Abstract
The Dresden Study on Parenting, Work, and Mental Health (“DResdner Studie zu Elternschaft, Arbeit, und Mentaler Gesundheit”, DREAM) aims to prospectively investigate the relationship between parental work participation, role distribution, stress factors, and their effects on perinatal outcomes and long-term family mental and somatic health in a community sample targeting N = 4,000 individuals, i.e., 2,000 couples, expecting a child and residing in Dresden, Germany (interim sample of N = 1,410 participants, recruitment ongoing). Various questionnaires are completed at four measurement points from pregnancy to 2 years postpartum (prolongation into middle childhood planned). Applying a multi-method approach, long-term endocrinological data (analyses of hair cortisol concentrations and other endogenous hormones, “DREAMHAIR”) and qualitative interview data (regarding gender role attitudes and distribution of domestic work, child care, and paid employment; “DREAMTALK”) are obtained. In this study protocol, the theoretical background, methods, and preliminary results considering sociodemographic characteristics during pregnancy and birth-related factors at 8 weeks postpartum are presented. Additionally, there is a focus on our endocrinological sub-study DREAMHAIR. In this sub-study currently comprising N = 152 participants, i.e., 88 families (recruitment ongoing), we want to gain knowledge on the transgenerational processes of stress regulation and psychopathology in the whole family by analyzing hair cortisol concentrations in both parents and children during the course from pregnancy (or after birth regarding children) to at least 2 years postpartum. By comparing data of the community sample to a clinical sample of mothers with postpartum mental disorders, their children, and their partners during the period between admission and discharge from a mother-baby unit and post-treatment (“DREAMMBU”), the course of mothers' psychopathology, parent-infant interaction, and infant regulation disorders with special regard to long-term endocrine correlates will be examined. With previous studies neglecting the fathers or partners involved, a major advantage of DREAM is the use of a multi-method and multi-level approach by examining the whole family in a longitudinal design. Therefore, the DREAM study will contribute to a better understanding of the role of social, work, and stress factors for mental and somatic health and its long-term endocrine correlates in the natural course of becoming a family.
Keywords: parental mental health, work participation, role distribution, peripartum stress, DREAM study, hair cortisol, multi-method approach, study protocol
Introduction
Expecting a child marks a transition involving several physiological, psychological, and structural changes for the individual as well as for the couple. The majority of German women reduces its work participation after giving birth to a child and continues staying at home after paid parental leave runs out 12 months postpartum (or after the stretched out parental leave ends 2 years postpartum for families who worked part-time for a while); and of those women who do return to their jobs, the majority only works part-time (Bundesministerium für Familie Senioren Frauen und Jugend, 2017a). German mothers are eligible to split the parental leave with the father and if the fathers take at least two so-called “fathers' months” of paid leave, the parental allowance is extended to 14 months in total. Although the amount of fathers taking paternal leave is increasing (with roughly one third taking the “fathers' months”), men usually stay at home for a shorter period compared to women and continue working the same amount of time afterwards (Bundesministerium für Familie Senioren Frauen und Jugend, 2017a). This imbalance is aggravated by several cultural reasons (e.g., when it is appropriate to work again and concerning distribution of labor between sexes) and structural reasons like the tax system (i.e., the German tax system penalizes married couples economically when both partners share domestic work, child care, and paid employment equally, leading to a polarization of working time), a cash-for-care benefit (“Betreuungsgeld”; which subsidies parents (mostly women) staying at home with their children until they turn 3 years old), and an insufficient access to day care. Short- and long-term consequences of mothers' longer parental leave and not being employed refer to an unbalanced distribution of domestic work and child care (Buehler and O'Brien, 2011; Schober and Zoch, 2015), unequal wages after re-entry in the labor market (Davies and Pierre, 2005; Bryan and Sevilla-Sanz, 2010), and a delay in their professional career which may result in an increasing dependency on the partner and consolidate a gender gap interfering with gender equality (Barker and Pawlak, 2011; Miani and Hoorens, 2014).
Beyond equality considerations, the impact of paid employment on health has to be considered. In this context two contrary hypotheses have been suggested: the role strain or scarcity hypothesis postulates that additional roles like being a working woman impair maternal health due to additional daily hassles and demands (Goode, 1960). Thus, it may be more challenging to care for oneself and for a child and meet its needs. In contrast, the role enhancement hypothesis suggests that women with several roles are healthier because of positive stimulating input in their professional life and better access to resources that help in dealing with these demands (Sieber, 1974; Marks, 1977). As a consequence, the mother may have more energy to dedicate herself to family life in her spare time. In accordance with the latter, there is recent evidence that maternal work participation may have a positive influence on mental and somatic health (Klumb and Lampert, 2004; Buehler and O'Brien, 2011; Frech and Damaske, 2012; Cruise et al., 2018). Nevertheless, further results suggest a negative (in line with the scarcity hypothesis) or missing association between maternal work participation and the mother's mental and somatic health (Schwab-Reese et al., 2017; Liu et al., 2018). Consistent with findings on negative associations, women have been found to have a greater risk for suffering from work-privacy conflict than men probably due to multiple private and occupational burdens (Garthus-Niegel et al., 2016). Thus, it may be hard to put compatibility of work and family into practice. In sum, the potential etiologic role of employment on health warrants further investigation. Indeed, as the above mentioned evidence mainly comes from cross-sectional studies conducted in the United States, it remains unclear whether the previous research results are applicable to working women and families in Europe or even Germany, where maternal work participation is comparatively low. Moreover, previous evidence also neglected the role of important confounding or moderating factors, e.g., precarious working conditions and psychosocial work stress (Klumb and Lampert, 2004; Buehler and O'Brien, 2011), despite of recent evidence indicating their negative impact on parents' mental and somatic health (Caparros-Gonzalez et al., 2017; Philpott et al., 2017).
Chronic effects of stress on mental and somatic health, e.g., caused by precarious working conditions or psychosocial work stress, have been closely linked to the activity of the body's stress response systems, particularly the hypothalamic-pituitary-adrenal (HPA) axis leading to the secretion of cortisol (Chrousos, 2009). Studies investigating the relationship between work participation or precarious working conditions and cortisol are predominantly based on traditional cortisol measures. For example, unemployment has been found to be linked with alteration of diurnal or overall cortisol secretion, e.g., in blood (e.g., Arnetz et al., 1991; Maier et al., 2006) or saliva (e.g., Grossi et al., 2001; Gallagher et al., 2016). The direction of findings is characterized by some inconsistency (review: Sumner and Gallagher, 2017), e.g., with some studies indicating elevated (e.g., Arnetz et al., 1991) or lowered (e.g., Gallagher et al., 2016) overall cortisol levels in unemployed people compared to employed people, while some studies failed to show such a difference (e.g., Ockenfels et al., 1995). Regarding the relations between psychosocial work stress on the activity of the HPA axis, study results support the relevance of endocrine correlates as a mediator of the impact of work stress on health although findings are characterized by a notable heterogeneity (review: Siegrist and Li, 2017). Part of the reason for mixed results may be due to limitations in the assessment of long-term cortisol secretion. Specifically, previous cortisol assessment methods particularly reflect short-term secretory activity over periods ranging from minutes (saliva, plasma) to hours (urine; Stalder et al., 2017). Given that acute cortisol secretion is highly volatile and affected by a range of situational factors (Stalder and Kirschbaum, 2012), these methods provide rather unreliable estimates of long-term cortisol output. The analysis of hair cortisol concentrations (HCC) constitutes a relatively recent tool that may increase the quality of the assessments of long-term cumulative cortisol levels in such research. Through an incorporation of lipophilic substances into the slowly growing hair matrix, HCC are supposed to be a non-invasive and easily obtainable retrospective marker of cortisol levels integrated over the previous months (reviews: Stalder and Kirschbaum, 2012; Stalder et al., 2017). Further advantages of hair cortisol analysis include the robustness to acute situational influences and the independency from non-compliance issues (Russell et al., 2012; Stalder and Kirschbaum, 2012; Stalder et al., 2017). Over the past years, considerable evidence has emerged in support of the general validity and reliability of hair cortisol analysis (review: Stalder and Kirschbaum, 2012). Specifically, recent studies have shown positive associations between HCC and cumulative cortisol data from repeated assessments using traditional cortisol measures (Sauvé et al., 2007; D'Anna-Hernandez et al., 2011; van Holland et al., 2012; Short et al., 2016). Further indirect support stems from research that found a correspondence of HCC data and the expected secretory pattern in conditions with well-known endocrine alterations (review: Stalder et al., 2017). For example, the well-known pattern of increasing cortisol levels over the course of pregnancy was confirmed by HCC data (Kirschbaum et al., 2009; D'Anna-Hernandez et al., 2011; Karlén et al., 2013; Hoffman et al., 2016).
However, evidence for HCC in relation to work participation and precarious working conditions remains rare and inconsistent. Some studies indicate links between HCC and unemployment (Dettenborn et al., 2010), job insecurity (Herr et al., 2017), and shift work (Manenschijn et al., 2011). Other studies have come to opposite findings underlining the need of further investigations on larger samples taking into account moderating and mediating factors within a longitudinal design (Janssens et al., 2017; van der Meij et al., 2018). Furthermore, HCC were found to serve as a marker of stress in several contexts, e.g., stress-related somatic conditions (Pereg et al., 2011; Manenschijn et al., 2013; Stalder et al., 2013; Kuehl et al., 2015) and mental disorders (review: Staufenbiel et al., 2013; Wester and van Rossum, 2015; Stalder et al., 2017; Steudte-Schmiedgen et al., 2017). Evidence suggests that HCC sensitively reflect clinical and/or stress-related conditions. For example, higher HCC were detected in patients with major depression (Dettenborn et al., 2012; Hinkelmann et al., 2013; Wei et al., 2015) and late-onset bipolar disorder (Manenschijn et al., 2012) while attenuation was seen in generalized anxiety disorder (Steudte et al., 2011) or posttraumatic stress disorder characterized by a long-term time-interval since traumatization (Steudte et al., 2013). Still, meta-analytic data revealed no consistent relationships with questionnaire-based measures of perceived stress or clinical symptoms (Stalder et al., 2017). This seems also to be evident among pregnant women, i.e., HCC were not consistently found to be related to prenatal psychological distress (review: Mustonen et al., 2018). Interestingly, Bowers et al. (2018) found an association between self-reports of distress and HCC during pregnancy only in women who experienced high levels of childhood adversity compared to women without such experiences. This supports the notion that early adversity contributes to the long-term activity of the HPA axis. Here, a longitudinal investigation of HCC over an extended period of time is warranted. However, the fact that HCC were more frequently related to the number of self-reported stressful or negative life events (Karlén et al., 2011, 2015; Grassi-Oliveira et al., 2012; Staufenbiel et al., 2014; Steudte-Schmiedgen et al., 2015) or traumatic events across the lifespan (Steudte et al., 2013; Steudte-Schmiedgen et al., 2016) suggests that stronger psychoendocrine correspondence may be achieved by using stress measures based on objectives criteria.
So far, only implications for the mother's health herself have been considered in this paper. More importantly, stress factors, e.g., precarious working conditions and psychosocial work stress, may not only be essential for the health of the mother herself, but also play a major role for the entire family and especially for development and health of the offspring (Lucas-Thompson et al., 2010; Jaursch and Lösel, 2011). In fact, the early environment is fundamental for long-term mental and somatic health of a child (Van den Bergh et al., 2017). Child outcomes have been found to be negatively affected by maternal mental disorders (Pearson et al., 2013; Gentile, 2017) and self-reported stress (Wadhwa et al., 2011; Van den Bergh et al., 2017) during pregnancy.
Long-term effects of maternal adversity on the offspring are referred to as fetal programming with a transgenerational transmission of alterations of the long-term activity of the HPA (Räikkönen et al., 2011; Beijers et al., 2014). Thus, cortisol has been considered as an important mediator of the effects of maternal stress on the developing brain of the fetus (review: Entringer et al., 2015). Specifically, this effect is assumed to be regulated by the placental enzyme 11 beta-hydroxysteroid dehydrogenase type 2 (11beta-HSD2) which converts cortisol in its inactive form cortisone (Beitins et al., 1973; Brown et al., 1996). Importantly, some proportion of active maternal cortisol passes through the placenta into the fetal compartment. In line with this assumption, adverse intrauterine conditions such as maternal anxiety (O'Donnell et al., 2012), severe infection (Johnstone et al., 2005), or alcohol exposure (Liang et al., 2011) have been found to co-occur with a down-regulation of placental 11beta-HSD2 activity. Another mechanism that may regulate the fetal programming effects of elevations in maternal cortisol is increased production of placental corticotrophin-releasing hormone (CRH), which, in turn, may affect the fetal HPA axis and the biosynthesis of adrenal steroids (review: Entringer et al., 2015).
Previous evidence found several parental risk factors that may affect long-term regulation of the body's stress response systems in the offspring, e.g., low socioeconomic status (Essex et al., 2002; Evans and Kim, 2007) or maternal psychopathology (Gentile, 2017). Specifically, changes in maternal cortisol regulation due to (traumatic) stress, anxiety, or depressiveness have been shown to result in altered fetal cortisol levels as measured in saliva (Yehuda et al., 2005; Brennan et al., 2008; Grant et al., 2009; Davis et al., 2011) and urine (Yehuda et al., 2002; Diego et al., 2004). However, the reported relationships between various measures of prenatal maternal stress and offspring cortisol are complex and heterogeneous (Van den Bergh et al., 2017) which may be partly the result of the use of short-term cortisol measures as mentioned earlier. Recently, research using HCC analysis among newborns is emerging (e.g., Yamada et al., 2007; Hoffman et al., 2017) highlighting the unique potential of neonatal HCC to reflect intrauterine glucocorticoid regulation. Specifically, it has been shown that cortisol levels of neonatal hair which was taken at birth mainly reflect the third trimester increase of maternal cortisol (Hollanders et al., 2017).
Studies examining HCC in infants found associations to maternal HCC during pregnancy, supporting the notion of a transgenerational transmission of alterations of the long-term activity of the HPA axis (Karlén et al., 2013; Romero-Gonzalez et al., 2018). As mentioned above, recent studies found close links between trauma exposure across the lifespan and long-term regulation of HPA axis activity (Steudte-Schmiedgen et al., 2016; Pervanidou et al., 2017). Interestingly, initial cross-sectional HCC research supports the notion of a relationship between lifetime trauma exposure, childhood abuse, and HCC during pregnancy (Schreier et al., 2015, 2016; Swales et al., 2018). A prospective study further confirmed associations between maternal lifetime trauma history, HCC reflecting the third trimester of pregnancy, and subsequent infant negative affectivity at the age of 6 month (Bosquet Enlow et al., 2017). This is commensurate with study data observing an association between maternal lifetime trauma exposure and increased HCC in older children (i.e., at the age of three and four), albeit this relationship was not found in infants under the age of two (Slopen et al., 2018). These promising findings are in line with the assumption of an intergenerational transmission of maternal childhood maltreatment and necessitate further prospective investigations (Buss et al., 2017).
Not only intrauterine but also postpartum factors can affect long-term activity of the HPA axis of children as measured by HCC analysis. Research about the role of parent-infant interaction is slowly emerging. For example, a study found that mothers with increased HCC were more intrusive and showed lower positive engagement synchrony with their offspring 6 months after delivery (Tarullo et al., 2017). This corresponds with a study showing an association between mother's parenting stress and depressiveness at 4 weeks postpartum and higher HCC in their infants at the age of one, which, in turn, were related to pronounced socioemotional problems (Palmer et al., 2013). Thus, both intrauterine and postpartum influences on the infant HPA axis can manifest in infant health and behavior, e.g., a difficult temperament or regulatory problems that can precede later psychopathology and impair further development of the child (Gunnar and Donzella, 2002; Hemmi et al., 2011; Davis and Sandman, 2012; Stein et al., 2014; Petzoldt et al., 2016). Still, evidence regarding the relations between maternal self-reported distress, activity of the HPA axis, and infant outcomes is rare, inconsistent, and mainly stems from studies assessing short-term cortisol (e.g., in saliva: Bosquet Enlow et al., 2017; Van den Bergh et al., 2017). Hence, there is need of further investigations to detect how maternal HCC are reflected in long-term changes of health and behavior problems and possibly underlying biological stress reactions of the child indicated by neonatal HCC.
Moreover, it is of significance whether psychological intervention can support a normalization of HPA axis dysregulation in both mother and child. Over the past years, evidence emerged supporting the notion that effective psychotherapy may improve this kind of dysregulations in patients suffering from posttraumatic stress disorder. Specifically, cortisol levels were found to increase in responders to psychotherapy while those of non-responders decreased (Olff et al., 2007; Yehuda et al., 2009, 2014), albeit with some inconsistency in findings (review and meta-analysis: Gerardi et al., 2010; Pacella et al., 2014; Schumacher et al., 2018). Further, evidence has accumulated in support of the potential of pre-treatment hormone concentrations as predictors of successful psychotherapeutic outcome in patients with posttraumatic stress disorder (review: Colvonen et al., 2017) and patients with affective and/or anxiety disorders (Fischer et al., 2018). Regarding postpartum mental disorders, treatments combining psychological, psychopharmacological, and interactional components in a mother-baby unit (MBU) are found to contribute to lower psychopathology (review: Connellan et al., 2017). So far, no study has investigated the role of long-term endocrine correlates as predictor and correlate of successful clinical outcome of such a treatment among mothers and their infants. If there are alterations of the long-term activity of the HPA axis going along with the therapy, considering the linkage between maternal and infant HPA axis, it can be reasonably assumed that not only maternal health but also infant health and behavior and its endocrine correlates may improve within treatment of postpartum mental disorders.
