Other research has demonstrated that adenosine, acting on A1 receptors, can phase shift the SCN circadian clock (Antle et al., 2001) and inhibit photic phase shifts of the SCN clock (Watanabe et al., 1996, Elliott et al., 2001, Sigworth and Rea, 2003). The inhibition of photic phase shifts may involve blocking presynaptic glutamate release (Watanabe et al., 1996, Hallworth et al., 2002). Not clear from these studies, however, is the source of the adenosine and the mechanisms regulating adenosine (or ATP) release.
With respect to the sleep-wake system, ATP and adenosine are well-known sleep regulatory substances (Clinton et al., 2011, Benington and Heller, 1995b, Holst and Landolt, 2015). ATP release from cells is thought to involve pannexin-1 channels (Lohman and Isakson, 2014). Knockout mice that lack this channel display an inverted waking/SWS ratio and are more active in both light and dark periods (Kovalzon et al., 2017). The extracellular actions of ATP also include affecting sleep homeostasis and recovery from sleep deprivation. First, stimulation of purine type 2 (P2) receptors by an ATP agonist can increase SWS in mice. Additionally, P2X7 receptor expression varies with sleep state, and sleep deprived mice lacking P2X7 receptors exhibit decreased recovery sleep responses (Krueger et al., 2010). These data support direct actions of extracellular ATP on sleep-wake processes in addition to those described below that are exerted by it metabolic product, adenosine.
Knockout mice lacking the 5'-ectonucleotidase enzyme CD73 required to convert AMP to adenosine exhibit increased SWS after sleep deprivation as compared to control mice (Zielinski et al., 2012). Adenosine enhances sleep in part through activating A2a receptors that inhibit the activity of wake-promoting neurons (Huang et al., 2014, Krueger et al., 2013, Petit et al., 2015). Astrocyte-derived adenosine can also modulate sleep through activating A1 receptors (Halassa et al., 2009). This group found that blocking gliotransmission reduces slow-wave activity and results in a decrease in sleep pressure. Moreover, they found that the sleep suppressing effects of an A1 receptor antagonist are prevented by blocking gliotransmission (Halassa et al., 2009). Research also supports adenosine released by astrocytes as being important for sleep-wake regulation (Blutstein and Haydon, 2013). The effects of adenosine are complex, however, since increases in glucose, which would be considered a signal of increased rather than depleted energy stores, can stimulate astrocytic release of adenosine in the VLPO of mice (Scharbarg et al., 2017). Interestingly, this study also showed that the glucose-induced increase in adenosine release was significantly greater in tissue collected at the beginning of the sleep period than the beginning of the activity period. It will be important in future studies to determine whether the circadian clock regulates this difference or if it is solely a result of differential sleep pressure.
Together, these data indicate that sleep homeostasis depends on both ATP and adenosine, with glial cells being a prominent source of both signaling molecules. The data also support adenosine and ATP playing important regulatory roles in the circadian system. Finally, there is tantalizing evidence for interactions between the two systems that involve extracellular purine signaling. Moving forward, it will be important to clarify the source(s) of both ATP and adenosine in both systems, what stimulates their release, and how changes in the extracellular environment (e.g, the availability of enzymes to convert ATP to adenosine; proximity of astrocytes to the synaptic active zone; ECS tortuosity) modulate their signaling capabilities.
3.5.2.3. Cytokines
Other potential gliotransmitters acting within the circadian and sleep-wake systems include cytokines such as TNFα, IL1β, and IL6. Cytokines are active in the periphery of the body, in blood plasma and in CSF, and cytokines produced in the periphery can cross the blood brain barrier and stimulate brain cells to release more cytokines and initiate additional immune responses (see Capuron and Miller et al., 2011 for review). Within the brain, cytokines can be released by neurons, astrocytes and microglia (Xu et al., 2016, Lau and Yu, 2004). Cytokine release into the extracellular space not only initiates or exacerbates immune responses by recruiting monocytes to the brain (D'Mello et al., 2009), but it also modulates synaptic plasticity associated with hippocampal learning and memory and drug addiction through multiple mechanisms (Maurer and Williams, 2017, Lacagnina et al., 2017). Cytokines can regulate membrane-localized molecules as well. For example, astrocyte-derived TNFα modulates hippocampal synaptic strength in part through increasing AMPAR surface expression (Stellwagen and Malenka, 2006). Another study found that TNFα is released from astrocytes in the hippocampus in an activity dependent manner and it regulates β3-integrin and N-cadherin expression in neurons (Cingolani and Goda, 2008). Similarly, a TNFα receptor has been shown to modulate N-cadherin expression in hippocampal neurons (Kubota et al., 2009).
A bidirectional link between the immune system and circadian rhythms is well established in regards to both peripheral clocks and the central clock. For example, there are circadian rhythms in basal plasma TNFα, IL1β, IL6 and the IL6 receptor (IL6R) in humans, although the source of these proteins is not known (Bauer et al., 1994, Born et al., 1997, Vgontzas et al., 1997, Vgontzas et al., 2005). There are also circadian rhythms in immune responses (Coogan and Wyse, 2008, Logan and Sarkar, 2012, Scheiermann et al., 2013). In the reverse direction, peripheral injection of lipopolysaccharide (LPS; an endotoxin serving as an immune challenge) induces phase shifts of locomotor activity rhythms in mice (Paladino et al., 2014) that involve TNFα-dependent mechanisms within the SCN. TNFα and IL1β can decrease expression of Per and Cry genes in fibroblast and neuronal cell cultures and in the liver by inhibiting BMAL-CLOCK transcriptional activity, and they decrease the behavioral activity of mice when administered during their active phase (Cavadini et al., 2007, Gast et al., 2012). These effects may involve the transcriptional regulator Twist1 (Meier et al., 2015). On the other hand, a separate study found that cell culture media collected after TNFα treatment, but not after IL1β treatment, increases Per1 expression in fibroblasts (Duhart et al., 2013). While the evidence for circadian-immune system interactions is extensive (see Coogan and Wyse, 2008; Scheiermann et al., 2013; Cermakian et al., 2013 for reviews), here we will focus primarily on the potential role of cytokines functioning as gliotransmitters to modulate the circadian clock.
Microglia isolated from hippocampus exhibit day/night rhythms in TNFα and IL1β mRNA and immune reactivity, with higher levels in the day than the night (Fonken et al., 2015), but whether these cytokines are acting as intercellular signaling molecules is not clear. Similarly, mRNA transcripts of both TNFα and IL1β in the hypothalamus exhibit diurnal expression that is highest during the light phase (Bredow et al., 1997, Taishi et al., 1997, Cearley et al., 2013). Moreover, administration of TNFα reduces expression of Dbp mRNA, a circadian regulated transcription factor, in SCN tissue (Cavadini et al., 2007). Finally, another study found that TNFα application shifts PER2 expression rhythms in SCN astrocyte cultures, and these cultures increase secretion of inflammatory markers CCL2 and IL6 in response to TNFα application (Paladino et al., 2014). Moreover, TNFα receptor mRNA levels are rhythmic in the SCN, with higher levels at night, and TNFα receptor knockout mice exhibit significantly longer free-running periods compared to wildtype mice (Paladino et al., 2014). While suggestive, more research on cytokine signaling in the SCN is needed. Also, investigating interactions of these cytokines with cellular adhesion molecules or extracellular proteases specifically in the SCN will be important in elucidating the extent to which cytokines participate in the extracellular regulatory mechanisms of the circadian clock.
Cytokines have been studied far more extensively in the context of sleep regulation, and there are excellent reviews of the accumulated data (Imeri and Opp, 2009, Jewett and Krueger, 2012, Clinton et al., 2011, Zielinski and Krueger, 2011, Krueger et al., 2011, Irwin and Opp, 2017). Substantial research has focused on the intersection between the sleep and immune systems in terms of how inflammatory responses can enhance sleep and how sleep disruption can exacerbate immune responses (Dantzer et al., 2008, Olofsson et al., 2012, Irwin and Opp, 2017, Xu et al., 2016). In addition to modulating each other, these interactions can significantly affect neuronal processes. For example, increases in circulating cytokines due to surgery or sickness can elicit the negative symptoms that occur in response to sleep loss or circadian dysregulation, including fatigue and impaired cognition and memory, and these effects are mimicked by administering exogenous cytokines (Clinton et al., 2011, Zielinski and Krueger, 2011). Similarly, memory impairments caused by sleep fragmentation or surgery are accompanied by increases in TNFα mRNA expression, and the mRNA changes but not the memory deficits are exacerbated when surgery is either preceded or followed by sleep fragmentation (Vacas et al., 2017). However, for the purposes of this review, we will focus more directly on evidence that cytokines such as TNFα and IL1β and IL6 function as signaling molecules in the brain that regulate sleep homeostasis under physiological conditions.
As reviewed extensively, (Krueger, 2008, Krueger et al., 2011, Imeri and Opp, 2009, Irwin and Opp, 2017) TNFα and IL1β protein and mRNA generally increase during wakefulness and decrease during sleep. Inhibiting their activity or expression decreases both SWS and REMS, while administering these proteins can induce long-lasting sleep (primarily SWS), even at doses that don’t elicit fever. They do not affect all sleep stages uniformly. Thus, low doses of both cytokines selectively increase SWS, at moderate levels they increase SWS and decrease REMS, and at even higher levels they inhibit both SWS and REMS (Krueger et al., 2011, Del Gallo and Opp, 2014). It is also noteworthy that TNFα and IL1β appear to affect sleep slightly differently across the circadian cycle. Mice lacking IL1β receptors have less SWS and REMS during their active period with no changes during their sleep period, while mice lacking TNFα receptors have decreases in SWS and REMS primarily during the end of their active period and throughout their sleep period (Fang et al., 1997, Fang et al., 1998).
One important question when exploring the central actions of cytokines on sleep is whether the cytokines are derived from the periphery or the brain. As reviewed elsewhere (Dantzer et al., 2008, Olofsson et al., 2012), peripherally derived inflammatory processes can signal the brain through a variety of pathways, including neural stimulation as well as through cytokines entering the brain. Nevertheless, we know that neurons and glial cells in cortical, brainstem and hypothalamic sleep regulatory regions express IL1β, TNFα and/or their receptors (see Irwin and Opp, 2017), and that these cytokines modulate neuronal activity in all these regions. Moreover, the effects of cytokines on sleep are cell-type specific. For example, when IL1β receptors are expressed solely in either astrocytes or neurons mice have more spontaneous REMS, their SWS exhibits enhanced delta power, and they have more consolidated sleep after short-term sleep deprivation. However, when IL1β receptors are only expressed in neurons, SWS after sleep deprivation has reduced delta power, supporting the need for astrocytic ILβ signaling in normal sleep homeostasis (Ingiosi et al., 2015). Intriguingly, this same study found that restricting IL1β receptor expression to either neurons or astrocytes prevents induction of IL1β and IL6 in the hypothalamus after IL1β administration and it prevents ILβ-induced increases in sleep and body temperature. Moreover, the REMS suppression induced by peripheral LPS injections is reduced in mice expressing IL1β receptors in neurons vs. those expressing IL1β receptors in astrocytes (Ingiosi and Opp, 2016). Together, these data suggest that IL1β receptor expression in both neurons and astrocytes is needed for normal cytokine actions on sleep, and that additional cells in the brain, such as endothelial or microglial cells, are important for IL1β’s sleep-inducing actions, especially regarding its actions within the hypothalamus.
Several studies have specifically investigated astrocyte and microglia involvement in cytokine regulation of sleep. Both astrocytes and microglia become activated after sleep loss and can release cytokines in multiple brain regions (Sofroniew, 2014, Greene et al., 2017, Wadhwa et al., 2017, Bellesi et al., 2015, Bellesi et al., 2017). In the hippocampus, 5 days of sleep deprivation increases the expression of GFAP and compliment type 3 receptors, which are indicators of activated astrocytes and microglia, respectively (Hsu et al., 2003). Focusing specifically on microglial involvement, inhibiting microglia with minocycline can prevent rebound SWS and REMS in mice after sleep deprivation (Wisor and Clegern, 2011), and minocycline administration to mice experiencing 48 hours of sleep deprivation decreases the cognitive impairments associated with sleep loss (Wadhwa et al., 2017). Another study found that mice with a constitutive deletion of toll-like receptor-4 which facilitates production of pro-inflammatory cytokines and is highly expressed in microglia and astrocytes (Hanke and Kielian, 2011), exhibit lower levels of REMS across the entire day and have higher levels of sleep specifically during the beginning of the wake period. They also exhibit less rebound sleep after mild sleep deprivation, suggesting an overall lower sleep drive (Wisor et al., 2011a). On the other hand, a variety of studies have shown that astrocytes can release both IL1β and TNFα in response to extracellular ATP (Krueger et al., 2011, Jewett and Krueger, 2012). Moreover, acute sleep loss of 8 hours induces astrocytic phagocytosis of neuronal synapses in the frontal cortex of mice, while activation of microglia in the same brain region only occurs after chronic sleep loss of over 4.5 days (Bellesi et al., 2017). These results suggest that structural changes occur during sleep loss, as indicated by astrocytic phagocytosis of synapses, and that they may be a result of cytokine activation.
