Abstract
Background
The distribution of visual impairment is an indicator of the health status of the population and for the frequency of diseases of the eye.
Methods
The Gutenberg Health Study (GHS) is a population-based cohort study in Germany concerning adults aged 35 to 74. 15 010 subjects from the Mainz–Bingen region underwent general medical and ophthalmological examination, with measurement of the distance-corrected visual acuity in each eye separately. As per the World Health Organization criteria, visual impairment was defined as an acuity below 0.3 in the better eye, and blindness as an acuity below 0.05. All patients who were found to be visually impaired or blind underwent further individual study with clinical history-taking, split-lamp examination, and fundus photography.
Results
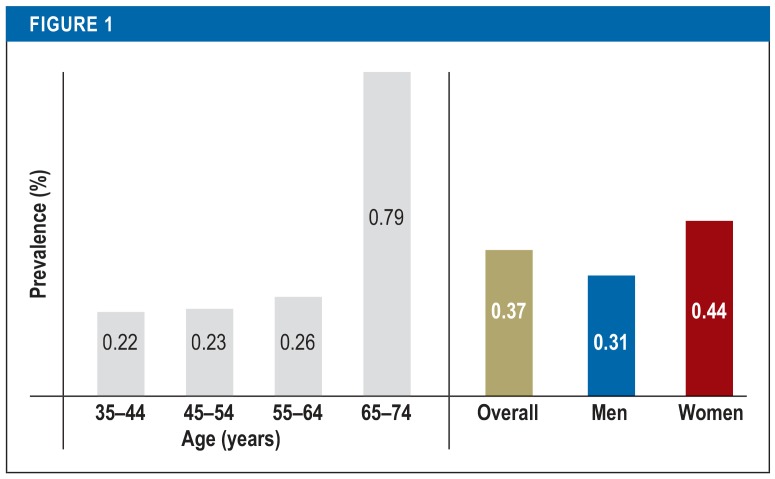
Data from 14 687 subjects were evaluated. The mean age of the participants was 55.0 years (standard deviation, 11.1 years). The prevalence of visual impairment was 0.37% (95% confidence interval [0.28; 0.49]) (n = 55) and was higher in women (0.44%) than in men (0.31%). Blindness was present in 0.05% [0.03; 0.11] (n = 8) of the subjects. The prevalence of visual impairment from age 65 onward was 0.79%, three times higher than in the younger age groups. 54.5% of the visually impaired subjects had multiple underlying ophthalmological pathologies.
Conclusion
The causes of visual impairment are manifold. Loss of vision is often the combined effect of multiple pathological factors. The etiology of visual impairment is thus a more complex matter than is commonly assumed.
Loss of the power of sight is a fundamentally life-changing event for the individuals affected and their families. That is not all, however; as the gravest endpoint of ocular diseases, blindness also says something about the underlying disease burden of the population. The prevalence of blindness and visual impairment thus represents an indicator of the general state of health.
The data from recent decades reveal certain trends in the distribution of blindness and visual impairment: The general prevalence of new cases of blindness has decreased, as have the avoidable causes of blindness (1). Happily, considerable reductions have been achieved, particularly in the rate of vision loss among young children (2). In contrast, however, the risk of visual impairment has increased for those with chronic and age-related diseases of the eye (3, 4).
The epidemiology of blindness and visual impairment is bound closely to demographic change. The number of elderly people in Germany will increase greatly in the foreseeable future, leading to a further rise in age-related ocular diseases and thus higher numbers of persons with vision loss (5– 7). In the recent past this development has been compensated by the fact that the relative risk of becoming blind has decreased (8– 10).
The predominant causes of blindness in the western industrialized nations in recent years have been age-related macular degeneration (AMD), glaucoma, and diabetic retinopathy (7, 11, 12). Globally, cataract has been the most frequently occurring reason for blindness (3, 13). To date, German studies of data from disease registries or records of allowances paid to the blind (14– 16) have assumed that vision loss is attributable to a single cause. Particularly in view of demographic changes, however, a more complex distribution of morbidity in the population must be assumed.
The aim of the population-based study presented here is to describe the prevalence of blindness and visual impairment in the adult German population and analyze the various reasons for loss of the power of sight.
