Abstract
Over the past decades, increases in life expectancy in most modern societies have raised questions about whether and to what extent individuals value possible extensions of their personal lifetime. In this vein, a new field of research emerged that investigates the determinants, concomitants, and consequences of longevity values and personal preferences for an extended lifetime across adulthood. Based on a review of available theoretical and empirical work, we identified 3 mindsets on the challenges and potentials of human longevity common in research as well as personal views: (a) an essentialist mindset that builds on ideal principles of an infinite life, aimed at conquering or significantly postponing a biologically determined aging process, (b) a medicalist mindset that appraises aging as being primarily based on quality of health, and (c) a stoicist mindset that associates longevity and lifetime extension with the experience of grace and meaning. In this regard, we submit that motivation for longevity and its behavioral consequences differ depending on what mindsets individuals adopt in a given developmental context. We suggest that mindsets of longevity motivation are embedded in personal belief systems (e.g., death acceptance) that may depend on health, and on context influences (e.g., culture). Mindsets of longevity motivation may be related to differences in health behavior and late-life preparation. We illustrate such ideas with an exploratory analysis from a cross-cultural data set. We discuss the possible implications of these mindsets of longevity motivation for the aging sciences, and with regard to individual ways of approaching old age.
Keywords: Attitudes about aging, Cross-cultural studies, End of life, Humanities, Life course/life span, Longevity motivation, Medicalism, Oldest old, Quality of life, Self-rated health
Translational Significance.
Contexts, personal beliefs, and functional health are thought to influence an individual’s motivation for longevity. Identifying mindsets of motivation for longevity may help to better understand preparation for old age and individual decisions in the aging process and may provide an opportunity for future intervention.
Longevity is both blessing and onus of the medical, technical, and social advances observed in most modern societies over the past century. There exist strong differences with regard to how individuals value the gains of additional years in life. In 1939, Piersol and Bortz were first to define an agenda for future gains in life expectancy, when they proclaimed that: “… it is for science to add life to years and not years to life” (p. 976). With this often-cited statement, Piersol and Bortz identified life quality and functional health as a key scope of biomedical aging research. However, with an increasing number of people experiencing extended life spans, many also come to appreciate the potentials for positive life experiences in these added on years even when conditions are adverse. Thus, adding life to years cannot be viewed simply as a medical issue because the quality of a prolonged life also depends on cognitive, behavioral, psychological, and social processes. There is some evidence that individuals show considerable adaptivity and resilience to aversive circumstances in all phases of life (Bonanno, 2004; Brandtstädter, 1999). Moreover, there is strong agreement in gerontology that old age reflects what Paul Baltes and collaborators (e.g., P. B. Baltes & Smith, 2003) coined as an “…incompleteness of the overall biogenetic architecture of the life course” (P. B. Baltes & Smith, 2003, p. 131), which often involves vulnerability and risks (Butler, 1975; Kruse, 2017). Accordingly, in many demographic, epidemiologic, and large-scale studies, it has been shown that extensions of life expectancy were associated with gains in both healthy years and years lived with disability, chronic health conditions, or need of care (Hay et al., 2017). In this vein, the final phase of very old age is generally considered to involve challenges, loss, and decline (P. B. Baltes & Smith, 2003; Tesch-Römer & Wahl, 2017). One implication is that the task of aging may not be restricted to maintaining health and functioning, but also includes adaptational tasks such as coping with disability and care needs (M. Baltes, Wahl, & Reichert, 1991). In other words, aging may also involve the need to accept some kind of vulnerability. Consequently, psychological resilience to adverse life conditions may foster motivation for longevity from early adulthood until very late in life.
In this vein, a new field of research has emerged that investigates individual preferences and attitudes toward longevity and extensions of lifetime. In the following, we review and discuss previous research on longevity motivation (Lang, Baltes, & Wagner, 2007) and related concepts such as attitudes toward an extended lifetime (Cicirelli, 2011), valuation of life (Lawton et al., 1999), and will to live (Carmel, 2011). Existing research on longevity motivation has often focused on specific phases of the life span such as late life (Carmel, 2011), young and middle adulthood (Bowen & Skirbekk, 2017) or end-of-life (Cicirelli, 2011). We are not aware of an integrative theoretical life-span approach that includes different approaches to longevity motivation in a comprehensive life-span perspective. For example, it is not well understood whether longevity desires differ from health-related preferences in young, middle-aged, or old-aged adulthood. In what ways do individuals across adulthood differ with regard to the meaning, and the perceived value of longevity? What are age-related determinants and consequences of varying mindsets of longevity motivation?—We begin our considerations by giving an overview on existing research on longevity desires. Based on these findings we submit a heuristic model of longevity motivation. We conducted an exploratory pilot analysis using a cross-cultural study to illustrate some of the assumptions of this heuristic model. We conclude this review with a discussion of future research issues that can be derived from the proposed heuristic model of longevity motivation.
Desired and Expected Longevity
In general, individuals in modern societies differ with regard to how strongly they esteem possible extensions of their personal lifetime (Cicirelli, 2011; Lang et al., 2007; Ekerdt, Koss, Li, Münch, Lessenich, & Fung, 2017). For example, some individuals think of lifetime extensions merely as products of biomedical advances. Consequently, a person may believe that a prolonged lifetime is only acceptable for oneself as long as one experiences autonomy or health. Other individuals may think of their personal lifetime and late life as a task that they want to accomplish regardless of whether this also involves experience of loss. There exist several studies, in which individuals reported their personal longevity motivations, based on questions such as “to what age would you like to live?.”, or “how long would you like to live?”, all of which we consider to have equivalent connotations. Especially when considered in relation to personal longevity expectations (e.g., “to what age do you expect to live?”) different mindsets become evident. For example, wanting to live as long as one expects reflects an acceptance of the finitude of one’s personal life. A desire to live much longer than one expects to live may indicate a desire to overcome actual limits of life expectancy. A wish to live less long than one expects to live may imply a negative or deprecating attitude toward aging.