Focusing on local cell networking, mixed astrocyte/neuron cortical cell cultures exhibit bursting activity, membrane oscillations, and slow-wave power changes consistent with changes in sleep state (Jewett et al., 2015). Electrical stimulation decreases these neuronal activity parameters, with rebounds in their expression 24 h later. Adding TNFα to the cultures induces the opposite effects, and these TNFα-induced changes are reversed by electrical stimulation. A more recent study (Poskanzer and Yuste, 2016) investigated astrocyte involvement in vivo. Using a combination of optogenetics and calcium imaging, they found that both spontaneous and induced increases in cortical astrocytic intracellular Ca2+ are immediately followed by rapid spikes in extracellular glutamate and a switch from fast (desynchronized) to slow (synchronized) oscillations in local field potentials, consistent with the onset of a SWS-type state. Together, the data from these studies are consistent with the idea that sleep states are an emergent property of local cell networks that rely on tightly regulated interactions between neurons and glial cells that include cytokine signaling.
Although most research on cytokine modulation of sleep homeostasis has focused on TNFα and IL1β, IL6 also participates in this process (Dantzer et al., 2008, Irwin and Opp, 2017). However, IL6 signaling is complex. As reviewed recently (Rothaug et al., 2016), “classical signaling” involves IL6 binding its membrane bound receptor (IL6R), which then binds to and stimulates dimerization of gp130 receptors, leading to activation of intracellular signaling processes. This form of signaling is somewhat restricted in the brain because IL6Rs are only expressed by microglia. However, the extracellular proteases ADAM10 and 17 can cleave IL6Rs to generate a soluble form (sIL6R). IL6 binding to sIL6R can then activate gp130 receptors on neighboring cells via “trans-signaling”. Because multiple cell types throughout the brain express gp130 receptors, this suggests that trans-signaling by IL6 is more widespread than classic signaling in the brain. Notably, this ‘trans’ signaling is similar to the ‘shedding’ of the extracellular subunit of LRP-1 discussed earlier, which expands its potential locus of interaction.
In this context, it is also important to note that ADAM17 was originally identified as the enzyme that cleaves and activates TNFα, and thus is also called TNFα converting enzyme (TACE) (Saftig and Reiss, 2011, Yang et al., 2011). In fact, there is a large literature showing that ADAM10 and 17 as well as several other MMPs have reciprocal regulatory roles within the peripheral and central immune systems (Saftig and Reiss, 2011, Yang et al., 2011). Although a thorough discussion of these interactions is outside the scope of this review, the data warrant more attention being given to their potential intersections with sleep homeostatic regulation.
The mechanisms through which cytokines modulate neuronal activity and vice versa, how neuronal activity modulates cytokine activity, likely involves multiple signaling processes. Cytokines can modulate the signaling of many neurotransmitters, including serotonin, glutamate, acetylcholine and GABA. However, these interactions are outside the scope of this review, and interested readers are directed towards other excellent reviews (Dantzer et al., 2008, Imeri and Opp, 2009, Irwin and Opp, 2017). More relevant to this review, neuronal activity likely alters cytokine expression and activity within the context of sleep homeostasis through mechanisms that involve a complex interaction between cytokines, purines, and NO. One model that has been put forward is based in part on extensive data (some reviewed in the previous sections) showing that increases in extracellular NO, ATP and adenosine accompany wakefulness/increased neuronal activity (Krueger, 2008, Krueger et al., 2011). ATP stimulation of P2X7 receptors can increase TNFα and IL1β activity and release. TNFα and IL1β in turn can stimulate NFkB to translocate into the nucleus where it can increase adenosine receptor expression. Additionally, NFkB can indirectly increase release of NO, prostaglandin and adenosine. Increases in all of these molecules contribute to inhibiting local neuronal activity. These interactions would alter neuronal activity at the level of local circuits, which could be modulated more globally by sleep regulatory centers.
In summary, the evidence indicates that cytokines are important players in maintaining sleep homeostasis, and they may serve as reporters of sleep disturbances. Moreover, it is likely that they act in coordination with NO and purines, all of which could be produced by glial cells. Although the importance of cytokines in sleep homeostasis is clear, more research is needed to parse out the precise role of astrocyte-, microglia-, and neuron-derived cytokines in the sleep-wake system, and what other cells might be involved. For example, the data on mice with selective expression of IL1 receptors in either astrocytes or neurons (Ingiosi et al., 2015) suggest that the actions of IL1 involve additional cells within the brain. We also do not know the extent to which other extracellular molecules modulate the actions of cytokines with respect to sleep homeostasis. The complex signaling by IL6 and its regulation by the extracellular proteases ADAM10/17 is just one example of this type of interaction. Finally, it will be important to clarify the intersecting mechanisms through which the circadian and sleep-wake systems regulate cytokines in the brain.
Taken together, it is evident that astrocytes are key regulators of both the circadian and sleep-wake systems (Fig. 3, Table 1). Their mechanisms of action likely involve a complex interplay between altering the physical structure of the ECS, releasing signaling molecules and modulating the composition of the ECM. However, much of this remains speculative as few circadian or sleep studies have directly assessed interactions between astrocytes and the ECM and their functional implications. A better understanding of these interactive processes within each system is a critical area of exploration.
Fig. 3.
Astrocyte-associated molecules and mechanisms implicated in SCN circadian system (A) and sleep-wake system (B) modulation. For the sleep-wake system, note that the figure collates data from a variety of brain regions. The strength of the data in both systems varies, from simple mRNA or protein expression through extensive functional evidence. The figure does not attempt to represent all of the astrocyte-linked mechanisms known or theorized to participate in each system, but rather aims to illustrate the potential commonalities and differences between the systems.
4. Conclusions and questions
Secreted molecules interacting in the extracellular space influence neuronal processing in various regions of the nervous system. Despite the crucial role that the ECM and interacting molecules play in a variety of brain functions, they remain largely understudied and poorly understood in most systems, with circadian and sleep-wake regulation being no exception. The evidence presented here demonstrates that these extracellular molecules can dramatically influence the functioning of both systems. Although the precise mechanisms have not been elucidated, one unifying concept to consider is that the sleep-wake and circadian systems integrate processes on a relatively slow timescale (hours vs. seconds or minutes) that doesn’t directly equate to the rapid synaptic signaling mechanisms of neurotransmitters. In contrast, the interactions occurring within the extracellular space, including structural changes, proteolytic processes, and ECM remodeling, generate changes in cell signaling that can integrate over longer time spans. Thus, their importance within the circadian and sleep-wake systems may lie in their ability to sense the rapid synaptic signaling events and transform them into broader changes in cell/network activity consistent with the daily changes orchestrated by both systems.
Table 1 summarizes many of the components of the extracellular environment that have been linked to the circadian and sleep-wake systems. However, our understanding of how these molecules work within these two systems still is largely superficial. Moreover, most extracellular molecules have not yet been studied, or have been studied primarily in one system or the other. Some of important questions that remain unanswered include: How do these proteins interact to influence each system? How pervasively does the ECM influence cell signaling in these systems? How do the expressions and actions of these molecules change over the course of a lifetime or in response to diseases or other disruptions? Although there is evidence that some of these extracellular processes are shared by other brain systems (e.g., the limbic and neuroendocrine systems), it is likely that each region utilizes a unique subset of these processes, and it will be important to clarify their different combinations and the functional consequences of these combinations associated with the circadian and sleep-wake systems. Additionally, in many cases it is not clear whether these extracellular processes are regulators or consequences of state changes generated by the two systems. Another major question is the extent to which microglia participate in these two systems. A role for microglia linking the immune and sleep systems is strong, but information on microglia in the SCN circadian system is scant. An additional complication stems from the heterogeneous nature of all the brain areas involved in these two systems. It will be imperative moving forward to better characterize the extracellular interactome of different cell types in each area. Along these lines, a recent paper used single-cell RNAseq to phenotype the transcriptome of 6 different populations of cortical GABAergic neurons (Paul et al., 2017). Intriguingly, differential expression of CAMS was one of the 6 categories of genes that distinguished these groups of neurons.
Lastly, when comparing the research from each of these two fields, it seems apparent that each can learn from the other. For example, the data on changes in ECS being critical for sleep-wake processes suggests that similar effects might be occurring in the SCN. Cytokine signaling has also been studied far more extensively in the sleep-wake system than the circadian system. Conversely, the involvement of extracellular proteases and their downstream targets in regulating circadian phase resetting suggests that more attention to these proteins in the sleep-wake system is warranted. While we do not propose that the ECM, extracellular proteins and glial processes will provide all the answers needed to completely understand the circadian and sleep-wake systems, we are confident that neither system will be fully understood without fully exploring these dynamic extracellular processes.
Competing Interests
The authors have none to declare.
Funding sources
None.
References
- Abrahao K.P., Salinas A.G., Lovinger D.M. Alcohol and the brain: neuronal molecular targets, synapses, and circuits. Neuron. 2017;96:1223. doi: 10.1016/j.neuron.2017.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Horani R.A. Serpin regulation of fibrinolytic system: implications for therapeutic applications in cardiovascular diseases. Cardiovasc. Hematol. Med. Chem. 2014;12:91–125. doi: 10.2174/1871525712666141106095927. [DOI] [PubMed] [Google Scholar]
- Antle M.C., Foley N.C., Foley D.K., Silver R. Gates and oscillators II: zeitgebers and the network model of the brain clock. J. Biol. Rhythm. 2007;22:14–25. doi: 10.1177/0748730406296319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antle M.C., Smith V.M., Sterniczuk R., Yamakwa G.R., Rakai B.D. Physiological responses of the circadian clock to acute light exposure at night. Rev. Endo Met. Disord. 2009;10:279–291. doi: 10.1007/s11154-009-9116-6. [DOI] [PubMed] [Google Scholar]
- Antle M.C., Steen N.M., Mistlberger R.E. Adenosine and caffeine modulate circadian rhythms in the Syrian hamster. NeuroReport. 2001;12:2901–2905. doi: 10.1097/00001756-200109170-00029. [DOI] [PubMed] [Google Scholar]