Methods
The Gutenberg Health Study (GHS) is a population-based cohort study carried out in the Mainz–Bingen region of Germany. A total of 15 010 probands between 35 and 74 years of age were recruited at random from the register of residents in the period from 2007 to 2012. Ophthalmological examination was accompanied by general medical and psychological questionnaires. The structure and contents of the study have been described in detail elsewhere (17– 19).
All of the probands gave their written informed consent for participation in the study. The GHS adhered to the tenets of Good Clinical Practice (GCP) and Good Epidemiological Practice (GEP) and conformed to the ethical principles of the Declaration of Helsinki. The study was approved by the ethics committee of the State Medical Association, Rhineland–Palatinate.
The probands’ visual acuity (vision) was measured with the aid of a refractometer (Humphrey HARK 599, Carl Zeiss Meditec AG).
Visual acuity was measured for distance vision using automatic correction for refractive errors. In the case of results below 0.1, the acuity at a distance of 1 m was tested using a Snellen chart. If that was not possible, finger counting, hand movement, and light perception were tested. We followed the World Health Organization (WHO) definitions of visual impairment as visual acuity of <0.3 and blindness as visual acuity of <0.05.
The causes of visual impairment were investigated case by case on the basis of the participants’ statements regarding their medical history, together with standardized slit-lamp examination and inspection of fundus images by two independent investigators (CW, AKS). If they failed to achieve consensus, a third investigator (HME) was consulted. The following were defined a priori as possible causes:
AMD
Glaucoma
Diabetic retinopathy
Corneal disease
Genetic illnesses
Severe myopia
Cataract
Amblyopia
Other pathologies.
The cases were analyzed as to ocular diseases; if two or more diseases were present, each was counted. Subgroup analyses were conducted by sex, age group, and comorbidities. Socioeconomic status, defined by income, education, and occupation, was rated on a scale from 3 (lowest possible score) to 21 (highest possible score) in analogy with the German Health Update (GEDA) 2009 (20). Associations of visual impairment with age, sex, and socioeconomic status were tested using multiple logistic regression analysis. All statistical analyses were performed with the software R version 3.3.1 (21).
Results
A total of 14 687 probands were included in our analyses. They were selected to ensure even distribution by sex and among four 10-year age groups (table 1). No study data were available for the remaining 323 probands from the original study cohort of 15 010 probands.
Table 1. The study population of the Gutenberg Health Study (GHS) with measurement of visual acuity.
| Study participants | 14 685 |
| Men | 7413 (50.5%) |
| Women | 7274 (49.5%) |
| Mean age | 55.0 years ± 11.1 |
| 35–44 years | 3225 (22.0%) |
| 45–54 years | 3921 (26.7%) |
| 55–64 years | 3876 (26.4%) |
| 65–74 years | 3663 (24.9%) |
The prevalence of visual impairment in the GHS study population was 0.37% (n = 55; 95% confidence interval [0.28; 0.49]), while the prevalence of blindness (vision <0.05) was 0.05% (n = 8; [0.03; 0.11]).
There were striking differences among the age groups. The prevalence of both visual impairment and blindness was more than 3 times greater in probands aged 65 to 74 years than in the younger age groups (figure 1). Accordingly, logistic regression analysis showed a statistically signification association between higher age and visual impairment (odds ratio [OR] = 1.46; [1.12; 1.93]; per 10 years; p = 0.006). There was a noticeable, albeit nonsignificant, connection with lower socioeconomic status (OR = 0.92; [0.86; 0.99]; p = 0.012). Comparing the sexes, the prevalence of visual impairment was somewhat higher in women than in men, but this difference also did not attain statistical significance (OR = 1.23; [0.71; 2.16]; p = 0.45).
Figure 1.
Prevalence of visual impairment in the Gutenberg Health Study (GHS) by age and sex
With regard to the causes of visual impairment, AMD was distributed evenly between female and male study participants (21.9% versus 21.7%), whereas glaucoma was found more often in women than in men (12.5% versus 8.7%).
Accompanying amblyopia was found in 21.8% of probands with visual impairment, slightly more frequently in men than in women (26.1% versus 18.8%). The probands aged 65 to 74 years showed higher rates of both AMD (34.5% versus 7.7%) and cataract (31.0% versus 7.7%) than the younger age groups.
