Abstract
Purpose
Like the classic trabeculectomy, the minimally invasive, ab interno XEN Glaucoma Gel Microstent (XEN‐GGM) creates a filtration bleb in the conjunctiva. The goal of this study was to investigate internal bleb morphology over time with anterior segment optical coherence tomography (AS‐OCT) after XEN‐GGM implantation.
Methods
In a prospective, single‐centre, single‐armed cohort study, blebs were characterized using AS‐OCT in 78 eyes of 60 patients at day 1, at weeks 1 and 2 and at months 1, 3, 6, 9 and 12 after XEN‐GGM implantation in patients with open‐angle glaucoma. Morphological bleb characteristics were correlated with IOP and surgical success.
Results
Anterior segment optical coherence tomography data indicate early and late bleb changes in the course of 12 months. Uniform blebs in AS‐OCTs showed higher IOPs at all examinations between week 1 (17.7 ± 4.8 mmHg versus 11.3 ± 7.1 mmHg, p = 0.001) and month 3 (16.4 ± 6.1 versus 13.4 ± 6.1, p = 0.04). Subconjunctival tissue separation bleb morphology was associated with lower mean IOPs during the course of 12 months (r = −0.75, p = 0.031). Predictors for surgical failure at month 12 were microcystic multiform bleb morphology in AS‐OCT at month 3 (60% versus 15%, relative risk 4.0, p = 0.043) and uniform bleb morphology at month 9 (33% versus 23%, relative risk 1.4, p = 0.015).
Conclusion
Bleb appearance after XEN surgery seems to be different to classic trabeculectomy literature. The present data suggest correlation of IOP and surgical long‐term success with bleb morphology in AS‐OCT. Prevalence of small diffuse cysts is directly associated with lower IOPs, while cystic encapsulation at 3 months predicts higher surgical failure.
Keywords: glaucoma, minimally invasive glaucoma surgery, subconjunctival implant, surgical success, XEN
Introduction
Since its introduction for surgical glaucoma treatment in 1968, much effort was made to improve the performance of trabeculectomy and other filtrating surgical procedures (Cairns 1968). In recent years safe, minimally invasive and effective procedures have been implemented clinically for glaucoma therapy (Saheb & Ahmed 2012; Saheb et al. 2013). In the evolving field of minimally invasive glaucoma surgery (MIGS), the XEN Glaucoma Gel Microstent (XEN‐GGM, Allergan Plc, Parsippany, NJ, USA) is implanted in an ab interno procedure and creates comparable outflow paths like trabeculectomy (Picht & Grehn 1998; Saheb & Ahmed 2012; Mastropasqua et al. 2014; Sheybani et al. 2015; Schlenker et al. 2017). The stent forms filtering blebs, but reduces conjunctival trauma during implantation to a minimum. Both blebs, whether they are formed by an ab interno approach or the classic ab externo trabeculectomy, have similar function, that is to absorb bypassed aqueous humour from the subconjunctival space (Schlenker et al. 2017).
The efficacy of trabeculectomy depends on the existence of an open shunt which delivers aqueous humour to a conjunctival bleb for fluid filtration into the capillary and lymphatic vascular system (Azuara‐Blanco & Katz 1998; Singh et al. 2007). Various grading and classification systems have been developed for clinical examination of blebs in slit lamp biomicroscopy after trabeculectomy (Picht & Grehn 1998; Cantor et al. 2003; Wells et al. 2004). Bleb morphology is not only an important variable for bleb function after trabeculectomy, but also a predictor of bleb‐related complications such as bleb leak, blebitis and bleb‐related endophthalmitis (Picht & Grehn 1998; Hu et al. 2003; Singh et al. 2007). However, the limitation of bleb morphology assessment with slit lamp biomicroscopy is the inability to image internal bleb morphology (Picht & Grehn 1998). Optical coherence tomography (OCT) has become a standard procedure for retinal diagnostics and subsequently for the morphological assessment of other parts of the eye, like the optic nerve head or the anterior segment (Huang et al. 2011). Because of its ability to show intrableb morphology, anterior segment optical coherence tomography (AS‐OCT) has been used for assessment of bleb morphology after trabeculectomy in recent studies (Picht & Grehn 1998; Leung et al. 2007; Singh et al. 2007; Sheybani et al. 2015). With this contact‐free method, interference with bleb morphology and bleb function is minimized. Low bleb wall reflectivity and presence of episcleral fluid have been reported to be associated with lower intraocular pressure (IOP) after trabeculectomy (Picht & Grehn 1998).
Like the classic trabeculectomy, the XEN‐GGM creates a filtration bleb in the conjunctiva as well. However, the bleb follows a minimally invasive, ab interno implantation of a biocompatible gelatine tube. As a consequence, and because of the minimal trauma due to the surgical procedure, one might expect a different bleb appearance in AS‐OCT compared to the classic trabeculectomy. The goal of this study was therefore 1.) to characterize XEN blebs using AS‐OCT in the first year after XEN‐GGM, 2.) to show changes in internal bleb morphology in the first year and 3.) to find predictors in internal bleb morphology for IOP and surgical success.
