Abstract
The temporomandibular joint forms one of the most fascinating and complex synovial joints in the body. Movements of the temporomandibular joint are regulated by an intricate neurological controlling mechanism, which is essential for the system to function normally and efficiently. Lack of such harmony may cause disruptive muscle behavior or structural damage to any of the components. The management of refractory pain and dysfunctions in the temporomandibular joint poses challenge both to the oral physician and maxillofacial surgeon. Arthrocentesis is a simple, minimally invasive technique that can be used instead of more invasive procedures in patients with pain that fails to respond to conventional conservative measures. This review provides a full comprehensive overview of the literature about the various technical and prognostic aspects in relation to arthrocentesis of the temporomandibular joint, and every clinician must take into account this consideration when performing this procedure in treating patients with temporomandibular disorders.
Keywords: Arthrocentesis, temporomandibular joint, temporomandibular joint disorders
INTRODUCTION
Temporomandibular disorder (TMD) is the most common cause of orofacial pain of nondental origin.[1,2] It is a term used to describe disorders involving the temporomandibular joints (TMJs), masticatory muscles, and occlusion resulting in muscle or TMJ pain, restricted movement, muscle tenderness, and intermittent joint sounds.[3,4] A treatment strategy for TMDs consists of various nonsurgical and surgical methods. A nonsurgical approach is recommended for initial management,[4,5,6] and if this failed, surgical intervention should be considered.[7] However, surgery in this region is associated with many risks. Arthrocentesis of TMJ has emerged over the years as a useful technique to manage TMDs. Arthrocentesis is commonly defined as the lavage of the TMJ without viewing the joint space using sterile needles and sterile irrigants so as to reduce the pain by removing inflammatory mediators from the joint or to increase the mandibular mobility by removing intra-articular adhesions by means of hydraulic pressure from irrigation of the upper chamber of the TMJ. Arthrocentesis is generally suggested in patients irresponsive to conservative therapies.[8,9]
Numerous clinical studies regarding this technique have been published in the literature. The present work is an attempt to critically review the published literature with regard to the critique of this technique and provides an overview of the current concepts regarding the arthrocentesis of TMJ, highlighting the technical considerations in performing the procedure as well as factors affecting the outcome of the procedure. Their possible indications and associated complications will also be discussed.
METHODS
To get up-to-date information, a web-based search was initiated using PubMed/Medline database, using the key terms “temporomandibular joint,” “temporomandibular disorders,” and “temporomandibular joint arthrocentesis” to determine the scope of coverage in well-documented articles. The search was subsequently refined to temporomandibular joint arthrocentesis. The sites of specialized scientific journals in the areas of oral and maxillofacial surgery, oral medicine, and other relevant journals were also used. The bibliographies were also reviewed to identify additional relevant studies.
ARTHROCENTESIS: AN EMERGING ALTERNATIVE TO SURGICAL INTERVENTION
Treatment strategies for TMDs are as diverse as the patients that present with it. Although in managing the TMDs, one should utilize first the conservative treatment; however, in some circumstances, surgery is usually considered to be the definitive treatment modality and sometimes the only treatment option.[10,11] The right combination of symptomatic history, clinical features, and radiological signs will readily reveal whether the TMD patient is an appropriate candidate for surgery.[10] There are various conditions where surgery plays a pivotal role such as:[11,12]
In case to restore and repair the damaged tissue or to remove tissue that cannot be salvaged
To promote healing of tissues by replacing missing tissues with grafts, for example, in case of chronically displaced disc or in case of collapsed articular cartilage and osteophytes that interfere with the smooth, pain-free function of the joint, and
When there is significant disease affecting the joint.
Dolwick and Dimitroulis[11] divided the indications for surgery into relative and absolute [Table 1]. From a clinical standpoint, the most common general indication for TMJ surgery is where the joint disorder remains refractory, or not responding to nonsurgical therapies,[4] or where the source of the pain and dysfunction is well localized to the TMJ region. Therefore, specific indications for TMJ surgery include the following:[11]
Table 1.
Indications for surgery by Dolwick and Dimitroulis
| Absolute indication |
| Ankylosis of TMJ (e.g., fibrous or osseous joint fusion) |
| Neoplasia (e.g., osteochondroma of the condyle) |
| Dislocation of TMJ either recurrent or chronic |
| Developmental disorders affecting the TMJ |
| Relative indication |
| Internal derangement of TMJ |
| Osteoarthrosis |
| Trauma to the TMJ |
TMJ=Temporomandibular joints
Chronic severe limited mouth opening and gross mechanical interferences such as painful clicking and crepitus that fail to respond to TMJ arthrocentesis and arthroscopy
Radiologically confirmed degenerative joint disease, with clinical features of intolerable pain and joint dysfunction, is essentially the key criterion for TMJ surgical intervention.
Controversy still surrounds the role of surgery in the management of pain and dysfunction of the TMJ. Surgery in the TMJ region is often associated with morbidity and fraught with many risks, and more often, it does not produce expected results. Surgery is often considered as an option of last resort. TMJ arthrocentesis procedure bridged the gap between surgical and nonsurgical treatment.[13] The aim of TMJ arthrocentesis is to make an intolerable situation tolerable. It is often considered to be the highly effective method to restore normal maximal mouth opening and functioning.
RATIONALE OF ARTHROCENTESIS
TMDs, either inflammatory or noninflammatory, are typically associated with structural alterations in joint tissues, such as cartilage degradation and subchondral bone alterations secondary to the change in the articular loading. In inflammatory TMDs, various mediators of inflammation, particularly cytokines, may be responsible for enzymatic degradation of the matrix. Macromolecular degradation of the matrix determines the physical and biological deterioration of the tissues and promotes the disease because the degradation fragments, proteoglycans, and collagen released into the synovial fluid generate inflammatory pain.[14] There are different types of inflammatory and anti-inflammatory cytokines, the balance of which affects the development of degenerative and inflammatory changes. Inflammatory cytokines include interleukin-1 (IL-1), IL-6, IL-8, and tumor necrosis factor-α while anti-inflammatory cytokines include IL-4, tissue inhibitors of metalloproteinases (TIMP-1), TIMP-2, and tumor growth factor transforming growth factor-β.[15] In the course of the inflammation, monocytes and macrophages quickly release IL-1 and IL-6. Fibroblasts and chondrocytes also have this ability, but at the same time, through the action of IL-6, they release TIMP as well. Further, synovial cells and mononuclear cells infiltrating the edge of the blood vessels also produce IL-6 in both synovial tissue and synovial fluid. High levels of IL-6 in the synovial fluid of the TMJ are associated with extensive acute synovitis.[16] In addition to this, the current clinical evidence also suggested that the TMJ pain or dysfunction may be attributed to alterations in joint pressure (negative intra-articular pressure) and biochemical constituents of the synovial fluid (failure of lubrication) which may lead to clicking and derangement of the TMJ.[15,17,18]
Arthrocentesis reduces the pain by allowing the elimination of inflammatory cells from the joint space and increases the mandibular mobility by removing intra-articular adhesions, eliminating the negative pressure within the joint, thus recovering disc and fossa space which reduces the mechanical obstruction caused by anterior disc displacement.[15,19,20,21,22,23]
PROCEDURE OF TEMPOROMANDIBULAR JOINT ARTHROCENTESIS – TECHNICAL CONSIDERATIONS
Various techniques for arthrocentesis have been mentioned in the literature which itself varies considerably over the period of time. Murakami et al.[24] first described a technique of TMJ arthrocentesis with pumping irrigation and hydraulic pressure to the upper joint cavity followed by manipulation of the jaw. After that, Nitzan et al.[19] described a technique utilizing the insertion of two needles into the upper joint compartment, permitting more effective lavage of the joint. In this technique, the landmarks for the insertion of needles are marked on the skin according to the method suggested by McCain et al.[25,26] for arthroscopy (posterolateral approach to the upper joint space).