- Archinti M., Britto M., Eden G., Furlan F., Murphy R., Degryse B. The urokinase receptor in the central nervous system. CNS Neurol. Disord. Drug Targets. 2011;10:271–294. doi: 10.2174/187152711794480393. [DOI] [PubMed] [Google Scholar]
- Areal C.C., Warby S.C., Mongrain V. Sleep loss and structural plasticity. Curr. Opin. Neurobiol. 2017;44:1–7. doi: 10.1016/j.conb.2020.07.004. [DOI] [PubMed] [Google Scholar]
- Artinian L.R., Ding J.M., Gillette M.U. Carbon monoxide and nitric oxide: interacting messengers in muscarinic signaling to the brain's circadian clock. Exp. Neurol. 2001;171:293–300. doi: 10.1006/exnr.2001.7781. [DOI] [PubMed] [Google Scholar]
- Barca-Mayo O., Pons-Espinal M., Follert P., Armirotti A., Berdondini L., De Pietri Tonelli D. Astrocyte deletion of Bmal1 alters daily locomotor activity and cognitive functions via GABA signalling. Nat. Commun. 2017;8:14336–14566. doi: 10.1038/ncomms14336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes A.K., Koul-Tiwari R., Garner J.M., Datta S. Activation of brain-derived neurotrophic factor-tropomyosin receptor kinase B signaling in the pedunculopontine tegmental nucleus: a novel mechanism for the homeostatic regulation of rapid eye movement sleep. J. Neurochem. 2017;141:111–123. doi: 10.1111/jnc.13938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrow S.L., Constable J.R., Clark E., El-Sabeawy F., McAllister A.K., Washbourne P. Neuroligin1: a cell adhesion molecule that recruits PSD-95 and NMDA receptors by distinct mechanisms during synaptogenesis. Neural Dev. 2009;4:17. doi: 10.1186/1749-8104-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer J., Hohagen F., Ebert T., Timmer J., Ganter U., Krieger S., Lis S., Postler E., Voderholzer U., Berger M. Interleukin-6 serum levels in healthy persons correspond to the sleep-wake cycle. Clin. Investig. 1994;72:315. doi: 10.1007/BF00180048. [DOI] [PubMed] [Google Scholar]
- Becquet D., Girardet C., Guillaumond F., Francois-Bellan A.-M., Bosler O. Ultrastructural plasticity in the rat suprachiasmatic nucleus, possible involvement in clock entrainment. Glia. 2008;56:294–305. doi: 10.1002/glia.20613. [DOI] [PubMed] [Google Scholar]
- Bellesi M., de Vivo L., Chini M., Gilli F., Tononi G., Cirelli C. Sleep loss promotes astrocytic phagocytosis and microglial activation in mouse cerebral cortex. J. Neurosci. 2017;37:5263–5273. doi: 10.1523/JNEUROSCI.3981-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellesi M., de Vivo L., Tononi G., Cirelli C. Effects of sleep and wake on astrocytes: clues from molecular and ultrastructural studies. BMC Biol. 2015;13:66. doi: 10.1186/s12915-015-0176-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Achour S., Pascual O. Astrocyte-neuron communication: functional consequences. Neurochem. Res. 2012;37:2464–2473. doi: 10.1007/s11064-012-0807-0. [DOI] [PubMed] [Google Scholar]
- Benington J.H., Heller H.C. Monoaminergic and cholinergic modulation of REM-sleep timing in rats. Brain Res. 1995;681:141–146. doi: 10.1016/0006-8993(95)00305-a. [DOI] [PubMed] [Google Scholar]
- Benington J.H., Heller H.C. Restoration of brain energy metabolism as the function of sleep. Prog. Neurobiol. 1995;45:347–360. doi: 10.1016/0301-0082(94)00057-o. [DOI] [PubMed] [Google Scholar]
- Black M.A., Deurveilher S., Seki T., Marsh D.R., Rutishauser U., Rafuse V.F., Semba K. Role of polysialylated neural cell adhesion molecule in rapid eye movement sleep regulation in rats. Eur. J. Neurosci. 2009;30:2190–2204. doi: 10.1111/j.1460-9568.2009.07000.x. [DOI] [PubMed] [Google Scholar]
- Blutstein T., Haydon P.G. The importance of astrocyte-derived purines in the modulation of sleep. Glia. 2013;61:129–139. doi: 10.1002/glia.22422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokiniec P., Shahbazian S., McDougall S.J., Berning B.A., Cheng D., Llewellyn-Smith I.J., Burke P.G.R., McMullan S., Muhlenhoff M., Hildebrandt H., Braet F., Connor M., Packer N.H., Goodchild A.K. Polysialic acid regulates sympathetic outflow by facilitating information transfer within the nucleus of the solitary tract. J. Neurosci. 2017;37:6558–6574. doi: 10.1523/JNEUROSCI.0200-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borbely A.A. A two process model of sleep regulation. Hum. Neurobiol. 1982;1:195–204. [PubMed] [Google Scholar]
- Borbely A.A., Daan S., Wirz-Justice A., Deboer T. The two-process model of sleep regulation: a reappraisal. J. Sleep. Res. 2016;25:131–143. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- Born J., Lange T., Hansen K., Molle M., Fehn H.L. Effects of sleep and circadian rhythm on human circulating immune cells. J. Immunol. 1997;158:4454–4464. [PubMed] [Google Scholar]
- Brancaccio M., Patton A.P., Chesham J.E., Maywood E.S., Hastings M.H. Astrocytes control circadian timekeeping in the suprachiasmatic nucleus via glutamatergic signaling. Neuron. 2017;93:1420–1435. doi: 10.1016/j.neuron.2017.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredow S., Guha-Thakurta N., Taishi P., Obal F., Jr, Krueger J.M. Diurnal variations of tumor necrosis factor alpha mRNA and alpha-tubulin mRNA in rat brain. Neuroimmunomodulation. 1997;4:84–90. doi: 10.1159/000097325. [DOI] [PubMed] [Google Scholar]
- Broese M., Riermann D., Hein L., Nissen C. a-Adrenergic receptor function, arousal and sleep: mechanisms and therapeutic implications. Pharmacopsychiatry. 2012;45:209–216. doi: 10.1055/s-0031-1299728. [DOI] [PubMed] [Google Scholar]
- Brown R.E., Basheer R., McKenna J.T., Strecker R.E., McCarley R.W. Control of sleep and wakefulness. Physiol. Rev. 2012;92:1087–1187. doi: 10.1152/physrev.00032.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruses J.L., Rutishauser U. Roles, regulation, and mechanism of polysialic acid function during neural development. Biochimie. 2001;83:635–643. doi: 10.1016/s0300-9084(01)01293-7. [DOI] [PubMed] [Google Scholar]
- Buhr E.D., Takahashi J.S. Molecular components of the mammalian circadian clock. Handb. Exp. Pharmacol. 2013;217:3–27. doi: 10.1007/978-3-642-25950-0_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caillol M., Devinoy E., Lacroix M.-C., Schirar A. Endothelial and neuronal nitric oxide synthases are present in the suprachiasmatic nuclei of Syrian hamsters and rats. Eur. J. Neurosci. 2000;12:649–661. doi: 10.1046/j.1460-9568.2000.00961.x. [DOI] [PubMed] [Google Scholar]
- Cavadini G., Petrzilka S., Kohler P., Jud C., Tobler I., Birchler T., Fontana A. TNF-a suppresses the expression of clock genes by interfering with E-box-mediated transcription. PNAS. 2007;104:12843–12848. doi: 10.1073/pnas.0701466104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caverzasio S., Amato N., Manconi M., Prosperetti C., Kaelin-Lang A., Hutchinson W.D., Galati S. Brain plasticity and sleep: implication for movement disorders. Neurosci. Biobehav Rev. 2018;86:21–35. doi: 10.1016/j.neubiorev.2017.12.009. [DOI] [PubMed] [Google Scholar]
- Cearley C., Churchill L., Krueger J.M. Time of day differences in IL1beta and TNFalpha mRNA levels in specific regions of the rat brain. Neurosci. Lett. 2013;352:61–63. doi: 10.1016/j.neulet.2003.07.019. [DOI] [PubMed] [Google Scholar]
- Cermakian N., Lange T., Golombek D., Sarkar D., Nakao A., Shibata S., Mazzoccoli G. Crosstalk between the circadian clock circuitry and the immune system. Chronobiol. Int. 2013;30:888. doi: 10.3109/07420528.2013.782315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemelli R.M., Willie J.T., Sinton C.M., Elmquist J.K., Scammell T., Lee C., Richardson J.A., Williams S.C., Xiong Y., Kisanuki Y., Fitch T.E., Nakazato M., Hammer R.E., Saper C.B., Yanagisawa M. Narcolepsy in orexin knockout mice: molecular genetics of sleep regulation. Cell. 1999;98:437–451. doi: 10.1016/s0092-8674(00)81973-x. [DOI] [PubMed] [Google Scholar]
- Cheng H.-Y.M., Obrietan K. Dexras1: shaping the responsiveness of the circadian clock. Sem. Cell Dev. Biol. 2006;17:345–351. doi: 10.1016/j.semcdb.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Chevilley A., Lesept F., Lenoir S., Ali C., Parcq J., Vivien D. Impacts of tissue-type plasminogen activator (tPA) on neuronal survival. Front. Cell Neurosci. 2015;9:415. doi: 10.3389/fncel.2015.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung S., Lee E.J., Yun S., Choe H.K., Park S.-B., Son H.J., Kim K.-S., Dluzen D.E., Lee I., Hwang O., Son G.H., Kim K. Impact of circadian nuclear receptor Rev-Erba on midbrain dopamine production and mood regulation. Cell. 2014;157:858–868. doi: 10.1016/j.cell.2014.03.039. [DOI] [PubMed] [Google Scholar]
- Cingolani L.A., Goda Y. Differential involvement of beta3 integrin in pre- and postsynaptic forms of adaptation to chronic activity deprivation. Neuron Glia Biol. 2008;4:179–187. doi: 10.1017/S1740925X0999024X. [DOI] [PubMed] [Google Scholar]
- Cirelli C., Tononi G., 2017. The sleeping brain. Cerebrum 2017:cer-07-17. [PMC free article] [PubMed]
- Clasadonte J., Prevot V. The special relationship: glia-neuron interactions in the neuroendocrine hypothalamus. Nat. Rev. Endocrinol. 2017;14:25–44. doi: 10.1038/nrendo.2017.124. [DOI] [PubMed] [Google Scholar]
- Clinton J.M., Davis C.J., Zielinshi M.R., Jewett K.A., Krueger J.M. Biochemical regulation of sleep and sleep biomarkers. J Clin. Sleep. Med. 2011;7:S38–S42. doi: 10.5664/JCSM.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo F., Meldolesi J. L1-CAM and N-CAM: from adhesion proteins to pharmacological targets. TIPS. 2015;36:769–781. doi: 10.1016/j.tips.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Colwell C.S. Linking neural activity and molecular oscillations in the SCN. Nat. Rev. 2011;12:553–569. doi: 10.1038/nrn3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coogan A.N., Wyse C.A. Neuroimmunology of the circadian clock. Brain Res. 2008;1232:112. doi: 10.1016/j.brainres.2008.07.087. [DOI] [PubMed] [Google Scholar]
- Cooper J., Rastogi A., Krizo J., Mintz E.M., Prosser R.A. Urokinase-type plasminogen activator modulates mammalian circadian clock phase regulation in tissue-type plasminogen activator knockout mice. Eur. J. Neurosci. 2017;45:805–815. doi: 10.1111/ejn.13511. [DOI] [PubMed] [Google Scholar]
- Cooper J., Prosser R., 2014. LRP-1 modulates glutamate-induced phase shifting in the mouse SCN circadian clock. Proceedings of the Biomedicine Science Engineering Conference.
- D'Mello C., Se T., Swain M.G. Cerebral microglia recruitmonocytes into the brain in response to tumor necrosis factor alpha signaling during peripheral organ inflammation. J. Neurosci. 2009;29:2089–2102. doi: 10.1523/JNEUROSCI.3567-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R., O'Connor J.C., Freund G.G., Johnson R.W., Kelley K.W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. 2008;9:46–57. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta S., Knapp C.M., Koul-Tiwari R., Barnes A.K. The homeostatic regulation of REM sleep: a role for localized expression of brain-derived neurotrophic factor in the brainstem. Beh. Brain Res. 2015;292:381–392. doi: 10.1016/j.bbr.2015.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumas-Meyer V., Champeil-Potokar G., Chaumontet C., Dahirel P., Papillon C., Congar P., Denis I. Fasting induces astroglial plasticity in the olfactory bulb glomeruli of rats. Glia. 2017;7:1–15. doi: 10.1002/glia.23280. [DOI] [PubMed] [Google Scholar]
- de Vivo L., Bellesi M., Marshall W., Bushong E.A., Ellisman M.H., Tononi G., Cirelli C. Ultrastructural evidence for synaptic scaling across the wake/sleep cycle. Science. 2017;355:507–510. doi: 10.1126/science.aah5982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Declerck P.J., Gils A. Three decades of research on plasminogen activator inhibitor-1: a multifacted serpin. Semin. Thromb. Hemost. 2013;39:356–364. doi: 10.1055/s-0033-1334487. [DOI] [PubMed] [Google Scholar]
- DeCoursey P.J., Buggy J. Restoration of locomotor rhythmicity in SCN-lesioned golden hamsters by transplantation of fetal SCN. Neurosci. Abstr. 1986:212. [Google Scholar]
- Del Gallo F., Opp M.R. The reciprocal link between sleep and immune responses. Arch. Ital. Biol. 2014;152:93–102. doi: 10.12871/000298292014234. [DOI] [PubMed] [Google Scholar]