Table 1 gives an overview on distributions of findings that were identified in recent empirical studies. The table combines findings from studies that used either quantitative or qualitative methods to assess longevity preferences in diverse samples from different phases of the human life course. In general, findings are heterogeneous and vary depending on the respective study design, method, age composition, and cultural backgrounds. For example, Ekerdt and colleagues (2017) interviewed 90 older adults in three different cultures. About 37% expressed no wish of “having more time in life,” either by directly expressing their desire for an end in the near future, or by referring to fate. About 48% of the respondents wished to live longer conditional on mental and physical health, and 15% expressed an unconditional wish to live longer. In the study of Karppinen and her colleagues (2016) individuals reported whether and why they would (not) “want to live to be 100?”—Out of the 1,405 older adults, one-third (32.9%) wanted to live to 100 years. Health was both a condition for wanting to reach 100 years (expressed by 45%) and a reason for not wanting to reach this age (expressed by 48%). Apart from this, 57% of the individuals wanting to reach 100 years expressed positive reasons for this such as curiosity or love for life. On the other side, 77% of the individuals not wanting to reach 100 years stated reasons expressing negative attitudes toward life in very old age. In a quantitative study based on a representative sample, Donner and colleagues (2016) assessed responses to two items: “How long do you wish to live?” and “If you could be physically and mentally the same as in your 20s, how long would like to live?” In response to the first item two-thirds (65%) preferred to live until 85 years, while under the condition of being healthy about 80% expressed a wish to live to at least 120 years (53% desired an unlimited lifetime).
Table 1.
Measurement and Distribution of Longevity Desires: An Overview of Findings
| Authors/sample | Sample items on longevity desire | Key findings |
|---|---|---|
|
Lang and colleagues (2007)
a
N = 364 (Study 2), M = 52 years (20–92 years); 54% female |
(1) What age would you like to reach? (2) How desirable would it be for you to reach the age you want to if you were confronted with a health problem resulting in frailty or need for care? |
(1) Desired years: M = 85, SD = 10; 17% desired to live beyond 90 (2) Not desirable: 75% |
|
Cicirelli (2011)
N = 109, M = 77 years (60–99 years), 64% female |
If you could choose and you knew you could maintain good health, how many more years would you like to live? | Wished for 16 more years (SD = 8.9) |
|
Karppinen, Laaokkonen, Strandberg, Tilvis, and Pitkälä (2012)
N = 283, M = 79 years (75–90 years), 62% female |
How many more years would you still wish to live? | Wished for 8 additional years on average: <5: 26%, 5–10: 56%, >10: 18% |
|
Donner and colleagues (2016)
N = 1,000, 20–70 years,b 67% female |
(1) How long would you like to live? (2) If you could be physically and mentally the same as in your 20s, how long would you like to live? |
(1) 65% → desire 85 years (2) 80% → 120 or more years (unlimited: 53%) |
|
Karppinen, Laakkonen, Strandberg, Huohvanainen, and Pitkala (2016)
N = 1,405, = 83 years (75– 96 years), 69% female |
(1) Do you want to live to be 100? (2) Why? (3) Why not? |
(1) 33% want to live to be 100 (2) for purpose in life: 57% (3) expecting disability: 48%; negative view of late life: 77% |
|
Ekerdt and colleagues (2017)
N = 90, 65–85 years,b 54% female |
(1) Would you like to have more time? (2) If someone would offer you extra years, how many would you like to get? What for? |
No wish for more time: 37%; conditional on health: 48%; unconditional wish for more years: 15% |
|
Bowen and Skirbeck (2017)a N = 1,631, M = 42 years (18–64 years), 50% female |
If you had your choice, how long would you like to live? That is, until what age? | Desired lifetime: 90 years (median); 17% prefer less than 80 years |
|
Ambrosi-Randic, Nekić, and Tucak Junaković (2018)
N = 423, M = 69 years (60–95 years), 57% female |
What age would you like to reach? How long do you expect to live? |
Desired average lifetime: 88 years (SD = 9), 4 years longer than expected |
aResponses more than 120 years were recoded as 120 in this study.
bMean age not reported.
Taken together, the available studies so far suggest that four general patterns of responses to questions on longevity desires can typically be observed, that is, (a) a conditional wish for longer life as long as one feels healthy (majority), (b) a wish to continue one’s life “as long as it goes” or for a few years (often accompanied by a reluctance to think about desired longevity), (c) unrealistic wishes for a very long or unlimited life (more often in samples of younger adults), and (d) no wish to live any longer than expected (more often observed in samples of very old adults). Next to such single item-based approaches of assessing preferred life duration (e.g., Lang et al., 2007), there are also other related research approaches that are based on different methods to assess motivation for prolonged and continuated life. A prominent example is the will-to-live construct used in the work of Carmel (Carmel, 2011; Carmel, Baron-Epel, & Shemy, 2007). The will-to-live scale is suitable for individuals who are currently facing situations in which they consciously question their will to live (e.g., old age, aversive life conditions). Research shows that expressions of will to live among very old individuals are—among others—associated with subjective aging indicators (Shrira, Carmel, Tovel, & Raveis, 2018) and longer survival (Carmel et al., 2007; Karppinen et al., 2012).
Attitudes on the Extension of Longevity: Motivational Mindsets
The available theoretical considerations and empirical findings on desired longevity point to a considerable heterogeneity and breadth of diverse research venues that are not yet well connected with each other. For example, research on the value of health or attitudes to dying and death often involve issues related to the valuation of life and longevity preferences (Cicirelli, 2011; Ditto, Druley, Moore, Danks, & Smucker, 1996; Karppinen et al., 2012; Lockhart et al., 2001). In an attempt to integrate some of the different lines of reasoning and research findings, we submit that there exist three widespread classes of attitudes, expectations, and preferences with regard to a possible extension of human lifetime in modern societies that may reflect different schools of thought, such as essentialism, medicalism, and stoicism. Table 2 summarizes the different primary motives that are associated with the three perspectives on longevity and life-time extension, that is, infinite life, healthy life, and dignified life. We submit that these three primary motives can be used to characterize different scientific approaches on longevity, as well as individual attitudes and preferences toward longevity in everyday thinking. We refer to such perspectives as mindsets that involve sets of representations, attitudes, and ways of thinking about the meaning and value of a prolonged live.
Table 2.
