Abstract
Objective
To evaluate the safety and feasibility of a modified poly(l‐lactic acid) (PLLA) atrial septal defect (ASD) occluder.
Methods
Forty‐five piglets were divided into two groups: an experimental group (n = 27) and a control group (n = 18). The experimental group underwent percutaneous implantation of a modified PLLA ASD device while the control group underwent percutaneous implantation of a widely used metal ASD device. X‐ray imaging, transthoracic echocardiography (TTE), electrocardiogram (ECG), histopathology and electron microscopic examination were performed at 7 days, 1, 3, 6, and 12 months after implantation.
Results
Twenty‐seven experimental piglets and 18 control piglets were all successfully implanted with modified biodegradable and metal ASD devices, respectively. While both devices exhibited very good occluding effects, the modified PLLA ASD devices were completely endothelialized at 3 months after implantation, and the endothelialization appeared to be more complete compared to the control group. Degradation of the PLLA devices was noted at 12 months follow‐up with no loss of integrity at the atrial septum.
Conclusion
This animal model with implanting of the occluders was effective and not associated with complications. The modified PLLA ASD devices are more controllable and practical than our previous devices. The implanted devices demonstrated good endothelialization and degradability in short and moderate term follow‐up. Long‐term studies are now underway to further evaluate the biodegradability of this novel device.
Keywords: atrial septal defect, biodegradable occluder, congenital heart disease, endothelialization, poly(l‐lactic acid)
1. INTRODUCTION
Atrial septal defect (ASD) is the third most common congenital heart defect and accounts for about 30% of the congenital heart disease population. With the development of ASD devices especially nickel‐titanium‐alloy double umbrella (DU) occluders and improvement of cardiac catheterization and interventions, percutaneous interventional treatment has become the first option for secundum ASD patients.1, 2
Nevertheless, metal devices are not a perfect solution with significant limitations. First, there are several complications reported after insertion. The potential complications include erosion, thrombus formation, pericardial effusion, inflammation, valve damage, delayed endothelialization, hemolytic phenomena, nickel allergy and aortic‐atrial fistula among others.3, 4, 5, 6, 7, 8 Second, the retained device obstructs access for future trans‐septal procedures such as electrophysiology interventions, mitral valve interventions, left atrial appendage closure, etc. Finally, some patients would prefer not to remaining a foreign body in their heart indefinitely. To address these issues, researchers and clinicians have envisioned a biodegradable septal occluder device.9, 10, 11, 12, 13, 14, 15, 16
We presented the outcomes of an animal experiment in swine with our poly(l‐lactic acid) (PLLA) biodegradable ASD devices in 2016.17 Although the outcomes showed the basic feasibility of the PLLA device, the device was difficult to prepare and fold into a sheath. Additionally, it was hard to adjust position after deployment in vivo. We also noted peri‐device inflammatory changes at 3 and 6 months follow‐up after implantation although this did not appear to have any recognizable clinical sequelae. In order to address these issues and to enhance its safety and feasibility, we modified the device and carried out the animal experiments. The outcomes are presented in the present article.
2. MATERIALS AND METHODS
2.1. The characteristics of the modified PLLA ASD device and delivery system
The modified biodegradable ASD is a self‐expandable “double‐umbrella” framework made of 0.15 mm PLLA wire meshes. Compared to the previous devices and delivery systems, we have made six improvements listed as follows (Figure 1):
The number of PLLA wire meshes constituting the device framework is reduced from 72 to 36.
The connector between the device and the delivery system is changed from a nitinol connecting multiwire to a screw connector that makes releasing devices from the delivery system easier.
One more radio‐opaque mark is added to the tip of the left disc as well as two radio‐opaque marks at both ends of the discs and two additional radio‐opaque marks to the waist. After the modification, the left disc can be identified more easily under fluoroscopy so that the device can be maneuvered into appropriate position in vivo.
One loader with a flare angle was added to the tip of a delivery system. The loader is designed such that one end dilates like a horn mouth to allow the PLLA device to be retracted with less force and the other end is of a regular size which connects with the delivery system. The loader makes it easier to retract the device into the delivery sheath, after assembly of the delivery system, without damaging the device frame.
The locking wire and button is replaced by a locking system that is composed of a PLLA stick. One end of the PLLA stick is attached to the left disc and the other end has an angled tip and internal screw connects with the delivery system. Once the angled tip is removed, the device can be locked so that the left disc and right disc can be fixed together. When the locking system is pushed back, the device can be unlocked once again.
