Abstract
Context:
Oral submucous fibrosis (OSMF) is an insidious, chronic, disabling disease that mainly affects the oral mucosa. Spirulina is a freshwater microalga which is considered as superfood by the WHO. Due to its antioxidant, anti-inflammatory, and immunomodulating properties, spirulina has shown promising results in the management of OSMF. A wide range of treatment modalities have been tried ranging from medical, physical, or surgical interventions, but combinations of these have shown better results.
Aims:
The study aimed to evaluate the efficacy of spirulina along with different physiotherapeutic modalities in the management of OSMF.
Setting and Design:
The present comparative study was conducted in the Department of Oral medicine and radiology, College of Dental Sciences, Davangere, Karnataka, India. The block randomization technique was used in the present study to enroll patients into three different groups.
Methods:
The study consisted of 45 OSMF patients who were divided randomly into three groups. All patients were given spirulina 500 mg twice a day for 3 months. Group A patients were instructed to perform isometric mouth exercises for 20 min, twice daily. Group B patients and Group C patients perform exercises using threaded tapered screw and mouth stretching device (MSD), respectively, ten times bilaterally twice a day. Clinical parameters such as burning sensation, mouth opening, tongue protrusion, and cheek flexibility were assessed every 15 days.
Statistical Analysis Used:
Descriptive data that included mean, numbers, and percentages were calculated for each group and were used for analysis. For intra- and inter-group comparison, paired t- and unpaired t-test was used, respectively. For all the tests, P = 0.05 or less was considered for statistical significance.
Results and Conclusion:
All the groups have shown statistically significant improvement in burning sensation, mouth opening, tongue protrusion, and cheek flexibility (P < 0.05). Group C patients have shown better results followed by Group B and Group A patients. In the present study, spirulina along with different physiotherapeutic modalities was well tolerated by the patients, and significant improvement was seen in the MSD group.
Keywords: Isometric exercises, mouth stretching device, oral submucous fibrosis, spirulina, threaded tapered screw
INTRODUCTION
Oral submucous fibrosis (OSMF) is a potentially malignant disorder, characterized by the formation of fibrotic bands in the oral and paraoral tissues, thereby limiting mouth opening.[1,2] Although in the literature both drugs and physiotherapy modalities have been used separately in the management of OSMF, in the present study, both are combined for synergistic effect.[3] The combination therapies have been said to be effective rather than use of either drugs or physiotherapy. Use of spirulina in the successful management of OSMF is attributed to its antioxidant, anti- inflammatory and immuno-modulating properties. Case reports stating isometric exercises, threaded tapered screw, mouth exercising device, etc., reverse atrophic changes, leading to the restoration of normal mucosa.[4]
Hence, this study was taken up to evaluate the efficacy of spirulina along with different physiotherapeutic modalities in the management of OSMF.
METHODS
The present clinical study was carried out in the Department of Oral Medicine and Radiology, College of Dental Sciences, Davangere, Karnataka, India. The study protocol was approved by the Ethical Committee of the Institutional review board (CODS/IRB/1977/2015–2016).
A total of 45 of 52 clinically diagnosed OSMF patients (based on the history and characteristic clinical features) who fulfilled the criteria were enrolled in the study.
Inclusion criteria
The inclusion criteria are as follows:
Clinically diagnosed OSMF cases
Patients willing to quit the habit
Patients agreed to come for follow-up.
Exclusion criteria
The exclusion criteria are as follows:
Patients with coexisting systemic illness
Patients who underwent any treatment for the same before.
From each patient, written informed consent was obtained. Patients were counseled to quit the habit completely before starting the treatment. After 15 days of quitting the habit completely, they were enrolled in the study.
A structured pro forma was used to record the patient's demographic data and clinical parameters, i.e., burning sensation, mouth opening, tongue protrusion, and cheek flexibility helped to measure the improvement in signs and symptoms. The intensity of the burning sensation was measured using the visual analog scale (VAS) of 1–10.
Mouth opening was measured from the mesioincisal angles of maxillary central incisor to mandibular central incisor using the Vernier caliper. Cheek flexibility (mm) was measured using Mathur and Jha method,[5] and tongue protrusion (mm) was recorded using the Vernier caliper from the mesioincisal angle of the upper central incisor to the tip of the tongue when the mouth is wide open and the tongue is at its maximum extension.
