Abstract
Background
In the field of prosthetics, the ultimate goal is to improve the clinical outcome by using a technique that prolongs the longevity of prosthesis. Active robotic-assisted total knee arthroplasty (TKA) is one such technique that is capable of providing accurate implant position and restoring mechanical alignment. Although relevant studies have been carried out, the differences in the efficacy and reliability between active robotic-assisted TKA and conventional arthroplasty have not yet been adequately discussed.
Methods
We referenced articles, including randomised controlled trials and comparative retrospective research, from PubMed, Embase, Cochrane Library and Web of Science, in order to compare active robotic-assisted TKA with the conventional technique. Data extraction and quality assessment were conducted for each study. Statistical analysis was performed using Revman V. 5.3.
Results
Seven studies with a total of 517 knees undergoing TKA were included. Compared with conventional surgery, active robotic TKA showed better outcomes in precise mechanical alignment (mean difference, MD: − 0.82, 95% CI: −1.15 to − 0.49, p < 0.05) and implant position, with lower outliers (p < 0.05), better functional score (Western Ontario and McMaster University, Knee Society Score functional score) and less drainage (MD: − 293.28, 95% CI: − 417.77 to − 168.79, p < 0.05). No significant differences were observed when comparing the operation time, range of motion and complication rates.
Conclusion
The current research demonstrates that active robotic-assisted TKA surgeries are more capable of improving mechanical alignment and prosthesis implantation when compared with conventional surgery. Further studies are required to investigate the potential benefits and long-term clinical outcomes of active robotic-assisted TKA.
Keywords: total knee arthroplasty, active robotic-assisted, conventional, systematic review, meta-analysis
Introduction
Total knee arthroplasty (TKA) is a common and reproducible treatment for refractory knee pain induced by degenerative knee arthritis. According to the database of Healthcare Cost and Utilization Project (HCUP) and J ournal of the A merican M edical A ssociation, over 600 000 TKA procedures were performed by 2010, and the number is continuously increasing.1 2 This growing tendency requires a high attention to patient satisfaction and prosthetic longevity.3 4
Perioperative factors such as surgical techniques, patient symptoms and implant selection were considered to influence postoperative survival and the patients’ quality of life.3–6 Despite the advances in etiological research, prosthetic design and surgical techniques, a proportion of the patients undergoing TKA remain dissatisfied and frequently in discomfort, due to instability of the implant.4 7–9 Robotic-assisted surgery was designed in an attempt to prevent this issue. Robotic systems, allowing accurate handling in a limited space, have been developed across many surgical areas.10–13 There are three types of robotic system, namely autonomous (active), hands-on (semi-active) and passive. The main difference among the three systems is the level of involvement of the surgeons during the operation. This technology was developed in knee arthroplasty surgery to better assist surgeons in the precision of bone cutting, mechanical alignment restoration and implant positioning, all of which assist in prolonging the survival of the implant.5 12–16
The active orthopaedic robot, named ‘Arthrobot’, was designed for operation in 1983. In the 1990s, the first robotic total hip arthroplasty (THA) was successfully performed under the assistance of a robotic system named ‘ROBODOC’.10 17
Compared with conventional TKA, robotic-assisted surgery involves the creation of a preoperative patient-specific model and corresponding surgical plan.10 During the operation, accurate bone cutting is performed by the robotic system based on the preoperative plan. Recent evidence showed a better clinical outcome, a lower rate of complications and improved postoperative limb alignment in patients undergoing robotic surgeries.18–20 As a result, robotic-assisted surgery became the preferred surgical technique and from 2008 to 2015, the proportion of robotic procedures had increased from 16.2% to 29.2%.21
However, the efficacy and reliability of robotic-assisted TKA surgery have not yet been thoroughly studied; this has led to some concerns regarding the cost, operation time and the potential for unexpected tissue injuries.5 16 19 22 To date, there is only one meta-analysis in the literature regarding robotic-assisted TKA; this study demonstrated a higher accuracy in mechanical alignment restoration and lower outliers.23 However, there were no collected data for coronal or sagittal inclination, nor any documented clinical complications. Therefore, the aim of this systematic review is to discuss and compare active robotic-assisted TKA and conventional techniques.
Materials and methods
The current research was conducted in reference to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.24
Search strategy
Existing articles from databases including PubMed, Embase, Cochrane Library and Web of Science were referenced. The research strategy included but was not limited to the following terms: ‘Arthroplasty, Replacement, Knee’ with all entry terms; ‘Robotic Surgical Procedures’ with all entry terms; and robot* and convention*. This component of the research was carried out by two different researchers. After screening titles and abstracts, unrelated articles were excluded. Final decisions regarding the inclusion of articles were determined by carefully screening the full texts of the remaining studies. If a controversy occurred, a third researcher was consulted.
Inclusion and exclusion criteria
The inclusion criteria for this review were as follows: (1) a randomised controlled trial (RCT) or non-RCT comparative study published after the year 2000; (2) the purpose of the research was to compare the efficacy and reliability of primary robotic-assisted TKA with conventional TKA and (3) the available data must include demographics and qualitative and quantitative results. Case reports, editorials and non-comparative observational studies were excluded from this meta-analysis.
