Abstract
Primary cardiac lymphoma (PCL) is a rare extranodal lymphoma that involves only the heart and/or pericardium. It is fatal in the absence of a prompt diagnosis and adequate therapy. Here, we report an immunocompetent 55‐year‐old Chinese man with palpitations and occasional chest distress for 1 month. Multimodal imaging work‐up showed a tumor infiltrated into the myocardium, which greatly contribute to a timely pathology diagnosis of PCL.
Keywords: cardiovascular imaging, immunocompetent, multimodal imaging, primary cardiac lymphoma
A 55‐year‐old man presented in our department with palpitations and occasional chest distress for 1 month. Biochemical examinations were all within normal limits and test for HIV was negative. On the day of hospitalization, an electrocardiogram showed a Q wave in the II, III, and aVF leads. Transthoracic echocardiography (TTE) demonstrated pericardial effusion with a multi‐segmental infiltrated ill‐defined hypoechoic mass that extensively affected the mitral and papillary muscle level of the left ventricular (LV) anterior wall (Figure 1A, Movie S1), the middle to upper part of the right ventricular (RV) free wall, the RV outflow tract, and the initial segment of the main pulmonary artery (Figure 1B). The thickness of the infiltrated wall ranged from 2.8 to 3.4 cm. The mitral and tricuspid valves were not affected, but the main pulmonary artery was narrowed where the peak systolic velocity measured 1.7 m/s. The myocardial contrast echocardiography (MCE) study revealed rich perfusion in the thickened RV wall myocardium similar to other myocardial segments (Figure 1C, Movie S2). Initially, a cardiac tumor was suspected. Cardiac magnetic resonance imaging (CMRI) confirmed the extent of the mass infiltration (Figure 1D and E, [Link], [Link]) of the TTE and showed the impairing motion of the lateral and inferior RV walls. Post‐contrast‐enhanced CMRI revealed non‐homogenous gadolinium enhancement of the tumor, areas of non‐enhancement implied pericardial effusion (Figure 1F, Movie S5). No evidence of mediastinal lymphadenopathy was observed. Furthermore, positron emission tomography/computed tomography (PET/CT) scan revealed elevated 18fluorodeoxyglucose accumulation with high standardized uptake values (maximum 9.8) in the RV free wall and the LV anterior wall, suggesting a malignant nature of the neoplasm, coronal views showed no evidence of distant metastatic disease (Figure 2A and B). The patient finally underwent an open chest biopsy through median sternotomy. The morphology and immunohistochemistry of excised masses revealed complete destructive replacement by CD20 + B‐lymphocytes (Figure 3). A diagnosis of primary diffuse large B cell lymphoma of the RV was made. The patient was started on a standard systemic chemotherapy protocol of 6 cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R‐CHOP) and showed a good response to the chemotherapy (Figure 2C and D). One year later, the patient was in complete clinical remission.
Figure 1.
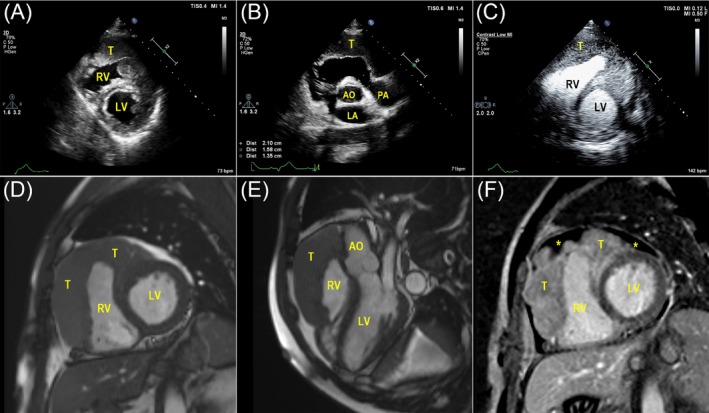
A, Left ventricular short‐axis views of TTE demonstrated the tumor formation in both the RV free wall and the LV anterior wall; B, In the aortic root short‐axis view, the main pulmonary artery was narrowed; C, MCE showed rich perfusion in the thickened myocardium; D and E, The extent of the mass infiltration revealed by CMRI was consistent with TTE; F, Post‐contrast‐enhanced CMRI showed hypo‐intensive non‐homogenous gadolinium‐enhanced masses, focal areas of non‐enhancement (asterisk) implied pericardial effusion. (T indicates tumor; LV, left ventricle; RV, right ventricle; AO, aortic; LA, left atrial)
Figure 2.
