Abstract
Objective
The International Cartilage Repair Society classification is the one mainly used to define chondral defects. However, this classification does not include delamination. The objective of the study is to describe the characteristics of this lesion to better explain its classification in the context of chondral lesions of the hip.
Design
We performed a retrospective analysis of 613 patients who underwent hip arthroscopy. In this group, the incidence, localization, histological characteristics, and association to femoroacetabular impingement as well as to other intraarticular lesions of acetabular delamination (AD) were analyzed. Preoperative magnetic resonance imaging accuracy and the different treatment options were also evaluated.
Results
In our series, the incidence of the AD was 37% (226 patients over 613). The average age of this group was significantly lower (39.3 years) than the entire group of patients. Isolated cam (P < 0.01) and pincer morphologies (P < 0.05) had a significant statistical association with the AD. This lesion was primarily localized at the acetabular chondrolabral junction, mainly on the anterosuperior quadrant. The intraarticular lesions more frequently associated to AD were labral lesions (94.25%, P < 0.01), ligamentum teres lesions (28.32%, P < 0.05), and femoral head chondral lesions (19.9%, P < 0.01). The histological examination of the AD was characterized by hypocellularity and structural disorder of the matrix, with fissures. Treatment remains controversial.
Conclusion
AD represents an intermediate stage in chondral damage and can be classified as a “2a” grade lesion. Histological examination confirms the intermediate and progressive character of this injury.
Keywords: delamination, femoroacetabular impingement, hip cartilage, classification
Introduction
The development and advances in the indications for arthroscopic treatment of hip pathologies inevitably lead to a pursuit of a more accurate definition and characterization of joint lesions.
Arthroscopy is still the technique of reference for the description of cartilage lesions in the hip.1 Anderson et al.2 have demonstrated a low sensitivity of magnetic resonance imaging (MRI) examinations in highlighting chondral injury (22%). In their experience, only one-third of the patients with delamination were diagnosed preoperatively through MRI.
The International Cartilage Repair Society (ICRS) classification3 is the one mainly used to define the chondral articular defects. Based on the lack of its correspondence for the hip, Konan et al.4 have proposed a further classification, specific for this articulation. This added classification, besides the histological characteristics, makes a precise reference to the localization of the chondral defects through an acetabular mapping system. The acetabular labrum articular disruption (ALAD)5 classification defines delamination or chondral flap as the third degree in a 4-stage classification and does not make any difference between the 2 conditions. The classification from Beck et al.6 is based on the morphology and depth of the chondral damage as an isolated lesion in the acetabulum. It distinguishes 4 degrees of progression of the lesions, where grade 1 is chondromalacia or cartilage fibrillation, and grade 4 is a full-thickness injury. As an intermediate stage, degree 2 is described as “debonding” or loss of chondral fixation but with an intact cartilage surface unlike grade 3 where there is already a loss of fixation and thinning of the cartilage and formation of a chondral flap. This classification has the advantage that it was created specifically for the hip, based on the damage occurring in cases of femoroacetabular impingement (FAI) syndrome. A potential disadvantage is that it was developed based on macroscopic findings in open surgery.
However, even in literature, a classification that includes the delamination is still missing. The missing clarity regarding the definition and description of such lesions makes it difficult to find in literature corresponding histopathological and epidemiological data, as well as treatment options.
We performed a retrospective analysis of 613 patients who underwent a hip arthroscopy, to study the histological characteristics, the incidence, localization, as well the association to FAI and other intra-articular lesions of the acetabular delamination (AD).
Treatment alternatives have also been investigated.
Materials and Methods
The 613 patients evaluated in the present study underwent hip arthroscopy between January 2010 and October 2016. The institutional review board of the involved hospital decided that no ethical approval was necessary. Among the 613 evaluated patients, 37% (226) presented an AD. The average age of the patients having an AD was 39.3 years (95% confidence interval [CI] = 37.64-40.91), significantly lower (P < 0.01) compared with an average age of 46.8 years (95% CI = 45.57-48.03) calculated for the whole group of 613 patients. In all cases, FAI syndrome was diagnosed with clinical symptoms and radiological findings: X-ray with standardized anteroposterior view, Dunn view, and false profile Lequesne view, MRI, and 3-dimensional computed tomography scan.