Data extraction and quality assessment
Data including basic information and clinical outcomes were extracted into statistical tables by two independent researchers. Primary outcome variables included mechanical alignment, accuracy of implant position and outliers. Secondary outcome variables included functional assessment through scoring scales (Hospital for Special Surgery [HSS], Knee Society Score [KSS], Western Ontario and McMaster University [WOMAC], etc), operation time, drainage, gap balance, range of motion (ROM) and complications.(online supplementary table 1)
postgradmedj-2018-136190supp001.docx (34.3KB, docx)
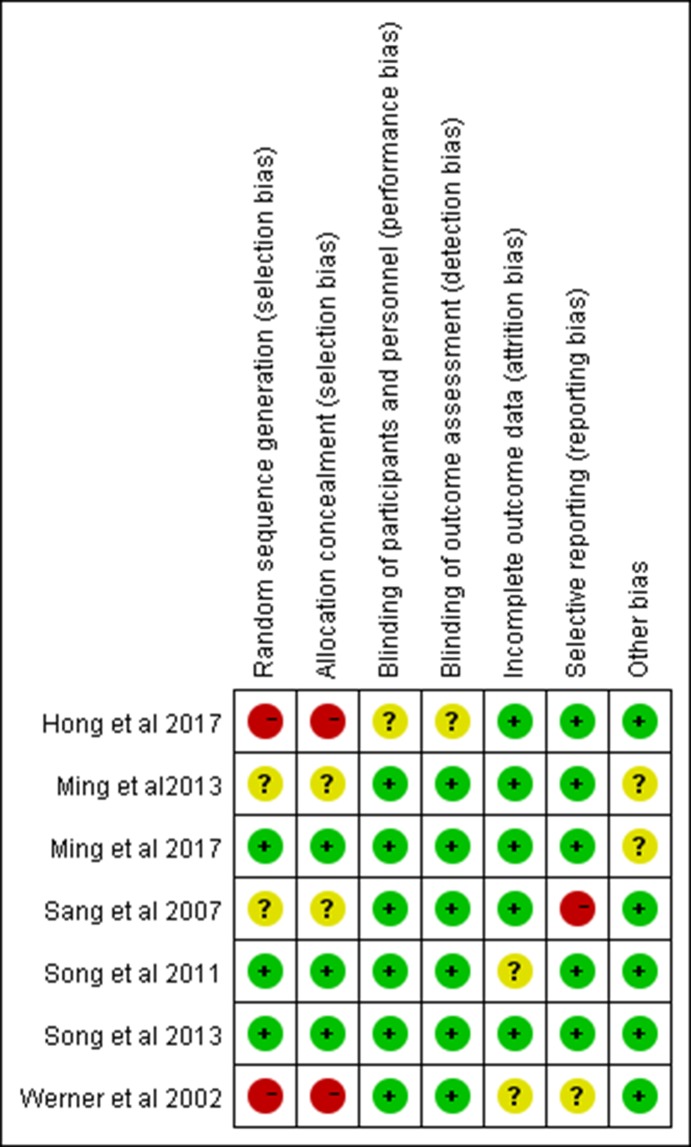
The levels of evidence of all collected studies were confirmed by the Oxford Centre for Evidence-Based Medicine—levels of evidence.25 Risks of bias were evaluated according to the Cochrane Collaboration and by the following criteria: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective reporting and other biases. Each item with an evaluation of ‘Yes’, ‘No’ or ‘Unclear’ indicated a low risk of bias, high risk of bias and lack of information or unknown risk of bias, respectively. For cohort studies, the Newcastle-Ottawa Scale was applied for quality evaluation through three perspectives scaled from 1 to 9: selection, comparability and exposure. For RCTs, we adopted the modified Jadad scale for quality assessment, with the maximum score being 8 and the lowest being 1. Sensitivity analysis was conducted to test the robustness of the outcome by removing one cohort and then calculating the results from the remainder.
Statistical analysis
Continuous outcomes and dichotomous outcomes were calculated using the mean difference (MD) and the OR, respectively. Statistical methods for each meta-analysis item are shown in table 1. A 95% CI was used to evaluate the significant difference between the two groups. The statistical heterogeneity among the included studies was assessed by a χ2 and I2; when I2 >50%, suggesting a significant heterogeneity, a random-effect model was used in the pooled result. In contrast, a fixed effect model was employed when I2 <50%. The overall effect was determined using a Z test. Meta-analysis was conducted by using Review Manager (Revman, V. 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Table 1.
Statistical methods for meta-analysis
| Outcome variable | Statistical method | Effect measure |
| Functional assessment | ||
| HSS | Inverse-variance | MD |
| WOMAC | Inverse-variance | MD |
| KSS functional score | Inverse-variance | MD |
| Radiological assessment | ||
| MA/FCI/TCI/FSI/TSI | Inverse-variance | MD |
| MA/FCI/TCI/FSI/TSI outliers | Peto | Peto OR |
| Surgical aspects | ||
| Operation time | Inverse-variance | MD |
| Drainage | Inverse-variance | MD |
| Range of motion | Inverse-variance | MD |
| Complication rate | ||
| Whole complication rate | Peto | Peto OR |
| Surgery-related complication rate | Peto | Peto OR |
| Infection rate | Peto | Peto OR |
FCI, femoral coronal inclination; FSI, femoral sagittal inclination; HSS, Hospital for Special Surgery; KSS, Knee Society Score; MA, mechanical alignment; TCI, tibial coronal inclination; TSI, tibial sagittal inclination; WOMAC, Western Ontario and McMaster University.
Results
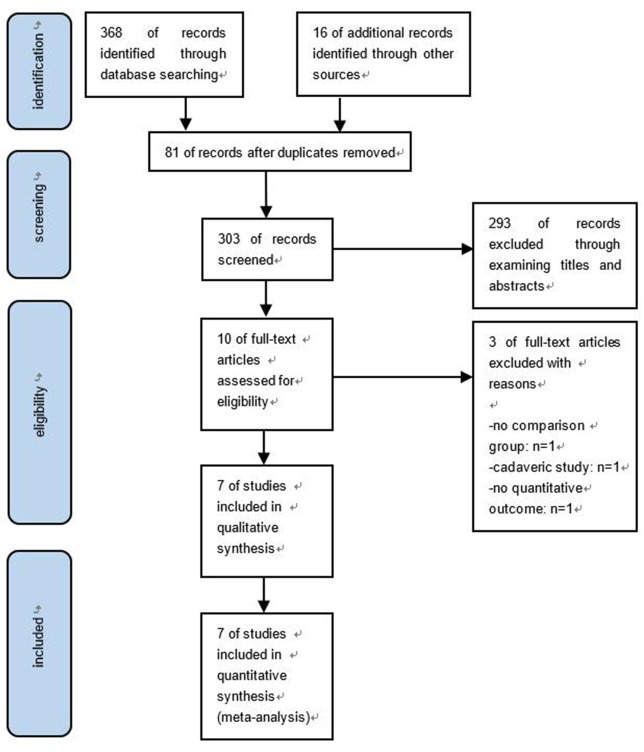
After a comprehensive search process (figure 1), 384 studies were collected from the database. Through discrete screenings, seven articles, with a total of 486 patients and 517 knees, including six RCTs and one retrospective study, were included in this research.26–32 Among them, two articles27 28 were based on the same cohort with different follow-up times; this was confirmed by the original authors via email. Therefore, for the same follow-ups during the same time periods, we selected data from the latest research after discussion with the authors. Although the RCT by Song et al 29 recruited a total of 100 subjects, 26 from the conventional group and 21 from the robotic-assisted group failed to follow-up. For this reason, we analysed data with the remaining 24 subjects from the conventional group and 29 from the robotic group. The demographic data and quality assessments are shown in table 2 and figure 2, respectively.
