Abstract
Cataract is currently the primary cause of blindness worldwide, and one of its main risk factors is solar ultraviolet radiation exposure. According to the localization of lens opacities, three main subtypes of cataract are recognized: nuclear, cortical and posterior subcapsular cataract. One of the main determinants of individual long‐term solar radiation exposure is outdoor work. We systematically reviewed scientific literature from the last 20 years to update the recent development of research on the risk of cataract in outdoor workers and on the specific subtypes involved, also investigating the methods applied to evaluate the occupational risk. A total of 15 studies were included in the review, of which 12 showed a positive association. The studies confirm the relationship of long‐term occupational solar radiation exposure with cortical cataract and give new support for nuclear cataract, although no substantial new data were available to support a relation with the posterior subcapsular subtype. In most of the studies, the exposure assessment was not adequate to support a representative evaluation of the ocular risk; however, outdoor work is clearly a relevant risk factor for cataract. Further research providing a better evaluation of the relation between solar radiation exposure levels and lens damage in workers is needed and aimed to establish adequate occupational exposure limits and better preventive measures, studying also their effectiveness.
Keywords: cortical cataract, nuclear cataract, occupational exposure, posterior subcapsular cataract, solar radiation, ultraviolet radiation
Introduction
Cataract is currently the primary cause of blindness worldwide, responsible for approximately 20 million cases, and the second most prevalent cause of visual impairment, accounting for approximately 81 million of a total number of 246 million cases (Pascolini & Mariotti 2012). Different risk factors are known for this disease, for example diabetes (Xu et al. 2016), but one of the main and most diffused risk factor is long‐term ultraviolet (UV) radiation exposure. Both UV‐A and UV‐B are absorbed by the lens and act with different mechanisms in inducing cataractogenesis, with a progressive chronic photochemical damage (West 1999; Löfgren 2016; Söderberg et al. 2016). The lens nucleus is particularly susceptible to UV‐A‐induced stress, able to determine changes in the lens fluorescence, increased yellowing and loss of pyridine nucleotides (Linetsky et al. 2014), by modulating gene expression and apoptotic stimuli in the lens epithelial cells (Andley et al. 2000, 2004). Considering UV‐B, in animal models, it has been showed that in vivo exposure to subthreshold dose of UV‐B can induce apoptosis in the lens epithelial cells and not in the lens fibre cells (Galichanin 2017).
The two main mechanisms for the induction of cataracts by ocular UV light exposure are oxidative stress and its resultant inflammation (Varma et al. 2011; Øsnes‐Ringen et al. 2013) and phototoxidation that may involve photosensitizers (Roberts 2011). These may be endogenous, as metabolites of inert tryptophan enzymatically modified with age (Balasubramanian 2000) or UV absorbing advanced glycation end products (Ortwerth et al. 1997), or exogenous photosensitizers, for example phototoxic drugs (Roberts 2002). All of these mechanisms produce reactive oxygen species (singlet oxygen and/or superoxide) which oxidize the lens proteins, with a progressive formation of opacities, finally developing into cataracts (Roberts 2011).
By large, the most diffuse source of UV exposure in humans is solar radiation, including the whole range of UV bands, even if the UV‐C and a large part of UV‐B are absorbed in the atmosphere, mainly by the ozone: the reduction in the ozone layer, currently ongoing, is increasing the exposure to UV‐B. Other optical bands included in the solar spectrum also have the potential to cause chronic photochemical lens damage, for example blue light, particularly in the presence of phototoxic drugs, but its role in cataract pathogenesis is less clear (Taylor et al. 1992; Sliney 2011).
Different cataract classifications based on morphological and/or etiological criteria are available, but in epidemiological studies, the most commonly used is the simplified system of three types based on the localization of lens opacities: nuclear cataract is the most frequent form, followed by cortical cataract and posterior subcapsular cataract (Hall et al. 1997; Thylefors et al. 2002). This classification has also been proposed by the World Health Organisation (Thylefors et al. 2002), according to whom a significant number of cataracts can be related to long‐term solar radiation exposure (the upper population attributable fraction of cortical cataract due to solar radiation is 25%). Furthermore, an increasing body of scientific data supports the role of solar radiation in inducing nuclear and posterior subcapsular cataract (World Health Organization 2006). Taken as a whole, this data indicate that a reduction in excessive long‐term solar radiation exposure can lead to the prevention of a significant number of visual impairments and blindness worldwide, and to a consequent parallel reduction in medical costs.
One of the main factors influencing individual long‐term solar radiation exposure is outdoor work (ICNIRP 2010). Outdoor workers are a large occupational group, including farmers, construction workers and others: only in Europe, the estimated number is about 14.5 million (European Agency for Safety and Health at Work 2009; Modenese et al. 2016). Another relevant aspect to be considered is the progressive ageing of the working population: cataract is a multifactorial disease, and its prevalence dramatically increases with age (Taylor 1999; Abraham et al. 2006; Prokofyeva et al. 2013). Thus, solar radiation exposure in outdoor workers may be a relevant factor in increasing the prevalence of cataract and reducing the age of onset.
Nevertheless, this relevant problem has received little, if any, attention, and in various countries (e.g. Italy), this chronic and disabling eye disease is still not included in the national official lists of occupational diseases, as well as the pterygium (Modenese & Gobba 2017).
The aims of this review were to update the knowledge of recent research developments concerning the risk of cataract in outdoor workers, and also on the specific subtypes involved. Furthermore, we also focus on the methods applied to evaluate the occupational risk related to long‐term ocular solar radiation exposure, which constitutes one of the main problems of epidemiological research in this field.
Materials and Methods
An electronic search in accordance with Preferred Reporting Items for Systematic Reviews and MetaAnalyses (Liberati et al. 2009) was performed in the Medline (through PubMed) and Scopus databases. Limiters were set to include scientific literature covering a period of twenty years, from 1st January 1997 to 1st January 2017. The systematic review was limited to original research articles with an available English abstract published in peer‐reviewed journals. Reviews, case reports, comments or letters were not considered.
The following search string was built: [‘cataract’ AND (work* OR job* OR occupation*) AND (‘outdoor’ OR ‘solar radiation’ OR sunlight OR UV)].
Two main types of studies were considered eligible for inclusion, in case of both longitudinal and cross‐sectional designs:
Studies evaluating the presence of cataracts in groups of outdoor workers, or in groups of the general population investigated also for their occupational solar radiation exposure history.
Studies in groups of patients with cataract, investigated for their occupational solar radiation exposure history, or at least classified as mainly outdoor or indoor workers according to their specific job.
