ABSTRACT
Background: The Hospital Readmissions Reduction Program (HRRP) began decreasing Medicare payments to hospitals reporting high readmission rates for individuals over 65. Thus, financially incentivizing hospitals to improve quality performance on preventable readmissions. Well-established research indicates that minorities are more frequently readmitted to hospitals, but it is unknown if community diversity is associated with 30-day readmission rates.
Objectives: To investigate the association between racial/ethnic diversity and hospitals’ 30-day readmission rates.
Methods: We linked the 2017 HRRP, American Hospital Association (AHA) database, Area Health Resource File, US Census Bureau Current Population Survey, and the Dartmouth Atlas HRR dataset to examine 30-day readmission rate for heart failure (HF), pneumonia (PN), acute myocardial infarction (AMI), and hip replacement (HR) surgery of 4,299 hospitals across 306 HRRs.
Results: Our findings indicate a statistically significant negative relationship between diversity and 30-day readmission rates for HF, PN, AMI, and HR with a hospital referral region (HRR). Thus, hospitals located in HRRs with diverse populations are more likely to have higher 30-day readmission rates for all conditions under Medicare’s HRRP
Conclusion: Better discharge follow-up, interventions, and use of support staff aimed at meeting needs associated with differences in communities and cultures are likely to prove more fruitful than traditional one-size fits all approaches to care.
KEYWORDS: Hospitals, quality of care, hospital readmission, older adults, reduction program
1. Introduction
As a measure of a hospital’s quality of care, hospital readmissions are a major concern for patients, hospitals, and policymakers. Previous studies have found that over 30% of patients age 65 and older who are hospitalized are readmitted within 360 days, and over 50% are readmitted during the first 30 days [1]. In addition, approximately 20% of all Medicare patients are readmitted within 30 days of discharge [2–4], with their readmission-associated financial burden on the Centers for Medicare and Medicaid Services (CMS) estimated to be $17 billion annually [5]. Of great concern are previous findings indicating that diverse communities have significant barriers associated with access to insurance and timely care [6], which may influence hospitals’ performance on this quality measure.
Improvement of health systems’ performance has been a concern for policymakers for several years. Due to the increased financial burden of 30-day readmission, CMS began restricting reimbursements for certain readmissions, such as those associated with congestive heart failure (HF), acute myocardial infarctions (AMI), and pneumonia (PN), in order to promote improved quality in healthcare delivery for its beneficiaries. In October 2012, CMS’ Hospital Readmissions Reduction Program (HRRP) began reducing Medicare payments for the Inpatient Prospective Payment System (IPPS) to hospitals experiencing excessive readmissions [7–9]. Excessive readmissions are measured by an algorithm of 30-day readmissions for AMI, HF, PN, chronic obstructive pulmonary disease (COPD), hip/knee replacement (HR), and coronary artery bypass graft surgery (CABG). A hospital’s expected readmission rate for each HRRP condition is the national mean readmission rate, risk-adjusted for certain patient characteristics present in the specific hospital [8,10,11].
However, these calculations do not adjust for the diversity or socioeconomic status of the community in which a hospital resides. This lack of statistical control in the predictive model is problematic for hospitals that primarily serve diverse patients [12,13]. At the hospital level, previous research has consistently indicated hospitals serving minority populations experience higher readmissions for HF, AMI, PN, and diabetes [14,15]. County characteristics that correlate highly with readmission rates include minority and vulnerable populations, socioeconomic status (negative correlation), educational level (negative correlation), high unemployment rate, a large number of individuals who never married, and a high percentage of Medicare recipients per 100,000 residents [15–17]. At the individual level, Martsolf et al. (2016) reported race, ethnicity, and low socioeconomic status affect hospitals’ excess readmission ratios and significantly impact hospitals’ risk for penalties.