Figure 1.
The flow chart of literature screening.
Table 2.
Basic information of the included researches
| Reference | Year | Study type | Level of evidence | Cases | Age Mean (SD) |
Robot type | Follow-up (months) | Quality assessment score (actual/total) |
| Hong et al 26 | 2017 | Cohort study | 2b | RA* 71 CA* 42 |
RA 66.3 (7.5) CA 67.8 (6.5) |
ROBODOC | 120 | 7/9 |
| Ming et al 27 | 2017 | RCT | 1b | RA 31 CA 29 |
RA 67.5 (8.6) CA 68.3 (7.7) |
ROBODOC | 24 | 8/8 |
| Ming et al 28 | 2013 | RCT | 1b | RA 31 CA 29 |
RA 67.5 (8.6) CA 68.3 (7.7) |
ROBODOC | 6 | 7/8 |
| Song et al 29 | 2013 | RCT | 2b | RA 50 CA 50 |
RA 66.1 (7.1) CA 64.8 (5.3) |
ROBODOC | 65 | 8/8 |
| Song et al 30 | 2011 | RCT | 1b | RA 30 CA 30 |
RA 67.0 (6.3) CA 67.0 (6.3) |
ROBODOC | 16 | 8/8 |
| Sang et al 31 | 2007 | RCT | 1b | RA 32 CA 30 |
RA 62.7 (6.5) CA 67.8 (6.4) |
ROBODOC | Not mentioned | 6/8 |
| Werner et al 32 | 2002 | RCT | 2b | RA 70 CA 52 |
RA 66.0 CA 68.0 |
CASPAR | Not mentioned | 6/8 |
CA, conventional arthroplasty; CASPAR, computer-assisted surgical planning and robotics; RA, robotic-assisted arthroplasty; RCT, randomised controlled trial.
Figure 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Functional assessment
In the included studies, several scores were collected including the KSS, the HSS, the WOMAC, the Oxford Knee Score (OKS) and the Short Form-36 (SF-36) Health Survey. Song et al 30 31 reported a gradual improvement in both the HSS and WOMAC scores from 3 months postoperative to the final follow-up; however, none of the comparisons between the robotic and conventional approaches were shown to be significant. Hong et al 26 also showed no difference in the HSS and WOMAC scores at the final follow-up. Ming et al 27 provided comparisons on the KSS, OKS and SF-36; although there was no significant difference in the OKS and KSS at the 2-year follow-up, the outcomes of the SF-36 general health at 6 months, the SF-36 vitality and SF-36 role emotional at 2 years were better in the robotic-assisted group. The HSS,26 29 30 WOMAC26 29 30 and KSS functional scores28 31 were included in the meta-analysis. Differences in the data were inconspicuous with regards to HSS, but significant in both the WOMAC and KSS functional scores 6 months after surgery. The results are shown in table 3.
Table 3.
Functional assessment
| Outcomes | Studies | Participants | MD (95% CI) | p Value | Heterogeneity I2 (%) |
|
| RA | CA | |||||
| HSS | 3 (26 29 30) | 130 | 96 | 0.82 (−0.85 to 2.49) | 0.34 | 0 |
| WOMAC | 3 (26 29 30) | 130 | 96 | −2.01 (−4.00 to −0.01) | 0.05 | 0 |
| KSS functional score | 2 (28 31) | 63 | 59 | 2.30 (0.18 to 4.42) | 0.03 | 0 |
CA, conventional arthroplasty; HSS, Hospital for Special Surgery; KSS, Knee Society Score; RA, robotic-assisted arthroplasty; WOMAC, Western Ontario and McMaster University.
Radiological assessment
Mechanical alignment and outliers
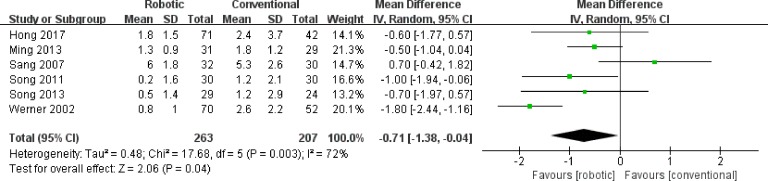
In the current review, six of the included studies compared the mechanical alignment, namely the hip–knee-ankle angle, between the robotic-assisted and conventional groups.26 27 29–32 The result of the collated data favoured the robotic group with a lower mechanical angle, and a significant difference existed in the pooled analysis (figure 3).
Figure 3.
Mechanical alignment of RA versus CA. Mean difference below 0 indicates lower hip–knee–ankle angle of RA group than CA. RA, robotic-assisted arthroplasty; CA, conventional arthroplasty.
In the collated studies, a mechanical outlier was defined as a malalignment >3°; among these studies, five reported an outlier rate in both groups receiving robotic-assisted and conventional surgeries. The data were pooled and the two groups were compared; results demonstrated a significantly lower outlier rate in the robotic-assisted group (figure 4 and table 4).
Figure 4.
Mechanical alignment outlier rate of RA versus CA. OR under 0 indicates lower rate in RA group. RA, robotic-assisted arthroplasty; CA, conventional arthroplasty.
Table 4.