Materials and Methods
In this prospective, single‐armed, single‐centre, longitudinal clinical trial, patients with open‐angle glaucoma (OAG) and insufficiently controlled IOP or intolerance to topical glaucoma therapy were treated with the XEN‐GGM. Exclusion criteria were angle closure glaucoma, congenital glaucoma, neovascular glaucoma or secondary glaucoma related to uveitis, as well as previous intraocular surgery except of selective laser trabeculoplasty or uncomplicated phacoemulsification with intracapsular lens implantation. The XEN‐GGM implantation was performed with or without combined cataract surgery between 2013 and 2015. Seventy‐eight eyes of 60 patients were enrolled. The study and data accumulation were carried out with prospective approval from the local ethic committees. Informed consents were obtained, and the study was performed according to the tenets of the Declaration of Helsinki.
A single XEN‐GGM was implanted (45 μm inner diameter and total length of 6 mm) in all study eyes (Schlenker et al. 2017). A Mitomycin C (MMC) solution was injected intratenon (4–8 μg, 0.05–0.1 ml) 20 min prior XEN‐GGM surgery using a 30 gauge needle.
Visits were scheduled at baseline (BL), day 1 (D1), week 1 (W1) and week 2 (W2), and months 1 (M1), 3 (M3), 6 (M6), 9 (M9) and 12 (M12) postoperatively. BL demographic data included diagnosis, IOP and number of glaucoma medications. Postoperative visits included IOP, number of glaucoma medications, AS‐OCT of the bleb and anterior chamber depth (ACD).
Anterior segment OCT
At each postoperative visit, all blebs were imaged with a commercially available AS‐OCT (Zeiss Visante OCT; Carl Zeiss Meditec AG, Oberkochen, Deutschland), which has been used commonly for the assessment of filtering blebs after trabeculectomy (Mastropasqua et al. 2014). All patients were asked to look downwards and the lid was retracted carefully without increasing IOP. Figure 1 shows the three scans, which were obtained longitudinally at the same location according to Tominaga et al. for trabeculectomies (Picht & Grehn 1998; Tominaga et al. 2010). Taken together, these three types of scans represent the main areas of filtration in the bleb.
Figure 1.
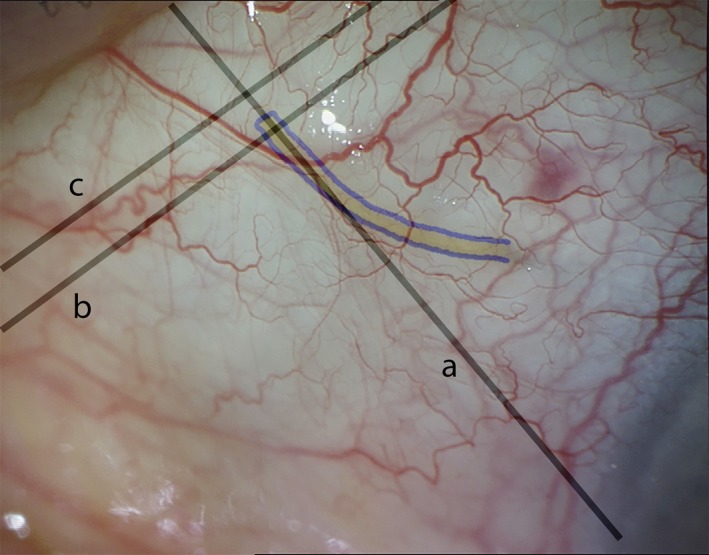
Location of anterior segment optical coherence tomography (AS‐OCT) scans for assessment of bleb morphology after XEN Glaucoma Gel Microstent (XEN‐GGM) implantation. Slit lamp photograph of a bleb 1 week after XEN‐GGM implantation. The XEN‐GGM is highlighted in blue. One scan was obtained radially to the limbus and through the outer part of the XEN‐GGM (a). A second scan perpendicular to the first one was taken to image the subconjunctival part of the XEN‐GGM close to its exit site (b). A third scan was taken parallel and 1 mm posterior to the outer XEN‐GGM lumen through the site of maximal bleb elevation (c).
Classification of bleb morphology
Bleb morphology in AS‐OCT was classified into four groups (see Fig. 2). The classification was carried out on the basis of visibility and position of intraconjunctival fluid‐filled spaces, as shown for trabeculectomy blebs before (Nakano et al. 2010).
Figure 2.
