Abstract
This study examined the feasibility of an adapted 2-week mindfulness meditation protocol for chronic stroke survivors. In addition, preliminary effects of this adapted intervention on spasticity and quality of life in individuals after stroke were explored. Ten chronic stroke survivors with spasticity listened to 2 weeks of short mindfulness meditation recordings, adapted from Jon Kabat-Zinn’s Mindfulness-Based Stress Reduction course, in a pre/post repeated measures design. Measures of spasticity, quality of life, mindfulness, and anxiety, along with qualitative data from participants’ daily journals, were assessed. On average, participants reported meditating 12.5 days of the full 15 days (mean 12.5 days, SD 0.94, range 8-15 days). Seven of the 10 participants wrote comments in their journals. In addition, there were no adverse effects due to the intervention. Exploratory preliminary analyses also showed statistically significant improvements in spasticity in both the elbow (P = .032) and wrist (P = .023) after 2 weeks of meditation, along with improvements in quality of life measures for Energy (P = .013), Personality (P = .026), and Work/Productivity (P = .032). This feasibility study suggests that individuals with spasticity following stroke are able to adhere to a 2-week home-based mindfulness meditation program. In addition, preliminary results also suggest that this adapted, short mindfulness meditation program might be a promising approach for individuals with spasticity following stroke. Future research should expand on these preliminary findings with a larger sample size and control group.
Keywords: stroke, mindfulness, spasticity, rehabilitation
Thirty percent of stroke survivors experience spasticity, a velocity-dependent increase in stretch reflexes, which negatively affects quality of life and activities of daily living.1 Spasticity is a secondary neurological symptom induced by neurological hyperreflexia seen in stroke and other neurological disorders.2 If left untreated, stroke survivors may develop contractures, which can further impede motor recovery and participation in activities of daily living.1 Spasticity is typically treated with medications, botox injections, baclofen intrathecal pumps, occupational therapy, and physical therapy, but current treatment options are often expensive and effectiveness is generally unsatisfactory.3 Thus, there is a need to find low-cost, effective, and accessible methods that have the potential to help reduce spasticity and promote recovery.
Increased spasticity has been linked to emotion-based stress, such as anxiety.4 Previous research has anecdotally linked mindfulness meditation, a technique that has been used to reduce anxiety, to decreased poststroke spasticity.4 Briefly, mindfulness meditation is a type of meditation that trains awareness and acceptance of the current inner and outer reality, and is often taught through Jon Kabat-Zinn’s 8-week Mindfulness-Based Stress Reduction (MBSR) course.5 MBSR was developed at the University of Massachusetts Medical Center’s Stress Reduction Clinic. The course is time intensive, taught in 8 weekly group classes by certified teachers, and includes at-home assignments. The total hours spent is around 75 hours over 8 weeks. The attitudinal foundations of the practice include nonjudging, patience, beginner’s mind, trust, nonstriving, acceptance, and letting go. These principles are thought to be helpful in achieving peace of mind.5 MBSR has been used as a way to learn mindfulness and also as a mindfulness-based intervention in clinical populations.6 In general, some studies have found that mindfulness meditation may be linked to the reduction of anxiety and pain, but it has not been directly connected to motor function or spasticity.7–9 Specifically, mindfulness intervention studies using MBSR have reported decreased mental fatigue in people with traumatic brain injury (TBI) or stroke6 and a reduction in psychological stress and improvement in cognitive function in patients with multiple sclerosis.10 One systematic review showed that mindfulness meditation helped patients cope with their chronic illnesses, including cancer, depression and general anxiety disorder, by improving their mood and anxiety symptoms.11 Furthermore, a randomized controlled trial investigated the effects of a 10-week Mindfulness-Based Cognitive Therapy (MBCT), which is a combination of MBSR with some insights from cognitive behavioral therapy, on individuals with TBI and symptoms of depression.12 Results from this