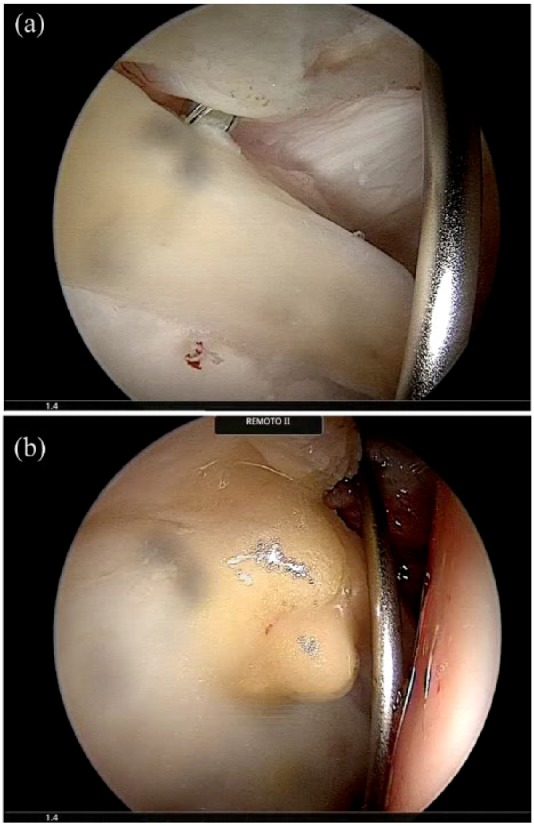
We defined AD as an area of fibrous degeneration of the cartilaginous surface and the transition zone (chondrolabral junction) as the result of a partial detachment from the subchondral bone without however exposing it, without an interruption of the fibrous layer ( Fig. 4a and b ). For this, we differentiated it from the chondral flap lesion in which there is a complete detachment of the chondral coat from the subchondral bone with its exposure ( Fig. 5a and b ). Therefore, according to the ICRS system, delamination was classified as a 2a grade lesion, evidencing a progression of the cartilage damage between grade 2 and grade 3.7
Figure 4.
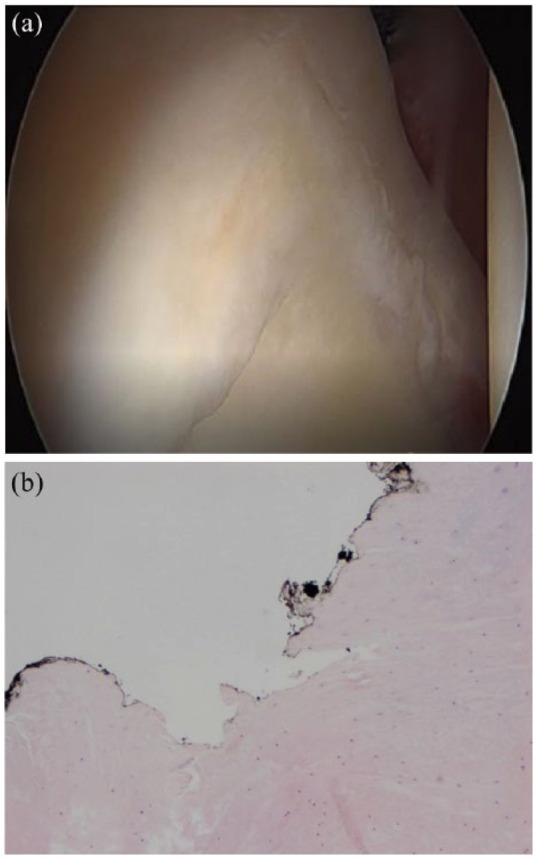
(a) Acetabular delamination. The fibrous layer is still intact on the joint surface, and the subchondral bone is not exposed. (b) Histological characteristics of delamination: hypocellularity and increased eosinophils of the matrix. The articular surface is marked with china ink. It presents itself as irregular and fibrillated.