Radiological assessment
| Outcomes | Studies | Participants | MD (95% CI) | OR (95% CI) | p Value | Heterogeneity I2 (%) |
|
| RA | CA | ||||||
| MA | 6 (26,27,29-32) | 263 | 207 | −0.71 (-1.38 to -0.04) | – | 0.04 | 72 |
| FCI | 3 (26, 29, 30) | 130 | 96 | −0.75 (-1.17 to -0.32) | – | <0.001 | 90 |
| TCI | 5 (26, 28-31) | 193 | 155 | −0.50 (−0.83 to −0.16) | – | 0.003 | 0 |
| FSI | 5 (26, 28-31) | 193 | 155 | −1.06 (−2.10 to −0.03) | – | 0.04 | 91 |
| TSI | 5 (26, 28-31) | 193 | 155 | −1.32 (−3.26 to 0.61) | – | 0.18 | 93 |
| MA outliers | 5 (26, 28-30, 32) | 231 | 177 | – | 0.11 (0.06 to 0.19) | <0.001 | 0 |
| FCI outliers | 3 (26, 29, 30) | 130 | 96 | – | 0.13 (0.06 to 0.30) | <0.001 | 0 |
| TCI outliers | 3 (26, 29, 30) | 130 | 96 | – | 0.13 (0.03 to 0.54) | 0.005 | 0 |
| FSI outliers | 3 (26, 29, 30) | 130 | 96 | – | 0.14 (0.06 to 0.29) | <0.001 | 0 |
| TSI outliers | 3 (26, 29, 30) | 130 | 96 | – | 0.14 (0.07 to 0.29) | <0.001 | 0 |
FCI, femoralcoronal inclination; FSI, femoral sagittal inclination; TCI, tibial coronal inclination; TSI, tibial sagittal inclination.
Accuracy of implant position
According to the Knee Society roentgenographic evaluation system,33 the femoral component alignment and tibial component alignment were evaluated through four different angles measured on anteroposterior (AP) and lateral radiographs of the studied knees; these included α (on the femoral coronal plane, the angle between the femoral anatomical axis and the joint line), β (tibial coronal inclination and the optimum 90°), γ (the femoral sagittal inclination and the optimum 0°), δ (tibial sagittal inclination and the optimum 83°) according to research performed by Hong et al 26 and Song et al 30. A concise figure is shown to clearly illustrate the four angles described above (figure 5). Five of the reviewed articles contained data relating to these angles.26 28–31 However, with respect to the α angle from the coronal plane, only two studies recorded this angle in AP view. The study by Sang et al 31 demonstrated a higher α angle in the robotic-assisted group (p<0.0001), whereas in the study by Ming et al,28 the α angle in the conventional group was higher (p=0.0004). The remaining three studies evaluated the femoral coronal alignment using an angle between the joint line and the femoral mechanical axis, known as the femoral coronal inclination angle, with an optimum of 90°. Data from these three studies were eligible for pooling. In order to directly reflect the accuracy of the implant position, we subtracted the inclination angle by its optimal value to calculate the deviation from the optimum. The results showed less deviation in the robotic-assisted group, although there were no significant differences. Similarly, the values of β, γ and δ were also evaluated by the aforementioned process. To conclude, patients in the robotic-assisted group demonstrated a lower deviation value concerning all three angles, with a statistically significant difference observed in β and γ, and no significant divergence in δ.
Figure 5.
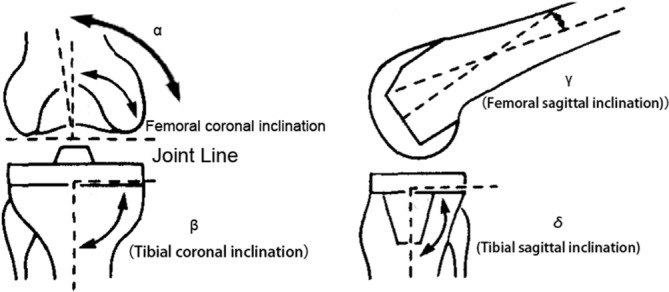
Assessment of femoral and tibial component alignment (referring to knee Society roentgenographic evaluation System33).
The outliers of the femoral and tibial inclination in both the coronal and sagittal plane (a value more than 3° from the optimum) were also examined in the three previously discussed studies. Data indicated a significantly lower outlier rate in the robotic-assisted group compared with the conventional group. No heterogeneity existed in the pooled analysis. The results are shown in table 4.
Surgical aspects
Operation time
Three RCTs recorded the operation duration and were therefore analysed in the pooled result.28–30 The assessment favoured conventional TKA for a shorter duration (table 5); however, the difference between robotic-assisted and conventional surgeries was marginally significant (p=0.08). With regards to the learning curve, Siebert et al 32 reported that, over the course of a total of 70 surgeries, the time required per operation declined from nearly 220 to 90 min.
Table 5.
Surgical aspects and other clinical outcomes
| Outcomes | Studies | Participants | MD (95% CI) | p value | Heterogeneity I2 (%) |
|
| RA | CA | |||||
| Operation time | 3 (28-30 | 111 | 109 | 15.97 (−2.08 to 34.03) | 0.08 | 96 |
| Drainage | 2 (29, 30 | 80 | 80 | −293.28 (−417.77 to −168.79) | <0.001 | 0 |
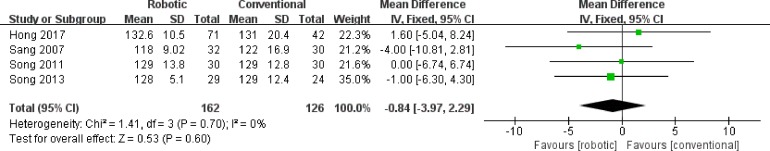
| Range of motion | 4 (26, 29-31) | 162 | 126 | −0.84 (−3.97 to 2.29) | 0.60 | 0 |
CA, conventional arthroplasty; MD, mean difference; RA, robotic-assisted arthroplasty.
Flexion-extension gap and gap asymmetry
The flexion-extension gap was evaluated in two studies. Although the gap balance was defined differently in both studies conducted by Song et al,29 30 the rate of the gap balance was higher in patients from the robotic-assisted group than those from the conventional group. Meanwhile, a lower mean medial-lateral gap asymmetry was also shown in the robotic-assisted group.