As mentioned above, the involvement of fathers with their children is slowly increasing (Barker and Pawlak, 2011; Bundesministerium für Familie Senioren Frauen und Jugend, 2017a). Still, the role of fathers and partners related to the mother has been widely neglected in previous studies. In particular, there is a lack of evidence with regard to the mechanisms through which the partner may have an impact on the child (Barker et al., 2017). Emerging research suggests that, in accordance to the evidence regarding mothers, early father-infant-interaction and parenting affect child development and behavior (Ramchandani et al., 2013; Parfitt et al., 2014). Consistent with this, psychopathology of the father has detrimental effects on parenting (review: Wilson and Durbin, 2010) and (maybe in turn) on child outcomes (Ramchandani et al., 2005; Sweeney and MacBeth, 2016). Regarding endocrinological aspects, recent studies indicate that couples' mental health and physiological states (especially cortisol) are associated with one another, which is assumed to have implications for health and functioning as a couple, e.g., role distribution or partnership satisfaction (Timmons et al., 2015), which, in turn, may have a direct or indirect impact on child outcomes (Hanington et al., 2012; Parfitt et al., 2014).
In conclusion, the impact of long-term effects of stress, e.g., caused by precarious working conditions or psychosocial work stress, on mental and somatic health of the whole family warrants more research. In particular, previous studies were limited to self-reported measures or short-term cortisol assessment methods (e.g., saliva or urine). Consequently, more detailed information about the HPA axis linkage between parents and in parent-child dyads is needed to examine the pathways of transgenerational transmission of long-term regulation of the HPA axis and possible approaches for intervention.
To close this gap, the current cohort study called Dresden Study on Parenting, Work, and Mental Health (DREAM; “DResdner Studie zu Elternschaft, Arbeit und Mentaler Gesundheit”) together with its sub-studies DREAMHAIR and DREAMTALK combining quantitative questionnaires, qualitative interviews, and long-term endocrine correlates aims to examine the impact of parental work participation, role distributions, and stress factors on family health longitudinally, i.e., during the course from late pregnancy to 2 years postpartum.
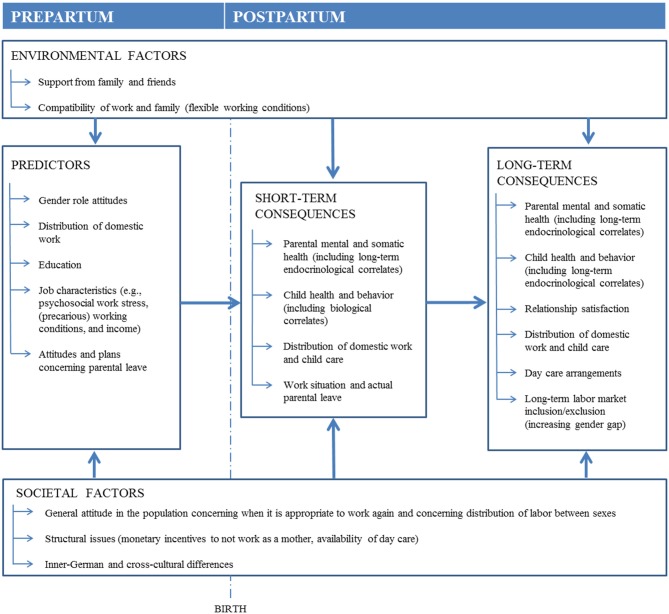
Based on the theoretical model shown in Figure 1, the following main questions will be investigated:
Figure 1.
Simplified theoretical model upon which the DREAM study is based.
How do mothers' and their partners' work participation and role distribution regarding domestic work, child care, and paid employment change in the course from pregnancy to 2 years postpartum; in particular, will there be a shift toward more traditional gender roles (DREAM and DREAMTALK)?
How are mothers' and their partners' mental and somatic health as well as child health and behavior influenced by their work participation over time and is a potential association influenced by confounding or moderating factors such as precarious working conditions and psychosocial work stress (DREAM and DREAMTALK)?
How does mothers' and their partners' mental health affect child health and behavior cross-sectionally and longitudinally (DREAM)?
How are HCC inter-related between the family members (mother, father, index child) cross-sectionally and longitudinally (DREAMHAIR)?
Are HCC predicted by stress factors (including precarious working conditions and psychosocial work stress)? How do HCC relate to mental health and behavioral outcomes of each family member cross-sectionally and longitudinally (DREAMHAIR)?
Regarding a clinical sample, are maternal mental disorders and long-term HCC of mothers (and partners if available) at admission to the MBU associated with behavioral outcomes and HCC of the child and how does this change during the course of psychotherapeutic treatment (DREAMMBU)?
With its multi-method approach addressing both parents and child, this study is unique in the research on the interplay of work participation, role distribution, and stress factors and its impact on perinatal outcome and mental and somatic health of the whole family. Considering the complex relationships between prenatal and postnatal psychological distress and long-term cortisol secretion in parents and their offspring, this study will make a significant contribution to the existing literature.
Methods and analyses
Overall Design and Procedure
The DREAM study is a prospective cohort study targeting a total community sample of N = 4,000 individuals, i.e., 2,000 couples, expecting a child in and around Dresden, Germany. Inclusion criteria are a current pregnancy, being a resident in the mentioned area, and sufficient German skills to complete the study questionnaires. In order to get a comprehensive picture of (becoming) parents in the area, there was no exclusion of comparatively rare groups, e.g., multiple pregnancies, couples of the same sex, and single persons. Since June 2017, pregnant women [subsequently referred to as (expectant) mothers], and the male or female partners they are currently involved with in a long-term relationship are recruited during pregnancy mainly in obstetrical clinics and midwife practices, with an interim sample of N = 1,410 participants who have completed the first questionnaire (T1) by the end of September 2018 (recruitment ongoing). The DREAM study has been approved by the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden (No: EK 278062015).
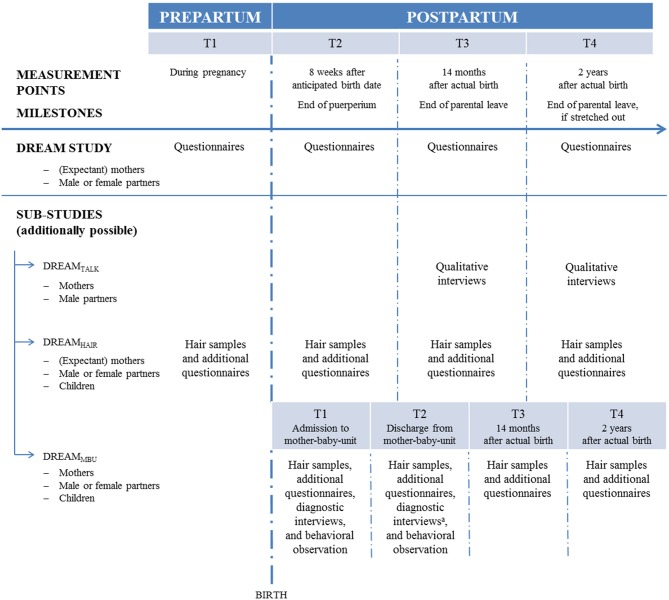
Following milestones for young German families, in the basic DREAM study there are four measurement points (Figure 2) starting with T1 during pregnancy and three postpartum assessment waves, i.e., T2 at 8 weeks after the anticipated birth date when puerperium is over, T3 at 14 months, and T4 at 2 years after the actual birth date. T3 and T4 go along with German parental allowance because T3 is at the time the parental allowance is over (if the couple took the full allowance and both parents were on parental leave for at least 2 months) and T4 is at the time the stretched out parental allowance (for families who worked part-time for a while) ends. A prolonged investigation of families into middle childhood is planned. The DREAM study is conducted in a larger city in East Germany where both maternal work participation and day care are a more frequent practice than in West Germany (Bundesministerium für Familie Senioren Frauen und Jugend, 2017a). Therefore, the DREAM study cooperates with a West German study called the Bremen Initiative to Foster Early Childhood Development (“BRISE”; Bremer Initiative zur Stärkung frühkindlicher Entwicklung). Moreover, data of the DREAM study will be compared to data of the Norwegian Akershus Birth Cohort (ABC study). This cross-cultural comparison to a country that is more progressive regarding gender considerations (Barker and Pawlak, 2011) will complement the results about the role of work participation for family health. For this purpose, measurement points and many instruments are matched.
Figure 2.
Assessment waves of the DREAM study and its sub-studies DREAMTALK (qualitative interview sub-study), DREAMHAIR (long-term endocrinological sub-study), DREAMMBU (clinical sub-study). Regarding the community sample, T1 during pregnancy, T2 8 weeks after anticipated birth date, T3 14 months, and T4 2 years after actual birth date (prolongation into middle childhood planned). Regarding the clinical sample, T1 at admission and T2 at discharge (hair samples will be taken 2 months after discharge) from mother-baby-unit, T3 14 months (will only be omitted if the sampling point at discharge from mother-baby-unit is not too close, i.e., 14 months postpartum ± 2 months), T4 at 2 years after actual birth date. aAt discharge, diagnostic interviews will only be omitted regarding children.
Applying a multi-method approach, the DREAM study is complemented by two sub-studies: DREAMHAIR (analysis of HCC and other endogenous steroid hormones) and DREAMTALK (qualitative interviews regarding gender role values and distribution of domestic work, child care, and paid employment). Participants meeting inclusion criteria for the particular sub-study are contacted again to be invited to participate in the sub-study. Due to the focus of this paper, the basic DREAM study and the sub-study DREAMHAIR are presented in detail.
Sub-studies
DREAMHAIR and DREAMMBU
The long-term endocrinological sub-study DREAMHAIR aims to examine the complex relationships between psychological distress and long-term steroid hormone levels in parent-child dyads from pregnancy to 2 years postpartum (prolongation into middle childhood planned). This sub-study consists of two branches: a community based approach (DREAMHAIR, already started) and a clinical approach (DREAMMBU, starting soon). Within the community branch, the community sample stems from the basic DREAM study. Within the clinical branch, a clinical sample of mothers with postpartum mental disorders, their partners (if available), and their children are recruited from a mother-baby day clinic. Data of the community and clinical sample will be combined for long-term analyses.
Recruitment for the community branch of the sub-study DREAMHAIR began 5 months after the start of the basic DREAM study. For this sub-study, all families whose expected delivery date is at least 4 weeks in the future are checked for inclusion criteria. Inclusion criteria for parents comprise a minimal hair length of 2 cm, no hair loss or baldness, no severe physical disease (e.g., cancer or adrenocortical dysfunction) over the last 5 years, and no use of glucocorticoid containing medication for the last 4 months. Regarding children, there are no particular reasons for exclusion other than no availability of hair (without a minimal hair length). Potentially confounding variables (e.g., medication, diseases) are assessed and used for further analyses. Inclusion criteria will be checked at every measurement point. If participants are excluded at a single measurement point due to temporary reasons, e.g., medication or too short hair, or they miss an assessment wave due to organizational reasons, they will be asked again at the next measurement point. Participants can join this sub-study as a couple or alone as long as each parent who has child custody provides her/his consent that child hair is also allowed to be taken.
After being enrolled into the basic DREAM study, hair samples of the eligible expectant mothers, their partners (i.e., N = 152 participants, i.e., 88 families, at T1 by the end of September 2018) and their children, are examined for HCC and other endogenous steroid hormones at four measurement points from pregnancy up to 2 years postpartum (Figure 2; prolongation into middle childhood planned). Regarding the parents, T1DREAMHAIR starts 4 to 6 weeks prior to the anticipated birth date which reflects HCC integrated during late pregnancy. Regarding the children, T1DREAMHAIR hair samples are taken soon after birth to gain information on intrauterine glucocorticoid regulation (Hollanders et al., 2017). The other measurement points (T2DREAMHAIR, T3DREAMHAIR, and T4DREAMHAIR) are equivalent to the basic DREAM study.
At the respective first measurement point, hair samples of community sample will be taken at their home or at the lab as preferred by the participants while hair samples of the clinical sample will be taken at the lab in any case. In both samples, the first hair sample is taken by trained staff. In order to self-administer hair samples at the follow-ups, participants get a video teaching how to take own and child hair samples themselves or with help of their partner or a friend. At the follow-ups, participants get a reminder when the next hair samples are due. As we are aware that this sub-study requires some more commitment by the participants compared to the basic questionnaire study, we put emphasis on personal contact to the participants. For instance, trained staff assists them with taking own or child hair sample if needed.
For the clinical branch (DREAMMBU), recruitment of a clinical sample of approximately N = 70 mothers with postpartum mental disorders who are treated in the day-care MBU at the Institute and Outpatient Clinics of Psychotherapy and Psychosomatic Medicine at the Technische Universität Dresden is planned starting by the year 2019 (DREAMMBU). In this MBU, mothers with severe postpartum mental disorders (e.g., depressive disorders, anxiety disorders, obsessive-compulsive disorders, and personality disorders) are treated together with their child (0–12 months old, mean child age at admission is 23.3 weeks (SD = 13.1) for averagely 8.5 weeks (SD = 3.1). Based on a treatment concept that is state of the art for postpartum mental disorders (Wortmann-Fleischer et al., 2012), patients get a treatment consisting of both mother focused (e.g., disorder specific psychotherapy, psychopharmacotherapy) and mother-infant-interaction focused components (e.g., mother group treatment, video-interaction-therapy, baby massage and handling, sensitivity training) conducted by a multi-professional team. Partners and other family members are involved in the treatment if possible.
For the clinical sub-study DREAMMBU, patients will be asked for written informed consent to take part in the study within the first week after admission. Their children and (if available) partners will also be included. As shown in Figure 2, hair samples of all participants will be taken four times: once at admission (T1DREAMMBU) to measure the steroid exposition during the 2 months prior to treatment and a second time (T2DREAMMBU) 2 months after discharge from MBU to assess HCC during the 2 months after treatment. Further, to compare the data of the clinical sample to the data of the community sample at T3DREAMHAIR and T4DREAMHAIR (14 and 24 months postpartum), a third (T3DREAMMBU), and fourth (T4DREAMMBU) hair sample of the clinical population will be taken [if the sampling point at discharge (T2DREAMMBU) is very close to T3DREAMHAIR (14 ± 2 months), one sampling point will be omitted].
In the clinical part of the sub-study DREAMMBU, patients and their partners will also go through the routine assessment of the treatment effects (Table 1) using a comprehensive assessment battery at admission and discharge. At admission, patients will be interviewed using the Structured Clinical Interview for DSM-IV (SCID I and SCID II; Wittchen et al., 1997). Both at admission and discharge, the Diagnostic Interview for Mental Disorders in Babies showing good to very good inter-rater reliability (Baby-DIPS; Popp et al., 2016), a semi-standardized observation of maternal sensitivity toward their baby's signals (Galeris, 2016; validation pending), and additional questionnaires regarding the maternal psychopathology and parenting as well as infant temperament, regulation disorders, and behavior will be obtained. There is an overlap between the MBU assessment and the basic DREAM assessment regarding all relevant measures.
Table 1.
Constructs and instruments in the basic DREAM study.