Figure 5.
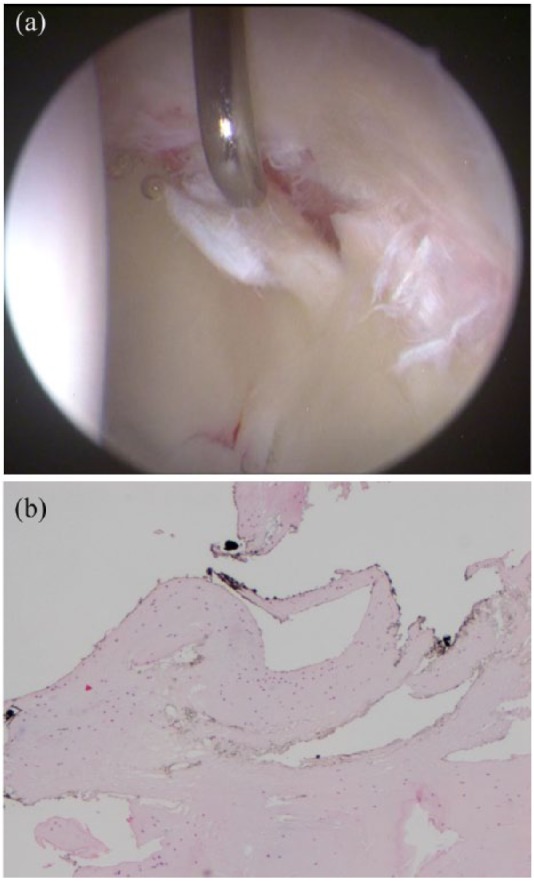
(a) Chondral flap: the chondral layer is discontinued and considerably exposes the subchondral bone. (b) Histological characteristics of the chondral flap: hypocellularity, marked eosinophils of the matrix. The articular surface is marked with china ink and presents itself as irregular, fibrillated, and fragmented.
The procedures were performed by the same senior surgeon, with more than 20 years of practice in hip arthroscopy. The AD was diagnosed by the presence of the arthroscopic “wave” or “carpet” signs ( Fig. 1 ). The arthroscopic procedures were performed with the patient in the lateral position, in total or spinal anesthesia. A shoe traction system (Traditional Lateral Hip Positioning System, Smith & Nephew Andover, MA) was used. Supra-trochanteric and supra-anterior-para-trochanteric arthroscopic portals were used in all cases. The localization of the acetabular chondral defects was reported using a mapping system ( Fig. 2 ).
Figure 1.
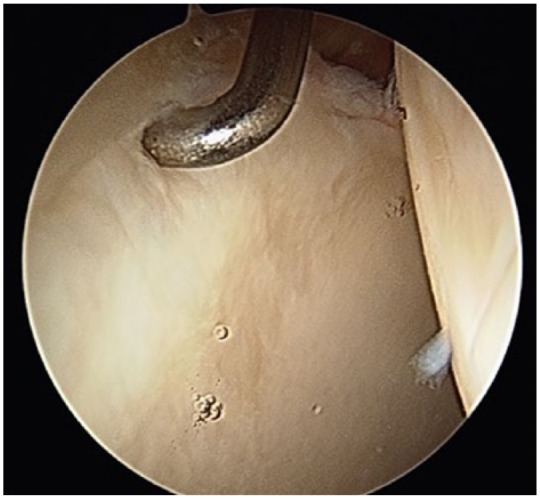
Wave sign: probing the periphery of the lesion, the superficial layer of degenerated fibrocartilage transfers movement at the center of the lesion.
Figure 2.
