Keywords: nerve regeneration, eosinopenia, eosinophil, ischemia, stroke, infarct volume, infection, clinical outcome, neutrophilia, risk factors, predictive factor, neural regeneration
Abstract
Previous data have revealed an association between eosinopenia and mortality of acute ischemic stroke. However, the relationship of eosinopenia with infarct volume, infection rate, and poor outcome of acute ischemic stroke is still unknown. The retrospective study included 421 patients (273 males, 65%; mean age, 68.0 ± 13.0 years) with first acute ischemic stroke who were hospitalized in the Second Affiliated Hospital of Soochow University, China, from January 2017 to February 2018. Laboratory data, neuroimaging results, and modified Rankin Scale scores were collected. Patients were divided into four groups according to their eosinophil percentage level (< 0.4%, 0.4–1.1%, 1.1–2.3%, ≥ 2.3%). Spearman’s correlation analysis showed that the percentage of eosinophils was negatively correlated with infarct volume (rs = −0.514, P < 0.001). Receiver operating characteristic analysis demonstrated that eosinopenia predicted a large infarct volume more accurately than neutrophilia; the area under curve was 0.906 and 0.876, respectively; a large infarct was considered as that with a diameter larger than 3 cm and involving more than two major arterial blood supply areas. Logistic regression analysis revealed that eosinophil percentage was an independent risk factor for acute ischemic stroke (P = 0.002). Moreover, eosinophil percentage was significantly associated with large infarct volume, high infection rate (pulmonary and urinary tract infections), and poor outcome (modified Rankin Scale score > 3) after adjusting for potential confounding factors (P-trend < 0.001). These findings suggest that eosinopenia has the potential to predict the severity of acute ischemic stroke. This study was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University, China (approval number: K10) on November 10, 2015.
Chinese Library Classification No. R446; R741
Introduction
Many studies have demonstrated an association of a poor stroke prognosis with neutrophilia (Wang et al., 2016), monocytosis, lymphopenia (Zierath et al., 2018), an increased neutrophil lymphocyte ratio (Tokgoz et al., 2013; Wang et al., 2016; Zhao et al., 2016; Qun et al., 2017), and C-reactive protein level (Wassertheil-Smoller et al., 2014; Lind et al., 2015). However, only a few studies have studied the severity of stroke in relation to eosinophils, which lead to endothelial dysfunction, thrombosis, and worsen inflammation (Ten et al., 1989; Slungaard et al., 1993; Wang et al., 2006; Moosbauer et al., 2007; Marzano et al., 2009; Kecoglu et al., 2014). Some researchers have reported that higher eosinophil levels are associated with stent thrombosis and stent restenosis (Niccoli et al., 2009). Reduced eosinophil count (< 40 cells/mm3) was initially found in patients with febrile diseases, cachectic, and the moribund state (Kirkeby, 1956; Abidi et al., 2011), and more recently found in those with acute coronary syndrome (Jiang et al., 2015) and heart failure (Shah et al., 2016). Recent studies have shown that eosinopenia is strongly associated with mortality and high infection rate in patients with stroke (Hori et al., 2016; Bolayir et al., 2017; Wang et al., 2017; Fan et al., 2018). Therefore, we investigated the association between eosinopenia and acute ischemic stroke (AIS), as well as the ability for eosinopenia to predict AIS severity.
Participants and Methods
Participants
A total of 421 patients with acute ischemic stroke (AIS) admitted to the Second Affiliated Hospital of Soochow University, China, from January 2017 to February 2018 after symptom onset were enrolled in this retrospective analysis. A control group of 104 age- and sex-matched healthy individuals were recruited from the medical examination center of our hospital.
The inclusion criterion was a first onset of AIS within 72 hours. According to World Health Organization-defined criteria, the diagnosis of ischemic stroke was based on patient history, clinical data, computed tomography (CT) and/or magnetic resonance imaging (MRI) (Sacco et al., 2013).
Patients with infection, asthma, eosinophilic esophagitis, and/or hypereosinophilic syndrome were excluded from this study.
This study was approved by Ethics Committee of the Second Affiliated Hospital of Soochow University (approval number: K10, Additional file 1 (41KB, pdf) ) on November 10, 2015. Patients or their family members provided written informed consent.
Laboratory measurements and CT/MRI scan
Blood samples were collected from patients the day after admission and analyzed using XN-10 (Syemex, Kobe, Japan), which was calibrated daily. Laboratory variables, including neutrophil and eosinophil counts, eosinophil percentage, C-reactive protein, fasting plasma glucose, low density lipoprotein-cholesterol, and homocysteine, were assayed at local laboratories. Eosinopenia was defined as an eosinophil percentage less than 0.4% (Krause and Boggs, 1987).
CT and MRI images were acquired by a multislice CT-scanner (Hispeed NX, GE, USA) and a 1.5 or 3.0 Tesla Philips Ingenia scanner, respectively. All patients received repeated CT or MRI within 24 to 96 hours after admission (n = 72 for CT, n = 349 for MRI). CT or diffusion-weighted MR imaging volume was measured using the ABC/2 formula (ellipsoid). Large infarct volume was defined as a large hemisphere infarction with a diameter more than 3 cm and that involved the blood supply area of two large, main arteries (Adams et al., 1993). Infection was defined as fever with clinical manifestations (such as urinary tract symptoms, productive cough, and pleuritic pain), laboratory inspection (such as leukopenia [4/L] or leukocytosis [12/L]), and imageological examination (such as chest CT penetration).
At 90 days after stroke onset, patient disability was evaluated using the modified Rankin Scale (Harrison et al., 2013; Pan et al., 2017; Zhou et al., 2019). Disability is rated on a scale from 0 to 6, as follows: 0: no symptoms; 1: no significant disability, able to carry out all usual activities despite the presence of some symptoms; 2: slight disability, able to look after own affairs without assistance, but unable to carry out all previous activities; 3: moderate disability, requires some help, but able to walk unassisted; 4: moderately severe disability, unable to attend to own bodily needs without assistance and unable to walk unassisted; 5: severe disability, requires constant nursing care and attention, bedridden, incontinent; 6: dead. A poor outcome was defined as a modified Rankin Scale score > 3.