Forty-five patients were enrolled in the study using a random sampling method, and block randomization technique was used to allot patients in different groups. All the patients were given spirulina 500 mg twice a day for 3 months. Threaded tapered screws were ordered from the Ganesha handicrafts private limited, West Bengal [Figure 1]. Mouth stretching device (MSD) was fabricated in the Department of Prosthodontics, College of Dental Sciences, Davangere, India, as described by Patil and Parkhedkar [Figure 2].[6]
Figure 1.

Threaded tapered screw
Figure 2.
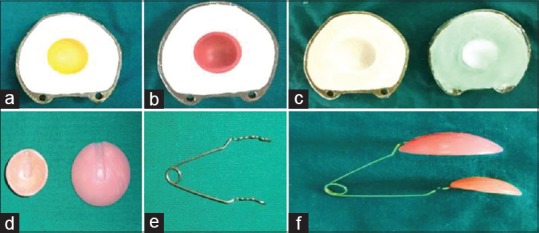
Fabrication of mold for preparing mouth stretching device (a-c) and preparation of mouth stretching device (d-f)
-
Group A – Isometric mouth exercises repeatedly for 20 min, twice daily. Patients were instructed to perform isometric mouth exercises such as
- Open their mouth until they perceive pain and then advised to hold for few seconds and relax
- Put their fingers intraorally in the buccal mucosa and stretch for few seconds and relax
- Blow their cheeks and advised to hold for few seconds
- To push the dorsum of the tongue against the palate as hard as possible
- To perform protrusive and lateral movements of the tongue.
Group B – Patients were instructed to place the threaded tapered screw device between the posterior teeth and rotate in clockwise direction manually ten times bilaterally twice a day
Group C – Patients were instructed to squeeze the cheek mucosa using the MSD by placing smaller plate intraorally and larger extraorally at different sites ten times bilaterally twice daily. In every visit, device was checked for every patient to rule out any defect. In case of any defect or fatigue induced into the coil, the device was replaced.
The clinical parameters recorded on the first visit were considered as the baseline. The patients were followed up every 15 days for 3 months with 7 readings for each patient from baseline to 6th visit. The follow-up was continued for the patients who were willing for further treatment. The patients were enquired for any side effects of the drug such as nausea, vomiting, headache, sweating, allergic reactions, and muscular weakness.
Statistical analysis used
Descriptive data that included mean, numbers, and percentages were calculated for each group and were used for analysis. For intragroup and intergroup comparison, paired t- and unpaired t-test was used, respectively. For all the tests, P = 0.05 or less was considered for statistical significance.
RESULTS
Patients enrolled in the study corresponded to the age of 19–70 years. Of 45 patients, 41 were male and four were female. In the present study, majority (40%) of the patients belonged to the third decade of life. A total of 32 (71.1%) patients were <40 years of age and 13 patients (28.8%) were >40 years of age. Table 1 summarizes the demographic data of enrolled patients.
Table 1.
Demographic data of the patients enrolled in the study
| Parameters | Group A | Group B | Group C |
|---|---|---|---|
| Males (n) | 14 | 14 | 13 |
| Females (n) | 1 | 1 | 2 |
| Mean age (years) | 38.3±12.8 | 31.8±9.5 | 38.8±11.6 |
A mean reduction of 3.8 ± 0.6 (59%), 4.7 ± 0.8 (70%), and 5 ± 0.8 (82%) with complete diminution in 3, 5, and 5 patients was procured in Group A patients, Group B patients, and Group C patients, respectively. There was highly significant reduction (P = 0.001) in burning sensation with successive visits in all the three groups. The improvement in mouth opening was highly significant in all the three groups with a mean of 3.2 mm in Group A patients, 5 mm in Group B patients, and 8 mm in Group C patients [Table 2 and Figures 3, 4].
Table 2.