In this review, only occupational solar radiation exposure related to outdoor work is considered. According to the European Agency for Safety and Health at Work, outdoor workers are defined as exposed to solar radiation for at least the 75% of their working time, and they are included in a nonexhaustive list of activities: farmers, silviculturists and horticulturists, farm workers, commercial garden and park workers, postmen and sorters, newspaper delivery workers, physical education instructors, trainers, coaches and childcare workers (European Agency for Safety and Health at Work 2009).
Workers exposed to artificial UV, as welders etc., have not been considered in the present review.
In the studies included in this review, solar radiation exposure was assessed using different methods: a) simple qualitative classification according to the general category of ‘outdoor’ and ‘indoor’ work, or according to the job performed, compared to the list of activities of the European Agency; b) more detailed evaluation of occupational solar radiation exposure based on questionnaire data or on measurements. In some group of workers, as military personnel, policemen and drivers, the exposure is highly variable: in these subjects, it is not easy to evaluate the respect of the criterium of the 75% of the working time exposed to solar radiation; accordingly, for these job categories, only studies where exposure was specifically estimated using questionnaires or measurements were included. Another inclusion criterium is the absence of workers possibly exposed to artificial optical radiation sources among controls, that is workers employed in the following sectors according to the European Commission: hot industries, such as glass and metal working; print industries; art and entertainment sector; medical and dentistry sectors in case of use of germicidal lamps, LASER treatments, curing light, cosmetic treatment sector in case of laser or LED/UV‐based treatments, department stores, pharmaceuticals and research sectors, but also sewage treatment sector, using UV germicidal lamps, other research activities involving LASER use, metal working sector involving welding and plastics manufacturing involving LASER bonding, (European Commission, 2011).
Data extraction was performed by one reviewer and checked by another. The extraction was performed by reading all of the available abstracts of the studies returned from the input string in the two databases. Following this, full papers were retrieved for all of the work that met the inclusion criteria. The reference listings of the selected papers were also checked to find other significant research articles.
Results
Study selection
The literature search resulted in 72 items being returned from Medline and 83 from Scopus. After the elimination of duplicates, 116 articles remained. The two authors independently examined the abstracts and agreed on the studies to be included in the review, according to the criteria earlier explained in the Methods section. Resultantly, 12 studies were selected and a further three were identified from the examination of references. A total of 15 studies were included in the review (Fig. 1).
Figure 1.
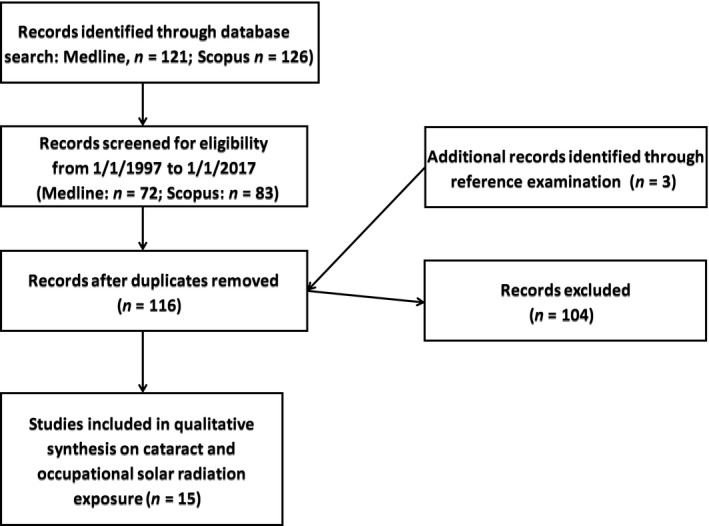
Selection process of the reviewed studies.
Main characteristics of the reviewed studies and cataract frequency in the examined samples
Table 1 shows the main characteristics of the reviewed studies and the cataract frequencies that were reported, also detailing the mention of specific cataract subtypes. Of the fifteen studies reviewed, only one had a longitudinal design (Mukesh et al. 2006). Nine studies were cross‐sectional with a case–control design (Ughade et al. 1998; Neale et al. 2003; Saadat & Farvardin‐Jahromi 2006; Pastor‐Valero et al. 2007; Echebiri et al. 2010; Theodoropoulou et al. 2011; El Chehab et al. 2012; Zarei et al. 2015; Yu et al. 2016). We also included two studies in this group conducted in samples of workers with an exposed/not exposed design (El Chehab et al. 2012; Yu et al. 2016). Another study conducted in workers, but without a control group, was also considered (Cherian et al. 2015). Four cross‐sectional studies were conducted across relatively large samples of the general adult population to evaluate cataract risk factors (Burton et al. 1997; Athanasiov et al. 2008, 2010; Rim et al. 2014). In total, eight studies were conducted in groups of patients with cataract (Ughade et al. 1998; Neale et al. 2003; Mukesh et al. 2006; Saadat & Farvardin‐Jahromi 2006; Pastor‐Valero et al. 2007; Echebiri et al. 2010; Theodoropoulou et al. 2011; Zarei et al. 2015).
Table 1.
Main characteristics of the studies reviewed and cataract frequency in the examined samples
| 1st Author, year | Place | Subjects groupsample size (n)/mean age (years) | Cataract frequency (%) and subtypes considered |
|---|---|---|---|
| Longitudinal | |||
| Mukesh et al. (2006) | Victoria State, south‐east Australia | PtA/2392/62.5 (at baseline) |
Overall 5‐years incidence = 20.9 (ACS) 7.7 (CC) 16.4 (NC) 7 (PSC) |
| Cross‐sectional/Case–control Prevalence | |||
| Yu et al. (2016) | East and West (Tibetans mountains) China | Wo/813/58.1 |
|
| Zarei et al. (2015) | Shiraz, South Iran | PtA/380/62.5 | /(ACS) |
| El Chehab et al. (2012) | Chamonix (mountain) and Lyon (plane), France | Wo/186/59.5 |
|
| Theodoropoulou et al. (2011) | Athens, Greece | PtA/628/n.av. (Range: 46–85) | Subtype frequency (%) among ACS = 66.8 (NC) 14.6 (CC) 19.4 (PSC) |
| Echebiri et al. (2010) | Lagos, south‐west and Kano, north‐central Nigeria | PtA/1060/n.av. (Range: 40–89) | n.av./(ACS) |
| Pastor‐Valero et al. (2007) | Valencia, Spain | PtA/677/66.3 | Subtype frequency (%) among ACS = 30 (NC) 12 (CC) 18.9 (PSC) 39 (mixed) |
| Saadat & Farvardin‐Jahromi (2006) | Shiraz, South Iran | PtA/190/63.9 | n.av./(ACS) |
| Neale et al. (2003) | Brisbane, East Australia | PtA/355/57.9 |
36.8 (ACS) 8 (CC) 28 (NC) 0.6 (PSC) *p based on a sample of 1555 subjects from which the NC cases have been extracted for the study |
| Ughade et al. (1998) | Nagpur, central India | PtA/524/n.av. (Range n.av., majority 51–70) | n.av./(ACS) |
| Cross‐Sectional | |||
| Cherian et al. (2015) | Marakkanam, south India | Wo/331/41.9 | 25.4 (ACS) |
| Rim et al. (2014) | South Korea | GP(A)/11591/58.4 | 40.1 (ACS) 7.4 (CC) 20.3 (NC) 0.3 (PSC) 7.5 (mixed) |
| Athanasiov et al. (2010) | Central Sri Lanka | GP(A)/1375/56.3 | 33.2 (ACS) 26.1 (CC) 4.5 (NC) 8.0 (PSC) |
| Athanasiov et al. (2008) | Central Myanmar | GP(A)/2044/57.9 | 40.4 (ACS) 20.9 (CC) 27.4 (NC) 11.3 (PSC) |
| Burton et al. (1997) | North Pakistan | GP(A)/797/55.6 | 36.3 (ACS); 42.8 in OW (n.s.d) |
ACS = all cataract subtypes, CC = cortical cataract, GP(A) = general population (Adults), NC = nuclear cataract, n.av. = no available data, n.s.d. = no significant difference, OW = outdoor workers, PSC = posterior subcapsular cataract, PtA = patients (Adults), s.d. = significant difference, Wo = workers.