The diameter of the PLLA baffle membrane is modified from 4 mm larger than the discs to 2 mm larger. This modification allows the use of smaller delivery sheaths to deploy the PLLA devices.
Figure 1.

Schematic drawing of (A) the previous PLLA ASD device and (B) the modified PLLA ASD device. Both A and B present (a) unlocked state, (b) locked state, and (c) device and delivery system. Six modifications have been made to device A that result in device B: Reduced PLLA wire meshes, screw connector, one more mark at the sealing tip of the left disc, a loader with flare angle, a locking system, downsized membrane
2.2. Animals
Forty‐five experimental piglets were divided into two groups. One group was comprised of 27 piglets (mean weight 26.9 kg), in which biodegradable ASD devices were implanted. In the other 18 piglets (mean weight 27.9 kg), HeartR nitinol ASD devices (Lifetech Company, Shenzhen, China) were implanted as a control group. Prior to operation, all animals underwent clinical examination and transthoracic echocardiography (TTE) scanning to demonstrate that they were healthy with morphologically normal hearts. All animals were obtained from Mingzhu Experimental Animal Scientific Technology Company (DongGuan city, Guangdong Province, China). The research was approved by the Research Ethics Committee of Guangdong General Hospital/Guangdong Academy of Medical Sciences.
2.3. Procedure and follow‐up
All experimental animals were under general anesthesia with intubation and ventilation. Through the femoral vein, we perforated the atrial septum with trans‐septal puncture technique followed by dilation of the septal defect using a 12–15 mm Cristal Balloon to create ASD models. We then implanted either a biodegradable polymer ASD device or a nonbiodegradable metal ASD device. The details of the procedure have been previously described.17 The diameter of the percutaneously created ASD ranged from 4.0 mm to 7.0 mm, with a mean diameter of 5.5 mm. According to the diameter of created ASD, we selected one of two sizes of biodegradable and metal devices, either an 8 mm or a 10 mm with 8F sheath.
The animals were followed up at 7 days, 1, 3, 6, and 12 months after implantations. All piglets were administered aspirin 3–5 mg/kg/d for up to 6 months after implantation. The animals were observed by professionals trained to record general characteristics that included behavior, eating, sleeping, breathing, the luster of skinny hair and the body temperature. The laboratory tests included complete blood count, electrolyte estimation, renal function tests, liver function tests and blood gas estimations. Laboratory tests were performed pre‐procedure and at 7 days, 1, 3, and 6 months after implantation. Chest radiography, TTE and electrocardiogram (ECG) were performed at each follow‐up. We also performed gross anatomical examination and histologic evaluation and scanning electron microscopy (SEM) examination by sacrificing 13 experimental animals at each group.
2.4. Statistical analysis
We used t‐tests to compare the product performance before and after design change and the difference between the two experimental groups. The statistical method of tolerance intervals was employed to compute a range of values for the product's characteristic, using the statistical software is Minitab.
3. RESULTS
3.1. ASD models and technical success rate
All 45 ASD models were created successfully in both the biodegradable group and the control group. Twenty‐eight PLLA ASD devices and 17 metal devices were implanted into 45 piglets. At the first attempt, 25 of the 28 PLLA devices were implanted. The remaining three PLLA devices were released in the left atria for retrieval tests and implanted after the second adjustment. All metal devices were implanted successfully on the first attempt.
Eight 10‐mm and seventeen 8‐mm PLLA devices (with molecular weights of the polymer 56 kDa and 30 kDa, respectively) were implanted into the experimental group animals. As a comparison, six 10 mm and twelve 8 mm metal devices were implanted into the animals of the control group.
There was no significant difference in the procedure time between the experimental group and the control group (11.2 vs. 10.8 minutes). So, the introduction of the biodegradable polymer into our novel occluder has not led to complication of operation in our experiments.
The modified platinum–iridium radio‐opaque markers were clearly visible under X‐ray images. TTE evaluation showed no shunting, mitral regurgitation or tricuspid regurgitation in all 45 piglets. ECGs confirmed that there were no arrhythmias during the procedures.
3.2. Postoperative follow‐up study
All animals survived in good physical condition with normal behavior, and no clinical evidence of limb ischemia, dyspnea or infection. There was no difference in the total number of leukocytes between the two groups at preprocedure and 1, 3, and 6 months after implantations (Figure 2).
