Abstract
Background
Mental health conditions are associated with adverse cardiovascular outcomes in patients with ischemic heart disease, and much of this risk can be attributed to poor health behaviors. Although all patients with ischemic heart disease should be referred for cardiac rehabilitation (CR), whether patients with mental health conditions are willing to participate in CR programs is unknown. We sought to compare CR participation rates among patients with ischemic heart disease with versus without comorbid depression and/or posttraumatic stress disorder (PTSD).
Methods and Results
We used national electronic health records to identify all patients hospitalized for acute myocardial infarction or coronary revascularization at Veterans Health Administration hospitals between 2010 and 2014. Multivariable logistic regression models were used to determine whether comorbid depression/PTSD was associated with CR participation during the 12 months after hospital discharge. Of the 86 537 patients hospitalized for ischemic heart disease between 2010 and 2014, 24% experienced PTSD and/or depression. Patients with PTSD and/or depression had higher CR participation rates than those without PTSD or depression (11% versus 8%; P<0.001). In comparison to patients without PTSD or depression, the odds of participation was 24% greater in patients with depression alone (odds ratio, 1.24; 95% CI, 1.15–1.34), 38% greater in patients with PTSD alone (odds ratio, 1.38; 95% CI, 1.24–1.54), and 57% greater in patients with both PTSD and depression (odds ratio, 1.57; 95% CI, 1.43–1.74).
Conclusions
Among patients with ischemic heart disease, the presence of comorbid depression and/or PTSD is associated with greater participation in CR, providing an important opportunity to promote healthy lifestyle behaviors and reduce adverse cardiovascular outcomes among these patients.
Keywords: cardiac rehabilitation, depression, mental health, participation, posttraumatic stress disorder
Subject Categories: Secondary Prevention, Mental Health, Cardiovascular Disease
Clinical Perspective
What Is New?
In the Veterans Health Administration, patients with posttraumatic stress disorder and/or depression are more likely to participate in cardiac rehabilitation after hospitalization for myocardial infarction or coronary revascularization than patients without posttraumatic stress disorder or depression.
What Are the Clinical Implications?
This provides an important opportunity to engage patients with comorbid ischemic heart disease and mental health disorders in collaborative care, aiming to effectively manage both conditions to reduce future cardiovascular risk.
Cardiac rehabilitation (CR), with a focus on exercise‐based training, is a class I recommendation from the American Heart Association and the American College of Cardiology for patients with coronary heart disease.1, 2, 3, 4, 5, 6 It is a cost‐effective means of reducing cardiovascular mortality and improving health‐related quality of life in patients with ischemic heart disease.1, 7, 8, 9 Among patient characteristics that may influence participation and adherence to CR, mental health disorders are of particular interest because they have the potential to both increase the risk of cardiovascular disease and act as a barrier against cardiovascular disease prevention.
The association of cardiovascular disease with mental health disorders is well established.10, 11, 12, 13, 14, 15, 16 Poor health behaviors, such as physical inactivity, smoking, unhealthy diet, and medication nonadherence, have been shown to contribute to an increased risk of cardiovascular disease in this population.16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Because the goal of CR is to reduce cardiovascular events by addressing poor health behaviors, patients with mental health disorders might greatly benefit from this service. However, several prior studies have suggested that mental health disorders, particularly depression, may be a barrier to participation in CR.26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 On the contrary, a recent study conducted on 158 991 Centers of Medicare and Medicaid beneficiaries hospitalized for acute myocardial infarction (MI) in 2008 found that patients with depression were more likely than those without depression to participate in CR after MI.40 Given the large burden of both cardiovascular and mental health disease in the veteran population, this research question is highly relevant to the Veterans Health Administration (VA). Therefore, we sought to determine whether veterans with depression and/or posttraumatic stress disorder (PTSD) were more or less likely than those without depression or PTSD to participate in CR after hospitalization for MI or coronary revascularization.
Methods
The data cannot be made available publicly to researchers for purposes of reproducing the results or replicating the procedure due to protected health information. However, analytic methods used in this article can be made available to other researchers on request.
We used electronic medical record data from the national VA Corporate Data Warehouse for our study. The VA is a national healthcare system with 152 hospitals. All patients who were hospitalized for ischemic heart disease (defined as acute MI, percutaneous coronary intervention [PCI], or coronary artery bypass grafting [CABG]) at any VA facility across the nation between 2010 and 2014 were included in the analysis. The International Classification of Diseases, Ninth Revision (ICD‐9), Current Procedural Terminology, and Healthcare Common Procedure Coding System codes used to identify these patients were as follows:
MI: ICD‐9 code 410.x.
