Short abstract
See Article Stehli et al
Keywords: Editorials, acute coronary syndrome, door‐to‐balloon time, sex, ST‐segment–elevation myocardial infarction, women
Subject Categories: Quality and Outcomes
Almost 3 decades ago, Dr Bernadine Healy used the term “Yentl's Syndrome” to describe the historical price women have had to pay for being different from men in health care, and specifically in terms of cardiovascular care.1 The heroine of the Isaac Bashevis Singer story, Yentl, had to disguise herself as a man in order to study the Talmud because being like a man was the price a woman had to pay for equality. Dr Healy noted that in cardiovascular disease (CVD), women remained second‐class citizens in terms of equity of treatment and outcomes of the disease that was most likely to kill them. This drove the cardiology community to implement changes to improve the prevention, treatment, and outcomes of women,2 and over time, led to the release of guidelines that were specific to women,3 increased research on sex differences in CVD, and initiated awareness campaigns targeted to women such as the American Heart Association's Go Red campaign. All have contributed to a reduction in deaths in women caused by CVD.4 Despite the progress, gaps still persist in how we treat women and the impact on outcomes, particularly in women with ST‐segment–elevation myocardial infarction (STEMI).5
Decades of tracking outcomes with Get With the Guidelines‐Coronary Artery Disease continue to show gaps in the treatment of women with STEMI,6, 7 and similar findings have been replicated throughout the world.8, 9, 10, 11 In this issue of the Journal of the American Heart Association (JAHA), the study by Stehli et al shows similar findings from a prospective contemporary registry from Australia.12 Specifically, this study showed delays not just in door‐to‐balloon (DTB) time for women with STEMI by >7 minutes when compared with men, but also a much greater delay in reported symptoms‐to‐door (STD) time by almost 30 minutes. Although STD and DTB times did not remain independent predictors of mortality in this study, the importance of early revascularization is well established. There was a significant increase in 30‐day mortality in women with STEMI compared with men. There was no sex difference in DTB or STD time in the non‐ST‐segment–elevation myocardial infarction group, as well as no sex difference seen in the 30‐day mortality for non‐ST‐segment–elevation myocardial infarction. Admittedly this study looked only at those who underwent a percutaneous intervention for either STEMI or non‐ST‐segment–elevation myocardial infarction, limiting the outcome to those who were chosen for an interventional approach.
For STEMI, it is well‐established that timeliness of revascularization is a key component to improving outcomes. Rapid DTB times save lives and as a result of quality improvement initiatives and public reporting, the DTB times have improved across the United States.13 Despite this, there have been persistent sex differences in timeliness of care, as measured by DTB time, with women of all ages being less aggressively treated when compared with men.14, 15 Protocol‐driven initiatives have been demonstrated to reduce sex gaps in STEMI treatment, particularly in terms of timeliness of care for women, resulting in a reduction in the 30‐day mortality rate, even though mortality rates still remained higher in women compared with men, even with the use of protocols.16
Unlike the improvements we have seen over time in DTB times, delays in seeking treatment have not improved,17 and as this study demonstrates the STD times are significantly longer in women with STEMI than in men.12 Ultimately the greatest delay to initiation of any treatment hinges on the STD time. In this prospective registry, there is no information regarding the patients’ symptoms, nor their mode of transportation to the hospital, both of which can affect timeliness of presentation and also initiation of treatment.12 However, awareness of cardiovascular risk is underappreciated in women, as demonstrated by the Women's Heart Alliance survey, with only 45% of women recognizing that CVD was the number 1 killer of women.18 Additionally, only a minority of primary care physicians even feel comfortable assessing CVD risk, making discussions (and therefore awareness) of risk less likely to happen in a physician's office.18 Effective public awareness campaigns and education are needed to help women understand their risk of CVD and also the need for timely care when it comes to surviving a heart attack. Additionally, education of the healthcare community is desperately needed to better serve our patient population.
There should be specific steps to improve outcomes of women after STEMI, including the following (Figure):
Public awareness and education of women: Specific efforts need to be made to ensure women understand their risk of CVD and understand the timeliness of care when experiencing a possible myocardial infarction. Awareness of symptoms that suggest a heart attack in women needs to be disseminated in the female population. Additionally, the need to call 9‐1‐1 for EMS transport to the closest emergency room should be an important part of the messaging, in order to initiate timely medical management. Current public awareness strategies have not reached a significant portion of the population, and there should be a public health effort made to reach women, particularly minority women, to a greater extent than what has been achieved thus far.