| Community sample (DREAM) | Clinical sample (DREAMMBU) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Constructs | Instruments | T1 | T2 | T3 | T4 | T1 | T2 | T3 | T4 |
| SOCIODEMOGRAPHIC AND SOCIOECONOMIC FACTORS | |||||||||
| Nationality and mother tongue | Questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | ||||||
| Education | Questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | ||||||
| Marital status | Questions derived from the Socio-Economic Panel (SOEP; TNS Infratest Sozialforschung, 2016) and self-generated questions | x | x | x | x | x | x | x | x |
| Children and former pregnancies | Questions derived from the BRISE study based on the BabyCare Project (Friese and Kirschner, 2003) | x | x | x | x | ||||
| Housing | Questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | x | x | x | x | x | x |
| WORK-RELATED FACTORS | |||||||||
| Working hours and professional group | Questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | x | x | x | x | x | |
| Job satisfaction and job burden | Questions derived from the BRISE study based on the BabyCare Project (Friese and Kirschner, 2003) and the Exploration Questionnaire for Identification of Differential Learning Paths in the Social Development in Toddler Age (“Explorationsfragebogen zur Identifikation differentieller Lernwege in den ersten beiden Lebensjahren”, IDL 0-2; Petermann et al., 2002) | x | x | x | x | x | x | x | |
| Sick leave and adaption of work situation in pregnancy | Questions derived from the ABC study (e.g., Dørheim et al., 2013) | x | x | x | x | x | x | x | |
| Shift work | Questions derived from the BRISE study based on the BabyCare Project (Friese and Kirschner, 2003) | x | x | x | |||||
| Precariousness | Employment Precariousness Scale–Revised (EPRES; Vives et al., 2015) | x | x | x | |||||
| Psychosocial work stress | Effort-Reward Imbalance Questionnaire (ERI; Siegrist, 1996; Rödel et al., 2004) | x | x | x | |||||
| Work-privacy conflict | One scale (work-privacy conflict) of the Copenhagen Psychosocial Questionnaire (COPSOQ; Kristensen et al., 2005; Nübling et al., 2005) | x | x | x | |||||
| Plans and actual parental leave | Self-generated questions | x | x | x | x | x | x | x | x |
| Satisfaction with distribution of parental leave | Self-generated questions | x | x | x | x | ||||
| DISTRIBUTION OF DOMESTIC WORK AND CHILD CARE | |||||||||
| Attitudes toward distribution of domestic work | Nine scales (effective communication about domestic labor, ministering to family needs, support of wage work, responsive to personal needs, avoiding conflict, coprovider orientation, valuing homemaking, standards, women's ultimate accountability) of the Orientation Toward Domestic Labor Questionnaire (ODL-Q; Hawkins et al., 1998) | x | x | x | |||||
| Distribution of domestic work and child care | Questions derived from the ABC study | x | x | x | x | ||||
| Time spent for domestic work and child care | Questions derived from the 1997 National Study of the Changing Workforce (Hall and MacDermid, 2009) | x | x | ||||||
| SOMATIC FACTORS | |||||||||
| Current and former somatic health | Questions derived from the ABC study (e.g., Garthus-Niegel et al., 2018; Junge et al., 2018) | x | x | x | x | x | x | x | x |
| Exercise and physical activity | Questions derived from the ABC study generated by health professionals (e.g., Gjestland et al., 2013) | x | x | x | x | x | x | x | |
| Health-related quality of life | Short-Form Health Survey (SF-8; Ware et al., 2001; Ellert et al., 2005) | x | x | ||||||
| Drugs | Questions derived from the ABC study generated by health professionals (e.g., Nordeng et al., 2012) | x | x | x | x | x | x | x | |
| Smoking | Slightly modified questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | x | x | x | x | x | x |
| Alcohol | Questions derived from the German National Cohort (German National Cohort Consortium, 2014) | x | x | x | x | x | x | x | x |
| MENTAL FACTORS | |||||||||
| Current and former mental disorders and treatments | Self-generated questions Structured Clinical Interview for DSM-IV (SCID I and SCID II; Wittchen et al., 1997) |
x | x | x | xx | x | x | x | |
| Use of early help | Self-generated questions | x | x | ||||||
| Symptoms of depression | Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; Bergant et al., 1998) | x | x | x | x | x | x | x | x |
| Psychopathological symptoms | Four scales (somatization, obsessiveness, anxiety and anger/hostility) of the Symptom Check List–Revised (Derogatis, 1977; Franke and Derogatis, 2002) Brief symptom inventory (BSI; Derogatis, 1993; Franke, 2000) |
x | x | x | x | x | x | x | x |
| Current and former critical life events | Questions derived from the BRISE study based on the Avon Longitudinal Study of Parents and Children (ALSPAC; Thomson et al., 2014) | x | x | x | x | x | |||
| Current and former posttraumatic stress reactions | Posttraumatic Diagnostic Scale (PDS; Ehlers et al., 1996; Foa et al., 1997) | xc | xc | xc | x | x | x | x | |
| Adverse childhood experiences | Childhood Trauma Questionnaire (CTQ; Bernstein and Fink, 1998; Wingenfeld et al., 2010) | xc | x | ||||||
| Intradyadic stress and extradyadic stress from daily hassles | Multidimensional Stress Questionnaire for Couples (“Multidimensionaler Stressfragebogen für Paare”, MDSP; Bodenmann, 2007) | x | x | ||||||
| RELATIONSHIP FACTORS | |||||||||
| Relationship satisfaction | Short version of the Partnership Questionnaire (“Kurzform des Partnerschaftsfragebogens,” PFB-K; Kliem et al., 2012) | x | x | x | x | x | x | x | x |
| Social support | Short version of the Social Support Questionnaire (“Fragebogen zur Sozialen Unterstützung,” F-SozU-14; Fydrich et al., 2009) | x | x | x | x | x | x | x | |
| PREGNANCY AND BIRTH-RELATED FACTORS | |||||||||
| Fear of childbirtha | Fear of Birth Scale (FOBS; Haines et al., 2011) | x | |||||||
| General information and complications during pregnancy and birtha | Maternity records (“Mutterpass”; Gemeinsamer Bundesausschuss, 2015), questions derived from the BRISE study, and self-generated questions | x | x | ||||||
| Birth experienceb | Salmon's Item List (SIL; Stadlmayr et al., 2001) | x | x | ||||||
| Overall birth experienceb | Question derived from the ABC study (e.g., Garthus-Niegel et al., 2014) | x | x | ||||||
| Fear for oneself/mother and child during birthb | Self-generated questions based on the ABC study (e.g., Garthus-Niegel et al., 2013) | x | x | ||||||
| Fear of a prospective birthb | Question derived from the ABC study | x | x | ||||||
| Birth-related post-traumatic stress reactions | Impact of Event Scale–Revised (IES-R; Weiss and Marmar, 1996; Maercker and Schützwohl, 1998) | x | x | ||||||
| CHILD-RELATED FACTORS | |||||||||
| Breastfeeding | Self-generated questions based on recommendations of the World Health Organization (World Health Organization, 2009) | x | x | x | x | x | x | x | |
| Parent-to-infant-bonding | Postpartum Bonding Questionnaire (PBQ; Brockington et al., 2001; Reck et al., 2006) | x | x | x | x | x | x | x | |
| Sensitivity toward baby's signals | Semi-standardized observation of maternal sensitivity (global score and six subscales) toward baby's signals (Galeris, 2016) | x | x | ||||||
| Parenting sense of competence | Parenting Sense of Competence Scale (“Fragebogen zum Kompetenzgefühl von Eltern,” FKE; Gibaud-Wattston and Wandersman, 1978, as cited in Johnston and Mash, 1989; Miller, 2001) | x | x | x | x | ||||
| Parenting stress | Parenting Stress Index (“Eltern-Belastungs-Inventar,” EBI; Abidin, 1995; Tröster, 2011) | x | x | x | x | ||||
| Infant regulation disorders | Structured Diagnostic Interview for Regulatory Problems in Infancy (“Diagnostisches Interview bei psychischen Störungen im Säuglings- und Kleinkindalter,” Baby-DIPS; Popp et al., 2016) | x | x | ||||||
| Child health | Medical records (“Kinderuntersuchungsheft”; Gemeinsamer Bundesausschuss, 2016) and questions derived from the ABC study | x | x | x | x | x | x | x | |
| Child development | Five scales (communication, gross motor, fine motor, problem solving, personal-social) of the 14 and 24 month version of the Ages and Stages Questionnaire-3 (ASQ-3; Squires and Bricker, 2009) | x | x | x | x | ||||
| Child temperament | One scale (fussy/difficult scale) of the Infant Characteristics Questionnaire (ICQ; Bates et al., 1979) | x | |||||||
| Infant Behavior Questionnaire (IBQ; Rothbart, 1981; Pauli-Pott et al., 1999) | x | ||||||||
| Child care | Questions derived from the Socio-Economic Panel (SOEP; TNS Infratest Sozialforschung, 2016) | x | x | x | x | x | x | ||
| PERSONALITY | Big Five Inventory–SOEP (BFI-S; Schupp and Gerlitz, 2008) | x | |||||||
| METACOGNITION | Metacognition Questionnaire–Short version (MFK-30; Wells and Cartwright-Hatton, 2004; Arndt et al., 2011) | x | |||||||
Regarding community sample (DREAM), T1 during pregnancy, T2 8 weeks after anticipated birth date, T3 14 months, and T4 2 years after actual birth date (prolongation into middle childhood planned). Regarding clinical sample (DREAMMBU), T1 at admission and T2 at discharge (hair samples will be taken 2 months after discharge) from mother-baby-unit, T3 14 months (will only be omitted if the sampling point at discharge from mother-baby-unit is not too close, i.e., 14 months postpartum ± 2 months), T4 at 2 years after actual birth date.
Only for expectant mothers.
Male and female partners only asked when they have attended birth.
Only for DREAMHAIR.
DREAMTALK
The qualitative DREAMTALK sub-study will start during summer 2019. A subsample targeting approximately N = 40 heterosexual couples, i.e., women and men engaged in a long-term relationship and living in the same household, will be interviewed on their gender role values and attitudes as well as thoughts about distribution of domestic work, child care, and paid employment. These attitudes will be compared to the actual situation. Additionally, both partners' satisfaction regarding their relationship and role distribution as well as how they explain a potential equality gap will be assessed. Results will be analyzed in relation to health-related outcomes measured in the basic DREAM study.
Based on a synthesis of previous studies on different task distributions (Crouter and Manke, 1997; Hall and MacDermid, 2009; Farrokhzad et al., 2010; Helms et al., 2010; Masterson and Hoobler, 2015; Bundesministerium für Familie Senioren Frauen und Jugend, 2017b), couples will be categorized into one of four groups by a cut-off threshold of hours spent on domestic work, child care, and paid employment to compare those groups: progressive couples sharing domestic work, child care, and paid work equally; traditional couples with women doing most of the domestic work and child care and men doing most of the paid work; as well as two interjacent groups.
As shown in Figure 2, qualitative interviews, specifically problem-centered interviews (PCI) following Witzel and Reiter (2012), will be carried out a few weeks after T3 and T4 of the basic DREAM study. This is at the time the regular and the stretched out parental allowance run out. The interviews will be analyzed using qualitative content analysis by Mayring (2010). Categories for the collected interview data will be established, yielding interpretations of the participants' answers in a replicable and systematic way.
Taking into account the participants' wishes, the interviews will take place at the couples' home or at the lab. Trained doctoral students following interview guidelines will conduct them. The project team aims to achieve a personal connection and identification with the study among the participants in order to keep attrition low.
Materials
The DREAM study is characterized by a multi-method approach combining quantitative questionnaires (basic DREAM study), long-term endocrine correlates (DREAMHAIR), and qualitative interviews (DREAMTALK). Study data are collected and managed using Research Electronic Data Capture (REDCap), a secure, web-based application designed to support data capture for research studies, hosted at the “Koordinierungszentrum für Klinische Studien” at the Faculty of Medicine of the Technische Universität Dresden, Germany (Harris et al., 2009). In this article, we focus on the questionnaire data and analysis of HCC.
Questionnaires
The DREAM study comprises several questionnaires as presented in Table 1. Standardized and validated instruments with good psychometric properties were preferably used. For example, the German version of the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; Bergant et al., 1998), a well-established, reliable, and valid instrument was obtained to measure prepartum and postpartum symptoms of depression, while the Effort-Reward Imbalance Questionnaire (ERI; Siegrist, 1996; Rödel et al., 2004) being characterized with satisfactory psychometric characteristics was used to assess psychosocial work stress. Where possible, instruments were chosen in agreement with the BRISE project team, the German National Cohort (German National Cohort Consortium, 2014), or the Norwegian ABC study to allow intra- and intercultural comparisons. If no German version of a questionnaire existed, the English or Norwegian version was translated into German and back-translated by a native speaker (validation still pending).
In the sub-studies, relevant questionnaires were added. In DREAMHAIR, participants complete a self-generated questionnaire about hair-related characteristics, e.g., washes per week, curls, or hair treatments (as described in Stalder et al., 2014). Additionally, hair analyses were complemented by trauma specific questionnaires (Table 1). Specifically, the checklist of the Posttraumatic Diagnostic Scale (PDS; Ehlers et al., 1996; Foa et al., 1997) to assess the nature and presence of the most upsetting traumatic event (A1 and A2 criteria of DSM-IV, time since occurrence) as well as the Childhood Trauma Questionnaire (CTQ; Bernstein and Fink, 1998; Wingenfeld et al., 2010) to measure the severity of childhood maltreatment were added. The German adaptions of both questionnaires have been found to be reliable and valid instruments similar to their English original versions (Griesel et al., 2006;Wingenfeld et al., 2010).
In order to attain best possible response and retention rates, participants can decide whether to complete online or paper-pencil versions of the questionnaires. By the end of September 2018, N = 1,410 participants, i.e., expectant mothers and their partners, have given consent to join the study and completed the first questionnaire which is necessary to take part in the follow-ups. Almost half of them (47.6%; n = 671) decided for the paper-pencil procedure with a somewhat larger ratio of expectant mothers (50.7%; n = 408) compared to their partners (43.5%; n = 259). After completing T1, the participants receive the subsequent questionnaires and reminders in the desired manner automatically, even if they missed one of the measurement points. To keep attrition low, participants get incentives together with the follow-up questionnaires at every measurement point, e.g., rompers, bibs, or books, to encourage them to answer in time. In case of breakup, participants will be contacted separately, so this is no reason to drop out.
Hair Cortisol Concentrations (HCC) Analyses
For analyses of HCC as part of the sub-study DREAMHAIR, a hair strand of a diameter of ~3 mm is taken scalp-near from a posterior vertex position. HCC will be determined in the 2 cm hair segment most proximal to the scalp. If permitted by the individuals' hair length, the next 2 cm of hair will additionally be analyzed. Based on a hair growth rate of ~1 cm/month (Wennig, 2000), these hair segments are assumed to represent integrated, cumulated cortisol levels over the 2 month or, if permitted, 4 month period prior to hair sampling. Hair samples will be stored in aluminum foil and sent to the Institute of Biological Psychology at the Faculty of Psychology of the Technische Universität Dresden. Hair analyses will be conducted following the liquid chromatography-tandem mass spectrometry (LC-MS/MS) protocol which is characterized by very good sensitivity, specificity, and reliability (Gao et al., 2013). Besides cortisol, the LC-MS/MS protocol allows the quantitative analysis of other endogenous steroid hormones, i.e., cortisone, testosterone, progesterone, corticosterone, dehydroepiandrosterone (DHEA), and androstenedione that may serve as important mediators in the development of psychopathology or psychological distress (Gao et al., 2013).
Sample
In this section, the interim samples of the basic DREAM study and the sub-study DREAMHAIR (community branch) by the end of September 2018 will be presented. The participants get no payment for their participation but incentives at every measurement point, e.g., rompers or bibs, as mentioned earlier. Additionally, a lottery is established so two participants may win vouchers and gifts every month.
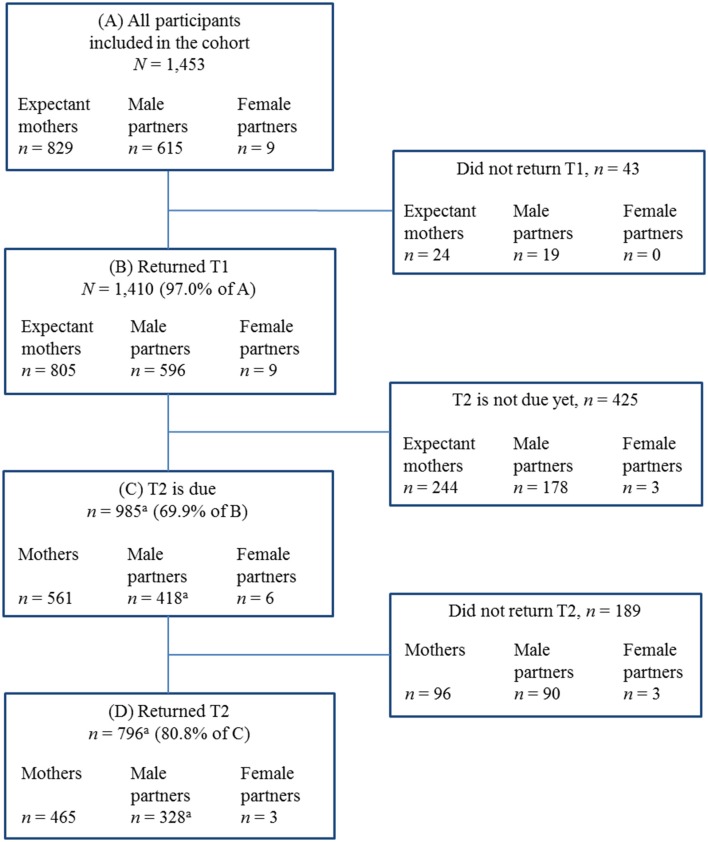
Interim Sample and Flow Chart of DREAM
The DREAM study addresses expectant mothers and their male or female partners in or around Dresden, Germany. The flow chart of the DREAM study is presented in Figure 3.
Figure 3.
Flow chart of the DREAM study. Notes: T1 during pregnancy, T2 8 weeks after anticipated birth date. Data from end of September 2018 (data collection is not finished yet, recruitment ongoing). Further future assessment waves (not due yet): T3 14 months and T4 2 years after actual birth date (prolongation into middle childhood planned). aMale partners' sample includes one male partner who did not return T1 but returned T2.
N = 1,453 expectant mothers and their partners have provided their written consent to participate from June 2017 to the end of September 2018 (recruitment still ongoing). Of those having provided consent, the vast majority of N = 1,410 (97.0%) participants completed the first questionnaire (T1) resulting in a sample of n = 805 expectant mothers (57.1%) and n = 596 male partners (42.3%), plus n = 9 female partners (0.6%). At T1, most of the participants joined the study as a couple (81.3%; n = 1,146 people, i.e., 573 couples), but in some cases an expectant mother participated without a partner (16.4%; n = 232) and a few partners participated without the expectant mother (2.3%; n = 32).
As shown in Table 2, participants who returned T1 were recruited in obstetrical clinics in Dresden and the surrounding area (79.5%; n = 1,120), i.e., at information events and tours of the delivery rooms, scheduled birth registration done by midwives, and at the inpatient prenatal treatment ward. Further participants were included from a freestanding birthing center (4.1%; n = 58), at birth preparation courses in midwife practices (6.7%; n = 95), and at the early care of the city of Dresden (“Frühe Hilfen”; 0.1%; n = 2). A certain number of participants (4.4%; n = 62) were recruited via other places, i.e., mainly via announcements in gynecological outpatient settings, child-related stores, websites, newspapers, and magazines of health insurances, or through personal contact. Also, some participants (5.2%; n = 73) could not be assigned to a specific recruitment way.
Table 2.
Total sample who returned T1 (N = 1,410) according to recruitment way.
| Recruitment way | Sample (N = 1,410) | |
|---|---|---|
| n | (%) | |
| Obstetrical clinics (N = 8): information evenings and tours of the delivery rooms | 1,049 | (74.4) |
| - there of Dresden (N = 5) | 961 | (91.6) |
| - there of surrounding area (N = 3) | 88 | (8.4) |
| Obstetrical clinic (N = 1): scheduled birth registration | 38 | (2.7) |
| Obstetrical clinic (N = 1): inpatient prenatal treatment ward | 33 | (2.4) |
| Freestanding birthing center (N = 1): information evenings | 58 | (4.1) |
| Midwife practices (N = 12): birth preparation courses | 95 | (6.7) |
| City of Dresden: early care (“Frühe Hilfen”) | 2 | (0.1) |
| Other places | 62 | (4.4) |
| Unknown places | 73 | (5.2) |
The number of different people approached was varying between the locations. For example, 25–100% of the attendees of the birth preparation courses knew the study already as they often visited at least one of the clinics' information evenings as well. In sum, there was personal contact to N = 9,477 persons (i.e., expectant mothers and their male or female partners). Given that n = 1,348 participants provided written informed consent (not including those who were recruited via other places) this would indicate a response rate of 14.2%. However, the true response rate is considerably higher but hard to calculate exactly because a much smaller number was eligible due to multiple visits.
