Abstract
Aim:
The aim of this study was to provide insight about all the common fascial space infections of the neck, their presentation, their etiology, complaints, length of stay, and the treatment given.
Patients and Methods:
It was conducted in a tertiary center in Nadiad, Gujarat, India. A total of 1034 patients were treated for fascial space infections of the neck in the hospital from 2001 to 2017. There were 63.24% male and 36.75% female with age ranging from 21 days to 96 years having the mean age of 31.4 years.
Results:
Odontogenic infection with poor oral hygiene as a cause was found in most (78.43%) of the abscesses. Diabetes was the most common comorbid condition found in 98 (9.47%) patients along with HIV found in ten (0.96%) patients. Pain (99.41%), fever (86.07%), swelling (86.94%), and dysphagia/odynophagia (67.21%) were the most common presenting symptoms. Ludwig's angina and submandibular abscess were found to be the most common deep head-and-neck space infection making up for 52% cases. The most common group of microorganisms isolated were Streptococcus sp. (19.82%) and Staphylococcus aureus (18.66%).
Conclusion:
Treatment was given in the form of incision and drainage of the abscesses (83.69%) and systemic antibiotics (100%). The most common space infection among the deep neck infections is the submandibular space infection (52%). If the etiological factor was not removed which mostly was carious teeth, high chances of recurrence were found (27.27%). Four patients required tracheostomy, and there was one mortality in the entire series.
Keywords: Abscess, cervical fascia, Ludwig's angina, neck space infection, odontogenic infection
INTRODUCTION
Acute cervical space infection occurring in the fascial spaces of the neck is a common occurrence in rural areas where dental hygiene is poor. Previously, tonsillar and paratonsillar areas were common sites from which infections used to spread to the deep neck spaces. With evolution of the antimicrobial therapy, the incidence of these infections has come down and odontogenic causes are now the most common source of deep neck space infections. Deaths and complications too have reduced due to timely intervention and availability of newer antimicrobial therapy with broad-spectrum coverage.[1] But still, some cases of deep fascial space infections prove challenging, especially in immunocompromised patients such as those suffering from HIV or diabetes where the spread is sometimes very rapid and can cause morbidity and mortality.[2] Treatment in the form of incision and drainage is carried out in most of the patients with the administration of broad-spectrum antibiotics. Other life-saving interventions such as tracheostomy may be required, when the airway is compromised.
The aim of this study is to give an insight into the retrospective analysis of 1034 cases of deep neck infections reported to our tertiary center where we have comprehensively studied the neck spaces involved, the causative organisms, the comorbid conditions, the treatment offered, complications encountered, and how we managed them.
PATIENTS AND METHODS
Medical records of a total of 1034 patients were reviewed for deep cervical fascial space infections at a tertiary center at Nadiad, Gujarat, India, from January 2001 to December 2017. All the patients were admitted and treated in the same hospital. The acute infections involved the following fascial spaces: peritonsillar space, canine space, buccal space, masseteric space, sublingual space/submandibular space (Ludwig's angina), parapharyngeal space, retropharyngeal space, and pretracheal and prelaryngeal spaces.