Mindsets of Longevity Motivation
| Mindset | Motive | Guiding principle | Research focus (sample) |
|---|---|---|---|
| Essentialist | Infinite life | Motivation for extended life span involves striving to overcome biological degeneration and health declines | Antiaging medicine, rejuvenation |
| Medicalist | Healthy life | Motivation for extension of lifetime is conditional on physical and mental health | Curative medicine, therapeutic intervention |
| Stoicist | Dignified life | Motivation for a long life reflects a wish for dignity and meaning even when there is loss and vulnerability | Palliative medicine, geriatric rehabilitation |
An essentialist mindset views aging as a degenerative process that is inevitably associated with physical loss. It reflects the idea that aging is a determined and undesirable process, and that the human mind is held captive in a deficient biological organism. Accordingly, pathological aging cannot be differentiated from normal or healthy aging. One implication is that aging per se is viewed as pathogenetic and ought to be pushed back, for example, with antiaging medicine (De Grey, 2003). Consequently, radical extensions of the life span are expected when antiaging research is successful. A focus in research, but also in personal lifestyles, is on turning off degenerative processes in the cell, skin, organism, or mind. We refer to this as essentialism because it reflects a belief that aging is essentially defined by biology (Weiss, 2018). Such perspectives also become evident in attempts of bio-technical approaches that aim at surmounting limitations of the human existence. Examples of an essentialist motivation for longevity are also reflected in transhumanist attitudes (More & Vita-More, 2013), and become evident in the work of organizations such as the Life Extension Foundation or the Calorie Restriction Society (McGlothin & Averill, 2008). Consequently, such mindsets may also be associated with a wish to live an extremely and to date unrealistically long life while disregarding implications or consequences on social, behavioral, cognitive, and motivational aging. Recent studies of Cicirelli (2011) and Ballinger, Tisdale, Sellen, and Martin (2017) suggest that the prevalence of essentialist mindsets can be estimated in the range of 3–10% of respondents who wish to live forever or wish to “overcome” the natural aging process.
A medicalist mindset involves that human aging is viewed as burdened only when pathology occurs, and that pathological aging is different from normal aging. In this perspective, aging is associated with age-related health risks, and defined as a medical challenge. One implication is that successful aging may be defined as an absence of disease and disability (Rowe & Kahn, 1997). There is a long and wide tradition regarding such mindsets on longevity that has generated a myriad of insights and improved understanding of the potentials for extending the healthy and active life expectancy (Hay et al., 2017). Medical and clinical research has identified some of the somatic, cellular, molecular, and genetic limitations of the human life span (Kirkwood, 2005). On an individual level, medicalism is reflected in an appreciation for an extended lifetime if health functioning can be maintained, and degenerative diseases such as dementia can be avoided. Another implication might be that when endorsing a medicalist mindset, individuals may prefer to avoid the vulnerability of old age and wish to die rather than to become chronically ill or demented. Such tendencies have been investigated in studies on health values and time trade-offs. Therein individuals are asked to equate a number of years living in imperfect health (e.g., severe pain, unconsciousness, or just the current health state) with the same or a smaller number of years living in perfect health (Ayalon & King-Kallimanis, 2010; Tsevat et al., 1998) or they are asked how long they would like to live under certain medical conditions (Ditto et al., 1996; Lawton et al., 1999). Related research investigated the wish for life-sustaining treatments under different illness scenarios (e.g., Carmel & Mutran, 1997). Results indicate that most individuals express a preference to not continue life in a severely restricted health condition, while a few others want to continue living even under such adverse circumstances. Thus, a majority seems to express health-conditional longevity desires that involve continuity of one’s personal capacities and resilience. In this vein, Rietjens and colleagues (2005) classified 35% of their representative life-span sample (N = 1,777 aged 20–93 years) to value quality over length of life, which reflects a medicalist perspective. Another 30% of respondents valued length over quality, and 35% were indecisive.
The stoicist mindset for living long reflects the idea that withstanding the challenges and risks of a long or prolonged life is part of the conditio humana (Cole & Sierpina, 2007), which involves striving for meaning in life, and for acceptance of one’s actual life condition (Butler, 1975; Erikson, 1959). We refer to this as stoicism which was an ancient hellenistic school founded by Zeno of Citium (332–262 BC) suggesting that the virtues of the human mind (e.g., wisdom, courage) prevail over all external hardships or constraints in life such as physical loss (cf. P. B. Baltes & Baltes, 1990). The challenges, needs, risks, or tasks within the aging process may thus appear manageable or at least bearable as long as there is meaning in life and a sense of grace (Carmel, 2011; Lawton et al., 1999). For example, palliative and hospice care is aiming to enhance well-being and to preserve a sense of dignity, when curative therapies become ineffective. Palliative care may thus foster meaning in life even in its final stages, and in severe chronical health conditions (Steinhauser et al., 2000). Preserving dignity and meaning in a prolonged life is pivotal to a stoicist mindset. Thus, having a worthy and dignified life may be emphasized over the absence of chronical diseases in late life. Regarding the desired extension of lifetime, we submit that holding a stoicist mindset may involve that individuals express a valuation of life per se and “as it comes.” This may also involve a discomfort or unwillingness to reflect about lifetime extension rather than about dignity and meaning in life. The stoicist motivation on longevity relies on an optimality principle of aging (P. B. Baltes & Baltes, 1990; Lang, Rohr, & Williger, 2011) that refers to a best possible life rather than to absolute standards of a good life.
Note that our description of these mindsets as essentialist, medicalist, or stoicist, is not intended as a typology. Rather we contend that the different patterns of longevity-related thinking may be present at the same time but with varying intensity or strength. For example, an individual may express a stoicist mindsets with regard to withstanding physical challenges, and at the same time follow a medicalist mindset that life is undesirable when suffering from Alzheimer’s disease. A distinctive characteristic of the three mindsets, however, pertains to which of the salient motives of infinite, healthy, and dignified life is actually prioritized. Any pairwise comparison of two (out of the three) motives reveals overlap but also distinctive features: For example, a motive to reach an infinite life may imply striving for a healthy life. The essentialist emphasis, however, lies on the idea of overcoming degeneration as a cause of age-related decline or death (De Grey, 2003; McGlothin & Averill, 2008; More & Vita-More, 2013). One may argue that an essentialist mindset is taking the medicalist mindset to the extremes.
The medicalist motive for a healthy life implies that life should also be meaningful. However, the scope of medicalist views primarily lies on maintaining health and functioning. In this perspective, it is conceded that “normal” aging may also entail gains (Ayalon & King-Kallimanis, 2010; P. B. Baltes & Smith, 2003; Butler, 1975; Piersol & Bortz, 1939; Tesch-Römer & Wahl, 2017). Finally, when prioritizing a motive of dignified life this does not preclude a wish to have a healthy life. Rather, a stoicist mindset implies a wish for prolonged lives to reflect meaning and grace irrespective of whether this involves chronical and severe health conditions (Butler, 1975; Carmel, 2011; Kruse, 2017). In sum, differentiating the three motivational mindsets contributes to improved understanding of longevity preferences and attitudes toward longer lives.