study indicated a reduction in symptoms of depression, which were maintained at 3 months.12 Mindfulness-based interventions are also being tested for feasibility and stress reduction in individuals with melanoma.13 In stroke and transient ischemic attack survivors, there is small but growing evidence that mindfulness promotes positive results for psychological and psychosocial health.14 One study confirmed the feasibility of an MBSR intervention on individuals after stroke and their caregivers.15 Furthermore, a pilot study with individuals after stroke using an 8-week MBCT intervention found a reduction in anxiety and depression and an increase in quality of life, including physical functioning.8
Because of the anecdotal evidence linking stress to increased spasticity and the clinical evidence linking meditation to decreased stress, particularly in stroke patients, here we conducted a feasibility study to determine whether an adapted, 2-week mindfulness meditation program could be successfully implemented with stroke survivors with stroke spasticity, and whether there might be any preliminary effects, quantitative or qualitative, on quality of life and spasticity following this program. In this feasibility study, we examined whether individuals after stroke were able to adhere to 2 weeks of daily, home-based mindfulness meditations using prerecorded audio recordings. Participants attended 2 in-person laboratory visits at the beginning and end of the study for assessments, but otherwise completed daily meditations via audio recordings at home. We chose 2 weeks for our intervention to limit the burden on participants, and we adapted the mindfulness materials from a well-known existing course (Jon Kabat-Zinn’s 8-week MBSR course), which was previously used in a successful pilot study with stroke patients.5,6 In addition, while MBSR is typically taught by an experienced teacher over a series of in-person sessions, studies have also shown successful mindfulness practice via audio/video recording,16 which allows for greater accessibility to mindfulness training for broader audiences, including those with mobility limitations. We anticipated that a short, 2-week home-based mindfulness program, based loosely on MBSR, may be less burdensome and more accessible to a wider population of individuals after stroke. In this pilot study, we examined participants’ adherence to the program and general impressions of this intervention. We also collected preliminary data to examine if there were any potential effects of mindfulness meditation on reduced anxiety and/or reduced poststroke spasticity.
Methods
Participants
We recruited individuals with chronic stroke (>1 year poststroke), older than 18 years, with moderate to severe motor deficits with self-reported spasticity or hypertonia, and with no prior mindfulness meditation experience (Table 1). Out of 11 subjects recruited, 1 participant dropped out of the study before completing both visits due to logistical issues, leaving a total sample of n = 10. Informed consent was obtained from all participants. The experimental protocol was approved by the university institutional review board and performed in accordance with the 1964 Declaration of Helsinki. This clinical trial has been registered with ClinicalTrials.gov.
Table 1.
Subject Characteristics.
| Characteristic | n | Mean, Median (Range) |
|---|---|---|
| Gender | ||
| Men | 9 | |
| Women | 1 | |
| Race/Ethnicity | ||
| White/Caucasian | 5 | |
| Asian | 3 | |
| Hispanic | 2 | |
| Age in years | 59.8, 58.5 (45-76) | |
| Years poststroke | 7.3, 7 (4-13) |
Mindfulness Meditation Training and Procedure
This study’s mindfulness meditation training was adapted from the first 2 weeks of the 8-week MBSR program created by Jon Kabat-Zinn and used audio recordings from an online version of the Kabat-Zinn course (made by a certified MBSR instructor) and from UCLA’s Mindful Awareness Research Center (MARC).5,16,17 Numerous mindfulness studies have implemented the full MBSR program or variations of the program using subsets of the recordings.6,18,19 We specifically used recordings that mirrored the first 2 weeks of the highly successful MBSR program, using the MBSR Week 1 Body Scan audio recording to ready the participants for their daily 3-minute Body Scan meditation during the first week, and using the MBSR Week 2 Sitting Meditation recording to prepare them for their daily 5-minute Sitting/Breathing meditation during the second week. The details regarding each visit and meditation are specified in Table 2.
Table 2.