Multiple studies have examined the impact of patient or county–level factors on hospitals’ 30-day readmission rates for congestive HF, AMI, and PN. These studies found that 30-day readmission rates are 10–20% higher for Blacks and Hispanics when compared to Whites for congestive HF, AMI, and PN, and following ambulatory surgery (i.e., hip replacement) [18–20]. Furthermore, a study reported that 42% of the disparity in hospitals’ readmissions are a result of hospitals’ performance, while the majority (58%) of readmissions are attributable to the demographic and socioeconomic characteristics of the community served [16].
Many studies have explored the impact of county [12,17], hospital [13,21], and patient characteristics [2,8]individually on hospitals’ performance on 30-day readmission for congestive HF, AMI, and PN. However, to our knowledge, no study has explored the impact of community diversity in a hospital referral region (HRR) as it relates to its demographics and racial/ethnic makeup, on a hospital’s 30-day readmission rate.
Therefore, exploring the impact of community diversity in the context of multi-racial and ethnic groups is critical in a continuously diversifying population. For instance, one in four Americans are from a different race and ethnicity, and by 2050 this is expected to grow to one in three [22]. Examining disparity within a hospital’s community as a whole rather than racial and ethnic group proportions provide an all-inclusive approach that may better identify underlying issues associated with barriers to care access, or to the manner by which organizations attempt to provide treatment that likely does not meet the needs of non-homogeneous groups. Thus, community diversity is assessed using a multi-group approach to that of the Theil’s H or the information theory index [23]. It measures the ‘evenness’ of a community in relation to quality of health-care services delivered [24]. This concept was first introduced in 2002 to assess the segregation among multiple racial and ethnic groups living in the same geographic area in the USA [24]. Understanding the degree of evenness (heterogenous communities or diverse communities) at a HRR provides a deeper examination of the disparity present currently within a hospital’s community.
1.1. Framework
To guide the study, we used the conceptual framework for understanding inequity [25]. The framework, modified in Figure 1, shows the relationship between determinants of health outcomes, whereby the health care system and related sectors are impacted by government policies and community factors, and their impact on health outcomes, particularly 30-day readmission rates [26]. There are a range of community factors that have been shown to influence health: a wider socioeconomic context, inequity, diversity, income and poverty, health service utilization, and social and community composition and structure [27,28]. For the purposes of this study, communities are defined as HRRs which best represent a hospital’s service area. A HRR is a geographic healthcare market where at least one hospital is present that performs complex cardiovascular procedures and neurosurgery [29]. The community-level measures of these factors help to account for some of the variations in readmission rates. In utilizing community factors as surrogates for patient-level characteristics, we can measure the individual effects of each factor on readmission rates, and determine the independent effects of other community-level characteristics on hospital readmission rates [16].
Figure 1.
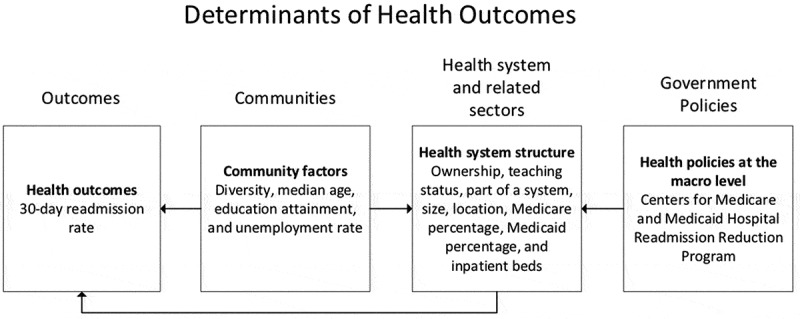
Conceptual framework for understanding health inequities.