Drainage
The postoperative drainage, reflecting blood loss, was presented in two articles.29 30 Results the from pooled data demonstrated a lower volume of blood loss among patients receiving robotic-assisted surgery than those who underwent the conventional procedure; the difference between the two groups was statistically significant and exhibited no heterogeneity (table 5).
Range of motion
All seven studies reported the ROM, both preoperatively and postoperatively. Siebert et al 31 demonstrated an accelerated rehabilitation of the ROM in the robotic group despite no specific quantification. The two studies by Ming et al 27 28 were excluded from the data pooling because the ROM at extension and flexion was recorded independently. In this study, there was no significant difference in the ROM at flexion between the two groups in preoperative time and 6-month and 2-year follow-ups. As for the pooled data of the remaining four studies,26 29–31 although a lower ROM was found in the robotic-assisted group, the difference was not statistically significant (figure 6 & table 5).
Figure 6.
Range of motion of RA vs Ca. Mean difference indicates similar outcome. RA, robotic-assisted arthroplasty; CA, conventional arthroplasty; MD, mean difference.
Complications and revisions
The studies involved in our meta-analysis all reported relevant complications following surgery. Sang et al 31 and Siebert et al 32 observed complications only in the robotic-assisted group, with a rate of 18.8% and 7.7%, respectively. Song et al 30 found no adverse events in patients undergoing either the robotic-assisted surgery or the conventional procedure. The remaining three studies were used for data pooling in three subgroups to compare the complication rates of the two experimental groups.26 28 29 Such complications included whole complications, surgery-related complications and infection. Among them, surgery-related complications were determined based on the Knee Society complication list associated with TKA published in 2014.34 However, the findings from the pooled data analysis failed to show any significant difference in the three subgroups (table 6).
Table 6.
Complication rate
| Outcomes | Studies | Participants | OR (95% CI) | p Value | Heterogeneity I2 (%) |
|
| RA | CA | |||||
| Whole complication rate | 3 (26, 28, 29) | 152 | 121 | 0.83 (0.38 to 1.80) | 0.63 | 0 |
| Surgery-related complication rate | 3 (26, 28, 29) | 152 | 121 | 0.95 (0.33 to 2.70) | 0.92 | 0 |
| Infection rate | 3 (26, 28, 29) | 152 | 121 | 0.99 (0.26 to 3.78) | 0.98 | 0 |
CA, conventional arthroplasty; RA, robotic-assisted arthroplasty.
We included infection for meta-analysis due to its clinical importance for surgeons. Other complications, such as deep vein thrombosis (DVT) and prosthetic instability, were excluded from the data collection because they either lacked sufficient support or were not considered as major relevant adversities. DVT was reported in the study by Ming et al,27 28 with two cases in the robotic group and one case in the conventional group. Only one patient who received conventional surgery in the study by Hong et al 26 demonstrated prosthetic instability.
Revision surgery is often required following postoperative complications such as periprosthetic joint infection or implant instability. In the study by Ming et al,27 one patient in the robotic-assisted group received revision surgery due to persistent lateral knee pain. Hong et al 26 reported revision surgery in five patients, two in the robotic-assisted group and three in the conventional group. Furthermore, Kaplan-Meier survival analysis of the data generated by Hong et al concluded that there was a higher 10 year survival rate among the patients who received robotic-assisted surgeries.
Sensitivity analysis and publication bias
Sensitivity analysis was performed by sequentially removing the data array in each study. As a result, the pooled data showed no significant changes; this may suggest that the involved outcomes are relatively stable and reliable. In terms of publication bias, according to the Cochrane Handbook, the funnel plot is not routinely necessary due to the fact that the number of articles is less than 10, and hence the power of the test is reduced. Despite this, we made two funnel plots to evaluate the potential bias; this included the comparisons on mechanical alignment outliers and the ROM. Both of the funnel plots showed a symmetrical figure within the 95% CI.
Discussion
Since it was first introduced to knee joint arthroplasty in the 1980s,10 robotic-assisted surgery has been broadly advocated for improvements in surgical accuracy.17 35 Such improvements include lower extremity mechanical alignment, component sizes and implantation, and soft tissue balance, which have all been proven to have a high correlation to clinical outcomes and implant survival.3 36–38 In order to ensure precise bone resection, and the appropriate selection and implantation of prostheses during robot-assisted operations, preoperative image examination is always recommended.5 14 18 19 Image data are then transferred to an integrated surgical planning system that creates a three-dimensional model of the patient's knee per the surgeon’s convenience. The process allows orthopaedists to create a prerequisite plan with which postoperative radiological outcome is predictable. In our meta-analysis, all the included studies used an autonomous system meaning that no surgeon was required during the operations.18 Despite the aforementioned advantages that robotic-assisted systems provide to TKA surgery, there remain clear adversities, such as the prolonged surgery duration, unexpected tissue injury and the uncertainty of the cost-effectiveness in a local hospital setting.5 39–41 Therefore, caution is advised when considering fully adopting these newly developed techniques.
To date, our research is the one of the first meta-analysis to compare the efficacy and reliability of active robotic-assisted TKA with conventional TKA. All the studies included in the meta-analysis used the autonomous system, ROBODOC, with an image-based technique as previously stated. One of the included studies was a retrospective study26 while the other six articles were RCTs.27–32 In our study, only articles published after the year 2000 were included; this was due to the rapid evolution of robotic systems in the 2000s, whereby considerable improvements were made in computer-aided work patterns, preoperative planning and precise bone management with less errors.13 22 The positive findings of our research were compared with conventional TKA. Results demonstrated that robotic-assisted surgeries offer benefits in alignment correction, implant accuracy with lower outliers, less drainage after surgery and a plausibly better score in the evaluation scales. No significant differences were found regarding the operation time, ROM and the complication rate between the two methods.
One limitation of our analysis is that since various evaluation systems were adopted to measure patients' clinical outcomes, there was insufficient data in each system, which made it difficult to organise and evaluate. The functional assessment of the WOMAC and KSS scoring system showed significantly higher scores in the robotic-assisted TKA group. The outcome of HSS also favoured the robotic group, although there was no significant difference. Further evidence is required to assess whether the patients’ quality of life can be affected by this score distinction.