By the end of September 2018, 80.8% (n = 796) of those participants T2 was due for (n = 985) have sent back the second questionnaire which is 8 weeks after the expected delivery date. The retention rate from T1 to T2 is best for mothers (82.9%; n = 465) followed by male (78.5%; n = 328) and female partners (50.0%; n = 3). As some participants do not send back the follow-ups in time but with some delay, we expect the retention rate to increase in the further course of the study.
Interim Sample and Flow Chart of DREAMHAIR
N = 603 participants, i.e., 317 families, were eligible for DREAMHAIR as the anticipated delivery date was at least 4 weeks in the future (for flow chart of DREAMHAIR see Supplementary Figure 1). Of those, n = 58 participants have been excluded at T1 due to drug intake, medical conditions, hair characteristics, or organizational reasons. These participants might be included again at future measurement points. Further n = 257 participants could not be enrolled because of lack of response or interest. For n = 136 participants T1 had not been due by the end of September 2018. As a result, the sample of DREAMHAIR has consisted of N = 152 participants, i.e., 88 families, at this time. This is n = 87 expectant mothers, n = 64 male partners, and n = 1 female partner who returned hair samples at T1. As the T1 sampling of the child is due a few days after childbirth, n = 59 child samples (with one pair of twins) have been taken at T1 so far. In some cases, child hair was too short to be taken (n = 13). Further n = 17 child hair samples were not due yet.
T2 was due for n = 98 participants, i.e., 58 families from whom the majority (87.8%) returned T2 in time. Regarding child hair at T2, n = 47 samples out of n = 59 children (with one pair of twins) were returned. Further n = 6 child samples were not available because hair was too short to be taken and n = 6 samples were not returned in time. In addition, n = 9 participants, i.e., 5 families (with n = 5 children) joined the DREAMHAIR study initially at T2 due to organizational reasons.
Planned Data Analyses
The DREAM study provides quantitative data of four measurement points during the course of pregnancy to (at least) 2 years postpartum. Therefore, data will be analyzed both cross-sectionally and longitudinally with regard to the respective objectives of the study. More specifically, for the longitudinal analyses, multiple linear regression analyses, simple logistic regression analyses, and multinomial logistic regression analyses will be conducted to examine how prepartum individual and family factors predict outcomes after birth, such as health of family members and mothers' and their partners' participation in the labor market. As we are dealing with panel data, we will also perform fixed effects regression analyses in order to control for unobserved heterogeneity. Moreover, latent growth curve analyses in the framework of structural equation modeling (Bollen and Curran, 2006) and autoregressive cross-lagged analyses will be conducted when testing whether prepartum factors predict changes in social, work, and stress factors after birth. Full information maximum likelihood estimation or multiple imputation techniques will be used, as such techniques are considered to the most adequate approaches to handle missing data (Schafer and Graham, 2002).
We will analyze data on the individual level, while we will also have the opportunity to control for the partners' reports when both mother and partner participated as a couple. If both mother and her partner (and their baby, with respect to DREAMHAIR and DREAMMBU) participate in the study, data sets can be combined using a family code.
Then, multi-level modeling as a beneficial statistical approach exceeding conventional methods will be applied, enabling us to analyze relations within and between dyads or triads while taking into account the shared variance in dyadic (couples) or triadic (couples and their child) structure of hierarchical data (Woltman et al., 2012; Davis et al., 2018). Multi-level modeling is also well-suited for examining changes over an extended period of time with several measurement points without being limited by missing data (Woltman et al., 2012).
Power Analyses
Power analyses for the basic DREAM study and DREAMHAIR were conducted by means of Monte Carlo simulations using the R package “semsim,” version 0.5–13 (Beaujean, 2014). We conducted Monte Carlo simulation studies with 10,000 samples and examined the stability of our results by re-running the analyses with three different seeds. Power analyses were performed assuming a multivariate normal distribution of all variables. Moreover, we also estimated power with multivariate distributions deviating from normality. More specifically, in accordance with the methodological literature (Muthén and Asparouhov, 2002), we examined power for non-normal distributions with a skewness of 2.0 and a kurtosis of 3.5. Non-normal distributions were generated by using the multivariate Fleishman transformation (Vale and Maurelli, 1983). We also varied the proportion of missingness in the dependent variable (which is assumed to be measured at T4 where attrition is an important issue) from 0 to 70%.
First, we estimated power when the whole DREAM targeted sample of 2,000 couples, i.e., 4,000 individuals, are used in the analyses. With a sample size of N = 2,000, power analyses for multiple regression analyses with a continuous construct such as depressive symptoms as outcome variable (one of the main outcome variables in the study) and five continuous predictors showed a very high statistical power of 99% or above to detect significant effects given a small effect size of β = 0.20 between predictors and the outcome and a 5% (two-sided) type I error. Such high power was obtained even for non-normally distributed data and up to 70% proportion of missing data in the outcome variable. Therefore, the sample size at T4 will be large enough to obtain very high statistical power even with a dropout rate of 70% over the four assessment points.
As the number of same-sex couples in our study is very small, our statistical power will most likely not be sufficient to perform subgroup analyses. Therefore, we would consider these family constellations as case studies, which can be used to generate hypotheses for further studies with a targeted focus on families with same-sex parents.
Regarding the sub-study DREAMHAIR, approximately 20% of participants of the basic DREAM study participate in DREAMHAIR; hence we estimate N = 360 couples, i.e., 720 individuals, will participate at T1. For N = 360, even with a dropout rate of 40% at T4, Monto Carlo simulations estimated a power of 93% (multivariate normal distribution) and 80% (non-normally distributed data) to detect small effect sizes of β = 0.20 between predictors and the outcome in multiple regression analyses with five predictors and a 5% (two-sided) type I error. Moreover, a somewhat larger effect size of β = 0.28 will be detected with a power of 94% (multivariate normal distribution) and a power of 80% (non-normally distributed data) in the unlikely case that attrition will be as high as 70%.
With respect to the sub-study DREAMMBU, the clinical sample will be much smaller (N = 70 mothers with their babies and, if available, partners). We expect a higher compliance of the clinical branch (compared to the community branch), as women are personally bound to our team. Specifically, this sample size allows to detect medium effects at an α-level of 0.05 and a statistical power of 0.80 (repeated measures ANOVA, four measurement points), assuming a moderate correlation (r = 0.50) among repeated measures as conducted using G*Power 3.1 (Faul et al., 2007, 2009). As we will be able to recruit participants for the clinical sample for a longer period than for the community sample, our sample size then will be sufficient to allow subgroup analyses as a function of responder status or pre-treatment HCC.
Regarding DREAMTALK, we are targeting N = 40 couples. In qualitative research, the sample size can generally be determined by saturation. While the sample size should be large enough to sufficiently describe the phenomenon of interest (Glaser and Strauss, 1967; Malterud et al., 2016), saturation is reached when no further information is gained by interviewing further participants (Kvale, 1996). Different authors have suggested sample sizes between 20 and 50 (Morse, 1994; Creswell and Poth, 2013). Therefore, we are confident that our subsample size will be large enough to reach saturation.
Altogether, the targeted sample size of the basic DREAM study and the subsample sizes of the sub-studies will be large enough to answer the main research questions.
First Results
In this chapter, preliminary results regarding the sample of the basic DREAM study are presented.
Sociodemographic Characteristics
Tables 3, 4 show preliminary sociodemographic characteristics of the basic DREAM study sample during pregnancy (T1). The majority of expectant women (96.0%), male partners (95.6%), and all female partners reported German to be the mother tongue. On average, at T1 expectant mothers were in gestational week 29.9 (SD = 6.1; Range = 10–41) and most had a singleton pregnancy (98.0%) while n = 11 women were pregnant with twins and n = 2 women with multiples. For the majority of them, it was the first child (expectant mothers: 78.3%; male partners: 76.0%; female partners: 77.8%).
Table 3.
Sociodemographic characteristics of expectant mothers and their partners during pregnancy (T1).
|
Expectant mothers (n = 805) |
Male partners to the mother (n = 596) |
Female partners to the mother (n = 9) |
|
|---|---|---|---|
| Age | 30.1 ± 4.0 (15-42) | 32.4 ± 5.0 (22-56) | 35.4 ± 6.5 (28-47) |
| Marital status | |||
| Married/registered same sex partnership | 336 (41.7) | 259 (43.4) | 8 (88.9) |
| Unmarried | 441 (54.8) | 311 (52.2) | 1 (11.1) |
| Divorced | 25 (3.1) | 22 (3.7) | 0 (0.0) |
| Widowed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Unknown | 2 (0.3) | 0 (0.0) | 0 (0.0) |
| Missing data | 1 (0.1) | 4 (0.7) | 0 (0.0) |
| Partnership | |||
| Yes | 791 (98.3) | 588 (98.7) | 9 (100.0) |
| Living together | |||
| Yes, permanently | 745 (94.2) | 555 (94.4) | 9 (100.0) |
| Yes, not permanently | 35 (4.4) | 26 (4.4) | 0 (0.0) |
| No | 7 (0.9) | 5 (0.9) | 0 (0.0) |
| Missing data | 4 (0.5) | 2 (0.3) | 0 (0.0) |
| No | 9 (1.1) | 2 (0.3) | 0 (0.0) |
| Missing data | 5 (0.6) | 6 (1.0) | 0 (0.0) |
| Number of children | |||
| 0 | 630 (78.3) | 453 (76.0) | 7 (77.8) |
| 1 | 143 (17.8) | 101 (17.0) | 1 (11.1) |
| 2 | 20 (2.5) | 24 (4.0) | 0 (0.0) |
| 3 | 4 (0.5) | 4 (0.7) | 0 (0.0) |
| 4 | 2 (0.2) | 0 (0.0) | 0 (0.0) |
| Missing data | 6 (0.7) | 14 (2.3) | 1 (11.1) |
| Education | |||
| No degree | 0 (0.0) | 2 (0.3) | 0 (0.0) |
| Lower secondary education level 2 | 7 (0.9) | 16 (2.7) | 0 (0.0) |
| Secondary school certificate | 164 (20.4) | 157 (26.3) | 5 (55.6) |
| Advanced technical college entrance qualification | 66 (8.2) | 51 (8.6) | 2 (22.2) |
| A-level through second chance education | 17 (2.1) | 16 (2.7) | 0 (0.0) |
| Subject-related or higher education entrance qualification (A-level) | 548 (68.1) | 341 (57.2) | 2 (22.2) |
| Still in school | 2 (0.2) | 0 (0.0) | 0 (0.0) |
| Unknown | 1 (0.1) | 2 (0.3) | 0 (0.0) |
| Missing data | 0 (0.0) | 11 (1.9) | 0 (0.0) |
| Professional qualification | |||
| No qualification | 4 (0.5) | 4 (0.7) | 0 (0.0) |
| Occupational apprenticeship | 285 (35.4) | 198 (33.2) | 6 (66.7) |
| Master of crafts | 30 (3.7) | 47 (7.9) | 1 (11.1) |
| University | 434 (53.9) | 277 (46.4) | 2 (22.2) |
| Doctoral degree | 34 (4.2) | 32 (5.4) | 0 (0.0) |
| Still in qualification | 15 (1.9) | 20 (3.4) | 0 (0.0) |
| Missing data | 3 (0.4) | 18 (3.0) | 0 (0.0) |
| Working hours per week | 37.5 ± 8.9 (2-68) | 40.9 ± 7.7 (1-70) | 40.7 ± 3.7 (35-45) |
| Net earnings on average | |||
| Up to 450 € | 25 (3.1) | 14 (2.3) | 0 (0.0) |
| 451 € to 850 € | 25 (3.1) | 11 (1.9) | 0 (0.0) |
| 851 € to 1,500 € | 224 (27.8) | 106 (17.8) | 4 (44.4) |
| 1,501 € to 2,500 € | 417 (51.8) | 307 (51.5) | 5 (55.6) |
| More than 2,500 € | 73 (9.1) | 125 (21.0) | 0 (0.0) |
| Not working or missing data | 41 (5.1) | 33 (5.5) | 0 (0.0) |
| Job burden | |||
| Not burdened | 73 (9.1) | 54 (9.1) | 0 (0.0) |
| A little bit burdened | 254 (31.5) | 163 (27.3) | 2 (22.2) |
| Moderately burdened | 269 (33.4) | 254 (42.6) | 3 (33.4) |
| Heavily burdened | 100 (12.4) | 79 (13.3) | 2 (22.2) |
| Very heavily burdened | 7 (0.9) | 11 (1.8) | 1 (11.1) |
| Not working or missing data | 102 (12.7) | 35 (5.9) | 1 (11.1) |
| Job satisfaction | |||
| Very satisfied | 103 (12.8) | 94 (15.8) | 1 (11.1) |
| Quite satisfied | 323 (40.1) | 282 (47.3) | 4 (44.5) |
| Neither unsatisfied nor satisfied | 132 (16.4) | 111 (18.6) | 2 (22.2) |
| Quite unsatisfied | 94 (11.7) | 57 (9.6) | 1 (11.1) |
| Very unsatisfied | 48 (6.0) | 18 (3.0) | 1 (11.1) |
| Not working or missing data | 105 (13.0) | 34 (5.7) | 0 (0.0) |
| Intention to take parental leave | |||
| Yes | 757 (94.0) | 477 (80.0) | 7 (77.8) |
| No | 5 (0.6) | 61 (10.3) | 2 (22.2) |
| Unknown | 2 (0.3) | 27 (4.5) | 0 (0.0) |
| Missing data | 41 (5.1) | 31 (5.2) | 0 (0.0) |
| Duration of parental leave as intended | 14.4 ± 5.0 (3-36) | 3.3 ± 3.0 (1-24) | 4.4 ± 3.7 (2-12) |
n (%) or M ± SD (Range).
Table 4.
Former (1 year ago) and current employment during pregnancy (T1).
| Expectant mothers (n = 805) | Male partners to the mother (n = 596) | Female partners to the mother (n = 9) | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Former employment (1 year ago) | |||
| No employment | 9 (1.1) | 5 (0.8) | 0 (0.0) |
| Not regularly employed | 8 (1.0) | 6 (1.0) | 0 (0.0) |
| Marginal employment | 39 (4.8) | 23 (3.9) | 0 (0.0) |
| Part-time | 185 (23.0) | 41 (6.9) | 0 (0.0) |
| Full-time | 498 (61.9) | 484 (81.2) | 8 (88.9) |
| Occupational retraining | 0 (0.0) | 1 (0.2) | 0 (0.0) |
| Volunteer | 2 (0.2) | 0 (0.0) | 0 (0.0) |
| Housewife/houseman | 3 (0.4) | 2 (0.3) | 0 (0.0) |
| Parental leave | 20 (2.5) | 1 (0.2) | 0 (0.0) |
| Still in school | 3 (0.4) | 1 (0.2) | 0 (0.0) |
| Still in apprenticeship | 17 (2.1) | 6 (1.0) | 0 (0.0) |
| Still in university | 86 (10.7) | 59 (9.9) | 0 (0.0) |
| Employment ban | 8 (1.0) | 0 (0.0) | 0 (0.0) |
| Occupational disability | 3 (0.4) | 0 (0.0) | 0 (0.0) |
| Other | 18 (2.2) | 9 (1.5) | 0 (0.0) |
| Missing data | 11 (1.4) | 7 (1.2) | 1 (0.0) |
| Current employment | |||
| No employment | 17 (2.1) | 5 (0.8) | 0 (0.0) |
| Not regularly employed | 2 (0.2) | 3 (0.5) | 0 (0.0) |
| Marginal employment | 21 (2.6) | 17 (2.9) | 0 (0.0) |
| Part-time | 135 (16.8) | 44 (7.4) | 1 (11.1) |
| Full-time | 359 (44.6) | 492 (82.6) | 8 (88.9) |
| Occupational retraining | 0 (0.0) | 2 (0.3) | 0 (0.0) |
| Volunteer | 1 (0.1) | 0 (0.0) | 0 (0.0) |
| Housewife/houseman | 9 (1.1) | 1 (0.2) | 0 (0.0) |
| Parental leave | 103 (12.8) | 1 (0.2) | 0 (0.0) |
| Still in school | 3 (0.4) | 0 (0.0) | 0 (0.0) |
| Still in apprenticeship | 6 (0.7) | 6 (1.0) | 0 (0.0) |
| Still in university | 62 (7.7) | 47 (7.9) | 0 (0.0) |
| Employment ban | 239 (29.7) | 0 (0.0) | 0 (0.0) |
| Occupational disability | 3 (0.4) | 0 (0.0) | 0 (0.0) |
| Other | 24 (3.0) | 8 (1.3) | 0 (0.0) |
| Missing data | 1 (0.1) | 4 (0.7) | 0 (0.0) |
Multiple answers were possible.
Mean age of expectant mothers was 30.1 years (SD = 4.0; Range = 15–42), 32.4 years of male partners (SD = 5.0; Range = 22–56), and 35.4 years of female partners (SD = 6.5; Range = 28–47).
Compared to the overall German population (Statistisches Bundesamt, 2018a,b) and the population of Dresden (Statistisches Landesamt Sachsen, 2018), participants are characterized by a rather high educational and professional level and full-time work status.
Regarding employment 1 year ago, i.e., prior to pregnancy, first analyses showed that a greater ratio of male partners (81.2%; n = 484) than expectant mothers (61.9%; n = 498) had a full-time position (χ2 = 62.153; df = 1; p < 0.01). Accordingly, a part-time position was hold by a greater ratio of expectant mothers (23.0%; n = 185) than male partners (6.9%; n = 41; χ2 = 66.032; df = 1; p < 0.01). These gender differences could be found irrespective of whether expecting the first child or already having children, i.e., the ratio holding a full-time position was lower in first-time mothers (72.1%; n = 446) compared to first-time fathers (80.4%; n = 360; χ2 = 9.702; df = 1; p < 0.01) as well as in mothers (28.4%; n = 48) compared to fathers already having children (87.4%; n = 111; χ2 = 101.521; df = 1; p < 0.01). Likewise, the ratio working part-time was higher both in first-time mothers and mothers already having children compared to the respective men.