Among the eight probands with visual acuity of less than 0.05 (blindness), two had hereditary eye diseases, but none had diabetic retinopathy. Logistic regression analysis revealed no significant association with cardiovascular risk factors such as smoking or overweight or with arterial hypertension, lipid metabolism disorders, or diabetes mellitus.
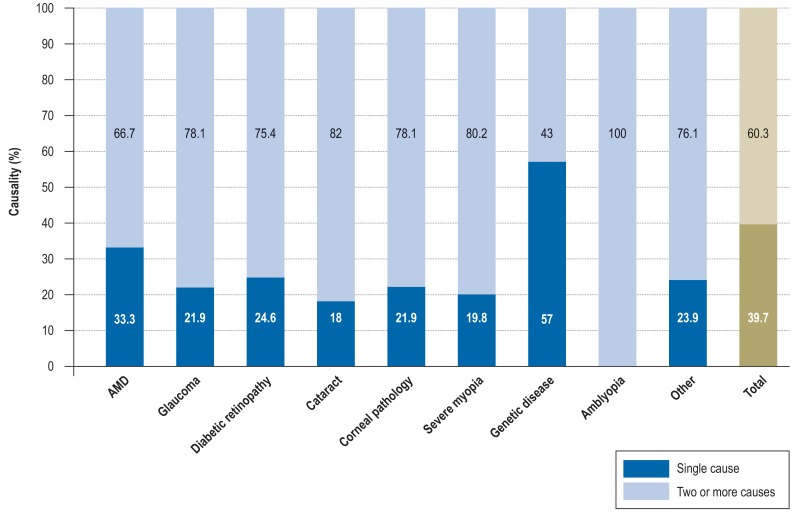
Thirty of the 55 study participants with visual impairment (54.5%) had two or more ophthalmological pathologies in parallel (figure 2). In all cases of genetically caused ocular disease there was only one pathology, but in all other categories the majority of probands had two or more diseases. Comparing the subgroups, more men than women had multiple causes of visual impairment (60.9% versus 50.0%). The same was true for those over 65 compared with those under 65 (62.1% versus 46.2%).
Figure 2.
Frequency of a single cause versus two or more causes (dark versus light shading) for visual impairment and blindness.
AMD = age-related macular degeneration
Discussion
Happily, the prevalence of visual impairment in the GHS study cohort was found to be low (0.37%). Blindness, according to the WHO definition of vision <0.05, had a prevalence of 0.05%. Calculations based on official disability statistics reveal a similar combined rate of 0.4% for visual impairment and blindness in the whole German population, rising as high as 2.4% in the 75 years and older age group (8).
There are distinct differences between the GHS findings and the results of studies carried out in other countries (table 3). These can be explained by the differing age structures of the study populations (vision loss is much more common in the elderly) or by varying approaches to recruitment of the probands. It must also be assumed, however, that morbidity varies across the regions of the world. Studies that project worldwide prevalence data onto Western Europe arrive at much higher figures of around 5% for visual impairment and 0.4% for blindness in adults over 50 years of age (22, 23), in stark contrast to the lower prevalence rates from studies carried out in western industrialized nations.
Table 3. Prevalence of blindness and visual impairment (WHO criteria) with best correction in population-based studies from various countries.
| Country |
Study population |
Year(s) of survey | Age group |
Prevalence of visual impairment/ blindness |
Remarks | Reference |
| Japan | 3870 | 2000–2001 | 40+ | 0.39/0.14 | (24) | |
| Canada | 962 | 2001 | 0+ | 0.36/0.04 | *1 | (25) |
| USA | 4582 | 2010–2013 | 50+ | 3.00/0.07 | *2 | (26) |
| Netherlands | 6775 | 1990–1993 | 55+ | 1.42/0.47 | *3 | (27) |
| China | 4438 | 2001 | 40+ | 1.00/0.40 | (28) | |
| Singapore | 3280 | 2004–2006 | 40–79 | 4.40/0.30 | *2 | (29) |
| Germany (Gutenberg Health Study) | 14 687 | 2007–2012 | 35–74 | 0.37/0.05 |
*1 The probands were recruited from patients attending for ophthalmological consultation
*2 Visual impairment also included uncorrected refractive errors, which made up around 50% of the cases
*3 Some of the probands were recruited in senior citizens’ homes
In general, the low prevalence of visual impairment goes along with a trend towards decreasing rates of new cases of severe vision loss. Although overall there are more visually impaired and blind people, owing to the growing global population and the demographic developments in western societies (8, 22), the age-specific prevalence of blindness and visual impairment went down by 26% between 1990 and 2015 (22). In Germany too, a decrease of over 40% in new cases of blindness was described for the period 1991 to 2008 (10). It thus seems that the improved health of the population is reflected in a low prevalence of visual impairment in the GHS study cohort.