There were 654 (63.24%) males and 380 (36.76%) females with age ranging from 21 days to 96 years having the mean age of 31.4 years. Postclinical examination in patients suspected to have deep neck space infection, radiological investigations were done in the form of ultrasonography (USG) or computerized tomography (CT) scan in case where the location and extent were not definite or to differentiate between cellulitis and abscess formation when there was doubt, especially in case of Ludwig's angina. Most of the deep abscesses – retropharyngeal and parapharyngeal abscesses were subject to radiological investigation in the form of a contrast CT scan, while the rest of them were either diagnosed clinically or using USG to confirm the extent, relationship with the neurovascular bundles and to decide the treatment plan. USG was performed on the patients using SAMSUNG RS 80 (South Korea) [Figure 1]. CT was performed on the patients in the supine position using PHILLIPS MX 16 CT SCAN (The Netherlands) [Figure 2]. Odontogenic infection as a cause was found in almost 78.43% of abscesses, foreign body in 0.58% of the cases, and infected tonsil in 10.15% of the cases. In the remaining cases, the abscesses could not be attributed to any particular cause. All the patients were monitored for possible threatening of airway obstruction, septicemia, and antibiotic therapy was started immediately without waiting for the culture and sensitivity. As these infections are of polymicrobial nature, combination therapy of broad-spectrum antibiotics is recommended for maximal antibiotic effect. Treatment was given in the form of incision and drainage of the abscesses (83.69%), and systemic antibiotics (100%) in the form of ceftriaxone + sulbactam (300 mg/kg body weight) and lincomycin (12 mg/kg body weight) were given intravenously (IV) 12 hourly for at least 3 days, followed by the same antibiotics given orally at least for 10 days. Spectrum sensitivity report normally takes around 4–5 days in the rural setup that we work in, and so we cannot wait for the same to initiate treatment. However, on retrospectively analyzing the spectrum sensitivity reports of our patients, 95% of our patients were sensitive to both the antibiotics used by us mentioned above, and 99% of the patients were sensitive to at least one of those antibiotics. Only seven cases in our study were resistant to both the antibiotics started by us. The causative organism in these cases was methicillin-resistant Staphylococcus aureus, which was sensitive to linezolid (a synthetic antibiotic of oxazolidinone class) and the same was started in the dose of 20 mg/kg/day in two divided doses. Supportive therapy, such as IV fluids, analgesics, and mouthwash, was given. Most patients presented with symptoms of pain, fever, dysphagia, and swelling. Some patients, however, also presented with symptoms such as trismus (10.44%), respiratory distress (0.34%), and change in voice (0.19%). Routine blood investigations done in all cases were hemogram, serum glutamate pyruvate transaminase, random blood sugar, serum creatinine, serum HIV, and hepatitis B surface antigen. Patients were followed up for at least 3-month postoperatively.
Figure 1.
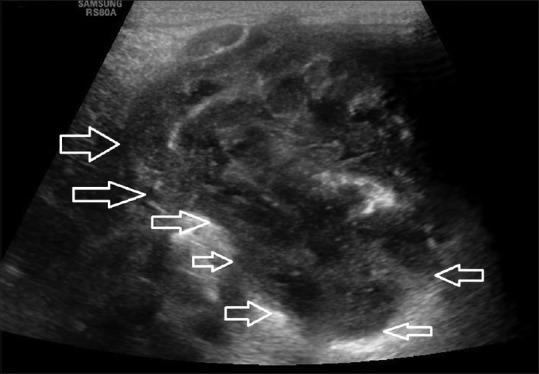
Ultrasound image revealing ill-defined loculated collection deep to sternocleidomastoid muscle extending to parapharyngeal space
Figure 2.

Computerized tomography scan postcontrast sagittal image of the neck reveals well-defined peripherally enhancing cystic lesion at anterior triangle extending to supraclavicular region suggestive of retropharyngeal abscess
RESULTS
Incidence of different fascial space infections of the neck
There were 654 male (63.25%) and 380 female (36.75%) in the study involving various spaces. The incidence of various types of space infections in 1034 patients is given in Figure 3.
Figure 3.
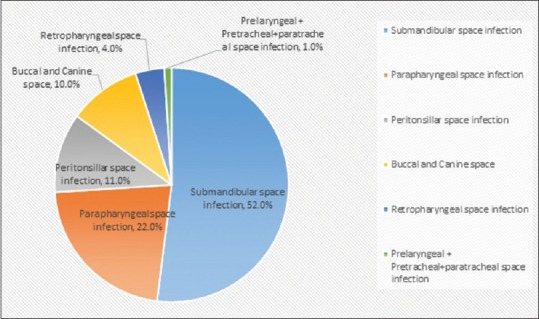
Pie chart showing the incidence of various space infections in our study
Of the 1034 patients, 538 (52%) patients had submandibular and sublingual space infection (Ludwig's angina). The second most common space infection was parapharyngeal space infection which affected about 227 (22%) patients. This was then followed by peritonsillar infection affecting 114 (11%) patients. Various other fascial spaces involved were buccal and canine space infection affecting 104 (10%) patients; retropharyngeal space infection affecting 41 (4%) patients and paratracheal, pretracheal, and prelaryngeal space infections affecting 10 (1%) patients.