Outcomes
The severity of AIS was determined by infarct volume, infection, and poor outcome.
Statistical analysis
SPSS statistical package 21.0 software (IBM, Armonk, NY, USA) was used for statistical analysis. Eosinophil percentage at admission was collapsed into quartiles. Normal distribution variables are presented as the mean ± SD and were compared using Student’s t tests. Non-normally distributed variables are presented as the interquartile range and were compared using Mann-Whitney U test or the Kruskal-Wallis rank sum test. Pearson’s chi-square test was used to compare the differences in categorical variables, including gender, hypertension, diabetes mellitus, coronary artery disease, current smoking, atrial fibrillation, thrombolytic therapy, infection, 30-day mortality, and stroke subtype. Spearman’s correlation test was used to explore correlations between variables. To predict the large infarct volume, the eosinophil percentage’s cut-off values were evaluated using receiver operating characteristic analyses. Youden’s index was used to test the eosinophil cut-off value. Backward stepwise logistic regression was applied to analyze predictor variables for large infarct volume, infection, and poor outcome. A value of P < 0.05 was considered statistically significant.
Results
Baseline characteristics of patients
Table 1 shows the baseline characteristics of participants. There were 273 men (65%) and 148 women (35%) and the average age was 68.0 ± 13.0 years old. Compared with the control group, patients with AIS had lower eosinophil counts in peripheral blood. Blood samples were collected at a mean ± SD of 39.1 ± 33.5 hours after AIS onset. The average counts of total peripheral eosinophil and neutrophil were 0.1 ± 0.1 × 109 and 5.4 ± 2.7 × 109 cells/L, respectively. A flow chart of the study procedure is shown in Figure 1.
Table 1.
Features of enrolled patients on admission
| Controls (n = 104) | Stroke patients (n = 421) | P-value | |
|---|---|---|---|
| Median age (years) | 69±10 | 68±13 | 0.065 |
| Male sex | 47(47) | 273(65) | 0.001* |
| Hypertension | 73(70) | 305(72) | 0.782 |
| Diabetes | 28(27) | 108(26) | 0.889 |
| Coronary artery disease | 8(8) | 16(4) | 0.15 |
| Atrial fibrillation | 3(3) | 88(21) | < 0.001* |
| Current smoking | 15(14) | 130(31) | 0.001* |
| Systolic blood pressure (mmHg) | 134±22 | 152±22 | < 0.001* |
| Fasting plasma glucose (mM) | 5.20(4.79–5.95) | 5.66(5.01–6.99) | < 0.001* |
| Neutrophils (× 109/L) | 3.40(2.73–4.40) | 4.50(3.50–6.70) | < 0.001* |
| Eosinophils (× 109/L) | 0.11(0.08–0.17) | 0.07(0.03–0.15) | < 0.001* |
| Eosinophil percentage (%) | 1.80(1.30–2.88) | 1.20(0.40–2.35) | < 0.001* |
| LDL-c (mM) | 2.43(1.83–3.15) | 2.89(2.25–3.50) | < 0.001* |
| Homocysteine (mM) | 11.65(9.28–14.30) | 13.20(10.90–17.45) | < 0.001* |
| C-reactive protein (mg/L) | 5.30(5.20–5.50) | 5.40(5.01–6.99) | 0.001* |
Data are expressed as the mean ± SD, median (interquartile range) or n(%). *Indicates significance, chi-square test, Mann-Whitney U test, or Student’s t test. LDL-c: Low density lipoprotein-cholesterol.
Figure 1.
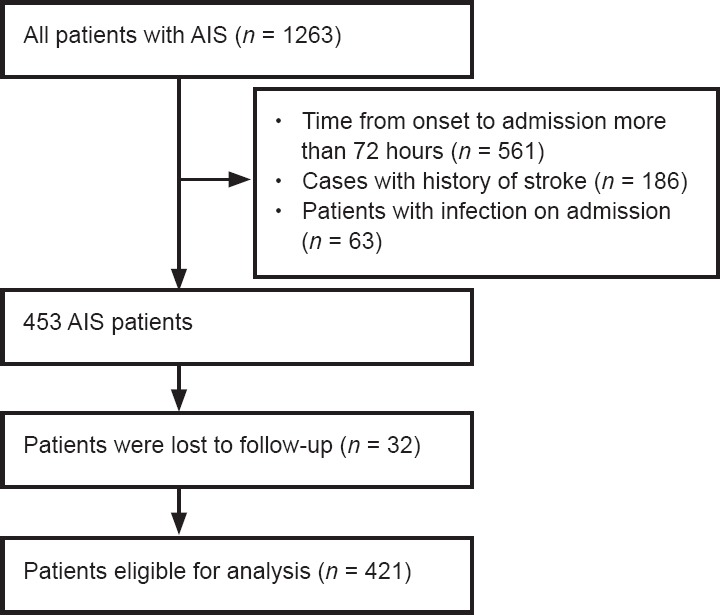
Flow chart of the study procedure.
AIS: Acute ischemic stroke.
Eosinopenia percentage is an independent risk factor for AIS
Compared with control group, the AIS group had higher levels of systolic blood pressure, fasting plasma glucose, homocysteine, C-reactive protein, low density lipoprotein-cholesterol, and neutrophil counts, and had a lower eosinophil count and eosinophil percentage (all P < 0.05). Meanwhile, the AIS group had higher rate of smoking and history of atrial fibrillation compared with the control group (both P < 0.05; Table 1). Furthermore, the binary logistic regression analysis revealed that, compared with the control group, the AIS group had significantly increased odds of having a current smoking status (OR = 3.504, 95% CI: 1.301–7.167, P = 0.010), atrial fibrillation (OR = 8.456, 95% CI: 2.327–30.726, P = 0.001), higher neutrophil levels (OR = 1.311, 95% CI: 1.082–1.580, P = 0.006), low-density lipoprotein cholesterol levels (OR = 1.982, 95% CI: 1.428–2.749, P < 0.001), and homocysteine levels (OR = 1.058, 95% CI: 1.002–1.118, P = 0.044), and lower levels of eosinophil percentage (OR = 0.711, 95% CI: 0.572–0.884, P = 0.002; Table 2).