Preprocedural considerations
TMJ arthrocentesis is a minimally invasive procedure[27,28] and can be comfortably performed under local anesthesia or intravenous conscious sedation or general anesthesia, depending on patient comfort and surgeon preference. Before performing the procedure, the following points should be kept in mind:[29]
The surgical field is properly draped and cleaned with povidone iodine or similar substance, particularly in preauricular region and ear
External auditory canal is protected from accumulation of blood and fluid using a cotton pledget
The auriculotemporal nerve block is given, and the areas of joint penetration should be infiltrated.
The two-needle technique
The classical technique to perform TMJ arthrocentesis utilizes double access to the joint cavity. This technique uses two needles, one for injecting and the other for aspirating the solution.[30]
For two-needle technique, access is performed by taking as indicator the Holmlund–Hellsing line (canthotragal line),[31] as depicted in Figure 1. A straight line is drawn on the skin joining the medial portion of the tragus of the ear to the outer canthus of the ipsilateral eye
Two points are marked on this line for needle insertion. The first, more posterior point will be marked at a distance of 10 mm from the tragus and 2 mm inferior to canthotragal line. This point corresponds to the posterior extent of the glenoid fossa. The second point will be marked at 20 mm anterior to tragus and 10 mm inferior to canthotragal line, which corresponds to the height of articular eminence[19,32,33,34]
The glenoid fossa is thin, with a range of 0.5–1.5 mm.[25,35] The dura and temporal lobe are located beneath the glenoid fossa. Joints may also be eroded by degenerative arthritis or previous infections. Hence, it is possible that during the procedure, this structure may get perforated. Therefore, the surgeon must be cautious not to insert the needle much into the joint space. About 25 mm depth is enough to reach to upper joint space[27]
To increase the joint space during arthrocentesis, the patient is usually asked to open the mouth and deviate it to the opposite side so as to distract the condyle from the glenoid fossa thereby increasing joint space. Nagori et al.[36] suggested that custom-made mouth prop is an effective tool to hold the mandible in eccentric position during arthrocentesis
With the patient's mouth open, the first needle is inserted into the superior joint space in the most posterior point directing upward, forward, and inward to a depth of about 20–25 mm, after the tip of the needle has come into contact with the posterior wall of the articular eminence[37]
This is followed by administration of irrigating solution (Hartmann solution [also known as Ringer's lactate solution] or physiological saline) through the first needle with the aim of distending the superior joint space.[29] This compartment will take up to 5 mL of fluid[31]
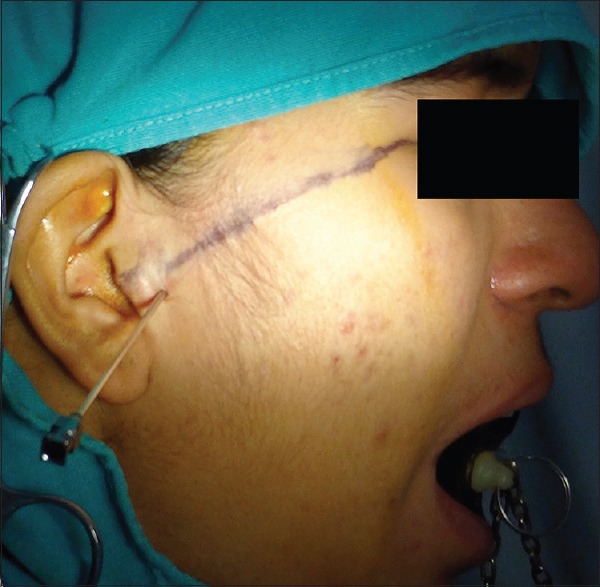
Now, the second needle is introduced in the distended compartment, in front of the first needle at the marked point, allowing the visualization of the solution and orienting the flow of the joint lavage solution,[29] as shown in Figure 2.
Figure 1.
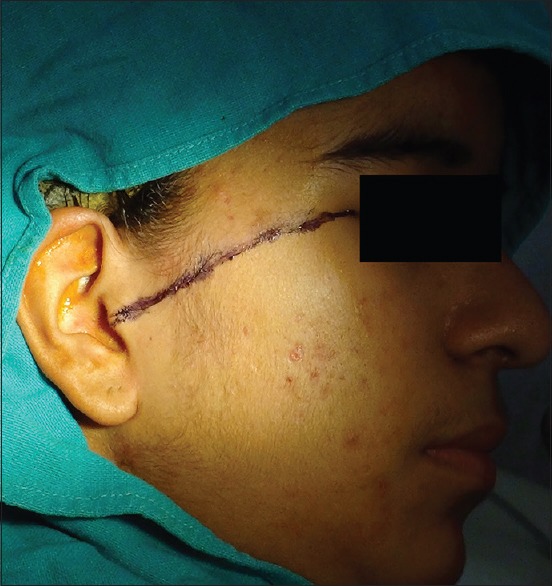
Holmlund–Hellsing line or canthotragal line
Figure 2.

Double-needle arthrocentesis
Laskin[38] mentioned that it is usually difficult to insert the second needle anterior to the first one, and therefore, he had inserted the anterior needle in the posterior recess of the upper joint compartment by placing it 3–4 mm anterior to the first one and suggested this technique to be much easier than the previous method. However, if the second needle is entered anterior to the first one, it is inserted into a narrower region of the upper joint compartment, and this may cause damage to the articular disc leading to failure of the outflow of irrigating solution. Alkan and Etöz[39] proposed a new technique, in which the posterior point of entry for the first needle was the same while the second needle is inserted 7 mm anterior from the middle of the tragus and 2 mm inferior along the canthotragal line. This second needle was adjusted parallel and almost 3 mm posterior to the first until bony contact was made. It was assumed that when the second needle is inserted posterior to the first one in the wider part of the upper joint compartment, the outflow of the solution from the joint cavity is easier to achieve. They thoroughly irrigated numerous joints with complete success by this technique and suggested that the use of this landmark as the default technique may be reasonable, as repeated insertions of a needle are uncomfortable both for physicians and patients and adversely affect the success of the treatment.