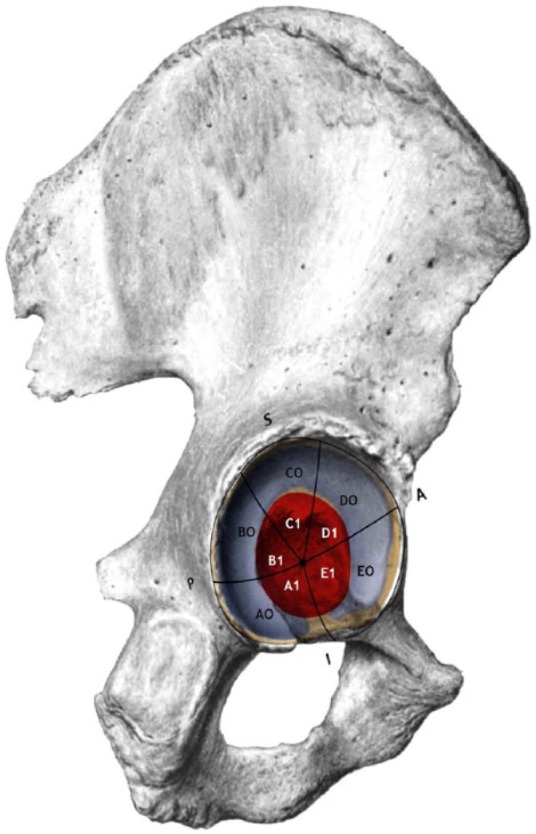
Acetabular mapping system.
The AD was treated by microfragmented adipose tissue transplant (LIPOGEMS), injected at a level of the interface between subchondral bone and delaminated cartilage, in accordance to the Villar technique8 ( Fig. 3a and b ).
Figure 3.
(a) Acetabular delamination (AD) area: A needle is introduced between the subchondral bone and the fibrous chondral layer. A second needle is placed into the joint space to aspirate the fluid. (b) Part of the transplant tissue outflows the chondrolabral junction area.
We used GraphPad Prism 5.0 for the statistical analysis. Varied epidemiological variables such as age, intraoperative diagnosis, femoral and acetabular morphologies, localization of the chondral defects, and other associated articular chondral lesions were studied.
Contingency tables considering the relationship between the presence of AD and both preoperative diagnosis and hip intraoperative assessed lesions were statistically analyzed by using the 2-tailed 95% confidence interval Fisher’s exact test.
In 5 patients with the AD, it was possible to perform an intraoperative biopsy, which was oriented by the surgeon marking the articular surface with ink and submitted for histological examination to the Surgical Pathology Department. Biopsies were processed as follows: specimens were placed in 10% formalin solution for 24 hours of fixation, then paraffin-embedded, and 5-µm sections were cut from paraffin blocks to perform hematoxylin and eosin staining. Slides were evaluated independently by 3 expert pathologists to assess cell and tissue morphology and the cartilage matrix.
Results
FAI syndrome was the preoperative diagnosis for the total group of patients included in the study, the prevalence and frequencies are indicated in Table 1 . Isolated cam morphology resulted in being a major statistically significant risk factor for the appearance of the AD (P < 0.01 with odds ratio 5.87). Same results were found for the isolated pincer morphology, whose association with AD also was statistically significant (P < 0.03 and odds ratio 1.79) and for the combined morphology (P < 0.01 and odds ratio 0.25). A statistical analysis of the correlation between alpha angle values and the AD was not conducted in this study.
Table 1.
Prevalence and Frequency of Femoroacetabular Impingement Morphologies in the Acetabular Delamination Group.
| Valid | Frequency | Percentage | Cumulative Percentage |
|---|---|---|---|
| Absent | 63 | 27.9 | 27.9 |
| Cam | 112 | 49.6 | 77.5 |
| Pincer | 24 | 10.6 | 88.1 |
| Combined | 27 | 11.9 | 100.0 |
| Total | 226 | 100.0 |
As for the localization, the major incidence of the AD was found at the C0 quadrant level (93.8%). The presence of AD was also statistically significant at the D0 quadrant level (incidence of 29.65%, P < 0.001 and odds ratio 0.10). Occasionally, we found AD at the A0 (0.4%), B0 (5.3%), B1 (0.4%), C1 (4.4%), and D1 (1,3%) quadrants. In no case, we found this type of lesion in the quadrants A1, E0, and E1.