A Heuristic Model of Motivation for Longevity
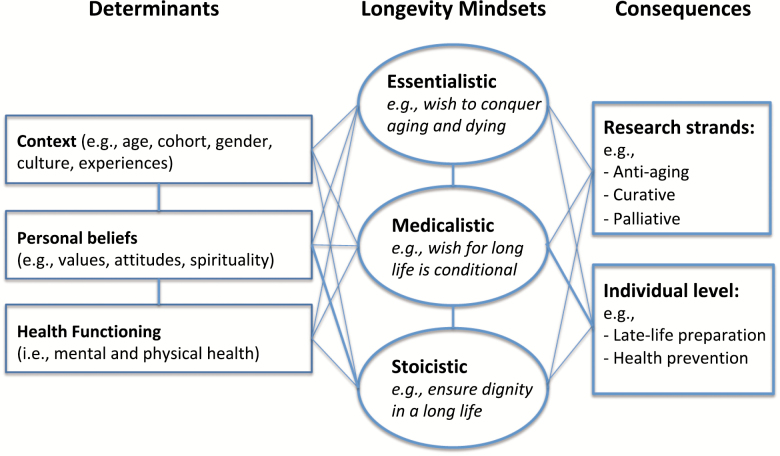
In 2007, Lang, Baltes, and Wagner proposed a preliminary information-theoretical model for the investigation of longevity motivation across adulthood. The model was built on the premise that individuals—in principle—do not know their personal future, and thus can only speculate about their preferences regarding very old age and late life. In this situation, individuals may rely on two broad sources of information about longevity, that is, (a) the cultural and societal contexts that organize the life span such as education, social structure, norms, and values, and (b) the experiential level of one’s personal biography, cognition, attitudes, and expectations. Lang and colleagues (2007) observed that the experiential-level sources of information better predicted personal desires of longevity than societal-level sources of information. Advancing and extending this model, we suggest that the different mindsets of longevity motivation depend on contextual influences (e.g., culture, age, gender, personal experiences), on health functioning as well as on personal beliefs (e.g., attitudes toward aging, religiosity, future perspectives, death acceptance). Figure 1 illustrates a heuristic model of determinants and consequences of the mindsets of longevity motivation. According to this model, mindsets of longevity motivation are depending on contextual influences, mental and physical health as well as on personal beliefs. For example, better access to social security and Medicare in one’s culture may be related to a stronger endorsement of stoicist mindsets. Personal belief systems may also differentiate between the three mindsets of longevity motivation: For example, a stoicist mindset may be associated with greater spirituality and death acceptance, whereas essentialist mindsets may be related to more secular beliefs and to more negative attitudes toward old age. Medicalist mindsets, in contrast may be associated with deficit-oriented views of aging, and with a stronger emphasis of personal health values. Moreover, personal belief systems may differ depending on mental and physical health functioning, as well as on the respective societal and cultural context.
Figure 1.
A heuristic model of motivational mindsets on longevity. Note. Lines from determinants (left column) to mindsets and to consequences are meant to indicate directed paths, whereas lines between essentialist, medicalist, and stoicist mindsets indicate the interplay among these.
While there is some research on age and gender differences in longevity motivation (e.g., Carmel et al., 2007; Lang et al., 2007), not much is known about the role of other contextual variables, health, and personal belief systems in this regard. For example, religious beliefs and spirituality may play a critical role with regard to how long one desires to live. Few studies have explicitly explored such associations. Ballinger and colleagues (2017) explored the role of religiosity with respect to endorsing lifetime extension to 100 years, 150 years or indefinitely. The vignettes presented in this study, envisioned either minimized health decay in a prolonged life (medicalist), or an arrested aging process (essentialist) as a condition for lifetime extension. Stronger religiosity (e.g., beliefs in god’s will) was generally associated with lower wishes for healthy prolongation of lifetime. Findings like that may however differ between religions and depending on the envisioned health condition (Carmel & Mutran, 1997).
The heuristic model also implies that the three mindsets of longevity motivation will be differentially related to consequences on the level of research strands as well as on the level of individual behavior. For example, a more medicalist mindset may involve a greater focus on health prevention. Stoicist mindsets may generate a palliative and accepting approach to longevity-related challenges. Lastly, essentialist mindsets may involve a greater emphasis on antiaging medicine, or on cosmetics. Consequently, we argue that each of the three mindsets may also be reflecting different agendas in scientific research, for example, with regard to focusing on antiaging experimental research in the lab, medical therapies for aging-related diseases, or intervention research that targets on resilience and maintaining a will to live.
There are very few examples for studies that seem to target all three mindsets of longevity motivation simultaneously, and thus help to bridge some of the gaps between the different perspectives. One example is an innovative and unique study that Cicirelli (2011) conducted with 109 adults aged 60–99 years. In this study participants reported if they would like to live forever (esssentialist), how long they would like to live if they could maintain good health (medicalist), and how the expected duration of one’s life was associated with one’s goals and meaning in life (stoicist). On average, study participants expressed unfavorable attitudes toward an infinite life and toward major life extension. If imagining to live forever or to live for 150 years, participants endorsed goals such as personal and societal achievement and helping others. If imagining to have 6 months left or up to 10 years, maintaining good relationships with others was considered more important. If imagining fewer than 6 months to be left in life, participants endorsed goals related to preparing for death.
A Pilot Study and Empirical Illustration
From our heuristic model (Figure 1) several implications and research questions can be derived for further research and improved understanding of the determinants and consequences of different mindsets of longevity motivation. To begin with and to give a preliminary empirical illustration of our conceptual arguments, we conducted an exploratory analysis with data from the international, interdisciplinary, and cross-cultural “Aging as Future (AaF)” Study (Rothermund, Lang, & Lessenich, 2012). Specifically, data stemmed from 1,678 participants of a cross-sectional online study conducted in 2016. Participants were initially recruited via agencies, local meeting points, and online platforms. Two hundred and twenty-eight participants were from Hong Kong, 281 from Taiwan, 175 from the United States, and 994 from Germany. Age ranged from 18 to 93 years with the average being 48.2 years (SD = 19.5). 52.6% were women, 31.5% were retired, and 71.2% lived in a relationship. Education was above average with 38.7% having a university degree. In addition, we used 4-year longitudinal data from the same study available for a subsample of 194 Germans, who participated in 2012 and 2016 (74% women; M = 53.3 years, SD = 16.3). Data were collected in an ongoing online study and participants were initially recruited via agencies, local meeting points, and online platforms.