PCI: ICD‐9 codes 00.66, 17.55, and 36.0x; Current Procedural Terminology codes 92973, 92974, 92980 to 92982, 92984, 92995, and 92996; and Healthcare Common Procedure Coding System codes G0290 and G0291.
CABG: ICD‐9 codes 36.10 to 36.16, 36.19, and 36.20; Current Procedural Terminology codes 33510 to 33514, 33516 to 33519, 33521 to 33523, 33530, 33533 to 33536, 33572, 35600, and 93564; and Healthcare Common Procedure Coding System codes S2205 to S2209.
We extracted data on CR participation using stop code 231 and/or Current Procedural Terminology codes 93797, 93798, S9472, S9473, G0422, and G0423. Participation was defined as having ≥2 CR encounters within 1 year of discharge. The reason for requiring 2 (versus 1) sessions was that initial sessions are sometimes devoted to registration and intake interviews, and we wanted to ensure that the definition of participation included at least one session of exercise training and/or health behavior education. Because only 34 VA facilities have on‐site CR programs, and it is common practice to refer patients to non‐VA programs that are paid for by the VA, we evaluated both VA and non‐VA CR. Data on comorbid conditions were extracted from the Corporate Data Warehouse, along with information on patient demographics. Comorbid conditions were defined as 1 inpatient or ≥2 outpatient encounters identified by ICD‐9 codes (Table S1) in the 1 year before index hospitalization. Comorbid PTSD and depression status were defined similarly using the following ICD‐9 codes:
Depression: codes 296.2x, 296.3x, 296.5x, 300.4, 309.x, and 311.xx.
PTSD: code 309.81.
Normality of distribution of age was tested, and difference in mean age between patients with no PTSD/depression, only PTSD, only depression, and both PTSD and depression was assessed using ANOVA. χ2 Tests were used to look at differences in distribution of categorical variables between the 4 groups. We used multivariable logistic regression to predict CR participation, adjusting for demographics, comorbid conditions, and indication for CR. We also calculated adjusted CR participation rates by PTSD/depression status. In addition, we calculated the number of distinct days that patients had an outpatient visit at a VA facility during the 1 year before hospitalization for MI, PCI, or CABG and stratified patients as “low” and “high” healthcare users with the 50th percentile as a cutoff. We conducted a sensitivity analysis to examine the effect of ambulatory care use by calculating and comparing adjusted participation rates between low and high healthcare users. All statistical analyses were performed using SAS Enterprise Guide, version 7.15 HF3 (SAS Institute, Cary, NC), and STATA, version 15.1 (StataCorp, College, TX), statistical packages.
This study was funded by the VA Quality Enhancement Research Initiative and approved by the San Francisco VA and the University of California, San Francisco, Institutional Review Boards. The requirement for informed consent was waived.
Results
Between 2010 and 2014, 86 537 patients were hospitalized for MI, PCI, or CABG at a VA facility (Table 1). The patients were 67 years old on average and predominantly men (98%), white (79%), and non‐Hispanic (91%). Overall, 24% (20 372/86 537) experienced PTSD and/or depression. The indication for CR was PCI in 44%, MI in 35%, and CABG in 21% of patients. Among the 86 537 patients, only 8.7% (n=7568) participated in ≥2 sessions of CR. However, among patients with PTSD and/or depression, the CR participation rate was 10.7%.
Table 1.