Improvement in clinical parameters from baseline to 6th visit
| Group | Visits | Burning sensation (VAS) | Mouth opening (mm) | Tongue protrusion (mm) | Cheek flexibility (mm) |
|---|---|---|---|---|---|
| Group A | Baseline | 6.4±2.3 | 25.5±4.9 | 34.8±7.9 | 1.8±0.5 |
| 1st visit | 5.9±2.0 | 25.6±4.8 | 34.9±7.9 | 1.9±0.5 | |
| 2nd visit | 5.6±2.0 | 26.2±4.7 | 35.3±7.8 | 2.0±0.6 | |
| 3rd visit | 4.9±1.8 | 26.7±4.9 | 35.8±8.0 | 2.2±0.6 | |
| 4th visit | 4.2±1.9 | 27.5±4.9 | 36.3±8.0 | 2.3±0.6 | |
| 5th visit | 3.5±1.9 | 28.2±5.3 | 36.9±8.0 | 2.5±0.7 | |
| 6th visit | 2.6±1.7 | 28.8±5.1 | 37.2±8.0 | 2.6±0.7 | |
| P | 0.001* | 0.001* | 0.001* | 0.001* | |
| Group B | Baseline | 6.7±2.5 | 32.0±6.9 | 45.4±8.5 | 2.2±0.5 |
| 1st visit | 6.1±2.3 | 32.4±7.0 | 45.7±8.5 | 2.3±0.6 | |
| 2nd visit | 5.6±2.2 | 33.2±7.1 | 45.9±9.3 | 2.5±0.5 | |
| 3rd visit | 5.0±2.3 | 34.4±7.0 | 46.5±9.3 | 2.8±0.6 | |
| 4th visit | 4.0±2.2 | 35.2±7.3 | 47.2±9.5 | 3.0±0.6 | |
| 5th visit | 2.9±1.9 | 36.3±7.3 | 48.8±8.6 | 3.2±0.6 | |
| 6th visit | 2.0±1.7 | 37.0±7.0 | 49.4±8.5 | 3.4±0.6 | |
| P | 0.001* | 0.001* | 0.001* | 0.001* | |
| Group C | Baseline | 6.1±2.1 | 35.5±5.5 | 44.4±9.9 | 2.4±0.4 |
| 1st visit | 5.4±1.9 | 35.8±5.4 | 44.6±9.7 | 2.6±0.4 | |
| 2nd visit | 4.6±1.7 | 37.4±5.5 | 45.6±9.7 | 2.8±0.4 | |
| 3rd visit | 4.0±1.6 | 39.0±5.6 | 46.8±9.7 | 3.1±0.4 | |
| 4th visit | 3.1±1.4 | 40.5±5.6 | 47.2±9.9 | 3.4±0.3 | |
| 5th visit | 2.2±1.1 | 42.1±5.6 | 47.2±9.9 | 3.6±0.3 | |
| 6th visit | 1.1±1.2 | 43.6±5.7 | 50.3±9.8 | 3.9±0.3 | |
| P | 0.001* | 0.001* | 0.001* | 0.001* |
For intragroup and intergroup comparison, paired t- and unpaired t-test were used, respectively. *P<0.05 was considered as statistically significant. VAS=Visual analog scale
Figure 3.
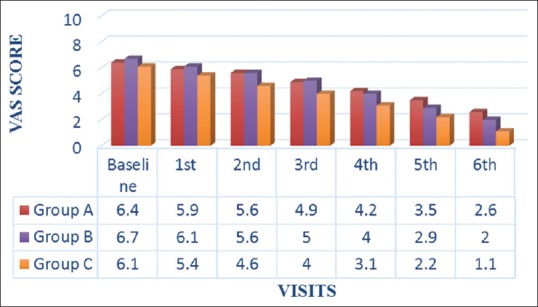
Intragroup and intergroup comparison of burning sensation from baseline to 6th visit
Figure 4.
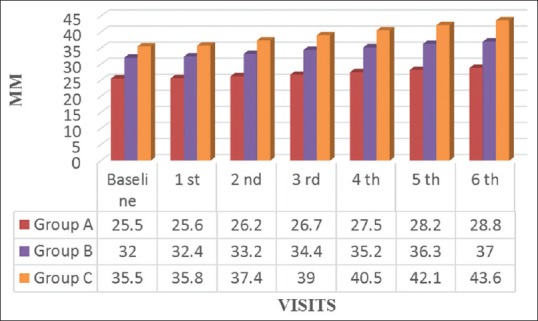
Intragroup and intergroup comparison of mouth opening from baseline to 6th visit
The improvement in tongue protrusion was statistically significant in all the three groups with a mean of 3.2 mm in Group A patients, 5 mm in Group B patients, and 7.5 mm in Group C patients. The mean improvement in cheek flexibility was significant in all the groups with a mean of 0.8 mm in Group A patients, 1.1 mm in Group B patients, and 1.4 mm in Group C patients [Table 2 and Figures 5, 6].
Figure 5.