Experimental Protocol.
| Day | Location | Description |
|---|---|---|
| Day 1 | Lab | |
| Premeditation | Introduction to Mindfulness | |
| Meditation | Meditation journals given | |
| Postmeditation | Modified Ashworth Scale | |
| Stroke-Specific Quality of Life | ||
| Hospital Anxiety and Depression Scale | ||
| Freiburg Mindfulness Inventory | ||
| Fugl-Meyer Upper Extremity | ||
| 39-Minute Body Scan Meditation | ||
| Introduction to daily journal | ||
| Days 2-7 | Home | 3-Minute Body Scan Meditation |
| Daily journal | ||
| Day 8 | Home | 39-Minute Sitting Meditation |
| Daily journal | ||
| Day 9-14 | Home | 5-Minute Breathing Meditation |
| Daily journal | ||
| Day 15 | Lab | |
| Premeditation | Modified Ashworth Scale | |
| Meditation | Stroke Specific Quality of Life | |
| Postmeditation | Hospital Anxiety and Depression | |
| Scale | ||
| Freiburg Mindfulness Inventory | ||
| Fugl-Meyer Upper Extremity | ||
| 39-Minute Body Scan Meditation | ||
| Meditation journals collected |
On the first day (day 1) participants came to our laboratory and completed baseline assessments, including the Modified Ashworth Scale (MAS), Fugl-Meyer Assessment, Stroke-Specific Quality of Life Scale (SSQoL), Freiburg Mindfulness Inventory (FMI), and Hospital Anxiety and Depression Scale (HADS). Next, with an experimenter present, they listened to a 32-minute Body Scan meditation, which is the same recording used in week 1 of the MBSR course. They also listened to a 7-minute Meditation for Working with Difficulties.16,17 The Working with Difficulties meditation was added because the content specifically involved focusing on body parts that might be causes of stress to the meditator (such as limbs with spasticity) versus neutral body parts (such as their unaffected side) and was hypothesized to be relevant to the study participants who had paresis following stroke. This long meditation served to introduce them to the technique with detailed instructions; an investigator was present to answer any questions they might have. They were then given an MP3 player with audio-guided meditations loaded onto it, instructed on how to use it at home, and provided with a daily journal.
For the next 2 weeks (day 2 to day 14), participants listened to short guided meditations each day in their homes using the provided MP3 player. After each daily meditation, subjects filled out their meditation journal. For days 2 to 7, they listened to a 3-minute Body Scan Meditation each day in order to practice the technique.17 On day 8 (the start of week 2), they listened to a 32-minute Sitting Meditation followed by the 7-minute Working with Difficulties meditation from day 1. This long meditation served as an introduction to week 2 of meditation, focusing more on breathing/sitting. From days 9 to 14, they listened to a 5-minute Breathing Meditation (similar to Sitting) to practice the new technique, mirroring what might be done in the MBSR course, although with a much shorter practice length, no instructor present, and done individually instead of a group. On the last day, day 15, subjects came back to the lab and repeated all the assessments and recordings from day 1.
Assessments
The primary objective of this study was to examine feasibility and adherence to an adapted home-based mindfulness meditation intervention for individuals with stroke. We asked participants to report each day they meditated in a home journal. For each day, they were also asked to rate the statement “I feel like I meditated for most of the session” on a Likert-type scale from 1 to 5, after their daily meditation session, along with optional space to write freeform comments. Both Likert-type and qualitative data were used in analyses to assess adherence to the protocol as well as general reactions to the intervention.
In addition, we also collected several measures to explore whether there were any observable preliminary effects from this intervention.
Spasticity was measured using the MAS at the wrist and elbow.20 In addition, the Fugl-Meyer Assessment was used to test upper limb sensorimotor impairments.21 Assessments were conducted by trained experimenters.
Three validated questionnaires were also given before and after the intervention to assess quality of life, mindfulness, anxiety, and depression: (1) the SSQoL survey was used to assess quality of life across several categories of Energy, Family Roles, Language, Mobility, Mood, Personality, Self-Care, Social Roles, Thinking, Upper Extremity Function, Vision, and Work/Productivity22; (2) the FMI23 was used to assess self-rated mindfulness competence on a scale of 1 to 5; and (3) the HADS was used to assess anxiety and depression on scale of 0 to 3.24
Data Analysis
We aimed to first examine the feasibility and adherence to the intervention, which is reported in terms of number of days meditated and number of days with journal entries.
In addition, we collected additional exploratory data on changes in spasticity, which we measured for both wrist and elbow, as well as changes in the quality of life, mindfulness, anxiety and depression, and self-rated scales. Paired Student’s t tests were used to compare these results before and after meditation.