Figure 2.
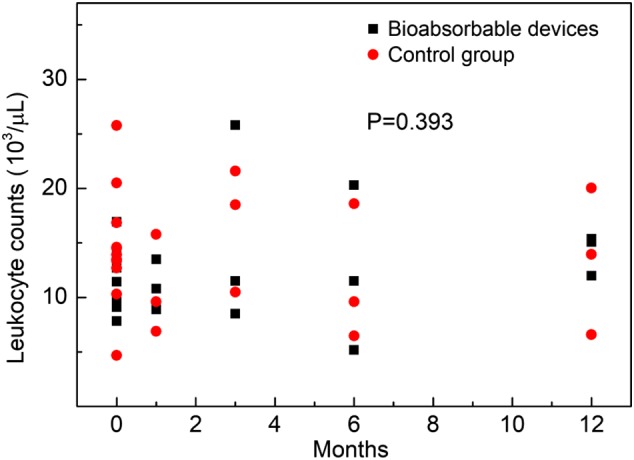
Leukocyte counts at pre‐procedure and at 1, 3, 6, and 12 months after implantations. No significant difference was found between biodegradable devices and control group
At 7 days, 1, 3, 6, and 12 months after implantation, good position and shape of implanted PLLA ASD devices were confirmed by X‐ray imaging (Figure 3). TTE showed that there was no residual shunting, thrombosis, pericardial effusion, mitral regurgitation or tricuspid regurgitation after device implantation (Figure 4). No arrhythmias were observed by ECG.
Figure 3.

The X‐ray images before (A) and after (B) releasing the PLLA device. The arrows indicate marks. Seven marks were shown clearly after releasing the polymer device
Figure 4.

Echo images at 6 months follow‐up. (A) Four chamber view; (B) short axis view. The arrows indicate the biodegradable device. The device exhibited an appropriate shape and no residual shunting
3.3. Macroscopic examination of cardiac anatomy
Animals from each group were sacrificed at the following time points: 7 days (n = 1), 1 month (n = 3), 3 months (n = 3), 6 months (n = 3), and 12 months (n = 3) after implantation. All sacrificed piglets demonstrated a normal heart shape, cardiac chamber volume and myocardial wall thickness. The position of each device was appropriate, and no vegetation or thrombus was observed. There was no evidence of injury to the mitral or tricuspid valves.
Macroscopic examination showed that the biodegradable occluders were partially covered with a layer of new endothelial tissue at 1 month after implantation and were covered completely at 3 months. In comparison, the surfaces of the metal occluders were partially covered with a layer of new endothelial tissue only at 3 months and the metal wires were still visible at 12 months. It appeared that the biodegradable device encouraged a greater extent of endothelial growth than the metal device. At 6 months, the biodegradable remained complete and in a good shape. At 12 months, the PLLA devices were partially degraded but still in a stable formation (Figure 5).
Figure 5.

Gross appearances of a PLLA device (A–C) and a metal device (D–F) taken from the pigs at indicated follow‐up spots. (A) At 3 months, the left disc (arrow) of a PLLA device was completely covered by new endothelial tissue, and PLLA wires were not visible; (B) at 6 months, the left disc of the PLLA device was completely covered; (C) at 12 months, the left of the PLLA device was partially degraded, and the rest was still in a firm formation; (D) at 3 months, the left disc of the metal device was covered partially by new endothelial tissues; (E and F) at 6 months (E) and 12 months (F), the left disc was almost covered by new endothelial tissue, and the metal wires were still visible
We also evaluated the gross inspection of other important organs, and did not find any abnormalities in the appearance of the lungs, liver, spleen, kidneys, or heart.
3.3.1. Histopathological examination
At 3, 6, and 12 months after implantation, the PLLA devices were surrounded by a large number of collagen fibers and fibroblasts, while a moderate number of inflammatory cells including neutrophils, lymphocytes, plasma cells, and multinuclear giant cells could also be observed. No necrotic tissue was noted. At 12 months, the PLLA wires were partly degraded. Similarly, a large number of collagen fibers and fibroblasts surrounded the metal device. A small number of inflammatory cells were also observed. The inflammatory cells surrounding the PLLA device were not significantly more numerous compared with the metal device at 3, 6, and 12 months follow‐up (Figure 6).
Figure 6.