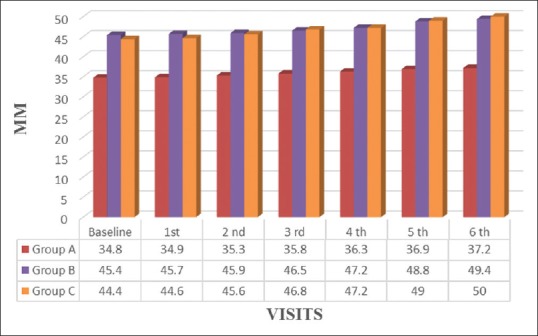
Intragroup and intergroup comparison of tongue protrusion from baseline to 6th visit
Figure 6.
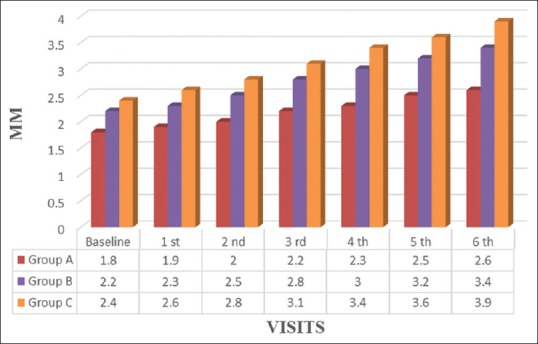
Intragroup and intergroup comparison of cheek flexibility from baseline to 6th visit
DISCUSSION
Since years, antioxidants are being widely used in the management of OSMF. Spirulina is a blue–green alga, rich in phycocyanins, carotenoids, minerals, and vitamins, especially Vitamin B12 and pro-vitamin A. Spirulina got attention in the literature mainly due to its cholesterol-regulating properties. Later, the antioxidant properties of spirulina were reported. Till date, few studies evaluating the antioxidant properties of spirulina have been conducted in humans. Spirulina shows favorable antioxidant effects and benefits the immune system of healthy human participants. In an in vivo study published in 2008, Park et al. stated that spirulina supplementation resulted in a significant rise in interleukin (IL)-2 concentration and a reduction in IL-6 concentration.[7]
In the present study, all the OSMF patients were in the spectrum of 19–70 years of age. Although 20 (44.4%) patients were <30 years of age, the study demonstrated that maximum patients, i.e., 40% belonged to the third decade of their life which is in consonance with various previous studies.[8] The deviation of the diseases toward younger age group is because of cheap, bright, easy available pouches of gutkha which delivers a sweet taste along with a euphoric state. Pan masala and gutkha have become popular in society due to aggressive campaigning and marketing.[9] In future, these habits can be seen in much younger age and teenagers leading to the occurrence of OSMF.[10,11]
The burning sensation was present in all the enrolled patients. It varied from 1 to 10 on the VAS scale with a mean of 6.4 ± 2.3, 6.7 ± 2.5, and 6.1 ± 2.1 in Group A, B, and C patients, respectively. The study was conducted on 80 patients, with the chief complaint element of burning sensation in the oral cavity.[10] In the present study, all the patients had displayed a statistically significant reduction in burning sensation with successive follow-ups. A mean reduction of 3.8 ± 0.6 (59%), 4.7 ± 0.8 (70%), and 5 ± 0.8 (82%) with complete diminution in 3, 5, and 5 patients was procured in Group A patients, Group B patients, and Group C patients, respectively. In the present study, Group C showed superior result than studies stated in the literature.[4,12] Antoxid (86.6%), pentoxifylline (86.6%), turmeric (87.90%), and levamisole (98.6%) have shown better results in reducing burning sensation as compared to the present study.[13,14,15]
The mean increment in mouth opening in Group A, B, and C was 3.2 mm, 5 mm, and 8 mm, respectively, at the end of the treatment period. The improvement in mouth opening in all the three groups was highly significant. However, the clinically better improvement was obtained in Group C patients followed by Group B patients and Group A patients. Various studies are stated in the literature with significant mean improvement in mouth opening using levamisole (2.9 mm), antoxid (3.1 mm), lycopene (3.4 mm, 5.38 mm), lycopene with Vitamin E (6.2 mm), pentoxifylline (7 mm), pentoxifylline with garlic pearls (5 mm), turmeric with tulsi (3–4 mm), and turmeric with black pepper (3.8 mm).[8,14,16,17,18,19] Group A patients in the present study have shown equivalent results to antoxid, levamisole, turmeric with tulsi, and turmeric with black pepper. Group B patients have shown comparable results to lycopene, lycopene with Vitamin E, and pentoxifylline with garlic pearls. Group C patients have shown better results than all the above studies with isometric exercises, therabite, dynasplint, ultrasound, shell-shaped jaw exerciser, and mouth exercising device.[20,21,22,23]