A preliminary qualitative analysis was also conducted to determine effects not captured by assessments, which could inform future experimental designs. The free form comments obtained from the subjects’ meditation journals were qualitatively analyzed using the Colaizzi method.25 Significant statements related to the content under study were extracted and compiled and coded by 2 researchers into a log. Each statement was given a meaning, which represented the content of each statement, and the formulated meanings that were similar were then sorted into groups. Afterward, themes emerged in which statements fit uniquely and were mutually exclusive of other themes. Rigorous peer review by the lead researcher was employed throughout each stage to minimize subjectivity.
Results
Feasibility and Adherence to the Meditation Protocol
Out of 11 subjects recruited, 1 participant dropped out of the study before completing both visits due to logistical issues, leaving a total sample of n = 10. All 10 individuals completed the meditation protocol and attended 2 in-person visits at our research laboratory (one at the beginning and another at the end of the study). On average, participants reported meditating 12.5 days of the full 15 days (mean 12.5 days, SD 0.94, range 8-15 days). In addition, 7 of the 10 participants wrote daily comments in their journals. No adverse events were reported during the course of this study. These results suggest that this protocol is feasible, although consideration should be given to the fact that participants may miss a few days in the course of the 2-week program. Participants suggested that a web or mobile app may be useful to remind them to complete their daily meditation and write daily journal comments.
Spasticity
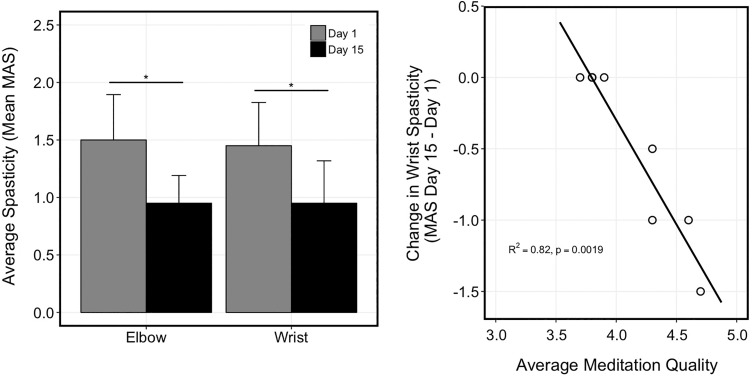
To assess whether there were any preliminary effects of mindfulness meditation on spasticity, we compared the MAS scores from the start of the study (the beginning of day 1, before the meditation for that day) with the beginning of day 15, before the meditation for that day. We found that spasticity significantly improved for the elbow, t(1, 9) = 2.5, P = .032, and wrist, t(1, 9) = 2.7, P = .023; Figure 1).
Figure 1.
Spasticity results. Left: Comparison of mean values for the Modified Ashworth shown for elbow (left) and wrist (right) at day 1 (white) and day 15 (black). Higher score indicates worse spasticity. Right: Correlation between average meditation quality (from 1 to 5, where 5 is best) and wrist spasticity change as measured by the Modified Ashworth Scale (MAS; negative change means improvement, or lessening, in spasticity) following 15 days of meditation.
Quality of Life and Mindfulness
To explore potential changes in quality of life, we then compared changes within the SSQoL, HADS, and FMI. In the SSQoL, the subscores for Energy, t(1, 8) = 2.7, P = .013; Personality, t(1, 9) = 2.7, P = .026; and Work/Productivity, t(1, 9) = 2.5, P = .032, improved the most, but when correcting for multiple comparisons across the 12 subscales in the SSQoL, they were not statistically significant (a corrected P < .0042 would be needed for significance; Table 3). There were no significant changes in scores for other subscores of the SSQoL, and no significant change in scores for the HADS or FMI.
Table 3.