The positioning of two needles within the joint cavity may cause some discomfort to patients, particularly at the time of the first lavage. A study evaluating the efficacy and tolerability of a cycle of 5 weekly hyaluronic acid injections performed after a classical two-needle arthrocentesis showed that the patient's perception of tolerability increased with time. Possible explanation for this is that with the sequential arthrocentesis interventions, the catabolytes are removed and adhesions are broken down, which made the insertion of the needles easier and consequently, the quality of the posttreatment course was improved.[40]
Recently, a technique using a single needle for both injection and ejection of irrigating solution has been described[31] and gave interesting results over a short period.[41]
The single-needle technique
The single-needle approach for the lavage of TMJ was based on the rationale that pumping saline injection into the superior joint compartment with the patient in an open mouth position provides enough pressure to release joint adherences and to allow fluid outflow when the patient closes his/her mouth,[33] as shown in Figure 3. The single-needle technique provides the underpressure fluid injection to expand the joint cavity[31] and to break joint adherences that are responsible for the reduced translatory movement of the condyle.[42,43] The injection-ejection process must be performed for up to 10 repetitions for a total amount of about 40 ml. This makes the single-needle technique indicated in the case of hypomobile joints with strong adherences or joints with degenerative changes that make the insertion of the second needle difficult.[31]
Figure 3.
Single-needle arthrocentesis
The single-needle arthrocentesis technique has several advantages over the traditional two-needle technique which are as follows:[31]
It is a simple, easier, and less invasive technique
As the positioning of a second needle could interfere with the stability of the first one in two-needle technique, the single-needle technique provides more sure and stable access to the joint cavity
There is reduction in postoperative pain and discomfort to the patient after the procedure which may be attributed to the lesser amount of anesthetic needed in the single-needle approach. This may further reduce the risks of postoperative facial nerve paresthesia
An anteriorly positioned second needle may cause trauma to the facial nerve, that lies anteriorly and medially to the glenoid fossa, which is the site where the second needle is usually inserted; single needle approach reduces the chances of such injuries
There is reduction in the execution time for the procedure to perform in single-needle approach
A single-needle technique might allow full retention of the injected hyaluronic acid within the joint compartment because the risk of hyaluronic acid flowing out through the second point of injection is absent.
However, this technique has certain limitations.[29]
Since the total circulating volume of the irrigating solution is very low, this technique is hardly able to eliminate algogenic substances present in the synovial fluid of the upper TMJ compartment, responsible for pain and bone and fibrocartilaginous changes
Even on exerting pressure on the syringe plunger on the fluid, only a part will return through the needle, regardless of patients closing their mouth. Part of the fluid may leak from the upper compartment toward the face, producing local edema which may generate intra- and post-operative pain.
Several studies have been performed over the years to compare the efficacy of the double- and single-needle arthrocentesis techniques. Sindel et al.[44] compared the efficacy of the double- and single-needle arthrocentesis techniques and found that the single-needle technique may be a good alternative with the advantages of easier application in cases where it is not possible to perform the double-needle technique. Şentürk et al.[45] compared the single-puncture technique with the double-puncture technique for arthrocentesis of the TMJ and found that arthrocentesis of the TMJ was successful with both techniques. Şentürk et al.[46] also evaluated the long-term effects of the single-puncture arthrocentesis (SPA) technique and found it to be an effective treatment method.
MODIFICATIONS IN ARTHROCENTESIS TECHNIQUES
With time, many modifications have been made in arthrocentesis methods to make this traditional procedure even simpler and less invasive.
Double needles in a single cannula
Alkan and Bas[47] used double needles in a single cannula having two adjacent irrigation and aspiration tubes that allow sufficient irrigation and lavage of the joint with the same device under the desired pressure. It is very safe and does not need another puncture to place the additional needle, such as with classic arthrocentesis. However, the major limitation of this technique is when there are major degenerative changes with decreased joint space and presence of osteophytes; it can be more difficult to enter this instrument into the joint space.
Shepard's single cannula
Rehman and Hall[48] used a similar device called a Shepard cannula that holds two needles together. Nevertheless, the device that keeps two needles together seems to be relatively thick, which has the potential to damage the nerve. Repetitive use of the device may cause the tips of the needles to blunt and increase the risk of infection. In a study conducted by Talaat et al.,[49] they compare single-needle arthrocentesis (Shepard cannula) with double-needle arthrocentesis with viscosupplementation for treating disc displacement without reduction of the TMJ and found that single-needle technique was easier to perform and required a shorter operative time, and therefore, it can be an alternative to the standard technique; however, it might add to the cost of the procedure.
Arthrocentesis technique with automatic irrigation under high pressure
Alkan and Kilic[50] described a modification of the arthrocentesis technique described by Nitzan et al.,[19] in which an irrigation pump from a surgical and dental implant motor was connected to the second needle, and automatic irrigation was initiated under high pressure. They considered that this modification provided the highest hydraulic pressure and made it possible to irrigate the upper joint space in 2 min with saline solution 300 ml. However, complications may develop in the surrounding tissues as a result of the high pressure if the irrigation pump is connected to the first needle without manual confirmation with the second needle. In addition, if the outlet needle suddenly blocks during the procedure, the surgeon must discontinue the irrigation immediately.
Concentric needles unit
Öreroğlu et al.[51] use a concentric-needle cannula system, i.e., using 2 different gauge needles placed in a concentric manner for SPA in TMJ and found it to be the least traumatic and perhaps the most feasible and cost-effective method for TMJ lavage.
IRRIGATING SOLUTIONS FOR ARTHROCENTESIS – VOLUME AND PRESSURE CONSIDERATIONS
The volume of solution used for lavage of the joint is considered to be very important in performing the arthrocentesis procedure. A number of irrigating solutions have been used in varying quantities and at different pressures.[21,52] The volume of solution used for TMJ arthrocentesis mentioned in various published studies varied widely and ranged from 50 to 500 mL.[53] Zardeneta et al.,[54] in their study, reported that approximately 100 mL of total perfusate is sufficient for therapeutic lavage of the joint. However, in the study by Kaneyama et al.,[21] they suggested that the ideal lavage volume of perfusate for arthrocentesis is between 300 and 400 mL.
Mostly, Ringer's lactate or physiological saline has been used for injecting into the superior joint space for arthrocentesis.[55] The fibrous tissue of the articular disc has a better tolerance for Ringer's solution than for an isotonic saline solution.[30,56] Since Ringer's lactate in comparison to other irrigants is close to Human serum, it is considered to be better tolerated by the tissues.[56,57]
The injection of fluid under pressure is a useful way of dealing with the adhesions that are considered to be the main cause of anchorage of the disc to the fossa or eminence or both resulting in reduced translation of condyle, and their release allows an immediate improvement in mouth opening.[31,58] Yura et al.[59] reported that low-pressure arthrocentesis (6.7 kPa) was unsuccessful in patients with severe adhesions whereas arthrocentesis under sufficient pressure (40 kPa) released them. They concluded that because irrigation under sufficient pressure can remove adhesions and widen the joint space, the technique might be useful for patients with closed lock and adhesions.