- Deurveilher S., Burns J., Semba K. Indirect projections from the suprachiasmatic nucleus to the ventrolateral preoptic nucleus: a dual tract-tacing study in rat. Eur. J. Neurosci. 2002;16:1195–1213. doi: 10.1046/j.1460-9568.2002.02196.x. [DOI] [PubMed] [Google Scholar]
- Diering G.H., Nirujogi R.S., Roth R.H., Worley P.F., Pandey A., Huganir R.L. Homer1a drives homeostatic scaling-down of excitatory synapses during sleep. Science. 2017;355:511–515. doi: 10.1126/science.aai8355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dines M., Lamprecht R. The role of Ephs and ephrins in memory formation. Int. J. Neuropsychopharm. 2016;19:1–14. doi: 10.1093/ijnp/pyv106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding J.M., Chen D., Weber E.T., Faiman L.E., Rea M.A., Gillette M.U. Resetting the biological clock: mediation of nocturnal circadian shifts by glutamate and NO. Science. 1994;266:1713–1717. doi: 10.1126/science.7527589. [DOI] [PubMed] [Google Scholar]
- Ding J.M., Faiman L.E., Hurst W.J., Kuriashkina L.R., Gillette M.U. Resetting the biological clock: mediation of nocturnal CREB phosphorylation via light, glutamate, and nitric oxide. J. Neurosci. 1997;17:667–675. doi: 10.1523/JNEUROSCI.17-02-00667.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dittrich L., Morairty S.R., Warrier D.R., Kilduff T.S. Homeostatic sleep pressure is the primary factor for activation of cortical nNOS/NK1 neurons. Neuropsychopharmacology. 2015;40:632–639. doi: 10.1038/npp.2014.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dityatev A., Rusakov D.A. Molecular signals of plasticity at the tetrapartite synapse. Curr. Opin. Neurobiol. 2011;21:353–359. doi: 10.1016/j.conb.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhart J.M., Leone M.J., Paladino N., Evans J.A., Castanon-Cervantes O., Davidson A.J., Golombek D.A. Suprachiasmatic astrocytes modulate the circadian clock in response to TNF-alpha. J. Immunol. 2013;191:4656–4664. doi: 10.4049/jimmunol.1300450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eban-Rothschild A., Appelbaum L., de Lecea L. Neuronal mechanisms for sleep/wake regulation and modulatory drive. Neuropsychopharmacology. 2018;2018 doi: 10.1038/npp.2017.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlen J.C., Brager A.J., Baggs J., Pinckney L., Gray C.L., Debruyne J.P., Esser K.A., Takahashi J.S., Paul K.N. Bmal1 function in skeletal muscle regulates sleep. eLife. 2017;6:e26557. doi: 10.7554/eLife.26557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Helou J., Belanger-Nelson E., Freyburger M., Dorsaz S., Curie T., La Spada F., Gaudreault P.-O., Beaumont E., Pouliot P., Lesage F., Frank M.G., Franken P., Mongrain V. Neuroligin-1 links neuronal activity to sleep-wake regulation. PNAS. 2013;110:9974–9979. doi: 10.1073/pnas.1221381110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott A.S., Nunez A.A. An ultrastructural study of somal appositions in the suprachiasmatic nucleus and anterior hypothalamus of the rat. Brain Res. 1994;662:278–282. doi: 10.1016/0006-8993(94)90826-5. [DOI] [PubMed] [Google Scholar]
- Elliott K.J., Weber E.T., Rea M.A. Adenosine A1 receptors regulate the response of the hamster circadian clock to light. Eur. J. Pharmacol. 2001;414:45–53. doi: 10.1016/s0014-2999(01)00786-5. [DOI] [PubMed] [Google Scholar]
- Evans J.A. Collective timekeeping among cells of the master circadian clock. J. Endocrinol. 2016;230:R27–R49. doi: 10.1530/JOE-16-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J., Wang Y., Krueger J.M. Mice lacking the TNF 44 kDa receptor fail to sleep more after TNFa treatment. J. Neurosci. 1997;17:5949–5955. doi: 10.1523/JNEUROSCI.17-15-05949.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J., Wang Y., Krueger K.E. Effects of interleukin-1b on sleep are mediated by the type I receptor. Am. J. Physiol. 1998;274:R660. doi: 10.1152/ajpregu.1998.274.3.R655. [DOI] [PubMed] [Google Scholar]
- Faraguna U., Vyazovskiy V.V., Nelson A.B., Tononi G., Cirelli C. A causal role for brain-derived neurotrphic factor in the homeostatic regulation of sleep. J. Neurosci. 2008;28:4088–4095. doi: 10.1523/JNEUROSCI.5510-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedorkova L., Rutishauser U., Prosser R.A., Shen H., Glass J.D. Removal of polysialic acid from the SCN potentiates nonphotic circadian phase resetting. Physiol. Behav. 2002;77:361–369. doi: 10.1016/s0031-9384(02)00880-6. [DOI] [PubMed] [Google Scholar]
- Fellin T., Sul J.-Y., D'Ascenzo M., Takano H., Pascual O., Haydon P.G. Bidirectional astrocyte-neuron communication: the many roles of glutamate and ATP. Novartis Found. Symp. 2017;276:208–217. doi: 10.1002/9780470032244.ch16. [DOI] [PubMed] [Google Scholar]
- Fenner B.M. Truncated TrkB: beyond a dominant negative receptor. Cytokine Growth Factors. 2012;23:15–24. doi: 10.1016/j.cytogfr.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Fields R.D., Araque A., Johansen-Berg H., Lim S.-S., Lynch G., Nave K.-A., Nedergaard M., Perez R., Sejnowski T., Wake H. Glial biology in learning and cognition. Neuroscientist. 2013;20:426–431. doi: 10.1177/1073858413504465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher S.P., Foster R.G., Peirson S.N. The circadian control of sleep. Handb. Exp. Pharmacol. 2013;217:157–183. doi: 10.1007/978-3-642-25950-0_7. [DOI] [PubMed] [Google Scholar]
- Fiumelli H., Jabaudon D., Magistretti P.J., Martin J.L. BDNF stimulates expression, activity and release of tissue-type plasminogen activator in mouse cortical neurons. Eur. J. Neurosci. 1999;11:1639–1646. doi: 10.1046/j.1460-9568.1999.00580.x. [DOI] [PubMed] [Google Scholar]
- Fonken L.K., Frank M.G., Kitt M.M., Barrientos R.M., Watkins L.R., Maier S.F. Microglia inflammatory responses are controlled by an intrinsic circadian clock. Brain Behav. Immunol. 2015;45:171–179. doi: 10.1016/j.bbi.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraigne J.J., Torontali Z.A., Snow M.B., Peever J.H. REM sleep at its core- circuits, neurotransmitters, and pathophysiology. Front. Neurol. 2015;6:123. doi: 10.3389/fneur.2015.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freyburger M., Pierre A., Paquette G., Belanger-Nelson E., Bedont J., Gaudreault P.O., Drolet G., Laforest S., Blackshaw S., Cermakian N., Doucet G., Mongrain V. EphA4 is involved in sleep regulation but not in the electrophysiological response to sleep deprivation. Sleep. 2016;39:613–624. doi: 10.5665/sleep.5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Futai K., Kim M.J., Hashikawa T., Scheiffele P., Sheng M., Hayashi Y. Retrograde modulation of presynaptic release probability through signaling mediated by PSD-95-neuroligin. Nat. Neurosci. 2007;10:186–195. doi: 10.1038/nn1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gakuba C., Gaberel T., Goursaud S., Bourges J., Di Palma C., Quenault A., Martinez de Lizarrondo S., Vivien D., Gauberti M. General anesthesia inhibits the activity of the "glymphatic system". Theranostics. 2018;8:710–722. doi: 10.7150/thno.19154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallego M., Virshup D.M. Post-translational modifications regulate the ticking of the circadian clock. Nat. Rev. 2007;8:139–148. doi: 10.1038/nrm2106. [DOI] [PubMed] [Google Scholar]
- Gast H., Gordic S., Petrzilka S., Lopez M., Muller A., Gietl A., Hock C., Birchler T., Fontana A. Transforming growth factor-beta inhibits the expression of clock genes. Ann. NY Acad. Sci. 2012;1261:79–87. doi: 10.1111/j.1749-6632.2012.06640.x. [DOI] [PubMed] [Google Scholar]
- Georgakopoulos A., Litterst C., Ghersi E., Baki L., Xu C., Serban G., Robakis N.K. Metalloproteinase/Presenilin1 processing of ephrinB regulates EphB-induced Src phosphorylation and signaling. EMBO J. 2006;25:1242–1252. doi: 10.1038/sj.emboj.7601031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gettins P.G.W., Olson S.T. Inhibitory serpins. New insights into their folding, polymerization, regulation and clearance. Biochem. J. 2016;473:2273–2293. doi: 10.1042/BCJ20160014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillette M.U., Reppert S.M. The hypothalamic suprachiasmatic nuclei: circadian patterns of vasopressin secretion and neuronal activity in vitro. Brain Res. Bull. 1987;19:135–139. doi: 10.1016/0361-9230(87)90176-6. [DOI] [PubMed] [Google Scholar]
- Gillette M.U., Wang T.A. Brain circadian oscillators and redox regulation in mammals. Antioxid. Redox Signal. 2014;20:2955–2965. doi: 10.1089/ars.2013.5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girardet C., Becquet D., Blanchard M.-P., Francois-Bellan A.M., Bosler O. Neuroglial and synaptic rearrangements associated with photic entrainment of the circadian clock in the suprachiasmatic nucleus. Eur. J. Neurosci. 2010;32:2133–2142. doi: 10.1111/j.1460-9568.2010.07520.x. [DOI] [PubMed] [Google Scholar]
- Girardet C., Blanchard M.-P., Ferracci G., Leveque C., Moreno M., Francois-Bellan A.-M., Becquet D., Bosler O. Daily changes in synaptic innervation of VIP neurons in the rat suprachiasmatic nucleus: contribution of glutamatergic afferents. Eur. J. Neurosci. 2010;31:359–370. doi: 10.1111/j.1460-9568.2009.07071.x. [DOI] [PubMed] [Google Scholar]
- Glass J., Grossman G., Prosser R., 2004. Removal of polysialylated NCAM from the SCN abolishes the sensitizing effect of brain-derived neurotropic factor on mouse photic phase-resetting. In: Proceedings of the Society Res Biol Rhythms#289.
- Glass J.D., Shen H., Fedorkova L., Chen L., Tomasiewicz H., Watanabe M. Polysialylated neural cell adhesion molecule modulates photic signaling in the mouse suprachiasmatic nucleus. Neurosci. Lett. 2000;280:207–210. doi: 10.1016/s0304-3940(00)00786-2. [DOI] [PubMed] [Google Scholar]
- Glass J.D., Watanabe M., Fedorkova L., Shen H., Ungers G., Rutishauser U. Dynamic regulation of polysialylated neural cell adhesion molecule in the suprachiasmatic nucleus. Neuroscience. 2003;117:203–211. doi: 10.1016/s0306-4522(02)00817-5. [DOI] [PubMed] [Google Scholar]
- Godin A.G., Varela J.A., Gao Z., Danne N., Pupuis J.P., Lounis B., Groc L., Cognet L. Single-nanotube tracking reveals the nanoscale organization of the extracellular space in the live brain. Nat. Nanotechnol. 2017;12:238–243. doi: 10.1038/nnano.2016.248. [DOI] [PubMed] [Google Scholar]
- Golombek D.A., Agostino P.V., Plano S.A., Ferreyra G.A. Signaling in the mammalian circadian clock: the NO-cGMP pathway. Neurochem. Int. 2004;45:929–936. doi: 10.1016/j.neuint.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Greene R.W. Role for neuronal nitric oxide synthase in sleep homeostasis and arousal. PNAS. 2013;110:19982–19983. doi: 10.1073/pnas.1319863110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene R.W., Bjorness T.E., Suzuki A. The adenosine-mediated, neuronal-glial, homeostatic sleep response. Curr. Opin. Neurobiol. 2017;44:242. doi: 10.1016/j.conb.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra-Gomes S., Sousa N., Pinto L., Oliveira J.F. Functional roles of astrocyte calcium elevations: from synapses to behavior. Front. Cell Neurosci. 2018;11:427. doi: 10.3389/fncel.2017.00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guldner F.H., Bahar E., Young C.A., Ingham C.A. Structural plasticity of optic synapses in the rat suprachiasmatic nucleus: adaptation to long-term influence of light and darkness. Cell Tissue Res. 1997;287:43–60. doi: 10.1007/s004410050730. [DOI] [PubMed] [Google Scholar]
- Gundersen V., Storm-Mathisen J., Hildegard Bergersen L. Neuroglial transmission. Physiol. Rev. 2015;95:695–726. doi: 10.1152/physrev.00024.2014. [DOI] [PubMed] [Google Scholar]
- Halassa M.M., Florian C., Fellin T., Munoz J.R., Lee S.Y., Abel T., Haydon P.G., Frank M.G. Astrocytic modulation of sleep homeostasis and cognitive consequences of sleep loss. Neuron. 2009;61:213–219. doi: 10.1016/j.neuron.2008.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallworth R., Cato M., Colbert C., Rea M.A. Presynaptic adenosine A1 receptors regulate retinohypothalamic neurotransmission in the hamster suprachiasmatic nucleus. J. Neurobiol. 2002;52:230–240. doi: 10.1002/neu.10080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halter K., Prosser R., (Submitted for publication) Time of day determines activity and role of matrix metalloproteinase-2 and -9 in the mammalian circadian clock.
