Abstract
Chronic diffuse sclerosing osteomyelitis (CDSO) is a disease that presents a rather unusual clinicoradiographic picture creating diagnostic and therapeutic problems. Involvement of the temporomandibular joint is not frequently observed in CDSO. We report a unique case of a 37-year-old male with cyclic episodes of insidious swelling and progressive trismus for the past 4 years. Each episode was followed by spontaneous remission after 2 weeks. Radiographic examination detected unilateral coarse trabeculae with ground-glass appearance of the left hemimandible and resorption of ipsilateral condyle. Computed tomography demonstrated endosteal sclerosis, cortical thickening, and condylar resorption, while magnetic resonance imaging revealed altered marrow intensity with postcontrast enhancement of the surrounding musculature. Bone histopathology was consistent with the diagnosis of osteomyelitis. Palliative antibiotic therapy and regular follow-up were recommended. Of particular interest in the present case is ipsilateral condylar resorption not associated with any dermato-skeletal conditions, which is uncommon in CDSO of the mandible.
Keywords: Condyle, osteomyelitis, sclerosis, temporomandibular joint, trismus
INTRODUCTION
Chronic diffuse sclerosing osteomyelitis (CDSO) as stated by Jacobsson is an uncommon disease that creates diagnostic and therapeutic dilemma. A predominantly endosteal proliferative reaction of the mandible to a low-grade infection and a cyclic course with symptom-free intervals are characteristic of CDSO.[1,2] The possibility is seldom considered, simply due to rarity of the disease.[1,3]
This condition predominantly affects the body of mandible. Temporomandibular joint (TMJ) involvement with resorption, ankylosis, or osteitis of adjacent bones does not frequently occur,[4] and reports of condylar resorption in CDSO are minimal despite numerous reports of sclerosis of mandible.[1,3,5,6,7] Although Baltensperger demonstrated mild destruction of the condyle in 6 of the 30 assessed cases, these patients also presented with skin manifestations consistent with the diagnosis of synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome.[8] Similar association of condylar resorption with SAPHO syndrome has been reported in literature.[4,9,10]
Herein, we report a peculiar case of CDSO of the left hemimandible with ipsilateral condylar resorption, not associated with any dermato-skeletal conditions, as seen in the past literature. The extent of the disease is clearly illustrated by computed tomography (CT) and magnetic resonance imaging (MRI). To the best of our knowledge, condylar resorption in CDSO without underlying systemic diseases, syndromes, or multifocal skeletal defects is relatively uncommon.
CASE REPORT
Patient history
A 37-year-old male patient reported to the Department of Oral Medicine and Radiology of this institution with a complaint of recurrent episodes of swelling with trismus for 4 years. There was no history of trauma, paresthesia, or skin lesions and no significant past medical or family history.
His dental history was significant for extraction of carious mandibular left third molar due to painful swelling, followed by complete resolution. After 2 months, the first episode of a sudden swelling occurred in the same region, with pain and trismus. The swelling began in the left submandibular region and gradually spread to the left masseteric region. He was advised antibiotics by a private physician, after which the symptoms resolved but reappeared within 2 months. The episodes recurred, with approximately eight episodes in a span of 1 year. Each episode began with a swelling, followed by restricted mouth-opening lasting for 2 weeks, followed by gradual resolution of swelling. The panoramic radiograph taken did not reveal any active infectious foci. However, there was evidence of mild mandibular sclerosis that was overlooked.
Clinical examination
Extraoral examination revealed facial asymmetry with a diffuse swelling over the left masseter region, approximately 7 cm × 5 cm in size [Figure 1a], afebrile, nontender, firm too hard on palpation, and overlying skin appeared taut. Mouth-opening restricted to 5 mm interincisal distance. No intraoral focus of infection was detected, and electric pulp vitality testing displayed vital response for all mandibular teeth. Provisional diagnosis of trismus secondary to chronic infection was suggested, as the present condition could be sequelae of the past acute lesion. The differential diagnosis of masseter hypertrophy and atraumatic variant of myositis ossificans was considered since these conditions are associated with long-term progressive trismus and swelling in the absence of dental infection. However, they do not explain the cyclic nature and spontaneous remission of the symptoms seen in this case.
Figure 1.