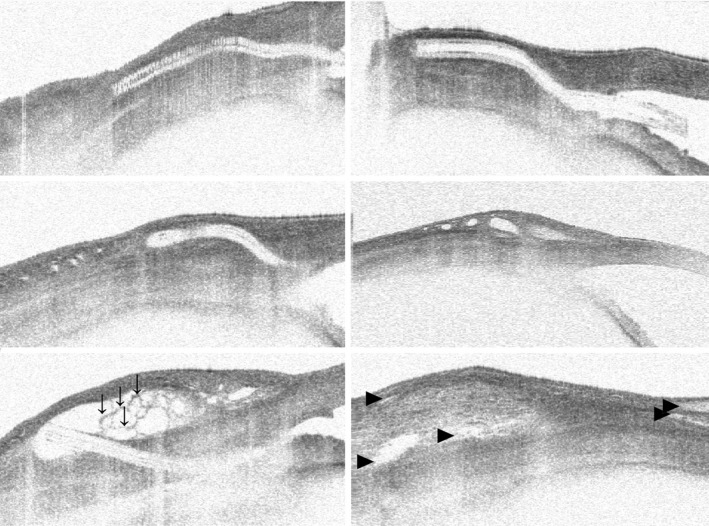
Bleb morphology in anterior segment optical coherence tomography (AS‐OCT) after XEN Glaucoma Gel Microstent implantation. Bleb morphology in AS‐OCT was classified into four groups: 1. uniform (no fluid‐filled hyporeflective spaces in subconjunctival space, top left and top right), 2. subconjunctival separation (multiple small spaces in more superficial layers, middle left and middle right), 3. microcystic multiform (multiple cystic hyporeflective areas in deep layer separated by thin septae, which are highlighted with “↓”; their thicker bleb wall makes the bleb appear encapsulated in AS‐OCT, Bottom left) and 4. multiple internal layer (hyporeflective spaces in deep and superficial layers of conjunctiva with channels of fluid parallel to the surface of the sclera; fluid‐filled spaces highlighted with “►”; bottom right).
Anterior chamber depth
In addition to bleb evaluations, ACD measurements were performed at every visit using AS‐OCT. The ACD was defined as the distance between anterior surface of the cornea and anterior border of the lens capsule.
Definition of surgical success
All patients were classified in two groups according to their medicated IOP at M12 (relative IOP reduction ≥20% compared to baseline defined as surgical success, relative IOP reduction <20% compared to baseline defined as surgical failure). In case of an increase in number of IOP lowering medications compared to baseline, a postoperative IOP <6 mmHg, loss of follow‐up or secondary IOP lowering procedure (except of needling procedures or standard cataract operation), the patient was also classified to the surgical failure group.
Statistical methods
Data were screened for consistency, outliers and continuously distributed variables for normality using probability plots. For analysing bleb morphology in AS‐OCT, McNemar's, Nam's and Wald's Z test, Pearson's chi‐square and the maximum likelihood test were used. Monte Carlo simulation was used to perform the tests in all cross‐tabulation tables. Odds ratios with 95% confidence intervals were also computed. With time series analysis, we assessed the correlations between the mean IOP and the corresponding frequency for a certain bleb morphology in AS‐OCT using a cross‐correlation coefficient with lag k = 0. One‐factorial anovas and mixed models with time as repeated factor were used to analyse IOP and number of medicaments with two‐sided, paired corresponding post hoc tests. A p‐value <5% indicates a statistical significant difference. All analyses were performed using statistica 13 (Hill, T. & Lewicki, P. Statistics: Methods and Applications. StatSoft, Tulsa, OK, USA), pasw 22 (IBM SPSS Statistics for Windows, Version 19.0., Armonk, NY, USA) and statxact 10 (Cytel Software 2013, Cambridge MA, USA).
Results
Study cohort
Thirty‐four right eyes (44%) and 44 left eyes (56%) of 43 female (55%) and 35 male (45%) patients were included in this analysis. In total, 78 eyes of 60 patients were assessed. Forty‐two eyes (54%) had combined cataract surgery and 36 eyes (46%) solo XEN‐GGM procedure. In 24 eyes (31%), pseudoexfoliation glaucoma, in one eye (1%), pigment dispersion glaucoma and in 53 eyes (58%), primary open‐angle glaucoma were present. Mean age was 71.8 years (SD: 11.0) at the operation, with a mean baseline IOP of 23.7 mmHg (SD: 5.4) and a number of 3.1 (SD: 0.9) IOP lowering medications preoperative. Mean central corneal thickness was 530.2 μm (SD: 36.0). In 47 eyes (60%), one or more needlings were performed. In total, 97 needling procedures were performed in the first year. Mean time until first needling after surgery was 137 days (SD: 106). None of the patients was subjected to a second XEN‐GGM implantation.
At each visit, a significant reduction of mean IOP and reduction of mean IOP lowering medications was achieved after XEN‐GGM implantation (Fig. 3, Table 1, each p < 0.001). Mean postoperative IOP ranged from 9.2 mmHg (95%CI 8.1–10.3) at D1 to 15.9 mmHg (95%CI 14.2–17.7) at M9 within the first year postoperatively.
Figure 3.