Guarda-Nardini et al.[33] in their study suggested that in case of adhesions or little adhesiveness, it is recommended to obstruct one of the needles, increasing the pressure on syringe plunger while the patient performs opening and laterality movements. If the movement is still limited, the assistant surgeon may perform the same movements aiming at breaking the possible adhesions and try to reestablish mouth opening pattern equal to or above 35 mm of laterality and protrusive of at least 4 mm. Similar observation had been reported by Dolwick MF[58], which showed that intermittent distension of the joint space by momentary blocking of the outflow needle and injection under pressure during lavage results in lysis of adhesions. Giacomo de Riu et al.[14] in their prospective clinical study on 30 consecutive patients with TMJ disorders found a significant reduction in pain in all the patients after arthrocentesis using saline and sodium hyaluronate injections. This pain reduction is attributed to high-pressure irrigation, which washes away inflammatory mediators, providing immediate pain relief.
However, it should be kept in mind that the pressure applied on the syringe during the procedure should be under control to avoid any complication.
POSTARTHROCENTESIS CONSIDERATIONS
At the end of lavage, it was proposed that steroids or sodium hyaluronate injection should be administered into the joint space to alleviate intracapsular inflammation.[60] The anti-inflammatory effects of intra-articular corticosteroids are useful for alleviating pain, swelling, and dysfunction in patients with inflammatory and noninflammatory joint diseases.[61,62] There are many glucocorticoid preparations, but methylprednisolone and triamcinolone (40 mg/1 ml) preparations are long acting and may be preferable.[61]
Postarthrocentesis, the patient should be kept on soft diet for a few days. Exercises of range of movement are started immediately and continued for several days. Analgesics should be prescribed as necessary for pain.[25,27,58]
Brennan and Ilankovan[63] suggested intra-articular injection of morphine (10 mg in 1 ml) as a long-acting analgesic in patients with continuing pain in the TMJ. In a study by Kunjur et al.,[64] they performed 405 arthrocentesis (with 50 ml of 0.9% normal saline solution followed by morphine 10 mg [in 1 ml] infusion) over a 10-year period for 298 patients and found significant reduction in pain score after arthrocentesis (P < 0.001) and 269 patients (90%) found the procedure beneficial. In another study, Furst et al.[65] reported that bupivacaine alone was a better analgesic than morphine alone or the combination of morphine and bupivacaine.
INDICATIONS
Arthrocentesis is used in patients with internal TMDs not responding to conservative clinical treatment
-
It is indicated in patients with anterior disc displacement with or without reduction.[29] Arthrocentesis has been reported to be up to 91% effective in treating patients with anterior disc displacement without reduction[21,66,67]
- Studies have shown that arthrocentesis can produce long-term relief of pain and dysfunction in patients with internal derangements of the TMJ.[68,69] Frost et al.[70] reported that arthrocentesis is the first line procedure for the treatment of acute and chronic closed lock of the TMJ in internal derangement. Similarly, Thomas et al.[71] also suggested in their study that arthrocentesis is a very useful technique for treatment of acute closed lock of TMJ.
-
Arthrocentesis can be used in cases of disc adhesions, either next to the fossa and/or the upper aspect of the articular tubercle, with mouth opening restrictions[29]
- In case of closed lock, the central portion of healthy disc indeed separates from the fossa, leaving rims fastened to surface of eminence causing increased negative pressure in closed space between fossa and disc. This pressure difference constitutes a force sufficient to keep the disc compressed against the fossa (suction cup effect).[27,72] Arthrocentesis abolishes this negative pressure, loosens the adhered disc, and reinstitutes its free sliding movement. It also helps the joint to reassume its normal movement bringing about recovery of intra-articular pressure fluctuations, which in turn allows perfusion of nutrients and medications. Thus, in patients with disc adhesions, there was marked improvement in mouth opening and decreased deviation.[73]
-
It can be used in cases of synovitis/capsulitis not responding to nonsurgical treatment[29]
- Substantial concentrations of inflammatory mediators of pain have been found in synovial fluid in patients with painful dysfunctional TMJs. Lavage of the upper joint space reduces pain by removing inflammation mediators from the joint.[37]
-
Arthrocentesis procedure can be implemented as palliation treatment for degenerative osteoarthritis[29,73,74]
- Patients of TMJ osteoarthritis complain of early morning stiffness in TMJ, severe joint pain, and limitation in mouth opening and function along with swelling in the respective area.[27] These symptoms arise due to joint overloading and increased intra-articular pressure, which leads to sclerosis of subchondral bone,[18] compromised blood supply which is due to pain, and absence of elimination of inflammatory substrates which are removed during normal joint mobilization.[27] Arthrocentesis forces apart the joint constituents and washes away inflamed synovial fluid, thereby reducing pain and loading effect thus in turn increasing mouth opening.[75,76]
It can be used in patients with painful joint noises occurring during mouth opening and/or closing.[29] Joint sounds such as clicking could be intermittent or constant which is caused by displacement of the disc. Arthrocentesis distends the upper joint compartment thereby relieving the lag, and disc-condyle complex moves synchronously reducing the clicking.[75]
CONTRAINDICATIONS
There are certain conditions where arthrocentesis procedure are strictly contraindicated. Contraindication for the procedure can be either absolute or relative.[37]
Absolute contraindication
An inflammatory focus (abscess or cellulitis) at the site of the needle insertion during arthrocentesis is generally considered an absolute contraindication for this procedure.
Relative contraindications
Bacteremia
Adjacent osteomyelitis
Coagulopathy
Malignant tumor.
COMPLICATIONS
Arthrocentesis procedure is associated with certain postoperative complications and sequelae. The severity of these complications depends on the anatomy of the TMJ and its related surrounding structures and also the method employed for the procedure (i.e., the single-needle or two-needle approaches). The frequency of these complications mentioned in the literature ranges between 2% and 10%.[37] In a retrospective study by Vaira et al.,[77] they concluded that the complications associated with the arthrocentesis are usually transient in nature.