Labral tears were the intra-articular lesion most frequently associated to AD (incidence of 94.25%, P < 0.01, and odds ratio 0.085), followed by ligamentum teres lesions (incidence of 28.32%, P < 0.05, and odds ratio 0.62) and femoral head chondral defect (incidence of 19.9%, P < 0.01, and odds ratio 0.16).
When labral tears were found (213 cases), it was fibrillary in 134 cases (62.9%), degenerate in 39 cases (18.3%), bruised or with extended zone of ecchymosis in 10 cases (4.42%), and unstable in 30 cases (14.0%), with only 1 case where it was completely detached.
In only 19 cases of 226 (8.4%) the preoperative MRI reported a chondral defect comparable to an AD.
Histology
The histological examination of the area affected by the acetabular delamination evidenced a considerable hypocellularity (about 30%) associated to fragmentation and fissuring of the matrix, extended till the subchondral bone but not involving the articular surface ( Fig. 4b ).
The matrix showed a considerable architectural disorder with diffuse eosinophils and myxoid degeneration foci ( Fig. 4b ).
The collagen fibrous layer appeared inverted in structure and orientation. Chondrocytes presented a nonhomogeneous distribution and were relatively more numerous in the deepest chondral layer. We also occasionally observed superficial microfoci with a slight increase in cellularity ( Fig. 6a and b ).
Figure 6.
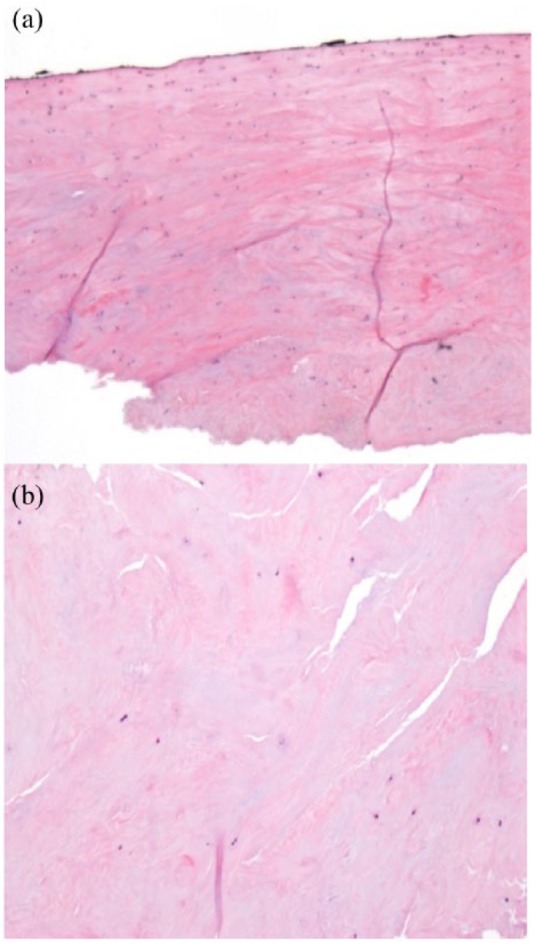
(a) Histological characteristics of delamination (enlarged 4×). The chondral coat is continuous. Matrix presents fissures which reach the subchondral bone, without exposing it. (b) Histological characteristics of delamination (enlarged 10×). The matrix appears structurally inverted with marked eosinophilia. Significant hypocellularity and fibrous degeneration is observed.