In fact, as shown in Table 5, these gender differences regarding employment 1 year ago, i.e., prior to pregnancy, were more pronounced in parents who already had children compared to first-time parents. Hence, among expectant mothers, first-time mothers (72.1%; n = 446) were working full-time more often than mothers already having children (28.4%; n = 48; χ2 = 108.140; df = 1; p < 0.01). Regarding part-time work, it was vice-versa, i.e., a higher ratio of mothers already having children (47.9%; n = 81) compared to first-time mothers (16.5%; n = 102) was working part-time (χ2 = 73.648; df = 1; p < 0.01). In male partners, no such a difference between first-time fathers and fathers already having children could be found regarding a full-time (80.4%; n = 360 vs. 87.4%; n = 111; χ2 = 3.314; df = 1; p = 0.07) or part-time position (7.1%; n = 32 vs. 7.1%; n = 9; (χ2 = 0.000; df = 1; p = 0.98).
Table 5.
Comparisons between sexes and first-time vs. parents already having children regarding full-time and part-time work status 1 year ago, i.e., prior to pregnancy (T1).
| Compared groups | Work status | n (%) | χ2 | df | p | |
|---|---|---|---|---|---|---|
| Comparison between sexes | EM0 vs. P0 | Full-time | EM0: 446 (72.1%) P0: 360 (80.4%) |
9.702 | 1 | 0.00 |
| Part-time | EM0: 102 (16.5%) P0: 32 (7.1%) |
20.626 | 1 | 0.00 | ||
| EM1+ vs. P1+ | Full-time | EM1+: 48 (28.4%) P1+: 111 (87.4%) |
101.521 | 1 | 0.00 | |
| Part-time | EM1+: 81 (47.9%) P1+: 9 (7.1%) |
57.160 | 1 | 0.00 | ||
| Comparison between first-time parents and parents already having children | EM0 vs. EM1+ | Full-time | EM0: 446 (72.1%) EM1+: 48 (28.4%) |
108.140 | 1 | 0.00 |
| Part-time | EM0: 102 (16.5%) EM1+: 81 (47.9%) |
73.648 | 1 | 0.00 | ||
| P0 vs. P1+ | Full-time | P0: 360 (80.4%) P1+: 111 (87.4%) |
3.314 | 1 | 0.07 | |
| Part-time | P0: 32 (7.1%) P1+: 9 (7.1%) |
0.000 | 1 | 0.98 |
At T1 (during pregnancy), participants were asked whether they have been working full-time or part-time 1 year ago, i.e., prior to pregnancy. EM0: first-time expectant mothers; EM1+: expectant mothers already having children; P0: first-time fathers (male partners); P1+: fathers (male partners) already having children.
Regarding current employment, i.e., during pregnancy, nearly one third of expectant mothers was in employment ban because of a health risk for mother or child (29.7%; n = 239). Further, the number of expectant mothers currently holding a full-time (44.6%; n = 359; χ2 = 101.327; df = 1; p < 0.01) and part-time position (16.8%; n = 135; χ2 = 23.539; df = 1; p < 0.01) was lower than 1 year ago (i.e., prior to pregnancy). In male partners, no such decrease regarding a full-time (χ2 = 1.333; df = 1; p = 0.25) and part-time position (exact p = 0.63) within the last year was found.
During pregnancy, the majority in all groups reported that they intended to take parental leave. Expectant mothers and male partners differed in the intention to take parental leave (94.0 vs. 80.0%; χ2 = 105.16, df = 2; p < 0.01). Further, expectant mothers intended to take parental leave for a longer period of time (M = 14.4 months; SD = 5.0; Range = 3–36) than male partners (M = 3.3 months; SD = 3.0; Range = 1–24; t(1209.48) = 48.57, p < 0.01, BCa 95%-CI [10.63; 11.56]).
Birth-Related Characteristics
By the end of September 2018, birth-related characteristics at T2 (Table 6) were available for n = 465 mothers who had given birth to their child during the period from July 2017 to July 2018 with preterm delivery in n = 13 cases (2.8%) which is lower than in the overall German population (in 2013: 8.7%, Statistisches Bundesamt; born in hospitals in 2017: 8.6 %, IQTIG–Institut für Qualitätssicherung und Transparenz im Gesundheitswesen, 2018). N = 465 mothers gave birth to n = 472 children with a nearly balanced gender ratio (51.5%; n = 243 female) which is representative for the overall German population (48.7% female) and Saxony (48.9% female) in 2017 (Statistisches Bundesamt, 2018d). Most of the children were delivered vaginally (80.6%; n = 375). The ratio of cesarean sections (18.5%; n = 86) was as low as it is typical for the area of Dresden (in 2013: 19.5%; Statistisches Bundesamt, 2015), i.e., lower than in Saxony (24.0%) and in the overall German population (30.5%) in 2017 (Statistisches Bundesamt, 2018c). The majority of partners attended birth (97.3%; n = 319 male partners and 100%; n = 3 female partners).
Table 6.
Birth-related characteristics as reported by the mothers 8 weeks after anticipated birth date (T2).
| Mothers (n = 465) | |
|---|---|
| n (%) | |
| Number of delivered children | |
| One | 459 (98.7) |
| Twins | 5 (1.1) |
| Multiples | 1 (0.2) |
| Preterm delivery | |
| Yes | 13 (2.8) |
| No | 445 (95.7) |
| Missing data | 7 (1.5) |
| Mode of delivery | |
| Spontaneous vaginal birth | 257 (55.3) |
| Vaginal birth induced by drugs | 81 (17.4) |
| Vaginal operative birth (with forceps or vacuum extraction) | 37 (7.9) |
| Planned cesarean section due to personal reasons | 2 (0.4) |
| Planned cesarean section due to medical reasons | 31 (6.7) |
| Unplanned cesarean section | 53 (11.4) |
| Missing data | 4 (0.9) |
| Sex of child (n = 472) | |
| Female | 243 (51.5) |
| Male | 221 (46.8) |
| Missing data | 8 (1.7) |
Dropout Analyses
Dropout analyses (tables on request) considering sociodemographic characteristics of completers vs. non-completers (whose T2 data were due by the end of September 2018) were conducted separately for expectant mothers (n = 465 vs. n = 96) and male partners (n = 328 vs. n = 90), but not for female partners due to the small sample sizes (n = 3 vs. n = 3). Completers and non-completers at T2 did not differ in sociodemographic characteristics with some exceptions.
Regarding expectant mothers, completers were reporting German as their mother tongue (96.8 vs. 91.7%; Fisher's exact test, p < 0.05) and intended to take parental leave (99.3 vs. 95.5%; Fisher's exact test, p < 0.01) more often than non-completers. While there were no differences regarding current employment, completers differed from non-completers regarding employment 1 year ago. Formerly, completers were working in a full-time position more often than non-completers (65.4 vs. 53.7%; χ2 = 4.674, df = 1, p < 0.05), while the ratio of not being regularly employed (0.2 vs. 4.2%; Fisher's exact test, p < 0.01) and being a housewife (0.0 vs. 2.1%; Fisher's exact test, p < 0.05) was lower in completers than in non-completers.
Regarding male partners, completers lived permanently together with the expectant mother more often (96.3 vs. 88.8%; Fisher's exact test, p < 0.05), had a higher education (e.g., 61.6 vs. 51.1% having a subject-related or higher education entrance qualification (A-level); U = 12113.0; z = −2.140; p < 0.05), and a higher professional qualification (e.g., 57.0 vs. 40.0% having a university or doctoral degree; U = 11458.0; z = −2.424; p < 0.05) than non-completers.
Discussion
Examining expectant mothers and their partners from pregnancy to at least 2 years postpartum, the DREAM study is one of the first prospective cohort studies investigating the changes of parental work participation and conditions, role distributions, and stress factors and its impact on perinatal outcomes and long-term mental and somatic health of the entire family while taking into account underlying biological processes regarding long-term activity of the HPA axis.
Altogether, major strengths of the DREAM study are (1) the prospective design stretching from one measurement point prepartum to at least three additional measurement points within the first two years postpartum (prolongation into middle childhood planned) which allows both longitudinal and cross-sectional analyses, (2) a unique multi-method approach combining quantitative data (using predominantly well-established scales) with long-term endocrinological data (DREAMHAIR) and qualitative interview data (DREAMTALK), (3) a large, representative community sample (interim sample of N = 1,410 participants by the end of September 2018, targeting N = 4,000 participants) of both mothers and male or female partners allowing the use of advanced statistical approaches such as multi-level modeling, (4) comparison to a clinical sample of mothers with postpartum mental disorders, their children, and (if available) their partners during the course from admission to discharge of a MBU tracking intervention effects and post-treatment, (5) a cooperation within Germany and abroad with matching instruments and assessment waves to facilitate internal and cross-cultural comparisons of findings.
Regarding the interim sample, first results of analyses conducted for this paper showed that our interim sample mainly consists of expectant mothers and their partners who expect their first child. This is because some of the recruitment ways like the clinics' information evenings or birth preparation courses are visited mainly by families expecting their first child. Nevertheless, it is exactly those parents who are of main interest, as the present study aims primarily at investigating the transition and change from being a couple to becoming a family. Further, there are slightly more expectant mothers than partners participating and the majority of participants has a rather high educational and professional level. This is in accordance with previous findings, i.e., people are more likely to participate in epidemiologic studies if they are female, well-educated, and/or have a higher socioeconomic status (e.g., Søgaard et al., 2004; Galea and Tracy, 2007; Gustavson et al., 2012). The self-selection bias might be even bigger in family studies. First, fathers might join or complete those studies more seldom than mothers. Second, particularly those fathers who do participate might be more involved in family matters or might have more progressive gender role values than nonparticipating fathers as discussed in Costigan and Cox (2001). Also, it is difficult to reach and recruit becoming fathers who are not in a relationship with the becoming mother or who are not accompanying their partners at the information evening or birth preparation courses. Moreover, it is conceivable that families interested in the compatibility of work and family may have contributed to the high ratio of expectant mothers and partners holding a full-time position. When speaking about the representativeness of the sample and generalizability of findings, the possibility of a healthy worker-effect has to be considered, i.e., in research on working populations, healthy and little burdened individuals are often overrepresented due to their greater likelihood of participating in workforce (Li and Sung, 1999; Shah, 2009).
Further, we showed that a higher ratio of first-time mothers has been working full-time prior to pregnancy compared to mothers already having a child/children. No such difference was found in male partners. This is in accordance with previous findings that German women but not men reduce their amount of working time after giving birth to a child (Bundesministerium für Familie Senioren Frauen und Jugend, 2017a). More importantly, this is in line with our postulation of an emerging gender gap interfering with gender equality as it has consequences for long-term labor market inclusion/exclusion (Barker and Pawlak, 2011; Miani and Hoorens, 2014). Altogether, this sample seems to be appropriate for examining our research questions as a pronounced number of working participants is needed to profoundly investigate the changes of parental work participation, role distributions, and stress factors and its long-term implications for family health.
Regarding birth-related characteristics, first analyses showed that the ratio of mothers who delivered by cesarean section is as low as typical for the region (Statistisches Bundesamt, 2015) while the rate of preterm deliveries of the interim DREAM sample is lower compared to the overall German population (Statistisches Bundesamt, 2015; IQTIG–Institut für Qualitätssicherung und Transparenz im Gesundheitswesen, 2018). A possible reason may be that participating mothers who had a preterm delivery were more likely to drop out because child care is more extensive in the early postpartum, i.e., an already sensitive period.
Dropout analyses found only a few differences between completers and non-completers at T2 indicating that (1) non-completing male partners had a lower educational level as well as professional qualification and lived more seldom permanently together compared to completing male partners and (2) non-completing mothers were speaking German as their mother tongue, working full-time, and planning to take parental leave less often than completing mothers. However, the DREAM study is characterized by a rather low dropout rate which is supported by our retention strategy using reminders and incentives (Booker et al., 2011). In future, we will still increase personal contact via telephone to participants who do not send back the follow-up questionnaires in time to reduce the attrition even more. This will be an additional strength in the further course of the study as we prospectively would like to add measurement points reaching into middle childhood. Hence, it will be possible to examine long-term effects on family health as well as on a potential gender gap regarding labor market inclusion/exclusion (Schober and Zoch, 2015).
To sum up, the DREAM study will contribute to a better understanding of the complex relationships between parental work participation, role distribution, and stress factors and its implications for perinatal outcome and long-term mental and somatic health of mothers, their partners in parenting, and children. With former studies neglecting confounding and moderating factors, this innovative study with its sub-studies allows a comprehensive picture of the family as a whole. To our knowledge, it is the first study combining work-related health implications with the assessment of long-term activity of the HPA axis as measured by HCC in each individual and parent-child dyad. In particular, examining the cumulated steroid hormones of both parents and their child in HCC data, the current findings will be valuable for understanding the transgenerational transmissions of long-term alterations of the HPA axis and the interplay as a couple. The comparison to a clinical sample of mothers, their children, and (if available) their partners who will be assessed during the course of a state-of-the-art treatment in a MBU will help to better understand the potential underlying mechanisms of these processes and intervention benefits. The clinical sub-study has further the potential to add evidence regarding the role of parent-child interaction for child health, particularly its temperament and regulation disorders. Moreover, it is unique to this research area to investigate both mother-child and father-child dyads. Finally, results will not only be of scientific interest but also of socio-political relevance as they will generate important findings warranted by this inter-disciplinary research field and thus may contribute moving these issues higher on the political agenda.
Ethics Statement
This study has been carried out in accordance with the recommondations of the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden with written consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. This protocol was approved by the DREAM steering group and by the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden (No: EK 278062015).
Author Contributions
SG-N has acquired the funding and been responsible for conception and design of the basic DREAM study with its sub-studies as well as the coordination and supervision of the (ongoing) data collection. JJ-H, SS-S, SG-N, and AF have been responsible for the conception and design of the sub-study DREAMHAIR. MK, VK, CA, CS, and AF supported the conduction of the study, especially through data collection. PW provided access to potential participants. KW provided resources for the acquisition of data in the DREAM study. CK advised the sub-study DREAMHAIR and provided support for hair cortisol analyses. MK and VK prepared the data for statistical analysis. VK performed the statistical analysis except from Monte Carlo simulations. TvS performed Monte Carlo simulations. VK wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We want to thank all (expectant) mothers and their partners for supporting our project. Furthermore, we want to thank all cooperating clinics and midwives for providing access to the potential participants as well as all students performing the recruitment. We wish to extend many thanks to all institutions supporting our lottery. We are further very grateful to Dr. Janice Hegewald who as a native English-speaking researcher back-translated the mentioned questionnaires.