HE staining of a PLLA occluder (A–C) and a metal occluder (D–F) at different follow‐up points (3 months for a and D, 6 months for B and E, and 12 months for C and F). At all of the three time points after implantation, the PLLA device (blue arrows) was surrounded by a large amount of collagen fibers (black arrows) and fibroblasts (green arrows). A moderate number of inflammatory cells and multinuclear giant cells could be observed; yet no necrotic tissue observed. The PLLA wires were partly degraded at 12 months. For the nonbiodegradable occlude, a large number of collagen fibers (black arrows) and fibroblasts (green arrows) surrounded the metal device (red arrows). A small number of inflammatory cells was also observed
HE staining also showed that there were no anomalies in the lung, liver, spleen, or kidney, and no infarction of these organs was observed in either of the groups.
3.4. SEM observations
At 3 and 6 months after implantation, the PLLA occluder was covered by a layer of fibrous tissues. In contrast, the metal occluder was covered not only by a layer of fibrous tissues but also by many endothelial cells at 3 and 6 months. At 12 months after implantation, the PLLA device was covered by a large number of endothelial cells similar to the metal device (Figure 7).
Figure 7.

Scanning electronic microscopic images of the PLLA occluder (A–C) and metal occlude (D–F) at different time points after implantation (×400). At 3 months (A) and 6 months (B), the PLLA occluders were covered by a layer of fibrous tissues. At 3 months (D) and 6 months (E), the metal occluders were not only covered by a layer of fibrous tissues, but also by many endothelial cells. At 12 months, both the PLLA occluders and the metal devices were covered by a large amount of endothelial cells
4. DISCUSSION
So far, some biodegradable ASD occlusion devices have been developed such as partially biodegradable devices including BioSTAR, Biodisk, and Double Biodisc devices, which have been discarded,9, 10, 11, 13, 14 and fully biodegradable devices including the Chinese Lantern (CL), the DU, PLGA/collagen membrane, and the polydioxanone (PDO), which are in progress.14, 15, 16, 18 The “Chinese Lantern” device made of fully biodegradable polymers (copolymer of caprolactone and lactate) consists of a soft portion and a structural skeleton.18 Although the animal experiment showed that the devices were in satisfactory position and stable after 1‐month follow‐up, this version of CL device may not be suitable for closure of a larger defect with insufficient anchorability and less coverage. The DU device was also made of polycaprolactone and polylactide, and is comprised of double self‐expandable umbrellas with a stem. The DU device was easy to prepare and fold into a 9F sheath and also easy to deploy and anchor.12 However, because the stem of the DU device is longer than septum, the DU device leaves a considerable gap between the umbrella discs and the septum, giving rise to potential thrombosis formation within the gap. The PLGA/collagen membrane was developed with a nanofiber matrix of blend of poly(dl‐lactide‐glycolide) and type I collagen which has mechanical properties comparable to those of commercial metallic occluders.16 PLGA starts significant bioresorption after 6 months of postimplantation, and thus degraded faster than PLLA.19, 20 The PDO ASD occluder made from biodegradable materials is a self‐expandable double‐disc device, similar in construction to the Amplatzer septal occlude.13 Animal experiments confirmed its effectiveness and biological compatibility. However, due to low elastic modulus, low tensile strength, the limited shape‐memory function of PDO, and the large diameter of PDO monofilament fibers (0.298 mm) compared with the nickel‐titanium wire (0.1 mm), the production of a larger occluder may be restricted.
We used PLLA as the matrix of the biodegradable occluder. PLLA is a semicrystalline polymer. The fibers are of high tensile strength, good flexibility, heat resistance, and good thermal stability.21 Due to its bioresorbability and biocompatibility in the human body, lactic acid‐based polymers have been used for resorbable sutures and prosthetic devices.22 Our initial PLLA occlude is a fully biodegradable device composed of a self‐expandable double‐disc weaved by seventy two 0.15 mm PLLA wires, three PLLA baffle membranes, a locking piece and two platinum–iridium radio‐opaque markers at both ends of the discs. We implanted percutaneously 17 PLLA ASD devices into piglets during the first animal experiment.17 The outcome was inspiring and 1‐year follow‐up studies showed ASD closure. We also identified some issues with the device such as difficulty in assembly and folding into a sheath before deployment, and difficult adjustment once the device is released in vivo. Additionally, there was some inflammation around the device at 3 and 6 months after implantation although this caused no harm to the main organs.