Table 2.
Variables related to acute ischemic stroke analyzed by binary logistic regression
| Category | OR | 95% CI | P-value |
|---|---|---|---|
| Current smoking | 3.504 | 1.301–7.167 | 0.01 |
| Atrial fibrillation | 8.456 | 2.327–30.726 | 0.001 |
| Neutrophils | 1.311 | 1.082–1.580 | 0.006 |
| Eosinophil percentage | 0.711 | 0.572–0.884 | 0.002 |
| LDL-c | 1.982 | 1.428–2.749 | < 0.001 |
| Homocysteine | 1.058 | 1.002–1.118 | 0.044 |
Model adjusted for sex, age, hypertension, diabetes mellitus, coronary artery disease, current smoking, atrial fibrillation, fasting plasma glucose, neutrophil count, LDL-c, homocysteine, and eosinophil percentage (backward stepwise (wald)). OR: Odds ratio; CI: confidence interval; LDL-c: low density lipoprotein-cholesterol.
Association between eosinopenia and infarct volume
Demographic and clinical features of the four groups of patients based on blood eosinophil percentage quartiles are shown in Table 3. There were no significant differences in admission blood pressure, fasting plasma glucose, or the premorbid risk factor profile expect atrial fibrillation across eosinophil percentage quartiles. Bivariate regression analysis revealed that patients with the lowest eosinophil percentage quartile (< 0.4%) had significantly larger lesion volumes than patients with the other three higher quartiles (P-trend < 0.001) (Figure 2 and Table 4). However, no significant differences were observed between the other three groups with higher quartiles. Spearman’s correlation analysis showed that infarct volume was negatively correlated with eosinophil percentage (rs = −0.514, P < 0.001). Finally, receiver operating characteristic curves were used to investigate the diagnostic value of eosinophils in predicting large infarct volume. An eosinophil percentage of 0.35% independently predicted a large infarct volume in AIS patients, with a sensitivity of 82.7% and a specificity of 89.1% (area under curve = 0.906; 95% CI: 0.870–0.943). Furthermore, by comparing the area under curve, we found that eosinopenia identified large infarct volume more accurately than neutrophilia (Figure 3 and Table 5).
Table 3.
Demographic and clinical features of the four patient groups based on blood eosinophil percentage quartiles
| Characteristic | Blood eosinophils percentage quartiles | P-value | |||
|---|---|---|---|---|---|
| 1st, < 0.4% (n = 104) |
2nd, 0.4–1.1% (n = 105) |
3rd, 1.1–2.3% (n = 107) |
4th, ≥ 2.3% (n = 105) |
||
| Demographics | |||||
| Median age (years) | 69±15 | 65±12 | 66±14 | 67±12 | 0.296 |
| Male sex | 6(59) | 68(65) | 69(65) | 75(71) | 0.29 |
| History | |||||
| Hypertension | 75(72) | 77(73) | 79(74) | 75(71) | 0.784 |
| Diabetes | 18(17) | 29(28) | 32(30) | 29(28) | 0.155 |
| Coronary artery disease | 9(9) | 1(1) | 3(3) | 3(3) | 0.023 |
| Atrial fibrillation | 44(42) | 19(18) | 11(10) | 14(13) | < 0.001* |
| Current smoking | 23(22) | 27(26) | 36(34) | 44(42) | 0.01 |
| Admission | |||||
| Systolic blood pressure (mmHg) | 150±24 | 150±20 | 156±22 | 152±21 | 0.819 |
| Diastolic blood pressure (mmHg) | 86±15 | 85±13 | 84±15 | 84±14 | 0.639 |
| Fasting plasma glucose (mM) | 6.01(5.06–7.09) | 5.44(4.76–6.58) | 5.60(4.94–7.33) | 5.34(4.95–6.61) | 0.049 |
| Admission NIHSS | 15(6–18) | 4(2–7) | 3(2–5) | 3(2–4) | < 0.001* |
| Discharge NIHSS | 12(4–17) | 3(1–6) | 2(1–5) | 2(1–3) | < 0.001* |
| Infarct volume (cm3) | 28.95(4.20–87.5) | 0.90(0.25–4.75) | 0.50(0.23–1.40) | 0.45(0.18–1.23) | < 0.001* |
| Thrombolytic therapy | 27(26) | 19(18) | 13(12) | 7(7) | 0.001* |
| Infection | 47(45) | 9(9) | 5(5) | 3(3) | < 0.001* |
| 30-day mortality | 23(30) | 2(2) | 0 | 0 | < 0.001* |
| Modified Rankin Scale Stroke subtype | 3(0–5) | 1(0–2) | 1(0–1) | 0(0–1) | < 0.001* |
| Large vessel atherosclerosis | 34(44) | 36(47) | 39(52) | 30(42) | 0.62 |
| Cardioembolic | 29(38) | 14(18) | 6(8) | 9(12) | < 0.001* |
| Small vessel disease | 9(12) | 23(30) | 26(35) | 32(44) | < 0.001* |
| Other | 3(4) | 0 | 1(1) | 0 | 0.119 |
| Unknown | 2(2) | 3(4) | 3(4) | 1(1) | 0.940 |
Data are expressed as the mean ± SD, median (interquartile range), or n(%). The stroke subtypes included dissecting aneurysm, vascular malformations, hypercoagulable states, hematologic disorders, fibromuscular dystrophy, and vasculitis. *Indicates significance, chi-square test, Kruskal-Wallis rank sum test. NIHSS: National Institutes of Health Scale Score.