Education of healthcare providers: There remains a gap in cardiovascular care for women, particularly in the setting of STEMI, as demonstrated by this recent study. Our educational mission to both understand sex differences in CVD and recognize gaps in care of women with any acute coronary syndrome is a vital first step to removing the gap in cardiovascular care and reducing the higher mortality seen in women. This must be mandatory in the medical education of physicians, but needs to be expanded beyond just medical students because the gaps in education exist in a significant portion of healthcare practitioners who care for women.18, 19
Protocol‐driven STEMI care: Systems‐based approaches have been demonstrated to reduce (but unfortunately, not eliminate) the sex gap in care with STEMI, improving adherence to guideline‐recommended treatment and outcomes in women.16 Broader implementation of such protocols through electronic health systems may help in the implementation of such approaches to improve the outcomes in women with STEMI.
Use of artificial intelligence in STEMI management: Artificial intelligence and machine learning may be future considerations for approaches to improving STEMI care and eliminating sex disparities. Artificial intelligence may be able to use predictive modeling of features of STEMI and provide a standardized approach to care, which can eliminate implicit bias in the care of women. More work needs to be done in this area, but artificial intelligence has important potential implications in the care of women.20
Increased research on sex disparities in STEMI and ongoing reporting of STEMI care by sex: The need for ongoing research into the factors that impact sex differences in CVD care and outcomes remains necessary given the persistence in sex disparities.7 Continued surveillance of the care of STEMI stratified by sex is necessary to track changes in these trends over time, to ensure equality in the cardiovascular care of women.
Figure 1.
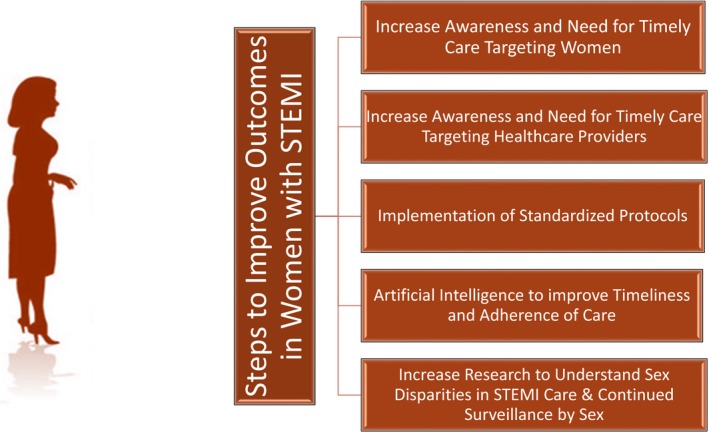
Steps to improve outcomes in women with STEMI. STEMI indicates ST‐segment–elevation myocardial infarction.
CVD remains the number 1 killer of women, but disparities in care contribute to this excess mortality. Recognition of where the gaps remain is the first step towards improving outcomes in STEMI in women. Targeted campaigns to improve the awareness of women for not only their risk of CVD, but also timeliness of care with STEMI are needed. Ongoing educational efforts of healthcare professionals and novel approaches to improving timely care of STEMI in women are needed urgently. We can do better. We must do better. For women, health care needs to be more than bikini medicine.
Disclosures
None.
(J Am Heart Assoc. 2019;8:e012873 DOI: 10.1161/JAHA.119.012873.)