Study Results.a
| Scale | Subscore | Day 1 (Mean ± SD) | Day 15 (Mean ± SD) | Day 15 vs Day 1 | |
|---|---|---|---|---|---|
| t(df) | P | ||||
| Modified Ashworth Scale (MAS) | |||||
| Elbow | 1.5 ± 1.25 | 0.95 ± 0.76 | 2.5 (9) | .032* | |
| Wrist | 1.45 ± 1.19 | 0.95 ± 1.17 | 2.7 (9) | .023* | |
| Fugl-Meyer Upper Extremity | |||||
| Motor function | 40.4 ± 19.43 | 40.4 ± 20.11 | 0.0 (9) | 1.0 | |
| Stroke-Specific Quality of Life (SSQoL) | |||||
| Energy | 9.22 ± 10.19 | 12.22 ± 7.44 | −2.7 (8) | .025* | |
| Family Roles | 8.50 ± 3.70 | 10.0 ± 3.63 | −1.1 (7) | .316 | |
| Language | 19.10 ± 6.0 | 21.7 ± 3.71 | −1.3 (9) | .235 | |
| Mobility | 22.0 ± 6.31 | 21.9 ± 5.07 | 0.1 (9) | .933 | |
| Mood | 18.2 ± 6.97 | 20.1 ± 4.65 | −1.2 (9) | .254 | |
| Personality | 9.50 ± 2.67 | 11.70 ± 2.71 | −2.7 (9) | .026* | |
| Self-Care | 22.25 ± 5.26 | 21.75 ± 4.53 | 1.1 (7) | .316 | |
| Social Roles | 15.56 ± 6.23 | 16.67 ± 6.06 | −0.5 (8) | .604 | |
| Thinking | 11.50 ± 2.95 | 12.0 ± 2.36 | −0.7 (9) | .475 | |
| Upper Extremity Function | 18.11 ± 5.16 | 17.56 ± 5.41 | 0.7 (8) | .489 | |
| Vision | 14.50 ± 0.97 | 14.4 ± 0.97 | 1.0 (9) | .343 | |
| Work/Productivity | 11.0 ± 3.27 | 12.1 ± 2.73 | −2.5 (9) | .032* | |
| Hospital Anxiety and Depression Scale (HADS) | |||||
| Anxiety | 6.0 ± 3.77 | 5.5 ± 3.95 | 1.2 (9) | .244 | |
| Depression | 4.5 ± 4.28 | 4.1 ± 3.14 | 0.45 (9) | .666 | |
| Freiburg Mindfulness Inventory (FMI) | 43.1 ± 8.61 | 42.3 ± 7.69 | 0.58 (9) | .579 | |
aMAS (spasticity), Fugl-Meyer (motor impairment), SSQoL, HADS (anxiety and depression), and FMI (self-perceived mindfulness ability) scores. Paired t tests are shown with t statistic (degrees of freedom) and P value.
*Indicates P < .05.
Motor Impairment
There were no significant changes in the Fugl-Meyer Assessment scores following the mindfulness meditation, t(0, 9) = 0.0, P = 1.0.
Correlations Between Change in Spasticity and Quality of Meditation
To understand whether changes in spasticity following meditation were due to the quality of the meditation, we analyzed the correlation between these measures for the individuals who returned their journals (n = 7; Figure 1). Although we note that this is a small sample, our preliminary results show a significant correlation (R 2 = 0.82, P = .0019; Figure 1) found between spasticity change in wrist and quality of meditation, as measured by ratings on the statement in the daily journal, “I felt like I meditated for most of the session.” That is, individuals who felt they were able to meditate for most of the session showed improvements in spasticity, while those who felt less capable of meditation showed little to no changes in spasticity. This preliminary finding could indicate that an individual’s perception of their performance may be a useful indicator of whether or not they will benefit from mindfulness meditation. For future long-term meditation studies, it may be useful to assess participant adherence and feedback within the first few days to determine whether or not the participant is likely to show benefits in the study.