Our HRR factors include diversity, healthcare market competition, unemployment, age, and education attainment. The construct of racial and ethnic differences relate to social division and discrimination, and thus, they are a social, but biological socio-economic factor [30]. These factors have been shown to impact access and use of health services. Previous research indicates that access to and the use of health services are associated with the patients’ likelihood for readmission; therefore, these factors will help explain some of the HRR-level variations in hospital readmission rates [16]. Additionally, we examined the impact of the Accountable Care Act of 2010 (ACA) – measured through the total performance score on hospitals 30-day readmission [5,31]. We defined the health system by the structure of health-care facilities, such as size, location, teaching status, and ownership. Finally, we examined health outcomes, by using 30-day readmission for HF, PN, AMI and HR. Health outcomes are indicators of the quality of care provided by hospitals; and the underlying reasoning behind CMS’ HRRP is that hospitals’ provision of quality care was not enough to prevent a relapse of poor health, requiring patients to seek out medical services once more. Previous research has found that the highest degree of health outcome disparities exist in facilities serving a high proportion of minority patients [32], therefore our study seeks to examine whether community factors and health care system factors have a significant impact on health outcomes: HRRP.
Given the influence that sociodemographic variables have on readmission rates, we are interested in determining if community racial/ethnic diversity is associated with 30-day readmission rate and hospitals’ performance on CMS’ HRRP. We hypothesize that community diversity is associated with an increase in 30-day readmission and a decrease in performance on HRRP.
2. Methods
2.1. Design and data sources
In this study, we used a secondary cross-sectional design to analyze census data of non-federal hospitals in the USA. We used the 2017 CMS HRRP, American Hospital Association (AHA) database, Area Health Resource File (AHRF), US Census Bureau Current Population Survey and the Dartmouth Atlas HRR dataset. The HRR dataset provides geographic boundaries of hospital referral regions, whereby a least one hospital has the capability and resources to provide specialized services and complex surgeries [29]. Data sets were merged using CMS Provider Number and HRR Federal Information Processing Standards (FIPS).
2.2. Readmission
Our outcome variables include unplanned risk-adjusted 30-day readmission rates for heart failure (HF), pneumonia (PN), acute myocardial infarction (AMI), and hip replacement (HR) surgery at the hospital level for inpatient discharges from 1 July 2014 to 30 June 2017.
2.3. Community diversity
Community diversity is defined by the representation of the six US races/ethnicities: White, Black or African American, American Indian and Alaska Native, Asian American, Native Hawaiian and Other Pacific Islander, as identified through US Census Bureau data. A diverse hospital referral region consists of a heterogeneous population, whereby all six races/ethnicities are equally represented [33]. Our primary independent variable was HRR-level diversity operationalized using an entropy index score and aggregated to the HRR level [34]. The entropy index score consists of the proportions of individuals 65 and older from the six racial/ethnic groups found in the US. The entropy index score measures evenness – the distribution of six ethnicities in an HRR, regardless of the size of the ethnic groups; the greater the score (range 0–1.8), the greater the diversity. A score of 1.8 identifies an even representation of each group, regardless of their respective sizes, within a defined HRR; meaning that each of the six groups would make up 16.66% of the population in the defined HRR.
2.4. Covariates
Our hospital control variables come from the AHA dataset and included: hospital bed size (small: 0–99, medium: 100–199, large: 200+), ownership (for-profit, not for profit and government), hospital location (rural and urban), teaching status (major, minor, non-teaching), hospital inpatient days per 1000, Medicare discharges percentage of total discharges, and Medicaid days as a percentage of total inpatient days.
Hospital size was used as an indicator of a hospital’s quality and resources [35], which can affect hospital readmission rates. Hospital ownership was utilized as a measure of the hospitals’ community orientation and gauge of community health [36]. Location was used as an indicator of a hospital’s quality as literature suggests where minorities seek care affects their health outcomes [37]. We also included hospitals’ teaching status as indicators of readmission rates and safety [38]. We used Medicare discharge percentage of total discharges and Medicaid days as a percentage of total inpatient days to assess hospital payer mix [39].
This study focuses on readmission rates among older adults, therefore, at the HRR level, we controlled for median age, unemployment rate among individuals 65 and older, and education attainment of individuals 65 and older (high school degree, some college, associate degree, bachelor’s degree, graduate degree) using data from the AHRF. We utilized unemployment rate and education attainment for individuals 65 and older (lower education attainment is associated with lower income) as proxy indicators of their socioeconomic status.