Average age of presentation
The mean age of the patients in this study was 31.4 years. The average age of patients having submandibular or sublingual space infection was 33 years. Similarly, the average age of patients affected by parapharyngeal space infection was 34 years, peritonsillar space infection was 32 years, and buccal and canine space infection was 45 years. The average age of patients affected by retropharyngeal space infection was 43 years, while that of pretracheal, para-tracheal, and prelaryngeal space infection was 39 years.
Common complaints
Pain was the most common presenting symptom and was found in all the patients in our study. Swelling, fever, trismus, and odynophagia were other common presenting symptoms. Respiratory distress was found in 1 (10%) patient of pre-/paratracheal infection, 2 (4.87%) patients of retropharyngeal space infection, and 1 (0.18%) patient of submandibular space infection. Change in voice was only noted in 2 (20%) cases of pre-/paratracheal space infection. Detailed format is given in Figure 4.
Figure 4.
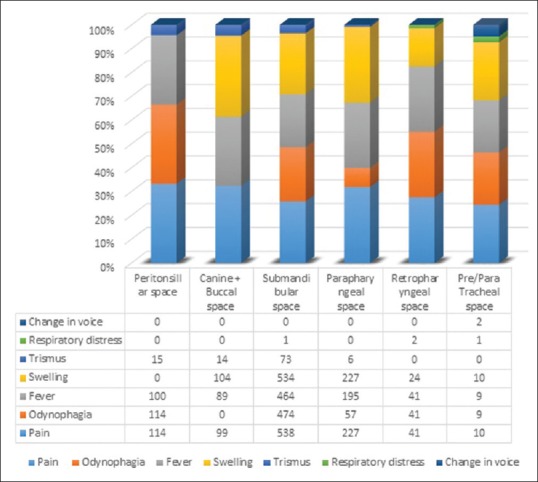
Common complaints seen in various space infections
Etiology
In general, 78.43% of all the space infections of the neck had odontogenic origin. In submandibular space infection, odontogenic origin made up to 495 (92%) cases as the etiological cause, followed by sialadenitis in 2 (0.37%) cases. Peritonsillar space infection occurred mostly due to the tonsillar etiology in 85 (74.56%) cases, followed by odontogenic cause in 14 (12.28%) cases and foreign body involvement in 2 (1.75%) cases. Parapharyngeal space infection occurred mostly due to odontogenic cause in 180 (79.29%) cases, followed by tonsillar infection in 18 (7.92%) cases. Chief etiology for canine + buccal space infection in our study was of the odontogenic origin found in 89 (85.57%) patients. The main etiological factor for retropharyngeal space infection in our study was odontogenic infection, which was seen in 33 (80.48%) cases, followed by foreign body involvement in 2 (4.87%) cases. One such case is given in Figure 5a. Postoperative photographs are shown in Figure 5b and c. The causative factor for pre-/paratracheal + prelaryngeal infection was trauma, foreign body involvement, and thyroiditis in 2 (20%), 2 (20%), and 2 (20%) patients, respectively. In rest of the cases, no particular etiological factor could be attributed.
Figure 5.