Regarding age, only one study in salt workers (Cherian et al. 2015) included subjects younger than 40 y/o (mean 41.9). The remaining 14 studies were conducted in groups of subjects older than 40, with a mean age between 55 and 60 years in eight studies, between 60 and 65 in two studies and above 65 in one study. In three cases, the mean age data were not available (Table 1).
Considering cataract incidence, evaluated in longitudinal study, an overall 5‐year incidence of all cataract subtypes of 20.9% was reported in a relatively aged group of patients (baseline mean age 62.5) (Mukesh et al. 2006). In this study, the incidence of the different subtypes was 16.4% for nuclear cataract, 7.7% for cortical cataract and 7% for posterior subcapsular cataract.
Considering cataract prevalence in adults of the general population, the range varied from 33.2% in central Sri Lanka (Athanasiov et al. 2010) to 40.4% in central Myanmar (Athanasiov et al. 2008), compared to a prevalence in outdoor workers, ranging from 37.2% in a sample of agricultural workers from Tibet (Yu et al. 2016) to 42.4% in mountain guides from France (El Chehab et al. 2012) and 42.8% in outdoor workers from north Pakistan (Burton et al. 1997). A lower prevalence (25.4%) was reported in a group of younger salt workers in India (Cherian et al. 2015).
Only 9 of the 15 studies evaluated the frequency of the cataract subtypes. Two (Pastor‐Valero et al. 2007; Yu et al. 2016) applied the LOCS II method (Chylack et al. 1989), four (Athanasiov et al. 2008, 2010; El Chehab et al. 2012; Rim et al. 2014) the LOCS III method (Chylack et al. 1993), and three (Neale et al. 2003; Mukesh et al. 2006; Theodoropoulou et al. 2011) used other methods. Furthermore, four studies included ‘mixed type’ cataracts in their classification (Mukesh et al. 2006; Pastor‐Valero et al. 2007; Rim et al. 2014; Yu et al. 2016), while the other studies classified only pure forms (cortical, nuclear and posterior subcapsular).
Nuclear cataract was the most frequent subtype reported in six studies (Neale et al. 2003; Mukesh et al. 2006; Pastor‐Valero et al. 2007; Athanasiov et al. 2008; Theodoropoulou et al. 2011; Rim et al. 2014), with cortical cataract featuring most prominently in the other three (Athanasiov et al. 2010; El Chehab et al. 2012; Yu et al. 2016). Considering subtype prevalence in the general population, the nuclear form ranged from 4.5% in central Sri Lanka (Athanasiov et al. 2010) to 28% in east Australia (Neale et al. 2003), the cortical subtype from 7.4% in South Korea (Rim et al. 2014) to 26.1% (Athanasiov et al. 2010), and posterior subcapsular cataract prevalence ranged from 0.3% (Rim et al. 2014) to 11.3% in central Myanmar (Athanasiov et al. 2008).
The subtype prevalence in outdoor workers was investigated in only two studies (El Chehab et al. 2012; Yu et al. 2016), and with uneven results (Löfgren 2016). In a group of farmers living at low altitude in East China, cortical cataract was the most frequent subtype, but in another group living at high altitude in the Tibetan mountains, mixed types had a much higher prevalence (18% versus 1% for cortical and 1% versus 24% for mixed type, respectively) (Yu et al. 2016). In French mountain guides working at high altitudes, the most frequent subtype was the cortical one (prevalence 30.8%), but the mixed type cataracts were not classified, and the prevalence of nuclear and posterior subcapsular cataracts was, respectively, 3.7 and 2.7% (El Chehab et al. 2012).
Working categories and main methods adopted for occupational solar radiation exposure assessment
Table 2 shows the different working categories with sunlight exposure considered in the reviewed studies, and the main methods adopted to evaluate occupational solar radiation exposure. As anticipated in Table 1, only three studies (El Chehab et al. 2012; Cherian et al. 2015; Yu et al. 2016) were specifically conducted in groups of outdoor workers. Furthermore, all of the studies evaluated occupational Sun exposure using different methods which are scarcely comparable. The methods used to assess occupational solar radiation exposure at work in the collected studies can be classified into five main types:
Table 2.
Occupational solar radiation exposure and cataract
| Main method applied to evaluate solar radiation exposure | Study (1st Author, year) | Working group(s) studied |
|---|---|---|
| Classification of the exposed workers based on their working category (e.g. outdoor versus indoor) | Athanasiov et al. (2008) | Agricultural workers |
| Athanasiov et al. (2010) | Agricultural workers | |
| Cherian et al. (2015) | Salt workers | |
| Mukesh et al. (2006) | Labourers | |
| Saadat & Farvardin‐Jahromi (2006) | Outdoor workers | |
| Zarei et al. (2015) | Outdoor workers | |
| Classification of occupational solar radiation exposure based on a (few) simple question(s) (e.g. how many hours usually spent outdoor per day?) | Ughade et al. (1998) | Outdoor workers |
| Echebiri et al. (2010) | Outdoor workers | |
| Rim et al. (2014) | Agricultural workers, forester, fishermen, labourers | |
| Theodoropoulou et al. (2011) | Outdoor workers (agricultural workers + others) | |
| Evaluation of solar radiation exposure based on environmental data (e.g. UV levels measured with radiometers or obtained from databases) | Burton et al. (1997) | Outdoor workers (AW + LB) |
| Detailed questionnaire‐based solar radiation exposure evaluation (e.g. including information on exposure history and adoption of protective/risky habits) | El Chehab et al. (2012) | Mountain guides |
| Neale et al. (2003) | Outdoor workers | |
| Comprehensive evaluation of solar radiation exposure based on both subjective and objective data (e.g. a detailed questionnaire‐based investigation + environmental data or individual exposure data) | Pastor‐Valero et al. (2007) | Outdoor workers |
| Yu et al. (2016) | Agricultural workers |
Working category: the authors arbitrarily classified activities as solar radiation exposed – outdoor workers or not exposed. This is the most frequently adopted method and features in six of the 15 studies (Mukesh et al. 2006; Saadat & Farvardin‐Jahromi 2006; Athanasiov et al. 2008, 2010; Cherian et al. 2015; Zarei et al. 2015).