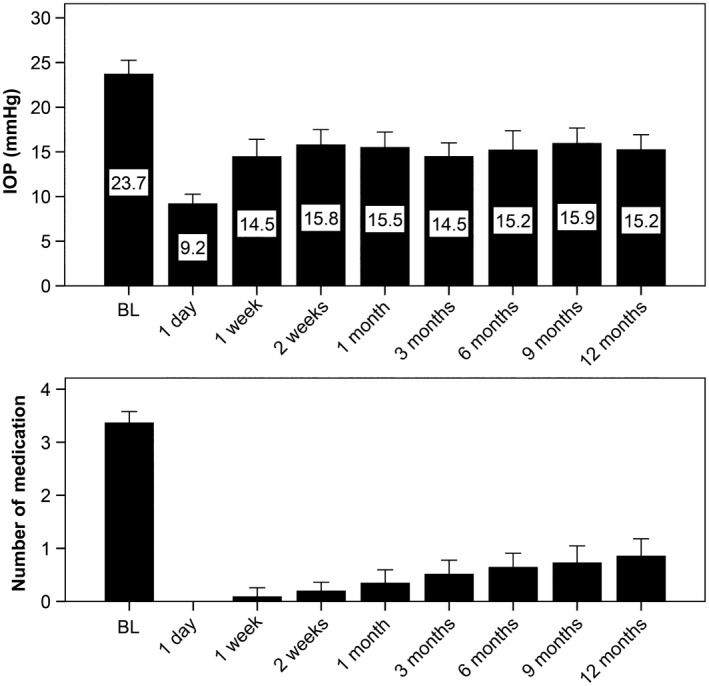
Course of intraocular pressure and number of glaucoma medications after XEN Glaucoma Gel Microstent implantation. Mean intraocular pressure (IOP, Top) ranged from 9.2 at day 1 to 15.9 mmHg at month 9 within the first year postoperatively. A significant mean IOP reduction could be achieved after XEN Glaucoma Gel Microstent implantation at each postoperative visit (each p < 0.001). A significant reduction in number of IOP lowering medications was also detected postoperatively (each p < 0.001, Bottom). Whiskers indicate 95% confidence intervals for means.
Table 1.
Outcome parameters after XEN Glaucoma Gel Microstent implantation in the first year
| IOP (95%CI, mmHg) | Number of glaucoma medications (95%CI) | AS‐OCT morphology | CCT (95%CI, μm) | ACD (95%CI, mm) | ||||
|---|---|---|---|---|---|---|---|---|
| Uniform (IOP ± SD; Meds ± SD) | Microcystic multiform (IOP ± SD; Meds ± SD) | Subconjunctival separation (IOP ± SD; Meds ± SD) | Multiple internal layer (IOP ± SD; Meds ± SD) | |||||
| Baseline | 23.7 (22.1–25.4) | 3.4 (3.2–3.6) | 530.2 (521.0–539.3) | 3.3 (2.8–3.8) | ||||
| Day 1 | 9.2 (8.1–10.3) | 0 (−) | 38% | 12% | 42% | 8% | 3.4 (3.2–3.7) | |
| Week 1 | 14.5 (12.5–16.4) | 0.1 (−0.1–0.3) | 28% | 12% | 40% | 21% | 3.6 (3.3–3.9) | |
| Week 2 | 15.8 (14.1–17.5) | 0.2 (0–0.4) | 48% | 13% | 24% | 15% | 3.5 (3.1–3.8) | |
| Month 1 | 15.5 (14.7–17.2) | 0.3 (0.1–0.6) | 47% | 5% | 32% | 16% | 3.5 (3.3–3.8) | |
| Month 3 | 14.5 (13.0–16.0) | 0.5 (0.2–0.8) | 46% | 9% | 29% | 16% | 3.6 (3.3–3.8) | |
| Month 6 | 15.2 (13.0–17.4) | 0.6 (0.4–0.9) | 52% | 12% | 19% | 16% | 3.6 (3.3–3.8) | |
| Month 9 | 15.9 (14.2–17.7) | 0.7 (0.4–1) | 43% | 24% | 16% | 17% | 3.6 (3.3–3.9) | |
| Month 12 | 15.2 (13.5–16.9) | 0.9 (0.5–1.2) | 27% (18.3 ± 8.0 mmHg; 1.9 ± 1.1) | 24% (16.2 ± 7.0 mmHg; 0.8 ± 1.2) | 22% (14.4 ± 3.5 mmHg; 0.5 ± 0.9) | 27% (14.1 ± 3.6 mmHg; 0.9 ± 1.1) | 3.6 (3.3–3.9) | |
ACD = anterior chamber depth; CCT = central corneal thickness.
Results of outcome parameters in the first year: Mean intraocular pressure (IOP) and mean number of glaucoma medications (Meds), 95% confidence interval (CI); anterior segment optical coherence tomography (AS‐OCT) bleb morphology distribution.
At M12, no differences in IOP between combined cataract versus solo procedure (solo: 14.9 mmHg [95%CI 12.6–17.3] versus combined: 15.3 mmHg [95%CI 13.2–17.3], p = 0.85), presence of pseudoexfoliation (absence: 15.8 mmHg [95%CI 13.7–17.9] versus presence: 13.9 mmHg [95%CI 11.6–16.3], p = 0.24), pigmentary dispersion (absence: 15.0 mmHg [95%CI 13.4–16.6] versus presence: 19.5 mmHg [95%CI 15.0–24.0], p = 0.43), position of the eye (right: 14.5 mmHg [95%CI 13.1–17.9] versus left: 14.5 mmHg [95%CI 12.8–16.3], p = 0.55) and sex (male: 14.1 mmHg [95%CI 12.6–15.7] versus female: 15.8 mmHg [95%CI 13.3–18.2], p = 0.29) were detected. At M12, there were no differences in number of IOP lowering medication between combined cataract versus solo procedure (solo: 1.0 [SD 1.2] versus combined: 0.9 [SD 1.1], p = 0.62), presence of pseudoexfoliation (absence: 1.2 [SD 1.2] versus presence: 0.7 [SD 1.0], p = 0.12), pigmentary dispersion (absence: 0.9 [SD 1.1] versus presence: 3 [SD n/a], p = 0.07), position of the eye (right: 1.0 [SD 1.1] versus left: 0.9 [SD 1.2], p = 0.65) and sex (male: 0.8 [SD 1.1] versus female: 1.1 [1.2], p = 0.44).