Qualitative Analysis of Journal Comments
As mentioned previously, we also collected freeform comments from participants in their daily journals to determine effects not captured by quantitative assessments, which could inform future experimental designs. Qualitative analysis of the participants’ written comments about the meditations revealed 3 themes: (1) mindfulness competency, (2) spasticity effects, and (3) general effects. Mindfulness competency was reflected in the participant comments as they reported being focused, alert and aware during meditation. One participant wrote, “Focused on discomfort when surveying body when prompted.” Another participant reported, “The awareness of the different sensation on my body were [sic] more noticeable. I was alert of not just my body noises but all the surrounding noises in the places I chose to meditate. I focused on the hemiplegic side of my body.” Effects on spasticity were reflected in comments as one participant wrote, “Layed [sic] on bed, immediately relaxed. Left-hand relaxed during session.” Another subject wrote, “My arm (elbow, wrist, and fingers) were looser and softer after meditation, and also felt much relaxed [sic].” The effects on spasticity were variable however; one person wrote, “I feel well relaxed, but I don’t feel the same loosened muscles in my left hand as the first session I had at the…[university] office. I remember at the 1st session my wrist and fingers were softer and looser.” Apart from its effects on spasticity, participants also reported feeling general mindfulness effects as one person wrote, “Relaxed and like personal time out.” Other comments indicated that “Longer spaces caught my mind wondering [sic] but relaxed.”
These freeform comments suggest that participants generally enjoyed and perceived benefits from the mindfulness meditation. Indeed, many participants asked to have the recordings for themselves to continue with after the completion of the study, which were provided for them.
Discussion
In this feasibility study, 10 individuals with chronic stroke and spasticity underwent an adapted 2-week mindfulness meditation program, using materials from the Kabat-Zinn MBSR course, with 2 lab visits and short daily meditations at home using MP3 recordings. Data from this feasibility study suggest that participant adherence was good during our 2-week home mindfulness training program. We note that there were no significant decreases in any of the measures of motor function or quality of life and no adverse events were reported, suggesting that this intervention is likely safe and feasible for individuals after stroke to complete at home. In addition, qualitative reports from participants indicated a general enjoyment and relaxation when completing these adapted mindfulness meditations, suggesting that most participants found this intervention enjoyable and not burdensome.
In addition, we collected exploratory preliminary measures of physical and psychosocial effects from the intervention to see if any changes could be elicited from only 2 weeks of mindfulness meditation. Preliminary intervention results showed that the 2-week paradigm improved spasticity in the elbow and wrist, suggesting that a short mindfulness training program may help to decrease spasticity. We see this both in the wrist and elbow of the affected limb, and these changes are echoed by the participants’ daily journal comments as well. It is worth noting that although our results indicate statistically significant decreases in spasticity, they are not considered clinically significant, as defined by a 1-point decrease in the MAS.26 Future research may explore whether longer meditation practices may result in greater improvements in spasticity.
Interestingly, improvements in spasticity were correlated with individuals’ perception of their meditation quality. This suggests that the home-based meditation program may be more successful with some individuals than others, based on their self-perceived ability to meditate. To our knowledge, this is the first preliminary evidence linking mindfulness meditation training with reduced poststroke spasticity. However, we acknowledge that this study’s weaknesses of not having a control group and using a small sample size limit the interpretation of these findings. These preliminary results warrant the need for future experiments, with a larger sample size and, most importantly, a control group, to corroborate these findings. If results are confirmed with appropriate controls in place, these findings would provide insight for future studies on mindfulness and physical rehabilitation. Recent studies have used active listening control groups to mimic the active thinking and listening, in order to isolate the effects of the mindfulness technique.7 Future studies should engage this kind of control, which mimics the intervention condition, to better elucidate the mechanism by which any observed changes in spasticity may occur.
Exploratory analyses also showed improvement in some aspects of quality of life, in line with previous mindfulness meditation studies in populations with chronic disease showing improvements in quality of life.27,28 Three subscores of SSQoL (Energy, Personality, Work/Productivity) improved after mindfulness meditation training, similar to previous reports following mindfulness training in stroke survivors.8 While in this small sample these results were not statistically significant after correcting for multiple comparisons, they do provide an indication of which factors might be explored further in larger studies examining changes following mindfulness training in individuals with stroke.