Fifth nerve deficit (0.1%–2.4%)[78]
-
Otic injury (0.5%–8.6%)[78,79]
- Mainly occurs due to close anatomical proximity of TMJ to the middle ear cavity and the cartilaginous wall of the ear canal. Otologic complications include perforation of the external auditory canal, the occurrence of blood clots in the external auditory canal, perforation of the tympanic membrane, partial hearing loss, a feeling of fullness of the ear, and vertigo.[30,78,79,80,82,83,84,85,86]
Edema due to leakage of the lavage fluid (Ringer's solution) into the extra-articular space[30,37]
Needle breakage (0.1%) within the joint[78]
-
Acute joint inflammation[37]
- This may be accompanied by preauricular edema, redness, pain, and restricted mouth opening
-
Allergic reaction
-
Intracranial perforation
Local jaw trauma as a function of the number of repeated punctures[29]
Violent vertigo, without hearing disorders[89]
-
Other complications include the following:[37]
- Preauricular hematoma
- Extradural hematoma
- Injury to the superficial temporal artery resulting in aneurysm
- Development of arteriovenous fistula and bleeding into the joint.
SUCCESS RATE AND PROGNOSIS
Several studies have found that arthrocentesis is capable of recovering normal mouth opening and reducing pain and functional disorder. Brennan and Ilankovan[63] stated that arthrocentesis is a relatively simple surgical procedure for patients with pain that cannot be improved by conservative treatments. In a clinical comparative prospective study by Tutamayi et al.[90] on 45 patients suffering from TMJ pain, it was found that although both arthrocentesis and conservative treatment are effective in the treatment of TMJ dysfunctions, arthrocentesis proved to be superior. The overall success rate for arthrocentesis was 87.1% and was 55.9% for conservative treatments. As such, the overall success rate of the arthrocentesis procedure mentioned in the literature varies considerably [Table 2].[53,68,91,92,93,94,95]
Table 2.
Success rate of the arthrocentesis procedure mentioned in the literature
It is believed that age, duration of symptoms, and oral habits may influence the prognosis of arthrocentesis.[95] Nitzan et al.[93] stated that after arthrocentesis, recovery of patients 40 years or older is usually slower, and Guarda-Nardini et al.[96] reported that arthrocentesis using hyaluronic acid is less effective for young patients under 45 years. Bruxism is thought to be one of the major contributing factors to the etiology of TMJ. In the study conducted by Kim et al.,[95] it is concluded that clenching and bruxism reduce the therapeutic effect of the arthrocentesis, and therefore, the success rate of the procedure is low in patients with these oral habits. Alpaslan et al.[69] also suggested that arthrocentesis is likely to be more effective for patients without bruxism.
CONCLUSION
It appears reasonable to conclude that TMJ arthrocentesis is a simple, less invasive, inexpensive, and highly effective procedure. It is a method with a minimum number of complications and significant clinical benefits. These features make arthrocentesis a valid treatment option for patients with TMJ disorders not responding to nonsurgical therapies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Irving J, Wood GD, Hackett AF. Does temporomandibular disorder pain dysfunction syndrome affect dietary intake? Dent Update. 1999;26:405–7. doi: 10.12968/denu.1999.26.9.405. [DOI] [PubMed] [Google Scholar]
- 2.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F, et al. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–62. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Bonjardim LR, Lopes-Filho RJ, Amado G, Albuquerque RL, Jr, Goncalves SR. Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students. Indian J Dent Res. 2009;20:190–4. doi: 10.4103/0970-9290.52901. [DOI] [PubMed] [Google Scholar]
- 4.Dimitroulis G. Temporomandibular disorders: A clinical update. BMJ. 1998;317:190–4. doi: 10.1136/bmj.317.7152.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyons MF. Current practice in the management of temporomandibular disorders. Dent Update. 2008;35:314–6, 318. doi: 10.12968/denu.2008.35.5.314. [DOI] [PubMed] [Google Scholar]
- 6.Wright EF, North SL. Management and treatment of temporomandibular disorders: A clinical perspective. J Man Manip Ther. 2009;17:247–54. doi: 10.1179/106698109791352184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jerjes W, Upile T, Abbas S, Kafas P, Vourvachis M, Rob J, et al. Muscle disorders and dentition-related aspects in temporomandibular disorders: Controversies in the most commonly used treatment modalities. Int Arch Med. 2008;1:23. doi: 10.1186/1755-7682-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diraçoğlu D, Saral IB, Keklik B, Kurt H, Emekli U, Ozçakar L, et al. Arthrocentesis versus nonsurgical methods in the treatment of temporomandibular disc displacement without reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:3–8. doi: 10.1016/j.tripleo.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Barkin S, Weinberg S. Internal derangements of the temporomandibular joint: The role of arthroscopic surgery and arthrocentesis. J Can Dent Assoc. 2000;66:199–203. [PubMed] [Google Scholar]
- 10.Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint: A critical review of the literature. Part 1. Int J Oral Maxillofac Surg. 2005;34:107–13. doi: 10.1016/j.ijom.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Dolwick MF, Dimitroulis G. Is there a role for temporomandibular joint surgery? Br J Oral Maxillofac Surg. 1994;32:307–13. doi: 10.1016/0266-4356(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 12.Dolwick MF, Sanders B. St. Louis: CV Mosby Co; 1985. TMJ Internal Derangement and Arthrosis – Surgical Atlas. [Google Scholar]
- 13.Singh S, Shivamurthy DM, Varghese D. Re: Rahal A, et al.: Single-puncture arthrocentesis – Introducing a new technique and a novel device. J Oral Maxillofac Surg. 2011;69:311. doi: 10.1016/j.joms.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 14.De Riu G, Stimolo M, Meloni SM, Soma D, Pisano M, Sembronio S, et al. Arthrocentesis and temporomandibular joint disorders: Clinical and radiological results of a prospective study. Int J Dent. 2013;2013:790648. doi: 10.1155/2013/790648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nishimura M, Segami N, Kaneyama K, Sato J, Fujimura K. Comparison of cytokine level in synovial fluid between successful and unsuccessful cases in arthrocentesis of the temporomandibular joint. J Oral Maxillofac Surg. 2004;62:284–7. doi: 10.1016/j.joms.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Emshoff R, Puffer P, Strobl H, Gassner R. Effect of temporomandibular joint arthrocentesis on synovial fluid mediator level of tumor necrosis factor-alpha: Implications for treatment outcome. Int J Oral Maxillofac Surg. 2000;29:176–82. [PubMed] [Google Scholar]