- Hanke M.L., Kielian T. Toll-like receptors in health and disease in the brain: mechanisms and therapeutic potential. Clin. Sci. 2011;121:367–387. doi: 10.1042/CS20110164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings G.A., Coleman T.A., Haudenschild C.C., Stefansson S., Smith E.P., Barthlow R., Cherry S., Sandkvist M., Lawrence D.A. Neuroserpin, a brain-associated inhibitor of tissue plasminogen activator is localized primarily in neurons. Implications for the regulation of motor learning and neuronal survival. J. Biol. Chem. 1997;272:33062–33067. doi: 10.1074/jbc.272.52.33062. [DOI] [PubMed] [Google Scholar]
- Hastings M.H., Brancaccio M., Maywood E.S. Circadian pacemaking in cells and circuits of the suprachiasmatic nucleus. J. Neuroendocr. 2014;26:2–10. doi: 10.1111/jne.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog E.D. Neurons and networks in daily rhythms. Nat. Rev. 2007;8:790–802. doi: 10.1038/nrn2215. [DOI] [PubMed] [Google Scholar]
- Holst S.C., Landolt H.-P. Sleep homeostasis, metabolism, and adenosine. Curr. Sleep Med. 2015;1:27–37. [Google Scholar]
- Hsu J.C., Lee Y.S., Chang C.N., Ling E.A., Lan C.T. Sleep deprivation prior to transient global cerebral ischemia attenuates glial reaction in the rat hippocampal formation. Brain Res. 2003;984:170–181. doi: 10.1016/s0006-8993(03)03128-7. [DOI] [PubMed] [Google Scholar]
- Huang Z.-L., Zhang Z., Qu W.-M. Roles of adenosine and its receptors in sleep-wake regulation. Int. Rev. Neurobiol. 2014;119:349–371. doi: 10.1016/B978-0-12-801022-8.00014-3. [DOI] [PubMed] [Google Scholar]
- Iasevoli F., Tomasetti C., de Bartolomeis A. Scaffolding proteins of the post-synaptic density contribute to synaptic plasticity by regulating receptor localization and distribution: relevance for neuropsychiatric diseases. Neurochem. Res. 2013;38:1–22. doi: 10.1007/s11064-012-0886-y. [DOI] [PubMed] [Google Scholar]
- Imeri L., Opp M.R. How (and why) the immune system makes us sleep. Nat. Rev. 2009;10:199–210. doi: 10.1038/nrn2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingiosi A.M., Opp M.R. Sleep and immunomodulatory responses to systemic lipopolysaccharide in mice selectively expressing interleukin-1 receptor 1 on neurons or astrocytes. Glia. 2016;64:780–791. doi: 10.1002/glia.22961. [DOI] [PubMed] [Google Scholar]
- Ingiosi A.M., Raymond R.M., Jr, Pavlova M.N., Opp M.R. Selective contributions of neuronal and astroglial interleukin-1 receptor 1 to the regulation of sleep. Brain Behav. Immun. 2015;48:244–257. doi: 10.1016/j.bbi.2015.03.014. [DOI] [PubMed] [Google Scholar]
- Irwin M.R., Opp M.R. Sleep health: reciprocal regulation of sleep and innate immunity. Neuropsychopharmacology. 2017;42:129–155. doi: 10.1038/npp.2016.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer R., Wang T.A., Gillette M.U. Circadian gating of neuronal functionality: a basis for iterative metaplasticity. Front. Syst. Neurosci. 2014;8:164. doi: 10.3389/fnsys.2014.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayakumar A.R., Apeksha A., Norenberg M.D. Role of matricellular proteins in disorders of the central nervous system. Neurochem. Res. 2017;42:858–875. doi: 10.1007/s11064-016-2088-5. [DOI] [PubMed] [Google Scholar]
- Jewett K.A., Krueger J.M. Humoral sleep regulation: interleukin-1 and tumor necrosis factor. Vit. Horm. 2012;89:241–257. doi: 10.1016/B978-0-12-394623-2.00013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewett K.A., Taishi P., Sengupta P., Roy S., Davis C.J., Krueger J.M. Tumor necrosis factor enhances the sleep-like state and electrical stimulation iduces a wake-like state in co-cultures of neurons and glia. Eur. J. Neurosci. 2015;42:2078–2090. doi: 10.1111/ejn.12968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang M., Polepalli J., Chen L.Y., Zhang B., Sudhof T.C., Malenka R.C. Conditional ablation of neurligin-1 in CA1 pyramidal neurons blocks LTP by a cell-autonomous NMDA receptor-independent mechanism. Mol. Psychiatry. 2017;22:375–383. doi: 10.1038/mp.2016.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju Y.E., Lucey B.P., Holtzman D.M. Sleep and Alzheimer disease pathology—a bidirectional relationship. Nat. Rev. Neurol. 2014;10:115–119. doi: 10.1038/nrneurol.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalderon N., Ahonen K., Federoff S. Developmental transition in plasticity properties of differentiating astrocytes: age-related biochemical profile of plasminogen activators in astroglial cultures. Glia. 1990;3:413–426. doi: 10.1002/glia.440030513. [DOI] [PubMed] [Google Scholar]
- Kalinchuk A.V., Stenberg D., Rosenberg P.A., Porkka-Heiskanen T. Inducible and neuronal nitric oxide synthases (NOS) have complementary roles in recovery sleep induction. Eur. J. Neurosci. 2006;24:1443–1456. doi: 10.1111/j.1460-9568.2006.05019.x. [DOI] [PubMed] [Google Scholar]
- Kanda T., Ohyama K., Muramoto H., Kitajima N., Sekiya H. Promising techniques to illuminate neuromodulatory control of the cerebral cortex in sleeping and waking states. Neurosci. Res. 2017;118:92–103. doi: 10.1016/j.neures.2017.04.009. [DOI] [PubMed] [Google Scholar]
- Kanekiyo T., Bu G. Receptor-associated protein interacts with amyloid-beta peptide and promotes its cellular uptake. J. Biol. Chem. 2009;284:33352–33359. doi: 10.1074/jbc.M109.015032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelai S., Maussion G., Noble F., Boni C., Ramoz N., Moalic J.-M., Peuchmaur M., Gorwood P., Simonneau M. Nrxn3 upregulation in the globus pallidus of mice developing cocaine addiction. NeuroReport. 2008;19:751–755. doi: 10.1097/WNR.0b013e3282fda231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrisk M.E., Cingolani L.A., Koleske A.J. ECM receptors in neuronal structure, synaptic plasticity, and behavior. Prog. Brain Res. 2014;214:101–131. doi: 10.1016/B978-0-444-63486-3.00005-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiessling S., O'Callaghan E.K., Freyburger M., Cermakian N., Mongrain V. The cell adhesion molecule EphA4 is involved in circadian clock functions. Genes Brain Behav. 2017 doi: 10.1111/gbb.12387. [DOI] [PubMed] [Google Scholar]
- Kovalzon V.M., Moiseenko L.S., Ambaryan A.V., Kurtenback S., Shestopalov V.I., Panchin Y.V. Sleep-wakefulnesss cycle and behavior in pannexin1 knockout mice. Behav. Brain Res. 2017;318:24–27. doi: 10.1016/j.bbr.2016.10.015. [DOI] [PubMed] [Google Scholar]
- Krizo J.A., Moreland L.E., Mou X., Prosser R.A., Mintz E.M. Regulation of locomotor activity in fed, fasted, and food-restricted mice lacking tissue-type plasminogen activator. BMC Physiol. 2018;18:2. doi: 10.1186/s12899-018-0036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger J.M. The role of cytokines in sleep regulation. Curr. Pharm. Des. 2008;14:3408–3416. doi: 10.2174/138161208786549281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger J.M., Clinton J.M., Winters B.D., Zielinski M.R., Taishi P., Jewett K.A., Davis C.J. Involvement of cytokines in slow wave sleep. Prog. Brain Res. 2011;193:39–47. doi: 10.1016/B978-0-444-53839-0.00003-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger J.M., Huang Y.H., Rector D.M., Buysse D.J. Sleep: a synchrony of cell activity-driven small network states. Eur. J. Neurosci. 2013;38:2199–2209. doi: 10.1111/ejn.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger J.M., Taishi P., De A., Davis C.J., Winters B.D., Clinton J., Szentirmai E., Zielinski M.R. ATP and the purine type 2X7 receptor affect sleep. J. Appl. Physiol. 2010;109:1318–1327. doi: 10.1152/japplphysiol.00586.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krystal A.D., Benca R.M., Kilduff T.S. Understanding the sleep-wake cycle: sleep, insomania, and the orexin system. J. Clin. Psychiatry. 2013;74(suppl. 1):3–20. doi: 10.4088/JCP.13011su1c. [DOI] [PubMed] [Google Scholar]
- Kubota K., Inoue K., Hashimoto R., Kumamoto N., Kosuga A., Tatsumi M., Kamijima K., Kunugi H., Iwata N., Ozaki N., Takeda M., Tohyama M. Tumor necrosis factor receptor-associated protein 1 regulates cell adhesion and synaptic morphology via modulation of N-cadherin expression. J. Neurochem. 2009;110:496–508. doi: 10.1111/j.1471-4159.2009.06099.x. [DOI] [PubMed] [Google Scholar]
- Kuhn M., Wolf E., Maier J.G., Mainberger F., Feige B., Schmid H., Burklin J., Maywald S., Mall V., Jung N.H., Reis J., Spiegelhalder K., Kloppel S., Sterr A., Eckert A., Riemann D., Normann C., Nissen C. Sleep recalibrates homeostatic and associative synaptic plasticity in the human cortex. Nat. Commun. 2016;7:12455. doi: 10.1038/ncomms12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacagnina M.J., Rivera P.D., Bilbo S.D. Glial and neuroimmune mechanisms as critical modulators of drug use and abuse. Neuropsychopharmacology. 2017;42:156–177. doi: 10.1038/npp.2016.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin A., Chen M.Y., Kirszenblat L., Reinhard J., vanSwinderen B., Claudianos C. Neurexin-1 regulates sleep and synaptic plasticity in Drosophila melanogaster. Eur. J. Neurosci. 2015;42:2455–2466. doi: 10.1111/ejn.13023. [DOI] [PubMed] [Google Scholar]
- Lau L.T., Yu A.C.H. Astrocytes produce and release interleukin-1, interleukin-6, tumor necrosis factor alpha and interferon-gamma following traumatic and metabolic injury. J. Neurotrauma. 2004;53:351–359. doi: 10.1089/08977150151071035. [DOI] [PubMed] [Google Scholar]
- Lavialle M., Serviere J. Circadian fluctuations in GFAP distribution in the Syrian hamster suprachiasmatic nucleus. NeuroReport. 1993;4:1243–1246. doi: 10.1097/00001756-199309000-00008. [DOI] [PubMed] [Google Scholar]
- Lee T.W., Coates L.C., Birch N.P. Neuroserpin regulates N-cadherin-mediated cell adhesion independently of its activity as an inhibitor of tissue plasminogen activator. J. Neurosci. Res. 2008;86:1243–1253. doi: 10.1002/jnr.21592. [DOI] [PubMed] [Google Scholar]
- Lee T.W., Tsang V.W.K., Loef E.J., Birch N.P. Physiological and pathological functions of neuroserpin: regulation of cellular responses through multiple mechanisms. Semin. Cell Dev. Biol. 2017;62:152–159. doi: 10.1016/j.semcdb.2016.09.007. [DOI] [PubMed] [Google Scholar]
- Lehman M.N., Silver R., Gladstone W.R., Kahn R.M., Gibson M., Bittman E.L. Circadian rhythmicity restored by neural transplant: immunocytochemical characterization of the graft and its integration with the host brain. J. Neurosci. 1986;7:1626–1638. doi: 10.1523/JNEUROSCI.07-06-01626.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesca G., Rudolf G., Labalme A., Hirsch E., Arzimanoglou A., Genton P., Motte J., de Saint Martin A., Valenti M.P., Boulay C., De Bellescize J., Keo-Kosal P., Boutry-Kryza N., Edery P., Sanlaville D., Szepetowski P. Epileptic encephalopathies of the Landau-Kleffner and continuous spike and waves during slow-wave sleep types: genomic dissection makes the link with autism. Epilepsy. 2012;53:1526–1538. doi: 10.1111/j.1528-1167.2012.03559.x. [DOI] [PubMed] [Google Scholar]
- Levy A.D., Omar M.H., Koleske A.J. Extracellular matrix control of dendritic spine and synapse structure and plasticity in adulthood. Front. Neuroanat. 2014;8:116. doi: 10.3389/fnana.2014.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Zhou Z., Zhang X., Tong H., Li P., Zhang Z.C., Jia Z., Xie W., Han J. Drosophila neuroligin 4 regulates sleep through modulating GABA transmission. J. Neurosci. 2013;13:15545–15554. doi: 10.1523/JNEUROSCI.0819-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang F.-Q., Allen G., Earnest D. Role of brain-derived neurotrophic factor in the circadian regulation of the suprachiasmatic pacemaker by light. J. Neurosci. 2000;20:2978–2987. doi: 10.1523/JNEUROSCI.20-08-02978.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang F.-Q., Sohrabji F., Miranda R., Earnest B., Earnest D. Expression of brain-derived neurotrophic factor and its cognate receptor, TrkB, in the rat suprachiasmatic nucleus. Exp. Neurol. 1998;151:184–193. doi: 10.1006/exnr.1998.6804. [DOI] [PubMed] [Google Scholar]
- Lin L., Faraco J., Li R., Kadotani H., Rogers W., Lin X., Qiu X., de Jong P.J., Nishino S., Mignot E. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell. 1999;98:365–376. doi: 10.1016/s0092-8674(00)81965-0. [DOI] [PubMed] [Google Scholar]