Footnotes
Funding. The DREAM study is funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation; GA 2287/4-1) and by the Deutsche Gesellschaft für Psychosomatische Frauenheilkunde und Geburtshilfe (DGPFG e.V., German Society of Psychosomatic Obstetrics and Gynecology).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2019.01273/full#supplementary-material
References
- Abidin R. R. (1995). Parenting Stress Index: Manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Arndt A., Patzelt J., Andor T., Hoyer J., Gerlach A. L. (2011). Psychometrische Gütekriterien des Metakognitionsfragebogens (Kurzversion, MKF-30). Z. Klin. Psychol. Psychother. 40, 107–114. 10.1026/1616-3443/a000087 [DOI] [Google Scholar]
- Arnetz B. B., Brenner S.-O., Levi L., Hjelm R., Petterson I.-L., Wasserman J., et al. (1991). Neuroendocrine and immunologic effects of unemployment and job insecurity. Psychother. Psychosom. 55, 76–80. 10.1159/000288412 [DOI] [PubMed] [Google Scholar]
- Barker B., Iles J. E., Ramchandani P. G. (2017). Fathers, fathering and child psychopathology. Curr. Opin. Psychol. 15, 87–92. 10.1016/j.copsyc.2017.02.015 [DOI] [PubMed] [Google Scholar]
- Barker G., Pawlak P. (2011). Men in Families and Family Policy in a Changing World. New York, NY: United Nations. [Google Scholar]
- Bates J. E., Freeland C. A. B., Lounsbury M. L. (1979). Measurement of infant difficultness. Child Dev. 50, 794–803. 10.2307/1128946 [DOI] [PubMed] [Google Scholar]
- Beaujean A. A. (2014). Sample size determination for regression models using Monte Carlo methods in R. Pract. Assess. Res. Eval. 19, 1–16. Available online at: http://pareonline.net/getvn.asp?v=19&n=12 (accessed on May 4, 2019). [Google Scholar]
- Beijers R., Buitelaar J. K., de Weerth C. (2014). Mechanisms underlying the effects of prenatal psychosocial stress on child outcomes: beyond the HPA axis. Eur. Child Adolesc. Psychiatry 23, 943–956. 10.1007/s00787-014-0566-3 [DOI] [PubMed] [Google Scholar]
- Beitins I. Z., Bayard F., Ances I. G., Kowarski A., Migeon C. J. (1973). The metabolic clearance rate, blood production, interconversion and transplacental passage of cortisol and cortisone in pregnancy near term. Pediatr. Res. 7, 509–519. 10.1203/00006450-197305000-00004 [DOI] [PubMed] [Google Scholar]
- Bergant A., Nguyen T., Heim K., Ulmer H., Dapunt O. (1998). Deutschsprachige Fassung und Validierung der Edinburgh postnatal depression scale. Dtsch. Med. Wochenschr. 123, 35–40. 10.1055/s-2007-1023895 [DOI] [PubMed] [Google Scholar]
- Bernstein D. P., Fink L. A. (1998). Childhood Trauma Questionnaire: A Retrospective Self-Report. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bodenmann G. (2007). Multidimensionaler Stressfragebogen für Paare (MDSP). Unpublished scale, University of Zurich, Switzerland. [Google Scholar]
- Bollen K. A., Curran P. J. (2006). Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: Wiley; 10.1002/0471746096 [DOI] [Google Scholar]
- Booker C. L., Harding S., Benzeval M. (2011). A systematic review of the effect of retention methods in population-based cohort studies. BMC Publ. Health 11:249. 10.1186/1471-2458-11-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosquet Enlow M., Devick K. L., Brunst K. J., Lipton L. R., Coull B. A., Wright R. J. (2017). Maternal lifetime trauma exposure, prenatal cortisol, and infant negative affectivity. Infancy 22, 492–513. 10.1111/infa.12176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers K., Ding L., Gregory S., Yolton K., Ji H., Meyer J., et al. (2018). Maternal distress and hair cortisol in pregnancy among women with elevated adverse childhood experiences. Psychoneuroendocrinology 95, 145–148. 10.1016/j.psyneuen.2018.05.024 [DOI] [PubMed] [Google Scholar]
- Brennan P. A., Pargas R., Walker E. F., Green P., Jeffrey Newport D., Stowe Z. (2008). Maternal depression and infant cortisol: influences of timing, comorbidity and treatment. J. Child Psychol. Psychatry 49, 1099–1107. 10.1111/j.1469-7610.2008.01914.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockington I. F., Oates J., George S., Turner D., Vostanis P., Sullivan M., et al. (2001). A screening questionnaire for mother-infant bonding disorders. Arch. Wom. Ment. Health 3, 133–140. 10.1007/s007370170010 [DOI] [Google Scholar]
- Brown R. W., Diaz R., Robson A. C., Kotelevtsev Y. V., Mullins J. J., Kaufman M. H., et al. (1996). The ontogeny of 11 beta-hydroxysteroid dehydrogenase type 2 and mineralocorticoid receptor gene expression reveal intricate control of glucocorticoid action in development. Endocrinology 137, 794–797. 10.1210/endo.137.2.8593833 [DOI] [PubMed] [Google Scholar]
- Bryan M. L., Sevilla-Sanz A. (2010). Does housework lower wages? Evidence for Britain. Oxf. Econ. Paper 63, 187–210. 10.1093/oep/gpq011 [DOI] [PubMed] [Google Scholar]
- Buehler C., O'Brien M. (2011). Mothers' part-time employment: Associations with mother and family well-being. J. Fam. Psychol. 25, 895–906. 10.1037/a0025993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundesministerium für Familie Senioren Frauen und Jugend (2017a). Familienreport 2017. Leistungen, Wirkungen, Trends. Berlin. [Google Scholar]
- Bundesministerium für Familie Senioren Frauen und Jugend (2017b). Zweiter Gleichstellungsbericht der Bundesregierung. Berlin. [Google Scholar]
- Buss C., Entringer S., Moog N. K., Toepfer P., Fair D. A., Simhan H. N., et al. (2017). Intergenerational transmission of maternal childhood maltreatment exposure: implications for fetal brain development. J. Am. Acad. Child Adolesc. Psychiatr. 56, 373–382. 10.1016/j.jaac.2017.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caparros-Gonzalez R. A., Romero-Gonzalez B., Strivens-Vilchez H., Gonzalez-Perez R., Martinez-Augustin O., Peralta-Ramirez M. I. (2017). Hair cortisol levels, psychological stress and psychopathological symptoms as predictors of postpartum depression. PLoS ONE 12:e0182817. 10.1371/journal.pone.0182817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrousos G. P. (2009). Stress and disorders of the stress system. Nat. Rev. Endocrinol. 5, 374–381. 10.1038/nrendo.2009.106 [DOI] [PubMed] [Google Scholar]
- Colvonen P. J., Glassman L. H., Crocker L. D., Buttner M. M., Orff H., Schiehser D. M., et al. (2017). Pretreatment biomarkers predicting PTSD psychotherapy outcomes: A systematic review. Neurosci. Biobehav. Rev. 75, 140–156. 10.1016/j.neubiorev.2017.01.027 [DOI] [PubMed] [Google Scholar]
- Connellan K., Bartholomaeus C., Due C., Riggs D. W. (2017). A systematic review of research on psychiatric mother-baby units. Arch. Wom. Ment. Health 20, 373–388. 10.1007/s00737-017-0718-9 [DOI] [PubMed] [Google Scholar]
- Costigan C. L., Cox M. J. (2001). Fathers' participation in family research: is there a self-selection bias? J. Fam. Psychol. 15, 706–720. 10.1037/0893-3200.15.4.706 [DOI] [PubMed] [Google Scholar]
- Cox J. L., Holden J. M., Sagovsky R. (1987). Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Creswell J. W., Poth C. N. (2013). Qualitative Inquiry and Research Design: Choosing Among Five Approaches. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Crouter A. C., Manke B. (1997). Development of a typology of dual-earner families: A window into differences between and within families in relationships, roles, and activities. J. Fam. Psychol. 11, 62–75. 10.1037/0893-3200.11.1.62 [DOI] [Google Scholar]
- Cruise S., Layte R., Stevenson M., O'Reilly D. (2018). Prevalence and factors associated with depression and depression-related healthcare access in mothers of 9-month-old infants in the Republic of Ireland. Epidemiol. Psychiatr. Sci. 27, 468–478. 10.1017/S2045796017000026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Anna-Hernandez K. L., Ross R. G., Natvig C. L., Laudenslager M. L. (2011). Hair cortisol levels as a retrospective marker of hypothalamic–pituitary axis activity throughout pregnancy: comparison to salivary cortisol. Physiol. Behav. 104, 348–353. 10.1016/j.physbeh.2011.02.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies R., Pierre G. (2005). The family gap in pay in Europe: a cross-country study. Labour Econom. 12, 469–486. 10.1016/j.labeco.2005.05.003 [DOI] [Google Scholar]
- Davis E. P., Glynn L. M., Waffarn F., Sandman C. A. (2011). Prenatal maternal stress programs infant stress regulation. J. Child Psychol. Psychatry 52, 119–129. 10.1111/j.1469-7610.2010.02314.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis E. P., Sandman C. A. (2012). Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology 37, 1224–1233. 10.1016/j.psyneuen.2011.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M., West K., Bilms J., Morelen D., Suveg C. (2018). A systematic review of parent–child synchrony: it is more than skin deep. Dev. Psychobiol. 60, 674–691. 10.1002/dev.21743 [DOI] [PubMed] [Google Scholar]
- Derogatis L. R. (1977). SCL-90-R. Administration, Scoring and Procedures Manual-I for the R(evised). John Hopkins University School of Medicine. [Google Scholar]
- Derogatis L. R. (1993). Brief Symptom Inventory (BSI), Administration, Scoring and Procedures Manual (3 ed.). Minneapolis: National Computer Systems. [Google Scholar]
- Dettenborn L., Muhtz C., Skoluda N., Stalder T., Steudte S., Hinkelmann K., et al. (2012). Introducing a novel method to assess cumulative steroid concentrations: increased hair cortisol concentrations over 6 months in medicated patients with depression. Stress 15, 348–353. 10.3109/10253890.2011.619239 [DOI] [PubMed] [Google Scholar]
- Dettenborn L., Tietze A., Bruckner F., Kirschbaum C. (2010). Higher cortisol content in hair among long-term unemployed individuals compared to controls. Psychoneuroendocrinology 35, 1404–1409. 10.1016/j.psyneuen.2010.04.006 [DOI] [PubMed] [Google Scholar]
- Diego M. A., Field T., Hernandez-Reif M., Cullen C., Schanberg S., Kuhn C. (2004). Prepartum, postpartum, and chronic depression effects on newborns. Psychiatr. Interper. Biol. Process. 67, 63–80. 10.1521/psyc.67.1.63.31251 [DOI] [PubMed] [Google Scholar]
- Dørheim S. K., Bjorvatn B., Eberhard-Gran M. (2013). Sick leave during pregnancy: a longitudinal study of rates and risk factors in a Norwegian population. Br. J. Obstet. Gynaecol. 120, 521–530. 10.1111/1471-0528.12035 [DOI] [PubMed] [Google Scholar]
- Ehlers A., Steil R., Winter H., Foa E. (1996). Deutsche Übersetzung der Posttraumatic Stress Diagnostic Scale (PDS). Unpublished manuscript, Warneford Hospital, Department of Psychiatry, University of Oxford, UK. [Google Scholar]
- Ellert U., Lampert T., Ravens-Sieberer U. (2005). Messung der gesundheitsbezogenen Lebensqualität mit dem SF-8. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 48, 1330–1337. 10.1007/s00103-005-1168-5 [DOI] [PubMed] [Google Scholar]
- Entringer S., Buss C., Wadhwa P. D. (2015). Prenatal stress, development, health and disease risk: a psychobiological perspective-2015 Curt Richter Award Paper. Psychoneuroendocrinology 62, 366–375. 10.1016/j.psyneuen.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essex M. J., Klein M. H., Cho E., Kalin N. H. (2002). Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol. Psychiatry 52, 776–784. 10.1016/S0006-3223(02)01553-6 [DOI] [PubMed] [Google Scholar]
- Evans G. W., Kim P. (2007). Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol. Sci. 18, 953–957. 10.1111/j.1467-9280.2007.02008.x [DOI] [PubMed] [Google Scholar]
- Farrokhzad S., Ottersbach M., Tunç M., Meuer-Willuweit A. (2010). Abschlussbericht Rollenverständnis von Frauen und Männern mit Zuwanderungsgeschichte unter Berücksichtigung Intergenerativer und Interkultureller Einflüsse. Düsseldorf and Berlin: Ministerium für Gesundheit, Emanzipation, Pflege und Alter des Landes Nordrhein-Westfalen, Referat Öffentlichkeitsarbeit and Bundesministerium für Familie, Senioren, Frauen und Jugend. [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A.-G. (2009). Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.-G., Buchner A. J. B. (2007). G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Fischer S., King S., Papadopoulos A., Hotopf M., Young A. H., Cleare A. J. (2018). Hair cortisol and childhood trauma predict psychological therapy response in depression and anxiety disorders. Acta Psychiatr. Scand. 138, 526–535. 10.1111/acps.12970 [DOI] [PubMed] [Google Scholar]
- Foa E. B., Cashman L., Jaycox L., Perry K. (1997). The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychol. Assess. 9, 445–451. 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- Franke G. H. (2000). Brief Symptom Inventory (BSI) von LR Derogatis (Kurzform der SCL-90-R). Deutsche Version. Göttingen: Beltz Test GmbH. [Google Scholar]
- Franke G. H., Derogatis L. R. (2002). SCL-90-R: Die Symptom-Checkliste von L. R. Derogatis. Göttingen: Beltz Test. [Google Scholar]
- Frech A., Damaske S. (2012). The relationships between mothers' work pathways and physical and mental health. J. Health Soc. Behav. 53, 396–412. 10.1177/0022146512453929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friese K., Kirschner W. (2003). Das BabyCare-Projekt. Gynäkologe 36, 403–412. 10.1007/s00129-003-1360-3 [DOI] [Google Scholar]
- Fydrich T., Sommer G., Tydecks S., Brähler E. (2009). Fragebogen zur Sozialen Unterstützung (F-SozU): Normierung der Kurzform (K-14). Z. Med. Psychol. 18, 43–48. [Google Scholar]
- Galea S., Tracy M. (2007). Participation rates in epidemiologic studies. Ann. Epidemiol. 17, 643–653. 10.1016/j.annepidem.2007.03.013 [DOI] [PubMed] [Google Scholar]
- Galeris M.-G. (2016). Postpartale psychische Erkrankungen: Risikofaktoren und Auswirkungen auf die Mutter-Kind-Interaktion [unpublished master's thesis]. Friedrich-Alexander-Universität Erlangen-Nürnberg. [Google Scholar]
- Gallagher S., Sumner R. C., Muldoon O. T., Creaven A.-M., Hannigan A. (2016). Unemployment is associated with lower cortisol awakening and blunted dehydroepiandrosterone responses. Psychoneuroendocrinology 69, 41–49. 10.1016/j.psyneuen.2016.03.011 [DOI] [PubMed] [Google Scholar]
- Gao W., Stalder T., Foley P., Rauh M., Deng H., Kirschbaum C. (2013). Quantitative analysis of steroid hormones in human hair using a column-switching LC–APCI–MS/MS assay. J. Chrom. B. 928, 1–8. 10.1016/j.jchromb.2013.03.008 [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S., Hegewald J., Seidler A., Nübling M., Espinola-Klein C., Liebers F., et al. (2016). The Gutenberg health study: associations between occupational and private stress factors and work-privacy conflict. BMC Publ. Health 16, 192. 10.1186/s12889-016-2881-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garthus-Niegel S., Horsch A., Ayers S., Junge-Hoffmeister J., Weidner K., Eberhard-Gran M. (2018). The influence of postpartum PTSD on breastfeeding: a longitudinal population-based study. Birth 45, 193–201. 10.1111/birt.12328 [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S., Knoph C., von Soest T., Nielsen C. S., Eberhard-Gran M. (2014). The role of labor pain and overall birth experience in the development of posttraumatic stress symptoms: a longitudinal cohort study. Birth 41, 108–115. 10.1111/birt.12093 [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S., von Soest T., Vollrath M. E., Eberhard-Gran M. (2013). The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Arch. Wom. Ment. Health 16, 1–10. 10.1007/s00737-012-0301-3 [DOI] [PubMed] [Google Scholar]
- Gemeinsamer Bundesausschuss (2015). Mutterpass. Richtlinien über die ärztliche Betreuung während der Schwangerschaft und nach der Entbindung: Mutterschafts-Richtlinien. Berlin. [Google Scholar]
- Gemeinsamer Bundesausschuss (2016). Kinder-Untersuchungsheft. Richtlinien über die Früherkennung von Krankheiten bei Kindern bis zur Vollendung des 6. Lebensjahres: Kinder-Richtlinien. [Google Scholar]
- Gentile S. (2017). Untreated depression during pregnancy: short-and long-term effects in offspring. A systematic review. Neuroscience 342, 154–166. 10.1016/j.neuroscience.2015.09.001 [DOI] [PubMed] [Google Scholar]
- Gerardi M., Rothbaum B. O., Astin M. C., Kelley M. (2010). Cortisol response following exposure treatment for PTSD in rape victims. J. Aggress. Maltreat. Trauma 19, 349–356. 10.1080/10926771003781297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- German National Cohort Consortium (2014). The German National Cohort: aims, study design and organization. Eur. J. Epidemiol. 29, 371–382. 10.1007/s10654-014-9890-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibaud-Wattston I., Wandersman L. P. (1978). Development and Utility of the Porenting Sense of Competence Scale. Paper presented at the meeting of the American Psychological Association, Toronto.