Notably, there were no significant changes in the FMI, or HADS, suggesting that, while participants felt some general benefits from meditation, reflected in changes in spasticity, the behavioral questionnaires and their daily journals, the short home program was likely not enough to make them feel like they had gained competency in daily life mindfulness (FMI) or anxiety and depression (HADS). This is understandable as they only engaged in 2 weeks of short meditations to reduce the time burden. Previous research shows that mindfulness is considered a skill that needs to be developed and that results occur with longer practice.29 However, these results suggest that at least some gains can be achieved even with a low-intensity mindfulness program.
In addition, we did not carefully examine the role of cognitive function in this 2-week meditation protocol. Although all our participants were cognitively able to attend both in-lab and at home sessions and provide verbal and written feedback, we did not explicitly collect any assessments of cognitive function, which might have affected their meditation practice. In particular, assessments of executive function, attention and inhibition may be useful additions to future studies examining the feasibility of a prolonged mindfulness meditation protocol in individuals after stroke.
Overall, although there may be large interindividual variability in response to mindfulness meditation and its effects on spasticity and quality of life, this small feasibility study suggests that it is a very low-cost, accessible, and safe technique that could be easily adopted by community-dwelling individuals with stroke.
Conclusions
This study provides preliminary evidence to support the feasibility of implementing an adapted 2-week mindfulness-based intervention for individuals with spasticity after stroke. In addition, our exploratory findings suggest that two weeks of short daily mindfulness meditation practice may lead to decreased spasticity and increased quality of life factors in individuals after stroke. Further research is needed with larger study populations and a control group to confirm these findings. However, this study suggests that a short, home-based mindfulness meditation program is an easy, low-risk, and low-cost protocol with potentially both physical and mental benefits for individuals with stroke.
Acknowledgments
We would like thank Dr Rael Cahn for his input and guidance on this project.
Footnotes
Author Contributions: All authors contributed to this manuscript. MW and S-LL designed the experiment. JC recruited the participants, and MW, DS, and JMA participated in the data collection. MW, DS, and S-LL analyzed the data. MW and DS wrote the manuscript. S-LL, JMA, and JC reviewed and edited the manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the National Institutes of Health (NIH) National Institute of Child Health and Development (NICHD) and National Center for Medical Rehabilitation Research (NCMRR) Extramural Program (K01HD091283). Its contents are solely the responsibility of the author and do not necessarily represent the official views of the NIH.
ORCID iD: David Saldana, MA, OTR/L  https://orcid.org/0000-0001-9378-629X
https://orcid.org/0000-0001-9378-629X
Ethical Approval: Informed consent was obtained from all participants. The experimental protocol was approved by the Institutional Review Board HS1500196 at the University of Southern California and performed in accordance with the 1964 Declaration of Helsinki.
Trial Registration: This clinical trial has been registered with ClinicalTrials.gov under the identifier NCT03534856.
References
- 1. Thibaut A, Chatelle C, Ziegler E, Bruno MA, Laureys S, Gosseries O. Spasticity after stroke: physiology, assessment and treatment. Brain Inj. 2013;27:1093–1105. doi:10.3109/02699052.2013.804202 [DOI] [PubMed] [Google Scholar]
- 2. Bose P, Hou J, Thompson FJ. Frontiers in neuroengineering traumatic brain injury (tbi)-induced spasticity: neurobiology, treatment, and rehabilitation In: Kobeissy FH, ed. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton, FL: CRC Press; 2015. [PubMed] [Google Scholar]
- 3. Kheder A, Nair KPS. Spasticity: pathophysiology, evaluation and management. Pract Neurol. 2012;12:289–298. doi:10.1136/practneurol-2011-000155 [DOI] [PubMed] [Google Scholar]