Characteristics of Veterans Hospitalized for Ischemic Heart Disease Between 2010 and 2014 by PTSD/Depression Status
| Characteristicsb | All (N=86 537) | No PTSD or Depression (N=66 165) | Depression Only (N=11 424) | PTSD Only (N=4077) | PTSD and Depression (N=4871) |
|---|---|---|---|---|---|
| Age, mean±SD, y | 66.75±9.50 | 67.38±9.64 | 65.00±9.62 | 65.05±7.32 | 63.72±7.34 |
| Sex | |||||
| Women | 1508 (1.7) | 971 (1.5) | 366 (3.2) | 48 (1.2) | 123 (2.5) |
| Men | 85 029 (98.3) | 65 194 (98.5) | 11 058 (96.8) | 4029 (98.8) | 4748 (97.5) |
| Racea | |||||
| White | 68 701 (79.4) | 52 550 (79.4) | 9259 (81.0) | 3138 (77.0) | 3754 (77.1) |
| Black | 10 913 (12.6) | 8200 (12.4) | 1414 (12.4) | 568 (13.9) | 731 (15.0) |
| Other | 1613 (1.9) | 1189 (1.8) | 193 (1.7) | 111 (2.7) | 120 (2.5) |
| Ethnicitya | |||||
| Not Hispanic | 78 933 (91.2) | 60 473 (91.4) | 10 364 (90.7) | 3676 (90.2) | 4420 (90.7) |
| Hispanic/Latino | 4470 (5.2) | 3176 (4.8) | 722 (6.3) | 259 (6.4) | 313 (6.4) |
| Marital statusa | |||||
| Married | 44 001 (50.8) | 33 785 (51.1) | 5027 (44.0) | 2430 (59.6) | 2759 (56.6) |
| Separated/divorced | 27 748 (32.1) | 20 786 (31.4) | 4271 (37.4) | 1167 (28.6) | 1524 (31.3) |
| Widowed | 7847 (9.1) | 6238 (9.4) | 1100 (9.6) | 224 (5.5) | 285 (5.9) |
| Single | 6842 (7.9) | 5273 (8.0) | 1018 (8.9) | 251 (6.2) | 300 (6.2) |
| Region | |||||
| Midwest | 21 038 (24.3) | 16 204 (24.5) | 2909 (25.5) | 816 (20.0) | 1109 (22.8) |
| Southeast | 18 830 (21.8) | 14 168 (21.4) | 2676 (23.4) | 920 (22.6) | 1066 (21.9) |
| North Atlantic | 16 997 (19.6) | 13 232 (20.0) | 2041 (17.9) | 861 (21.1) | 863 (17.7) |
| Continental | 15 574 (18.0) | 11 585 (17.5) | 2256 (19.7) | 740 (18.2) | 993 (20.4) |
| Pacific | 14 098 (16.3) | 10 976 (16.6) | 1542 (13.5) | 740 (18.2) | 840 (17.2) |
| Indication for CR | |||||
| Acute myocardial infarction | 30 287 (35.0) | 22 487 (34.0) | 4752 (41.6) | 1372 (33.7) | 1676 (34.4) |
| Coronary artery bypass grafting | 18 205 (21.0) | 14 903 (22.5) | 1767 (15.5) | 796 (19.5) | 739 (15.2) |
| Percutaneous coronary intervention | 38 045 (44.0) | 28 775 (43.5) | 4905 (42.9) | 1909 (46.8) | 2456 (50.4) |
| Comorbid conditions | |||||
| Hypertension | 69 243 (80.0) | 51 048 (77.2) | 10 250 (89.7) | 3582 (87.9) | 4363 (89.6) |
| Dyslipidemia | 62 911 (72.7) | 45 811 (69.2) | 9600 (84.0) | 3332 (81.7) | 4168 (85.6) |
| Diabetes mellitus | 38 792 (44.8) | 28 022 (42.4) | 6074 (53.2) | 2063 (50.6) | 2633 (54.1) |
| Heart failure | 20 339 (23.5) | 14 700 (22.2) | 3528 (30.9) | 894 (21.9) | 1217 (25.0) |
| Stroke | 6279 (7.3) | 4209 (6.4) | 1284 (11.2) | 299 (7.3) | 487 (10.0) |
| Peripheral vascular disease | 14 962 (17.3) | 10 876 (16.4) | 2414 (21.1) | 731 (17.9) | 941 (19.3) |
| Chronic obstructive pulmonary disease | 18 796 (21.7) | 12 936 (19.6) | 3323 (29.1) | 1060 (26.0) | 1477 (30.3) |
| Chronic kidney disease | 15 752 (18.2) | 11 696 (17.7) | 2511 (22.0) | 646 (15.8) | 899 (18.5) |
| Valvular heart disease | 15 616 (18.0) | 11 624 (17.6) | 2399 (21.0) | 673 (16.5) | 920 (18.9) |
| Arrhythmias | 20 431 (23.6) | 15 407 (23.3) | 3017 (26.4) | 917 (22.5) | 1090 (22.4) |
| Cancer | 11 832 (13.7) | 8892 (13.4) | 1742 (15.2) | 526 (12.9) | 672 (13.8) |
| Dementia | 1693 (2.0) | 1033 (1.6) | 440 (3.9) | 91 (2.2) | 129 (2.6) |
| Anemia | 14 661 (16.9) | 10 356 (15.7) | 2668 (23.4) | 642 (15.7) | 995 (20.4) |
| Alcohol abuse/dependence | 6222 (7.2) | 3133 (4.7) | 1638 (14.3) | 488 (12.0) | 963 (19.8) |
| Tobacco use | 27 112 (31.3) | 18 648 (28.2) | 4777 (41.8) | 1518 (37.2) | 2169 (44.5) |
| Obesity | 13 390 (15.5) | 8913 (13.5) | 2465 (21.6) | 819 (20.1) | 1193 (24.5) |
| CR | |||||
| Yes | 7568 (8.7) | 5397 (8.2) | 1130 (9.9) | 445 (10.9) | 596 (12.2) |
| No | 78 969 (91.3) | 60 768 (91.8) | 10 294 (90.1) | 3632 (89.1) | 4275 (87.8) |
Data are given as number (percentage) of each group, unless otherwise indicated. CR indicates cardiac rehabilitation; PTSD, posttraumatic stress disorder.