This association is particularly explicit in the strikingly low prevalence of diabetes-related visual impairment. The prevalence of diabetes in the GHS is 7.5% (30), corresponding to the findings of other studies on the distribution of diabetes in the German population (31). Of the identified diabetics in the GHS, 21.7% showed diabetes-related retinal changes (30). The fact that only 3.6% of the visually impaired probands had diabetic retinopathy, together with the complete absence in our study of blindness due to diabetes, underlines the tendency described in earlier studies, namely a reduction in diabetes-induced blindness in Germany over recent decades (32, 33).
In agreement with the findings of other studies, the GHS showed that the frequency of visual impairment is around 3 times higher in the elderly (over 65 years of age). We also found a difference between the sexes, with an around 50% higher prevalence of visual impairment in women; however, this was not statistically relevant. Stevens et al. (2) and Abou-Gareeb et al. (34) also observed around 50% more visual impairments in women. Furthermore, they established that the difference is even more pronounced in western industrialized nations than in developing countries. The reasons for this difference in prevalence between the sexes may be differing sex-specific morbidity risks for ocular diseases such as glaucoma.
One conspicuous finding of our study was the distribution of the causes of visual impairment. In over half the cases identified, loss of vision was due to concatenations of various factors. Previous studies of German populations often showed that progression to blindness was predominantly (in up to three fourths of cases) due to the ocular diseases AMD, glaucoma, and diabetic retinopathy (14, 15, 35). However, surveys of registry data and collections of case studies primarily capture new cases of blindness, tending to neglect longstanding cases of visual impairment. It follows that particularly genetically induced ocular diseases are highly relevant as a health risk at population level, because they often manifest early and persist lifelong.
The prevention of visual impairment comprises not only the treatment of specific diseases of the eye, but also the detection and treatment of potentially sight-threatening circumstances. For this reason, closer attention should be paid to amblyopia and severe myopia. These conditions do not in themselves constitute causes of blindness, but can lead to visual impairment in combination with other ocular diseases.
Amblyopia was present in 5.6% of the study participants in the GHS cohort (36), and severe myopia (more than 6 dpt) in 3.5% (37). With regard to amblyopia, it is important to identify suspected cases in early childhood and train the weaker eye. For severe myopia, which can lead to macular changes (myopic maculopathy) as well as to defects and subsequent detachments of the retina, regular follow-up visits and early treatment are advisable to prevent major progression.
Effective prevention also requires interdisciplinary cooperation. Particularly primary care physicians, internists, occupational physicians, and pediatricians must work to detect possibly vision-threatening developments at an early stage and initiate referral for ophthalmological consultation. Nonophthalmological measures can also reduce the danger of visual impairment: for instance, factors leading to vascular occlusion in the eye can be treated early or occupational physicians can take steps to reduce the danger of injury in the workplace.
Visual impairment can be prevented. Worldwide, 65% of cases of blindness and 76% of visual impairments are thought to be avoidable (3). It is thought that the prevalence of visual impairment is up to 10 times lower in western industrialized nations than in developing countries (2). The low prevalence figures in our study can probably thus be interpreted as showing the success of good ophthalmological and medical care. However, a population-based study cannot indicate to what extent individual eye operations, treatment of cardiovascular risk factors, or other medical measures have actually prevented visual impairment.
Our results may be limited by selection bias, in that blind and visually impaired persons in the original cohort may possibly have decided not to participate due to their poor vision and were thus not included in the study group. Therefore, despite an elaborate recall procedure during proband selection the results of the study may be excessively positive. A further limitation is represented by the lack of uniform worldwide definitions of blindness and visual impairment, making it difficult to compare the findings of studies with different designs. We decided to apply the WHO criteria in order to achieve the greatest possible comparability with other epidemiological studies. Using the widespread German definition of blindness as visual acuity = 0.02 would have hampered comparison with studies from other countries.
