Summary
Quality of life after critical illness is becoming increasingly important as survival improves. Various measures have been used to study the quality of life of patients discharged from intensive care. We systematically reviewed validated measures of quality of life and their results. We searched PubMed, CENTRAL, CINAHL, Web of Science and Open Grey for studies of quality of life, measured after discharge from intensive care. We categorised studied populations as: general; restricted to level‐3 care or critical care beyond 5 days; and septic patients. We included quality of life measured at any time after hospital discharge. We identified 48 studies. Thirty‐one studies used the Medical Outcomes Study 36‐Item Short Form Health Survey (SF‐36) and 19 used the EuroQol‐5D (EQ‐5D); eight used both and nine used alternative validated measures. Follow‐up rates ranged from 26–100%. Quality of life after critical care was worse than for age‐ and sex‐matched populations. Quality of life improved for one year after hospital discharge. The aspects of life that improved most were physical function, physical role, vitality and social function. However, these domains were also the least likely to recover to population norms as they were more profoundly affected by critical illness.
Keywords: critical care, intensive care units, quality of life, sepsis
Introduction
Critical illness cared for on an intensive care unit (ICU) imposes a high treatment burden on patients and is an economic burden for the healthcare provider. The short‐term survival of patients admitted to ICUs is well documented through comparative audit systems, such as the UK Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme 1 or the Australia and New Zealand Intensive Care Society (ANZICS) CORE system in Australasia, Oman, India and Hong Kong 2. There is increased interest in studying and quantifying the quality of life of patients as survival after critical illness improves 3. For survivors, the effects of critical illness persist long after hospital discharge. However, health‐related quality of life (HRQoL) data after hospital discharge are not routinely collected on a scale comparable to the national audit programmes. Comparison of these studies is difficult as different measurement tools and assessment times are used. For patients and the healthcare workers advising them, data on quality of life after critical illness informs discussions about treatment choices and expectations. Academics and policymakers need reliable data on quality of life to determine the economic burden of the treatment and long‐term survival following critical illness.
Previous systematic reviews on this topic 4, 5, 6, 7, 8, 9, 10 included studies that are now well over 15 years old, when quality of life was new to ICU outcome research. Existing reviews have systematically examined changes in quality of life after discharge from an ICU. Only limited information on the time course of summary measures has been presented. Many studies used their own (non‐validated) measures that are difficult to compare 5, 6. Studies have reported reduced quality of life after discharge from an ICU compared with the general population, and poor participant retention.
We undertook a systematic review of studies published after 1999 that investigated health‐related quality of life in patients discharged from an ICU. Our aims were to identify the instruments used and to provide a synthesis of data on changes in quality of life after hospital discharge. We have looked for trends in the data, in contrast with previous narrative studies that might have missed some of the nuances of the existing research.
Methods
Our prospectively registered protocol followed the PRISMA guidelines for systematic reviews 11, 12. In brief, we searched PubMed, CENTRAL, CINAHL, the Web of Science and Open Grey for studies of health‐related quality of life (HRQoL) after discharge from an ICU, published in any language from January 2000 to January 2018. Our search terms were: (‘quality of life’ OR ‘qaly’ OR ‘health‐related quality of life’) AND (‘intensive care’ OR ‘icu’ OR ‘critical care’ OR ‘itu’ OR ‘intensive treatment unit’ OR ‘intensive therapy unit’). We searched title, abstracts and key words using MeSH terms where applicable.
We included prospective cohort studies, retrospective cohort studies, case–control studies, cross‐sectional studies and randomised controlled trials (from which we used data from the control group). We restricted included studies to: adults (≥ 16 years); discharged from a general ICU after the year 1999; and quality of life assessments with a validated scale more than 3 months after hospital discharge, for the total cohort or sub‐groups of interest. We did not include studies of a population restricted by age (other than children), disease or category of outcome or uncontrolled interventional studies. One author (AG) extracted study data, which included: study purpose; inclusion and exclusion criteria; number of participants; assessment tools, times, mode and measurements; attrition; sepsis definition; and author competing interests. Two other authors (DY or PW) were consulted to clarify data. We combined quality of life scores for sub‐groups if reported in sufficient detail. We used the Newcastle–Ottawa scale to assess study methodological quality, which generates an aggregate score of 0–8 13. We also subjectively evaluated: inclusion and exclusion criteria; follow‐up rates; participants lost to follow‐up; comparator populations; and competing interests. We did not use quality assessments to exclude studies.
We plotted absolute scores against time and calculated a weighted mean based on the number of replies. For studies that repeated assessments, we calculated and plotted the change in score per month against the time midpoint for that period. We did not correct for multiple testing. Figures were plotted using R Core v3.4.1 14. Where studies reported a normal (reference) population for comparison with means and standard deviations, we compared these with the results for each domain for those discharged from an ICU using an unpaired Student's t‐test. We considered SF‐12 mental component summary and physical component summaries comparable to SF‐36 15. We considered RAND‐36 comparable to SF‐36 in all domains except pain and general health 16. We considered SF‐20 the same as SF‐36 except for vitality and emotional role domains. We categorised studies into one of three sub‐groups, depending on the population: an unselected general cohort of patients discharged from an ICU; a selected cohort that stayed more than 5 days in an ICU 17; or a selected cohort admitted to an ICU with a diagnosis of sepsis.