To begin with, we focused our analysis on two single-item measures of desired longevity (i.e., “To what age would you like to live?”) and expected longevity (i.e., “To what age do you expect to live?”). To be clear, we do not suggest that only two indicators will suffice to capture the breadth and depth of the three mindsets of longevity motivation. Rather, we use this approach to explore to what extent the mindsets may already become discernable in the response patterns of such succinct indicators of longevity desires. The valid responses to the question on desired longevity ranged from 25 to 500 years. For example, 106 individuals (6.4%) wanted to live for 120 years or longer and hence, wished for a life span that clearly exceeds current demographic expectations. Such answers may reflect the wish to overcome or crucially postpone aging and dying. In contrast, 127 individuals (7.6%) wished to live for 70 years or less. One potential reason for such low longevity desires might be the wish to avoid old age as a phase of heightened vulnerability and health declines. Most participants (86.0%) however wished for a life span ranging from 71 to 119 years, with a mean desired longevity of M = 88.9 years (SD = 8.3) which is comparable to prior studies (e.g., Ambrosi-Randic et al., 2018; Lang et al., 2007). However, 14 participants gave illogical, and invalid responses (i.e., lower than current chronological age), and had to be excluded from the analysis.
In a next step, we used the responses to the question “To what age do you expect to live?” as an anchor for an individual’s longevity desire. For example, one could imagine two individuals who both would like to live for 105 years. One has a family history of exceptional longevity and thus expects to become 105 years. The other one expects to live to the age of 75. Whereas the former seems to accept his or her expected longevity as desirable, the latter expresses a wish for a significantly longer life than he or she actually expects. Within our sample, 11.8% wished to die earlier than they expected, 35.6% wished to live exactly as long as they expected, 33.3% had longevity desires moderately exceeding their personal longevity expectations (by 10 years or less), and 19.3% had longevity desires strongly exceeding their personal longevity expectations (by more than 10 years). These discrepancy groups differed significantly in age, F(3) = 64.84, p < .001, and gender, χ2(3) = 37.73, p < .001. Specifically, the group with concordant longevity desires and expectations was the oldest, whereas the group that wished for much longer lives than expected was the youngest and predominantly male. In contrast, the group that wished for shorter lives than expected was predominantly female.
Individuals whose longevity desires and expectations are highly similar may show a greater acceptance of the expected life duration and may thus be more likely to hold stoicist attitudes. In contrast, the stronger longevity desires and longevity expectations diverge, the more likely medicalist and essentialist attitudes may become. We suggest that the interplay between desired and expected life duration contributes to improved understanding of an individual’s motivation for longevity. More specific, we contend that the discrepancy between desired minus expected longevity may be used to illustrate individual differences related to contextual influences, health, and personal belief systems as suggested in the heuristic model. In the following, we present two preliminary illustrations in the scope of the proposed heuristic model. First, we explored effects of context (i.e., culture), personal belief systems (i.e., death acceptance), and health functioning (i.e., self-rated health, Figure 1) on the interplay of desired and expected longevity. Second, we used a longitudinal subsample to explore stability and change of longevity motivation across 4 years as well as potential behavioral consequences (i.e., on health behaviors). To the best of our knowledge, this is the first empirical exploration of longitudinal changes in longevity desires based on an age-heterogeneous sample of nonclinical study participants.
Determinants of Motivation for Longevity
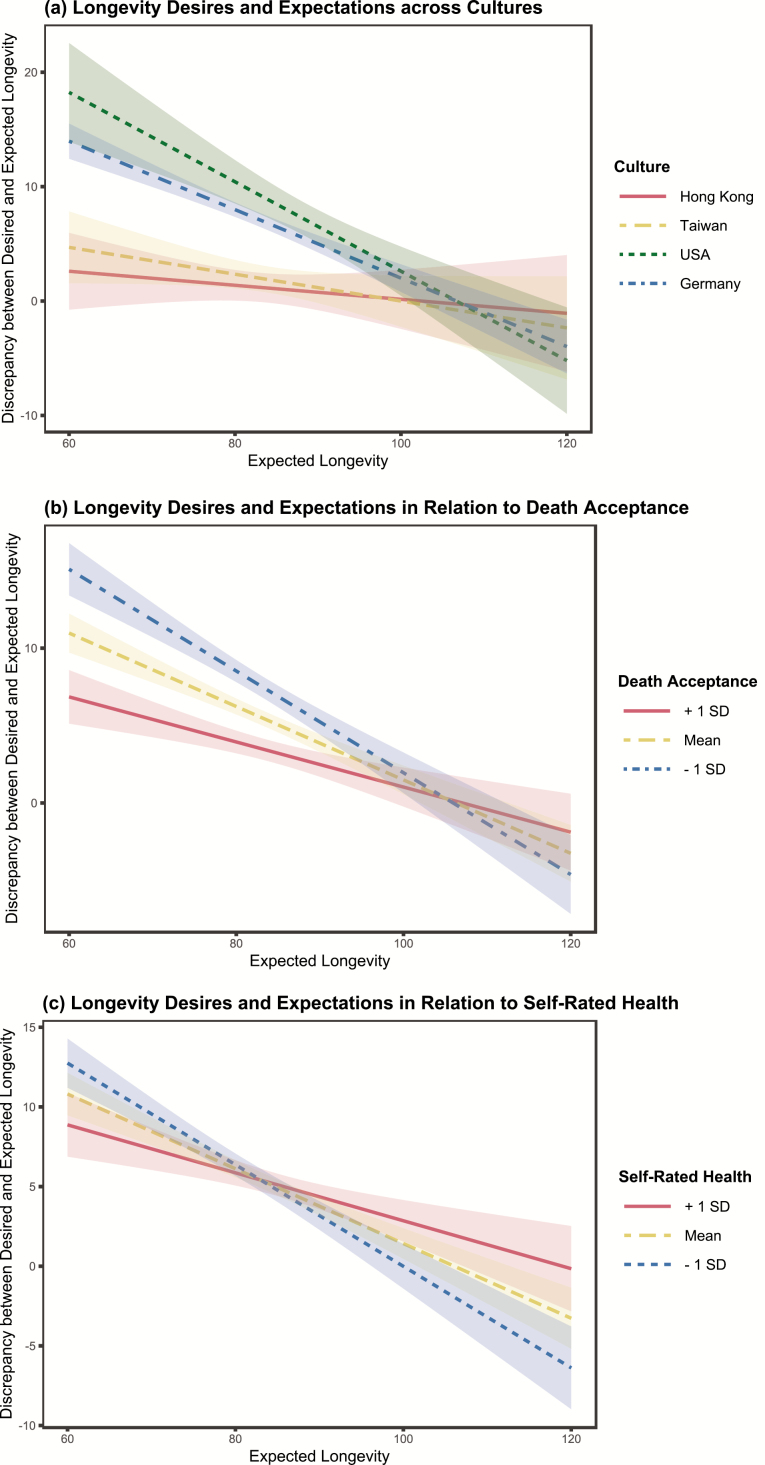
We chose to investigate one indicator of each proposed class of determinants in relation to patterns of longevity desires and expectations. Context was represented here by culture differences (Germany, Hong Kong, United States, Taiwan). Personal beliefs were represented by death acceptance (measured with one item from Brandstädter & Wentura, 1994: “I look towards the end of life with calm”). Health functioning was represented by self-rated health measured with one item ranging from 1 (very good) to 5 (bad). To allow for convenient interpretation of findings, we display the results graphically in Figure 2. The graphically displayed interplays of longevity desires and longevity expectations with culture, death acceptance, and self-rated health also reached significance in a corresponding regression analysis, before and after controlling for effects of age, gender, education, and family status. Education was made comparable across cultures with ISCED categories ranging from 1 (primary education) to 8 (doctoral degree).