Simple question(s): subjects were classified as outdoor workers based on the number of hours usually spent working outdoors, which was assessed with one or a few simple questions (Ughade et al. 1998; Echebiri et al. 2010; Theodoropoulou et al. 2011; Rim et al. 2014).
Environmental data: specific characteristics of the workplace were collected. These included for example the altitude and the presence of UV‐reflecting fresh snow for working in mountain areas; meteorological data on solar radiation (e.g. irradiance); and spot UV measurements (Burton et al. 1997).
Questionnaire‐based evaluation: this group included studies based on detailed questionnaires, aimed to evaluate different aspects of long‐term occupational exposure to solar radiation. Only two such studies were found. In a French study on mountain guides (El Chehab et al. 2012), the questionnaire considered various items, such as the number of days skiing per year, the number of days worked above 5000 m, the percentage of activity between 1000 and 3000 m of altitude, the percentage of activity on snow, the type of eye protection used, and the time wearing protection during working activities. In an Australian study limited to nuclear cataract cases (Neale et al. 2003), exposure during various decades of working life (20–29, 30–39, 40–49, 50–59, >60 years) and the use of protective sunglasses were assessed and the results were merged to classify the subjects into three groups: low, medium or high lifetime solar radiation exposure.
Integrated estimate of the exposure: two studies developed an articulated method to estimate the cumulative long‐term occupational solar radiation exposure, integrating subjective and objective data. A Chinese study (Yu et al. 2016) combined data on the number of hours spent working outdoor, collected by a short questionnaire and also environmental data relating to erythema annual UV irradiance, to build a cumulative exposure index. A Spanish study (Pastor‐Valero et al. 2007) elaborated another example of cumulative exposure index, based on a more detailed subjective evaluation considering the mean number of daily and weekly outdoor working hours, the total number of employment years and the use of protective equipment, and also on collected data on UV environmental irradiance based on measurements performed with dosimeters and meteorological databases.
Results of the association between occupational solar radiation exposure and cataract, considering the main subtypes involved
Table 3 shows the results of the association between occupational solar radiation exposure and cataract, also considering the main subtypes involved.
Table 3.
Main results of the studies reviewed considering occupational solar radiation (SR) exposure and cataract
| 1st Author, year | Results concerning cataract (subtypes) and occupational SRE | Other cataract risk factors considered |
|---|---|---|
| Longitudinal | ||
| Mukesh et al. (2006) | RR(adj) for CC = 2.2 (1.03–4.9) | A, G, DB, SM, ORF (myopia, vitamin intake) |
| Cross‐Sectional/Case–Control | ||
| Yu et al. (2016) |
OR (cr) (ACS) = 2.45 [1.56‐3.81] OR (adj) (ACS) = 2.61 [1.45‐4.67] |
A, G, Edu, SM, AC, ORF (fruit–vegetable intake) |
| Zarei et al. (2015) |
OR (cr) (ACS) = 1.7 [1.0–2.8] ACS* = 2.7 [1.2–6.3] (OW with particular gene polymorphism) |
A, G |
| El Chehab et al. (2012) |
P (ACS, CC): MG (higher) vs controls (p < 0.01) P (NC): MG (lower) vs controls (p < 0.01) OR (cr) Working on snow: ACS = 1.1 [1.03–1.17]; CC = 1.07 [1.01–1.15] Wearing ski mask at work: ACS = 0.5 [0.26–0.96] Working at >3 km: ACS = 1.05 [1.01–1.09]; CC = 1.05 [1.01–1.09] Photochromic lenses: ACS = 0.53 [0.29–0.96];CC=0.47 [0.25–0.9] OtRe: higher frequency of lens micro‐opacities (p < 0.01) and higher lens density (p = 0.01) in MG |
A, G |
| Theodoropoulou et al. (2011) |
OR (adj) (ACS) = 2.03 [1.32–3.12] (CC) = 1.74 [0.77–3.96] (NC) = 1.77 [1.10–2.85] (PSC) = 2.84 [1.41–5.72] |
A, G, SM, BMI, DB, AC, NOSRE, ORF (familiarity, drugs) |
| Echebiri et al. (2010) |
OR (cr) (ACS) = 1.8 [1.5–2.9] in Lagos (urban contest) = 5.9 [4.8–6.9] in Kano (rural contest) |
A, G, SM, Edu; BMI; AC |
| Pastor‐Valero et al. (2007) |
OR (adj) (ACS) = 0.99 [0.57–1.73]; 1.19 [0.69–2.03]a
(NC) = 3.68 [1.50–9.01]; 3.19 [1.24–8.21]a (CC) = 0.67 [0.22–2.00]; 1.19 [0.78–1.09]a (PSC) = 0.57 [0.22–1.45]; 0.57 [0.20–1.60]a |
A, G, SM, AC, Edu, ORF (serum levels of antioxidants) |
| Saadat & Farvardin‐Jahromi (2006) | OR (cr) (ACS) = 1.46 [0.52–4.04]b | A, G |
| Neale et al. (2003) |
OR (cr) (NC) = 2.8 (1.39–5.63)c; 2.18 (1.15–4.11)d
=1.59 (0.84–3.01)e OR (adj) (NC) = 2.9 (1.14–7.6)c; 2.11 (0.74–5.98)d =1.61 (0.70–3.71)e |
A, G, Edu, SM, DB, NOSRE |
| Ughade et al. (1998) |
OR (cr) (ACS) = 2.75 [1.52–4.97] OR (adj) (ACS) = 1.87 [0.94–3.71] |
A, G, BMI, Edu, DB, AC, SM, ORF (glaucoma, myopia, familiarity, drugs) |
| Cross‐Sectional | ||
| Cherian et al. (2015) | P (ACS) = 25.4% | / |
| Rim et al. (2014) |
OR (cr) (ACS) = 6.8 [5.6–8.3]f; 3.6 [2.9–4.4]g
; 1.7 [1.6–1.9]h
OR (adj) (ACS) = 1.1 [0.8–1.4]f; 1.1 [0.8–1.4]g; 1.1 [1.0–1.2]h |
A, G, AC, BMI, DB, SM, Edu, NOSRE |
| Athanasiov et al. (2010) | N.A | A, G, SM, Edu; BMI, DB |
| Athanasiov et al. (2008) |
OR(adj) (ACS) = 0.9 [0.6–1.4]; (NC) = 1.0 [0.6–1.8]; (CC) = 0.70 [0.3–1.7]; (PSC) = 0.9 [0.3–2.9] |
A, G, SM, Edu; BMI |
| Burton et al. (1997) | P (ACS): higher in male OW living in areas with lower UV irradiance (p < 0.00l) | A, BMI |
A = age, AC = alcohol consumption, ACS = all cataract subtypes, AW = agricultural workers, BMI = body mass index, CC = cortical cataract, CI = confidence interval, DB = diabetes, Edu = education, G = gender, LB = labourers, MG = mountain guides, NA = no association, NC = nuclear cataract, NOSRE = nonoccupational solar radiation exposure, OR (adj) = adjusted odd ratio [95% CI], OR (cr) = crude odds ratio [95% CI], ORF = other risk factors (to be specified), OtRe = other results, OW = outdoor workers, P = prevalence, PSC = posterior subcapsular cataract, RR (adj) = adjusted relative risk [95% CI], SM = smoking history, SRE = solar radiation exposure, SW = salt workers.