- Gjestland K., Bø K., Owe K. M., Eberhard-Gran M. (2013). Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. Br. J. Sports Med. 47, 515–520. 10.1136/bjsports-2012-091344 [DOI] [PubMed] [Google Scholar]
- Glaser B. G., Strauss A. L. (1967). Discovery of Grounded Theory: Strategies for Qualitative Research. Piscataway, NJ: Transaction. [Google Scholar]
- Goode W. J. (1960). A theory of role strain. Am. Sociol. Rev. 25, 483–496. 10.2307/2092933 [DOI] [Google Scholar]
- Grant K. A., McMahon C., Austin M. P., Reilly N., Leader L., Ali S. (2009). Maternal prenatal anxiety, postnatal caregiving and infants' cortisol responses to the still-face procedure. Dev. Psychobiol. 51, 625–637. 10.1002/dev.20397 [DOI] [PubMed] [Google Scholar]
- Grassi-Oliveira R., Pezzi J. C., Daruy-Filho L., Viola T. W., Francke I. D. A., Leite C. E., et al. (2012). Hair cortisol and stressful life events retrospective assessment in crack cocaine users. Am. J. Drug Alcohol Abuse 38, 535–538. 10.3109/00952990.2012.694538 [DOI] [PubMed] [Google Scholar]
- Griesel D., Wessa M., Flor H. (2006). Psychometric qualities of the German version of the Posttraumatic Diagnostic Scale (PTDS). Psychol. Assess. 18, 262–268. 10.1037/1040-3590.18.3.262 [DOI] [PubMed] [Google Scholar]
- Grossi G., Perski A., Lundberg U., Soares J. (2001). Associations between financial strain and the diurnal salivary cortisol secretion of long-term unemployed individuals. Integr. Physiol. Behav. Sci. 36, 205–219. 10.1007/BF02734094 [DOI] [PubMed] [Google Scholar]
- Gunnar M. R., Donzella B. (2002). Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 27, 199–220. 10.1016/S0306-4530(01)00045-2 [DOI] [PubMed] [Google Scholar]
- Gustavson K., von Soest T., Karevold E., Røysamb E. (2012). Attrition and generalizability in longitudinal studies: findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Publ. Health 12:918. 10.1186/1471-2458-12-918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines H., Pallant J. F., Karlström A., Hildingsson I. (2011). Cross-cultural comparison of levels of childbirth-related fear in an Australian and Swedish sample. Midwifery 27, 560–567. 10.1016/j.midw.2010.05.004 [DOI] [PubMed] [Google Scholar]
- Hall S. S., MacDermid S. M. (2009). A typology of dual earner marriages based on work and family arrangements. J. Family Econom. Issues 30, 215–225. 10.1007/s10834-009-9156-9 [DOI] [Google Scholar]
- Hanington L., Heron J., Stein A., Ramchandani P. (2012). Parental depression and child outcomes–is marital conflict the missing link? Child Care Health Dev. 38, 520–529. 10.1111/j.1365-2214.2011.01270.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P. A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J. G. (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins A. J., Marshall C. M., Allen S. M. (1998). The orientation toward domestic labor questionnaire: exploring dual-earner wives' sense of fairness about family work. J. Fam. Psychol. 12, 244–258. 10.1037/0893-3200.12.2.244 [DOI] [Google Scholar]
- Helms H. M., Walls J. K., Crouter A. C., McHale S. M. (2010). Provider role attitudes, marital satisfaction, role overload, and housework: a dyadic approach. J. Fam. Psychol. 24, 568–577. 10.1037/a0020637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmi M. H., Wolke D., Schneider S. (2011). Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Arch. Dis. Child. 96, 622–629. 10.1136/adc.2010.191312 [DOI] [PubMed] [Google Scholar]
- Herr R. M., Barrech A., Gündel H., Lang J., Quinete N. S., Angerer P., et al. (2017). Effects of psychosocial work characteristics on hair cortisol – findings from a post-trial study. Stress 20, 363–370. 10.1080/10253890.2017.1340452 [DOI] [PubMed] [Google Scholar]
- Hinkelmann K., Muhtz C., Dettenborn L., Agorastos A., Wingenfeld K., Spitzer C., et al. (2013). Association between childhood trauma and low hair cortisol in depressed patients and healthy control subjects. Biol. Psychiatry 74, e15–e17. 10.1016/j.biopsych.2013.04.021 [DOI] [PubMed] [Google Scholar]
- Hoffman M. C., D'Anna-Hernandez K., Benitez P., Ross R. G., Laudenslager M. L. (2017). Cortisol during human fetal life: Characterization of a method for processing small quantities of newborn hair from 26 to 42 weeks gestation. Dev. Psychobiol. 59, 123–127. 10.1002/dev.21433 [DOI] [PubMed] [Google Scholar]
- Hoffman M. C., Mazzoni S. E., Wagner B. D., Laudenslager M. L. (2016). Measures of maternal stress and mood in relation to preterm birth. Obstet. Gynecol. 127, 545–552. 10.1097/AOG.0000000000001287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollanders J. J., van der Voorn B., Kieviet N., Dolman K. M., de Rijke Y. B., van den Akker E. L. T., et al. (2017). Interpretation of glucocorticoids in neonatal hair: a reflection of intrauterine glucocorticoid regulation? Endocr. Connect. 6, 692–699. 10.1530/EC-17-0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IQTIG–Institut für Qualitätssicherung und Transparenz im Gesundheitswesen (2018). Bundesauswertung zum Erfassungsjahr 2017. Geburtshilfe. Qualitätsindikatoren. Berlin. [Google Scholar]
- Janssens H., Clays E., Fiers T., Verstraete A., De Bacquer D., Braeckman L. (2017). Hair cortisol in relation to job stress and depressive symptoms. Occup. Med. 67, 114–120. 10.1093/occmed/kqw114 [DOI] [PubMed] [Google Scholar]
- Jaursch S., Lösel F. (2011). Mütterliche Berufstätigkeit und kindliches Sozialverhalten. Kindheit Entwicklung 20, 164–172. 10.1026/0942-5403/a000052 [DOI] [Google Scholar]
- Johnston C., Mash E. J. (1989). A measure of parenting satisfaction and efficacy. J. Clin. Child Psychol. 18, 167–175. 10.1207/s15374424jccp1802_8 [DOI] [Google Scholar]
- Johnstone J. F., Bocking A. D., Unlugedik E., Challis J. R. G. (2005). The effects of chorioamnionitis and betamethasone on 11β, hydroxysteroid dehydrogenase types 1 and 2 and the glucocorticoid receptor in preterm human placenta. J. Soc. Gynecol. Investig. 12, 238–245. 10.1016/j.jsgi.2005.01.029 [DOI] [PubMed] [Google Scholar]
- Junge C., von Soest T., Weidner K., Seidler A., Eberhard-Gran M., Garthus-Niegel S. (2018). Labor pain in women with and without severe fear of childbirth: a population-based, longitudinal study. Birth 2018, 1–9. 10.1111/birt.12349 [DOI] [PubMed] [Google Scholar]
- Karlén J., Frostell A., Theodorsson E., Faresjö T., Ludvigsson J. (2013). Maternal influence on child HPA axis: a prospective study of cortisol levels in hair. Pediatrics 2013, e1333–e1340. 10.1542/peds.2013-1178 [DOI] [PubMed] [Google Scholar]
- Karlén J., Ludvigsson J., Frostell A., Theodorsson E., Faresjö T. (2011). Cortisol in hair measured in young adults-a biomarker of major life stressors? BMC Clin. Pathol. 11:1. 10.1186/1472-6890-11-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlén J., Ludvigsson J., Hedmark M., Faresjö Å., Theodorsson E., Faresjö T. (2015). Early psychosocial exposures, hair cortisol levels, and disease risk. Pediatrics 2015, e1450–e1457. 10.1542/peds.2014-2561 [DOI] [PubMed] [Google Scholar]
- Kirschbaum C., Tietze A., Skoluda N., Dettenborn L. (2009). Hair as a retrospective calendar of cortisol production—increased cortisol incorporation into hair in the third trimester of pregnancy. Psychoneuroendocrinology 34, 32–37. 10.1016/j.psyneuen.2008.08.024 [DOI] [PubMed] [Google Scholar]
- Kliem S., Job A.-K., Kröger C., Bodenmann G., Stöbel-Richter Y., Hahlweg K., et al. (2012). Entwicklung und Normierung einer Kurzform des Partnerschaftsfragebogens (PFB-K) an einer repräsentativen deutschen Stichprobe. Z. Klin. Psychol. Psychother. 41, 81–89. 10.1026/1616-3443/a000135 [DOI] [Google Scholar]
- Klumb P. L., Lampert T. (2004). Women, work, and well-being 1950–2000:: a review and methodological critique. Soc. Sci. Med. 58, 1007–1024. 10.1016/S0277-9536(03)00262-4 [DOI] [PubMed] [Google Scholar]
- Kristensen T. S., Hannerz H., Høgh A., Borg V. (2005). The Copenhagen Psychosocial Questionnaire-a tool for the assessment and improvement of the psychosocial work environment. Scand. J. Work. Environ. Health 31, 438–449. 10.5271/sjweh.948 [DOI] [PubMed] [Google Scholar]
- Kuehl L. K., Hinkelmann K., Muhtz C., Dettenborn L., Wingenfeld K., Spitzer C., et al. (2015). Hair cortisol and cortisol awakening response are associated with criteria of the metabolic syndrome in opposite directions. Psychoneuroendocrinology 51, 365–370. 10.1016/j.psyneuen.2014.09.012 [DOI] [PubMed] [Google Scholar]
- Kvale S. (1996). InterViews: An Introduction to Qualitative Research Interviewing. Thousand Oaks, CA: Sage. [Google Scholar]
- Li C.-Y., Sung F.-C. (1999). A review of the healthy worker effect in occupational epidemiology. Occup. Med. 49, 225–229. 10.1093/occmed/49.4.225 [DOI] [PubMed] [Google Scholar]
- Liang G., Chen M., Pan X.l., Zheng J., Wang H. (2011). Ethanol-induced inhibition of fetal hypothalamic–pituitary–adrenal axis due to prenatal overexposure to maternal glucocorticoid in mice. Exp. Toxicol. Pathol. 63, 607–611. 10.1016/j.etp.2010.04.015 [DOI] [PubMed] [Google Scholar]
- Liu C. H., Phan J., Yasui M., Doan S. (2018). Prenatal life events, maternal employment, and postpartum depression across a diverse population in New York City. Community Ment. Health J. 54, 1–10. 10.1007/s10597-017-0171-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas-Thompson R. G., Goldberg W. A., Prause J. (2010). Maternal work early in the lives of children and its distal associations with achievement and behavior problems: a meta-analysis. Psychol. Bull. 136, 915–942. 10.1037/a0020875 [DOI] [PubMed] [Google Scholar]
- Maercker A., Schützwohl M. (1998). Erfassung von psychischen belastungsfolgen: die impact of event skala-revidierte version (IES-R). Diagnostica 44, 130–141. 10.1037/t55092-000 [DOI] [Google Scholar]
- Maier R., Egger A., Barth A., Winker R., Osterode W., Kundi M., et al. (2006). Effects of short-and long-term unemployment on physical work capacity and on serum cortisol. Int. Arch. Occup. Environ. Health 79, 193–198. 10.1007/s00420-005-0052-9 [DOI] [PubMed] [Google Scholar]
- Malterud K., Siersma V. D., Guassora A. D. (2016). Sample size in qualitative interview studies: guided by information power. Qual. Health Res. 26, 1753–1760. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- Manenschijn L., Schaap L., van Schoor N. M., van der Pas S., Peeters G. M. E. E., Lips P. T. A. M., et al. (2013). High long-term cortisol levels, measured in scalp hair, are associated with a history of cardiovascular disease. J. Clin. Endocrinol. Metab. 98, 2078–2083. 10.1210/jc.2012-3663 [DOI] [PubMed] [Google Scholar]
- Manenschijn L., Spijker A. T., Koper J. W., Jetten A. M., Giltay E. J., Haffmans J., et al. (2012). Long-term cortisol in bipolar disorder: associations with age of onset and psychiatric co-morbidity. Psychoneuroendocrinology 37, 1960–1968. 10.1016/j.psyneuen.2012.04.010 [DOI] [PubMed] [Google Scholar]
- Manenschijn L., van Kruysbergen R. G., de Jong F. H., Koper J. W., van Rossum E. F. (2011). Shift work at young age is associated with elevated long-term cortisol levels and body mass index. J. Clin. Endocrinol. Metab. 96, E1862–E1865. 10.1210/jc.2011-1551 [DOI] [PubMed] [Google Scholar]
- Marks S. R. (1977). Multiple roles and role strain: Some notes on human energy, time and commitment. Am. Sociol. Rev. 42, 921–936. 10.2307/2094577 [DOI] [Google Scholar]
- Masterson C. R., Hoobler J. M. (2015). Care and career: a family identity-based typology of dual-earner couples. J. Organ. Behav. 36, 75–93. 10.1002/job.1945 [DOI] [Google Scholar]
- Mayring P. (2010). Qualitative Inhaltsanalyse. Grundlagen und Techniken. Weinheim: Beltz Verlag; 10.1007/978-3-531-92052-8_42 [DOI] [Google Scholar]
- Miani C., Hoorens S. (2014). Parents at Work: Men and Women Participating in the Labour Force. Short Statistical Report No. 2 [Online]. Available online at: https://www.rand.org/pubs/research_reports/RR348.html (accessed September 9, 2018).
- Miller Y. (2001). Erziehung von Kindern im Kindergartenalter: Erziehungsverhalten und Kompetenzüberzeugungen von Eltern und der Zusammenhang zu Kindlichen Verhaltensstörungen [dissertation]. Technische Universität Carolo-Wilhelmina zu Braunschweig. [Google Scholar]
- Morse J. M. (1994). Designing funded qualitative research, in Handbook of Qualitative Research, eds Denizin N. K., Lincoln Y.S. (Thousand Oaks, CA: Sage, 220–235. [Google Scholar]
- Mustonen P., Karlsson L., Scheinin N. M., Kortesluoma S., Coimbra B., Rodrigues A. J., et al. (2018). Hair cortisol concentration (HCC) as a measure for prenatal psychological distress—a systematic review. Psychoneuroendocrinology 92, 21–28. 10.1016/j.psyneuen.2018.03.019 [DOI] [PubMed] [Google Scholar]
- Muthén B., Asparouhov T. (2002). Using Mplus Monte Carlo simulations in Practice: A Note on Non-normal Missing Data in Latent Variable Models. Mplus Web Notes: No. 2 [Online]. Available online at: http://www.statmodel.com/download/webnotes/mc2.pdf (accessed September 9, 2018).
- Nordeng H., Hansen C., Garthus-Niegel S., Eberhard-Gran M. (2012). Fear of childbirth, mental health, and medication use during pregnancy. Arch. Wom. Ment. Health 15, 203–209. 10.1007/s00737-012-0278-y [DOI] [PubMed] [Google Scholar]
- Nübling M., Stößel U., Hasselhorn H.-M., Michaelis M., Hofmann F. (2005). Methoden zur Erfassung psychischer Belastungen. Erprobung eines Messinstruments (COPSOQ). Bremerhaven. [Google Scholar]
- Ockenfels M. C., Porter L., Smyth J., Kirschbaum C., Hellhammer D. H., Stone A. A. (1995). Effect of chronic stress associated with unemployment on salivary cortisol: overall cortisol levels, diurnal rhythm, and acute stress reactivity. Psychosom. Med. 57, 460–467. 10.1097/00006842-199509000-00008 [DOI] [PubMed] [Google Scholar]
- O'Donnell K. J., Jensen A. B., Freeman L., Khalife N., O'Connor T. G., Glover V. (2012). Maternal prenatal anxiety and downregulation of placental 11β-HSD2. Psychoneuroendocrinology 37, 818–826. 10.1016/j.psyneuen.2011.09.014 [DOI] [PubMed] [Google Scholar]
- Olff M., de Vries G.-J., Güzelcan Y., Assies J., Gersons B. P. R. (2007). Changes in cortisol and DHEA plasma levels after psychotherapy for PTSD. Psychoneuroendocrinology 32, 619–626. 10.1016/j.psyneuen.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Pacella M. L., Feeny N., Zoellner L., Delahanty D. L. (2014). The impact of ptsd treatment on the cortisol awakening response. Depress. Anxiety 31, 862–869. 10.1002/da.22298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer F. B., Anand K. J. S., Graff J. C., Murphy L. E., Qu Y., Völgyi E., et al. (2013). Early adversity, socioemotional development, and stress in urban 1-year-old children. J. Pediatr. 163, 1733–1739. 10.1016/j.jpeds.2013.08.030 [DOI] [PubMed] [Google Scholar]
- Parfitt Y., Pike A., Ayers S. (2014). Infant developmental outcomes: a family systems perspective. Infant Child Dev. 23, 353–373. 10.1002/icd.1830 [DOI] [Google Scholar]
- Pauli-Pott U., Ries-Hahn A., Kupfer J., Beckmann D. (1999). Konstruktion eines Fragebogens zur Erfassung des frühkindlichen Temperaments im Elternurteil-Ergebnisse für den Altersbereich drei bis vier Monate. Prax. Kinderpsychol. Kinderpsychiatr. 48, 231–246. [PubMed] [Google Scholar]
- Pearson R. M., Evans J., Kounali D., Lewis G., Heron J., Ramchandani P. G., et al. (2013). Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry 70, 1312–1319. 10.1001/jamapsychiatry.2013.2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereg D., Gow R., Mosseri M., Lishner M., Rieder M., Van Uum S., et al. (2011). Hair cortisol and the risk for acute myocardial infarction in adult men. Stress 14, 73–81. 10.3109/10253890.2010.511352 [DOI] [PubMed] [Google Scholar]
- Pervanidou P., Agorastos A., Kolaitis G., Chrousos G. P. (2017). Neuroendocrine responses to early life stress and trauma and susceptibility to disease. Eur. J. Psychotraumatol. 8:1351218 10.1080/20008198.2017.1351218 [DOI] [Google Scholar]
- Petermann U., Reinartz H., Petermann F. (2002). IDL 0-2: Ein Explorationsbogen zur Identifikation differentieller Lernwege in der Sozialentwicklung. Z. Klin. Psychol. Psychiatr. Psychother. 50, 427–457. Available online at: https://www.researchgate.net/publication/272415513_IDL_0-2_Ein_Explorationsbogen_zur_Identifikation_differentieller_Lernwege_in_der_Sozialentwicklung (accessed May 4, 2019). [Google Scholar]
- Petzoldt J., Wittchen H. U., Einsle F., Martini J. (2016). Maternal anxiety versus depressive disorders: specific relations to infants' crying, feeding and sleeping problems. Child Care Health Dev. 42, 231–245. 10.1111/cch.12292 [DOI] [PubMed] [Google Scholar]
- Philpott L. F., Fitzgerald S., Leahy-Warren P., Savage E. (2017). Stress in fathers in the perinatal period: a systematic review. Midwifery 55, 113–127. 10.1016/j.midw.2017.09.016 [DOI] [PubMed] [Google Scholar]
- Popp L., Fuths S., Seehagen S., Bolten M., Gross-Hemmi M., Wolke D., et al. (2016). Inter-rater reliability and acceptance of the structured diagnostic interview for regulatory problems in infancy. Child Adolesc. Psychiatr. Ment. Health 10, 21. 10.1186/s13034-016-0107-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Räikkönen K., Seckl J. R., Pesonen A.-K., Simons A., Van den Bergh B. R. H. (2011). Stress, glucocorticoids and liquorice in human pregnancy: programmers of the offspring brain. Stress 14, 590–603. 10.3109/10253890.2011.602147 [DOI] [PubMed] [Google Scholar]
- Ramchandani P., Stein A., Evans J., O'Connor T. G., Team A. S. (2005). Paternal depression in the postnatal period and child development: a prospective population study. Lancet 365, 2201–2205. 10.1016/S0140-6736(05)66778-5 [DOI] [PubMed] [Google Scholar]