- Liu A., Zhou Z., Dang R., Zhu Y., Qi J., He G., Leung C., Pak D., Jia Z., Xie W. Neuroligin 1 regulates spines and synaptic plasticity via LIMK1/cofilin-mediated actin reorganization. J. Cell Biol. 2016;212:449–463. doi: 10.1083/jcb.201509023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Grace K.P., Horner R.L., Cortez M.A., Shao Y., Jia Z. Neuroligin 3 R451C mutation alters electroencephalography spectral activity in an animal model of autism spectrum disorders. Mol. Brain. 2017;10:10. doi: 10.1186/s13041-017-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan R.W., Sarkar D.K. Circadian nature of immune function. Mol. Cell. Endocrinol. 2012;349:82–90. doi: 10.1016/j.mce.2011.06.039. [DOI] [PubMed] [Google Scholar]
- Lohman A.W., Isakson B.E. Differentiating connexin hemichannels and pannexin channels in cellular ATP release. FEBS Lett. 2014;588:1379–1398. doi: 10.1016/j.febslet.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackiewicz M., Shockley K.R., Romer M.A., Galante R.J., Zimmerman J.E., Naidoo N., Baldwin D.A., Jensen S.T., Churchill G.A., Pack A.I. Macromolecule biosynthesis: a key function of sleep. Physiol. Genom. 2007;31:441–457. doi: 10.1152/physiolgenomics.00275.2006. [DOI] [PubMed] [Google Scholar]
- Mackiewicz M., Zimmerman J.E., Shockley K.R., Churchill G.A., Pack A.I. What are microarrays teaching us about sleep? Trends Mol. Med. 2009;15:79–87. doi: 10.1016/j.molmed.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen C.D., Ferraris G.M.S., Andolfo A., Cunningham O., Sidenius N. uPAR-induced cell adhesion and migration: vitronectin provides the key. J. Cell Biol. 2007;177:927–939. doi: 10.1083/jcb.200612058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier W., Bednorz M., Meister S., Roebroek A., Weggen S., Schmitt U., Pietrzik C.U. LRP1 is critical for the surface distribution and internalization of the NR2B NMDA receptor subtype. Mol. Neurodegen. 2013;8:25. doi: 10.1186/1750-1326-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malarkey E.B., Parpura V. Mechanisms of glutamate release from astrocytes. Neurochem. Int. 2008;52:142–154. doi: 10.1016/j.neuint.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malemud C.J. Matrix metalloproteinases (MMPs) in health and disease: an overview. Front. Biosci. 2006;11:1696–1701. doi: 10.2741/1915. [DOI] [PubMed] [Google Scholar]
- Masos T., Miskin R. mRNAs encoding urokinase-type plasminogen activator and plasminogen activator inhibitor-1 are elevated in the mouse brain following kainate-mediated excitation. Mol. Brain Res. 1997;47:157–169. doi: 10.1016/s0169-328x(97)00040-5. [DOI] [PubMed] [Google Scholar]
- Massart R., Freyburger M., Suderman M., Paquet J., El Helou J., Belanger-Nelson E., Rachalski a, Koumar O.C., Carrier J., Szyf M., Mongrain V. The genome-wide landscape of DNA methylation and hydroxymethylation in response to sleep deprivation impacts on synaptic plasticity genes. Transl. Psychiatry. 2014;4:e347. doi: 10.1038/tp.2013.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuki T., Takasu M., Hirose Y., Murakoshi N., Sinton C.M., Motoike T., Yangisawa M. GABAA receptor-mediated input change on orexin neurons following sleep deprivation in mice. Neuroscience. 2015;284:217–224. doi: 10.1016/j.neuroscience.2014.09.063. [DOI] [PubMed] [Google Scholar]
- Maurer S.V., Williams C.L. The cholinergic system modulates memory and hippocampal plasticity via its interactions with non-neuronal cells. Front. Immunol. 2017;8:1489. doi: 10.3389/fimmu.2017.01489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medcalf R.L. Fibrinolysis: from blood to the brain. J. Thromb. Haemost. 2017 doi: 10.1111/jth.13849. [DOI] [PubMed] [Google Scholar]
- Meier D., Lopez M., Franken P., Fontana A., 2015. Twist1 is a TNF-inducible inhibitor of Clock mediated activation of Period genes. PLOS One, 0137229. [DOI] [PMC free article] [PubMed]
- Meijer J.H., Schwartz W.J. In search of the pathways for light-induced pacemaker resetting in the suprachiasmatic nucleus. J. Biol. Rhythm. 2003;18:235–249. doi: 10.1177/0748730403018003006. [DOI] [PubMed] [Google Scholar]
- Menger G.J., Lu K., Thomas T., Cassone V.M., Earnest D.J. Circadian profiling of the transcriptome in immortalized rat SCN cells. Physiol. Genom. 2005;21:370–381. doi: 10.1152/physiolgenomics.00224.2004. [DOI] [PubMed] [Google Scholar]
- Merino P., Diaz A., Yepes M. Urokinase-type plasminogen activator (uPA) and its receptor (uPAR) promote neurorepair in the ischemic brain. Recept. Clin. Investig. 2017;4 [PMC free article] [PubMed] [Google Scholar]
- Michaluk P., Kolodziej L., Mioduszewska B., Wilczynski G.M., Dzwonek J., Jaworski J., Gorecki D.C., Ottersen O.P., Kaczmarek L. Beta-dystroglycan as a target for MMP-9, in response to enhanced neuronal activity. J. Biol. Chem. 2007;282:16036–16041. doi: 10.1074/jbc.M700641200. [DOI] [PubMed] [Google Scholar]
- Michel S., Clark J.P., Ding J.M., Colwell C.S. Brain-derived neurotrophic factor and neurotrophin receptors modulate glutamate-induced phase shifts of the suprachiasmatic nucleus. Eur. J. Neurosci. 2006;24:1109–1116. doi: 10.1111/j.1460-9568.2006.04972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkelsen J.D., Larsen P.J., Mick G., Vrang N., Ebling F.J.P., Maywood E.S., Hastings M.H., Moller M. Gating of retinal inputs through the suprachiasmatic nucleus: role of excitatory neurotransmission. Neurochem. Int. 1995;27:263–272. doi: 10.1016/0197-0186(95)00039-b. [DOI] [PubMed] [Google Scholar]
- Miles L.A., Parmer R.J. Plasminogen receptors: the first quarter century. Semin. Thromb. Hemost. 2013;39:329–337. doi: 10.1055/s-0033-1334483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milev N.B., Rey G., Valekunja U.K., Edgar R.S., O'Neill J.S., Reddy A.B. Analysis of the redox oscillations in the circadian clockwork. Method Enzym. 2015;552:185–210. doi: 10.1016/bs.mie.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J.D. On the nature of the circadian clock in mammals. Am. J. Physiol. 1993;264:R821–R832. doi: 10.1152/ajpregu.1993.264.5.R821. [DOI] [PubMed] [Google Scholar]
- Miller M.W., Spear L.P. The alcoholism generator. Alcohol Clin. Exp. Res. 2006;30:1466–1469. doi: 10.1111/j.1530-0277.2006.00177.x. [DOI] [PubMed] [Google Scholar]
- Minor K.H., Peterson C.B. PAI-1 promotes the self-association of vitronectin into complexes exhibiting altered incorporation into the extracellular matrix. J. Biol. Chem. 2002;277:10377. doi: 10.1074/jbc.M109564200. (-10345) [DOI] [PubMed] [Google Scholar]
- Miranda E., Lomas D.A. Neuroserpin: a serpin to think about. Cell Mol. Life Sci. 2006;63:709–722. doi: 10.1007/s00018-005-5077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongrain V., Hernandez S.A., Pradervand S., Dorsaz S., Curie T., Hagiwara G., Gip P., Heller H.C., Franken P. Separating the contribution of glucocorticoids and wakefulness to the molecular and electrophysiological correlates of sleep homeostasis. Sleep. 2010;33:1147–1157. doi: 10.1093/sleep/33.9.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore R.Y. Organization and function of a central nervous system circadian oscillator: the suprachiasmatic hypothalamic nucleus. Fed. Proc. 1983;42:2783–2789. [PubMed] [Google Scholar]
- Moore R.Y. Organization of the mammalian circadian system. CIBA Found. Symp. 1995;183:88–106. [PubMed] [Google Scholar]
- Moore R.Y., Lenn N.J. A retinohypothalamic projection in the rat. J. Comp. Neurol. 1972;146:1–14. doi: 10.1002/cne.901460102. [DOI] [PubMed] [Google Scholar]
- Morairty S.R., Dittrich L., Pasumarthi R.K., Valladao D., Heiss J.E., Geraschchenko D., Kilduff T.S. A role for cortical nNOS/NK1 neurons in coupling homeostatic sleep drive to EEG slow wave activity. PNAS. 2013;110:20272–20277. doi: 10.1073/pnas.1314762110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin L.P. SCN organization reconsidered. J. Biol. Rhythm. 2007;22:3–13. doi: 10.1177/0748730406296749. [DOI] [PubMed] [Google Scholar]
- Moriya T., Yamanouchi S., Fukushima T., Shimazoe T., Shibata S., Watanabe S. Involvement of 5-HT1A receptor mechanisms in the inhibitory effects of methamphetamine on photic responses in the rodent suprachiasmatic nucleus. Brain Res. 1996;740:261–267. doi: 10.1016/s0006-8993(96)00860-8. [DOI] [PubMed] [Google Scholar]
- Mou X., Peterson C.B., Prosser R.A. Tissue-type plasminogen activator-plasmin-BDNF modulate glutamate-induced phase-shifts of the mouse suprachiasmatic circadian clock in vitro. Eur. J Neurosci. 2009;30:1451–1460. doi: 10.1111/j.1460-9568.2009.06946.x. [DOI] [PubMed] [Google Scholar]
- Muir E.M., Adcock K.H., Morgenstern D.A., Clayton R., von Stillfried N., Rhodes K., Ellis C., Fawcett J.W., Rogers J.H. Matrix metalloproteases and their inhibitors are produced by overlapping populations of activated astrocytes. Mol. Brain Res. 2002;100:103–117. doi: 10.1016/s0169-328x(02)00132-8. [DOI] [PubMed] [Google Scholar]
- Murai K.K., Nguyen L.N., Irie F., Yamaguchi Y., Pasquale E.B. Control of hippocampal dendritic spine morphology through ephrin-A3/EphA4 signaling. Nat. Neurosci. 2003;6:153–160. doi: 10.1038/nn994. [DOI] [PubMed] [Google Scholar]
- Murphy S., Simmons M.L., Agullo L., Garcia A., Feinstein D.L., Galea E., Reis D.J., Minc-Golomb D., Schwartz J.P. Synthesis of nitric oxide in CNS glial cells. TINS. 1993;16:323–328. doi: 10.1016/0166-2236(93)90109-y. [DOI] [PubMed] [Google Scholar]
- Nadir Y., Saharov G., Hoffman R., Keren-Politansky A., Tzoran I., Brenner B., Shochat T. Heparanase procoagulant activity, factor Xa, and plasminogen activator inhibitor 1 are increased in shift work female nurses. Ann. Hematol. 2015;94:1213–1219. doi: 10.1007/s00277-015-2345-8. [DOI] [PubMed] [Google Scholar]
- Nakaya M., Sanada K., Fukada Y. Spatial and temporal regulation of mitogen-activated protein kinase phosphorylation in the mouse suprachiasmatic nucleus. Biochem. Biophys. Res. Commun. 2003;305:494–501. doi: 10.1016/s0006-291x(03)00791-5. [DOI] [PubMed] [Google Scholar]
- Nambu T., Sakurai T., Mizukami K., Hosoya Y., Yanagisawa M., Goto K. Distribution of orexin neurons in the adult rat brain. Brain Res. 1999;827:243–260. doi: 10.1016/s0006-8993(99)01336-0. [DOI] [PubMed] [Google Scholar]
- Ng K.-S., Leung H.-W., Wong P.T.H., Low C.-M. Cleavage of the NR2B subunit amino terminus of N-methyl-D-aspartate (NMDA) receptor by tissue plasminogen activator. Identification of the cleavage site and characterization of ifenprodil and glycine affinities on truncated NMDA receptor. J. Biol. Chem. 2012;287:25520–25529. doi: 10.1074/jbc.M112.374397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris E.H., Strickland S. Modulation of NR2B-regulated contextual fear in the hippocampus by the tissue plasminogen activator system. PNAS. 2007;104:13473–13478. doi: 10.1073/pnas.0705848104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Callaghan E.K., Ballester Roig M.N., Mongrain V. Cell adhesion molecules and sleep. Neurosci. Res. 2017;116:29–38. doi: 10.1016/j.neures.2016.11.001. [DOI] [PubMed] [Google Scholar]
- O'Connor E.C., Bariselli S., Bellone C. Synaptic basis of social dysfunction: a focus on postsynapticc proteins linking group-I mGluRs with AMPARs and NMDARs. Eur. J. Neurosci. 2014;39:1114–1129. doi: 10.1111/ejn.12510. [DOI] [PubMed] [Google Scholar]
- Obiang P., Macrez R., Julliene A., Bertrand T., Lesept F., Ali C., Maubert E., Vivien D., Agin V. GluN2D subunit-containing NMDA receptors control tissue plasminogen activator-mediated spatial memory. J. Neurosci. 2012;32:12726–12734. doi: 10.1523/JNEUROSCI.6202-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olofsson P.S., Rosas-Ballina M., Levine Y.A., Tracey K.J. Rethinking inflammation: neural circuits in the regulation of immunity. Immunol. Rev. 2012;248:188–204. doi: 10.1111/j.1600-065X.2012.01138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ota Y., Zanetti A.T., Hallock R.M. The role of astrocytes in the regulation of synaptic plasticity and memory formation. Neural Plast. 2013;2013:185463. doi: 10.1155/2013/185463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paladino N., Mul Fedele M.L., Duhart J.M., Marpegan L., Golombek D.A. Modulation of mammalian circadian rhythms by tumor necrosis factor-alpha. Chronobiol. Int. 2014;31:668–679. doi: 10.3109/07420528.2014.886588. [DOI] [PubMed] [Google Scholar]