Figure 2.
Longevity desires and expectations as related to (a) culture, (b) death acceptance, and (c) self-rated health. Note. For reasons of statistical clarity and presentation, extreme longevity desires and expectations smaller than 60 and larger than 120 were adjusted to 60 and 120 years, respectively.
We tested the possible moderation effects for each of the three determinants (i.e., culture, self-rated health, death acceptance) on the association between expected longevity and the discrepancy score between desired and expected longevity. We refer to this association as it depicts the interplay between desired and expected longevity in relation to expected longevity itself. Specifically, the observed discrepancies between desired minus expected longevity were strongest when expecting one’s lifetime to end before 90 years. This means, the younger one expects to die, the more likely it is to desire to live beyond one’s expectations (r = −.23, p < .001). This association was however observed to be weaker in Taiwan and Hong Kong (when compared with Germany and United States, Figure 2a), weaker when death acceptance was reported to be strong (Figure 2b), and weaker when health was reported to be good (Figure 2c).
Desired and expected longevity were highly concordant within the two Eastern samples from Taiwan and Hong Kong. In contrast, individuals from the United States and Germany tended to wish for (much) longer lives, especially when they expected their own life to be rather short (the regression weights of expected longevity on the discrepancy to desired longevity were b = −.33, p < .001, for the United States, and b = −.24, p < .001, for Germany when Hong Kong served as a reference category). This result may hint to a greater likelihood of essentialist tendencies within the two Western cultures.
Among individuals, who reported strong death acceptance and good health, the discrepancies between desired and expected longevity were low when compared with those, who felt less accepting of death (Figure 2b) and less healthy (Figure 2c). The interaction terms of death acceptance × expected longevity, b = .93, p < .001, and self-rated health × expected longevity, b = −.85, p < .001, significantly predicted the discrepancy between desired and expected longevity. This indicates that individuals who accepted their death, wished for life durations close to their personal expectations, and may thus express a more stoicist attitude toward prolonged longevity. With regard to self-rated health, associations were a bit more complex (Figure 2c). Individuals in relatively good self-rated health seemed to express longevity desires that only slightly exceeded their expectations. Individuals who felt less healthy however, showed more extreme discrepancies between longevity desires and expectations. They wished for much longer lives when they expected to die early, but for much shorter lives when they expected to live a long life. This pattern points to some of the dynamics involved in medicalist mindsets of longevity motivation.
Change and Stability of Desired Longevity and Effects on Health Behavior
To illustrate the malleability of mindsets related to longevity desires and expectations, we explored the rank-order stability and patterns of change within the 4-year longitudinal subsample. For desired longevity, the 4-year stability was r = .57, p < .001. Thereby, 33% wished for the exact same life duration at T1 and T2. Further 36% wished for a shorter life duration at T2 in comparison to T1 with a mean difference of M = −8.5 years (SD = 7.5), and 31% wished for a longer life at T2 compared with T1 (M = +8.2 years, SD = 8.8). For expected longevity, the 4-year stability was clearly higher, r = .79, p < .001. Thereby, 34% expected the exact same life duration at T1 and T2. Further 31% expected a shorter life duration at T2 compared with T1 with a mean difference of −6.44 years (SD = 4.34 years). Another 34% expected a longer life at T2 compared with T1 with a mean difference of +5.91 years (4.78 years). Both measures thus varied over the period of 4 years, however, the extent of variation was larger for desired longevity than for expected longevity. The discrepancy between desired and expected longevity had a 4-year stability of r = .51, p < .001. Most individuals (44%) thereby expressed a stable positive discrepancy (i.e., they wished to live longer than expected at both time points). Further 21% expressed a stable equilibrium (i.e., desired longevity was equal to expected longevity at both time points), and 4% expressed a stable negative discrepancy. Altogether 31% of response patterns involved a change of direction over time (e.g., from wishing to live shorter than expected to wishing to live longer than expected).
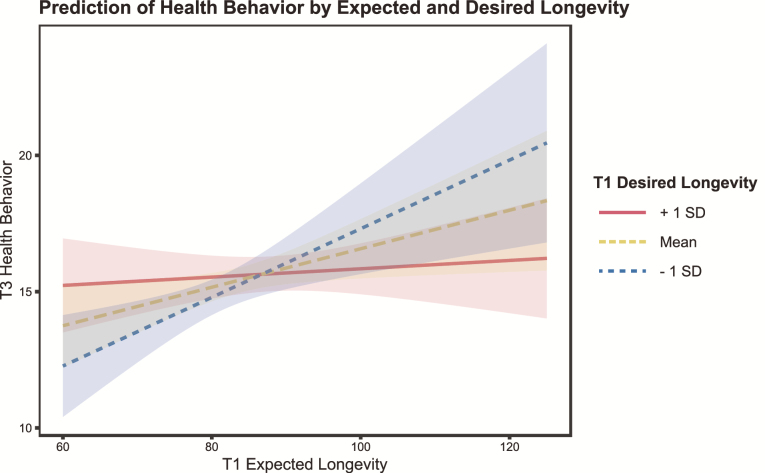
An explorative analysis of this longitudinal data suggested that patterns of desired and expected longevity were associated with changes in health behaviors over 4 years. After controlling for chronological age, gender, education, family status, and the T1 health behavior score, the T3 health behavior score (aggregated over self-reported frequencies of physical activity, healthy nutrition, and an active lifestyle; ranging from 0 to 21; Cronbach’s α = .68) was significantly predicted by an interaction between desired and expected longevity, b = −.57, p = .005. As illustrated in Figure 3, the interaction suggested that health behaviors were most frequent among individuals who desired shorter lives than they expected. On the other hand, when longevity expectations were rather low, a higher desired longevity seemed to motivate individuals to behave in a healthy way.
Figure 3.