In Germany, the individual federal states assess eligibility for benefits such as blind person’s allowance and determine the sum to be paid. For these purposes, further parameters such as visual field limitation are taken into account. In addition, the upper age limit of our study precludes any conclusions concerning the age group 75 years and over, which according to German federal disability statistics accounts for more than 53% of cases of blindness and visual impairment (38).
Summary
The prevalence of blindness and visual impairment in our probands was rather low, and this presumably applies also to the segment of the adult population represented by the study cohort. Our data show that visual impairment often has to be seen as the consequence of two or more parallel disease processes. Successful prevention of vision loss therefore depends not only on optimization of ophthalmological treatment procedures, but also on early detection of potentially blindness-inducing conditions.
Table 2. The causes of visual impairment and blindness (n = 55, multiple responses possible).
| Ocular disease | Frequency (n) | % |
| Age-related macular degeneration (AMD) | 12 | 21.8 |
| Glaucoma | 6 | 10.9 |
| Diabetic retinopathy | 2 | 3.6 |
| Cataract | 11 | 20.0 |
| Corneal pathology | 9 | 16.4 |
| Genetic disease | 10 | 14.5 |
| Severe myopia | 8 | 18.2 |
| Amblyopia | 12 | 21.8 |
| Other causes | 18 | 32.7 |
| including: | ||
| Status post retinal detachment | 5 | 9.1 |
| Status post injury | 4 | 7.3 |
| Status post vascular occlusion | 2 | 3.6 |
| Status post neoplasia | 1 | 1.8 |
| Status post enucleation | 3 | 5.5 |
| Strabismus | 2 | 3.6 |
| Nystagmus | 2 | 3.6 |
| Uveitis, Coats disease, epiretinal gliosis | 1 each | 1.8 |
Key Messages.
The Gutenberg Health Study (GHS) is a population-based survey of the health status of the adult population in the Mainz–Bingen region of Germany.
The prevalence of visual impairment in the GHS study cohort (age range 35 to 74 years) was 0.37%. The prevalence in the age group 65 to 74 years was 3 times that in younger participants.
Most of those with visual impairment exhibited two or more ocular diseases in parallel.
Risk constellations such as amblyopia, severe short-sightedness, and previous damage to the eye, e.g., retinal detachment or injury, are common contributory causes of visual impairment.
Many ocular diseases can be detected early and treated effectively. Measures to prevent visual impairment should take the wide variety of etiological factors into account.
Acknowledgments
Translated from the original German by David Roseveare
Acknowledgments
We are grateful to all of the study participants for their willingness to contribute their data to this research project, and to all members of the study personnel for their commitment.
Funding
The Gutenberg Health Study was financed by the state government of Rhineland–Palatinate (Rhineland–Palatinate Foundation for Innovation, project AZ 961–386261/733), the research programs Science Shapes the Future (Wissen schafft Zukunft) and the Center for Translational Vascular Biology (CTVB) of the University of Mainz, and the companies Boehringer Ingelheim, Philips Medical Systems, and Novartis Pharma, including non-tied funding for the Gutenberg Health Study.
Footnotes
Conflict of interest statement
Prof. Wild has received study support (third-party funding) from Boehringer Ingelheim and Philips GmbH.
Prof. Schuster’s position as professor for ophthalmological care research was endowed by the Eye Foundation (Stiftung Auge) and is financed by the German Ophthalmological Society (Deutsche Ophthalmologische Gesellschaft) and the Association of Ophthalmologists in Germany (Berufsverband der Augenärzte Deutschlands e.V.). He has received study support (third-party funding) from Bayer Vital, Novartis, and Heidelberg Engineering.
The remaining authors declare that no conflict of interests exists.