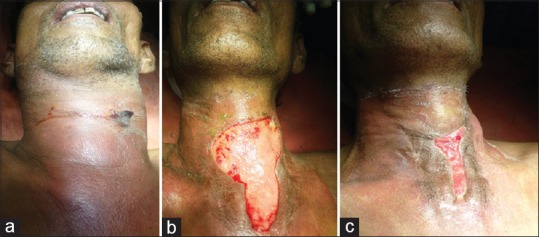
(a) Clinical photographs of a patient having retropharyngeal space infection – Preoperative photograph. (b) 14th-day postoperative photograph. (c) 28th-day postoperative photograph
Comorbid conditions
In our study, the most common comorbid condition found was diabetes and HIV. Diabetes was found in 98 (9.47%) patients, while HIV was present in 10 (0.96%) patients.
Treatment given
Only 13 (11%) patients of peritonsillar space infection and 102 (19%) patients of submandibular space infection were treated by antibiotics alone. These 115 (11.12%) patients were treated with the combination of ceftriaxone + sulbactam and lincomycin along with supportive therapy as mentioned previously. Rest all the patients were treated by a combined approach of surgery in the form of incision and drainage and injectable broad-spectrum antibiotics as mentioned previously.
Other interventions required
Other interventions such as foreign body removal were carried out in one patient (0.87%) of peritonsillar space infection and two patients (4.87%) of retropharyngeal space infection. In cases where airway was compromised, tracheostomy was performed. It was performed in 1 (0.18%) patient of submandibular space infection, 1 (1%) patient of pre-/paratracheal space infection, and 2 (4.87%) patients of retropharyngeal space infection. The overall mortality rate was 0.1%. Revision surgery (incision and drainage) was required in 12 (1.16%) patients. All the patients had odontogenic infection as an etiological cause and had not undergone treatment for same post the first surgery.
Average length of stay in the hospital
Patients with deeper infections such as retropharyngeal and pre-/paratracheal and prelaryngeal fascial infections on an average take 7.5 and 8.4 days of hospital admission, respectively, which tells about the severity of the infection. Patients having parapharyngeal and submandibular space infection have an average hospital stay of 3.4 and 3.6 days, respectively, while that of peritonsillar and buccal/canine space infection have an average stay of 1.2 and 2.2 days, respectively.
Thus, deeper fascial neck infections such as retropharyngeal, pretracheal, paratracheal, and prelaryngeal space infections have a higher hospital stay requiring continuous in-hospital patient administration due to the increased severity of the infection. Patients with submandibular and parapharyngeal space infection have a lesser stay in the hospital as compared to the patients having retropharyngeal and pretracheal space infection explaining the better management and lesser comparative morbidity.
Complications
We had one mortality in the entire series (0.1%), and it was a patient of retropharyngeal abscess and the cause of death was mediastinitis. Revision surgery was required in 12 (1.16%) patients and most of these patients (0.58%) were of canine/buccal space infection as postprimary drainage of the abscess, they did not undergo treatment for their odontogenic infection. Recurrent laryngeal nerve palsy was noted in 1 (0.1%) patient who was having paratracheal abscess.
DISCUSSION
Submandibular space/sublingual space infection (Ludwig's angina) was the most commonly affected space in our study, followed by the parapharyngeal and peritonsillar space infection. In 52% of our patients, submandibular space/sublingual space was affected, while 22% of the patients had parapharyngeal space infection and in 11% of patients, the peritonsillar space infection was present. Probably, as odontogenic infection was the most common contributing factor (78.43%) for the fascial space infections in our study, the submandibular and sublingual spaces which are the ones in most proximity to the mandibular teeth were affected. For all the cases of space infection involving various spaces, broad-spectrum empirical antibiotic therapy should be started as soon as possible in all the patients, as early aggressive management prevents life-threatening complications such as descending mediastinitis, septic shock, upper airway obstruction, jugular vein thrombosis, cavernous septic embolus, carotid artery rupture, aorticopulmonary fistula, acute renal failure, and disseminated intravascular coagulation.[3,4] Many other space infection then get involved after the spread from submandibular space. Our findings were similar to many other studies found in the literature where too the submandibular/sublingual space was most commonly affected.[5,6]
The organisms most commonly isolated in our study were the ones which are usually found in the oral cavity and oropharynx. Mixed organisms having aerobic and anaerobic activity were found. Data for only 796 patients (76.98%) are available having positives cultures. The negative cultures may be due to the prior antibiotic therapy which would make it sterile. The number of culture reports which showed no organisms was 238 (23.02%). Various organisms had been isolated from the patients with the space infections. The culture was positive for 205 cases of Streptococcus viridans sp. (19.82%) and 193 cases of S. aureus (18.66%) which was also similar to those found in other studies.[1,7,8,9,10] Rest of the details are given in Table 1.