Considering also the use of protective equipment.
OW with null genotype of glutathione S‐transferase M1 – OR (cr).
Medium exposure group.
High exposure group.
High exposure and low sunglasses use group.
AW + fishermen + forester.
LB.
SRE ≥ 5 hr/day.
All cataract subtypes
Considering all the subtypes of cataract, 12 of the 15 studies found a positive association with occupational solar radiation exposure. In particular, the only longitudinal study (Mukesh et al. 2006) found a positive adjusted relative risk of 2.2 for the general category of outdoor workers defined as ‘labourers’. Three cross‐sectional studies found a significant positive odds ratio (OR) adjusted for various covariates such as age, gender, smoking habit and education (Theodoropoulou et al. 2011; Rim et al. 2014; Yu et al. 2016). The highest OR was of 2.61 for Chinese agricultural workers with a UV annual exposure higher than 2700 joules per square‐metre, based on a semi‐quantitative evaluation (Yu et al. 2016). A Spanish study (Pastor‐Valero et al. 2007) found an adjusted OR of 1.19, considering also the use of protecting equipment, but the confidence interval was not significant. Another four studies (Ughade et al. 1998; Saadat & Farvardin‐Jahromi 2006; Echebiri et al. 2010; Zarei et al. 2015) found positive associations with significant crude ORs ranging from 1.7 (Zarei et al. 2015) to 5.9 (Echebiri et al. 2010). In two studies from Iran (Saadat & Farvardin‐Jahromi 2006; Zarei et al. 2015), a specific association with cataract was found in outdoor workers with particular genetic polymorphisms. A Pakistani study (Burton et al. 1997) showed a higher prevalence of cataract in male outdoor workers (p < 0.001), while a French study (El Chehab et al. 2012) on mountain guides found a higher prevalence of cataracts in these workers (p < 0.01) and also a higher frequency of micro‐opacities of the lens (p < 0.01) and higher lens density (p = 0.01). Only two studies (Athanasiov et al. 2008, 2010) stemmed from the same research group (one conducted in Sri Lanka and one in Myanmar on two large general population groups) found no association between cataract and occupational solar radiation exposure. Finally, an Indian study on salt workers (Cherian et al. 2015) evaluated only the prevalence of cataracts (25.4% in a group of outdoor workers) and did not offer any further possible associations, and an Australian study (Neale et al. 2003) did not consider types of cataracts other than the nuclear forms.
Specific cataract subtypes: nuclear, cortical and posterior subcapsular cataracts
Six studies evaluated the association between nuclear cataract and occupational solar radiation exposure. Three found significant positive adjusted ORs. These ranged from 3.68 in a Spanish study (Pastor‐Valero et al. 2007) (the OR was reduced to 3.19 considering the use of protective equipment), 2.9 for outdoor workers with a medium solar radiation exposure in an Australian study (Neale et al. 2003) and 1.77 in a Greek study (Theodoropoulou et al. 2011). However, in three studies, no association was observed (Athanasiov et al. 2008, 2010; El Chehab et al. 2012).
Five studies evaluated the association between cortical cataract and occupational solar radiation exposure. Two European studies conducted in Spain (Pastor‐Valero et al. 2007) and Greece (Theodoropoulou et al. 2011) found a positive adjusted OR for occupational solar radiation exposure, but the confidence interval was not significant. A French study on mountain guides (El Chehab et al. 2012) found a higher prevalence of cortical cataract compared to the not exposed group (p < 0.01). This subtype was also positively associated with working on snow and with working at an altitude higher than 3,000 metres, respectively, with significant crude ORs of 1.07 and 1.05. Furthermore, the use of photochromic lenses was negatively associated (OR=0.47). In two studies from the same group, no association was observed (Athanasiov et al. 2008, 2010).
Finally, five studies evaluated posterior subcapsular cataract (Pastor‐Valero et al. 2007; Athanasiov et al. 2008, 2010; Theodoropoulou et al. 2011; El Chehab et al. 2012), but only in a Greek study (Theodoropoulou et al. 2011), an adjusted positive OR of 2.84 was found for outdoor workers.
Discussion
General overview of the studies and limitations of the systematic review
The quality of the analysis performed in the studies is rather inhomogeneous, and some weaknesses can be observed. However, considering the scarce number of studies which have been published on the topic, to analyse all the associated literature of interest, we decided not to exclude any pertinent study. Another problem is that the study designs applied by the researchers are quite different and, hence, scarcely comparable. This therefore precludes any possibility of conducting a meta‐analysis. As an example, for the classification of lens opacities, the majority of the studies applied the Lens Opacity Classification System (Chylack et al. 1989, 1993) but used different versions, and a few studies also considered a mixed cataract subtype.
But, the most important cause of inhomogeneity found in the reviewed studies was the method used to evaluate occupational solar radiation exposure. Notably, only two studies had developed a semi‐quantitative index of cumulative exposure (Pastor‐Valero et al. 2007; Yu et al. 2016), and only one considered parameters influencing ocular exposure, such as the use of sunglasses (Pastor‐Valero et al. 2007). All of the other remaining studies classified solar radiation exposure according to different, and scarcely comparable methods, and, in some cases, simply as ‘outdoor’ and ‘indoor’ activities based on a theoretical list. As artificial UV exposure was not considered in this study, any potential occupational exposure in cases, and/or in controls, was considered exclusion criteria.