References
- 1.Bourne RR, Jonas JB, Flaxman SR, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe: 1990-2010. Br J Ophthalmol. 2014;98:629–638. doi: 10.1136/bjophthalmol-2013-304033. [DOI] [PubMed] [Google Scholar]
- 2.Stevens GA, White RA, Flaxman SR, et al. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology. 2013;120:2377–2384. doi: 10.1016/j.ophtha.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 3.Bourne RR, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. 2013;1:e339–e349. doi: 10.1016/S2214-109X(13)70113-X. [DOI] [PubMed] [Google Scholar]
- 4.Krumpaszky HG, Klauss V. Epidemiology of blindness and eye disease. Ophthalmologica. 1996;210:1–84. doi: 10.1159/000310663. [DOI] [PubMed] [Google Scholar]
- 5.Wolfram C, Pfeiffer, N. Weißbuch zur Situation der ophthalmologischen Versorgung in Deutschland. Deutsche Ophthalmologische Gesellschaft (DOG), ed. 2012 [Google Scholar]
- 6.Knauer C, Pfeiffer N. Erblindung in Deutschland - heute und 2030. Ophthalmologe. 2006;103:735–741. doi: 10.1007/s00347-006-1411-y. [DOI] [PubMed] [Google Scholar]
- 7.Finger RP, Fimmers R, Holz FG, Scholl HP. Incidence of blindness and severe visual impairment in Germany: projections for 2030. Invest Ophthalmol Vis Sci. 2011;52:4381–4389. doi: 10.1167/iovs.10-6987. [DOI] [PubMed] [Google Scholar]
- 8.Wolfram C, Pfeiffer N. Blindness and low vision in Germany 1993-2009. Ophthalmic Epidemiol. 2012;19:3–7. doi: 10.3109/09286586.2011.628136. [DOI] [PubMed] [Google Scholar]
- 9.Finger RP, Bertram B, Wolflram C, Holz FG. Blindness and visual impairment in Germany—a slight fall in prevalence. Dtsch Arztebl Int. 2012;109:484–489. doi: 10.3238/arztebl.2012.0484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Claessen H, Genz J, Bertram B, et al. Evidence for a considerable decrease in total and cause-specific incidences of blindness in Germany. Eur J Epidemiol. 2012;27:519–524. doi: 10.1007/s10654-012-9705-7. [DOI] [PubMed] [Google Scholar]
- 11.Congdon N, O‘Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 12.Kocur I, Resnikoff S. Visual impairment and blindness in Europe and their prevention. Br J Ophthalmol. 2002;86(7):716–722. doi: 10.1136/bjo.86.7.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster A, Gilbert C, Johnson G. Changing patterns in global blindness: 1988-2008. Community Eye Health. 2008;21:37–39. [PMC free article] [PubMed] [Google Scholar]
- 14.Finger RP, Fimmers R, Holz FG, Scholl HP. Prevalence and causes of registered blindness in the largest federal state of Germany. Br J Ophthalmol. 2011;95:1061–1067. doi: 10.1136/bjo.2010.194712. [DOI] [PubMed] [Google Scholar]
- 15.Krumpaszky HG, Ludtke R, Mickler A, Klauss V, Selbmann HK. Blindness incidence in Germany A population-based study from Wurttemberg-Hohenzollern. Ophthalmologica. 1999;213:176–182. doi: 10.1159/000027415. [DOI] [PubMed] [Google Scholar]
- 16.Trautner C, Haastert B, Giani G, Berger M. Incidence of blindness in southern Germany between 1990 and 1998. Diabetologia. 2001;44:147–150. doi: 10.1007/s001250051592. [DOI] [PubMed] [Google Scholar]
- 17.Mirshahi A, Ponto KA, Hohn R, Wild PS, Pfeiffer N. Ophthalmologische Aspekte der Gutenberg Gesundheitsstudie (GHS): eine interdisziplinäre prospektive populationsbasierte Kohortenstudie. Ophthalmologe. 2013;110:210–217. doi: 10.1007/s00347-012-2666-0. [DOI] [PubMed] [Google Scholar]
- 18.Wild PS, Zeller T, Beutel M, et al. Die Gutenberg Gesundheitsstudie. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55:824–829. doi: 10.1007/s00103-012-1502-7. [DOI] [PubMed] [Google Scholar]
- 19.Höhn RKU, Peto T, Blettner M, et al. The ophthalmic branch of the Gutenberg health study: study design, cohort profile and self-reported diseases. PLoS One. 2015;10 doi: 10.1371/journal.pone.0120476. e0120476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lampert T, Kroll LE, Muters S, Stolzenberg H. Messung des sozioökonomischen Status in der Studie Gesundheit in Deutschland (GEDA) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:131–143. doi: 10.1007/s00103-012-1583-3. [DOI] [PubMed] [Google Scholar]