One of the most important outcomes of the current research is the accurate coronal alignment restoration of the afflicted legs. In order to improve the clinical and functional outcomes, and therefore extend the longevity of the implant while also reducing the likelihood of prosthetic loosening, an adequate alignment technique has been explored.42 43 Mechanical alignment is recognised as the gold standard in TKA37 42–45; it is achieved through perpendicular cuts with respect to the femoral and tibial mechanical axis.45 Yet, the definition of a safe zone of hip–knee–ankle angle has been a challenge to orthopaedists. A neutral mechanical axis within ±3°, known as the safe zone, is believed to be the optimal target due to its close connection to improved prosthesis survival; such a connection was proven by data from previous studies.46–48 By analysing the aforementioned information, we discovered that the mechanical angle and the rate of mechanical alignment outliers in the robotic-assisted group were lower than those in the conventional surgery group. Heterogeneity concerning mechanical alignment outliers was acceptable. However, as for the mechanical angle, high heterogeneity was detected but could be reduced by eliminating the study by Siebert et al 32 and re-evaluating the remaining studies. It is important to note that the outcome with a statistical difference was unchanged by this exclusion. The factors contributing to this heterogeneity included unclear random sequence generation, allocation concealment at the beginning of the study and the application of a different robotic system (computer-assisted surgical planning and robotics) to the other studies (ROBODOC).32 The pooled data indicated a relatively higher accuracy in the robotic system compared with the manual procedure.
Precise implantation of the prostheses is recognised as another important factor contributing to implant survival.3 36 42 Additionally, Kim et al confirmed the significance of prosthetic implantation alignment.36 Previous studies also suggested that posterior inclination of the tibial component influences the postoperative ROM and prosthetic stability.36 42 49 It is evident that the robotic-assisted procedure can increase the accuracy and precision of the component placement. In this meta-analysis, we found that apart from sagittal tibial inclination, the remaining three measured angles were significantly lower in the robotic-assisted group than those in the conventional group. When considering the high heterogeneity of the included studies, caution is advised when interpreting the outcomes. Through sensitivity analysis, we found the greatest heterogeneity in the studies by Song et al 30 and Sang et al 31; this may be a result of the relatively high attrition and selection biases (figure 2). Additionally, it was justified that with the help of the robotic system, the number of implant outliers was comparatively lower. In conclusion, it is evident that a robotic-assisted system not only enhances implant accuracy but also reduces alignment errors in both the coronal and sagittal planes. The advantages of the robotic system were mainly attributed to its comprehensive preoperative plan, intraoperative monitoring, excellent surface quality, patient-specific resection angle, and appropriate intervention by surgeons.28
The ROM of the knee contributes to a distinctive part of functional restoration in TKA surgeries. However, approximately 1% of the patients that receive joint replacement still encounter postoperative stiffness that severely damage the knee function and consequently negatively affects the patients’ daily life.50 Insufficient knee ROM is usually caused by inappropriate component sizing, a tight extension or flexion gap, component malalignment or malrotation, a lack of rehabilitation and other complications.50 A robotic system can, in theory, avoid the aforementioned issues, yet in our analysis, the pooled ROM data showed no difference between the two surgical methods. In the study by Ming et al,27 28 the mean flexion angle of the patients in the robotic group was slightly lower than that of the conventional group, although it was not entirely clear whether this distinction would affect the functional capacity.
The operation duration is undoubtedly an important factor when evaluating novel techniques, as a prolonged operation could lead to infection, blood loss and other complications.51 52 There is a paucity of related articles comparing the operation time between the two surgical techniques. While Ming et al 28 reported that both surgical techniques were performed in a similar duration, Song et al 29 30 reported an increased duration of the robotic-assisted surgeries. The pooled result from the current analysis was only marginally significant with a high heterogeneity (I2=96%). According to Siebert et al,32 robotic systems require a learning curve that may have a negative impact on the duration of TKA surgeries; the time for planning, registration and milling could also influence the operation duration.
The drainage volume reflects visible blood loss after surgery. Among the included studies, only two reported drainage; in both, the volume of blood lost was significantly lower in the robotic-assisted group than in the conventional group. Song et al 29 30 considered this lower blood loss by the robotic-assisted procedure to be related to no reaming of the intramedullary canal; therefore, robotic-assisted surgery is potentially conducive to reducing blood loss. However, further data are required to investigate the relationship between blood loss and the application of robotic-assisted techniques in the context of TKA surgeries.
With the progression of technology, robots are frequently used in today's TKA procedures,13 18 19 lowering the possibility of complications during and after surgery. From detailed data analysis, it was evident that there were no significant differences in the total complication rate in patients undergoing either robotic-assisted or manual surgeries. In two of the three studies,28 29 a number of complications that were not directly related to TKA surgeries were also recorded. We screened surgery-related complications in order to evaluate whether the robotic system resulted in an increase in safety issues; again, neither the TKA complication rate nor the infection rate exhibited a difference in outcome. Several complications, such as instability and anterior knee pain, which may lead to a decline in patients’ quality of life, resulted in the patients receiving revision surgeries.8 53 54 However, relevant data are sparse in our meta-analysis and since revision surgeries are not common, studies with larger sample groups are necessary.
Our study has several limitations. One such limitation was the relatively small sample size of seven studies, with a total of 486 patients. With multiple statistical testing performed, the incidence of type 1 errors was potentially enhanced, which could influence the reliability of positive findings. Furthermore, as the robotic systems evolve with time, this can result in heterogeneity among the included studies. Among these studies, one performed bilateral TKA simultaneously30 with one side using the robotic technique and the other by the conventional procedure. Additionally, one non-RCT study was included in our analysis,26 which may have led to bias. In addition to introducing bias, the included studies may also contain statistical errors. Four of the included studies26 28 31 32 were found with allocation bias, and two31 32 with reporting bias, which may have contributed to heterogeneity. Moreover, a high heterogeneity could be detected in several of the comparisons, which, in turn, lead to a reduction in the confidence level; to avoid this influence, we conducted a sensitivity analysis. It is also important to note that several of the clinically significant events, such as blood loss and gap balance, were not thoroughly discussed due to inadequate reporting. Additional data are therefore required in order for us to discuss the two surgical methods in greater detail.