Another possible problem, not considered in the studies included in this review, is the potential role of occupational eye injuries in cataract induction: this may represent a possible limitation; on the other hand, traumatic cataract is usually related to significant blunt or penetrating ocular trauma that currently are relatively rare in outdoor workers according to our recent data (Gobba et al. 2017).
Associations between cataract, its main subtypes and occupational solar radiation exposure
To discuss the results of our review considering the association between cataract, its main subtypes and occupational solar radiation exposure, we would like to start from the main results of a 2002 review (McCarty & Taylor 2002) that considered 22 epidemiologic studies on humans published from 1977 to 2000. Of these, nine evaluated occupational solar radiation exposure (one of these from Burton et al. (1997) is included also in this review). The conclusions of McCarty & Taylor were that the majority of the epidemiological studies reviewed supported an association between UV‐B and the development of cortical cataract and perhaps posterior subcapsular cataract.
Fifteen years on, the results of our systematic review confirm that there is a solid association between occupational solar radiation exposure in outdoor workers and cataract development. Twelve of the 15 studies found a positive association, and specifically, one longitudinal study found a significant adjusted relative risk in labourers, taking into account also leisure solar radiation exposure (Mukesh et al. 2006), and five studies found positive adjusted ORs for cataract or at least for one subtype (Neale et al. 2003; Pastor‐Valero et al. 2007; Theodoropoulou et al. 2011; Rim et al. 2014; Yu et al. 2016).
Regarding the cataract subtypes, the nuclear form is confirmed to be the most frequent subtype of age‐related cataract, followed by cortical, and with posterior subcapsular as the least frequent. The major recent evidence for a causal relationship between occupational solar radiation exposure and cataract has been found for the nuclear subtype, with three positive adjusted ORs (Neale et al. 2003; Pastor‐Valero et al. 2007; Theodoropoulou et al. 2011), followed by the cortical form with three studies finding positive unadjusted associations (Pastor‐Valero et al. 2007; Theodoropoulou et al. 2011; El Chehab et al. 2012), and posterior subcapsular cataract with a single positive adjusted OR (Theodoropoulou et al. 2011). Considering this, the reviewed data confirm the association between occupational solar radiation exposure and cortical cataract, while new evidence of a relationship between the nuclear subtype and long‐term occupational solar radiation exposure has been added from recent scientific literature. It has to be particularly noted that the oxidative mechanism for the formation of nuclear cataracts differs from that of cortical cataracts: the paper from Neale et al. suggests that the majority of UV‐induced lens damage occurs before 30 years of age in the cortical lens fibres progressively pushed to the centre of the nucleus with the ageing of the lens, supporting the role of a cumulative effect of occupational solar radiation exposure, especially if started at early ages. Finally, the data on PCS are less conclusive: this form is typical, for example, of subjects with a history of chronic use of steroid drugs or with specific ocular comorbidities (Andjelic et al. 2017), while no clear association with outdoor work emerges.
Regarding the prevalence of cataract in outdoor workers, with the exception of the Indian study that included younger workers, in our review, we found prevalence of around 40%. Similar prevalence can be observed in general adult populations living at low latitude in Asia, Africa, South America and Oceania, while in Europe, the prevalence is approximately half (Taylor 1999; McCarty & Taylor 2002; Abraham et al. 2006; WHO 2006; Prokofyeva et al. 2013). This suggests that outdoor work is a relevant factor in influencing the development of cataract in particular where levels of environmental UV irradiance are lower, while its influence is less significant at higher environmental UV levels. This observation is supported by the data of Burton et al., showing a significant association of cataract in outdoor workers living in areas with lower UV irradiance, but not in another group living at high altitude (Burton et al. 1997).
Occupational solar radiation exposure assessment and cataract
One of the main objectives of this review was also to identify the main methods applied to evaluate long‐term ocular exposure to solar radiation in outdoor workers. Unfortunately, we did not find any significant advances in the modelling of cumulative solar radiation exposure assessment, in particular considering the different optical radiation bands that are able to induce photochemical damage of the lens. The methods theorized by McCarty, Rosenthal, Taylor, West and others and applied in various North American and Australian studies in the early 1990s (Taylor 1989; Rosenthal et al. 1991; Taylor et al. 1992; McCarty et al. 1996; West et al. 1998) are still the most precise methods in evaluating long‐term cumulative sunlight exposure, and, in particular, in estimating the UV‐B dose reaching the lens. Only two studies in this review adopted semi‐quantitative methods to evaluate occupational long‐term solar radiation exposure. Yu et al. elaborated a simple cumulative exposure index based on the subjective assessment of the mean daily hours spent outdoors, and the average environmental annual erythema UV exposure based on meteorological databases. However, they did not further consider exposure of the eye and the role of different UV bands. The Spanish study of Pastor‐Valero et al. elaborated a cumulative solar radiation exposure index integrating data from a detailed interview and combined with dosimeter‐based UV environmental irradiance measurements and data from meteorological databases. This study currently offers the most detailed cumulative exposure assessment, even if no measurement of individual ocular exposure considering different UV bands (and including blue light) has been performed. Nevertheless, the strength of the Spanish study (Pastor‐Valero et al. 2007), as well as of the French (El Chehab et al. 2012), the Greek (Theodoropoulou et al. 2011) and the two Australian studies (Neale et al. 2003; Mukesh et al. 2006) included in this review, is the consideration of protective measures, and in particular of the use of sunglasses and their possible role in preventing cataract in outdoor workers. For ocular exposure, albedo (the fraction of solar energy reflected from the Earth) is a relevant phenomenon (International Commission on Non‐Ionizing Radiation Protection, 2010), but only the French study has considered the role of the snow in this respect, reflecting up to 90% of UV rays.
Lastly, and as previously mentioned, the differences in methods used to evaluate occupational solar radiation exposure have limited the possibility of undertaking a more detailed analysis of the relationship between the main factors influencing ocular lens exposure to sunlight (e.g. altitude, reflective surfaces, protective equipment), and the frequency of cataract in outdoor workers.
Conclusions
In our systematic review of the last 20 years of related scientific literature, we found 15 studies evaluating the frequency and association of cataract with occupational solar radiation exposure. A positive association was observed in 12 of these studies, confirming the role of outdoor work as a relevant risk factor for cataract, and so supporting the need to include this disease among occupational diseases for both preventive purposes and also from the perspective of workers’ compensation. The studies also confirm the relation of long‐term occupational solar radiation exposure with cortical cataract but give also new support for nuclear cataract, although no substantial new data have been found on the relation with posterior subcapsular cataract. As a final observation, in the last 20 years, only a few studies concerning cataract in workers exposed to solar radiation have been published, and in most of the studies, the exposure assessment was inadequate for a representative evaluation of the ocular risk, and the classification of the types of cataracts applied is lacking in homogeneity. Another problem is an inadequate/incomplete consideration of known risk factors.