Table 1.
Various organisms isolated from the patients
| Organism | Number of patients |
|---|---|
| Negative culture | 238 |
| Streptococcus viridans sp. | 205 |
| Staphylococcus aureus | 193 |
| Neisseria sp. | 97 |
| Haemophilus sp. | 81 |
| Bacteroides | 72 |
| Non-A β-streptococcus | 58 |
| Streptococcus pyogenes | 41 |
| Fusobacterium | 29 |
| Prevotella | 12 |
| Eikenella | 8 |
In our study, there were 98 (9.48%) diabetic patients and 10 (0.96%) HIV patients; 29 patients among them were having the blood glucose under control by diet and exercise, and 51 patients were on oral medication for the same while the rest 18 patients were made stable using insulin. Ten patients (0.96%) were HIV affected for which antiretroviral therapy was started. The blood glucose control was done in the diabetic patients along with the initiation of the treatment. In the studies by Huang et al.[11] and Gujrathi et al.,[10] again diabetes was found to be the most common comorbid condition. Comparison of various studies and the present study is given in Figure 6.
Figure 6.
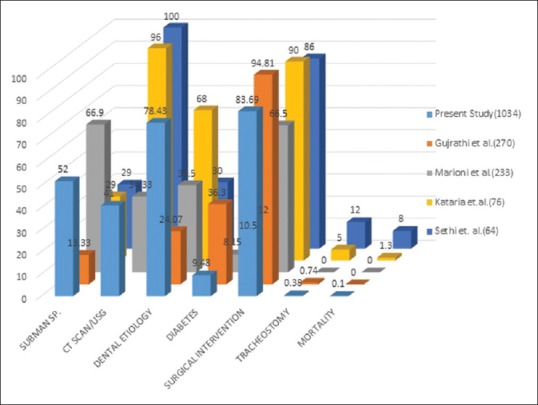
Comparison of the present work with previous other published relevant work in the literature regarding deep neck infections
The three important keys to successful management of any deep neck infections are: (1) protection and control of airway, (2) antibiotic therapy, and (3) surgical drainage.
As per Levitt's thinking, “antibiotics are not a substitute for surgery, they should be used in conjunction with proper surgical drainage.”[12] The empirical therapy to be started should focus on those organisms which are isolated commonly in the oral cavity such as Streptococcus species and S. aureus. Improvement on Gram-negative coverage should be taken into consideration in debilitated or immunocompromised patients. The duration of antibiotic culture should be decided on the patient's general condition such as healthy granulation, presence of slough, induration, decreasing of signs, and symptoms.