2.5. Statistical analyses
In this study, we conducted descriptive statistics and multilevel Poisson regressions to explore the influence of community diversity on hospitals’ 30-day readmission rates. Our outcome variable, hospital rate of readmission, is a count variable; therefore, Poisson regressions were used to model the data associated with this variable. All analysis was performed using Stata 14 SE [40]. All variables were tested for multicollinearity along with Akaike’s and Schwarz’s Bayesian information criteria for model fit. In accordance with the policy of the University, the Institutional Review Board (IRB) categorized the research as exempt since the study analyzed secondary data that is publicly available.
3. Results
Our sample consisted of 4,382 hospitals across 306 HRRs. Over 60% of the hospitals in our sample were not-for-profit, non-teaching, and part of a system (Table 1). Half of the hospitals are small hospitals and only 10% of our sample consisted of large hospitals with over 200 beds. The majority of hospitals (57.9%) were located in rural areas. The highest 30-day readmission rate was for heart failure averaging 60.46. The lowest 30-day readmission rate was for hip replacement surgery with a mean of 28.92. The average hospital Medicare and Medicaid percentage was 52.14 and 19.80 with a standard deviation of 18.15 and 14.47, respectively. The average inpatient days per 1000 was 38.92. At the HRR level, the average entropy score was 0.77, with an unemployment rate of 5.02 and a median age of 39.30. Across all HRRs, the average percentage of individuals with a graduate degree was less than 10% and about 30% of the population had at least a high school degree.
Table 1.
Descriptive statistics of hospitals participating in readmissions reduction program (n = 4382) and their hospital referral region (n = 306).
| Frequency | Percent | |
|---|---|---|
| Hospital ownership | ||
| Government | 1,017 | 23.21 |
| For-profit | 686 | 15.65 |
| Not-for-profit | 2,679 | 61.14 |
| Teaching status | ||
| Major | 231 | 5.27 |
| Minor | 1,441 | 32.88 |
| Non-teaching | 2,710 | 61.84 |
| Part of a system | ||
| No | 1,549 | 35.35 |
| Yes | 2,833 | 64.65 |
| Hospital size | ||
| Small | 2,221 | 50.68 |
| Medium | 1,713 | 39.09 |
| Large | 448 | 10.22 |
| Hospital location | ||
| Rural | 2,537 | 57.9 |
| Urban | 1,845 | 42.1 |
| Mean | Standard Deviation | |
| Heart Failure 30-day readmission rate | 60.46 | 26.59 |
| Pneumonia 30-day readmission rate | 42.98 | 19.43 |
| Hip Replacement Surgery 30-day readmission rate | 28.92 | 14.30 |
| Acute Myocardial Infarction 30-day readmission rate | 44.50 | 16.91 |
| Hospital Medicare percentage | 52.14 | 18.15 |
| Hospital Medicaid percentage | 19.80 | 14.46 |
| Hospital inpatient days per 1000 | 38.92 | 56.48 |
| Entropy index score | 0.77 | 0.27 |
| Unemployment rate | 5.02 | 1.10 |
| Median age | 39.30 | 2.95 |
| Percent with High School degree | 30.38 | 5.32 |
| Percent with some college education | 21.65 | 2.94 |
| Percent with associate degree | 8.47 | 1.79 |
| Percent with bachelors | 16.72 | 3.73 |
| Percent with graduate degree | 9.68 | 3.44 |
Table 2 displays the multi-level Poisson regression analysis results. We found a statistically significant difference between community diversity and hospitals’ 30-day readmission rates for heart failure (p < 0.001), pneumonia (p < 0.001), hip replacement surgery (p = 0.01), and AMI (p = 0.01). For every one-unit increase in community diversity (entropy index score), the expected 30-day readmission rate is multiplied by a factor of 1.150 for heart failure, 1.258 for pneumonia, 1.161 for hip replacement surgery and 1.098 for AMI, while holding all other variables in the model constant. When we examined hospital characteristics, we found that across all four 30-day readmission rate conditions, for-profit and government hospitals were at a greater risk for higher 30-day readmission rates. Minor teaching hospitals were at a lower risk for 30-day readmission rate (p < 0.001) across all four conditions (HF: 0.936; Pneumonia: 0.940; Hip replacement surgery: 0.977; AMI: 0.976;). Furthermore, hospitals that are part of a system were also at a lower risk for 30-day readmission rate across all four conditions. Small hospitals were found to be at a greater risk for higher 30-day readmission rates compared to larger hospitals (HF: 1.315; Pneumonia: 1.116; Hip replacement surgery: 1.405; AMI: 1.590). Medium hospitals were also found to be at a greater risk for higher 30-day readmission rates compared to larger hospitals in heart failure (1.044) and AMI (1.050). Rural hospitals were found to be at a lower risk for 30-day readmission rates for heart failure (0.984) and pneumonia (0.969) but a higher risk for hip replacement surgery (1.062) and AMI (1.085) 30-day readmission rates. We also found a statistical difference between hospital Medicare percentage, Medicaid percentage and inpatient days per 1000, however, the effect size is small.