Classification of bleb morphology
The distribution of morphological characteristics assessed by AS‐OCT at different visits is shown in Fig. 4. An overview of significant changes in AS‐OCT morphology between visits is listed in Table 2.
Figure 4.
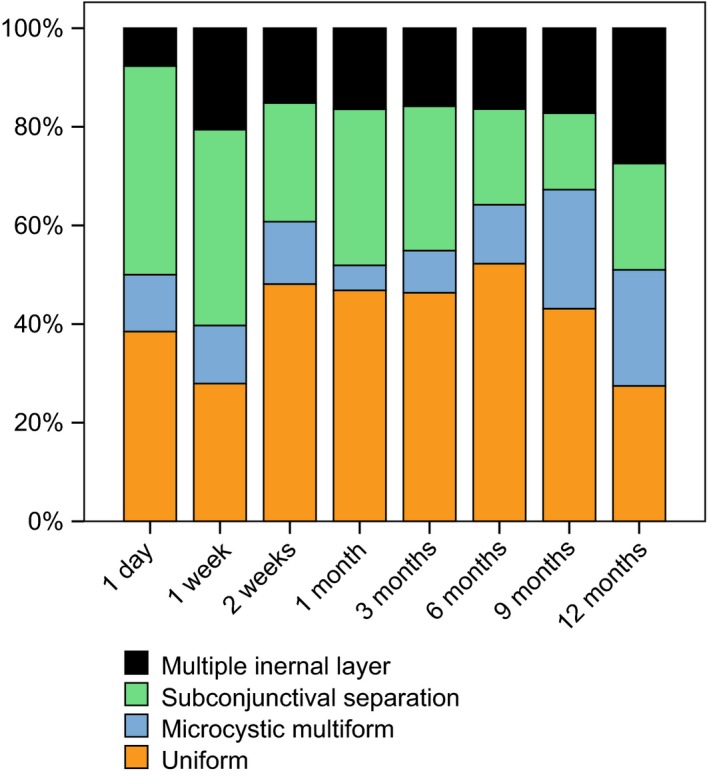
Stacked histograms of bleb morphology in anterior segment optical coherence tomography (AS‐OCT) after XEN Glaucoma Gel Microstent implantation over time. Uniform bleb morphology showed at week 1 (p < 0.004) higher mean intraocular pressure (IOP) compared to the other three morphologies in AS‐OCT separately. Comparing uniform bleb morphology against all other morphologies combined, a statistically significant higher mean intraocular pressure (IOP) was detected in uniform blebs at week 1 (p < 0.001), week 2 (p < 0.001), month 1 (p = 0.005) and month 3 (p = 0.04). A strong negative correlation between the timelines of subconjunctival separation morphology prevalence at all visits in the AS‐OCT and the mean IOP could be shown (r = −0.75, p = 0.031). Significant changes of bleb morphology in AS‐OCT between visits are shown in Table 2.
Table 2.
Changes of anterior segment optical coherence tomography (AS‐OCT) bleb morphology distribution after XEN Glaucoma Gel Microstent implantation in the first year
| Morphology | Early or late change? | Compared visits | Trend | Relative change (ORc) | 95% confidence intervals | p‐Value |
|---|---|---|---|---|---|---|
| Uniform | Early | W1 → W2 | ↑ | 4.3 | 1.3–18 | 0.0124 |
| W1 → M1 | ↑ | 6 | 1.4–37.5 | 0.0075 | ||
| D1 → M6 | ↑ | 5 | 1.2–32 | 0.0209 | ||
| Late | W2 → M12 | ↓ | 0.33 | 0.12–0.88 | 0.025 | |
| M1 → M12 | ↓ | 0.33 | 0.12–0.88 | 0.0253 | ||
| M3 → M12 | ↓ | 0.36 | 0.1–0.99 | 0.0389 | ||
| M6 → M12 | ↓ | 0.1 | 0.005–0.64 | 0.0067 | ||
| M9 → M12 | ↓ | 0.13 | 0.006–0.8 | 0.0196 | ||
| Subconjunctival separation | Early | W1 → W2 | ↓ | 0.29 | 0.09–0.87 | 0.0184 |
| W1 → M1 | ↓ | 0.29 | 0.09–0.87 | 0.0184 | ||
| W1 → M3 | ↓ | 0.5 | 0.17–1.23 | 0.0184a | ||
| Late | W1 → M6 | ↓ | 0.31 | 0.11–0.84 | 0.0164 | |
| W1 → M9 | ↓ | 0.13 | 0.02–0.51 | 0.0016 | ||
| W1 → M12 | ↓ | 0.31 | 0.11–0.84 | 0.0164 | ||
| M3 → M6 | ↓ | 0.22 | 0.03–1 | 0.0348 | ||
| M3 → M9 | ↓ | 0.29 | 0.09–0.87 | 0.0184 | ||
| M3 → M12 | ↓ | 0.33 | 0.1–1.0 | 0.0455 | ||
| Multiple internal layer | Late | D1 → M12 | ↓ | 0.13 | 0.006–0.8 | 0.0196 |
| W1 → M12 | ↑ | 5.5 | 1.3–35 | 0.0126 | ||
| W2 → M12 | ↑ | 5.5 | 1.3–35 | 0.0126 | ||
| M1 → M12 | ↑ | 4.5 | 1.0–29 | 0.0348 | ||
| M3 → M12 | ↑ | Infinity | 2.8‐infinity | 0.0016 | ||
| M9 → M12 | ↑ | 4.5 | 1.0–29 | 0.0348 | ||
| Microcystic multiform | Late | M1 → M9 | ↑ | 4.3 | 1.3–17.8 | 0.0124 |
| M1 → M12 | ↑ | 10 | 1.6–214 | 0.0067 | ||
| M3 → M9 | ↑ | 4.3 | 1.3–17.8 | 0.0124 | ||
| M6 → M9 | ↑ | 4.0 | 0.79–26.2 | 0.033b |
All visits were compared against all visits. Just statically significant results of changes are shown. Clinically significant results are bolded. ↑ indicating an increase in AS‐OCT morphology, ↓ indicating a decrease in AS‐OCT morphology between shown visits.