Conclusions
Active robotic-assisted TKA provides a more accurate mechanical alignment and implant position, better functional scores and lower blood loss compared with the conventional technique. There were no significant differences regarding the operation time, ROM or complication rates. Further studies are required to evaluate the long-term clinical outcomes of active robotic-assisted TKA surgeries.
What is already known on the subject.
After conventional TKA surgery, a proportion of patients remainfrequently uncomfortable due to the implant instability, which influences postoperative survival and patients’ quality of life.
Robotic-assisted TKA has been shown to provide abetter clinical outcome, a lower rate of complications and improvedpostoperative limb alignment in patients according to recent evidence.
Robotic systems can be divided into three different types:autonomous, hands-on and passive. The main difference among the three systemsis the level of involvement of the surgeons during the operation.
Main messages.
The outcomes of mechanical alignment restoration and implant position from active robotic-assisted total knee arthroplasty (TKA) were superior to that of conventional TKA.
Robotic-assisted TKA provided better functional scores and reduced blood loss. There were no differences in the operation time, postoperative range of motion or complication rates, between the two groups.
Further studies are required to evaluate the long-term clinical outcomes of active robotic-assisted arthroplasty.
Current research questions.
Why is the ROM not improved with robotic-assisted surgery?
Is the long-term outcome in favour of robotic surgery?
From the point of view that a robotic technique offers precise operative management, is active robotic-assisted TKA capable of avoiding more complications than conventional TKA?
Acknowledgments
We express heartful gratitude to all those including the colleagues in our institution, professional peers and supervisors, who provided significant help to our research. We also appreciated the support from National Natural Science Foundation in China (No. 81871740).
Footnotes
Contributors: YR planned the study and wrote the manuscript. SC and YR gathered data from literatures and designed statistical analyses. JW and BF revised the manuscript. XW and BF supervised the study.
Funding: This study was supported by a grant from the National Natural Science Foundation in China (No. 81871740).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. HCPUnet, Healthcare Cost and Utilization Project Agency for healthcare research and quality. Available: http://hcupnet.ahrq.gov/ [Accessed 20 Dec 2012].
- 2. Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA 2012;308:1227–36. 10.1001/2012.jama.11153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rand JA, Trousdale RT, Ilstrup DM, et al. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am 2003;85-A:259–65. 10.2106/00004623-200302000-00012 [DOI] [PubMed] [Google Scholar]
- 4. Von Keudell A, Sodha S, Collins J, et al. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 2014;21:180–4. 10.1016/j.knee.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 5. Lonner JH, Fillingham YA, Pros FYA. Pros and cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty 2018;33:2007–13. 10.1016/j.arth.2018.03.056 [DOI] [PubMed] [Google Scholar]
- 6. Bawa HS, Wera GD, Kraay MJ, et al. Predictors of range of motion in patients undergoing manipulation after TKA. Clin Orthop Relat Res 2013;471:258–63. 10.1007/s11999-012-2591-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wylde V, Learmonth I, Potter A, et al. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg 2008;90:1172–9. [DOI] [PubMed] [Google Scholar]
- 8. Song I-S, Sun D-H, Chon J-G, et al. Results of revision surgery and causes of unstable total knee arthroplasty. Clin Orthop Surg 2014;6:165–72. 10.4055/cios.2014.6.2.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McAuley JP, Engh GA, Ammeen DJ. Treatment of the unstable total knee arthroplasty. Instr Course Lect 2004;53. [PubMed] [Google Scholar]
- 10. Ng AT, Tam PC. Current status of robot-assisted surgery. Hong Kong Med J 2014;20:241–50. 10.12809/hkmj134167 [DOI] [PubMed] [Google Scholar]
- 11. Jung M, Morel P, Buehler L, et al. Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg 2015;400:283–92. 10.1007/s00423-015-1278-y [DOI] [PubMed] [Google Scholar]
- 12. Karthik K, Colegate-Stone T, Dasgupta P, et al. Robotic surgery in trauma and orthopaedics: a systematic review. Bone Joint J 2015;97-B 10.1302/0301-620X.97B3.35107 [DOI] [PubMed] [Google Scholar]
- 13. Lang JE, Mannava S, Floyd AJ, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br 2011;93:1296–9. 10.1302/0301-620X.93B10.27418 [DOI] [PubMed] [Google Scholar]
- 14. Davies BL, Rodriguez y Baena FM, Barrett AR, et al. Robotic control in knee joint replacement surgery. Proc Inst Mech Eng H 2007;221:71–80. 10.1243/09544119JEIM250 [DOI] [PubMed] [Google Scholar]
- 15. Hill C, El-Bash R, Johnson L, et al. Robotic joint replacement surgery: does technology improve outcomes? Health Care Manag 2015;34:128–36. 10.1097/HCM.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 16. Netravali NA, Shen F, Park Y, et al. A perspective on robotic assistance for knee arthroplasty. Adv Orthop 2013;2013(2, supplement):1–9. 10.1155/2013/970703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liow MHL, Chin PL, Pang HN, et al. THINK surgical TSolution-One® (Robodoc) total knee arthroplasty. Sicot J 2017;3 10.1051/sicotj/2017052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty 2016;31:2353–63. 10.1016/j.arth.2016.05.026 [DOI] [PubMed] [Google Scholar]
- 19. Banerjee S, Cherian JJ, Elmallah RK, et al. Robotic-assisted knee arthroplasty. Expert Rev Med Devices 2015;12:727–35. 10.1586/17434440.2015.1086264 [DOI] [PubMed] [Google Scholar]
- 20. Rosenberger RE, Hoser C, Quirbach S, et al. Improved accuracy of component alignment with the implementation of image-free navigation in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2008;16:249–57. 10.1007/s00167-007-0420-y [DOI] [PubMed] [Google Scholar]
- 21. Boylan M, Suchman K, Vigdorchik J, et al. Technology-assisted hip and knee arthroplasties: an analysis of utilization trends. J Arthroplasty 2018;33:1019–23. 10.1016/j.arth.2017.11.033 [DOI] [PubMed] [Google Scholar]
- 22. Parsley BS. Robotics in orthopedics: a brave new World. J Arthroplasty 2018;33:2355–7. 10.1016/j.arth.2018.02.032 [DOI] [PubMed] [Google Scholar]
- 23. Mannan A, Vun J, Lodge C, et al. Increased precision of coronal plane outcomes in robotic-assisted total knee arthroplasty: A systematic review and meta-analysis. Surgeon 2018;16:237–44. 10.1016/j.surge.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 24. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. CEBM Oxford centre for evidence-based medicine – levels of evidence. Available: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ [Accessed Mar 2009].