Figure 2.
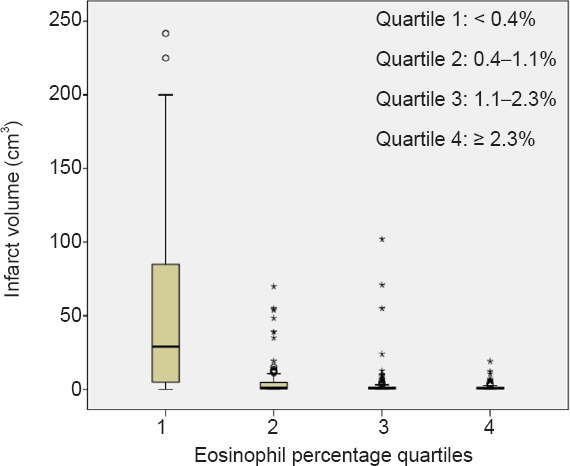
Infarct volume distribution in patients with AIS according to eosinophil percentage quartiles.
Box plot showing the median volumes (solid bar), minimum/maximum values (whiskers), and interquartile range (bar width) across eosinophil quartiles.
Table 4.
Eosinopenia predicts large infarct volume
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P-trend | OR (95% CI) | P-trend | |
| Eosinophil (%) | < 0.001 | < 0.001 | ||
| ≥ 2.3 | 1.00(Ref.) | 1.00(Ref.) | ||
| 2.3–1.1 | 4.039 (0.444–36.750) | 2.416 (0.543–10.749) | ||
| 1.1–0.4 | 9.750 (1.213–78.391) | 4.988 (1.227–20.274) | ||
| < 0.4 | 88.324 (25.237–605.333) | 50.791 (12.751–426.635) | ||
Model adjusted for sex, age, hypertension, diabetes mellitus, coronary artery disease, current smoking, fasting plasma glucose, neutrophil count, stroke subtype, and thrombolytic therapy [multivariate logistic regression, backward stepwise (wald)]. Large infarct volume was defined as a large hemisphere infarction: the diameter of infarct was more than 3 cm and involved more than two large arteries in the main supply area. OR: Odds ratio; CI: confidence interval; Ref.: referent quartile.
Figure 3.
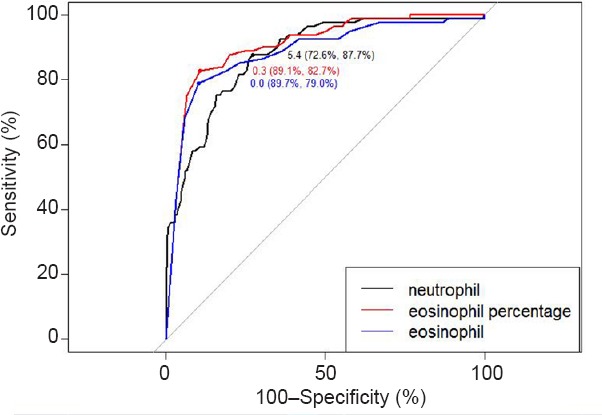
Different types of white blood cells in predicting large infarct volume.
Receiver-operating characteristic analysis for neutrophil, eosinophil, and eosinophil percentage in predicting large infarct volume.
Table 5.
Area under curve, sensitivity, and specificity of the different predictors
| Variable | Area under curve | Sensitivity | Specificity | Cut-off value | |
|---|---|---|---|---|---|
| 95% CI | P-value | ||||
| Eosinophil (%) | 0.906 (0.870–0.943) | < 0.001 | 0.827 | 0.891 | 0.35 |
| Eosinophil (× 109/L) | 0.884 (0.838–0.929) | < 0.001 | 0.79 | 0.897 | 0.025 |
| Neutrophil (× 109/L) | 0.876 (0.835–0.917) | < 0.001 | 0.877 | 0.726 | 5.45 |
CI: Confidence interval.
Eosinopenia is associated with high infection rate and poor outcome
As shown in Table 3, patients with eosinopenia showed a worse clinical outcome (modified Rankin Scale scores > 3) and higher infection rate than patients without eosinopenia (P < 0.001). After adjusting for potential confounders, the odds of infection and poor outcome were significantly higher in participants with the lowest eosinophil quartile compared with those in the highest quartile (OR = 7.275; 95%CI: 1.881–28.133; P-trend < 0.001; OR = 8.855; 95% CI: 2.130–36.815; P-trend < 0.001) (Tables 6 and 7).
Table 6.
Eosinopenia indicates infection
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P-trend | OR (95% CI) | P-trend | |
| Eosinophil (%) | < 0.001 | < 0.001 | ||
| ≥ 2.3 | 1.00(Ref.) | 1.00(Ref.) | ||
| 2.3–1.1 | 1.667 (0.388–7.158) | 1.504 (0.330–6.859) | ||
| 1.1–0.4 | 3.187 (0.838–12.125) | 2.465 (0.618–9.831) | ||
| < 0.4 | 28.035 (8.349–94.139) | 7.275 (1.881–28.133) | ||
Model adjusted for Sex, age, hypertension, diabetes mellitus, coronary artery disease, current smoking, fasting plasma glucose, neutrophil count, stroke subtype, and thrombolytic therapy [multivariate logistic regression, backward stepwise (wald)]. OR: Odds ratio; CI: confidence interval; Ref: referent quartile.
Table 7.
Eosinopenia predicts poor outcomes (modified Rankin Scale scores > 3)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P-trend | OR (95% CI) | P-trend | |
| Eosinophil (%) | < 0.001 | < 0.001 | ||
| ≥ 2.3 | 1.00(Ref.) | 1.00(Ref.) | ||
| 2.3–1.1 | 2.747 (0.707–10.656) | 2.416 (0.543–10.749) | ||
| 1.1–0.4 | 4.804 (1.327–17.394) | 4.988 (1.227–20.274) | ||
| < 0.4 | 30.291 (9.024–101.676) | 8.855 (2.130–36.815) | ||
Model adjusted for sex, age, hypertension, diabetes mellitus, coronary artery disease, current smoking, fasting plasma glucose, neutrophil count, stroke subtype, and thrombolytic therapy [multivariate logistic regression, backward stepwise (wald)]. Poor outcome was defined as having a modified Rankin Scale score > 3. OR: Odds ratio; CI: confidence interval; Ref.: referent quartile.