In order to address these issues, we modified the device and made some improvements as follows: We reduced the profile of the device including downsizing baffle membranes, reducing PLLA wires, so that a smaller sheath can be used to deliver the biodegradable device (12 mm device with an 8F sheath). We used a new locking system to replace the previous locking wire and button which is hardly unlocked after being locked. The retrieval tests demonstrated that the new locking system is more scientific and has more ability to tolerate operators making mistakes. We added one more radio‐opaque marks at the tip of the left disc and two more radio‐marks at the waist. After the modification, the three radio‐marks form a triangle. When the left disc is opened, the marks can help operators identify more accurately the shape of the left disc under radiography. Other modifications including using a screw connector and adding a flare loader enable releasing devices more easily in vivo and inserting a device into a delivery sheath without damaging the device frame. We also compared the operations time between the two groups, and the outcome showed no difference.
Biodegradable ASD devices require two special functions to heal atrial septal heart defects: endothelialization and degradability. If a biodegradable device has degraded and deformed before complete endothelialization, there will be a risk of residual shunt. As a result, it is imperative that biodegradable devices facilitate complete endothelialization prior to biodegradation. Although some reports showed most ASD devices fully endothelialize within 3 months in animal experiments,23, 24 there are very few reports in human. One study in humans, in which the Clamshell device was deployed showed that endothelialization with complete coverage of the device can be expected as early as 2.7 months.25 However, some cases reported that there was still incomplete endothelialization at 12 months after the implantation of metal ASD occluder devices.26, 27, 28, 29, 30 In the present study, the PLLA ASD device was completely covered by neointima at 3 months after implantation. The endothelialization of the PLLA device appeared to be superior to the metal device.
The previous animal experiment with the PLLA ASD device showed severe inflammation around the device at 3 and 6 months after implantation.17 Although the inflammatory reaction caused no harm to main organs in that experiment, we hope to decline the reaction and reduce the potential risk as much as possible. To address that, we reduced the quantity of the PLLA wire meshes to half with the number of the wires from 72 to 36. The tensile strength of the device discs was kept through a new weave technique, although the quantity of the wires reduced. Hematoxylin and eosin staining showed only moderate inflammation at 3, 6, and 12 months. The inflammatory cells around the PLLA device were a little more prominent but not significantly increased compared to the metal device.
PLLA degrades through the hydrolysis of backbone ester groups and the degradation rate depends on the PLLA crystallinity, molecular weight, molecular weight distribution, morphology, water diffusion rate into the polymer, and the stereoisomeric content.31 The degradation rate is often considered to be an important selection criterion for biomedical applications.32 The expected time to mostly degrade a PLLA device is about 3 years. Gross anatomical examination and histologic evaluation illustrated that the PLLA devices still kept a stable formation in vivo at 12 months follow‐up. This outcome thus meets the criterion that the PLLA device was degraded after complete endothelialization. We will continue to evaluate the long‐term degradation of the PLLA device in vivo.
5. LIMITATIONS
The present study has a few limitations. As we were unable to create a larger ASD animal model by trans‐septal puncture, this study was designed to implant small and medium biodegradable devices. Furthermore, the experimental piglets were only followed‐up for only 12 months. Nevertheless, this study was aimed to test the feasibility of our modified biodegradable device and to progressively evaluate the efficacy and safety of this device in swine. Thus, the present study did achieve its objectives.
6. CONCLUSION
Our modified PLLA biodegradable device was operable. Compared to the common metal device, the polymer device allows improved endothelial growth. At 12 months after implantation, the PLLA devices started to be degraded and still kept a stable formation. Long‐term studies are now under way to evaluate the biodegradability of the novel device.
ACKNOWLEDGMENTS
This work was financially supported by National Key R&D Program of China (Grant No. 2016YFC1100300) and Guangdong Science and Technology Department of China (Grant No. 2015B070701008). Shenzhen Sanming medical project of China.
Li B‐N, Xie Y‐M, Xie Z‐F, et al. Study of biodegradable occluder of atrial septal defect in a porcine model. Catheter Cardiovasc Interv. 2019;93:E38–E45. 10.1002/ccd.27852
Funding information National Key R&D Program of China, Grant/Award Number: 2016 YFC1100300; Guangdong Science and Technology Department of China, Grant/Award Number: 2015B070701008; Shenzhen Sanming medical project of China
[Correction added on 9 Nov, after first online publication: Dr. Zhang's address was corrected.]