- 26. Yang HY, Seon JK, Shin YJ, et al. Robotic total knee arthroplasty with a Cruciate-Retaining implant: a 10-year follow-up study. Clin Orthop Surg 2017;9:169–76. 10.4055/cios.2017.9.2.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liow MHL, Goh GS, Wong MK, et al. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2017;25:2942–51. 10.1007/s00167-016-4076-3 [DOI] [PubMed] [Google Scholar]
- 28. Liow MH, Xia Z, Wong MK, et al. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty 2014;29:2373–7. 10.1016/j.arth.2013.12.010 [DOI] [PubMed] [Google Scholar]
- 29. Song EK, Seon JK, Yim JH, et al. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013;471:118–26. 10.1007/s11999-012-2407-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Song EK, Seon JK, Park SJ, et al. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2011;19:1069–76. 10.1007/s00167-011-1400-9 [DOI] [PubMed] [Google Scholar]
- 31. Park SE, Lee CT, Se Park CL. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007;22:1054–9. 10.1016/j.arth.2007.05.036 [DOI] [PubMed] [Google Scholar]
- 32. Siebert W, Mai S, Kober R, et al. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173–80. 10.1016/S0968-0160(02)00015-7 [DOI] [PubMed] [Google Scholar]
- 33. Ewald FC. The knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 1989;248:9–12. [PubMed] [Google Scholar]
- 34. Iorio R, Della Valle CJ, Healy WL, et al. Stratification of standardized TKA complications and adverse events: a brief communication. Clin Orthop Relat Res 2014;472:194–205. 10.1007/s11999-013-2980-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Decking J, Theis C, Achenbach T, et al. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand 2004;75:573–9. 10.1080/00016470410001448 [DOI] [PubMed] [Google Scholar]
- 36. Kim YH, Park JW, Kim JS, et al. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 2014;38:379–85. 10.1007/s00264-013-2097-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991;73:709–14. 10.1302/0301-620X.73B5.1894655 [DOI] [PubMed] [Google Scholar]
- 38. Bugbee WD, Mizu-uchi H, Patil S, et al. Accuracy of implant placement utilizing customized patient instrumentation in total knee arthroplasty. Adv Orthop 2013;2013:1–6. 10.1155/2013/891210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Swank ML, Alkire M, Conditt M, et al. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop 2009;38(2 Suppl):32–6. [PubMed] [Google Scholar]
- 40. Wysocki RW, Sheinkop MB, Virkus WW, et al. Femoral fracture through a previous pin site after computer-assisted total knee arthroplasty. J Arthroplasty 2008;23:462–5. 10.1016/j.arth.2007.03.019 [DOI] [PubMed] [Google Scholar]
- 41. Chun YS, Kim KI, Cho YJ, et al. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 2011;26:621–5. 10.1016/j.arth.2010.05.017 [DOI] [PubMed] [Google Scholar]
- 42. Gromov K, Korchi M, Thomsen MG, et al. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 2014;85:480–7. 10.3109/17453674.2014.940573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Abdel MP, Oussedik S, Parratte S, et al. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J 2014;96-B:857–62. 10.1302/0301-620X.96B7.33946 [DOI] [PubMed] [Google Scholar]
- 44. Schiraldi M, Bonzanini G, Chirillo D, et al. Mechanical and kinematic alignment in total knee arthroplasty. Ann Transl Med 2016;4 10.21037/atm.2016.03.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cherian JJ, Kapadia BH, Banerjee S, et al. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med 2014;7:89–95. 10.1007/s12178-014-9218-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 2009;24:560–9. 10.1016/j.arth.2008.02.018 [DOI] [PubMed] [Google Scholar]
- 47. Longstaff LM, Sloan K, Stamp N, et al. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 2009;24:570–8. 10.1016/j.arth.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 48. Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 2009;24(6 Suppl):39–43. 10.1016/j.arth.2009.04.034 [DOI] [PubMed] [Google Scholar]
- 49. Sah AP, Scott RD, Iorio R. Angled polyethylene insert exchange for sagittal tibial malalignment in total knee arthroplasty. J Arthroplasty 2008;23:141–4. 10.1016/j.arth.2006.12.107 [DOI] [PubMed] [Google Scholar]
- 50. Nelson CL, Kim J, Lotke PA. Stiffness after total knee arthroplasty. J Bone Joint Surg Am 2005;87 Suppl 1:264–70. 10.2106/JBJS.E-00345 [DOI] [PubMed] [Google Scholar]
- 51. Naranje S, Lendway L, Mehle S, et al. Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop Relat Res 2015;473:64–9. 10.1007/s11999-014-3628-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Liabaud B, Patrick DA, Jr. GJA. Higher body mass index leads to longer operative time in total knee arthroplasty. J Arthroplasty 2013;28:563–5. [DOI] [PubMed] [Google Scholar]
- 53. Bozic KJ, Lau E, Ong K, et al. Risk factors for early revision after primary TKA in Medicare patients. Clin Orthop Relat Res 2013;471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Berend ME, Ritter MA, Keating EM, et al. Use of screws and cement in revision TKA with primary or revision specific prosthesis with up to 17 years followup. J Arthroplasty 2015;30:86–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
postgradmedj-2018-136190supp001.docx (34.3KB, docx)