- Pang P.T., Lu B. Regulation of late-phase LTP and long-term memory in normal and aging hippocampus: role of secreted proteins tPA and BDNF. Ageing Res Rev. 2004;3:407–430. doi: 10.1016/j.arr.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Pang P.T., Teng H.K., Zaitsev E., Woo N.T., Sakata K., Zhen S., Teng K.K., Yung W.-H., Hempstead B.L., Lu B. Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science. 2004;306:487–491. doi: 10.1126/science.1100135. [DOI] [PubMed] [Google Scholar]
- Panja D., Bramham C.R. BDNF mechanisms in late LTP formation: a synthesis and breakdown. Neuropharmacology. 2014;76:664–676. doi: 10.1016/j.neuropharm.2013.06.024. [DOI] [PubMed] [Google Scholar]
- Pannasch U., Freche D., Dallerac G., Ghezali G., Escartin C., Ezan P., Cohen-Salmon M., Benchenane K., Abudara V., Dufour A., Lubke J.H.R., Deglon N., Knott G., Holcman D., Rouach N. Connexin 30 sets synaptic strength by controlling astroglial synapse invasion. Nat. Neurosci. 2014;17:549–558. doi: 10.1038/nn.3662. [DOI] [PubMed] [Google Scholar]
- Papouin T., Dunphy J., Tolman M., Foley J.C., Haydon P.G. Astrocytic control of synaptic function. Philos. Trans. R. Soc. B. 2017;372:20130154. doi: 10.1098/rstb.2016.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park Y.K., Goda Y. Integrins in synapse regulation. Nat. Rev. 2016;17:745–756. doi: 10.1038/nrn.2016.138. [DOI] [PubMed] [Google Scholar]
- Parpura V., Fisher E.S., Lechleiter J.D., Schousboe A., Waagepetersen H.S., Brunet S., Baltan S., Verkhratsky A. Glutamate and ATP at the interface between signaling and metabolism in astroglia: examples from pathology. Neurochem. Res. 2017;42:19–34. doi: 10.1007/s11064-016-1848-6. [DOI] [PubMed] [Google Scholar]
- Pascual O., Casper K.B., Kubera C., Zhang J., Revilla-Sanchez R., Sul J.Y., Takano H., Moss S.J., McCarthy K., Haydon P.G. Astrocytic purinergic signaling coordinates synaptic networks. Science. 2005;310:113–116. doi: 10.1126/science.1116916. [DOI] [PubMed] [Google Scholar]
- Paul A., Crow M., Raudales R., He M., Gillis J., Huang Z.J. Transcriptional architecture of synaptic communication delineates GABAergic neuron identity. Cell. 2017;171:522–539. doi: 10.1016/j.cell.2017.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlak R., Magarinos A.M., Melchor J., McEwen B., Strickland S. Tissue plasminogen activator in the amygdala is critical for stress-induced anxiety-like behavior. Nat. Neurosci. 2003;6:168–174. doi: 10.1038/nn998. [DOI] [PubMed] [Google Scholar]
- Pawlak R., Melchor J.P., Matys T., Skrzypiec A.E., Strickland S. Ethanol-withdrawl seizures are controlled by tissue plasminogen activator via modulation of NR2B-containing NMDA receptors. PNAS. 2005;102:443–448. doi: 10.1073/pnas.0406454102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlak R., Rao B.S.S., Melchor J.P., Chattarji S., McEwen B., Strickland S. Tissue plasminogen activator and plasminogen mediate stress-induced decline of neuronal and cognitive functions in the mouse hippocampus. PNAS. 2005;102:18201–18206. doi: 10.1073/pnas.0509232102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peixoto R.T., Kunz P.A., Kwon H., Mabb A.M., Sabatini B.L., Philpot B.D., Ehlers M.D. Transsynaptic signaling by activity-dependent cleavage of neuroligin-1. Neuron. 2012;76:396–409. doi: 10.1016/j.neuron.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perea G., Araque A. Communication between astrocytes and neurons: a complex language. J. Physiol. 2002;96:199–207. doi: 10.1016/s0928-4257(02)00007-4. [DOI] [PubMed] [Google Scholar]
- Petit J.-M., Burlet-Godinot S., Magistretti P.J., Allaman I. Glycogen metabolism and the homeostatic regulation of sleep. Metab. Brain Dis. 2015;30:263–279. doi: 10.1007/s11011-014-9629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plano S.A., Golombek D.A., Chiesa J.J. Circadian entrainment to light-dark cycles involves extracellular nitric oxide communication within the suprachiasmatic nuclei. Eur. J. Neurosci. 2010;31:876–882. doi: 10.1111/j.1460-9568.2010.07120.x. [DOI] [PubMed] [Google Scholar]
- Podor T.J., Peterson C.B., Lawrence D.A., Stefansson S., Shaughnessy S.G., Foulon D.M., Butcher M., Weitz J.I. Type 1 plasminogen activator inhibitor binds to fibrin via vitronectin. J. Biol. Chem. 2000;275:19788–19794. doi: 10.1074/jbc.M908079199. [DOI] [PubMed] [Google Scholar]
- Poskanzer K.E., Yuste R. Astrocytes regulate cortical state switching in vivo. PNAS. 2016;113:E2675–E2684. doi: 10.1073/pnas.1520759113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presta M., Ennas M.G., Torelli S., Ragnotti G., Gremo F. Synthesis of urokinase-type plasminogen activator and type-1 plasminogen activator inhibitor in neuronal cultures of human fetal brain: stimulation by phorbol ester. J. Neurochem. 1990;55:1647–1654. doi: 10.1111/j.1471-4159.1990.tb04951.x. [DOI] [PubMed] [Google Scholar]
- Prosser R.A., Gillette M.U. The mammalian circadian clock in the suprachiasmatic nuclei is reset in vitro by cAMP. J. Neurosci. 1989;9:1073–1081. doi: 10.1523/JNEUROSCI.09-03-01073.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosser R.A., Rutishauser U., Ungers G., Fedorkova L., Glass J.D. Intrinsic role of polysialylated neural cell adhesion molecule in photic phase resetting of the mammalian circadian clock. J. Neurosci. 2003;23:652–658. doi: 10.1523/JNEUROSCI.23-02-00652.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puentes-Mestril C., Aton S.J. Linking network activity to synaptic plasticity during sleep: hypotheses and recent data. Front. Neural Circ. 2017;11:e00061. doi: 10.3389/fncir.2017.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralph M.R. Circadian rhythms – mammalian aspects. Semin. Cell Dev. Biol. 1996;7:821–830. [Google Scholar]
- Ramanathan A., Nelson A.R., Sagare A.P., Zlokovic B.V. Impaired vascular-mediated clearance of brain amyloid beta in Alzheimer's disease: the role, regulation and restoration of LRP1. Front. Aging Neurosci. 2015;7:136. doi: 10.3389/fnagi.2015.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector D.M., Topchiy I.A., Carter K.M., Rojas M.J. Local functional state differences between rat cortical columns. Brain Res. 2005;1047:45–55. doi: 10.1016/j.brainres.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Reissner C., Runkel F., Missler M. Neurexins. Genome Biol. 2013;14:213. doi: 10.1186/gb-2013-14-9-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose C.R., Felix L., Zeug A., Deitrich D., Reiner A., Henneberger C. Astroglial glutamate signaling and uptake in the hippocampus. Front. Mol. Neurosci. 2018;10:451. doi: 10.3389/fnmol.2017.00451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothaug M., Becker-Pauly C., Rose-John S. The role of interleukin-6 signaling in nervous tissue. Biochim. Biophys. Acta. 2016;1863:1218–1227. doi: 10.1016/j.bbamcr.2016.03.018. [DOI] [PubMed] [Google Scholar]
- Ruben M.D., Hogenesch J.B. Circadian rhythms: move over neurons - astrocytes mediate SCN clock function. Curr. Biol. 2017;27:R350–R352. doi: 10.1016/j.cub.2017.03.055. [DOI] [PubMed] [Google Scholar]
- Rudenko G. Dynamic control of synaptic adhesion and organizing molecules in synaptic plasticity. Neural Plast. 2017;2017:6526151. doi: 10.1155/2017/6526151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusak B. Neural mechanisms for entrainment and generation of mammalian circadian rhythms. Fed. Proc. 1979;38:2689. (-2595) [PubMed] [Google Scholar]
- Saftig P., Reiss K. The "A disintegrin and metalloproteases" ADAM10 and ADAM 17: novel drug targets with therapeutic potential? Eur. J. Cell Biol. 2011;90:525–535. doi: 10.1016/j.ejcb.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Sarowar T., Chhabra R., Vilella A., Boeckers T.M., Zoli M., Grabrucker A.M. Activity and circadian rhythm influence synaptic Shank3 protein levels in mice. J. Neurochem. 2016;138:887–895. doi: 10.1111/jnc.13709. [DOI] [PubMed] [Google Scholar]
- Scammell T.E., Arrigoni E., Lipton J.O. Neural circuitry of wakefulness and sleep. Neuron. 2017;93:747–765. doi: 10.1016/j.neuron.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scemes E., Giaume C. Astrocyte calcium waves: what they are and what they do. Glia. 2006;54:716–725. doi: 10.1002/glia.20374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharbarg E., Daenens M., Lemaitre F., Geoffroy H., Guille-Collignon M., Gallopin T., Rancillac A. Astrocyte-derived adenosine is central to the hynogenic effect of glucose. Sci. Rep. 2017;6:19107. doi: 10.1038/srep19107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiermann C., Kunisaki Y., Frenette P.S. Circadian control of the immune system. Nat. Rev. Immunol. 2013;13:190–198. doi: 10.1038/nri3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz M.D., Congdon S., de la Iglesa H.O. Phase misalignment between suprachiasmatic neuronal oscillators impairs photic behavioral phase shifts but not photic induction of gene expression. J. Neurosci. 2010;30:13150–13156. doi: 10.1523/JNEUROSCI.1853-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeds N.W., Akison L., Minor K. Role of plasminogen activator in spinal cord remodeling after spinal cord injury. Resp. Physiol. Neurobiol. 2009;169:141–149. doi: 10.1016/j.resp.2009.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senkov O., Andjus P., Radenovic L., Soriano E., Dityatev A. Neural ECM molecules in synaptic plasticity, learning, and memory. Prog. Brain Res. 2014;214:53–80. doi: 10.1016/B978-0-444-63486-3.00003-7. [DOI] [PubMed] [Google Scholar]
- Shapiro-Reznik M., Jilg A., Lerner H., Earnest D.J., Zisapel N. Diurnal rhythms in neurexins transcripts and inhibitory/excitatory synapse scaffold proteins in the biological clock. PLOS One. 2012;7:e37894. doi: 10.1371/journal.pone.0037894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H., Glass J.D., Seki T., Watanabe M. Ultrastructural analysis of polysialylated neural cell adhesion molecule in the suprachiasmatic nuclei of the adult mouse. Anat. Rec. 1999;256:448–457. doi: 10.1002/(SICI)1097-0185(19991201)256:4<448::AID-AR11>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Shen H., Watanabe M., Tomasiewicz H., Glass J.D. Genetic deletions of NCAM and PSA impair circadian function in the mouse. Physiol. Behav. 2001;73:185–193. doi: 10.1016/s0031-9384(01)00468-1. [DOI] [PubMed] [Google Scholar]
- Sheng L., Leshchyns'ka I., Sytnyk V. Cell adhesion and intracellular calcium signaling in neurons. Cell Commun. Signal. 2013;11:94. doi: 10.1186/1478-811X-11-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherpa A.D., Xiao F.R., Joseph N., Aoki C., Hrabetova S. Activation of beta-adrenergic receptors in rat visual cortex expands astrocytic processes and reduces extracellular space volume. Synapse. 2016;70:307–316. doi: 10.1002/syn.21908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibata S., Moore R.Y. Electrical and metabolic activity of suprachiasmatic nucleus neurons in hamster hypothalamic slices. Brain Res. 1988;438:374–378. doi: 10.1016/0006-8993(88)91367-4. [DOI] [PubMed] [Google Scholar]
- Sigworth L.A., Rea M.A. Adenosine A1 receptors regulate the response of the mouse circadian clock to light. Brain Res. 2003;960:246–251. doi: 10.1016/s0006-8993(02)03896-9. [DOI] [PubMed] [Google Scholar]
- Slaker M., Blacktop J.M., Sorg B.A. Caught in the net: perineuronal nets and addiction. Neural Plast. 2016;2016:7538208. doi: 10.1155/2016/7538208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A.C.W., Scofield M.D., Kalivas P.W. The tetrapartite synapse: extracellular matrix remodeling contributes to corticoaccumbens plasticity underlying drug addiction. Brain Res. 2015;1628:29–39. doi: 10.1016/j.brainres.2015.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A.J., Verkman A.S. The "glymphatic" mechanism for solute clearance in Alzheimer's disease: game changer or unproven speculation? FASEB J. 2018 doi: 10.1096/fj.201700999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofroniew M.V. Multiple roles for astrocytes as effectors of cytokines and inflammatory mediators. Neuroscientist. 2014;20:160–172. doi: 10.1177/1073858413504466. [DOI] [PubMed] [Google Scholar]
