Abstract
The prevalence of tattoos is increasing and as such every physician must be aware of the potential adverse events associated with tattooing. Here we present a 36-year-old man with a recent history of skin-coloured papules appearing suddenly in a 20-year-old tattoo on the right forearm. Biopsy and histologic examination confirmed a diagnosis of verrucae planae or flat warts. Tattoo-associated human papilloma virus infections develop clinical manifestations after long latency periods and are often difficult to treat. The risk of tattoo-related human papilloma virus infection should be discussed when considering acquiring a tattoo.
Keywords: Tattoo, verrucae, warts, black ink, human papilloma virus
Introduction
The process of aesthetic tattooing involves the implantation of pigment into the upper and middle dermis to create pictures, words, geometric patterns and other aesthetically desirable designs. Historically, tattoo-associated infection rates were much higher with common transmission and implantation of Staphylococcus and Streptococcus bacteria resulting in erysipelas, cellulitis, gangrene and sepsis.1 Advances in sterile technique have reduced the infectious risks associated with tattooing; however, even recently there have been reports of transmission of hepatitis B, hepatitis C and human immunodeficiency virus (HIV).1–3 Several cases of human papilloma virus (HPV) infections associated with tattoos have been reported.4–7 It is believed that HPV infection in tattoos is attributable either to the inoculation of the area from the tattooing process or the immunomodulatory effects of the tattoo inks. Here we present a case of a 36-year-old man who developed verrucae plana within his 20-year-old tattoo. This case adds to the literature of tattoo-associated HPV infections and serves as a reminder of the risk of tattooing even with advanced sterile technique.
Case presentation
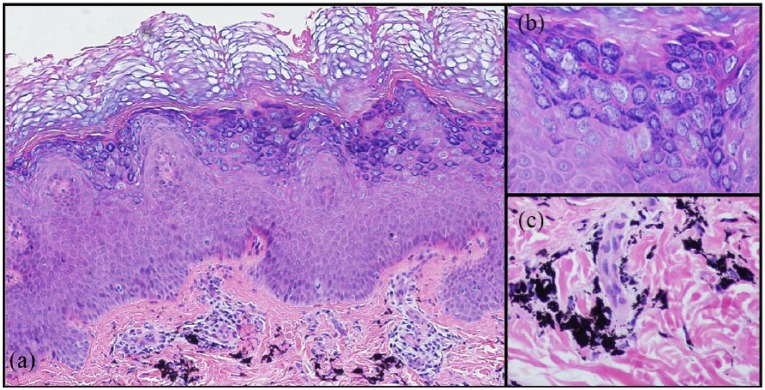
This 36-year-old man presented with a 6-month history of skin-coloured flat-topped papules within a black coloured tattoo (Figure 1). The tattoos over the arms and forearms were applied over 20 years prior by a professional tattoo artist and there was no previous history of cutaneous eruptions within the tattoos. The skin-coloured papules presented suddenly with no associated symptoms. The number of papules within the tattoo had been increasing from the initial time of onset. Hundreds of papules were present at the time of presentation. The patient had no other medical conditions and was not taking any prescription medications. There was a dermatologic history of atopic dermatitis for which topical corticosteroids were used for occasional flares. There was no history of cigarette smoking or intravenous drug use. Full cutaneous examination did not reveal the presence of these skin-coloured flat-topped papules anywhere on the body apart from the tattooed areas of the right forearm and arm. All laboratory investigations were normal including negative tests for HIV and hepatitis. The differential diagnosis included lichen nitidus, papular eczema, papular sarcoidosis, lichen planus and verrucae planae.
Figure 1.
(a) Clinical photograph of the right ventral forearm showing white to skin-coloured flat-topped papules confined to areas of tattoo pigment. (b) Close-up of flat-topped papules with area of scale that developed after treatment with liquid nitrogen cryotherapy.