Results
We identified 11,927 records from which we included 48 studies (Fig. 1 and See Online Supporting Information, Table S1). Fifteen studies scored 6 or more on the Newcastle–Ottawa scale (see also Supporting Information, Appendix S1 and Table S3) 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32. Many of the other studies scored a maximum of 5 due to their cross‐sectional design without comparator. Response rates exceeded 50% in 41 of 48 studies (See Online Supporting Information, Table S1). Response rates were greatest in studies that used an interview for few participants and lowest for studies that sent postal questionnaires to many participants. Assessments were most commonly performed 6 months and 12 months after ICU or hospital discharge.
Figure 1.
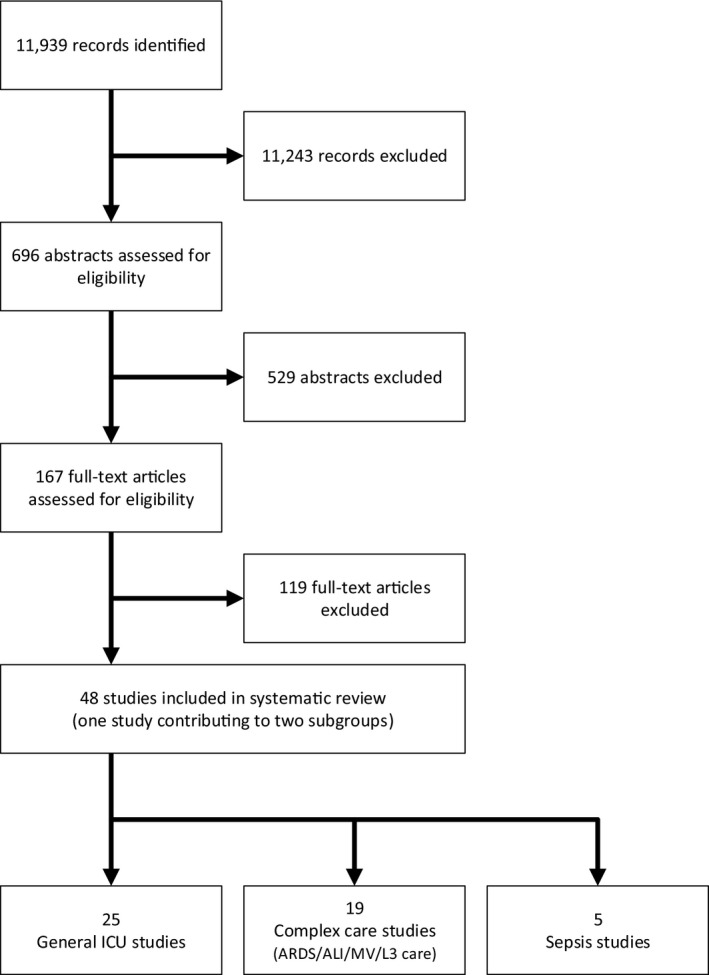
The search of the literature for studies of health‐related quality of life after critical illness and the systematic selection of 48 studies for narrative review.
Twenty‐five studies investigated a general ICU patient cohort 20, 23, 25, 26, 28, 29, 30, 32, 33, 34, 35, 36, 37, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 66. Nineteen studies selected patients who required either level‐3 care or prolonged ICU care 18, 19, 21, 24, 31, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63. Five studies selected patients admitted to an ICU with sepsis 22, 27, 46, 64, 65. One study reported a general patient cohort and those diagnosed with sepsis 46. Thirty studies used the ‘Short Form’ family of surveys (SF‐36, RAND‐36, SF‐20 and SF‐12) 18, 19, 21, 22, 23, 25, 26, 27, 28, 30, 33, 34, 35, 36, 37, 39, 40, 41, 50, 51, 52, 53, 54, 55, 56, 59, 62, 64, 65, 66. Twenty studies used the EQ‐5D; this was more commonly used after 2010 18, 21, 24, 29, 32, 40, 41, 42, 43, 44, 45, 46, 47, 54, 55, 56, 57, 58, 63, 64. Two studies reported Self‐Image Profile 31, 61 and one Nottingham Health Proflie 60. The Quality of Life Spanish 20, RAND‐36 48 and SF‐20 49 tools were each used in one study. Seventeen studies compared their results to a reference population 18, 19, 22, 23, 24, 26, 27, 29, 34, 40, 41, 48, 49, 50, 60, 64, 66. Twenty‐five studies repeated assessments 18, 19, 20, 21, 22, 23, 25, 31, 34, 35, 39, 41, 47, 48, 49, 51, 52, 53, 54, 56, 57, 58, 59, 64, 66. Fifteen studies used the same measure to retrospectively determine quality of life before hospital admission 18, 19, 20, 21, 22, 23, 25, 27, 28, 40, 52, 54, 58, 63, 65.