Discussion
ICRS classification of chondral lesions,3 in our opinion, gives more considerable importance to the depth of the lesion, while, in the hip, the extension and the location of the defect must be taken into greater consideration: acetabular delamination is not considered in this classification system. At the same time, the wave sign, specific for the AD, is not applicable with the grade 1 or 2 “softening” described in the ICRS classification. This latter lesion is defined as a superficial chondral lesion, which is not associated with subchondral bone detachment. In previous literature, delamination has been classified as a grade 3 lesion by Konan et al.4
In the ALAD classification,5 AD is identified to the same degree (grade 3) of chondral flap: this statement is not matched with our histological data, in which the degeneration of the cartilaginous surface is associated with an involvement of the transition zone (finding not present in chondral flap), without exposition of the subchondral bone. The AD is better applicable, in our opinion, to an intermediate stage, grade 2, described by Beck et al.6 as “debonding” or loss of chondral fixation but with an intact cartilage surface. Mygind-Klavsen et al.,9 have defined delamination as a fibrous degeneration of the chondral coat associated with a macroscopic detachment from the subchondral bone.
In any case, there is lack of a precise definition for this type of lesion.
We have therefore classified delamination as a stage 2a lesion, referring to the ICRS classification, differentiating it from a stage 2 where the fibrous degeneration of chondral surface is not associated to a subchondral bone detachment. We also distinguish it from a stage 3 where the damage of the chondral coat reaches the subchondral bone and exposes it. In this sense, it reflexes the progressive nature of the lesion, that should be considered as an intermediate stage in the evolution toward an arthritic degeneration. The histological study supports the progressive and intermediate characteristics.
The morphological alterations found in the hip were already described with the introduction of FAI concept,10 as a result of the abnormal contact between the acetabular surface and femoral neck. The FAI syndrome, especially the cam morphology,11 is indeed in our experience the most frequent pathology found in patients with the AD.
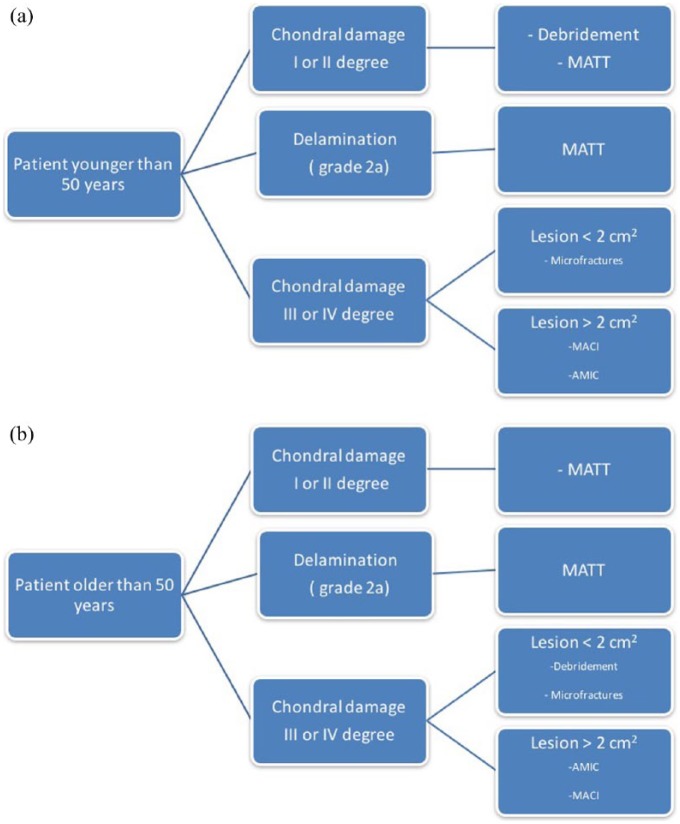
Figure 7a and b describe the type of chondral lesions we treat by a decision tree, based on a recent publication.12
Figure 7.
(a) Decision tree for patients younger than 50 years. (b) Decision tree for patients older than 50 years.
The primary aim in the treatment of AD is to regenerate the chondral layer, which underwent a fibrous degeneration and at the same time stabilize it to the subchondral bone.
Villar et al.8 reported a series of 19 patients whose lesion was treated with an injection of fibrin glue, experiencing an improvement in pain and functionality after 6 to 12 months from the surgery
Mardones and Larrain13 used mononuclear cellular concentrate (MCC) in PRP matrix in 13 cases, after the microfracture. The authors report improvement in all patients at 3 and 6 months.