Contributor Information
Yu‐Mei Xie, Email: xymay@126.com.
Zhi‐Wei Zhang, Email: drzhangzhiwei@sina.com.
REFERENCES
- 1. Fischer G, Masura J, Kramer HH, Gavora P. Transcatheter occlusion of secundum atrial septal defects with self‐centering Amplatzer septal occluder. Prog Pediatri Cardiol. 1998;9:119‐124. [Google Scholar]
- 2. Bissessor N. Current perspectives in percutaneous atrial septal defect closure devices. Med Dev: Evid Res. 2015;8:297‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Divekar A, Gaamangwe T, Shaikh N, Raabe M, Ducas J. Cardiac perforation after device closure of atrial septal defects with the Amplatzer septal occluder. J Am Coll Cardiol. 2005;45:1213‐1218. [DOI] [PubMed] [Google Scholar]
- 4. Lai DW, Saver JL, Araujo JA, Reidl M, Tobis J. Pericarditis associated with nickel hyper‐sensitivity to the Amplatzer occluder device: A case report. Catheter Cardiovasc Interv. 2005;66:424‐426. [DOI] [PubMed] [Google Scholar]
- 5. Khodaverdian RA, Jones KW. Metal allergy to Amplatzer occluder device presented as severe bronchospasm. Ann Thor Surg. 2009;88:2021‐2022. [DOI] [PubMed] [Google Scholar]
- 6. Luermans JG, Post MC, Yilmaz A. Late device thrombosis after atrial septal defect closure. Eur Heart J. 2010;31:142. [DOI] [PubMed] [Google Scholar]
- 7. Abaci A, Unlu S, Alsancak Y, Kaya U, Sezenoz B. Short and long term complications of device closure of atrial septal defect and patent foreman ovale: Meta‐analysis of 28,142 patients from 203 studies. Catheter Cardiovas Interv. 2013;82:1123‐1138. [DOI] [PubMed] [Google Scholar]
- 8. Bardino DJ, McElhinney DB, Kaza AK, Mayer JE Jr. Analysis of the US food and drug administration manufacture and user facility device experience database for adverse events involving Amplatzer septal occluder devices and comparison with the society of thoracic surgery congenital cardiac surgery database. J Thorac Cardiovasc Surg. 2009;137:1334‐1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jux C, Bertram H, Wohlsein P, Bruegmann M, Paul T. Interventional atrial septal defect closure using a totally bioresorbable occluder matrix: Development and preclinical evaluation of the BioSTAR device. J Am Coll Cardiol. 2006;48:161‐169. [DOI] [PubMed] [Google Scholar]
- 10. Karagianni A, Abrahamsson P, Furenas E, Eriksson P, Dellborg M. Closure of persistent foramen oval with the BioSTAR biodegradable PFO closure device: Feasibility and long‐term outcome. Scand Cardiovasc J. 2011;45:267‐272. [DOI] [PubMed] [Google Scholar]
- 11. Happel CM, Laser KT, Sigler M, Kececioglu D, Sandica E, Hass NA. Single center experience: Implantation failures, early, and late complications after implantation of a partially biodegradable ASD/PFO‐device (BioSTAR®). Catheter Cardiovasc Interv. 2015;85:990‐997. [DOI] [PubMed] [Google Scholar]
- 12. Duong‐Hong D, Tang Y‐D, Wu W, et al. Fully biodegradable septal defect occluder—A double umbrella design. Catheter Cardiovasc Interv. 2010;76:711‐718. [DOI] [PubMed] [Google Scholar]
- 13. Pavcnik D, Takulve K, Uchida BT, et al. Biodisc: A new device for closure of patent foramen ovale: A feasibility study in swine. Catheter Cardiovasc Interv. 2010;75:861‐867. [DOI] [PubMed] [Google Scholar]
- 14. Pavcnik D, Tekulve K, Uchida BT, et al. Double BioDisc: A new bioprosthetic device for transcatheter closure of atrial septal defects—A feasibility study in adult sheep. Radiol Oncol. 2012;46:89‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhu YF, Huang XM, Cao J, et al. Animal experimental study of the fully biodegradable atrial septal defect (ASD) occluder. J Biomed Biotechnol. 2012;2012:735989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu SJ, Peng KM, Hsiao CY, Liu KS, Chung HT, Chen JK. Novel biodegradable polycaprolactone occlusion device combining nano‐fibrous PLGA/collagen membrane for closure of atrial septal defect (ASD). Ann Biomed Eng. 2011;39:2759‐2766. [DOI] [PubMed] [Google Scholar]