The estimated quality of life before admission to hospital was always worse than normal for a similar population, except for one study of septic patients. Quality of life remained worse than the reference population in most studies until follow‐up was complete (see also Supporting Information, Table S2), except for the domains of emotional role and mental health, which sometimes fully recovered six or more months after discharge.
Figure 2 summarises the weighted mean domain scores and their change up to 5 years after hospital discharge for populations of general ICU survivors in 14 studies that used the short form (SF) surveys 23, 25, 26, 30, 34, 35, 36, 37, 39, 40, 46, 48, 49, 66. Quality of life was always worse than population norms for all domains except bodily pain. We did not plot results for three studies: two reported median scores 28, 33, and the results in one study were inconsistent with their methods 67. Mean physical function, physical role, vitality and social function always improved during the first 6 months after hospital discharge, whereas the summary of physical components and mental components changed little. One study reported the Quality of Life in Spanish without reference to population norms, with findings similar to the SF surveys 20. Figure 3 summarises the equivalent scores for 10 studies that used the EQ‐5D‐3L and EQ VAS up to 12 months after hospital discharge 29, 32, 40, 41, 42, 43, 44, 45, 46, 47. Two studies reported more than one time‐point 41, 47, one of which reported improved scores with time.
Figure 2.
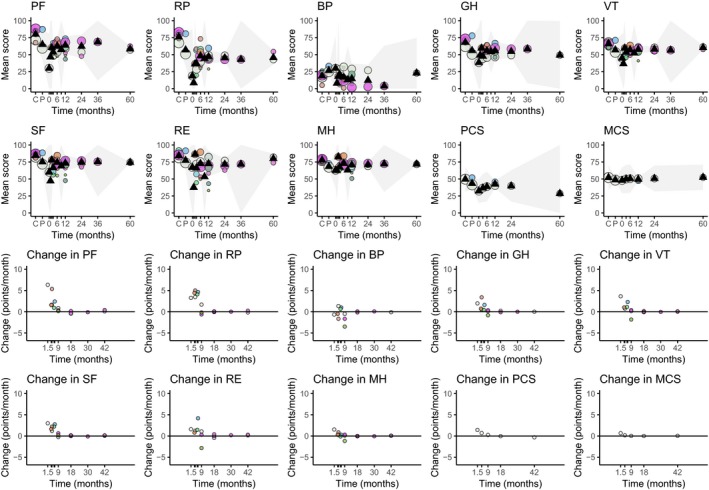
General ICU population – bubble plots of mean SF36v2 domain score against time (top two rows) and change in score against time (bottom two rows). Black triangles denote the weighted mean at each time‐point, the grey overlay denotes the 95%CI of the weighted mean (where calculable). Each colour represents a different study with circle area proportional to the number of participants. Headers: PF, physical functioning; RP, physical role functioning; BP, bodily pain; GH, general health perceptions; VT, vitality; SF, social role functioning; RE, emotional role functioning; MH, mental health; PCS, physical component score; MCS, mental component score. C, control; P, before ICU.
Figure 3.
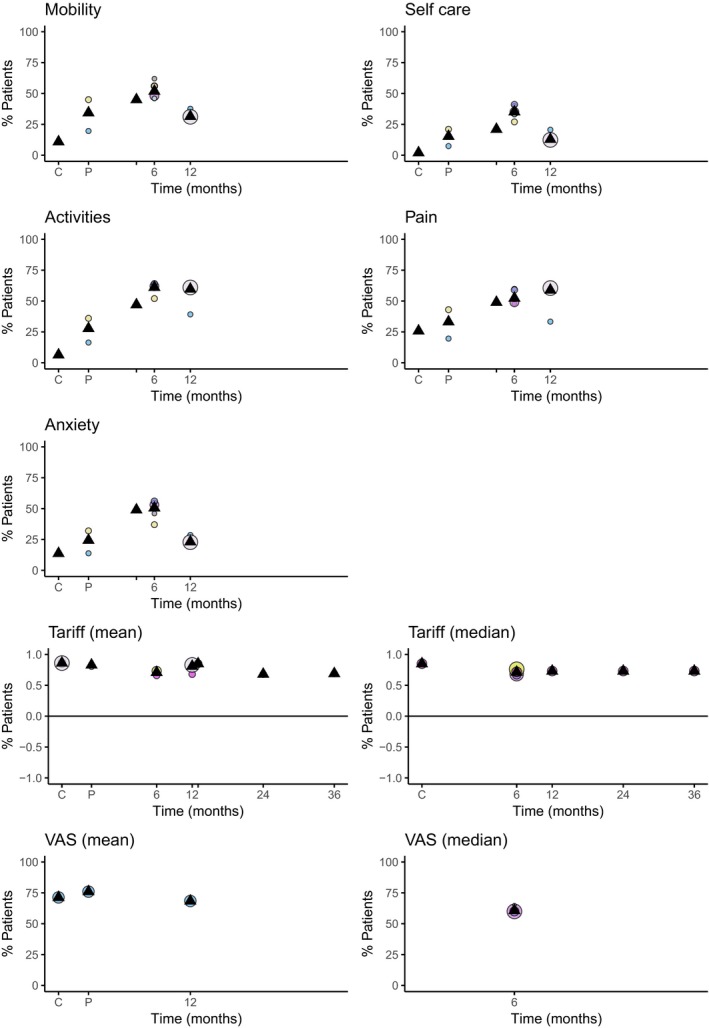
General ICU population – bubble plots of the percentage of participants reporting problems in answer to each EQ‐5D domain and the corresponding mean or median EQ‐5D tariff score and visual analogue scale against time. Black triangles denote the weighted mean at each time‐point. Each colour represents a different study with circle area proportional to the number of participants. C, control; P, before ICU.