(a) Frontal view of a 37-year-old male with unilateral swelling over the left masseter region (arrow) extending superoinferiorly from the level of the zygomatic arch to the inferior border of the mandible and anteroposteriorly extending from the malar region to the tragus. (b) Panoramic radiograph demonstrating unilateral homogeneous sclerosis (ground-glass appearance) of the left hemimandible
Radiographic examination
Intraoral periapical radiographs showed a coarse trabecular pattern (sclerotic appearance) in mandibular left premolar and molar region. Panoramic radiography revealed unilateral diffuse sclerosis of the left hemimandible with ground-glass appearance, extending from distal aspect of the left canine region to the ipsilateral condyle, involving the body, ramus, condyle, and coronoid process with prominent condylar head resorption [Figure 1b]. Anteriorly, the periphery of the sclerotic bone appeared to merge with the adjacent normal bone. The left inferior alveolar nerve canal (IANC) was visible, coursing through the medullary sclerosis without deviation. However, the cortex of the left IANC was indistinct, with a radiodensity similar to surrounding sclerotic trabeculae.
On comparison with the past panoramic radiograph, we could appreciate the significant resorption of left condyle that occurred over a span of 3 years, along with narrowing of the left sigmoid notch due to unilateral hyperostosis. Multislice CT examination detected left hemimandibular extensive endosteal sclerosis, a well-preserved intact anatomy with cortical thickening and mild periosteal bone formation. Condylar head resorption and loss of demarcation of the cortical-medullary border were also noted [Figures 2 and 3]. Sclerosis was the predominant appearance with lack of osteolysis.
Figure 2.
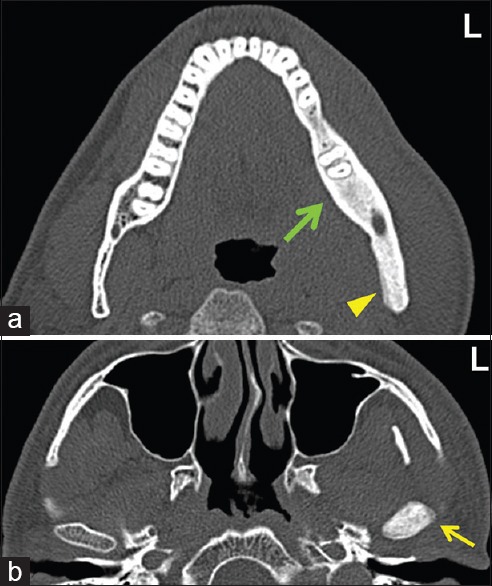
(a) Axial computed tomography image showing extensive medullary sclerosis of the left hemimandible (arrow), unilateral thickening of the cortex, and mild periosteal new bone formation on posterior aspect of the left ramus (arrowhead). (b) Image showing Increased marrow density of the left condyle (arrow) with loss of demarcation of the cortical-medullary border
Figure 3.
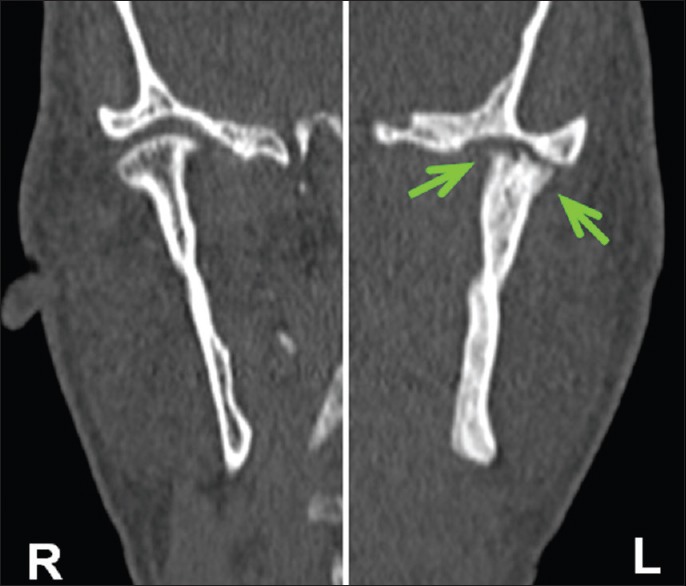
Coronal computed tomography (cropped) images showing sclerosis and resorption of the left condyle (arrows)
MRI revealed an altered marrow signal intensity of the left hemimandible appearing hypointense on TI-weighted images and hyperintense on T2-weighted images [Figure 4]. Postgadolinium contrast images demonstrated unilateral intramedullary enhancement, with enhancement of overlying musculature such as the left buccinator, masseter, medial and lateral pterygoid, mylohyoid, and hyoglossus muscles [Figure 5]. This suggested a diagnosis of diffuse sclerosing osteomyelitis of the left hemimandible with inflammatory changes in soft-tissue spaces and ipsilateral condylar resorption. Owing to the overall radiographic appearance, a diagnosis of diffuse sclerosing osteomyelitis was suggested.