Prediction of T2 health behavior by T1 expected longevity and T1 desired longevity.
Conclusion and Future Outlook
To sum up, in accordance with our proposed heuristic model, we observed that the interplay of desired and expected longevity varied depending on culture, death acceptance, and self-rated health as prototypical indicators of determinants. Based on such preliminary findings, future research should include further indications of determinants related to context, health functioning, and personal belief systems to predict mindsets of longevity motivation. Moreover, items explicitly targeting on each of the three mindsets of longevity motivation should be used. In this vein, future research may benefit from including additional indicators of motivation for longevity. In a perfect scenario, items and indicators specifically addressing one of the three mindsets for longevity motivation might be applied. We submit that a more straightforward identification of the three mindsets requires more variables that capture some of the specific characteristics of each profile. Examples might be questions like “If you could, would you want to live forever?” (Cicirelli, 2011) for the essentialist profile, “If you could trade one year in perfect health for ten years in decent health and dependency on the help of others, would you do so?” (Lawton et al., 1999) for the medicalist profile, and “Do you think you will be able to accept your own old age with all its positive and negative aspects, and challenges?” for the stoicist profile.
Finally, across a time interval of 4 years, a substantial number of individuals seemed to change their respective motivation for longevity. According to our heuristic model, one may assume that such changes depend on changes in context, personal beliefs, and health functioning. Further research may investigate the determinants of such changes in longevity motivation in more systematic ways with longitudinal and experimental research designs.
Motivation for longevity and extension of lifetime reflect a new and emerging issue in most modern societies. Not much is known about what motivates individuals at different ages to wish to live a long life under the different circumstances that old age may entail. In an attempt to integrate existing theoretical considerations and empirical findings, we submitted a heuristic model for investigating the determinants and consequences of three mindsets of longevity motivation, that is, an essentialist, medicalist, and stoicist mindset. In an empirical illustration with cross-cultural data, we observed that the interplay of desired and expected longevity was related to effects of culture, self-rated health, and death acceptance. Moreover, preliminary longitudinal data suggests that longevity desires are malleable over time, and also predict changes in health behaviors. Future research may have to make use of more mixed-method designs to also address the possible differences between these mindsets in narrative portrayals, in addition to quantitative indicators. Lastly, it is suggested that the mindsets also have differential behavioral consequences with regard to how individuals invest in late-life preparation and in what ways they want to approach old age.
Funding
This work was supported by a grant of the Volkswagen Foundation [Az 93 273 to F. R. Lang].
Acknowledgment
We are grateful to Franziska Damm for her valuable comments on an earlier version of this article.
Conflict of Interest
None reported.
References
- Ambrosi-Randić N., Nekić M., & Tucak Junaković I (2018). Felt age, desired, and expected lifetime in the context of health, well-being, and successful aging. International Journal of Aging & Human Development, 87, 33–51. doi: 10.1177/0091415017720888 [DOI] [PubMed] [Google Scholar]
- Ayalon L., & King-Kallimanis B. L (2010). Trading years for perfect health: Results from the Health and Retirement Study. Journal of Aging and Health, 22, 1184–1197. doi: 10.1177/0898264310371980 [DOI] [PubMed] [Google Scholar]
- Ballinger S., Tisdale T. C., Sellen D. L., & Martin L. A (2017). Slowing down time: An exploration of personal life extension desirability as it relates to religiosity and specific religious beliefs. Journal of Religion and Health, 56, 171–187. doi: 10.1007/s10943-016-0218-7 [DOI] [PubMed] [Google Scholar]
- Baltes P. B., & Baltes M. M (1990). Psychological perspectives on successful aging: The model of selective optimization with compensation. In Baltes P. B., & Baltes M. M. (Eds.), Successful aging: Perspectives from the behavioral sciences (pp. 1–34). New York: Cambridge University Press. [Google Scholar]
- Baltes P. B., & Smith J (2003). New frontiers in the future of aging: From successful aging of the young old to the dilemmas of the fourth age. Gerontology, 49, 123–135. doi: 10.1159/000067946 [DOI] [PubMed] [Google Scholar]
- Baltes M., Wahl H., & Reichert M (1991). Successful aging in long-term care institutions. In Schaie K. W., & Lawton M. P. (Eds.), Annual review of gerontology and geriatrics (Vol. 11, pp. 311–337). New York: Springer. [Google Scholar]
- Bonanno G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist, 59, 20–28. doi: 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- Bowen C. E., & Skirbekk V. (2017). Old age expectations are related to how long people want to live. Ageing & Society, 37, 1898–1923. doi:10.1017/s0144686x16000726 [Google Scholar]
- Brandstädter J. (1999). Sources of resilience in the aging self: Toward integrating perspectives. In Hess T. M. & Blanchard-Fields F. (Eds.), Social cognition and aging (pp. 123–141). San Dieco, CA: Academic Press. doi: 10.1006/drev.2001.0539 [DOI] [Google Scholar]
- Brandtstädter J., & Wentura D (1994). Veränderungen der Zeit- und Zukunftsperspektive im Übergang zum höheren Erwachsenenalter: Entwicklungspsychologische und differentielle Aspekte. [Changes in time perspectives and attitudes toward the future during the transition to later adulthood: Developmental psychology and differential aspects]. Zeitschrift für Entwicklungspsychologie und Pädagogische Psychologie, 26, 2–21. [Google Scholar]
- Butler R. N. (1975). Why survive? Being old in America. Baltimore: The Johns Hopkins University Press. [Google Scholar]
- Carmel S. (2011). The will to live as an indicator of well-being and predictor of survival in old age. In Poon L. & Cohen-Mansfield J. (Eds.), Understanding well-being in the oldest old (pp. 281–289). New York, NY: Cambridge University Press. doi: 10.1017/CBO9780511920974.017 [DOI] [Google Scholar]