Supplementary Information (Fig. S1) summarises the weighted mean domain scores and their change up to 5 years after hospital discharge for populations of patients requiring complex care in 12 studies that used the SF surveys 18, 19, 21, 50, 51, 52, 53, 54, 55, 56, 59, 61. Quality of life was always worse than population norms, including before hospital admission. Mean physical function, physical role, vitality and social function generally improved in the first 5 months after discharge. Supplementary Information (Fig. S2) summarises the equivalent scores for nine studies that used the EQ‐5D up to 12 months after hospital discharge 18, 21, 24, 54, 55, 56, 57, 58, 63. Population domain norms were not reported. Quality of life, in domains other than anxiety and depression, improved after discharge, except in two studies that reported EQ‐5D‐3L index scores 18, 56, neither of which reported changes with time. The EQ‐5D‐VAS was reported in three studies, one of which reported an improvement in quality of life with time 54. Quality of life remained worse than population norms 18, 24, 63.
Supplementary Information (Fig. S3) summarises the weighted mean domain scores and their change between 6 months and 5 years after hospital discharge for populations of septic patients in four studies that used the SF surveys 22, 27, 64, 65. Quality of life was always worse than population norms, except for Total Body Pain. Physical function, physical role and social function improved within 5 months of discharge. Quality of life did not improve 42–60 months after discharge 64. Two studies used EQ‐5D 46, 64. One 18 reported multiple time‐points and showed no improvement with time. No comparisons were made with population controls or pre‐hospital assessment in EQ‐5D domains.
Discussion
In this systematic review, patients surviving critical illness had worse health‐related quality of life when compared with population norms. Quality of life incompletely recovered after hospital discharge. This was consistent for populations with heterogeneous critical illnesses, septic populations and populations ventilated for more than 5 days.
Some systematic reviews have suggested that health‐related quality of life may return to population norms more than one year after discharge, whereas others have not 68, 69, 70. Three papers that we did not include, two of which preceded 2000 and the other took a long time to recruit participants, have suggested that most survivors have a good quality of life 1–6 years after hospital discharge 71, 72, 73. It has also been suggested that septic populations and those with prolonged critical care have worse quality of life than other patients discharged from critical care 9. Our paper does not support either contention. Our study suggests that the greatest health improvements occur in the first year after discharge from hospital, with little further improvement for all sub‐groups and in all health domains. This suggests that interventions to improve health after critical illness might be most effective in the first year after hospital discharge.
Health‐related quality of life scores for populations, had they not been critically ill, are usually estimated from population norms, provided by copyright holders for the EuroQoL or Short Forms, or from survivors trying to remember their health before they became critically unwell. The weakness of using population norms is that they do not account for pre‐existing morbidity. The accuracy of recalled health is uncertain, although it might be reasonable up to 3 months after hospital discharge 74. In our review, health before critical illness recalled by patients was worse than population norms. This suggests that much of the ‘failure to recover’ (to population norms) indicates recovery to pre‐existing chronic illness by patients who overestimated their previous quality of life. However, critical illness is likely to permanently worsen the health of patients with chronic disease 41. The most appropriate comparison group varies with the purpose of the comparison. The development of interventions to improve health‐related quality of life would be informed by the net change in the health of large cohorts of patients who have survived critical illness. Healthcare economics would be better informed by gross changes in health. Population norms are most useful in identifying the domains of health that are most affected by critical illness.
There is increasing emphasis on the psychological sequelae of admission to intensive care 38, 75, 76, 77, 78. In general, critical illness affects psychological health less than physical health and therefore can improve less after hospital discharge. Interventions to improve health after critical illness might be more successful for physical health than psychological health and sample size calculations for clinical trials should incorporate smaller effect sizes for psychological interventions.
Two factors that might limit the applicability of our findings are the high mortality from critical illness and the loss of many patients during follow‐up. We think that the high mortality rate – relative to the general population – does not inherently bias our results, providing that mortality is accurately and independently tracked. Health probably affects patient participation during months and years of follow‐up: the health of participants under surveillance might be better than the health of participants lost to surveillance. Only half of the studies in our review compared health with a reference population, whereas comparison with a large cohort who had survived critical illness was not used by any study, which we think would be the most helpful comparison. We felt that the variety of tools used to measure health‐related quality of life precluded quantitative pooling of results.