Nam score test.
Wald Z test without continuity correction.
Odds ratio.
Anterior chamber depth
Mean ACD was not significantly different in one of the morphological categories in AS‐OCT at each visit (Table 1, p = 0.21–0.89). During different postoperative visits, ACD had no influence on success rate at M12 (p = 0.32–0.96).
Correlations with surgical success
Eighty per cent of the patients were classified as surgical success at M12 according to the criteria defined in the methods section. Predictors for surgical failure at M12 were microcystic multiform bleb morphology in AS‐OCT at M3 (60% versus 15%, relative risk 4.0, p = 0.043) and uniform bleb morphology at M9 (33% versus 23%, relative risk 1.4, p = 0.015).
Correlations with IOP
Uniform bleb morphology was associated with higher mean IOPs at W1 to M3 when compared to the other bleb morphologies in AS‐OCT (W1: 17.7 ± 4.8 mmHg versus 11.3 ± 7.1 mmHg, p < 0.001; W2: 18.3 ± 6.1 versus 12.7 ± 4.2, p < 0.001; M1: 16.7 ± 6.3 versus 12.3 ± 4.7, p = 0.005; M3: 16.4 ± 6.1 versus 13.4 ± 6.1, p = 0.04). In contrast to this finding, subconjunctival separation bleb morphology was associated with lower IOPs. In particular, time series analysis showed a strong negative correlation between the timelines of subconjunctival separation morphology prevalence in the AS‐OCT and the mean IOP during the first year postoperative (cross‐correlation with lag 0: r = −0.75, p = 0.031). No further correlations between the timelines of all other morphology prevalence in AS‐OCT and the mean IOP were detected in time series analysis (p = 0.12–0.68).
Discussion
This prospective study describes bleb appearance using AS‐OCT after XEN‐GGM implantation. The XEN‐GGM procedure might distinguish in its intrableb appearance compared to trabeculectomy due to minimally invasiveness. This led to the use of AS‐OCT as a method to characterize intrableb morphology after XEN‐GGM implantation. We here applied an AS‐OCT grading systems known from trabeculectomy studies before (Nakano et al. 2010). Patient baseline characteristics and demographic data of this study were comparable to other studies investigating trabeculectomy blebs with AS‐OCT (Picht & Grehn 1998; Singh et al. 2007; Mastropasqua et al. 2014).
OCT findings
Several studies on the morphology of trabeculectomy blebs using UBM or AS‐OCT have been performed before (Picht & Grehn 1998; Wells et al. 2004; Leung et al. 2007; Singh et al. 2007; Pfenninger et al. 2011) amongst which Nakano et al. showed that 2 weeks after trabeculectomy, 20.8% of the blebs were classified uniform with the same grading algorithm used in the present study (Nakano et al. 2010). Uniform blebs show no fluid cavities or spaces in the conjunctiva. The present data suggest a higher rate of uniform blebs (48%) 2 weeks after XEN‐GGM implantation. Under consideration of good postoperative efficacy, this might be explained by differences in wound healing compared to trabeculectomy because of different degrees of conjunctival trauma.
Development of bleb morphology over time
Bleb morphology changes over time. There are early changes and late changes indicating different phases of bleb maturation.
As shown in Fig. 4, the proportion of subconjunctival separation morphology is highest in the first week and decreases continuously in the course of bleb development over time. This seems feasible because even in a low traumatized tissue, fibrotic reactions in filtration blebs and consequently an increase in outflow resistance are to be expected. Therefore, some of the blebs with a diffuse distribution of small cysts intraconjuntivally loose their appearance to a more homogenous appearance without detectable fluids in AS‐OCT. This is manifested by the increasing proportion of uniform bleb morphology during early bleb development. Changes in the first weeks may be caused by primary fibrotic processes and wound healing response to the low surgical trauma in the area of implantation. Preventing or modulating these changes with antifibrotic treatments may therefore increase outcomes for patients in this phase and should mainly focus on the first 4 weeks postoperatively.