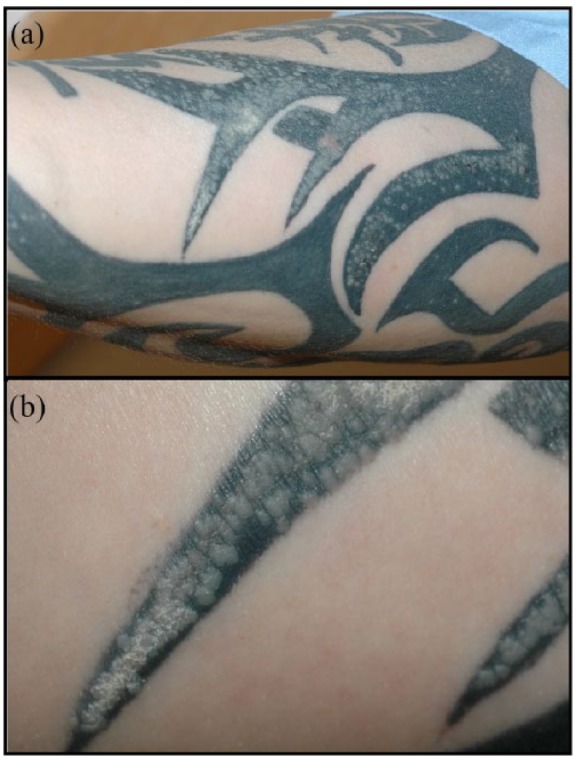
A biopsy was taken from the right forearm and sent for histopathological examination. Histopathology revealed keratinocytes with HPV-induced changes and a diagnosis of verrucae planae was made by the pathologist (Figure 2). The hematoxylin and eosin (H&E) stained slides revealed an epidermis with orthokeratosis, papillomatosis, areas of hypergranulosis and pathognomonic koilocytes. The black tattoo ink was identified in the dermis below the verrucae. Given the diagnosis of verrucae planae associated with tattoo, therapy would have to be tailored to this very unique clinical situation taking into consideration the effects of therapeutics on the tattoo ink.
Figure 2.
(a) Histopathology of biopsy specimen stained with Hematoxylin and Eosin (H&E) showing verrucae planae (200×). (b) Higher magnification of verruca plana showing koilocytes consistent with HPV infection (400×). (c) Higher magnification of tattoo dye particles within the dermis (400×).
Initial treatment consisted of one cycle of light liquid nitrogen cryotherapy directed at two test areas. Unfortunately, this did not result in clinical improvement and a slight scale developed in the treated areas. Topical treatments such as 5% 5-fluorouracil or 5% imiquimod were offered as the next option while informing the patient that these treatments may affect the integrity of the tattoo colour. The patient did not return for follow-up and no further treatments were provided.
Discussion
The prevalence of tattoos in the general population is estimated at 15% to 25% with a higher prevalence among younger men and women.8,9 As the population of tattooed men and women grow, there have been a growing number of reports of complications associated with tattoos.1,8,9 By far the most common reactions to tattoos are the inflammatory reactions. These inflammatory reactions range from koebnerization of existing inflammatory conditions to allergic reactions against components of the tattoo. Less likely, but perhaps more important, are the risks of infection associated with tattoos. Tattoos have been associated with the transmission of HIV, hepatitis B, hepatitis C, syphilis, tuberculosis, leprosy and other mycobacteria infections.1 There have also been several reports HPV infections associated with tattoos.4,5,10 In particular, it appears that black tattoo ink has a higher risk of verrucae development and HPV infection.7
Here we present a case of tattoo-associated verrucae planae or flat warts that developed over 20 years from the time of initial tattooing. Verrucae planae are usually caused by HPV-3, -10, -28 and -49 and have a predilection for the face, larynx and hands. They normally present as white/pink to skin-coloured flat-topped papules. The mechanism by which HPV localizes to the tattoo may involve either traumatic implantation of HPV during the tattoo process or the contamination of the tattoo inks or instruments or by localized immunosuppression that occurs secondary to the tattoo ink. Prior to this case, the longest latency period between tattooing and the development of HPV infection had been 10 years.5 In general, there is a long latency period between tattooing and the manifestations of the HPV infection. The mean latency period is about 5 years. This suggests that the immune system is able to control the infection, and that some immune system perturbation likely results in the development of clinical disease. In one case report, exposure to sunlight resulted in the development of verrucae two and half years after tattooing.10 The patient presented here did not identify any events that may have contributed to the development of verrucae planae.
The main treatment options for verrucae planae involve the use of topical 5% 5-fluorouracil or 5% imiquimod.11,12 The success of these treatments in tattoo-associated verrucae has been limited perhaps due to the deeper implantation of the virus. In addition, there is evidence that some of these topical treatments, particularly imiquimod, may affect the aesthetics of the tattoo.13,14 Other topical treatments that can be considered for verrucae planae include 10% salicyclic acid, 10%–30% glycolic acid and 0.025%–0.05% tretinoin.12 There have also been reports of successful treatment of warts in tattoos with squaric acid dibutylester that did not disrupt the integrity of the tattoo.15 Destructive treatment options such as ablative laser, curetting or surgical excision may also be considered but these modalities may cause significant damage to the tattoo and may result in scarring. In our case, a trial of liquid nitrogen cryotherapy did not result in any significant clinical improvement and superficial scale developed in the areas treated.