- 17. Xie Z‐F, Wang S‐S, Zhang Z‐W, et al. A novel‐design poly‐l‐lactic acid biodegradable device for closure of atrial septal defect: Long‐term results in swine. Cardiology. 2016;135:179‐187. [DOI] [PubMed] [Google Scholar]
- 18. Wu W, Yip J, Tang Y‐D, et al. A novel biodegradable septal defect occluder: The “Chinese lantern” design, proof of concept. Innovations. 2011;6:221‐230. [DOI] [PubMed] [Google Scholar]
- 19. Martina N, Mohammad A, Berto JB, et al. Historical development of atrial septal defect closure devices: What we learn from the past. Expert Rev Med Dev 2016;13(6):555–568. [DOI] [PubMed] [Google Scholar]
- 20. Wu LP, Ding JD. In vitro degradation of three‐dimensional porous poly(d,l‐lactide‐co‐glycolide) scaffolds for tissue engineering. Biomaterials. 2004;25(27):5821‐5830. [DOI] [PubMed] [Google Scholar]
- 21. Gupta B, Revagade N, Hilborn J. Poly(lactic acid) fiber: An overview. Prog Polym Sci. 2007;32:455‐482. [Google Scholar]
- 22. Aura R, Harte B, Selke S. An overview of polylactides as packaging material. Macromol Bisosci. 2004;4:835‐864. [DOI] [PubMed] [Google Scholar]
- 23. Sharafuddin MJA, Glu X, Titus JL, Urness M, Cervera‐Ceballos JJ, Amplatz K. Transvenous closure of secundum atrial septal defects: Preliminary results with a new self‐expanding nitinol prosthesis in a swine model. Circulation. 1997;95:2162‐2168. [DOI] [PubMed] [Google Scholar]
- 24. Sideris EB, Sideris SE, Fowlks JP, Ehly RL, Smith JE, Gulde RE. Transvenous atrial septal occlusion in piglets with a “buttoned” double disc device. Circulation. 1990;81:312‐318. [DOI] [PubMed] [Google Scholar]
- 25. Kreutzer J, Ryan CA, Gauvreau K, Van Praagh R, Anderson JM, Jenkins KJ. Healing response to the clamshell device for closure of intracardiac defects in humans. Catheter Cardiovasc Interv. 2001;54:101‐111. [DOI] [PubMed] [Google Scholar]
- 26. Slesnick TC, Nugent AW, Fraser CD, Cannon BC. Incomplete endothelialization and late development of acute bacterial endocarditis after implantation of an amplatzer septal occluder device. Circulation. 2008;117:e326‐e327. [DOI] [PubMed] [Google Scholar]
- 27. Amedro P, Soulatges C, Fraisse A. Infective endocarditis after device closure of atrial septal defects: Case report and review of the literature. Catheter Cardiovasc Interv. 2017;89:324‐334. [DOI] [PubMed] [Google Scholar]
- 28. Bialkowski J, Pawlak S, Banaszak P. Incomplete endothelialisation of an Amplatzer Septal Occluder device followed by meningitis and late acute bacterial endocarditis. Cardiol Young. 2016;26:808‐810. [DOI] [PubMed] [Google Scholar]
- 29. Zahr F, Katz WE, Toyoda Y, Anderson WD. Late bacterial endocarditis of an Amplatzer atrial septal defect occluder device. Am J Cardiol. 2010;105:279‐280. [DOI] [PubMed] [Google Scholar]
- 30. Astroulakis Z, Ei‐Gamel A, Hill JM. Failed endothelialisation of a percutaneous atrial septal defect closure device. Heart. 2008;94:580. [DOI] [PubMed] [Google Scholar]
- 31. Janorkar AV, Metters AT, Hirt DE. Modification of poly(lactic acid) films: Enhanced wettability from surface‐confirmed photografting and increased degradation rate due to an artifact of the photografting process. Macromolecules. 2004;37:9151‐9159. [Google Scholar]
- 32. Tokiwa Y, Calabia BP. Biodegradability and biodegradation of poly(lactide). Appl Mocrobiol Biotechnol. 2006;72:244‐251. [DOI] [PubMed] [Google Scholar]