For the abovementioned reasons, there is considerable scope for further research in this field. Among relevant aspects to be considered for a significant advancement of the knowledge in this field, at least the following deserve specific attention:
In the exposure evaluation, lifetime ocular exposure to ultraviolet radiation must be considered, including both occupational and leisure time, possibly integrating objective data available through databases, as local UV Index or other meteorological data, and/or also field measurements, with subjective data obtained from questionnaires.
The individual protective habits that may influence ocular UV exposure must be investigated, including for example frequency of use and characteristics of the hats and sunglasses adopted (shape, types of UV filters, etc.).
Individual relevant clinical information that can integrate the UV exposure history, as a detailed anamnesis on the episodes of skin erythema and sunburns in childhood and as adults, on the intake of photosensitizing drugs (e.g. antibiotics, antimalarials,) and others.
Cataract in future studies deserves a better characterization, for example diagnosis should be based on slit lamp examinations, possibly including also OCT images, and the classification and description of cataract morphology should be standardized using adequate methods, as the LOCS, enabling a better comparison of the evidence.
In our opinion, studies with these characteristics will lead to a better comprehension of the relationship between solar radiation exposure levels and lens damage in outdoor workers, possibly enabling the development of adequate occupational exposure limits and of a more effective prevention.
References
- Abraham AG, Condon NG & West Gower E (2006): The new epidemiology of cataract. Ophthalmol Clin North Am 19: 415–425. [DOI] [PubMed] [Google Scholar]
- Andjelic S, Drašlar K, Hvala A & Hawlina M (2017): Anterior lens epithelium in cataract patients with retinitis pigmentosa—scanning and transmission electron microscopy study. Acta Ophthalmol 95: e212–e220. [DOI] [PubMed] [Google Scholar]
- Andley UP, Song Z, Wawrousek EF, Fleming TP & Bassnett S (2000): Differential protective activity of alpha A‐ and alphaB‐crystallin in lens epithelial cells. J Biol Chem 275: 36823–36831. [DOI] [PubMed] [Google Scholar]
- Andley UP, Patel HC, Xi JH & Bai F (2004): Identification of genes responsive to UV‐A radiation in human lens epithelial cells using complementary DNA microarrays. Photochem Photobiol 80: 61–71. [DOI] [PubMed] [Google Scholar]
- Athanasiov PA, Casson RJ, Sullivan T, Newland HS, Shein WK, Muecke JS, Selva D & Aung T (2008): Cataract in rural Myanmar: prevalence and risk factors from the Meiktila Eye Study. Br J Ophthalmol 92: 1169–1174. [DOI] [PubMed] [Google Scholar]
- Athanasiov PA, Edussuriya K, Senaratne T, Sennanayake S, Sullivan T, Selva D & Casson RJ (2010): Cataract in central Sri Lanka: prevalence and risk factors from the Kandy Eye Study. Ophthalmic Epidemiol 17: 34–40. [DOI] [PubMed] [Google Scholar]
- Balasubramanian D (2000): Ultraviolet radiation and cataract. J Ocul Pharmacol Ther 16: 285–297. [DOI] [PubMed] [Google Scholar]
- Burton M, Fergusson E, Hart A, Knight K, Lary D & Liu C (1997): The prevalence of cataract in two villages of northern Pakistan with different levels of ultraviolet radiation. Eye (Lond) 11: 95–101. [DOI] [PubMed] [Google Scholar]
- Cherian J, Singh Z, Bazroy J, Purty AJ, Natesan M & Chavada VK (2015): Study of morbidity pattern among salt workers in Marakkanam, Tamil Nadu, India. J Clin Diagn Res 9: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chylack LT Jr, Leske MC, McCarthy D, Khu P, Kashiwagi T & Sperduto R (1989): Lens opacities classification system II (LOCS II). Arch Ophthalmol 107: 991–997. [DOI] [PubMed] [Google Scholar]
- Chylack LT Jr, Wolfe JK, Singer DM et al. (1993): The lens opacities classification system III. The longitudinal study of cataract study group. Arch Ophthalmol 111: 831–836. [DOI] [PubMed] [Google Scholar]
- Echebiri SI, Odeigah PG & Myers SN (2010): Case‐control studies and risk factors for cataract in two population studies in Nigeria. Middle East Afr J Ophthalmol 17: 303–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Chehab H, Blein JP, Herry JP et al. (2012): Ocular phototoxicity and altitude among mountain guides. J Fr Ophtalmol 35: 809–815. [DOI] [PubMed] [Google Scholar]
- European Agency for Safety and Health at Work (2009): Outlook 1 – New and emerging risks in occupational safety and health. Luxembourg: Office for Official Publications of the European Communities; Available at: https://osha.europa.eu/en/node/6842/file_view. (Accessed on 5 Sep 2017). [Google Scholar]
- European Commission ‐ Directorate‐General for Employment, Social Affairs and Inclusion Unit B.3 (2011): Non‐binding guide to good practice for implementing Directive 2006/25/EC ‘Artificial Optical Radiation’. Luxembourg: Publications Office of the European Union; Available at: https://publications.europa.eu/it/publication-detail/-/publication/556b55ab-5d1a-4119-8c5a-5be4fd845b68/language-en. (Accessed on 5 Sep 2017). [Google Scholar]
- Galichanin K (2017): Exposure to subthreshold dose of UVR‐B induces apoptosis in the lens epithelial cells and does not in the lens cortical fibre cells. Acta Ophthalmol 95: 834–838. [DOI] [PubMed] [Google Scholar]
- Gobba F, Dall'Olio E, Modenese A, De Maria M, Campi L & Cavallini GM (2017): Work‐related eye injuries: a relevant health problem. main epidemiological data from a highly‐industrialized area of Northern Italy. Int J Environ Res Public Health 14: pii: E604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AB, Thompson JR, Deane JS & Rosenthal AR (1997): LOCS III versus the Oxford clinical cataract classification and grading system for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthalmic Epidemiol 4: 179–194. [DOI] [PubMed] [Google Scholar]
- International Commission on Non‐Ionizing Radiation Protection (2010): ICNIRP Statement. Protection of workers against ultraviolet radiation. Health Phys 99: 66–87. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J et al. (2009): The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151: 65–94. [DOI] [PubMed] [Google Scholar]