Future research should report SF‐36 as one measure of health‐related quality of life after critical illness, as it would allow comparison with most published studies, repeated within the first year to capture most of the change in quality of life that might be affected by interventions. Methods should be developed to better establish quality of life before critical illness and to adjust for pre‐existing disease.
In conclusion, health‐related quality of life after critical illness was most often measured with SF‐36. Quality of life after critical illness was worse than age‐ and sex‐matched norms. Improvements in quality of life occurred in the first year after discharge in four domains: physical function; physical role; vitality and social function. Interventions to aid recovery after critical illness are most likely to have an effect in the first year after hospital discharge.
Supporting information
Figure S1. Bubble plots of mean domain score against time and change (expressed in points per month) against time.
Figure S2. Bubble plots of the percentage of people reporting problems in answer to each EQ‐5D domain and the corresponding mean or median EQ‐5D tariff score and visual analogue scale against time.
Figure S3. Bubble plots of mean domain score against time and change (expressed in points per month) against time.
Table S1. Papers investigating a health‐related quality of life after critical illness, arranged by: population studied; assessment tool and then alphabetically.
Table S2. Time points with scores significantly different from population comparisons.
Table S3. Newcastle–Ottawa Score for cohort studies.
Appendix S1. Newcastle–Ottawa quality assessment scale for cohort studies.
Appendix S2. PubMed search.
Acknowledgements
We thank S. Dutton, Lead Medical Statistician for Oxford Clinical Trials Research Unit, T. Petrinic, Outreach Librarian, University of Oxford Cairns Library, John Radcliffe Hospital Oxford and V. Westgate for proof‐reading and improving the wording of the manuscript. No conflicts of interest are declared. This review is registered on the PROSPERO database (CRD42015024700).
You can respond to this article at http://www.anaesthesiacorrespondence.com
References
- 1. Harrison DA, Brady AR, Rowan K. Case mix, outcome and length of stay for admissions to adult, general critical care units in England, Wales and Northern Ireland: the Intensive Care National Audit & Research Centre Case Mix Programme Database. Critical Care 2004; 8: R99–R111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hart GK. The ANZICS CORE: an evolution in registry activities for intensive care in Australia and New Zealand. Critical Care and Resuscitation 2008; 10: 83–8. [PubMed] [Google Scholar]
- 3. Intensive Care Society . Guidelines for the provision of intensive care services. 2016. Url: https://www.ficm.ac.uk/sites/default/files/gpics_ed.1.1_-_2016_-_final_with_covers.pdf. Last accessed 14/07/18.
- 4. Adamson H. Quality of life after a critical illness : a review of the literature 1998–2003. Master Thesis, University of Sydney 2004; 18: 1–91. [Google Scholar]
- 5. Chaboyer W, Elliott D. Health‐related quality of life of ICU survivors: review of the literature. Intensive and Critical Care Nursing 2000; 16: 88–97. [DOI] [PubMed] [Google Scholar]
- 6. Elliott D. Measuring the health outcomes of general ICU patients: a systematic review of methods and findings. Australian Critical Care 1999; 12: 132–40. [DOI] [PubMed] [Google Scholar]
- 7. Hayes JA, Black NA, Jenkinson C, et al. Outcome measures for adult critical care: a systematic review. Health Technology Assessment 2000; 4: 1–111. [PubMed] [Google Scholar]
- 8. Black NA, Jenkinson C, Hayes JA, et al. Review of outcome measures used in adult critical care. Critical Care Medicine 2001; 29: 2119–24. [DOI] [PubMed] [Google Scholar]
- 9. Oeyen SG, Vandijck DM, Benoit DD, Annemans L, Decruyenaere JM. Quality of life after intensive care: a systematic review of the literature. Critical Care Medicine 2010; 38: 2386–400. [DOI] [PubMed] [Google Scholar]
- 10. Dowdy DW, Eid MP, Sedrakyan A, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Medicine 2005; 31: 611–20. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. British Medical Journal 2009; 339: b2535. [PMC free article] [PubMed] [Google Scholar]
- 12. Gerth AM, Watkinson PJ, Young JD. Changes in health‐related quality of life (HRQoL) after discharge from intensive care unit: a protocol for a systematic review. British Medical Journal Open 2015; 5: e009508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wells G, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Third Symposium on Systematic Reviews: Beyond the Basics. Oxford, July 2000. 2000. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 20/12/2016).