In summary, we present a case of verrucae planae associated with a tattoo after a long latency period of more than 20 years. This long-term infectious risk needs to be communicated to patients considering tattoos, as treatment options often have limited efficacy and may negatively impact the aesthetics of the tattoo.
Footnotes
Author contributions: M.G.K. and S.M.W. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content: M.G.K. and S.M.W. Statistical analysis, obtained funding: none reported. Administrative, technical, or material support: none required. Study supervision: S.M.W.
Declaration of conflicting interests: M.G.K. has been a speaker for AbbVie, Actelion, Aralez, Janssen, Novartis and Sanofi Genzyme; and has served on advisory boards for AbbVie, Actelion, Amgen, Celgene, Eli Lilly, Janssen, Leo, Novartis, Sanofi Genzyme, Valeant. S.M.W. has been a speaker and participated in advisory boards for Valeant Pharmaceuticals. No direct conflicts of interest are noted for this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: The patient has provided signed consent for the publication and dissemination of the pictures and information in this case report.
References
- 1. Kazandjieva J, Tsankov N. Tattoos: dermatological complications. Clin Dermatol 2007; 25(4): 375–382. [DOI] [PubMed] [Google Scholar]
- 2. Doll DC. Tattooing in prison and HIV infection. Lancet 1988; 1(8575–8576): 66–67. [DOI] [PubMed] [Google Scholar]
- 3. Samuel MC, Doherty PM, Bulterys M, et al. Association between heroin use, needle sharing and tattoos received in prison with hepatitis B and C positivity among street-recruited injecting drug users in New Mexico, USA. Epidemiol Infect 2001; 127(3): 475–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baxter SY, Deck DH. Tattoo-acquired verruca plana. Am Fam Physician 1993; 47(4): 732. [PubMed] [Google Scholar]
- 5. Miller DM, Brodell RT. Verruca restricted to the areas of black dye within a tattoo. Arch Dermatol 1994; 130(11): 1453–1454. [PubMed] [Google Scholar]
- 6. Trefzer U, Schmollack KP, Stockfleth E, et al. Verrucae in a multicolored decorative tattoo. J Am Acad Dermatol 2004; 50(3): 478–479. [DOI] [PubMed] [Google Scholar]
- 7. Ramey K, Ibrahim J, Brodell RT. Verruca localization predominately in black tattoo ink: a retrospective case series. J Eur Acad Dermatol Venereol 2016; 30(10): e34–e36. [DOI] [PubMed] [Google Scholar]
- 8. Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006; 55(3): 413–421. [DOI] [PubMed] [Google Scholar]
- 9. Heywood W, Patrick K, Smith AM, et al. Who gets tattoos? Demographic and behavioral correlates of ever being tattooed in a representative sample of men and women. Ann Epidemiol 2012; 22(1): 51–56. [DOI] [PubMed] [Google Scholar]
- 10. Brajac I, Loncarek K, Stojnic-Sosa L, et al. Delayed onset of warts over tattoo mark provoked by sunburn. J Eur Acad Dermatol Venereol 2005; 19(2): 247–248. [DOI] [PubMed] [Google Scholar]
- 11. Gladsjo JA, Alio Saenz AB, Bergman J, et al. 5% 5-Fluorouracil cream for treatment of verruca vulgaris in children. Pediatr Dermatol 2009; 26(3): 279–285. [DOI] [PubMed] [Google Scholar]
- 12. Kwok CS, Gibbs S, Bennett C, et al. Topical treatments for cutaneous warts. Cochrane Database Syst Rev 2012; 9: CD001781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Solis RR, Diven DG, Colome-Grimmer MI, et al. Experimental nonsurgical tattoo removal in a guinea pig model with topical imiquimod and tretinoin. Dermatol Surg 2002; 28(1): 83–86; discussion 86–87. [DOI] [PubMed] [Google Scholar]
- 14. Berman B, Poochareon VN, Villa AM. Novel dermatologic uses of the immune response modifier imiquimod 5% cream. Skin Therapy Lett 2002; 7(9): 1–6. [PubMed] [Google Scholar]
- 15. Fania L, Sordi D, Pagnanelli G, et al. Tattoo and warts: efficacy of topical immunotherapy. Eur J Dermatol 2017; 27(3): 322–323. [DOI] [PubMed] [Google Scholar]