- Linetsky M, Raghavan CT, Johar K, Fan X, Monnier VM, Vasavada AR & Nagaraj RH (2014): UVA light‐excited kynurenines oxidize ascorbate and modify lens proteins through the formation of advanced glycation end products: implications for human lens aging and cataract formation. J Biol Chem 289: 17111–17123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löfgren S (2016): Solar ultraviolet radiation cataract (2017). Exp Eye Res 156: 112–116. [DOI] [PubMed] [Google Scholar]
- McCarty CA & Taylor HR (2002): A review of the epidemiologic evidence linking ultraviolet radiation and cataracts. Dev Ophthalmol 35: 21–31. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Lee SE, Livingston PM, Bissinella M & Taylor HR (1996): Ocular exposure to UV‐B in sunlight: the Melbourne visual impairment project model. Bull World Health Organ 74: 353–360. [PMC free article] [PubMed] [Google Scholar]
- Modenese A, Bisegna F, Borra M, Grandi C, Gugliermetti F, Militello A & Gobba F (2016): Outdoor work and solar radiation exposure: Evaluation method for epidemiological studies. Med Pr 67: 577–587. [DOI] [PubMed] [Google Scholar]
- Modenese A & Gobba F (2017): Occupational exposure to solar radiation at different latitudes and pterygium: a systematic review of the last 10 years of scientific literature. Int J Environ Res Public Health 5: E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukesh BN, Le A, Dimitrov PN, Ahmed S, Taylor HR & McCarty CA (2006): Development of cataract and associated risk factors: the Visual Impairment Project. Arch Ophthalmol 124: 79–85. [DOI] [PubMed] [Google Scholar]
- Neale RE, Purdie JL, Hirst LW & Green AC (2003): Sun exposure as a risk factor for nuclear cataract. Epidemiology 14: 707–712. [DOI] [PubMed] [Google Scholar]
- Ortwerth BJ, Prabhakaram M, Nagaraj RH & Linetsky M (1997): The relative UV sensitizer activity of purified advanced glycation endproducts. Photochem Photobiol 65: 666–672. [DOI] [PubMed] [Google Scholar]
- Øsnes‐Ringen O, Azqueta AO, Moe MC, Zetterström C, Røger M, Nicolaissen B & Collins AR (2013): DNA damage in lens epithelium of cataract patients in vivo and ex vivo. Acta Ophthalmol 91: 652–656. [DOI] [PubMed] [Google Scholar]
- Pascolini D & Mariotti SP (2012): Global estimates of visual impairment: 2010. Br J Ophthalmol 96: 614–618. [DOI] [PubMed] [Google Scholar]
- Pastor‐Valero M, Fletcher AE, de Stavola BL & Chaqués‐Alepúz V (2007): Years of sunlight exposure and cataract: a case‐control study in a Mediterranean population. BMC Ophthalmol 7: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokofyeva E, Wegener A & Zrenner E (2013): Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol 91: 395–405. [DOI] [PubMed] [Google Scholar]
- Rim TH, Kim MH, Kim WC, Kim TI & Kim EK (2014): Cataract subtype risk factors identified from the Korea National Health and Nutrition Examination survey 2008‐2010. BMC Ophthalmol 14: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE (2002): Screening for ocular phototoxicity. Int J Toxicol 21: 491–500. [DOI] [PubMed] [Google Scholar]
- Roberts JE (2011): Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens 37: 246–249. [DOI] [PubMed] [Google Scholar]
- Rosenthal FS, West SK, Munoz B, Emmett EA, Strickland PT & Taylor HR (1991): Ocular and facial skin exposure to ultraviolet radiation in sunlight: a personal exposure model with application to a worker population. Health Phys 61: 77–86. [DOI] [PubMed] [Google Scholar]
- Saadat M & Farvardin‐Jahromi M (2006): Occupational sunlight exposure, polymorphism of glutathione S‐transferase M1, and senile cataract risk. Occup Environ Med 63: 503–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliney DH (2011): Intraocular and crystalline lens protection from ultraviolet damage. Eye Contact Lens 37: 250–258. [DOI] [PubMed] [Google Scholar]
- Söderberg PG, Talebizadeh N, Yu Z & Galichanin K (2016): Does infrared or ultraviolet light damage the lens? Eye (Lond) 30: 241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HR (1989): Ultraviolet radiation and the eye: an epidemiologic study. Trans Am Ophthalmol Soc 87: 802–853. [PMC free article] [PubMed] [Google Scholar]
- Taylor HR (1999): Epidemiology of age‐related cataract. Eye (Lond) 13: 445–448. [DOI] [PubMed] [Google Scholar]
- Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB & Bressler NM (1992): The long‐term effects of visible light on the eye. Arch Ophthalmol 110: 99–104. [DOI] [PubMed] [Google Scholar]
- Theodoropoulou S, Theodossiadis P, Samoli E, Vergados I, Lagiou P & Tzonou A (2011): The epidemiology of cataract: a study in Greece. Acta Ophthalmol 89: e167–e173. [DOI] [PubMed] [Google Scholar]
- Thylefors B, Chylack LT Jr, Konyama K, Sasaki K, Sperduto R, Taylor HR & West S, WHO Cataract Grading Group (2002): A simplified cataract grading system. Ophthalmic Epidemiol 9: 83–95. [DOI] [PubMed] [Google Scholar]
- Ughade SN, Zodpey SP & Khanolkar VA (1998): Risk factors for cataract: a case control study. Indian J Ophthalmol 46: 221–227. [PubMed] [Google Scholar]
- Varma SD, Kovtun S & Hegde KR (2011): Role of ultraviolet irradiation and oxidative stress in cataract formation‐medical prevention by nutritional antioxidants and metabolic agonists. Eye Contact Lens 37: 233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West S (1999): Ocular ultraviolet B exposure and lens opacities: a review. J Epidemiol 9: 97–101. [DOI] [PubMed] [Google Scholar]
- West SK, Duncan DD, Muñoz B, Rubin GS, Fried LP, Bandeen‐Roche K & Schein OD (1998): Sunlight exposure and risk of lens opacities in a population‐basedstudy: the Salisbury Eye Evaluation project. JAMA 280: 714–718. [DOI] [PubMed] [Google Scholar]
- WHO (2006): Environmental burden of disease series, No. 13 In: Prüss‐Üstün A, Zeeb H, Mathers C. & Repacholi M. (ed.). Solar ultraviolet radiation: global burden of disease from solar ultraviolet radiation. Geneva: World Health Organization. [Google Scholar]
- Xu X, He J, Xu X et al. (2016): Cataract was the principle cause of visual impairment and blindness in Shanghai residents with type 2 diabetes. Acta Ophthalmol 94: e246–e247. [DOI] [PubMed] [Google Scholar]
- Yu JM, Yang DQ, Wang H et al. (2016): Prevalence and risk factors of lens opacities in rural populations living at two different altitudes in China. Int J Ophthalmol 9: 610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarei N, Saadat I & Farvardin‐Jahromi M (2015): The relationship between NQO1 C609T and CAT C‐262Tgenetic polymorphisms and the risk of age‐related cataracts. Mol Biol Res Commun 4: 143–149. [PMC free article] [PubMed] [Google Scholar]