Number of patients with missing race, n=5310 (6.1%); missing ethnicity, n=3134 (3.6%); and missing marital status, n=99 (0.1%).
Patient characteristics were compared across the 4 categories of PTSD/depression status using ANOVA for age and χ2 tests for categorical variables. P<0.0001 for all variables.
Among the 20 372 patients with PTSD and/or depression, 11 424 (56%) experienced depression alone, 4077 (20%) experienced PTSD alone, and 4871 (24%) experienced both depression and PTSD (Table 1). The CR participation rate was 8.2% in patients without depression or PTSD, 9.9% in patients with depression alone, 10.9% in patients with PTSD alone, and 12.2% in those with both PTSD and depression.
Upon running logistic regression models to further evaluate the association between depression, PTSD, and CR participation, we found that, compared with patients who had neither depression nor PTSD, those with depression alone had a 24% greater odds (odds ratio [OR], 1.24; 95% CI, 1.16–1.33), those with PTSD alone had a 39% greater odds (OR, 1.39; 95% CI, 1.25–1.54), and those with both depression and PTSD had a 54% greater odds (OR, 1.54; 95% CI, 1.40–1.69) of participating in CR on unadjusted analysis (Table 2). These associations remained statistically significant after adjusting for age, sex, race, ethnicity, marital status, region, indication for CR, and comorbid health conditions (models 1‐4). After adjusting for all covariates, patients with both PTSD and depression had a 57% greater odds (OR, 1.57; 95% CI, 1.43–1.74) of participating in CR than those without depression or PTSD.
Table 2.
Multivariable Logistic Regression Models Evaluating PTSD and Depression as Predictors of CR Participation
| Variable | Odds Ratio (95% CI)* | ||||
|---|---|---|---|---|---|
| Unadjusted | Model 1 | Model 2 | Model 3 | Model 4 | |
| No PTSD or depression | Reference | Reference | Reference | Reference | Reference |
| Depression only | 1.24 (1.16–1.33) | 1.19 (1.11–1.27) | 1.17 (1.09–1.26) | 1.26 (1.17–1.35) | 1.24 (1.15–1.34) |
| PTSD only | 1.39 (1.25–1.54) | 1.34 (1.20–1.49) | 1.36 (1.22–1.51) | 1.43 (1.28–1.59) | 1.38 (1.24–1.54) |
| PTSD and depression | 1.54 (1.40–1.69) | 1.45 (1.32–1.60) | 1.46 (1.33–1.61) | 1.62 (1.47–1.78) | 1.57 (1.43–1.74) |
Model 1: adjusted for age and sex. Model 2: adjusted for age, sex, race, ethnicity, marital status, and region. Model 3: adjusted for age, sex, race, ethnicity, marital status, region, and indication for CR. Model 4: adjusted for age, sex, race, ethnicity, marital status, region, indication for CR, and comorbid conditions. CR indicates cardiac rehabilitation; PTSD, posttraumatic stress disorder.
When calculating multivariable adjusted CR participation rates by PTSD/depression status, we found that among patients without PTSD or depression, only 8.3% participated in ≥2 sessions of CR. In comparison, 10.1% of patients with depression alone, 11% of patients with PTSD alone, and 12.3% of patients with both PTSD and depression participated in CR. Overall CR participation rates increased steadily from 2010 to 2014. However, the association of PTSD/depression with higher participation stayed the same (Figure). Patients with both PTSD and depression had the highest adjusted rates of CR participation across all years, approaching 14.5% in 2014.
Figure 1.