- 14. R core team . R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. http://www.r-project.org. [Google Scholar]
- 15. Lacson E, Xu J, Lin SF, Dean SG, Lazarus JM, Hakim RM. A comparison of SF‐36 and SF‐12 composite scores and subsequent hospitalization and mortality risks in long‐term dialysis patients. Clinical Journal of the American Society of Nephrology 2010; 5: 252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hays RD, Sherbourne CD, Mazel RM. The rand 36‐item health survey 1.0. Health Economics 1993; 2: 217–27. [DOI] [PubMed] [Google Scholar]
- 17. Valentin A, Ferdinande P, ESICM Working Group on Quality Improvement . Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Medicine 2011; 37: 1575–87. [DOI] [PubMed] [Google Scholar]
- 18. Cuthbertson BH, Roughton S, Jenkinson D, MacLennan G, Vale L. Quality of life in the five years after intensive care: a cohort study. Critical Care 2010; 14: R6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Denehy L, Skinner EH, Edbrooke L, et al. Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months of follow‐up. Critical Care 2013; 17: R156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fildissis G, Zidianakis V, Tsigou E, et al. Quality of life outcome of critical care survivors eighteen months after discharge from intensive care. Croatian Medical Journal 2007; 48: 814–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Griffiths J, Hatch RA, Bishop J, et al. An exploration of social and economic outcome and associated health‐related quality of life after critical illness in general intensive care unit survivors: a 12‐month follow‐up study. Critical Care 2013; 17: R100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hofhuis JG, Spronk PE, van Stel HF, Schrijvers AJ, Rommes JH, Bakker J. The impact of severe sepsis on health‐related quality of life: a long‐term follow‐up study. Anesthesia and Analgesia 2008; 107: 1957–64. [DOI] [PubMed] [Google Scholar]
- 23. Hofhuis JGM, van Stel HF, Schrijvers AJP, Rommes JH, Spronk PE. ICU survivors show no decline in health‐related quality of life after 5 years. Intensive Care Medicine 2015; 41: 495–504. [DOI] [PubMed] [Google Scholar]
- 24. Linko R, Suojaranta‐Ylinen R, Karlsson S, Ruokonen E, Varpula T, Pettilä V; FINNALI study investigators . One‐year mortality, quality of life and predicted life‐time cost‐utility in critically ill patients with acute respiratory failure. Critical Care 2010; 14: R60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Myhren H, Ekeberg Ø, Stokland O. Health‐related quality of life and return to work after critical illness in general intensive care unit patients: a 1‐year follow‐up study. Critical Care Medicine 2010; 38: 1554–61. [DOI] [PubMed] [Google Scholar]
- 26. McKinley S, Fien M, Elliott R, Elliott D. Health‐related quality of life and associated factors in intensive care unit survivors 6 months after discharge. American Journal of Critical Care 2016; 25: 52–8. [DOI] [PubMed] [Google Scholar]
- 27. Nesseler N, Defontaine A, Launey Y, Morcet J, Mallédant Y, Seguin P. Long‐term mortality and quality of life after septic shock: a follow‐up observational study. Intensive Care Medicine 2013; 39: 881–8. [DOI] [PubMed] [Google Scholar]
- 28. Skinner EH, Warrillow S, Denehy L. Health‐related quality of life in Australian survivors of critical illness. Critical Care Medicine 2011; 39: 1896–905. [DOI] [PubMed] [Google Scholar]
- 29. Soliman IW, de Lange DW, Peelen LM, et al. Single‐center large‐cohort study into quality of life in Dutch intensive care unit subgroups, 1 year after admission, using EuroQoL EQ‐6D‐3L. Journal of Critical Care 2015; 30: 181–6. [DOI] [PubMed] [Google Scholar]
- 30. van der Schaaf M, Beelen A, Dongelmans DA, Vroom MB, Nollet F. Functional status after intensive care: a challenge for rehabilitation professionals to improve outcome. Journal of Rehabilitation Medicine 2009; 41: 360–6. [DOI] [PubMed] [Google Scholar]
- 31. van der Schaaf M, Beelen A, Dongelmans DA, Vroom MB, Nollet F. Poor functional recovery after a critical illness: a longitudinal study. Journal of Rehabilitation Medicine 2009; 41: 1041–8. [DOI] [PubMed] [Google Scholar]
- 32. Wolters AE, van Dijk D, Pasma W, et al. Long‐term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort study. Critical Care 2014; 18: R125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abelha FJ, Santos CC, Maia PC, Castro MA, Barros H. Quality of life after stay in surgical intensive care unit. BMC Anesthesiology 2007; 7: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Boyle M, Murgo M, Adamson H, Gill J, Elliott D, Crawford M. The effect of chronic pain on health related quality of life amongst intensive care survivors. Australian Critical Care 2004; 17: 104–13. [DOI] [PubMed] [Google Scholar]
- 35. Chaboyer W, Foster M, Creamer J. Health status of ICU survivors: a pilot study. Australian Critical Care 2002; 15: 21–6. [DOI] [PubMed] [Google Scholar]
- 36. Karachi F, Hanekom S, Faure M. Health‐related quality of life of patients 12 months following surgical intensive care discharge. South African Journal of Physiotherapy 2011; 67: 28–34. [Google Scholar]