- Ramchandani P. G., Domoney J., Sethna V., Psychogiou L., Vlachos H., Murray L. (2013). Do early father–infant interactions predict the onset of externalising behaviours in young children? Findings from a longitudinal cohort study. J. Child Psychol. Psychatry 54, 56–64. 10.1111/j.1469-7610.2012.02583.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reck C., Klier C. M., Pabst K., Stehle E., Steffenelli U., Struben K., et al. (2006). The German version of the Postpartum Bonding Instrument: psychometric properties and association with postpartum depression. Arch. Wom. Ment. Health 9, 265–271. 10.1007/s00737-006-0144-x [DOI] [PubMed] [Google Scholar]
- Rödel A., Siegrist J., Hessel A., Brähler E. (2004). Fragebogen zur Messung beruflicher Gratifikationskrisen. J. Indiv. Differ. 25, 227–238. 10.1024/0170-1789.25.4.227 [DOI] [Google Scholar]
- Romero-Gonzalez B., Caparros-Gonzalez R. A., Gonzalez-Perez R., Delgado-Puertas P., Peralta-Ramirez M. I. (2018). Newborn infants' hair cortisol levels reflect chronic maternal stress during pregnancy. PLoS ONE 13:e0200279. 10.1371/journal.pone.0200279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart M. K. (1981). Measurement of temperament in infancy. Child Dev. 52, 569–578. 10.2307/1129176 [DOI] [Google Scholar]
- Russell E., Koren G., Rieder M., Van Uum S. (2012). Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology 37, 589–601. 10.1016/j.psyneuen.2011.09.009 [DOI] [PubMed] [Google Scholar]
- Sauvé B., Koren G., Walsh G., Tokmakejian S., Van Uum S. H. M. (2007). Measurement of cortisol in human hair as a biomarker of systemic exposure. Clin. Investig. Med. 30, 183–191. 10.25011/cim.v30i5.2894 [DOI] [PubMed] [Google Scholar]
- Schafer J. L., Graham J. W. (2002). Missing data: our view of the state of the art. Psychol. Methods 7, 147–177. 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Schober P. S., Zoch G. (2015). Kürzere Elternzeit von Müttern: gleichmäßigere Aufteilung der Familienarbeit? DIW Wochenbericht 82, 1190–1196. Available online at: http://hdl.handle.net/10419/125498 (accessed May 4, 2019). [Google Scholar]
- Schreier H. M., Enlow M. B., Ritz T., Coull B. A., Gennings C., Wright R. O., et al. (2016). Lifetime exposure to traumatic and other stressful life events and hair cortisol in a multi-racial/ethnic sample of pregnant women. Stress 19, 45–52. 10.3109/10253890.2015.1117447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreier H. M., Enlow M. B., Ritz T., Gennings C., Wright R. J. (2015). Childhood abuse is associated with increased hair cortisol levels among urban pregnant women. J. Epidemiol. Commun. Health 69, 1169–1174. 10.1136/jech-2015-205541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher S., Niemeyer H., Engel S., Cwik J. C., Knaevelsrud C. (2018). Psychotherapeutic treatment and HPA axis regulation in posttraumatic stress disorder: A systematic review and meta-analysis. Psychoneuroendocrinology 98, 186–201. 10.1016/j.psyneuen.2018.08.006 [DOI] [PubMed] [Google Scholar]
- Schupp J., Gerlitz J.-Y. (2008). BFI-S: big five inventory-SOEP, in Zusammenstellung Sozialwissenschaftlicher Items und Skalen. ZIS Version, ed Glöckner-Rist A. (Bonn: Gesis; ). [Google Scholar]
- Schwab-Reese L. M., Ramirez M., Ashida S., Peek-Asa C. (2017). Psychosocial employment characteristics and postpartum maternal mental health symptoms. Am. J. Ind. Med. 60, 109–120. 10.1002/ajim.22666 [DOI] [PubMed] [Google Scholar]
- Shah D. (2009). Healthy worker effect phenomenon. Indian J. Occup. Environ. Med. 13, 77–79. 10.4103/0019-5278.55123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short S. J., Stalder T., Marceau K., Entringer S., Moog N. K., Shirtcliff E. A., et al. (2016). Correspondence between hair cortisol concentrations and 30-day integrated daily salivary and weekly urinary cortisol measures. Psychoneuroendocrinology 71, 12–18. 10.1016/j.psyneuen.2016.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieber S. D. (1974). Toward a theory of role accumulation. Am. Sociol. Rev. 39, 567–578. 10.2307/2094422 [DOI] [Google Scholar]
- Siegrist J. (1996). Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1, 27–41. 10.1037/1076-8998.1.1.27 [DOI] [PubMed] [Google Scholar]
- Siegrist J., Li J. (2017). Work stress and altered biomarkers: a synthesis of findings based on the effort–reward imbalance model. Int. J. Environ. Res. Public Health 14:1373. 10.3390/ijerph14111373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N., Roberts A. L., LeWinn K. Z., Bush N. R., Rovnaghi C. R., Tylavsky F., et al. (2018). Maternal experiences of trauma and hair cortisol in early childhood in a prospective cohort. Psychoneuroendocrinology 98, 168–176. 10.1016/j.psyneuen.2018.08.027 [DOI] [PubMed] [Google Scholar]
- Søgaard A. J., Selmer R., Bjertness E., Thelle D. (2004). The Oslo Health Study: The impact of self-selection in a large, population-based survey. Int. J. Equity Health 3:3. 10.1186/1475-9276-3-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires J., Bricker D. (2009). Ages and Stages Questionnaires (ASQ-3). A Parent-Completed Child Monitoring System. Baltimore, MD: Paul H Brookes Publishing. [Google Scholar]
- Stadlmayr W., Bitzer J., Hösli I., Amsler F., Leupold J., Schwendke-Kliem A., et al. (2001). Birth as a multidimensional experience: comparison of the English-and German-language versions of Salmon's Item List. J. Psychosom. Obstet. Gynecol. 22, 205–214. 10.3109/01674820109049975 [DOI] [PubMed] [Google Scholar]
- Stalder T., Kirschbaum C. (2012). Analysis of cortisol in hair–state of the art and future directions. Brain. Behav. Immun. 26, 1019–1029. 10.1016/j.bbi.2012.02.002 [DOI] [PubMed] [Google Scholar]
- Stalder T., Kirschbaum C., Alexander N., Bornstein S. R., Gao W., Miller R., et al. (2013). Cortisol in hair and the metabolic syndrome. J. Clin. Endocrinol. Metab. 98, 2573–2580. 10.1210/jc.2013-1056 [DOI] [PubMed] [Google Scholar]
- Stalder T., Steudte-Schmiedgen S., Alexander N., Klucken T., Vater A., Wichmann S., et al. (2017). Stress-related and basic determinants of hair cortisol in humans: a meta-analysis. Psychoneuroendocrinology 77, 261–274. 10.1016/j.psyneuen.2016.12.017 [DOI] [PubMed] [Google Scholar]
- Stalder T., Tietze A., Steudte S., Alexander N., Dettenborn L., Kirschbaum C. (2014). Elevated hair cortisol levels in chronically stressed dementia caregivers. Psychoneuroendocrinology 47, 26–30. 10.1016/j.psyneuen.2014.04.021 [DOI] [PubMed] [Google Scholar]
- Statistisches Bundesamt (2015). Gesundheit in Deutschland. Wiesbaden: Destatis. [Google Scholar]
- Statistisches Bundesamt (2018a). Bevölkerung und Erwerbstätigkeit. Erwerbsbeteiligung der Bevölkerung. Ergebnisse des Mikrozensus zum Arbeitsmarkt 2017 [Online]. Available online at: https://www.destatis.de/DE/Publikationen/Thematisch/Arbeitsmarkt/Erwerbstaetige/ErwerbsbeteiligungBevoelkung.html (accessed October 23, 2018).
- Statistisches Bundesamt (2018b). Bildungsstand der Bevölkerung. Ergebnisse des Mikrozensus 2017 [Online]. Available online at: https://www.destatis.de/DE/Publikationen/Thematisch/BildungForschungKultur/Bildungsstand/BildungsstandBevoelkerung.html (accessed October 23, 2018).
- Statistisches Bundesamt (2018c). Krankenhausstatistik - Grunddaten der Krankenhäuser und Vorsorge- oder Rehabilitationseinrichtungen [Online]. Available online at: https://www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Gesundheit/Krankenhaeuser/Tabellen/KrankenhausentbindeungenKaiserschnitt.html (accessed November 12, 2018).
- Statistisches Bundesamt (2018d). Lebendgeborene Bundesländer [Online]. Available online at: https://www-genesis.destatis.de/genesis/online/logon?language=deandsequenz=tabelleErgebnisandselectionname=12612-0100 (accessed November 12, 2018).
- Statistisches Landesamt Sachsen (2018). Mikrozensusergebnisse: Bevölkerung nach Schulabschluss und Berufsabschluss [Online]. Available online at: http://www.dresden.de/de/leben/stadtportrait/statistik/bevoelkerung-gebiet/mikrozensus.php (accessed October 23, 2018).
- Staufenbiel S. M., Koenders M. A., Giltay E. J., Elzinga B. M., Manenschijn L., Hoencamp E., et al. (2014). Recent negative life events increase hair cortisol concentrations in patients with bipolar disorder. Stress 17, 451–459. 10.3109/10253890.2014.968549 [DOI] [PubMed] [Google Scholar]
- Staufenbiel S. M., Penninx B. W., Spijker A. T., Elzinga B. M., van Rossum E. F. (2013). Hair cortisol, stress exposure, and mental health in humans: a systematic review. Psychoneuroendocrinology 38, 1220–1235. 10.1016/j.psyneuen.2012.11.015 [DOI] [PubMed] [Google Scholar]
- Stein A., Pearson R. M., Goodman S. H., Rapa E., Rahman A., McCallum M., et al. (2014). Effects of perinatal mental disorders on the fetus and child. Lancet 384, 1800–1819. 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- Steudte S., Kirschbaum C., Gao W., Alexander N., Schönfeld S., Hoyer J., et al. (2013). Hair cortisol as a biomarker of traumatization in healthy individuals and posttraumatic stress disorder patients. Biol. Psychiatry 74, 639–646. 10.1016/j.biopsych.2013.03.011 [DOI] [PubMed] [Google Scholar]
- Steudte S., Stalder T., Dettenborn L., Klumbies E., Foley P., Beesdo-Baum K., et al. (2011). Decreased hair cortisol concentrations in generalised anxiety disorder. Psychiatry Res. 186, 310–314. 10.1016/j.psychres.2010.09.002 [DOI] [PubMed] [Google Scholar]
- Steudte-Schmiedgen S., Kirschbaum C., Alexander N., Stalder T. (2016). An integrative model linking traumatization, cortisol dysregulation and posttraumatic stress disorder: Insight from recent hair cortisol findings. Neurosci. Biobehav. Rev. 69, 124–135. 10.1016/j.neubiorev.2016.07.015 [DOI] [PubMed] [Google Scholar]
- Steudte-Schmiedgen S., Stalder T., Schönfeld S., Wittchen H.-U., Trautmann S., Alexander N., et al. (2015). Hair cortisol concentrations and cortisol stress reactivity predict PTSD symptom increase after trauma exposure during military deployment. Psychoneuroendocrinology 59, 123–133. 10.1016/j.psyneuen.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Steudte-Schmiedgen S., Wichmann S., Stalder T., Hilbert K., Muehlhan M., Lueken U., et al. (2017). Hair cortisol concentrations and cortisol stress reactivity in generalized anxiety disorder, major depression and their comorbidity. J. Psychiatr. Res. 84, 184–190. 10.1016/j.jpsychires.2016.09.024 [DOI] [PubMed] [Google Scholar]
- Sumner R. C., Gallagher S. (2017). Unemployment as a chronic stressor: A systematic review of cortisol studies. Psychol. Health 32, 289–311. 10.1080/08870446.2016.1247841 [DOI] [PubMed] [Google Scholar]
- Swales D. A., Stout-Oswald S. A., Glynn L. M., Sandman C., Wing D. A., Davis E. P. (2018). Exposure to traumatic events in childhood predicts cortisol production among high risk pregnant women. Biol. Psychol. 139, 186–192. 10.1016/j.biopsycho.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney S., MacBeth A. (2016). The effects of paternal depression on child and adolescent outcomes: a systematic review. J. Affect. Disord. 205, 44–59. 10.1016/j.jad.2016.05.073 [DOI] [PubMed] [Google Scholar]
- Tarullo A. R., John A. M. S., Meyer J. S. (2017). Chronic stress in the mother-infant dyad: Maternal hair cortisol, infant salivary cortisol and interactional synchrony. Infant Behav. Dev. 47, 92–102. 10.1016/j.infbeh.2017.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson R. M., Allely C. S., Purves D., Puckering C., McConnachie A., Johnson P. C., et al. (2014). Predictors of positive and negative parenting behaviours: evidence from the ALSPAC cohort. BMC Pediatr. 14:247. 10.1186/1471-2431-14-247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmons A. C., Margolin G., Saxbe D. E. (2015). Physiological linkage in couples and its implications for individual and interpersonal functioning: a literature review. J. Fam. Psychol. 29:720. 10.1037/fam0000115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- TNS Infratest Sozialforschung (2016). SOEP 2016 – Erhebungsinstrumente 2016 (Welle 33) des Soziooekonomischen Panels: Personenfragebogen, Stichproben A-L3. SOEP Survey Papers 345: Series A. Berlin: DIW/SOEP. [Google Scholar]
- Tröster H. (2011). Eltern-Belastungs-Inventar (EBI); deutsche Version des Parenting Stress Index (PSI) von R. R. Abidin. Göttingen: Hogrefe. [Google Scholar]
- Vale C. D., Maurelli V. A. (1983). Simulating multivariate nonnormal distributions. Psychometrika 48, 465–471. 10.1007/BF02293687 [DOI] [Google Scholar]
- Van den Bergh B. R. H., van den Heuvel M. I., Lahti M., Braeken M., de Rooij S. R., Entringer S., et al. (2017). Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2017:003 10.1016/j.neubiorev.2017.07.003 [DOI] [PubMed] [Google Scholar]
- van der Meij L., Gubbels N., Schaveling J., Almela M., van Vugt M. (2018). Hair cortisol and work stress: importance of workload and stress model (JDCS or ERI). Psychoneuroendocrinology 89, 78–85. 10.1016/j.psyneuen.2017.12.020 [DOI] [PubMed] [Google Scholar]
- van Holland B. J., Frings-Dresen M. H. W., Sluiter J. K. (2012). Measuring short-term and long-term physiological stress effects by cortisol reactivity in saliva and hair. Int. Arch. Occup. Environ. Health 85, 849–852. 10.1007/s00420-011-0727-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vives A., González F., Moncada S., Llorens C., Benach J. (2015). Measuring precarious employment in times of crisis: the revised Employment Precariousness Scale (EPRES) in Spain. Gac. Sanit. 29, 379–382. 10.1016/j.gaceta.2015.06.008 [DOI] [PubMed] [Google Scholar]
- Wadhwa P. D., Entringer S., Buss C., Lu M. C. (2011). The contribution of maternal stress to preterm birth: issues and considerations. Clin. Perinatol. 38, 351–384. 10.1016/j.clp.2011.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J. E., Kosinski M., Dewey J. E., Gandek B. (2001). How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Lincoln, RI: QualityMetric Incorporated. [Google Scholar]
- Wei J., Sun G., Zhao L., Yang X., Liu X., Lin D., et al. (2015). Analysis of hair cortisol level in first-episodic and recurrent female patients with depression compared to healthy controls. J. Affect. Disord. 175, 299–302. 10.1016/j.jad.2015.01.023 [DOI] [PubMed] [Google Scholar]
- Weiss D. S., Marmar C. R. (1996). The impact of event scale - revised, in Assessing psychological trauma and PTSD, eds Wilson J. P., Keane T. M. (New York, NY: Guilford Press, 399–411. [Google Scholar]
- Wells A., Cartwright-Hatton S. (2004). A short form of the metacognitions questionnaire: properties of the MCQ-30. Behav. Res. Ther. 42, 385–396. 10.1016/S0005-7967(03)00147-5 [DOI] [PubMed] [Google Scholar]
- Wennig R. (2000). Potential problems with the interpretation of hair analysis results. Forensic Sci. Int. 107, 5–12. 10.1016/S0379-0738(99)00146-2 [DOI] [PubMed] [Google Scholar]
- Wester V. L., van Rossum E. F. C. (2015). Clinical applications of cortisol measurements in hair. Eur. J. Endocrinol. 2015, M1–M10. 10.1530/EJE-15-0313 [DOI] [PubMed] [Google Scholar]
- Wilson S., Durbin C. E. (2010). Effects of paternal depression on fathers' parenting behaviors: a meta-analytic review. Clin. Psychol. Rev. 30, 167–180. 10.1016/j.cpr.2009.10.007 [DOI] [PubMed] [Google Scholar]
- Wingenfeld K., Spitzer C., Mensebach C., Grabe H. J., Hill A., Gast U., et al. (2010). Die deutsche version des childhood trauma questionnaire (CTQ): erste befunde zu den psychometrischen Kennwerten. Psychother. Psych. Med. 60, 442–450. 10.1055/s-0030-1247564 [DOI] [PubMed] [Google Scholar]
- Wittchen H.-U., Wunderlich U., Gruschwitz S., Zaudig M. (1997). Strukturiertes klinisches Interview für DSM-IV. Achse I und II. Göttingen: Hogrefe. [Google Scholar]
- Witzel A., Reiter H. (2012). The Problem-Centred Interview. Principles and Practice. London: Sage; 10.4135/9781446288030 [DOI] [Google Scholar]
- Woltman H., Feldstain A., MacKay J. C., Rocchi M. (2012). An introduction to hierarchical linear modeling. Tutor. Quant. Methods Psychol. 8, 52–69. 10.20982/tqmp.08.1.p052 [DOI] [Google Scholar]
- World Health Organization (2009). Infant and Young Child Feeding. Model Chapter for Textbooks for Medical Students and Allied Health Professionals. France: World Health Organization. [PubMed] [Google Scholar]
- Wortmann-Fleischer S., von Einsiedel R., Downing G. (2012). Stationäre Eltern-Kind-Behandlung. Ein interdisziplinärer Leitfaden. Stuttgart: Kohlhammer. [Google Scholar]
- Yamada J., Stevens B., de Silva N., Gibbins S., Beyene J., Taddio A., et al. (2007). Hair cortisol as a potential biologic marker of chronic stress in hospitalized neonates. Neonatology 92, 42–49. 10.1159/000100085 [DOI] [PubMed] [Google Scholar]
- Yehuda R., Bierer L. M., Sarapas C., Makotkine I., Andrew R., Seckl J. R. (2009). Cortisol metabolic predictors of response to psychotherapy for symptoms of PTSD in survivors of the World Trade Center attacks on September 11, 2001. Psychoneuroendocrinology 34, 1304–1313. 10.1016/j.psyneuen.2009.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R., Engel S. M., Brand S. R., Seckl J., Marcus S. M., Berkowitz G. S. (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. J Clin Endocrinol Metab 90, 4115–4118. 10.1210/jc.2005-0550 [DOI] [PubMed] [Google Scholar]
- Yehuda R., Halligan S. L., Bierer L. M. (2002). Cortisol levels in adult offspring of Holocaust survivors: relation to PTSD symptom severity in the parent and child. Psychoneuroendocrinology 27, 171–180. 10.1016/S0306-4530(01)00043-9 [DOI] [PubMed] [Google Scholar]
- Yehuda R., Pratchett L. C., Elmes M. W., Lehrner A., Daskalakis N. P., Koch E., et al. (2014). Glucocorticoid-related predictors and correlates of post-traumatic stress disorder treatment response in combat veterans. Interface Focus 4:20140048. 10.1098/rsfs.2014.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.