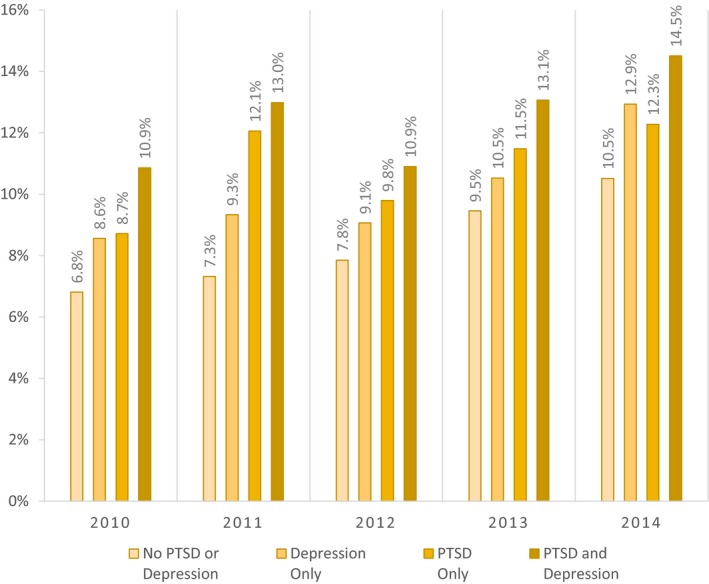
Adjusted cardiac rehabilitation participation rates by posttraumatic stress disorder (PTSD)/depression status and year.
The median number of days during which patients had an outpatient visit at a VA facility during the 1 year before hospitalization was 27. Using this median cut point, 52% (45 255/86 537) were categorized as low ambulatory healthcare users, with ≤27 outpatient visit days, and 48% were classified as high users. Among high users, patients with PTSD and/or depression continued to experience higher odds of CR participation in comparison to patients without PTSD or depression (Table 3). Among low users, patients with PTSD alone or PTSD and depression were more likely to participate in CR, but those with depression did not have significantly different odds of participation in comparison to those without PTSD or depression (OR, 1.12; 95% CI, 0.99–1.26).
Table 3.
Multivariable Regression Analysisb and Adjusted CR Participation Rates, Stratified by Level of Ambulatory Healthcare Use
| Variable | Odds Ratio (95% CI)a | Adjusted Participation Rate, % | ||
|---|---|---|---|---|
| Low Users | High Users | Low Users | High Users | |
| No PTSD or depression | Reference | Reference | 8.8 | 7.8 |
| Depression only | 1.12 (0.99–1.26) | 1.37 (1.24–1.51) | 9.7 | 10.2 |
| PTSD only | 1.27 (1.06–1.52) | 1.49 (1.30–1.71) | 10.8 | 10.9 |
| PTSD and depression | 1.43 (1.16–1.75) | 1.66 (1.48–1.87) | 12.0 | 12.2 |
CR indicates cardiac rehabilitation; PTSD, posttraumatic stress disorder.
Low and high ambulatory healthcare users: defined using a cutoff of the 50th percentile of the distribution of distinct number of days that patients had an outpatient clinic visit at a Veterans Health Administration facility in the 1 year before hospitalization for myocardial infarction, percutaneous coronary intervention, or coronary artery bypass grafting. The 50th percentile for this population was 27 visit days.
Logistic regression models included age, sex, race, ethnicity, marital status, region, indication for CR, and comorbid conditions as covariates.
Discussion
CR is currently a class I recommendation for secondary prevention in patients with coronary heart disease.1, 2, 3, 4, 5, 6 Our study found that depression and PTSD were highly predictive of participation in CR among veterans hospitalized for MI, PCI, or CABG. Although overall CR participation rates have increased over time, the difference in rates by PTSD/depression status has been consistent. This provides an important opportunity to engage these patients not only in treatment for their mental health condition but to promote healthy lifestyle changes that will reduce risk of cardiovascular events.
Our results differ from several prior studies that have reported lower participation in CR among patients with mental health disorders.26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 However, many of these studies had small sample sizes and examined populations that were referred to CR (rather than eligible for CR). If eligible patients with mental health disorders were more likely to agree to referral, examining the referred patients could have missed any effect of mental health disorders on participation. In addition, most prior studies have evaluated patients referred to a single CR program, whereas we examined national CR participation rates across multiple programs. More importantly, our findings are consistent with those of one prior study that examined national participation rates. Among 158 991 Centers of Medicare and Medicaid beneficiaries hospitalized for MI in 2008, this study found that patients with depression were more likely than those without depression to participate in CR after MI.40 These findings suggest that, among all patients eligible for CR, those with mental health conditions are more likely to participate. Compared with this Medicare population, the VA population in our study had a far lower percentage of women and a much higher prevalence of depression. However, the results point to important evidence that, across different patient populations and healthcare systems, mental health disorders may not be barriers to CR participation.