Late bleb morphology in AS‐OCT is distinctly reflected by three different changes. Firstly, a decrease in uniform bleb morphology (in contrast to an increase in the early postoperative phase). Secondly, a further decrease in subconjunctival separation morphology and thirdly, an increase in multiple internal layer morphology. Given the fact that there are late bleb formation processes at 12 months postoperatively seems remarkable and is also reflected in the course of IOP. This late bleb formation process may be caused by secondary capillary and lymphatic vessel ingrowths, which create new intraconjunctival fluid drainage pathways, that is the bleb is getting more structured (Bouhenni et al. 2016). If this secondary bleb formation process does not happen perfectly, bigger cysts may occur: seen as an increase in microcystic multiform morphology in the late phase. Late cystic bleb formation in AS‐OCT therefore may be a dismissed attempt to form fluid paths in the late bleb (Bouhenni et al. 2016). This reflects the decreasing potency of the bleb and is supported by the increasing use of IOP lowering medications during the period of observation.
Relations of IOP and surgical success with bleb morphology
Correlations between bleb morphology and success, function or IOP after trabeculectomy have been shown before: (Wells et al. 2006; Leung et al. 2007; Singh et al. 2007; Tominaga et al. 2010; Mastropasqua et al. 2012; Conlon et al. 2017) due to inconsistent definitions of success, function as well as different time protocols, results in the scientific literature are sometimes contradictory (Mastropasqua et al. 2014). Although Tominaga et al. found a significant positive correlation between bleb wall thickness and IOP, the authors did not show a significant correlation between the height or extent of the filtering bleb and IOP (Picht & Grehn 1998). Independently of this finding, Pfenninger et al. reported a direct correlation between reflectivity of the fluid‐filled cavity and IOP (Pfenninger et al. 2011).
Above‐average bleb performance
Subconjunctival separation bleb morphology in AS‐OCT had lower mean IOPs over the first year, which seems to reflect the OCT characteristic of a well‐functioning early bleb. Diffuse distribution of fluid with small cysts seems to be a sign for less fibrosis and consequently a lower outflow resistance of the bleb.
Below‐average bleb performance
In the present study, uniform blebs show no signs of fluid in AS‐OCT and are associated with higher IOP during the early postoperative phase. They also were predictive for higher surgical failure at M12. Microcystic multiform morphology at M3 was a predictor for higher surgical failure at M12. In contrast, we did not find an early phase predictor for IOP at M12 in AS‐OCT. Subconjunctival separation morphology and microcystic multiform morphology both show signs of fluid in AS‐OCT. Microcystic multiform morphology imposes by its encapsulated appearance which seems responsible for higher IOPs than seen in bleb configuration with higher degrees of subconjunctival separation morphology. The finding at M3 was not surprising, since bleb encapsulations also peak in the first postoperative months of clinical observation.
Based on the present findings, multiple small spaces in superficial layers (subconjunctival separation morphology) form an ideal bleb after XEN‐GGM. On the contrary, no fluid in AS‐OCT or an encapsulated appearance (uniform morphology and microcystic multiform morphology) seems to be inferior signs for prognosis and may demand further interventions (e.g. needlings or increase in IOP lowering medications). Because encapsulation at M3 and dry blebs at M9 seem to be prevalent in surgical failure, this can be interpreted as a difference between early and late bleb formation processes. The additional information gained with AS‐OCT can help the surgeon to better estimate points in time for interventions and also allows for better prediction of long‐term efficacy of the procedure.
Mitomycin C and needlings
As MMC is commonly used for improvement of surgical results in trabeculectomy by reducing fibrosis postoperatively, a foregoing MMC injection might influence bleb morphology after the XEN‐GGM (De Fendi et al. 2013). Although only a low dose (4–8 μg) was applied, all study eyes had a foregoing intratenon injection of MMC, which should be considered when interpreting the results of this study. Needlings are frequently performed after filtrating glaucoma surgery. These procedures affect bleb appearance as well as function and therefore are a limitation of this study. Because of its prospective nature, visiting windows during this study were set in advance and not re‐appointed because of needling procedures. Including data on this basis was a conscious decision by the authors as secondary intervention rate (e.g. 5‐FU injections or needlings) of up to 50% is common after trabeculectomy (Kirwan et al. 2013; Koutsonas et al. 2014). The rather high needling rate in the present study reflects the early experience in the use of this implant. However, the findings suggest a better definition of needling protocols for future studies assessing bleb morphology to allow for better interpretation of future findings.
The present data suggest different intrableb appearance after XEN‐GGM implantation when compared to data from classic trabeculectomy literature. AS‐OCT data indicate early and late bleb changes in the course of 12 months. Bleb efficacy seems to follow bleb morphology and the present data can be helpful in decision‐making for bleb interventions after XEN surgery. Our findings might be helpful to the surgeon to estimate long‐term efficacy of the procedure and can be used to identify patients, which should be followed up in shorter intervals.
This research was supported by the Research Program of Experimental Ophthalmology and Glaucoma Research/Paracelsus Medical University Salzburg, Fuchs Foundation, and Adele Rabensteiner Foundation. HR is consultant to Allergan Plc.