About 83.69% of the patients underwent surgical intervention along with antibiotic support, while in 11.12% of cases, only antibiotic administration sufficed which is almost the same as compared to the study by Sethi and Stanley.[13] Deep neck infection still at a cellulitis stage can be treated by antibiotics itself.[3] Surgical drainage should be established when the cellulitis stage is transformed in the abscess stage. However, in the absence of abscess stage, incision, and drainage is performed in those who deteriorate clinically or fail to improve after 2 days of initiation of the antibiotic therapy.[14]
Management of airway is most essential and challenging in treating patients with deep neck infections.[10] Har-El et al.[15] reported that the need for tracheotomy was common in retropharyngeal and submandibular abscesses. Whenever a patient of deep neck space infection presents with difficulty in breathing, tracheostomy becomes the gold standard and the first line of treatment to secure the airway and save the life of the patient.[16] Intubation is not preferred because of the extensive edema in the laryngopharynx and the risk of the abscess opening internally leading to aspiration when intubation is attempted. In our study also, tracheostomy was required in 0.38% cases of deep neck infections which is not consistent with the study by Kataria et al.[14] and Eftekharian et al.[17]
In our study, we treated 13 patients (11%) of peritonsillar space infection and 102 patients (19%) of submandibular space infection using antibiotics only. Significant number of these infections was not frank abscess but was cellulitis which may respond conservatively to the broad-spectrum antibiotic therapy only without the need of surgical intervention. Thus, 115 patients (11.12%) in our study were treated only using antibiotics. Surgical intervention was done in 83.69% of cases in our study, which was consistent with the studies by Mumtaz et al.,[18] Eftekharian et al.,[17] and Har-El et al.[15] with surgical intervention required in approximately 78%, 79%, and 90% of the cases, respectively.
The odontogenic infection was found to be the most common cause (78.43% of cases) in our present study for deep neck infections which is consistent with the study by Tschiassny[19] which had 70% of cases. Thus, treatment is not complete unless the etiological cause for the infection is removed. If incision and drainage is done without removing the cause, recurrence of the infection develops and a second surgery is required. In our study, 12 patients (1.16%) required revision surgery in the form of incision and drainage again along with the removal of the odontogenic cause.
CONCLUSION
According to our study, it could be concluded that the most common infection among the deep neck infections is the submandibular/sublingual space infection seen in 538 (52%) cases. The most common cause for the deep neck infections was odontogenic infection found in 811 cases making up to 78.43% of the total population.
If the etiologic cause is not removed primarily, high chances are present for the infection to recur. In our study, out of 44 cases wherein the etiologic cause (odontogenic) was not treated, 12 (27.27%) cases developed recurrence and revision surgery (incision and drainage) was required. The most common organisms isolated from the sites of infection were S. viridans sp. found in 205 (19.82%) cases and S. aureus found in 193 (18.66%) cases. The most common comorbid conditions were found to be diabetes, which was found in 98 (9.47%) cases and HIV which was found in 10 (0.96%) patients.
Retropharyngeal space infection is considered to be the most dreaded condition with high morbidity and mortality rates due to the space extending to the superior mediastinum, thus being a greater risk to the airway as well as complications such as mediastinitis. The only mortality that occurred in our study was of the patient having retropharyngeal space infection. Tracheostomy was required in two patients of the 41 patients (4.87%) of retropharyngeal infection indicating that of all the fascial spaces affected, it is associated with maximum morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Naresh Hundiya Imaging Center for the timely help with the scans.