We were not able to determine why patients with mental disorders were more likely to participate in CR. It seems less likely that patients with mental health disorders, particularly those with severe PTSD or depressive symptoms, might agree to CR referral; yet, paradoxically, we found that they were more likely to seek help. One possible explanation is that a greater connection to health care among patients with mental health disorders might offer more opportunities to enroll, as evidenced by our findings after stratification by healthcare use. Another possibility is that providers might be more likely to refer patients who have poor health behaviors, and the presence of mental health conditions is associated with poor health behaviors. A third possibility is that the presence of a mental health disorder could increase a patient's interest in the social support aspects of CR. Although there is need to study this association qualitatively, the results compel the exploration of mental health care as an opportunity for primordial and primary prevention of cardiovascular diseases, more colloquially called prehabilitation.
Conversely, greater participation in CR also provides a unique opportunity to help patients obtain treatment for mental health disorders and improve their health behaviors. CR offers the opportunity to improve mental health care by use of the collaborative care model.41 Prior studies have shown that CR is associated with a reduction in depressive symptoms among patients with depression.42, 43, 44 Whether treatment of depression is associated with a reduction in cardiovascular events is still debatable, and there is limited evidence from some clinical trials suggesting longer survival rates among patients treated for depression who had a significant improvement in depressive symptoms in comparison to those who had no significant change in depressive symptoms.45, 46 However, CR for patients with mental health disorders offers opportunities to explore new models of multidisciplinary care aimed at improving the poor health behaviors associated with mental health disorders with the aim of improving cardiovascular health.
Our study does have several limitations. First, we relied on data from electronic health records and were unable to validate concurrent depression and PTSD through chart review. Second, we were unable to determine the severity of depression and PTSD or account for medication use. Third, our population consisted predominantly of older men, limiting the generalizability of our results. Finally, although some VA facilities offer patients a choice between home‐ and facility‐based CR programs, the same stop code is used for both types of CR. Therefore, there was no way for us to evaluate whether the association of mental health conditions with participation differed for home‐ versus facility‐based CR programs.
Conclusions
Among veterans hospitalized for MI, PCI, or CABG, those with depression and/or PTSD were significantly more likely to participate in CR than those without depression and/or PTSD. These findings suggest that mental health conditions may not be a barrier to CR and that CR may, in fact, provide an opportunity for greater mental health care and support.
Sources of Funding
The study was funded by the Veterans Health Administration Quality Enhancement Research Initiative.
Disclosures
None.
Supporting information
Table S1. List of ICD‐9 Codes Used to Define Comorbid Conditions in Veterans Hospitalized With Ischemic Heart Disease Between 2010–2014
(J Am Heart Assoc. 2019;8:e011639 DOI: 10.1161/JAHA.118.011639.)
This study was presented in abstract form at the American Heart Association's Epidemiology and Prevention, Lifestyle and Metabolic Health Scientific Sessions, March 20 to 23, 2018, in New Orleans, LA.