- 37. Khoudri I, Ali Zeggwagh A, Abidi K, Madani N, Abouqal R. Measurement properties of the short form 36 and health‐related quality of life after intensive care in Morocco. Acta Anaesthesiologica Scandinavica 2007; 51: 189–97. [DOI] [PubMed] [Google Scholar]
- 38. Sukantarat KT, Williamson RCN, Brett SJ. Psychological assessment of ICU survivors: a comparison between the Hospital Anxiety and Depression scale and the Depression. Anxiety and Stress Scale. Anaesthesia 2007; 62: 239–43. [DOI] [PubMed] [Google Scholar]
- 39. Svenningsen H, Tønnesen EK, Videbech P, Frydenberg M, Christensen D, Egerod I. Intensive care delirium – effect on memories and health‐related quality of life – a follow‐up study. Journal of Clinical Nursing 2014; 23: 634–44. [DOI] [PubMed] [Google Scholar]
- 40. Badia Castelló M, Trujillano Cabello J, Serviá Goixart L, March Llanes J, Rodríguez‐Pozo A. Changes in health‐related quality of life after ICU according to diagnostic category. Comparison of two measurement instruments. Medicina Intensiva 2008; 32: 203–15. [DOI] [PubMed] [Google Scholar]
- 41. Orwelius L, Nordlund A, Nordlund P, et al. Pre‐existing disease: the most important factor for health‐related quality of life long‐term after critical illness: a prospective, longitudinal, multicentre trial. Critical Care 2010; 14: R67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Aldecoa C, Pico S, Rico J, Vazquez B, Alonso A, Herreras JIG. The impact of intensive care attendance on health‐related quality of life. Intensive Care Medicine 2010; 36: S394. [Google Scholar]
- 43. Dagge A, Frada R, Campos M, et al. Quality of life in general intensive care unit survivors. Intensive Care Medicine 2010; 36: S394. [Google Scholar]
- 44. Granja C, Lopes A, Moreira S, Dias C, Costa‐Pereira A, Carneiro A. Patients' recollections of experiences in the intensive care unit may affect their quality of life. Critical Care 2005; 9: R96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Khoudri I, Belayachi J, Dendane T, et al. Measuring quality of life after intensive care using the Arabic version for Morocco of the EuroQol 5 Dimensions. BMC Research Notes 2012; 5: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Orwelius L, Lobo C, Teixeira Pinto A, Carneiro A, Costa‐Pereira A, Granja C. Sepsis patients do not differ in health‐related quality of life compared with other ICU patients. Acta Anaesthesiologica Scandinavica 2013; 57: 1201–5. [DOI] [PubMed] [Google Scholar]
- 47. Vainiola T, Pettilä V, Roine RP, Räsänen P, Rissanen AM, Sintonen H. Comparison of two utility instruments, the EQ‐5D and the 15D, in the critical care setting. Intensive Care Medicine 2010; 36: 2090–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Steenbergen S, Rijkenberg S, Adonis T, Kroeze G, van Stijn I, Endeman H. Long‐term treated intensive care patients outcomes: the one‐year mortality rate, quality of life, health care use and long‐term complications as reported by general practitioners. BMC Anesthesiology 2015; 15: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Van Rompaey B, Schuurmans MJ, Shortridge‐Baggett LM, Truijen S, Elseviers M, Bossaert L. Long term outcome after delirium in the intensive care unit. Journal of Clinical Nursing 2009; 18: 3349–57. [DOI] [PubMed] [Google Scholar]
- 50. Chiumello D, Taccone P, Berto V, et al. Long‐term outcomes in survivors of acute respiratory distress syndrome ventilated in supine or prone position. Intensive Care Medicine 2012; 38: 221–9. [DOI] [PubMed] [Google Scholar]
- 51. Elliott D, McKinley S, Alison J, et al. Health‐related quality of life and physical recovery after a critical illness: a multi‐centre randomised controlled trial of a home‐based physical rehabilitation program. Critical Care 2011; 15: R142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Klimasauskas A, Sereike I, Klimasauskiene A, Kekstas G, Ivaskevicius J. The impact of medical conditions on the quality of life of survivors at discharge from intensive care unit. Medicina 2011; 47: 270–7. [PubMed] [Google Scholar]
- 53. Wei X, Day AG, Ouellette‐Kuntz H, Heyland DK. The association between nutritional adequacy and long‐term outcomes in critically ill patients requiring prolonged mechanical ventilation: a multicenter cohort study. Critical Care Medicine 2015; 43: 1569–79. [DOI] [PubMed] [Google Scholar]
- 54. Batterham AM, Bonner S, Wright J, Howell SJ, Hugill K, Danjoux G. Effect of supervised aerobic exercise rehabilitation on physical fitness and quality‐of‐life in survivors of critical illness: an exploratory minimized controlled trial (PIX study). British Journal of Anaesthesia 2014; 113: 130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Burnham EL, Hyzy RC, Paine R, et al. Chest CT features are associated with poorer quality of life in acute lung injury survivors. Critical Care Medicine 2013; 41: 445–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cuthbertson BH, Rattray J, Campbell MK, et al. The PRaCTICaL study of nurse led, intensive care follow‐up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ (Online) 2009; 339: b3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Das Neves AV, Vasquez DN, Loudet CI, et al. Symptom burden and health‐related quality of life among intensive care unit survivors in Argentina: a prospective cohort study. Journal of Critical Care 2015; 30: 1049–54. [DOI] [PubMed] [Google Scholar]