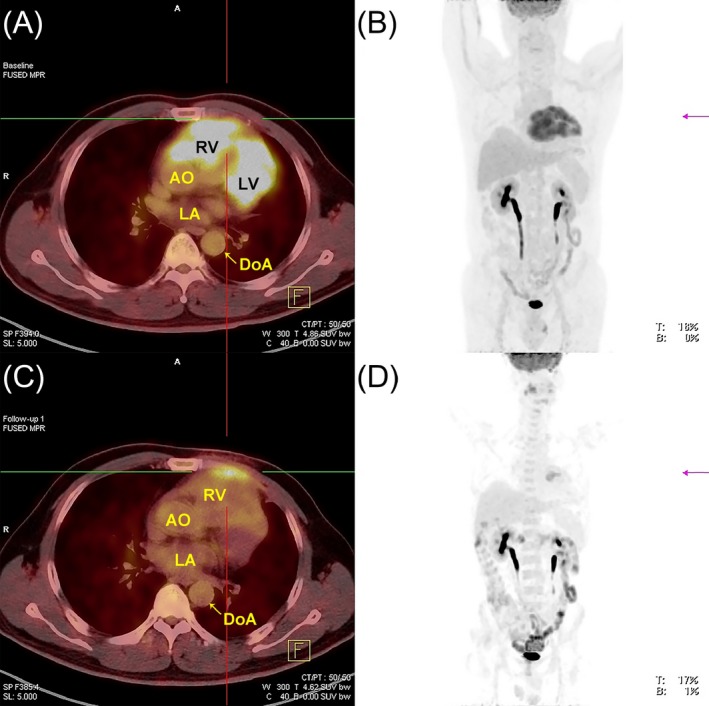
Baseline PET/CT revealed abnormal elevated 18fludeoxyglucose uptake in only the RV free wall and the LV anterior wall demonstrated in anterior PET maximum intensity projection image (A) and axial fusion PET/CT image (B); PET/CT following 6 months of chemotherapy shows marked interval decrease in FDG uptake with an associated decrease in overall size of the mass (C‐D). (T indicates tumor; LV, left ventricle; RV, right ventricle; AO, aortic; LA, left atrial; DoA, descending aorta)
Figure 3.