- Carmel S., Baron-Epel O., & Shemy G (2007). The will-to-live and survival at old age: Gender differences. Social Science & Medicine, 65, 518–523. doi: 10.1016/j.socscimed.2007.03.034 [DOI] [PubMed] [Google Scholar]
- Carmel S., & Mutran E (1997). Wishes regarding the use of life-sustaining treatments among elderly persons in Israel: An explanatory model. Social Science & Medicine, 45, 1715–1727. doi:10.1016/s0277-9536(97)00104-4 [DOI] [PubMed] [Google Scholar]
- Cicirelli V. G. (2011). Elders’ attitudes toward extending the healthy life span. Journal of Aging Studies, 25, 84–93. doi: 10.1016/j.jaging.2010.08.011 [DOI] [Google Scholar]
- Cole T. R., & Sierpina M (2007). Humanistic gerontology and the meaning(s) of aging. In Ferraro K. & Vilmoth J. (Eds.), Gerontology: Perspectives and issues (3rd ed., pp. 245–255). New York: Springer. [Google Scholar]
- Ditto P. H., Druley J. A., Moore K. A., Danks J. H., & Smucker W. D (1996). Fates worse than death: The role of valued life activities in health-state evaluations. Health Psychology, 15, 332–343. doi: 10.1037/0278-6133.15.5.332 [DOI] [PubMed] [Google Scholar]
- Donner Y., Fortney K., Calimport S. R., Pfleger K., Shah M., & Betts-LaCroix J (2016). Great desire for extended life and health amongst the American public. Frontiers in Genetics, 6, 353. doi: 10.3389/fgene.2015.00353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekerdt D. J., Koss C. S., Li A., Münch A., Lessenich S., & Fung H. H (2017). Is longevity a value for older adults? Journal of Aging Studies, 43, 46–52. doi: 10.1016/j.jaging.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Erikson E. H. (1959). Identity and the life cycle: Selected papers. Oxford, UK: International Universities Press. [Google Scholar]
- de Grey A. D. (2003). The foreseeability of real anti-aging medicine: Focusing the debate. Experimental Gerontology, 38, 927–934. doi:10.1016/s0531-5565(03)00155-4 [DOI] [PubMed] [Google Scholar]
- Hay S. I., Abajobir A. A., Abate K. H., Abbafati C., Abbas K. M., Abd-Allah F.,…Aboyans V (2017). Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390, 1260–1344. doi: 10.1016/S0140-6736(17)32130-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karppinen H., Laakkonen M. L., Strandberg T. E., Huohvanainen E. A., & Pitkala K. H (2016). Do you want to live to be 100? Answers from older people. Age and Ageing, 45, 543–549. doi: 10.1093/ageing/afw059 [DOI] [PubMed] [Google Scholar]
- Karppinen H., Laakkonen M. L., Strandberg T. E., Tilvis R. S., & Pitkälä K. H (2012). Will-to-live and survival in a 10-year follow-up among older people. Age and Ageing, 41, 789–794. doi: 10.1093/ageing/afs082 [DOI] [PubMed] [Google Scholar]
- Kirkwood T. B. (2005). Understanding the odd science of aging. Cell, 120, 437–447. doi: 10.1016/j.cell.2005.01.027 [DOI] [PubMed] [Google Scholar]
- Kruse A. (2017). Lebensphase hohes Alter. Verletzlichkeit und Reife [Life phase old age. Vulnerability and maturity]. Berlin, Germany: Springer. [Google Scholar]
- Lang F. R., Baltes P. B., & Wagner G. G (2007). Desired lifetime and end-of-life desires across adulthood from 20 to 90: A dual-source information model. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, P268–P276. doi: 10.1093/geronb/62.5.p268 [DOI] [PubMed] [Google Scholar]
- Lang F. R., Rohr M. K., & Williger B (2011). Modeling success in life-span psychology: The principles of selection, optimization, and compensation. In Fingerman K., Berg C., Antonucci T., & Smith J. (eds.), Handbook of lifespan development (pp. 57–85). New York: Springer Publishing Company. [Google Scholar]
- Lawton M. P., Moss M., Hoffman C., Grant R., Ten Have T., & Kleban M. H (1999). Health, valuation of life, and the wish to live. The Gerontologist, 39, 406–416. doi: 10.1093/geront/39.4.406 [DOI] [PubMed] [Google Scholar]
- Lockhart L. K., Bookwala J., Fagerlin A., Coppola K. M., Ditto P. H., Danks J. H., & Smucker W. D (2001). Older adults’ attitudes toward death: Links to perceptions of health and concerns about end-of-life issues. Omega, 43, 331–347. doi: 10.2190/09B5-CCWE-D5GA-F0MA [DOI] [PubMed] [Google Scholar]
- McGlothin P., & Averill M (2008). The CR way. Using the secrets of calorie restriction for a longer, healthier life. New York: HarperCollins Publishers. [Google Scholar]
- More M., & Vita-More N. (Eds.). (2013). The transhumanist reader: Classical and contemporary essays on the science, technology, and philosophy of the human future. Chichester, UK: John Wiley & Sons. doi: 10.1002/9781118555927 [DOI] [Google Scholar]
- Piersol G. M., & Bortz E. L (1939). The aging process: A medical-social problem. Annals of Internal Medicine, 12, 964–977. doi: 10.7326/0003-4819-12-7-964 [DOI] [Google Scholar]
- Rietjens J. A. C., van der Heide A., Voogt E., Onwuteaka-Philipsen B. D., van der Maas P. J., & van der Wal G. (2005). Striving for quality or length at the end-of-life: attitudes of the Dutch general public. Patient Education and Counseling, 59, 158–163. doi:10.1016/j.pec.2004.10.012 [DOI] [PubMed] [Google Scholar]
- Rothermund K., Lang F. L., & Lessenich S (2012). Ageing as future—Future-related activities regarding age and aging in cross-cultural perspective (Unpublished manuscript). University of Jena. [Google Scholar]
- Rowe J. W., & Kahn R. L (1997). Successful aging. The Gerontologist, 37, 433–440. doi: 10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- Shrira A., Carmel S., Tovel H., & Raaveis V. H (2018). Reciprocal relationships between the will-to-live and successful aging. Aging and Mental Health. Advance online publication. doi: 10.1080/13607863.2018.1499011 [DOI] [PubMed] [Google Scholar]
- Steinhauser K. E., Christakis N. A., Clipp E. C., McNeilly M., McIntyre L., & Tulsky J. A (2000). Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA, 284, 2476–2482. doi: 10.1001/jama.284.19.2476 [DOI] [PubMed] [Google Scholar]
- Tesch-Römer C., & Wahl H. W (2017). Toward a more comprehensive concept of successful aging: Disability and care needs. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 310–318. doi: 10.1093/geronb/gbw162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsevat J., Dawson N. V., Wu A. W., Lynn J., Soukup J. R., Cook E. F.,…Phillips R. S (1998). Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project. JAMA, 279, 371–375. doi: 10.1001/jama.279.5.371 [DOI] [PubMed] [Google Scholar]
- Weiss D. (2018). On the inevitability of aging: Essentialist beliefs moderate the impact of negative age stereotypes on older adults’ memory performance and physiological reactivity. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 925–933. doi: 10.1093/geronb/gbw087 [DOI] [PubMed] [Google Scholar]