References
- 1. Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise‐based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta‐analysis. J Am Coll Cardiol. 2016;67:1–12. [DOI] [PubMed] [Google Scholar]
- 2. Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW; American Heart Association Science Advisory and Coordinating Committee . Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. [DOI] [PubMed] [Google Scholar]
- 3. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd‐Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA; World Heart Federation and the Preventive Cardiovascular Nurses Association . AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. [DOI] [PubMed] [Google Scholar]
- 4. Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, Pack Q, Sanderson BK, Wang TY. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11:e000037. [DOI] [PubMed] [Google Scholar]
- 5. Wenger NK, Froelicher ES, Smith LK, Ades PA, Berra K, Blumenthal JA, Certo CM, Dattilo AM, Davis D, DeBusk RF. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995(17):1–23. [PubMed] [Google Scholar]
- 6. Simon M, Korn K, Cho L, Blackburn GG, Raymond C. Cardiac rehabilitation: a class 1 recommendation. Cleve Clin J Med. 2018;85:551–558. [DOI] [PubMed] [Google Scholar]
- 7. Wong WP, Feng J, Pwee KH, Lim J. A systematic review of economic evaluations of cardiac rehabilitation. BMC Health Serv Res. 2012;12:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frederix I, Vandijck D, Hens N, De Sutter J, Dendale P. Economic and social impact of increased cardiac rehabilitation uptake and cardiac telerehabilitation in Belgium—a cost‐benefit analysis. Acta Cardiol. 2018;73:222–229. [DOI] [PubMed] [Google Scholar]
- 9. De Gruyter E, Ford G, Stavreski B. Economic and social impact of increasing uptake of cardiac rehabilitation services: a cost benefit analysis. Heart Lung Circ. 2016;25:175–183. [DOI] [PubMed] [Google Scholar]
- 10. Boscarino JA. PTSD is a risk factor for cardiovascular disease: time for increased screening and clinical intervention. Prev Med. 2012;54:363–364; author reply 365. [DOI] [PubMed] [Google Scholar]
- 11. Case SM, Sawhney M, Stewart JC. Atypical depression and double depression predict new‐onset cardiovascular disease in U.S. adults. Depress Anxiety. 2018;35:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BH. Meta‐analysis of anxiety as a risk factor for cardiovascular disease. Am J Cardiol. 2016;118:511–519. [DOI] [PubMed] [Google Scholar]
- 13. Rosenbaum S, Stubbs B, Ward PB, Steel Z, Lederman O, Vancampfort D. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta‐analysis. Metabolism. 2015;64:926–933. [DOI] [PubMed] [Google Scholar]
- 14. Sumner JA, Kubzansky LD, Elkind MS, Roberts AL, Agnew‐Blais J, Chen Q, Cerda M, Rexrode KM, Rich‐Edwards JW, Spiegelman D, Suglia SF, Rimm EB, Koenen KC. Trauma exposure and posttraumatic stress disorder symptoms predict onset of cardiovascular events in women. Circulation. 2015;132:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22:613–626. [DOI] [PubMed] [Google Scholar]
- 16. Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Blumenthal JA. Targeting lifestyle change in patients with depression. J Am Coll Cardiol. 2013;61:631–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blumenthal JA, Babyak MA, Carney RM, Huber M, Saab PG, Burg MM, Sheps D, Powell L, Taylor CB, Kaufmann PG. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Med Sci Sports Exerc. 2004;36:746–755. [DOI] [PubMed] [Google Scholar]
- 19. Brummett BH, Babyak MA, Siegler IC, Mark DB, Williams RB, Barefoot JC. Effect of smoking and sedentary behavior on the association between depressive symptoms and mortality from coronary heart disease. Am J Cardiol. 2003;92:529–532. [DOI] [PubMed] [Google Scholar]
- 20. Elderon L, Whooley MA. Depression and cardiovascular disease. Prog Cardiovasc Dis. 2013;55:511–523. [DOI] [PubMed] [Google Scholar]
- 21. Hamer M. Psychosocial stress and cardiovascular disease risk: the role of physical activity. Psychosom Med. 2012;74:896–903. [DOI] [PubMed] [Google Scholar]
- 22. Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–2162. [DOI] [PubMed] [Google Scholar]
- 23. Hamer M, Stamatakis E, Steptoe A. Psychiatric hospital admissions, behavioral risk factors, and all‐cause mortality: the Scottish Health Survey. Arch Intern Med. 2008;168:2474–2479. [DOI] [PubMed] [Google Scholar]
- 24. Win S, Parakh K, Eze‐Nliam CM, Gottdiener JS, Kop WJ, Ziegelstein RC. Depressive symptoms, physical inactivity and risk of cardiovascular mortality in older adults: the Cardiovascular Health Study. Heart. 2011;97:500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ye S, Muntner P, Shimbo D, Judd SE, Richman J, Davidson KW, Safford MM. Behavioral mechanisms, elevated depressive symptoms, and the risk for myocardial infarction or death in individuals with coronary heart disease: the REGARDS (Reason for Geographic and Racial Differences in Stroke) study. J Am Coll Cardiol. 2013;61:622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–1035. [PubMed] [Google Scholar]