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1. Healy B. The Yentl syndrome. N Engl J Med. 1991;325:274–276. [DOI] [PubMed] [Google Scholar]
- 2. Mosca L, Hammond G, Mochari‐Greenberger H, Towfighi A, Albert MA; American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on High Blood Pressure Research, and Council on Nutrition, Physical Activity and Metabolism . Fifteen‐year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263, e1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd‐Jones DM, Newby LK, Pina IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D'Armiento J, Kris‐Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra‐Strobos N, Urbina EM, Vaccarino V, Wenger NK. Effectiveness‐based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 5. Gulati M. Improving the cardiovascular health of women in the nation: moving beyond the bikini boundaries. Circulation. 2017;135:495–498. [DOI] [PubMed] [Google Scholar]
- 6. Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–2810. [DOI] [PubMed] [Google Scholar]
- 7. Edmund Anstey D, Li S, Thomas L, Wang TY, Wiviott SD. Race and sex differences in management and outcomes of patients after ST‐elevation and non‐ST‐elevation myocardial infarct: results from the NCDR. Clin Cardiol. 2016;39:585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hao Y, Liu J, Liu J, Yang N, Smith SC Jr, Huo Y, Fonarow GC, Ge J, Taubert KA, Morgan L, Zhou M, Xing Y, Ma CS, Han Y, Zhao D. Sex differences in in‐hospital management and outcomes of patients with acute coronary syndrome. Circulation. 2019;139:1776–1785. [DOI] [PubMed] [Google Scholar]
- 9. De Luca L, Marini M, Gonzini L, Boccanelli A, Casella G, Chiarella F, De Servi S, Di Chiara A, Di Pasquale G, Olivari Z, Caretta G, Lenatti L, Gulizia MM, Savonitto S. Contemporary trends and age‐specific sex differences in management and outcome for patients with ST‐segment elevation myocardial infarction. J Am Heart Assoc. 2016;5:e004202 DOI: 10.1161/JAHA.116.004202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alabas OA, Gale CP, Hall M, Rutherford MJ, Szummer K, Lawesson SS, Alfredsson J, Lindahl B, Jernberg T. Sex differences in treatments, relative survival, and excess mortality following acute myocardial infarction: national cohort study using the SWEDEHEART registry. J Am Heart Assoc. 2017;6:e007123 DOI: 10.1161/JAHA.117.007123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jae Lee H, Lansky A, Mehta S, Haimi I, Salwan R, Zambahari R, Chen Y, Hassan F, Parise H, Fasila M, Kontsevaya A, Huay Cheem T, Baumbach A, Granger C, Grines C, Jacobs A, Tresukosol D, Soerianata S, Dy T. Gender disparities in ST‐elevation myocardial infarction care and outcomes in emerging countries: a global lumen organization for women (GLOW) initiative and call to action. J Am Coll Cardiol. 2016;67(13 supplement):2356. [Google Scholar]
- 12. Stehli J, Martin C, Brennan A, Dinh DT, Lefkovits J, Zaman S. Sex differences persist in time to presentation, revascularization and mortality in myocardial infarction treated with percutaneous coronary intervention. J Am Heart Assoc. 2019;8:e012161 DOI: 10.1161/JAHA.119.012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door‐to‐balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roswell RO, Kunkes J, Chen AY, Chiswell K, Iqbal S, Roe MT, Bangalore S. Impact of sex and contact‐to‐device time on clinical outcomes in acute ST‐segment elevation myocardial infarction‐findings from the National Cardiovascular Data Registry. J Am Heart Assoc. 2017;6:e004521 DOI: 10.1161/JAHA.116.004521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. D'Onofrio G, Safdar B, Lichtman JH, Strait KM, Dreyer RP, Geda M, Spertus JA, Krumholz HM. Sex differences in reperfusion in young patients with ST‐segment‐elevation myocardial infarction: results from the VIRGO study. Circulation. 2015;131:1324–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Huded CP, Johnson M, Kravitz K, Menon V, Abdallah M, Gullett TC, Hantz S, Ellis SG, Podolsky SR, Meldon SW, Kralovic DM, Brosovich D, Smith E, Kapadia SR, Khot UN. 4‐Step protocol for disparities in STEMI care and outcomes in women. J Am Coll Cardiol. 2018;71:2122–2132. [DOI] [PubMed] [Google Scholar]
- 17. Andersson PO, Lawesson SS, Karlsson J‐E, Nilsson S, Thylén I; SymTime Study G . Characteristics of patients with acute myocardial infarction contacting primary healthcare before hospitalisation: a cross‐sectional study. BMC Fam Pract. 2018;19:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bairey Merz CN, Andersen H, Sprague E, Burns A, Keida M, Walsh MN, Greenberger P, Campbell S, Pollin I, McCullough C, Brown N, Jenkins M, Redberg R, Johnson P, Robinson B. Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the Women's Heart Alliance. J Am Coll Cardiol. 2017;70:123–132. [DOI] [PubMed] [Google Scholar]
- 19. Miller VM, Rice M, Schiebinger L, Jenkins MR, Werbinski J, Nunez A, Wood S, Viggiano TR, Shuster LT. Embedding concepts of sex and gender health differences into medical curricula. J Womens Health (Larchmt). 2013;22:194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson KW, Torres Soto J, Glicksberg BS, Shameer K, Miotto R, Ali M, Ashley E, Dudley JT. Artificial intelligence in cardiology. J Am Coll Cardiol. 2018;71:2668–2679. [DOI] [PubMed] [Google Scholar]