Association between eosinophil percentage quartiles and stroke subtype
As illustrated in Table 3, the Trial of Org 10172 in Acute Stroke Treatment (TOAST) stroke subtypes exhibited significantly different eosinophil percentages (P < 0.001). In the lowest eosinophil percentage quartile, 38% of stroke cases were classified as the cardioembolic subtype, with a greater proportion than the other three higher eosinophil percentage quartiles (18%, 8%, and 12%, respectively; P < 0.001). Moreover, there was larger proportion of brain small vessel occlusions in the highest quartile than in the lowest quartile (44% vs. 12%, P < 0.001). Among eosinophil percentage quartiles, there was no significant difference of the proportions of brain large-vessel stroke.
Discussion
The present study shows that patients with the lowest eosinophil percentage quartile (< 0.4%) had remarkably larger infarct volume, a higher rate of infection, and poorer outcomes relative to the other three higher quartiles. Our results reveal that eosinopenia can predict AIS severity after adjustment for potential confounders.
Our results were consistent with previous studies that have demonstrated the prognostic significance of eosinopenia and mortality in patients with AIS (Hori et al., 2016; Wang et al., 2017; Fan et al., 2018). Some researchers have identified a positive relationship between neutrophilia and large infarct volume (Buck et al., 2008; Pagram et al., 2016). In our study, we found that eosinopenia might identify the large infarct volume more accurately than neutrophilia by comparing the area under curve. Thus, eosinophil percentage might have the potential to serve as a biomarker to predict the severity of cerebral infarction. Even though the proportion of eosinophils in peripheral blood is low, eosinopenia can occur in very rare cases. A previous study reported that only 24 patients out of 24,300 with a normal leukocyte count had eosinopenia (Krause and Boggs, 1987).
The exact mechanisms underlying the relationship between eosinopenia and AIS severity remain unclear. There are several potential explanations for the sharp reduction in the eosinophil count in critical AIS. First, there is an excessive loss of eosinophils through apoptosis and degranulation. Some studies have suggested that eosinopenia can be caused by acute stress (Bass et al., 1980; Pazdrak et al., 2016). An acute stress response may occur in patients with large infarct volume that can stimulate the release of adrenal glucocorticosteroids and epinephrine, leading to eosinopenia by apoptosis (Cayrol and Girard, 2018). However, a decrease in circulating eosinophils does not appear to be a result of adrenal mediation alone, since because this was also noted in adrenalectomized rabbits (Bass et al., 1980). Moreover, acute stress responses involving the hypothalamic-pituitary axis and autonomic nervous system can lead to stroke-induced immunological suppression, and thus increase the risk of infection (Dirnagl et al., 2007). Next, the infarct volume is a major determinant of susceptibility to infection after stroke (Hug et al., 2009). Post-ischemic inflammation is a universally accepted pathogenesis of AIS. A rise in total peripheral leukocyte number is associated with large infarct volume and increased AIS severity (Pozzilli et al., 1985; Audebert et al., 2004). Some cytokines, such as N-formyl-methionyl-leucyl-phenylalanine (Weller and Spencer, 2017) and high-concentration galectin-1 (O’Sullivan and Bochner, 2018), have been found to induce eosinophil apoptosis. Other work has found that the degranulation of eosinophils caused cytotoxic protein-mediated thrombosis and endothelial injury to promote brain infarctions (Wang et al., 2017). Another explanation for the reduction in eosinophil counts in peripheral blood is that eosinophil migrates to tissues. One study has suggested that eosinophils increased in the thrombus and decreased in peripheral blood of patients with acute coronary syndrome (Jiang et al., 2015). However, some researchers have reported that the large thrombus has high eosinophil counts both in thrombi and peripheral blood in patients with acute coronary syndrome (Sakai et al., 2009; Sundstrom et al., 2017). These different results may be attributed to differences in the patient population studied and the timing of blood sample collection. Furthermore, thrombi were noticeably large in patients with great eosinophil infiltration (Sakai et al., 2009). Consistently, our results showed that, in the lowest eosinophil percentage quartile, 38% of stroke cases were classified as the cardioembolic subtype. This may demonstrate that eosinophils promote thrombus formation and growth. Migration of eosinophils to tissues is mediated by numerous inflammatory mediators, including cytokines and activating factors (Koenderman, 2013). Bass (1977) showed that eosinopenia was caused by inflammatory factors in acute infection. Ravin et al. (2016) reported that eosinophils can engulf bacterial organisms such as Staphylococcus aureus, Escherichia coli, Listeria monocytogenes, and Pseudomonas aeruginosa via phagocytosis (Weller and Goetzl, 1980; Lehrer et al., 1989). Eosinophil granule proteins, including eosinophil cationic protein, eosinophil peroxidase, and major basic protein (Wardlaw, 1994), have an anti-bacterial and antiviral effect (Persson et al., 2001; Bystrom et al., 2011; Ohno, 2012). Eosinophil cationic protein also influences the proliferation of T and B lymphocytes (Rosenberg, 1998; Liao et al., 2016; Ravin and Loy, 2016). The number of antigen-specific plasma B cells is reportedly decreased in eosinophil-deficient mice (Pagram et al., 2016). In other work, pneumonia events were negatively correlated with blood eosinophil counts in patients with chronic obstructive pulmonary disease (Pavord et al., 2016).