References
- Azuara‐Blanco A & Katz LJ (1998): Dysfunctional filtering blebs. Surv Ophthalmol 43: 93–126. [DOI] [PubMed] [Google Scholar]
- Bouhenni RA, Al Jadaan I, Rassavong H, Al Shahwan S, Al Katan H, Dunmire J, Krasniqi M & Edward DP (2016): Lymphatic and blood vessel density in human conjunctiva after glaucoma filtration surgery. J Glaucoma 25: e35–e38. [DOI] [PubMed] [Google Scholar]
- Cairns JE (1968): Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 66: 673–679. [PubMed] [Google Scholar]
- Cantor LB, Mantravadi A, WuDunn D, Swamynathan K & Cortes A (2003): Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana Bleb Appearance Grading Scale. J Glaucoma 12: 266–271. [DOI] [PubMed] [Google Scholar]
- Conlon R, Saheb H & Ahmed II (2017): Glaucoma treatment trends: a review. Canadian Journal of Ophthalmology. Journal Canadien D'ophtalmologie 52: 114–124. [DOI] [PubMed] [Google Scholar]
- De Fendi LI, Arruda GV, Scott IU & Paula JS (2013): Mitomycin C versus 5‐fluorouracil as an adjunctive treatment for trabeculectomy: a meta‐analysis of randomized clinical trials. Clin Exp Ophthalmol 41: 798–806. [DOI] [PubMed] [Google Scholar]
- Hu CY, Matsuo H, Tomita G, Suzuki Y, Araie M, Shirato S & Tanaka S (2003): Clinical characteristics and leakage of functioning blebs after trabeculectomy with mitomycin‐C in primary glaucoma patients. Ophthalmology 110: 345–352. [DOI] [PubMed] [Google Scholar]
- Huang J, Liu X, Wu Z, Guo X, Xu H, Dustin L & Sadda S (2011): Macular and Retinal Nerve Fiber Layer Thickness Measurements in Normal Eyes With the Stratus OCT, the Cirrus HD‐OCT, and the Topcon 3D OCT‐1000. J Glaucoma 20: 118–125. [DOI] [PubMed] [Google Scholar]
- Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ, McNaught AI & Agrawal P (2013): Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology 120: 2532–2539. [DOI] [PubMed] [Google Scholar]
- Koutsonas A, Remky A & Plange N (2014): [Long‐term results after trabeculectomy with 5‐fluorouracil]. Ophthalmologe 111: 749–756. [DOI] [PubMed] [Google Scholar]
- Leung CK, Yick DW, Kwong YY et al. (2007): Analysis of bleb morphology after trabeculectomy with Visante anterior segment optical coherence tomography. Br J Ophthalmol 91: 340–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastropasqua R, Fasanella V, Agnifili L, Curcio C, Ciancaglini M & Mastropasqua L (2014): Anterior segment optical coherence tomography imaging of conjunctival filtering blebs after glaucoma surgery. Biomed Res Int 2014: 610623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakano N, Hangai M, Nakanishi H, Inoue R, Unoki N, Hirose F, Ojima T & Yoshimura N (2010): Early trabeculectomy bleb walls on anterior‐segment optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 248: 1173–1182. [DOI] [PubMed] [Google Scholar]
- Pfenninger L, Schneider F & Funk J (2011): Internal reflectivity of filtering blebs versus intraocular pressure in patients with recent trabeculectomy. Invest Ophthalmol Vis Sci 52: 2450–2455. [DOI] [PubMed] [Google Scholar]
- Picht G & Grehn F (1998): Classification of filtering blebs in trabeculectomy: biomicroscopy and functionality. Curr Opin Ophthalmol 9: 2–8. [DOI] [PubMed] [Google Scholar]
- Saheb H & Ahmed IIK (2012): Micro‐invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol 23: 96–104. [DOI] [PubMed] [Google Scholar]
- Saheb H, Ianchulev T & Ahmed IIK (2013): Optical coherence tomography of the suprachoroid after CyPass Micro‐Stent implantation for the treatment of open‐angle glaucoma. Br J Ophthalmol 98: 19–23. [DOI] [PubMed] [Google Scholar]
- Schlenker MB, Gulamhusein H, Conrad‐Hengerer I et al. (2017): Efficacy, safety, and risk factors for failure of standalone Ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology 124: 1579–1588. [DOI] [PubMed] [Google Scholar]
- Sheybani A, Reitsamer H & Ahmed IIK (2015): Fluid dynamics of a novel micro‐fistula implant for the surgical treatment of glaucoma. Invest Ophthalmol Vis Sci 56: 4789–4795. [DOI] [PubMed] [Google Scholar]
- Singh M, Chew PT, Friedman DS et al. (2007): Imaging of trabeculectomy blebs using anterior segment optical coherence tomography. Ophthalmology 114: 47–53. [DOI] [PubMed] [Google Scholar]
- Tominaga A, Miki A, Yamazaki Y, Matsushita K & Otori Y (2010): The assessment of the filtering bleb function with anterior segment optical coherence tomography. J Glaucoma 19: 551–555. [DOI] [PubMed] [Google Scholar]
- Wells AP, Crowston JG, Marks J et al. (2004): A pilot study of a system for grading of drainage blebs after glaucoma surgery. J Glaucoma 13: 454–460. [DOI] [PubMed] [Google Scholar]
- Wells AP, Ashraff NN, Hall RC & Purdie G. (2006): Comparison of two clinical Bleb grading systems. Ophthalmology 113: 77–83. [DOI] [PubMed] [Google Scholar]