The maximum increase in tongue protrusion was observed in Group C, followed by Groups B and C with 5.8 mm, 4 mm, and 2.4 mm, respectively. Groups B and A have shown better results than topical aloe vera gel, turmeric and black pepper, nigella sativa, and pentoxifylline together.[13,15,24] The mean increment in cheek flexibility for patients in Group A, Group B, and Group C was 0.8 mm, 1.1 mm, and 1.4 mm, respectively, after the treatment. All the groups have shown significant increment in cheek flexibility. The present study has shown better results than turmeric with black pepper, nigella sativa, and aloe vera gel.[13,24]
In our study, all three groups have shown statistically significant results in all parameters. MSD has shown better results as compared to threaded tapered screw and isometric exercises in the present study. On comparing with other physiotherapeutic modalities such as therabite, dynasplint, and shell-shaped jaw exerciser, MSD has shown better results.[20,21,23] Physiotherapy is generally considered mainstay for the management of restricted mouth opening and is often used alone or in combination with other modalities. Regular physical exercise resulted in improved muscle vascularity, increased muscle mass and protein metabolism, decreased muscle fatigability and increased strength, reversal of atrophic changes within the mucosa, and restoration of the normal structure.
Therefore, spirulina has shown better results with various physiotherapeutic modalities in the management of OSMF. Further studies involving larger sample size and longer follow-up are recommended.
CONCLUSION
In the present study, spirulina along with isometric exercises, threaded tapered screw, and MSD was well tolerated by the patients and showed statistically significant improvement in all the clinical parameters such as burning sensation, mouth opening, tongue protrusion, and cheek flexibility. The MSD has shown better results than isometric exercises and threaded tapered screw in the present study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tak J, Gupta N, Bali R. Oral submucous fibrosis: A review article on etiopathogenesis. Kathmandu Univ Med J (KUMJ) 2014;12:153–6. doi: 10.3126/kumj.v12i2.13666. [DOI] [PubMed] [Google Scholar]
- 2.Gupta J, Srinivasan SV, Daniel J. Efficacy of betamethasone, placental extract and hyaluronidase in the treatment of OSMF: A comparative study. EJ Dent. 2012;1:132–5. [Google Scholar]
- 3.Singh N, Hebbale M, Mhapuskar A, Ul Nisa S, Thopte S, Singh S. Effectiveness of Aloe vera and antioxidant along with physiotherapy in the management of oral submucous fibrosis. J Contemp Dent Pract. 2016;17:78–84. doi: 10.5005/jp-journals-10024-1806. [DOI] [PubMed] [Google Scholar]
- 4.Chole RH, Gondivkar SM, Gadbail AR, Balsaraf S, Chaudhary S, Dhore SV, et al. Review of drug treatment of oral submucous fibrosis. Oral Oncol. 2012;48:393–8. doi: 10.1016/j.oraloncology.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 5.Mathur RM, Jha T. Normal oral flexibility-A guideline for SMF cases. J Indian Dent Assoc. 1993;64:139–43. [Google Scholar]
- 6.Patil PG, Parkhedkar RD. New graft-stabilizing clip as a treatment adjunct for oral submucous fibrosis. J Prosthet Dent. 2009;102:191–2. doi: 10.1016/S0022-3913(09)60146-3. [DOI] [PubMed] [Google Scholar]
- 7.Park HJ, Lee YJ, Ryu HK, Kim MH, Chung HW, Kim WY, et al. A randomized double-blind, placebo-controlled study to establish the effects of spirulina in elderly Koreans. Ann Nutr Metab. 2008;52:322–8. doi: 10.1159/000151486. [DOI] [PubMed] [Google Scholar]
- 8.Kumar A, Bagewadi A, Keluskar V, Singh M. Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:207–13. doi: 10.1016/j.tripleo.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Javed F, Altamash M, Klinge B, Engström PE. Periodontal conditions and oral symptoms in gutka-chewers with and without type 2 diabetes. Acta Odontol Scand. 2008;66:268–73. doi: 10.1080/00016350802286725. [DOI] [PubMed] [Google Scholar]