- 21.R Core Team R. R Foundation for Statistical Computing. Vienna: Austria; 2016. A language and environment for statistical computing. [Google Scholar]
- 22.Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 23.Stevens GA, White RA, Flaxman SR, et al. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology. 2013;120:2377–2384. doi: 10.1016/j.ophtha.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 24.Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu T, Kitazawa Y. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology. 2006;113:1354–1362. doi: 10.1016/j.ophtha.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 25.Maberley DA, Hollands H, Chuo J, et al. The prevalence of low vision and blindness in Canada. Eye. 2006;20:341–346. doi: 10.1038/sj.eye.6701879. [DOI] [PubMed] [Google Scholar]
- 26.Varma R, Kim JS, Burkemper BS, et al. Prevalence and causes of visual impairment and blindness in Chinese American adults: The Chinese American Eye Study. JAMA Ophthalmol. 2016;134:785–793. doi: 10.1001/jamaophthalmol.2016.1261. [DOI] [PubMed] [Google Scholar]
- 27.Klaver CC, Wolfs RC, Vingerling JR, Hofman A, De Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol. 1998;116:653–658. doi: 10.1001/archopht.116.5.653. [DOI] [PubMed] [Google Scholar]
- 28.Xu L, Cui T, Yang H, et al. Prevalence of visual impairment among adults in China: the Beijing Eye Study. Am J Ophthalmol. 2006;141:591–593. doi: 10.1016/j.ajo.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 29.Wong TY, Chong EW, Wong LW, et al. Prevalence and causes of low vision and blindness in an urban malay population: the Singapore Malay Eye Study. Arch Ophthalmol. 2008;126:1091–1099. doi: 10.1001/archopht.126.8.1091. [DOI] [PubMed] [Google Scholar]
- 30.Raum P, Lamparter J, Ponto KA, et al. Prevalence and cardiovascular associations of diabetic retinopathy and maculopathy: results from the Gutenberg Health Study. PloS One. 2015;10 doi: 10.1371/journal.pone.0127188. e139527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heidemann C, Du Y, Schubert I, Rathmann W, Scheidt-Nave C. Prävalenz und zeitliche Entwicklung des bekannten Diabetes mellitus: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5-6):668–677. doi: 10.1007/s00103-012-1662-5. [DOI] [PubMed] [Google Scholar]
- 32.Hörle S, Gruner F, Kroll P. Epidemiologie diabetischer Erblindungen - eine Übersicht. Klin Monbl Augenheilkd. 2002;219:777–784. doi: 10.1055/s-2002-36318. [DOI] [PubMed] [Google Scholar]
- 33.Genz J, Scheer M, Trautner C, Zollner I, Giani G, Icks A. Reduced incidence of blindness in relation to diabetes mellitus in southern Germany? Diabet Med. 2010;27:1138–1143. doi: 10.1111/j.1464-5491.2010.03081.x. [DOI] [PubMed] [Google Scholar]
- 34.Abou-Gareeb I, Lewallen S, Bassett K, Courtright P. Gender and blindness: a meta-analysis of population-based prevalence surveys. Ophthalmic Epidemiol. 2001;8:39–56. doi: 10.1076/opep.8.1.39.1540. [DOI] [PubMed] [Google Scholar]
- 35.Trautner C, Haastert B, Richter B, Berger M, Giani G. Incidence of blindness in southern Germany due to glaucoma and degenerative conditions. Invest Ophthalmol Vis Sci. 2003;44(3):1031–1034. doi: 10.1167/iovs.02-0304. [DOI] [PubMed] [Google Scholar]
- 36.Elflein HM, Fresenius S, Lamparter J, Pitz S, Pfeiffer N, Binder H, et al. The prevalence of amblyopia in Germany: data from the prospective, population-based Gutenberg Health Study. Dtsch Arztebl Int. 2015;112:338–344. doi: 10.3238/arztebl.2015.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolfram C, Hohn R, Kottler U, et al. Prevalence of refractive errors in the European adult population: the Gutenberg Health Study (GHS) Br J Ophthalmol. 2014;98:857–861. doi: 10.1136/bjophthalmol-2013-304228. [DOI] [PubMed] [Google Scholar]
- 38.Statistisches Bundesamt. Wiesbaden: 2017. Statistik der Schwerbehinderten Menschen 2015. [Google Scholar]