- 4. Bhimani R, Anderson L. Clinical understanding of spasticity: implications for practice. Rehabil Res Pract. 2014;2014:279175 doi:10.1155/2014/279175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kabat-Zinn J. Mindfulness-based stress reduction (MBSR) standards of practice In: Haruki Y, Ishii Y, Suzuki M, eds. Comparative and Psychological Study on Meditation. Delft, Netherlands: Eburon; 1996:161–169. [Google Scholar]
- 6. Johansson B, Bjuhr H, Rönnbäck L. Mindfulness-based stress reduction (MBSR) improves long-term mental fatigue after stroke or traumatic brain injury. Brain Inj. 2012;26:1621–1628. doi:10.3109/02699052.2012.700082 [DOI] [PubMed] [Google Scholar]
- 7. Creswell JD, Pacilio LE, Lindsay EK, Brown KW. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1–12. doi:10.1016/j.psyneuen.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 8. Moustgaard A, Bedard M, Felteau M. Mindfulness-based cognitive therapy (MBCT) for individuals who had a stroke: results from a pilot study. J Cogn Rehab. 2007;25:4–10. [Google Scholar]
- 9. Zeidan F, Gordon NS, Merchant J, Goolkasian P. The effects of brief mindfulness meditation training on experimentally induced pain. J Pain. 2010;11:199–209. doi:10.1016/j.jpain.2009.07.015 [DOI] [PubMed] [Google Scholar]
- 10. Blankespoor RJ, Schellekens MPJ, Vos SH, Speckens AEM, de Jong BA. The effectiveness of mindfulness-based stress reduction on psychological distress and cognitive functioning in patients with multiple sclerosis: a pilot study. Mindfulness (N Y). 2017;8:1251–1258. doi:10.1007/s12671-017-0701-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78:169–183. doi:10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bédard M, Felteau M, Marshall S, et al. Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: results from a randomized controlled trial. J Head Trauma Rehabil. 2014;29:E13–E22. [DOI] [PubMed] [Google Scholar]
- 13. Russell L, Ugalde A, Milne D, et al. Feasibility of an online mindfulness-based program for patients with melanoma: study protocol for a randomised controlled trial. Trials. 2018;19:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lawrence M, Booth J, Mercer S, Crawford E. A systematic review of the benefits of mindfulness-based interventions following transient ischemic attack and stroke. Int J Stroke. 2013;8:465–474. doi:10.1111/ijs.12135 [DOI] [PubMed] [Google Scholar]
- 15. Jani BD, Simpson R, Lawrence M, Simpson S, Mercer SW. Acceptability of mindfulness from the perspective of stroke survivors and caregivers: a qualitative study. Pilot Feasibility Stud. 2018;4:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Potter D. Online mindfulness-based stress reduction (MBSR). https://palousemindfulness.com/. Accessed September 1, 2016.
- 17. Winston D. Free guided meditations. http://marc.ucla.edu/mindful-meditations. Accessed September 1, 2016.
- 18. Altschuler A, Rosenbaum E, Gordon P, Canales S Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life—a pilot feasibility study. Support Care Cancer. 2011;20:1291–1297. [DOI] [PubMed] [Google Scholar]
- 19. Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun. 2008;22:969–981. doi:10.1016/j.bbi.2008.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207. [DOI] [PubMed] [Google Scholar]
- 21. Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med. 1975;7:13–31. [PubMed] [Google Scholar]
- 22. Williams LS, Weinberger M, Harris LE, Clark DO, Biller J. Development of a stroke-specific quality of life scale. Stroke. 1999;30:1362–1369. [DOI] [PubMed] [Google Scholar]
- 23. Walach H, Bucheld N, Buttenmuller V, Kleinnecht N, Schimdt S. Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI). Pers Individ Dif. 2006;40:1543–1555. [Google Scholar]
- 24. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi:10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 25. Shosha GA. Employment of Coalizzi’s strategy in descriptive phenomenology: a reflection of a researcher. Eur Sci J. 2012;8:31–43. [Google Scholar]
- 26. AbilityLab. Rehab measure: Ashworth scale/modified Ashworth scale. https://www.sralab.org/rehabilitation-measures/ashworth-scale-modified-ashworth-scalehttp://www.rehabmeasures.org/Lists/RehabMeasures/DispForm. Accessed May 24, 2019.
- 27. Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–474. [DOI] [PubMed] [Google Scholar]
- 28. Carlson LE, Doll R, Stephen J, et al. Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J Clin Oncol. 2013;31:3119–3126. doi:10.1200/JCO.2012.47.5210 [DOI] [PubMed] [Google Scholar]
- 29. Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol Bull. 2006;132:180–211. doi:10.1037/0033-2909.132.2.180 [DOI] [PubMed] [Google Scholar]