Another option considers the utilization of autologous chondrocites.14 Even if the implementation of autologous chondrocytes has a beneficial in repairing the chondral damage, it requires 2-step surgical procedures and therefore poses considerable problems both ethically as well as economically.
Increasing attention has been given to the role of autologous mesenchymal cells in chondral regeneration.15 One of the primary sources for mesenchymal cells collection is the bone marrow aspirate. Anyway, there are still no significant clinical reports on results applying this technique.
Adipose tissue represents an abundant and easily accessible source of bioactive tissue with cellular content up to 500 times more than bone marrow.16 In our study, all the patients affected by an AD underwent treatment with the injection of microfragmented adipose tissue transplant in between the subchondral bone and the delaminated chondral layer. Although this procedure seems to be very useful in the short-term follow-up, results must be evaluated in the medium- and long-term outcomes.
Finally, different treatment options have been proposed in the literature ( Table 2 ), but they remain controversial with the need of medium- to long-term follow-up evaluations.
Table 2.
Different Treatment Options in the Literature.
| Authors | No. of Patients | Technique | Follow-up (Months) |
|---|---|---|---|
| Tzaveas and Villar (2010)8 | 19 cases | Injection of fibrin glue | 6-12 |
| Mardones and Larrain (2016)13 | 13 cases | Mononuclear cellular concentrate (MCC) in platelet-rich plasma matrix, after the microfracture | 3-6 |
| Fontana et al. (2012)14 | 15 cases | Autologous chondrocyte transplantation | 74 |
| Jannelli and Fontana (2017)12 | / | Microfragmented adipose tissue transplantation (MATT) | — |
Kaya et al,17 in a recent publication, have demonstrated that in patients with cam morphology, the chondral damage develops mainly on the superior and anterosuperior quadrants.
Anderson et al.2 assumed a protective role in the pincer morphology of FAI syndrome concerning the acetabular chondral damage. On the contrary, Camacho-Alvarez and Mardones-Peterman18 reported a high association rate between AD and pincer at the anterosuperior and anterior areas of the acetabulum.
In our study, the AD was prevalently localized at the chondrolabral junction with different degrees of labral damage, which nevertheless never appeared calcified. These data confirm its intermediate characters and the differences with the chondral flap, in which the chondrolabral junction is not injured.
The presence of more frequent localization at the anterior-superior quadrants (C0 and D0) can be explained by a significant association with cam morphology.
We have also evidenced that AD was often associated with central compartment lesions, such as femoral head chondropathy and ligamentum teres lesion. That suggests a complex alteration of the biomechanics of the hip, in which the tangential and shear forces are increased. Therefore, the AD would be the expression of this biomechanical modification at the level of the acetabular chondral layer.
This study has some limitations. First, the correlation between the values of alpha angle and the presence of AD was not calculated. Also, the clinical correlation between the presence of AD, symptoms or clinical outcome score was not evaluated.
Conclusion
Delamination should be considered as an intermediate stage of chondral damage, in which a fibrous degeneration of the cartilage is associated to a partial detachment from the subchondral bone. Delamination could be classified as a “2a” grade if the ICRS classification of chondral damages is considered the classification of choice.
In our study, the AD was mainly located at the chondro-labral junction on the anterior-superior acetabular quadrants. Labral tears, ligamentum teres damages, and femoral head chondropathy were the most associated lesions.
The AD was most frequently associated with isolated cam and pincer morphologies.
Even if the use of new biotechnologies seems to be promising, treatment remains controversial, and we hope that the introduction of this new category of classification could push surgeons to find new strategies for treatment.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The institutional review board of the involved hospital decided that no ethical approval was necessary as it was thought that for this retrospective study the informed consent of the patients was sufficient.
Informed Consent: Written informed consent was obtained from all subjects before the study.
Trial Registration: Not applicable.