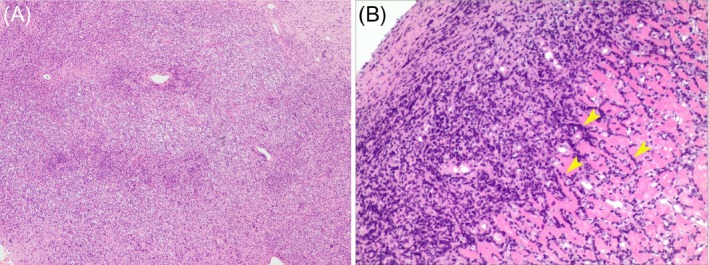
Histopathological examination with hematoxylin‐eosin staining of the right heart endomyocardium (A) revealed a dense atypical lymphocytic diffuse infiltration in the myocardium. B, Higher power shows large atypical lymphoid cells (arrowhead) with large, irregular, or round nuclei and a small cytoplasmic area
PCL is extremely rare, representing only 1.3% of all primary cardiac tumors and 0.5% of all extranodal lymphomas.1 Patients usually die within a few months after being diagnosed.2 Prompt diagnosis and early R‐CHOP chemotherapy treatment appear to be the only chance for cure.3 However, the clinical manifestations may be heterogeneous.4 Multimodal approaches greatly aid in the diagnosis and characterization of cardiac masses. Electrocardiogram and echocardiography represent a quick noninvasive approach to evaluate patients with lung‐ and heart‐related symptoms. MCE can be used to evaluate the blood supply of the mass; in general, PCL exhibits rich perfusion in the thickened myocardium that distinguishes the mass from normal myocardium. In comparison, CMR techniques yield accurate and reproducible data regarding soft‐tissue and tumorous infiltration of the myocardium and pericardium, myocardial perfusion, myocardial fibrosis, LV and RV size and function, and valvular regurgitation. PCL demonstrates heterogeneous enhancement after intravenous contrast material administration and less likely than sarcomas to have necrosis, involve the valves, and extend into heart chambers. MRI is performed for diagnosis, while CT is used for serial monitoring of the treatment response. PET/CT is crucial in determining whether a mass is benign or malignant, providing additional information about the metabolic activity of lesions. Certain features, such as high 18fluorodeoxyglucose avidity on PET, suggest a malignant tumor rather than a benign tumor. The final diagnosis must still be confirmed by biopsy.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
Supporting information
Movie S1. Indicate the Figure 1A. TTE left ventricular short‐axis views demonstrated the tumor formation in both the RV free wall and the LV anterior wall
Movie S2. Indicate the Figure 1C. MCE showed rich perfusion in the thickened myocardium
Movie S3. Indicate the Figure 1D. CMRI showed that the tumor infiltrated the RV free wall and extended across the interventricular septum into the LV anterior wall
Movie S4. Indicate the Figure 1E. CMRI showed that the tumor infiltrated up to the pulmonary artery root
Movie S5. Indicate the Figure 1F. Post‐contrast‐enhanced CMRI showed non‐homogenous gadolinium enhancement of the tumor, areas of non‐enhancement implied pericardial effusion (asterisk)
Wang S, Li M, Zhang L, Xie M. Multimodal imaging evaluation of a primary cardiac lymphoma in an immunocompetent patient. Echocardiography. 2018;35:2121–2123. 10.1111/echo.14150
Drs Shuyuan Wang and Meng Li contributed equally to this work.
Contributor Information
Li Zhang, Email: zli429@hust.edu.cn.
Mingxing Xie, Email: xiemx@hust.edu.cn.
REFERENCES
- 1. Burke A, Jeudy J Jr, Virmani R. Cardiac tumours: an update: cardiac tumours. Heart. 2008;94:117–123. [DOI] [PubMed] [Google Scholar]
- 2. Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large‐B‐cell lymphoma. N Engl J Med. 2002;346:235–242. [DOI] [PubMed] [Google Scholar]
- 3. Dawson MA, Mariani J, Taylor A, et al. The successful treatment of primary cardiac lymphoma with a dose‐dense schedule of rituximab plus CHOP. Ann Oncol. 2006;17:176–177. [DOI] [PubMed] [Google Scholar]
- 4. Petrich A, Cho SI, Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer. 2011;117:581–589. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Movie S1. Indicate the Figure 1A. TTE left ventricular short‐axis views demonstrated the tumor formation in both the RV free wall and the LV anterior wall
Movie S2. Indicate the Figure 1C. MCE showed rich perfusion in the thickened myocardium
Movie S3. Indicate the Figure 1D. CMRI showed that the tumor infiltrated the RV free wall and extended across the interventricular septum into the LV anterior wall
Movie S4. Indicate the Figure 1E. CMRI showed that the tumor infiltrated up to the pulmonary artery root
Movie S5. Indicate the Figure 1F. Post‐contrast‐enhanced CMRI showed non‐homogenous gadolinium enhancement of the tumor, areas of non‐enhancement implied pericardial effusion (asterisk)