Figure 4.
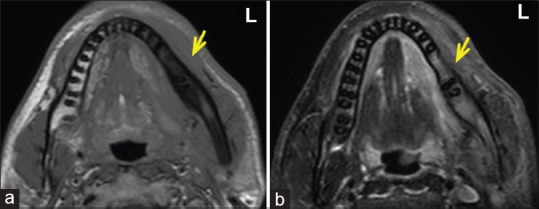
Axial magnetic resonance imaging sections showing left hemimandible (arrow) appearing (a) hypointense on TI-weighted image and (b) hyperintense on T2-weighted image
Figure 5.
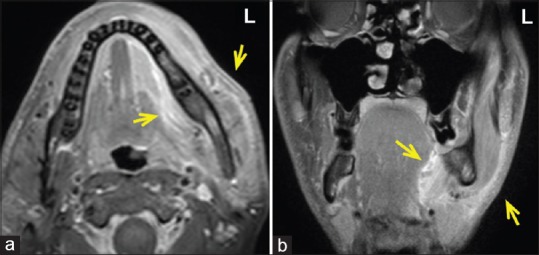
Postgadolinium T1-weighted images showing unilateral intramedullary enhancement, along with ill-defined enhancement of the overlying soft tissues (a) hypertrophic and hyperintense appearance of the left masseter and mylohyoid muscles (arrows) and (b) hyperintensity of the left buccinator and hyoglossus muscles (arrows)
Laboratory investigations
Erythrocyte sedimentation rate was 66 mm/h, and C-reactive protein was also elevated (11.9 mg/dl). Other blood investigations were within normal limits. Bone culture predominantly showed lymphocytes; histopathology revealed few devitalized and viable bony fragments with fibrocollagenous tissue, lymphocyte infiltration, hemorrhage, and few congested capillaries. These features were consistent with the diagnosis of chronic osteomyelitis.
Surgical treatment of such a diffuse lesion is not recommended; and hence, hyperbaric oxygen therapy was advised. However, due to financial constraints, the patient was unwilling to undergo the advised treatment. Palliative antibiotic therapy with tablet Augmentin 625 mg TDS for 5 days (Amoxicillin 500 mg + Clavulanic Acid 125 mg) as and when the episodes occur and regular follow-up was recommended.
DISCUSSION
The term CDSO is primarily descriptive of the radiological appearance of a pathological bone reaction.[2] CDSO, also known as osteomyelitis sicca, primary chronic osteomyelitis, chronic sclerosing nonsuppurative osteomyelitis, or reactive hyperplasia of bone,[1] is a rare disease of unknown etiology, insidious in onset, and lacks an acute state.[2]
CDSO can occur at any age from 10 to 72 years[3] and is characterized by a nonsuppurative process of recurrent swelling, trismus, and dull pain.[5] It commonly affects the body of the mandible. However, Kodama et al. reported disease progression leading to the involvement of TMJ and temporal bone through extension of sclerosis from the ramus.[4] Similarly, the present case displayed extensive sclerosis along with an unusual finding of significant condylar resorption. Previous literature suggests that resorption by gradual reduction of the affected mandibular volume is a natural attempt to restore the balance between available circulatory capacity and tissue volume.[1]
The entity CDSO is reported to be a localized form of chronic recurrent multifocal osteomyelitis (CRMO) due to their identical clinical course, radiological, and histopathological features.[3,9,10] CRMO is multifocal, but mandibular involvement is uncommon, and our patient did not present with multifocal skeletal manifestations as seen in CRMO. Some authors also consider CDSO to be a mandibular localization of SAPHO syndrome, with typical features being medullary sclerosis, subcortical erosions, and ankylosis of the condyle along with skin manifestations.[4] Reports of condylar resorption associated with SAPHO syndrome have also been documented.[4,9,10] The present case did not present with any dermatological manifestations. In contrast to previous reports, of particular interest in our case is the presence of condylar resorption, which is uncommon in true CDSO.
There are multiple confounding contributors toward disease progression which makes diagnostic isolation a challenge. Low virulence organisms are of etiological importance in intramedullary osseous infection causing sclerosis.[1,6] However, bone cultures fail to be conclusive.[1,2,3] In the present case, history of cyclic episodes and predomination of lymphocytes could explain the presence of a chronic low-grade infection.