- 27. Casey E, Hughes JW, Waechter D, Josephson R, Rosneck J. Depression predicts failure to complete phase‐II cardiac rehabilitation. J Behav Med. 2008;31:421–431. [DOI] [PubMed] [Google Scholar]
- 28. Caulin‐Glaser T, Maciejewski PK, Snow R, LaLonde M, Mazure C. Depressive symptoms and sex affect completion rates and clinical outcomes in cardiac rehabilitation. Prev Cardiol. 2007;10:15–21. [DOI] [PubMed] [Google Scholar]
- 29. Glazer KM, Emery CF, Frid DJ, Banyasz RE. Psychological predictors of adherence and outcomes among patients in cardiac rehabilitation. J Cardiopulm Rehabil. 2002;22:40–46. [DOI] [PubMed] [Google Scholar]
- 30. Kronish IM, Rieckmann N, Halm EA, Shimbo D, Vorchheimer D, Haas DC, Davidson KW. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med. 2006;21:1178–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Predictors of attendance at cardiac rehabilitation after myocardial infarction. J Psychosom Res. 2001;51:497–501. [DOI] [PubMed] [Google Scholar]
- 32. McGrady A, McGinnis R, Badenhop D, Bentle M, Rajput M. Effects of depression and anxiety on adherence to cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2009;29:358–364. [DOI] [PubMed] [Google Scholar]
- 33. Resurreccion DM, Moreno‐Peral P, Gomez‐Herranz M, Rubio‐Valera M, Pastor L, Caldas de Almeida JM, Motrico E. Factors associated with non‐participation in and dropout from cardiac rehabilitation programmes: a systematic review of prospective cohort studies. Eur J Cardiovasc Nurs. 2019;18:38–47. [DOI] [PubMed] [Google Scholar]
- 34. Ruano‐Ravina A, Pena‐Gil C, Abu‐Assi E, Raposeiras S, van ‘t Hof A, Meindersma E, Bossano Prescott EI, Gonzalez‐Juanatey JR. Participation and adherence to cardiac rehabilitation programs: a systematic review. Int J Cardiol. 2016;223:436–443. [DOI] [PubMed] [Google Scholar]
- 35. Swardfager W, Herrmann N, Marzolini S, Saleem M, Farber SB, Kiss A, Oh PI, Lanctot KL. Major depressive disorder predicts completion, adherence, and outcomes in cardiac rehabilitation: a prospective cohort study of 195 patients with coronary artery disease. J Clin Psychiatry. 2011;72:1181–1188. [DOI] [PubMed] [Google Scholar]
- 36. Turk‐Adawi KI, Oldridge NB, Tarima SS, Stason WB, Shepard DS. Cardiac rehabilitation enrollment among referred patients: patient and organizational factors. J Cardiopulm Rehabil Prev. 2014;34:114–122. [DOI] [PubMed] [Google Scholar]
- 37. Turner SC, Bethell HJ, Evans JA, Goddard JR, Mullee MA. Patient characteristics and outcomes of cardiac rehabilitation. J Cardiopulm Rehabil. 2002;22:253–260. [DOI] [PubMed] [Google Scholar]
- 38. Yohannes AM, Yalfani A, Doherty P, Bundy C. Predictors of drop‐out from an outpatient cardiac rehabilitation programme. Clin Rehabil. 2007;21:222–229. [DOI] [PubMed] [Google Scholar]
- 39. Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–1823. [DOI] [PubMed] [Google Scholar]
- 40. Zullo MD, Gathright EC, Dolansky MA, Josephson RA, Cheruvu VK, Hughes JW. Influence of depression on utilization of cardiac rehabilitation postmyocardial infarction: a study of 158 991 Medicare beneficiaries. J Cardiopulm Rehabil Prev. 2017;37:22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, Peterson D, Rutter CM, McGregor M, McCulloch D. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brosse AL, Sheets ES, Lett HS, Blumenthal JA. Exercise and the treatment of clinical depression in adults: recent findings and future directions. Sports Med. 2002;32:741–760. [DOI] [PubMed] [Google Scholar]
- 43. Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure‐Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES; American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, American Heart Association Council on Clinical Cardiology, American Heart Association Council on Epidemiology and Prevention, American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research, American Psychiatric Association . Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. [DOI] [PubMed] [Google Scholar]
- 44. Milani RV, Lavie CJ. Impact of cardiac rehabilitation on depression and its associated mortality. Am J Med. 2007;120:799–806. [DOI] [PubMed] [Google Scholar]
- 45. Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, Cornell C, Saab PG, Kaufmann PG, Czajkowski SM, Jaffe AS; ENRICHD Investigators . Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466–474. [DOI] [PubMed] [Google Scholar]
- 46. Glassman AH, Bigger JT Jr, Gaffney M. Psychiatric characteristics associated with long‐term mortality among 361 patients having an acute coronary syndrome and major depression: seven‐year follow‐up of SADHART participants. Arch Gen Psychiatry. 2009;66:1022–1029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. List of ICD‐9 Codes Used to Define Comorbid Conditions in Veterans Hospitalized With Ischemic Heart Disease Between 2010–2014