- 17.Dolwick MF. Intra-articular disc displacement. Part I: Its questionable role in temporomandibular joint pathology. J Oral Maxillofac Surg. 1995;53:1069–72. doi: 10.1016/0278-2391(95)90126-4. [DOI] [PubMed] [Google Scholar]
- 18.Alpaslan C, Bilgihan A, Alpaslan GH, Güner B, Ozgür Yis M, Erbaş D, et al. Effect of arthrocentesis and sodium hyaluronate injection on nitrite, nitrate, and thiobarbituric acid-reactive substance levels in the synovial fluid. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:686–90. doi: 10.1067/moe.2000.105518. [DOI] [PubMed] [Google Scholar]
- 19.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163–7. doi: 10.1016/0278-2391(91)90409-f. [DOI] [PubMed] [Google Scholar]
- 20.Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: A follow-up study. Br J Oral Maxillofac Surg. 1995;33:23–6. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 21.Kaneyama K, Segami N, Nishimura M, Sato J, Fujimura K, Yoshimura H, et al. The ideal lavage volume for removing bradykinin, interleukin-6, and protein from the temporomandibular joint by arthrocentesis. J Oral Maxillofac Surg. 2004;62:657–61. doi: 10.1016/j.joms.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 22.Moses JJ, Sartoris D, Glass R, Tanaka T, Poker I. The effect of arthroscopic surgical lysis and lavage of the superior joint space on TMJ disc position and mobility. J Oral Maxillofac Surg. 1989;47:674–8. doi: 10.1016/s0278-2391(89)80004-7. [DOI] [PubMed] [Google Scholar]
- 23.Sembronio S, Albiero AM, Toro C, Robiony M, Politi M. Is there a role for arthrocentesis in recapturing the displaced disc in patients with closed lock of the temporomandibular joint? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:274–80. doi: 10.1016/j.tripleo.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Murakami KI, Iizuka T, Matsuki M, Ono T. Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint. Cranio. 1987;5:17–24. doi: 10.1080/08869634.1987.11678169. [DOI] [PubMed] [Google Scholar]
- 25.McCain JP. St. Louis: Mosby; 1996. Principles and Practice of Temporomandibular Joint Arthroscopy. [Google Scholar]
- 26.McCain JP, de la Rua H, LeBlanc WG. Puncture technique and portals of entry for diagnostic and operative arthroscopy of the temporomandibular joint. Arthroscopy. 1991;7:221–32. doi: 10.1016/0749-8063(91)90111-a. [DOI] [PubMed] [Google Scholar]
- 27.Nitzan DW. Arthrocentesis – Incentives for using this minimally invasive approach for temporomandibular disorders. Oral Maxillofac Surg Clin North Am. 2006;18:311–28, vi. doi: 10.1016/j.coms.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Monje-Gil F, Nitzan D, González-Garcia R. Temporomandibular joint arthrocentesis. Review of the literature. Med Oral Patol Oral Cir Bucal. 2012;17:e575–81. doi: 10.4317/medoral.17670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grossmann E. Arthrocentesis techniques applied to arthrogenic temporomandibular joint disorders. Rev Dor Sao Paulo. 2012;13:374–81. [Google Scholar]
- 30.Tozoglu S, Al-Belasy FA, Dolwick MF. A review of techniques of lysis and lavage of the TMJ. Br J Oral Maxillofac Surg. 2011;49:302–9. doi: 10.1016/j.bjoms.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Guarda-Nardini L, Manfredini D, Ferronato G. Arthrocentesis of the temporomandibular joint: A proposal for a single-needle technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:483–6. doi: 10.1016/j.tripleo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Neeli AS, Umarani M, Kotrashetti SM, Baliga S. Arthrocentesis for the treatment of internal derangement of the temporomandibular joint. J Maxillofac Oral Surg. 2010;9:350–4. doi: 10.1007/s12663-010-0155-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guarda-Nardini L, Ferronato G, Manfredini D. Two-needle vs. Single-needle technique for TMJ arthrocentesis plus hyaluronic acid injections: A comparative trial over a six-month follow up. Int J Oral Maxillofac Surg. 2012;41:506–13. doi: 10.1016/j.ijom.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 34.Reddy R, Reddy VS, Reddy S, Reddy S. Arthrocentesis – A minimally invasive treatment of temporomandibular joint dysfunction: Our experience. J Dr NTR Univ Health Sci. 2013;2:196–200. [Google Scholar]
- 35.Warnke T, Carls FR, Sailer HF. A new method for assessing the temporomandibular joint quantitatively by dental scan. J Craniomaxillofac Surg. 1996;24:168–72. doi: 10.1016/s1010-5182(96)80051-5. [DOI] [PubMed] [Google Scholar]
- 36.Nagori SA, Chattopadhyay PK, Kumar S, Kamalpathey K. Custom-made mouth prop for TMJ arthrocentesis: A technical note. Oral Maxillofac Surg. 2017;21:75–7. doi: 10.1007/s10006-016-0601-2. [DOI] [PubMed] [Google Scholar]
- 37.Tvrdy P, Heinz P, Pink R. Arthrocentesis of the temporomandibular joint: A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159:31–4. doi: 10.5507/bp.2013.026. [DOI] [PubMed] [Google Scholar]
- 38.Laskin DM. Needle placement for arthrocentesis. J Oral Maxillofac Surg. 1998;56:907. doi: 10.1016/s0278-2391(98)90043-x. [DOI] [PubMed] [Google Scholar]
- 39.Alkan A, Etöz OA. A new anatomical landmark to simplify temporomandibular joint arthrocentesis. Br J Oral Maxillofac Surg. 2010;48:310–1. doi: 10.1016/j.bjoms.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 40.Guarda-Nardini L, Masiero S, Marioni G. Conservative treatment of temporomandibular joint osteoarthrosis: Intra-articular injection of sodium hyaluronate. J Oral Rehabil. 2005;32:729–34. doi: 10.1111/j.1365-2842.2005.01505.x. [DOI] [PubMed] [Google Scholar]
- 41.Manfredini D, Guarda-Nardini L, Ferronato G. Single-needle temporomandibular joint arthrocentesis with hyaluronic acid injections. Preliminary data after a five-injection protocol. Minerva Stomatol. 2009;58:471–8. [PubMed] [Google Scholar]
- 42.Nitzan DW, Etsion I. Adhesive force: The underlying cause of the disc anchorage to the fossa and/or eminence in the temporomandibular joint – A new concept. Int J Oral Maxillofac Surg. 2002;31:94–9. doi: 10.1054/ijom.2001.0153. [DOI] [PubMed] [Google Scholar]