The above findings indicate that the eosinophils respond to immune cells, infections, and inflammation to protect against pathogenic microorganism. This could explain why patients with eosinopenia had an increased infection rate. Several studies and reviews have emphasized the role of infection as a risk factor for mortality and poor outcome following stroke (Meisel et al., 2005). Recent studies have shown that eosinopenia is strongly associated with mortality and higher infection rate in patients with stroke (Hori et al., 2016; Bolayir et al., 2017; Wang et al., 2017; Fan et al., 2018). In our study, we also found that patients with eosinopenia have poor outcomes.
By exploring how eosinophil count is associated with infarct volume, infection rate, and poor outcome, this is the first report to identify eosinopenia as a predictive factor for AIS severity.
This study has some limitations that should be noted. First, this was a retrospective study, blood samples and CT/MRI collected in different time that may influence the eosinophil counts and infarction volumes. Second, the blood samples were collected from patients the day after admission, and so the eosinophil count might have been influenced by medication. Third, thrombus samples from the infarction area of AIS patients could not be directly obtained so we could not have concluded that eosinophil promotes thrombus formation and growth. These limitations lead to a lack of the direct evidence on association between eosinophils and thrombosis.
In summary, eosinopenia may result in high infection rates, large cerebral infarction volumes, and poor outcomes in patients with AIS.
To conclude, patients with eosinopenia may have high infection rates, large volume of cerebral infarction and poor outcome in AIS.
Additional files:
Additional file 1 (41KB, pdf) : Hospital Ethics Approval (Chinese).
Additional file 2: Open peer review report 1 (128.2KB, pdf) .
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
Financial support: None.
Institutional review board statement: This study was approved by Ethics Committee of the Second Affiliated Hospital of Soochow University, China (approval number: K10) on November 10, 2015. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a prior approval by the institution’s human research committee.
Declaration of participants consent: The authors certify that they have obtained all appropriate participants consent forms. In the forms, the participants or their family members have given their consent for the participant’s images and other clinical information to be reported in the journal. The participants or their family members understand that the participants’ names and initials will not be published and due efforts will be made to conceal the participants’ identity.
Reporting statement: This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Biostatistics statement: The statistical methods of this study were reviewed by the biostatistician of the Second Affiliated Hospital of Soochow University, China.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Individual participant data that underlie the results reported in this article, after deidentification (text, tables, figures, and appendices) will be in particular shared. Study protocol form will be available. The data will be available immediately following publication without end date. Anonymized trial data will be available indefinitely at www.figshare.com.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Jigar Pravinchandra, Florida Atlantic University, USA.
P-Reviewer: Pravinchandra J; C-Editor: Zhao M; S-Editors: Wang J, Li CH; L-Editors: Qiu Y, Song LP; T-Editor: Jia Y
References
- 1.Abidi K, Belayachi J, Derras Y, Khayari ME, Dendane T, Madani N, Khoudri I, Zeggwagh AA, Abouqal R. Eosinopenia, an early marker of increased mortality in critically ill medical patients. Intensive Care Med. 2011;37:1136–1142. doi: 10.1007/s00134-011-2170-z. [DOI] [PubMed] [Google Scholar]
- 2.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE., 3rd Classification of subtype of acute ischemic stroke Definitions for use in a multicenter clinical trial. TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 3.Audebert HJ, Rott MM, Eck T, Haberl RL. Systemic inflammatory response depends on initial stroke severity but is attenuated by successful thrombolysis. Stroke. 2004;35:2128–2133. doi: 10.1161/01.STR.0000137607.61697.77. [DOI] [PubMed] [Google Scholar]
- 4.Bass DA. Reproduction of the eosinopenia of acute infection by passive transfer of a material obtained from inflammatory exudate. Infect Immun. 1977;15:410–416. doi: 10.1128/iai.15.2.410-416.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bass DA, Gonwa TA, Szejda P, Cousart MS, DeChatelet LR, McCall CE. Eosinopenia of acute infection: Production of eosinopenia by chemotactic factors of acute inflammation. J Clin Invest. 1980;65:1265–1271. doi: 10.1172/JCI109789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolayir A, Cigdem B, Gokce SF, Bolayir HA, Kayim Yildiz O, Bolayir E, Topaktas SA. The effect of eosinopenia on mortality in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2017;26:2248–2255. doi: 10.1016/j.jstrokecerebrovasdis.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Buck BH, Liebeskind DS, Saver JL, Bang OY, Yun SW, Starkman S, Ali LK, Kim D, Villablanca JP, Salamon N, Razinia T, Ovbiagele B. Early neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke. 2008;39:355–360. doi: 10.1161/STROKEAHA.107.490128. [DOI] [PubMed] [Google Scholar]
- 8.Bystrom J, Amin K, Bishop-Bailey D. Analysing the eosinophil cationic protein-a clue to the function of the eosinophil granulocyte. Respir Res. 2011;12:10. doi: 10.1186/1465-9921-12-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cayrol C, Girard JP. Interleukin-33 (IL-33): a nuclear cytokine from the IL-1 family. Immunol Rev. 2018;281:154–168. doi: 10.1111/imr.12619. [DOI] [PubMed] [Google Scholar]