Table 2.
The effects of hospital referral region diversity on 30-day readmission rates of older adults (n = 4340) 30-day readmission rate.
| Heart Failure |
Pneumonia |
Hip Replacement Surgery |
Acute Myocardial Infarction |
|||||
|---|---|---|---|---|---|---|---|---|
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Hospital Characteristics | ||||||||
| Hospital ownership (referent: Not-for-profit) | ||||||||
| Government | 1.119* | [1.107,1.132] | 1.074* | [1.060,1.089] | 1.135* | [1.118,1.153] | 1.050* | [1.037,1.064] |
| For-profit | 1.116* | [1.102,1.130] | 1.131* | [1.115,1.148] | 1.035* | [1.017,1.055] | 1.028* | [1.013,1.044] |
| Teaching status (referent: Non-teaching) | ||||||||
| Major | 1.012 | [0.986,1.039] | 1.004 | [0.976,1.034] | 0.968 | [0.930,1.008] | 1.022 | [0.988,1.056] |
| Minor | 0.936* | [0.926,0.946] | 0.964* | [0.952,0.976] | 0.879* | [0.865,0.893] | 0.927* | [0.916,0.939] |
| Part of a system (referent: No) | 0.937* | [0.928,0.946] | 0.940* | [0.929,0.951] | 0.977* | [0.963,0.990] | 0.976* | [0.965,0.986] |
| Hospital size (referent: Large) | ||||||||
| Small | 1.315* | [1.280,1.351] | 1.116* | [1.083,1.150] | 1.405* | [1.346,1.466] | 1.590* | [1.535,1.648] |
| Medium | 1.044* | [1.021,1.068] | 1.016 | [0.991,1.041] | 0.988 | [0.953,1.024] | 1.050* | [1.019,1.081] |
| Rural (referent: Urban) | 0.984* | [0.973,0.995] | 0.969* | [0.956,0.982] | 1.062* | [1.045,1.079] | 1.085* | [1.072,1.099] |
| Hospital Medicare percentage | 0.998* | [0.998,0.998] | 0.998* | [0.997,0.998] | 1.000* | [0.999,1.000] | 0.999* | [0.999,0.999] |
| Hospital Medicaid percentage | 1.000 | [0.999,1.000] | 0.998* | [0.998,0.999] | 1.002* | [1.001,1.002] | 1.002* | [1.001,1.002] |
| Hospital inpatient days per 1000 | 1.000* | [1.000,1.000] | 1.000 | [1.000,1.000] | 0.999* | [0.999,0.999] | 0.999* | [0.999,0.999] |
| Hospital Referral Region Characteristics | ||||||||
| Entropy Index Score | 1.159* | [1.028,1.306] | 1.258* | [1.111,1.424] | 1.161* | [1.033,1.305] | 1.098* | [1.022,1.180] |
| Median age | 0.994 | [0.986,1.002] | 0.998 | [0.990,1.006] | 0.992* | [0.984,1.000] | 0.994* | [0.990,0.999] |
| Percent with some college education | 0.991 | [0.981,1.001] | 0.988* | [0.978,0.999] | 0.985* | [0.975,0.995] | 0.995 | [0.989,1.001] |
| Percent with bachelors | 1.000 | [0.987,1.013] | 1.001 | [0.988,1.015] | 0.986* | [0.974,0.998] | 0.997 | [0.989,1.004] |
Note: Coefficients; 95% confidence intervals in brackets; * p < 0.05; Non-significant covariates were removed: Unemployment rate, Percent with High School degree, Percent with associate degree, Percent with graduate degree
When we examined community characteristics, we found that for every unit increase in median age, the expected 30-day readmission rate for hip replacement surgery and AMI is multiplied by a factor of 0.992 and 0.994 (decreased rate of 30-day readmissions). We also found for every unit increase in college-educated individuals or bachelors-educated individuals, the expected 30-day readmission rate for hip replacement is multiplied by a factor of 0.985 and 0.986, respectively.