- 43.Guarda Nardini L, Tito R, Beltrame A. Treatment of temporo-mandibular joint closed-lock using intra-articular injection of mepivacaine with immediate resolution durable in time (six months follow-up) Minerva Stomatol. 2002;51:21–8. [PubMed] [Google Scholar]
- 44.Sindel A, Uzuner F, Sindel M, Tozoğlu S. Comparison of the efficiency of irrigation of single and double-needle techniques of temporomandibular joint arthrocentesis: A cadaver study. Cranio. 2017;35:405–9. doi: 10.1080/08869634.2017.1279825. [DOI] [PubMed] [Google Scholar]
- 45.Şentürk MF, Tüzüner-Öncül AM, Cambazoğlu M. Prospective short term comparison of outcomes after single or double puncture arthrocentesis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2016;54:26–9. doi: 10.1016/j.bjoms.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 46.Şentürk MF, Yıldırım D, Bilgir E, Fındık Y, Baykul T. Long-term evaluation of single-puncture temporomandibular joint arthrocentesis in patients with unilateral temporomandibular disorders. Int J Oral Maxillofac Surg. 2018;47:98–102. doi: 10.1016/j.ijom.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 47.Alkan A, Baş B. The use of double-needle canula method for temporomandibular joint arthrocentesis: Clinical report. Eur J Dent. 2007;1:179–82. [PMC free article] [PubMed] [Google Scholar]
- 48.Rehman KU, Hall T. Single needle arthrocentesis. Br J Oral Maxillofac Surg. 2009;47:403–4. doi: 10.1016/j.bjoms.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 49.Talaat W, Ghoneim MM, Elsholkamy M. Single-needle arthrocentesis (Shepard cannula) vs. Double-needle arthrocentesis for treating disc displacement without reduction. Cranio. 2016;34:296–302. doi: 10.1080/08869634.2015.1106810. [DOI] [PubMed] [Google Scholar]
- 50.Alkan A, Kilic E. A new approach to arthrocentesis of the temporomandibular joint. Int J Oral Maxillofac Surg. 2009;38:85–6. doi: 10.1016/j.ijom.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Öreroğlu AR, Özkaya Ö, Öztürk MB, Bingöl D, Akan M. Concentric-needle cannula method for single-puncture arthrocentesis in temporomandibular joint disease: An inexpensive and feasible technique. J Oral Maxillofac Surg. 2011;69:2334–8. doi: 10.1016/j.joms.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 52.Yura S, Totsuka Y. Relationship between effectiveness of arthrocentesis under sufficient pressure and conditions of the temporomandibular joint. J Oral Maxillofac Surg. 2005;63:225–8. doi: 10.1016/j.joms.2004.06.053. [DOI] [PubMed] [Google Scholar]
- 53.Al-Belasy FA, Dolwick MF. Arthrocentesis for the treatment of temporomandibular joint closed lock: A review article. Int J Oral Maxillofac Surg. 2007;36:773–82. doi: 10.1016/j.ijom.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 54.Zardeneta G, Milam SB, Schmitz JP. Elution of proteins by continuous temporomandibular joint arthrocentesis. J Oral Maxillofac Surg. 1997;55:709–16. doi: 10.1016/s0278-2391(97)90583-8. [DOI] [PubMed] [Google Scholar]
- 55.Sanromán JF. Closed lock (MRI fixed disc): A comparison of arthrocentesis and arthroscopy. Int J Oral Maxillofac Surg. 2004;33:344–8. doi: 10.1016/j.ijom.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 56.Shinjo H, Nakata K, Shino K, Hamada M, Nakamura N, Mae T, et al. Effect of irrigation solutions for arthroscopic surgery on intraarticular tissue: Comparison in human meniscus-derived primary cell culture between lactate ringer's solution and saline solution. J Orthop Res. 2002;20:1305–10. doi: 10.1016/S0736-0266(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 57.Ebenezer V, Balakrishnan R, Vivek M, Elumalai M. Usage of Ringer's lactate treatment in temporomandibular joint disorder. Biomed Pharmacol J. 2012;5:345–9. [Google Scholar]
- 58.Dolwick MF. Temporomandibular joint surgery for internal derangement. Dent Clin North Am. 2007;51:195–208. doi: 10.1016/j.cden.2006.10.003. vii-viii. [DOI] [PubMed] [Google Scholar]
- 59.Yura S, Totsuka Y, Yoshikawa T, Inoue N. Can arthrocentesis release intracapsular adhesions? Arthroscopic findings before and after irrigation under sufficient hydraulic pressure. J Oral Maxillofac Surg. 2003;61:1253–6. doi: 10.1016/s0278-2391(03)00724-9. [DOI] [PubMed] [Google Scholar]
- 60.Ohnishi M. Arthroscopy and arthroscopic surgery of the temporomandibular joint (TMJ) Rev Stomatol Chir Maxillofac. 1990;91(2):143–50. [PubMed] [Google Scholar]
- 61.Laskin DM, Greene CS, Hylander WL. 1st ed. Chicago: Quintessence; 2006. Temporamandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment; pp. 441–81. [Google Scholar]
- 62.Wenneberg B, Koop S, Grondahl HG. Long term effect of intra-articular injections of glucocorticosteroids into the TMJ: a clinical and radiographic 8 year follow up. J Craniomandib Disord. 1991;5:11–8. [PubMed] [Google Scholar]
- 63.Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg. 2006;64:949–51. doi: 10.1016/j.joms.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 64.Kunjur J, Anand R, Brennan PA, Ilankovan V. An audit of 405 temporomandibular joint arthrocentesis with intra-articular morphine infusion. Br J Oral Maxillofac Surg. 2003;41:29–31. doi: 10.1016/s0266-4356(02)00286-3. [DOI] [PubMed] [Google Scholar]
- 65.Furst IM, Kryshtalskyj B, Weinberg S. The use of intra-articular opioids and bupivacaine for analgesia following temporomandibular joint arthroscopy: A prospective, randomized trial. J Oral Maxillofac Surg. 2001;59:979–83. doi: 10.1053/joms.2001.25820. [DOI] [PubMed] [Google Scholar]
- 66.Nitzan DW, Price A. The use of arthrocentesis for the treatment of osteoarthritic temporomandibular joints. J Oral Maxillofac Surg. 2001;59:1154–9. doi: 10.1053/joms.2001.26716. [DOI] [PubMed] [Google Scholar]
- 67.Emshoff R. Clinical factors affecting the outcome of arthrocentesis and hydraulic distension of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:409–14. doi: 10.1016/j.tripleo.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 68.Carvajal WA, Laskin DM. Long-term evaluation of arthrocentesis for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2000;58:852–5. doi: 10.1053/joms.2000.8201. [DOI] [PubMed] [Google Scholar]
- 69.Alpaslan C, Dolwick MF, Heft MW. Five-year retrospective evaluation of temporomandibular joint arthrocentesis. Int J Oral Maxillofac Surg. 2003;32:263–7. doi: 10.1054/ijom.2003.0371. [DOI] [PubMed] [Google Scholar]
- 70.Frost DE, Kendell BD. Part II: The use of arthrocentesis for treatment of temporomandibular joint disorders. J Oral Maxillofac Surg. 1999;57:583–7. doi: 10.1016/s0278-2391(99)90080-0. [DOI] [PubMed] [Google Scholar]