- 10.Hazarey VK, Erlewad DM, Mundhe KA, Ughade SN. Oral submucous fibrosis: Study of 1000 cases from central India. J Oral Pathol Med. 2007;36:12–7. doi: 10.1111/j.1600-0714.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 11.Sinor PN, Gupta PC, Murti PR, Bhonsle RB, Daftary DK, Mehta FS, et al. A case-control study of oral submucous fibrosis with special reference to the etiologic role of areca nut. J Oral Pathol Med. 1990;19:94–8. doi: 10.1111/j.1600-0714.1990.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 12.Shah PH, Venkatesh R, More CB, Vassandacoumara V. Comparison of therapeutic efficacy of placental extract with dexamethasone and hyaluronic acid with dexamethasone for oral submucous fibrosis – A retrospective analysis. J Clin Diagn Res. 2016;10:ZC63–6. doi: 10.7860/JCDR/2016/20369.8652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pipalia PR, Annigeri RG, Mehta R. Clinicobiochemical evaluation of turmeric with black pepper and Nigella sativa in management of oral submucous fibrosis-a double-blind, randomized preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:705–12. doi: 10.1016/j.oooo.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 14.Warnakulasuriya S, Kerr AR. Oral submucous fibrosis: A review of the current management and possible directions for novel therapies. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:232–41. doi: 10.1016/j.oooo.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Rajendran R, Rani V, Shaikh S. Pentoxifylline therapy: A new adjunct in the treatment of oral submucous fibrosis. Indian J Dent Res. 2006;17:190–8. doi: 10.4103/0970-9290.29865. [DOI] [PubMed] [Google Scholar]
- 16.Goel S, Ahmed J. A comparative study on efficacy of different treatment modalities of oral submucous fibrosis evaluated by clinical staging in population of Southern Rajasthan. J Cancer Res Ther. 2015;11:113–8. doi: 10.4103/0973-1482.139263. [DOI] [PubMed] [Google Scholar]
- 17.Maher R, Aga P, Johnson NW, Sankaranarayanan R, Warnakulasuriya S. Evaluation of multiple micronutrient supplementation in the management of oral submucous fibrosis in Karachi, Pakistan. Nutr Cancer. 1997;27:41–7. doi: 10.1080/01635589709514499. [DOI] [PubMed] [Google Scholar]
- 18.Liu J, Chen F, Wei Z, Qiu M, Li Z, Dan H, et al. Evaluating the efficacy of pentoxifylline in the treatment of oral submucous fibrosis: A meta-analysis. Oral Dis. 2018;24:706–16. doi: 10.1111/odi.12715. [DOI] [PubMed] [Google Scholar]
- 19.Srivastava A, Agarwal R, Chaturvedi TP, Chandra A, Singh OP. Clinical evaluation of the role of tulsi and turmeric in the management of oral submucous fibrosis: A pilot, prospective observational study. J Ayurveda Integr Med. 2015;6:45–9. doi: 10.4103/0975-9476.146563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen EG, Deschler DG, Walsh K, Hayden RE. Early use of a mechanical stretching device to improve mandibular mobility after composite resection: A pilot study. Arch Phys Med Rehabil. 2005;86:1416–9. doi: 10.1016/j.apmr.2004.10.035. [DOI] [PubMed] [Google Scholar]
- 21.Stubblefield MD, Manfield L, Riedel ER. A preliminary report on the efficacy of a dynamic jaw opening device (dynasplint trismus system) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch Phys Med Rehabil. 2010;91:1278–82. doi: 10.1016/j.apmr.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Chaudhry Z, Gupta SR, Oberoi SS. The efficacy of ErCr:YSGG laser fibrotomy in management of moderate oral submucous fibrosis: A preliminary study. J Maxillofac Oral Surg. 2014;13:286–94. doi: 10.1007/s12663-013-0511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patil PG, Patil SP. Novel mouth-exercising device for oral submucous fibrosis. J Prosthodont. 2012;21:556–60. doi: 10.1111/j.1532-849X.2012.00874.x. [DOI] [PubMed] [Google Scholar]
- 24.Sudarshan R, Annigeri RG, Sree Vijayabala G. Aloe vera in the treatment for oral submucous fibrosis – A preliminary study. J Oral Pathol Med. 2012;41:755–61. doi: 10.1111/j.1600-0714.2012.01168.x. [DOI] [PubMed] [Google Scholar]