- Song I., Dityatev A. Crosstalk between glia, extracellular matrix and neurons. Brain Res. Bull. 2017 doi: 10.1016/j.brainresbull.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Stellwagen D., Malenka R.C. Synaptic scaling mediated by glial TNF-a. Nature. 2006;440:1054–1059. doi: 10.1038/nature04671. [DOI] [PubMed] [Google Scholar]
- Stockwell J., Jakova E., Cayabyab F.S. Adenosine A1 and A2A receptors in the brain: current research and their role in neurodegeneration. Molecules. 2017;22:22040676. doi: 10.3390/molecules22040676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney A.M., Fleming K.E., McCauley J.P., Rodriguez M.F., Martin E.T., Sousa A.A., Leapman R.D., Scimemi A. PAR1 activation induces rapid changs in glutamate uptake and astrocyte morphology. Sci. Rep. 2017;7:43606. doi: 10.1038/srep43606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sytnyk V., Leshchyns'ka I., Schachner M. Neural cell adhesion molecules of the immunoglobulin superfamily regulate synapse formation, maintenance, and function. TINS. 2017;40:295–308. doi: 10.1016/j.tins.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Taishi P., Bredow S., Guha-Thakurta N., Obal F., Jr, Krueger J.M. Diurnal variations of interleukin-1 beta mRNA and beta-actin mRNA in rat brain. J. Immunol. 1997;75:69–74. doi: 10.1016/s0165-5728(97)00002-7. [DOI] [PubMed] [Google Scholar]
- Taishi P., Sanchez C., Wang Y., Fang J., Harding J.W., Krueger J.M. Conditions that affect sleep alter the expression of molecules associated with synaptic plasticity. Am. J. Physiol. 2001;281:R839–R845. doi: 10.1152/ajpregu.2001.281.3.R839. [DOI] [PubMed] [Google Scholar]
- Thalhammer A., Cingolani L.A. Cell adhesion and homeostatic synaptic plasticity. Neuropharmacology. 2014;78:23–30. doi: 10.1016/j.neuropharm.2013.03.015. [DOI] [PubMed] [Google Scholar]
- Theodosis D.T., Piet R., Poulain D.A., Oliet S.H.R. Neuronal, glial and synaptic remodeling in the adult hypothalamus: functional consequences and role of cell surface and extracellular matrix adhesion molecules. Neurochem. Int. 2004;45:491–501. doi: 10.1016/j.neuint.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Thimgan M.S., Gottschalk L., Toedebusch C., McLeland J., Rechtschaffen A., Gilliland-Roberts M., Duntley S.P., Shaw P.J. Cross-translational studies in human and drosophila identify markers of sleep loss. PLOS One. 2013;8:12. doi: 10.1371/journal.pone.0061016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong H.W., Li Q., Zhang Z.C., Li Y., Han J.H. Neurexin regulates nighttime sleep by modulating synaptic transmission. Sci. Rep. 2016;6:14. doi: 10.1038/srep38246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsien R.Y. Very long-term memories may be stored in the pattern of holes in the perineuronal net. PNAS. 2013;110:12456–12461. doi: 10.1073/pnas.1310158110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tso C.F., Simon T., Greenlaw A.C., Puri T., Mieda M., Herzog E.D. Astrocytes regulate daily rhythms in the suprachiasmatic nucleus and behavior. Curr. Biol. 2017;27:1055–1061. doi: 10.1016/j.cub.2017.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vacas S., Degos V., Maze M. Fragmented sleep enhances postoperative neuroinflammation but not cognitive dysfunction. Anesth. Analg. 2017;124:270–276. doi: 10.1213/ANE.0000000000001675. [DOI] [PubMed] [Google Scholar]
- Van De Craen B., Declerck P.J., Gils A. The biochemistry, physiology and pathological roles of PAI-1 and the requirements for PAI-1 inhibition in vivo. Throm. Res. 2012;130:576–585. doi: 10.1016/j.thromres.2012.06.023. [DOI] [PubMed] [Google Scholar]
- van den Pol A.N., Finkbeiner S.M., Cornell-Bell A.H. Calcium excitability and oscillations in suprachiasmatic nucleus neurons and glia in vitro. J. Neurosci. 1992;12:2648–2664. doi: 10.1523/JNEUROSCI.12-07-02648.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Pol A.N., Strecker G.J., Dudek F.E. Excitatory and inhibitory amino acids and synaptic transmission in the suprachiasmatic nucleus. In: Buijs R.M., Kalsbeek A., Romijn H.J., Pennartz C.M.A., Mirmiran M., editors. Hypothalamic Integration of Circadian Rhythms. Elsevier; Amsterdam: 1996. pp. 41–56. [DOI] [PubMed] [Google Scholar]
- van Gool B., Dedieu S., Emonard H., Roebroek A.J.M. The matricellular receptor LRP1 forms an interface for signaling and endocytosis in modulation of the extracellular tumor environment. Front. Pharmacol. 2015;6:271. doi: 10.3389/fphar.2015.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varbanov H., Dityatev A. Regulation of extrasynaptic signaling by polysialylated NCAM: impact for synaptic plasticity and cognitive functions. Mol. Cell Neurosci. 2016 doi: 10.1016/j.mcn.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Vgontzas A.N., Bixler E.O., Lin H.M., Prolo P., Trakada G., Chrousos G.P. IL-6 and its circadian secretion in humans. Neuroimmunomodulation. 2005;12:131–140. doi: 10.1159/000084844. [DOI] [PubMed] [Google Scholar]
- Vgontzas A.N., Papanicolaou D.A., Bixler E.O., Kales A., Tyson K., Chrousos G.P. Elevation of plasma cytokines in disorders of excissive daytime sleepiness: role of sleep disturbance and obesity. J. Clin. Endocrinol. Metab. 1997;82:1313–1316. doi: 10.1210/jcem.82.5.3950. [DOI] [PubMed] [Google Scholar]
- Wadhwa M., Prabhakar A., Ray K., Roy K., Kumari P., Jha P.K., Kishore K., Kumar S., Panjwani U. Inhibiting the microglia activation improves the spatial memory and adult neurogenesis in rat hippocampus during 48 h of sleep deprivation. J. Neuroinflamm. 2017;14:222. doi: 10.1186/s12974-017-0998-z. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Wang Z., Haydon P.G., Yeung E.S. Direct observation of calcium-independent intercellular ATP signaling in astrocytes. Anal. Chem. 2000;72:2001–2007. doi: 10.1021/ac9912146. [DOI] [PubMed] [Google Scholar]
- Watanabe A., Moriya T., Nisikawa Y., Araki T., Hamada T., Shibata S., Watanabe S. Adenosine A1-receptor agonist attenuates the light-induced phase shifts and fos expression in vivo and optic nerve stimulation-evoked field potentials in suprachiasmatic nucleus in vitro. Brain Res. 1996;740:329–336. doi: 10.1016/s0006-8993(96)00881-5. [DOI] [PubMed] [Google Scholar]
- Watson A.J., Henson K., Dorsey S.G., Frank M.G. The truncated TrkB receptor influences mammalian sleep. Am. J. Physiol. 2015;308:R119–R207. doi: 10.1152/ajpregu.00422.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M., Zhao B.Y., Huo K., Deng Y.N., Shang S.H., Liu J., Li Y.B., Ma L.Y., Jiang Y., Dang L.J., Chen C., Wei S., Zhang J.L., Yang H.L., Gao F., Qu Q.M. Sleep Deprivation Induced Plasma Amyloid-beta Transport Disturbance In Healthy Young Adults. J. Alzheimer Dis. 2017;57:899–906. doi: 10.3233/JAD-161213. [DOI] [PubMed] [Google Scholar]
- Wiera G., Mozrzymas J.W. Extracellular proteolysis in structural and functional plasticity of mossy fiber synapses in hippocampus. Front. Cell. Neurosci. 2015;9:427. doi: 10.3389/fncel.2015.00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisor J.P., Clegern W.C. Quantification of short-term slow wave sleep homeostasis and its disruption by minocycline in the laboratory mouse. Neurosci. Lett. 2011;490:165–169. doi: 10.1016/j.neulet.2010.11.034. [DOI] [PubMed] [Google Scholar]
- Wisor J.P., Clegern W.C., Schmidt M.A. Toll-like receptor 4 is a regulator of monocyte and electroencephalographic responses to sleep loss. Sleep. 2011;34:1335–1345. doi: 10.5665/SLEEP.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisor J.P., Gerashchenko D., Kilduff T.S. Sleep-active neuronal nitric oxide synthase-positive cells of the cerebral cortex: a local regulator of sleep? Curr. Top. Med. Chem. 2011;11:2483–2489. doi: 10.2174/156802611797470367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojtowicz T., Brzdak P., Mozrzymas J.W. Diverse impact of acute and long-term extracellular proteolytic activity on plasticity of neuronal excitability. Front. Cell Neurosci. 2015;9:313. doi: 10.3389/fncel.2015.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Womac A.D., Burkeen J.F., Neuendorff N., Earnest D.J., Zoran M.J. Circadian rhythms of extracellular ATP accumulation in suprachiasmatic nucleus cells and cultured astrocytes. Eur. J. Neurosci. 2009;30:869–876. doi: 10.1111/j.1460-9568.2009.06874.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M.L., Rettori V., al-Shekhlee A., Bongiorno P.B., Canteros G., McCann S.M., Gold P.W., Licinio J. Inducible nitric oxide synthase gene expression in the brain during systemic inflammation. Nat. Med. 1996;2:581–584. doi: 10.1038/nm0596-581. [DOI] [PubMed] [Google Scholar]
- Wright J.W., Harding J.W. Contributions of matrix metalloproteinases to neural plasticity, habituation, associative learning and drug addiction. Neural Plast. 2009;2009:579382. doi: 10.1155/2009/579382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu F., Catano M., Echeverry R., Torre E., Haile W.B., An J., Chen C., Cheng L., Nicholson A., Tong F.C., Park J., Yepes M. Urokinase-type plasminogen activator promotes dendritic spine recovery and improves neurological outcome following ischemic stroke. J. Neurosci. 2014;34:14219–14232. doi: 10.1523/JNEUROSCI.5309-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L., Kang H., Xu Q., Chen M.J., Liao Y., Thiyagarajan M., O'Donnell J., Christensen D.J., Nicholson C., Iliff J.J., Takano T., Deane R., Nedergaard M. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., He D., Bai Y. Microglia-mediated inflammation and neurodegenerative disease. Mol. Neurobiol. 2016;53:6709–6715. doi: 10.1007/s12035-015-9593-4. [DOI] [PubMed] [Google Scholar]
- Yamada S., Takayama Y., Okada M., Nagai K. Effect of continuous infusion of anti-L1 antibody into the third cerebral ventricle above the suprachiasmatic nucleus on the circadian rhythm of locomotor activity in rats. Biol. Rhythm. Res. 1999;30:573–582. [Google Scholar]
- Yamada S., Takayama Y., Seki T., Okada M., Nagai K. Changes in L1 and NCAM expression in the rat suprachiasmatic nucleus during growth and after orbital enucleation. Dev. Brain Res. 2003;143:189–198. doi: 10.1016/s0165-3806(03)00131-7. [DOI] [PubMed] [Google Scholar]
- Yang Y., Hill J.W., Rosenberg G.A. Multiple roles of metalloproteinases in neurological disorders. Prog. Mol. Biol. 2011;99:241–263. doi: 10.1016/B978-0-12-385504-6.00006-3. [DOI] [PubMed] [Google Scholar]
- Yu X., Franks N.P., Wisden W. Sleep and sedative states induced by targeting the histamine and noradrenergic systems. Front. Neural Circ. 2018;12:4. doi: 10.3389/fncir.2018.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X., Zecharia A., Zhang Z., Yang Q., Yustos R., Jager P., Vyssotski A.L., Maywood E.S., Chesham J.E., Ma Y., Brickley S.G., Hastings M.H., Franks N.P., Wisden W. Circadian factor BMAL1 in histaminergic neurons regulates sleep architecture. Curr. Biol. 2014;24:2838–2844. doi: 10.1016/j.cub.2014.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan H., Vance K.M., Junge C.E., Geballe M.T., Snyder J.P., Hepler J.R., Yepes M., Low C.-M., Traynelis S.F. The serine protease plasmin cleaves the amino-terminal domain of the NR2A subunit to relieve zinc inhibition of the N-methyl-D-aspartate receptors. J. Biol. Chem. 2009;284:12862–12873. doi: 10.1074/jbc.M805123200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhu X., Huang C., Zhang X. Molecular changes in he medial prefrontal cortex and nucleus accumbens are associated with blocking the behavioral sensitization to cocaine. Sci. Rep. 2015;5:16172. doi: 10.1038/srep16172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuo M., Holtzman D.M., Li Y., Osaka H., DeMaro J., Jacquin M., Bu G. Role of tissue plasminogen activator receptor LRP in hippocampal long-term potentiation. J. Neurosci. 2000;20:542–549. doi: 10.1523/JNEUROSCI.20-02-00542.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski M.R., Krueger J.M. Sleep and innate immunity. Front. Biosci. 2011;3:632–642. doi: 10.2741/s176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski M.R., Ping T.S., Clinton J.M., Krueger J.M. Ectonucleotidase-knockout mice lack non-REM sleep responses to sleep deprivation. Eur. J. Neurosci. 2012;35:1789–1798. doi: 10.1111/j.1460-9568.2012.08112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]