CT reveals the variable degree of hyperostosis and sclerosis, which are the most striking patterns seen in CDSO. Involvement of the cortical bone results in thickening and sometimes visible loss of the cortical-medullar border, rendering cortical bone is indistinguishable from cancellous bone, as seen in the present case. On MRI, edematous marrow with high-signal intensity is evident on T2-weighted images.[9] CT evaluation or combination of CT with MRI is optimal, as CT provides a distinctive appearance of the sclerotic bone, while MRI defines the extent of the inflammatory process.[10]
The management with long-term antibiotic therapy in early stages of the disease can have a beneficial effect by shortening the clinical episode.[1,6] In chronic stage, however, surgical decortication combined with antimicrobial therapy might be the most effective treatment.[6,7] Considering the extensive mandibular involvement in the present case, surgical treatment was not recommended as the bone in CDSO is hypovascular and healing will be protracted. Hyperbaric oxygen therapy is recommended as lowered oxygen tension and anaerobic infection are presumed.[7] Several reports have suggested promising results with bisphosphonates as they decrease bone resorption and bone turnover.[6,7] However, bisphosphonates are still far from being a standard of care in the treatment of CDSO due to several reasons, one being the risk of inducing osteonecrosis.[7]
CONCLUSION
CDSO commonly affects the mandibular body; however, the present case demonstrated radiographic evidence of endosteal sclerosis extending up to the condylar head, leading to significant resorption. As this case presented with unspecific clinical symptoms, absence of an acute state of infection, and had an obscure etiology; it was important to review the whole course of the disease and utilize various imaging modalities to establish the correct diagnosis. Its localized occurrence with lack of association with commonly reported conditions such as CRMO and SAPHO syndrome created a diagnostic dilemma. The entity remains a diagnosis of exclusion; sufficient knowledge and awareness of the condition are imperative as it can aid in early diagnosis which perhaps will result in a less morbid intervention for resolution.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jacobsson S. Diffuse sclerosing osteomyelitis of the mandible. Int J Oral Surg. 1984;13:363–85. doi: 10.1016/s0300-9785(84)80062-9. [DOI] [PubMed] [Google Scholar]
- 2.Baltensperger MM, Eyrich GK. Berlin: Springer Verlag; 2008. Osteomyelitis of the Jaws; pp. 5–50. [Google Scholar]
- 3.van Merkesteyn JP, Groot RH, Bras J, McCarroll RS, Bakker DJ. Diffuse sclerosing osteomyelitis of the mandible: A new concept of its etiology. Oral Surg Oral Med Oral Pathol. 1990;70:414–9. doi: 10.1016/0030-4220(90)90200-c. [DOI] [PubMed] [Google Scholar]
- 4.Kodama Y, Tanaka R, Kurokawa A, Ohnuki H, Sultana S, Hayashi T, et al. Severe destruction of the temporomandibular joint with complete resorption of the condyle associated with synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e128–33. doi: 10.1016/j.oooo.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Marí A, Morla A, Melero M, Schiavone R, Rodríguez J. Diffuse sclerosing osteomyelitis (DSO) of the mandible in SAPHO syndrome: A novel approach with anti-TNF therapy. Systematic review. J Craniomaxillofac Surg. 2014;42:1990–6. doi: 10.1016/j.jcms.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Montonen M, Lindqvist C. Diagnosis and treatment of diffuse sclerosing osteomyelitis of the jaws. Oral Maxillofac Surg Clin North Am. 2003;15:69–78. doi: 10.1016/s1042-3699(02)00073-0. [DOI] [PubMed] [Google Scholar]
- 7.Soubrier M, Dubost JJ, Ristori JM, Sauvezie B, Bussière JL. Pamidronate in the treatment of diffuse sclerosing osteomyelitis of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:637–40. doi: 10.1067/moe.2001.119739. [DOI] [PubMed] [Google Scholar]
- 8.Baltensperger M, Grätz K, Bruder E, Lebeda R, Makek M, Eyrich G, et al. Is primary chronic osteomyelitis a uniform disease? Proposal of a classification based on a retrospective analysis of patients treated in the past 30 years. J Craniomaxillofac Surg. 2004;32:43–50. doi: 10.1016/j.jcms.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Monsour PA, Dalton JB. Chronic recurrent multifocal osteomyelitis involving the mandible: Case reports and review of the literature. Dentomaxillofac Radiol. 2010;39:184–90. doi: 10.1259/dmfr/23060413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel R, Jacob R, Lee K, Booth TN. Parotid swelling and chronic recurrent multifocal osteomyelitis of mandible in children. Int J Pediatr Otorhinolaryngol. 2015;79:47–52. doi: 10.1016/j.ijporl.2014.10.042. [DOI] [PubMed] [Google Scholar]