ORCID iD: Jannelli Eugenio  https://orcid.org/0000-0003-4447-1480
https://orcid.org/0000-0003-4447-1480
References
- 1. Lubowitz JH, Poehling GG. Hip arthroscopy: an emerging gold standard. Arthroscopy. 2006;22(12):1257-9. doi: 10.1016/j.arthro.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 2. Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91(2):305-13. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 3. Ellermann JM, Donald B, Rohr S, Takahashi T, Tompkins M, Nelson B, et al. Magnetic resonance imaging of osteochondritis dissecans: validation study for the ICRS classification system. Acad Radiol. 2016;23(6):724-9. doi: 10.1016/j.acra.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 4. Konan S, Rayan F, Meermans G, Witt J, Haddad FS. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br. 2011;93(3):332-6. doi: 10.1302/0301-620X.93B3.25322. [DOI] [PubMed] [Google Scholar]
- 5. Kelly BT, Philippon MJ. Arthroscopic hip anatomy. In: Callaghan JJ, Rosenberg AG, Rubash HE, editors. The adult hip. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. p. 78-9. [Google Scholar]
- 6. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012-8. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 7. Fontana A, Mancini D, Gironi A, Acerbi A. Hip osteochondral lesions: arthroscopic evaluation. Hip Int. 2016;26(Suppl 1):17-22. doi: 10.5301/hipint.5000406. [DOI] [PubMed] [Google Scholar]
- 8. Tzaveas AP, Villar RN. Arthroscopic repair of acetabular chondral delamination with fibrin adhesive. Hip Int. 2010;20(1):115-9. [DOI] [PubMed] [Google Scholar]
- 9. Mygind-Klavsen B, Grønbech Nielsen T, Maagaard N, Kraemer O, Hölmich P, Winge S, et al. Danish Hip Arthroscopy Registry: an epidemiologic and perioperative description of the first 2000 procedures. J Hip Preserv Surg. 2016;3(2):138-45. doi: 10.1093/jhps/hnw004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 11. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15(9):561-70. [DOI] [PubMed] [Google Scholar]
- 12. Jannelli E, Fontana A. Arthroscopic treatment of chondral defects in the hip: AMIC, MACI, microfragmented adipose tissue transplantation (MATT) and other options. SICOT J. 2017;3:43. doi: 10.1051/sicotj/2017029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mardones R, Larrain C. Cartilage restoration technique of the hip. J Hip Preserv Surg. 2015;3(1):30-6. doi: 10.1093/jhps/hnv061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fontana A, Bistolfi A, Crova M, Rosso F, Massazza G. Arthroscopic treatment of hip chondral defects: autologous chondrocyte transplantation versus simple debridement—a pilot study. Arthroscopy. 2012;28(3):322-9. doi: 10.1016/j.arthro.2011.08.304. [DOI] [PubMed] [Google Scholar]
- 15. Eslaminejad MB, Poor EM. Mesenchymal stem cells as a potent cell source for articular cartilage regeneration. World J Stem Cells. 2014;6(3):344-54. doi: 10.4252/wjsc.v6.i3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fraser JK, Wulur I, Alfonso Z, Hedrick MH. Fat tissue: an underappreciated source of stem cells for biotechnology. Trends Biotechnol. 2006;24(4):150-4. doi: 10.1016/j.tibtech.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 17. Kaya M, Suzuki T, Emori M, Yamashita T. Hip morphology influences the pattern of articular cartilage damage. Knee Surg Sport Traumatol Arthrosc. 2016;24(6):2016-23. doi: 10.1007/s00167-014-3297-6. [DOI] [PubMed] [Google Scholar]
- 18. Camacho-Alvarez D, Mardones-Peterman R. Femoroacetabular impingement: association between the over-coverage and acetabular cartilage delamination areas [in Spanish]. Rev Esp Cir Ortop Traumatol. 2013;57(2):111-6. doi: 10.1016/j.recot.2012.11.005. [DOI] [PubMed] [Google Scholar]