- 58. Gonzales M, Manzano FM, Quintana M, et al. Health‐related quality of life after intensive care: a long‐term follow‐up study. Intensive Care Medicine 2013; 39: S503. [Google Scholar]
- 59. Jackson JC, Hart RP, Gordon SM, et al. Six‐month neuropsychological outcome of medical intensive care unit patients. Critical Care Medicine 2003; 31: 1226–34. [DOI] [PubMed] [Google Scholar]
- 60. Masclans JR, Roca O, Muñoz X, et al. Quality of life, pulmonary function, and tomographic scan abnormalities after ARDS. Chest 2011; 139: 1340–6. [DOI] [PubMed] [Google Scholar]
- 61. Orme J, Romney JS, Hopkins RO, et al. Pulmonary function and health‐related quality of life in survivors of acute respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine 2003; 167: 690–4. [DOI] [PubMed] [Google Scholar]
- 62. Wade DM, Howell DC, Weinman JA, et al. Investigating risk factors for psychological morbidity three months after intensive care: a prospective cohort study. Critical Care 2012; 16: R192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hodgson CL, Udy AA, Bailey M, et al. The impact of disability in survivors of critical illness. Intensive Care Medicine 2017; 43: 992–1001. [DOI] [PubMed] [Google Scholar]
- 64. Cuthbertson BH, Elders A, Hall S, et al. Mortality and quality of life in the five years after severe sepsis. Critical Care 2013; 17: R70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Schmidt K, Worrack S, Von Korff M, et al. Effect of a primary care management intervention on mental health‐related qualityof life among survivors of sepsis: a randomized clinical trial. Journal of the American Medical Association 2016; 315: 2703–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sukantarat KT, Burgess PW, Williamson RCN, Brett SJ. Prolonged cognitive dysfunction in survivors of critical illness. Anaesthesia 2005; 60: 847–53. [DOI] [PubMed] [Google Scholar]
- 67. Duggan MC, Wang L, Wilson JE, Dittus RS, Ely EW, Jackson JC. The relationship between executive dysfunction, depression, and mental health‐related quality of life in survivors of critical illness: results from the BRAIN‐ICU investigation. Journal of Critical Care 2017; 37: 72–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Flaatten H, Kvåle R. Survival and quality of life 12 years after ICU. A comparison with the general Norwegian population. Intensive Care Medicine 2001; 27: 1005–11. [DOI] [PubMed] [Google Scholar]
- 69. Kvale R, Flaatten H. Changes in health‐related quality of life from 6 months to 2 years after discharge from intensive care. Health and Quality of Life Outcomes 2003; 1: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kvåle R, Flaatten H. Changes in intensive care from 1987 to 1997 ‐ has outcome improved? A single centre study. Intensive Care Medicine 2002; 28: 1110–16. [DOI] [PubMed] [Google Scholar]
- 71. García Lizana F, Peres Bota D, De Cubber M, Vincent J‐L. Long‐term outcome in ICU patients: what about quality of life? Intensive Care Medicine 2003; 29: 1286–93. [DOI] [PubMed] [Google Scholar]
- 72. Graf J, Wagner J, Graf C, Koch KC, Janssens U. Five‐year survival, quality of life, and individual costs of 303 consecutive medical intensive care patients – a cost‐utility analysis. Critical Care Medicine 2005; 33: 547–55. [DOI] [PubMed] [Google Scholar]
- 73. Kaarlola A, Pettilä V, Kekki P. Quality of life six years after intensive care. Intensive Care Medicine 2003; 29: 1294–9. [DOI] [PubMed] [Google Scholar]
- 74. Capuzzo M, Bertacchini S, Davanzo E, et al. Health‐related quality of life before planned admission to intensive care: memory over three and six months. Health and Quality of Life Outcomes 2010; 8: 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hb A, Wheeler M. Psychological consequences of critical illness: what is the long term impact on patients and how can nurses help? CONNECT: The World of Critical Care Nursing 2007; 5: 7p. [Google Scholar]
- 76. Jutte JE, Erb CT, Jackson JC. Physical, cognitive, and psychological disability following critical illness: what is the risk? Seminars in Respiratory and Critical Care Medicine 2015; 36: 943–58. [DOI] [PubMed] [Google Scholar]
- 77. Papathanassoglou ED. Psychological support and outcomes for ICU patients. Nursing in Critical Care 2010; 15: 118–28. [DOI] [PubMed] [Google Scholar]
- 78. Pattison N. Psychological implications of admission to critical care. British Journal of Nursing 2005; 14: 708–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Bubble plots of mean domain score against time and change (expressed in points per month) against time.
Figure S2. Bubble plots of the percentage of people reporting problems in answer to each EQ‐5D domain and the corresponding mean or median EQ‐5D tariff score and visual analogue scale against time.
Figure S3. Bubble plots of mean domain score against time and change (expressed in points per month) against time.
Table S1. Papers investigating a health‐related quality of life after critical illness, arranged by: population studied; assessment tool and then alphabetically.
Table S2. Time points with scores significantly different from population comparisons.
Table S3. Newcastle–Ottawa Score for cohort studies.
Appendix S1. Newcastle–Ottawa quality assessment scale for cohort studies.
Appendix S2. PubMed search.