- 10.Dirnagl U, Klehmet J, Braun JS, Harms H, Meisel C, Ziemssen T, Prass K, Meisel A. Stroke-induced immunodepression: experimental evidence and clinical relevance. Stroke. 2007;38:770–773. doi: 10.1161/01.STR.0000251441.89665.bc. [DOI] [PubMed] [Google Scholar]
- 11.Fan L, Gui L, Chai EQ, Wei CJ. Routine hematological parameters are associated with short- and long-term prognosis of patients with ischemic stroke. J Clin Lab Anal. 2018 doi: 10.1002/jcla.22244. doi: 10.1002/j.cla22244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison JK, McArthur KS, Quinn TJ. Assessment scales in stroke: clinimetric and clinical considerations. Clin Interv Aging. 2013;8:201–211. doi: 10.2147/CIA.S32405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hori YS, Kodera S, Sato Y, Shiojiri T. Eosinopenia as a predictive factor of the short-term risk of mortality and infection after acute cerebral infarction. J Stroke Cerebrovasc Dis. 2016;25:1307–1312. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Hug A, Dalpke A, Wieczorek N, Giese T, Lorenz A, Auffarth G, Liesz A, Veltkamp R. Infarct volume is a major determiner of post-stroke immune cell function and susceptibility to infection. Stroke. 2009;40:3226–3232. doi: 10.1161/STROKEAHA.109.557967. [DOI] [PubMed] [Google Scholar]
- 15.Jiang P, Wang DZ, Ren YL, Cai JP, Chen BX. Significance of eosinophil accumulation in the thrombus and decrease in peripheral blood in patients with acute coronary syndrome. Coron Artery Dis. 2015;26:101–106. doi: 10.1097/MCA.0000000000000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kecoglu S, Demir M, Uyan U, Melek M. The effects of eosinophil on the left atrial thrombus in patients with atrial fibrillation. Clin Appl Thromb Hemost. 2014;20:285–289. doi: 10.1177/1076029613483208. [DOI] [PubMed] [Google Scholar]
- 17.Kirkeby K. Diagnostic and prognostic significance of eosinopenia in acute myocardial infarction. Am J Med Sci. 1956;232:50–56. doi: 10.1097/00000441-195607000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Koenderman L. Priming: a critical step in the control of eosinophil activation. In: Lee JJ, Rosenberg HF, editors. Eosinophils in health and disease. Waltham: Academic Press, USA; 2013. [Google Scholar]
- 19.Krause JR, Boggs DR. Search for eosinopenia in hospitalized patients with normal blood leukocyte concentration. Am J Hematol. 1987;24:55–63. doi: 10.1002/ajh.2830240108. [DOI] [PubMed] [Google Scholar]
- 20.Lehrer RI, Szklarek D, Barton A, Ganz T, Hamann KJ, Gleich GJ. Antibacterial properties of eosinophil major basic protein and eosinophil cationic protein. J Immunol. 1989;142:4428–4434. [PubMed] [Google Scholar]
- 21.Liao W, Long H, Chang CC, Lu Q. The eosinophil in health and disease: from bench to bedside and back. Clin Rev Allergy Immunol. 2016;50:125–139. doi: 10.1007/s12016-015-8507-6. [DOI] [PubMed] [Google Scholar]
- 22.Lind L, Siegbahn A, Lindahl B, Stenemo M, Sundstrom J, Arnlov J. Discovery of new risk markers for ischemic stroke using a novel targeted proteomics chip. Stroke. 2015;46:3340–3347. doi: 10.1161/STROKEAHA.115.010829. [DOI] [PubMed] [Google Scholar]
- 23.Marzano AV, Tedeschi A, Fanoni D, Bonanni E, Venegoni L, Berti E, Cugno M. Activation of blood coagulation in bullous pemphigoid: role of eosinophils, and local and systemic implications. Br J Dermatol. 2009;160:266–272. doi: 10.1111/j.1365-2133.2008.08880.x. [DOI] [PubMed] [Google Scholar]
- 24.Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci. 2005;6:775–786. doi: 10.1038/nrn1765. [DOI] [PubMed] [Google Scholar]
- 25.Moosbauer C, Morgenstern E, Cuvelier SL, Manukyan D, Bidzhekov K, Albrecht S, Lohse P, Patel KD, Engelmann B. Eosinophils are a major intravascular location for tissue factor storage and exposure. Blood. 2007;109:995–1002. doi: 10.1182/blood-2006-02-004945. [DOI] [PubMed] [Google Scholar]
- 26.Niccoli G, Schiavino D, Belloni F, Ferrante G, La Torre G, Conte M, Cosentino N, Montone RA, Sabato V, Burzotta F, Trani C, Leone AM, Porto I, Pieroni M, Patriarca G, Crea F. Pre-intervention eosinophil cationic protein serum levels predict clinical outcomes following implantation of drug-eluting stents. Eur Heart J. 2009;30:1340–1347. doi: 10.1093/eurheartj/ehp120. [DOI] [PubMed] [Google Scholar]
- 27.O’Sullivan JA, Bochner BS. Eosinophils and eosinophil-associated diseases: an update. J Allergy Clin Immunol. 2018;141:505–517. doi: 10.1016/j.jaci.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ohno I. Eosinophils are now recognized to play a role in health and disease, with a functional diversity due to multifaceted biological properties. Preface. Int Arch Allergy Immunol. 2012;158(Suppl 1):1. doi: 10.1159/000337733. [DOI] [PubMed] [Google Scholar]
- 29.Pagram H, Bivard A, Lincz LF, Levi C. Peripheral immune cell counts and advanced imaging as biomarkers of stroke outcome. Cerebrovasc Dis Extra. 2016;6:120–128. doi: 10.1159/000450620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pan JW, Yu XR, Zhou SY, Wang JH, Zhang J, Geng DY, Zhang TY, Cheng X, Ling YF, Dong Q. Computed tomography perfusion and computed tomography angiography for prediction of clinical outcomes in ischemic stroke patients after thrombolysis. Neural Regen Res. 2017;12:103–108. doi: 10.4103/1673-5374.198994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pavord ID, Lettis S, Anzueto A, Barnes N. Blood eosinophil count and pneumonia risk in patients with chronic obstructive pulmonary disease: a patient-level meta-analysis. Lancet Respir Med. 2016;4:731–741. doi: 10.1016/S2213-2600(16)30148-5. [DOI] [PubMed] [Google Scholar]