- 71.Thomas H, Neelakantan RS, Thomas TK. Role of arthrocentesis in the management of acute closed lock of TM joint: A pilot study. J Maxillofac Oral Surg. 2012;11:390–3. doi: 10.1007/s12663-012-0354-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nitzan DW. Arthrocentesis for management of severe closed lock of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1994;6:245–57. [Google Scholar]
- 73.Singh S, Varghese D. Single puncture arthrocentesis of temporomandibular joint; introducing a novel device: A pilot study. Natl J Maxillofac Surg. 2013;4:193–7. doi: 10.4103/0975-5950.127650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fonseca R, Marciani R, Turvey T. 2nd ed. St. Louis (MO): Saunders, Elsevier; 2009. Oral and Maxillofacial Surgery; pp. 833–815. [Google Scholar]
- 75.Emshoff R, Puffer P, Rudisch A, Gassner R. Temporomandibular joint pain: Relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-alpha. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:442–9. doi: 10.1067/moe.2000.108801. [DOI] [PubMed] [Google Scholar]
- 76.Emshoff R, Rudisch A. Are internal derangement and osteoarthrosis linked to changes in clinical outcome measures of arthrocentesis of the temporomandibular joint? J Oral Maxillofac Surg. 2003;61:1162–7. doi: 10.1016/s0278-2391(03)00676-1. [DOI] [PubMed] [Google Scholar]
- 77.Vaira LA, Raho MT, Soma D, Salzano G, Dell’aversana Orabona G, Piombino P, et al. Complications and post-operative sequelae of temporomandibular joint arthrocentesis. Cranio. 2018;36:264–7. doi: 10.1080/08869634.2017.1341138. [DOI] [PubMed] [Google Scholar]
- 78.McCain JP, Sanders B, Koslin MG, Quinn JH, Peters PB, Indresano AT, et al. Temporomandibular joint arthroscopy: A 6-year multicenter retrospective study of 4,831 joints. J Oral Maxillofac Surg. 1992;50:926–30. doi: 10.1016/0278-2391(92)90047-4. Erratum in: J Oral Maxillofac Surg 1992;50:1349. [DOI] [PubMed] [Google Scholar]
- 79.Tsuyama M, Kondoh T, Seto K, Fukuda J. Complications of temporomandibular joint arthroscopy: A retrospective analysis of 301 lysis and lavage procedures performed using the triangulation technique. J Oral Maxillofac Surg. 2000;58:500–5. doi: 10.1016/s0278-2391(00)90010-7. [DOI] [PubMed] [Google Scholar]
- 80.González-García R, Rodríguez-Campo FJ, Escorial-Hernández V, Muñoz-Guerra MF, Sastre-Pérez J, Naval-Gías L, et al. Complications of temporomandibular joint arthroscopy: A retrospective analytic study of 670 arthroscopic procedures. J Oral Maxillofac Surg. 2006;64:1587–91. doi: 10.1016/j.joms.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 81.Rahal A, Poirier J, Ahmarani C. Single-puncture arthrocentesis – Introducing a new technique and a novel device. J Oral Maxillofac Surg. 2009;67:1771–3. doi: 10.1016/j.joms.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 82.Carls FR, Engelke W, Locher MC, Sailer HF. Complications following arthroscopy of the temporomandibular joint: Analysis covering a 10-year period (451 arthroscopies) J Craniomaxillofac Surg. 1996;24:12–5. doi: 10.1016/s1010-5182(96)80071-0. [DOI] [PubMed] [Google Scholar]
- 83.McCain JP. Complications of TMJ arthroscopy. J Oral Maxillofac Surg. 1988;46:256. doi: 10.1016/0278-2391(88)90002-x. [DOI] [PubMed] [Google Scholar]
- 84.McCain JP, de la Rua H. Foreign body retrieval: A complication of TMJ arthroscopy. Report of a case. J Oral Maxillofac Surg. 1989;47:1221–5. doi: 10.1016/0278-2391(89)90019-0. [DOI] [PubMed] [Google Scholar]
- 85.Murphy MA, Silvester KC, Chan TY. Extradural haematoma after temporomandibular joint arthroscopy. A case report. Int J Oral Maxillofac Surg. 1993;22:332–5. doi: 10.1016/s0901-5027(05)80660-5. [DOI] [PubMed] [Google Scholar]
- 86.Koslin MG. Advanced arthroscopic surgery. Oral Maxillofac Surg Clin North Am. 2006;18:329–43, vi. doi: 10.1016/j.coms.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 87.Holmlund A, Gynther G, Axelsson S. Efficacy of arthroscopic lysis and lavage in patients with chronic locking of the temporomandibular joint. Int J Oral Maxillofac Surg. 1994;23:262–5. doi: 10.1016/s0901-5027(05)80104-3. [DOI] [PubMed] [Google Scholar]
- 88.Reitzen SD, Babb JS, Lalwani AK. Significance and reliability of the house-brackmann grading system for regional facial nerve function. Otolaryngol Head Neck Surg. 2009;140:154–8. doi: 10.1016/j.otohns.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 89.Vaira LA, Soma D, Meloni SM, Dellàversana Orabona G, Piombino P, De Riu G, et al. Vertiginous crisis following temporomandibular joint athrocentesis: A case report. Oral Maxillofac Surg. 2017;21:79–81. doi: 10.1007/s10006-016-0603-0. [DOI] [PubMed] [Google Scholar]
- 90.Tutamayi SH, Al-Kamali RK. Arthrocentesis versus conservative treatments for TMJ dysfunctions: A preliminary prospective study. Zanco J Med Sci. 2014;18:739–45. [Google Scholar]
- 91.Murakami K, Hosaka H, Moriya Y, Segami N, Iizuka T. Short-term treatment outcome study for the management of temporomandibular joint closed lock. A comparison of arthrocentesis to nonsurgical therapy and arthroscopic lysis and lavage. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:253–7. doi: 10.1016/s1079-2104(05)80379-8. [DOI] [PubMed] [Google Scholar]
- 92.Hosaka H, Murakami K, Goto K, Iizuka T. Outcome of arthrocentesis for temporomandibular joint with closed lock at 3 years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:501–4. doi: 10.1016/s1079-2104(96)80193-4. [DOI] [PubMed] [Google Scholar]
- 93.Nitzan DW, Samson B, Better H. Long-term outcome of arthrocentesis for sudden-onset, persistent, severe closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997;55:151–7. doi: 10.1016/s0278-2391(97)90233-0. [DOI] [PubMed] [Google Scholar]
- 94.Murakami K, Segami N, Okamoto M, Yamamura I, Takahashi K, Tsuboi Y. Outcome of Arthroscopic Surgery for Internal Derangement of the Temperomandibular Joint: Long-term results covering 10 years. J Craniomaxillofac Surg. 2000;28(5):264–71. doi: 10.1054/jcms.2000.0162. [DOI] [PubMed] [Google Scholar]
- 95.Kim YH, Jeong TM, Pang KM, Song SI. Influencing factor on the prognosis of arthrocentesis. J Korean Assoc Oral Maxillofac Surg. 2014;40:155–9. doi: 10.5125/jkaoms.2014.40.4.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Guarda-Nardini L, Olivo M, Ferronato G, Salmaso L, Bonnini S, Manfredini D, et al. Treatment effectiveness of arthrocentesis plus hyaluronic acid injections in different age groups of patients with temporomandibular joint osteoarthritis. J Oral Maxillofac Surg. 2012;70:2048–56. doi: 10.1016/j.joms.2012.05.018. [DOI] [PubMed] [Google Scholar]