REFERENCES
- 1.Agarwal AK, Sethi A, Sethi D, Mrig S, Chopra S. Role of socioeconomic factors in deep neck abscess: A prospective study of 120 patients. Br J Oral Maxillofac Surg. 2007;45:553–5. doi: 10.1016/j.bjoms.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Bottin R, Marioni G, Rinaldi R, Boninsegna M, Salvadori L, Staffieri A, et al. Deep neck infection: A present-day complication. A retrospective review of 83 cases (1998-2001) Eur Arch Otorhinolaryngol. 2003;260:576–9. doi: 10.1007/s00405-003-0634-7. [DOI] [PubMed] [Google Scholar]
- 3.Sakaguchi M, Sato S, Ishiyama T, Katsuno S, Taguchi K. Characterization and management of deep neck infections. Int J Oral Maxillofac Surg. 1997;26:131–4. doi: 10.1016/s0901-5027(05)80835-5. [DOI] [PubMed] [Google Scholar]
- 4.Bridgeman A, Wiesenfeld D, Hellyar A, Sheldon W. Major maxillofacial infections. An evaluation of 107 cases. Aust Dent J. 1995;40:281–8. doi: 10.1111/j.1834-7819.1995.tb04814.x. [DOI] [PubMed] [Google Scholar]
- 5.Parhiscar A, Har-El G. Deep neck abscess: A retrospective review of 210 cases. Ann Otol Rhinol Laryngol. 2001;110:1051–4. doi: 10.1177/000348940111001111. [DOI] [PubMed] [Google Scholar]
- 6.Meher R, Jain A, Sabharwal A, Gupta B, Singh I, Agarwal AK, et al. Deep neck abscess: A prospective study of 54 cases. J Laryngol Otol. 2005;119:299–302. doi: 10.1258/0022215054020395. [DOI] [PubMed] [Google Scholar]
- 7.Yang SW, Lee MH, See LC, Huang SH, Chen TM, Chen TA, et al. Deep neck abscess: An analysis of microbial etiology and the effectiveness of antibiotics. Infect Drug Resist. 2008;1:1–8. doi: 10.2147/idr.s3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhise SV, Rahmani F, Pawde AM. Clinical study of neck space abscesses in rural population. IOSR J Dent Med Sci. 2014;13:41–7. [Google Scholar]
- 9.Marioni G, Staffieri A, Parisi S, Marchese-Ragona R, Zuccon A, Staffieri C, et al. Rational diagnostic and therapeutic management of deep neck infections: Analysis of 233 consecutive cases. Ann Otol Rhinol Laryngol. 2010;119:181–7. doi: 10.1177/000348941011900306. [DOI] [PubMed] [Google Scholar]
- 10.Gujrathi AB, Ambulgekar V, Kathait P. Deep neck space infection – A retrospective study of 270 cases at tertiary care center. World J Otorhinolaryngol Head Neck Surg. 2016;2:208–13. doi: 10.1016/j.wjorl.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang TT, Liu TC, Chen PR, Tseng FY, Yeh TH, Chen YS, et al. Deep neck infection: Analysis of 185 cases. Head Neck. 2004;26:854–60. doi: 10.1002/hed.20014. [DOI] [PubMed] [Google Scholar]
- 12.Levitt GW. The surgical treatment of deep neck infections. Laryngoscope. 1971;81:403–11. doi: 10.1288/00005537-197103000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Sethi DS, Stanley RE. Deep neck abscesses – Changing trends. J Laryngol Otol. 1994;108:138–43. doi: 10.1017/s0022215100126106. [DOI] [PubMed] [Google Scholar]
- 14.Kataria G, Saxena A, Bhagat S, Singh B, Kaur M, Kaur G, et al. Deep neck space infections: A study of 76 cases. Iran J Otorhinolaryngol. 2015;27:293–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Har-El G, Aroesty JH, Shaha A, Lucente FE. Changing trends in deep neck abscess. A retrospective study of 110 patients. Oral Surg Oral Med Oral Pathol. 1994;77:446–50. doi: 10.1016/0030-4220(94)90221-6. [DOI] [PubMed] [Google Scholar]
- 16.Cho SY, Woo JH, Kim YJ, Chun EH, Han JI, Kim DY, et al. Airway management in patients with deep neck infections: A retrospective analysis. Medicine (Baltimore) 2016;95:e4125. doi: 10.1097/MD.0000000000004125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eftekharian A, Roozbahany NA, Vaezeafshar R, Narimani N. Deep neck infections: A retrospective review of 112 cases. Eur Arch Otorhinolaryngol. 2009;266:273–7. doi: 10.1007/s00405-008-0734-5. [DOI] [PubMed] [Google Scholar]
- 18.Mumtaz RM, Arain AA, Suhail A, Rajput SA, Mohammad A, Nabeel H. Deep neck space infections: Retrospective review of 46 patients. J Cranio Max Dis. 2014;3:21–5. [Google Scholar]
- 19.Tschiassny K. Ludwig's angina: An anatomic study of the role of the lower molar teeth in its pathogenesis. Arch Otolaryngol. 1943;38:485–96. [Google Scholar]