- 32.Pazdrak K, Straub C, Maroto R, Stafford S, White WI, Calhoun WJ, Kurosky A. Cytokine-induced glucocorticoid resistance from eosinophil activation: protein phosphatase 5 modulation of glucocorticoid receptor phosphorylation and signaling. J Immunol. 2016;197:3782–3791. doi: 10.4049/jimmunol.1601029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Persson T, Andersson P, Bodelsson M, Laurell M, Malm J, Egesten A. Bactericidal activity of human eosinophilic granulocytes against Escherichia coli. Infect Immun. 2001;69:3591–3596. doi: 10.1128/IAI.69.6.3591-3596.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pozzilli C, Lenzi GL, Argentino C, Bozzao L, Rasura M, Giubilei F, Fieschi C. Peripheral white blood cell count in cerebral ischemic infarction. Acta Neurol Scand. 1985;71:396–400. doi: 10.1111/j.1600-0404.1985.tb03219.x. [DOI] [PubMed] [Google Scholar]
- 35.Qun S, Tang Y, Sun J, Liu Z, Wu J, Zhang J, Guo J, Xu Z, Zhang D, Chen Z, Hu F, Xu X, Ge W. Neutrophil-to-lymphocyte ratio predicts 3-month outcome of acute ischemic stroke. Neurotox Res. 2017;31:444–452. doi: 10.1007/s12640-017-9707-z. [DOI] [PubMed] [Google Scholar]
- 36.Ravin KA, Loy M. The eosinophil in infection. Clin Rev Allergy Immunol. 2016;50:214–227. doi: 10.1007/s12016-015-8525-4. [DOI] [PubMed] [Google Scholar]
- 37.Rosenberg HF. The eosinophil ribonucleases. Cell Mol Life Sci. 1998;54:795–803. doi: 10.1007/s000180050208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sakai T, Inoue S, Matsuyama TA, Takei M, Ota H, Katagiri T, Koboyashi Y. Eosinophils may be involved in thrombus growth in acute coronary syndrome. Int Heart J. 2009;50:267–277. doi: 10.1536/ihj.50.267. [DOI] [PubMed] [Google Scholar]
- 40.Shah AD, Denaxas S, Nicholas O, Hingorani AD, Hemingway H. Low eosinophil and low lymphocyte counts and the incidence of 12 cardiovascular diseases: a CALIBER cohort study. Open heart. 2016;3:e000477. doi: 10.1136/openhrt-2016-000477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Slungaard A, Vercellotti GM, Tran T, Gleich GJ, Key NS. Eosinophil cationic granule proteins impair thrombomodulin function. A potential mechanism for thromboembolism in hypereosinophilic heart disease. J Clini Invest. 1993;91:1721–1730. doi: 10.1172/JCI116382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sundstrom J, Soderholm M, Borne Y, Nilsson J, Persson M, Ostling G, Melander O, Orho-Melander M, Engstrom G. Eosinophil cationic protein, carotid plaque, and incidence of stroke. Stroke. 2017;48:2686–2692. doi: 10.1161/STROKEAHA.117.018450. [DOI] [PubMed] [Google Scholar]
- 43.Ten RM, Pease LR, McKean DJ, Bell MP, Gleich GJ. Molecular cloning of the human eosinophil peroxidase. Evidence for the existence of a peroxidase multigene family. J Exp Med. 1989;169:1757–1769. doi: 10.1084/jem.169.5.1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tokgoz S, Kayrak M, Akpinar Z, Seyithanoglu A, Guney F, Yuruten B. Neutrophil lymphocyte ratio as a predictor of stroke. J Stroke Cerebrovasc Dis. 2013;22:1169–1174. doi: 10.1016/j.jstrokecerebrovasdis.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 45.Wang F, Hu S, Ding Y, Ju X, Wang L, Lu Q, Wu X. Neutrophil-to-lymphocyte ratio and 30-day mortality in patients with acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:182–187. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 46.Wang J, Ma L, Lin T, Li SJ, Chen LL, Wang DZ. The significance of eosinophils in predicting the severity of acute ischemic stroke. Oncotarget. 2017;8:104238–104246. doi: 10.18632/oncotarget.22199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang JG, Mahmud SA, Thompson JA, Geng JG, Key NS, Slungaard A. The principal eosinophil peroxidase product, HOSCN, is a uniquely potent phagocyte oxidant inducer of endothelial cell tissue factor activity: a potential mechanism for thrombosis in eosinophilic inflammatory states. Blood. 2006;107:558–565. doi: 10.1182/blood-2005-05-2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wardlaw AJ. Eosinophils in the 1990s: new perspectives on their role in health and disease. Postgrad Med J. 1994;70:536–552. doi: 10.1136/pgmj.70.826.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wassertheil-Smoller S, McGinn A, Allison M, Ca T, Curb D, Eaton C, Hendrix S, Kaplan R, Ko M, Martin LW, Xue X. Improvement in stroke risk prediction: role of C-reactive protein and lipoprotein-associated phospholipase A2 in the women’s health initiative. Int J Stroke. 2014;9:902–909. doi: 10.1111/j.1747-4949.2012.00860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weller PF, Goetzl EJ. The human eosinophil: roles in host defense and tissue injury. Am J Pathol. 1980;100:791–820. [PMC free article] [PubMed] [Google Scholar]
- 51.Weller PF, Spencer LA. Functions of tissue-resident eosinophils. Nat Rev Immunol. 2017;17:746–760. doi: 10.1038/nri.2017.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao L, Dai Q, Chen X, Li S, Shi R, Yu S, Yang F, Xiong Y, Zhang R. Neutrophil-to-lymphocyte ratio predicts length of stay and acute hospital cost in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25:739–744. doi: 10.1016/j.jstrokecerebrovasdis.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 53.Zhou J, Ma MM, Fang JH, Zhao L, Zhou MK, Guo J, He L. Differences in brain-derived neurotrophic factor gene polymorphisms between acute ischemic stroke patients and healthy controls in the Han population of southwest China. Neural Regen Res. 2019;14:1404–1411. doi: 10.4103/1673-5374.253525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zierath D, Tanzi P, Shibata D, Becker KJ. Cortisol is more important than metanephrines in driving changes in leukocyte counts after stroke. J Stroke Cerebrovasc Dis. 2018;27:555–562. doi: 10.1016/j.jstrokecerebrovasdis.2017.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