4. Discussion
This study examined the incidence of 30-day readmissions at hospitals within different levels of diversity among older adults. Our analysis revealed that the more diverse the HRR, the worse the 30-day readmission rates across four conditions (heart attack, pneumonia, hip replacement surgery and AMI). Our study findings show that community diversity is associated with an increase in 30-day readmission and a decrease in performance on HRRP. Our findings are consistent with studies of overall incidents of 30-day readmission rates [21,41]. Our work contributes to the literature by demonstrating that community characteristics significantly affect hospital readmission rates. Our analysis revealed hospitals that serve communities with minority and vulnerable populations, low socioeconomic status, low educational levels, high unemployment rates, and high percentage of Medicare recipients per 100,000 residents have increased readmissions. Current literature also indicates additional community and hospital characteristics (i.e., Medicare, Medicaid, education attainment) impact 30-day readmissions [9,11,12]. While the effect sizes are small (IRR close to 1), but significant [42] this research highlights how hospitals work in silos or as a part of their own health system and may not fully engage with the community. This can be critical to improving care provided to older adults.
An important implication for the future is a need for a change to CMS’ HRRP calculations, which would factor in community diversity, and thereby eliminate ‘punishments’ for organizations that care for racial/ethnic minorities. Our findings suggest that community diversity does significantly influence HRRP and readmissions. Yet, as previously mentioned, aspects out of hospitals’ control, such as community factors (location, racial/ethnic make-up of the population, income, etc.), have been found to significantly and consistently influence the likelihood of CMS readmission penalties, but still remain unaccounted for in CMS’ calculations of readmission rates [43]. Additionally, a multitude of studies which have run predictive readmission models still fail to address community diversity imbalance, even though this is a frequent problem that affects model training and impacts the ability to correctly evaluate data [44].
Another significant implication of our results is that hospitals serving a more diverse HRR have a higher number of 30-day readmissions and therefore are financially penalized. Therefore, it is possible that in the future, hospitals would avoid placement in diverse community in order to avoid quality-based penalties, which would decrease access to care for individuals in a diverse community. Furthermore, health care policies such as HRRP may financially hurt hospitals treating these diverse populations, such as safety net hospitals. Safety-net hospitals treat the highest amount of racial/ethnic minorities and highly diverse communities, and usually experience significant economic constraints [45]. The financial stability of safety net hospitals is historically very uncertain as they rely heavily on funding from federal and local governments, meaning that they are highly susceptible to changes in health care policy, such as HRRP. Currently, safety-net hospitals are experiencing a gap in funding due to Medicaid’s decrease in disproportionate hospital funding [46,47]. In addition to a lack of funding, financial penalties imposed by CMS quality-based policies, could further damage the financial stability of safety-net hospitals and their ability to affectively care for patients.
Our findings highlight a potential need for multidisciplinary teams that are composed of case managers, patient advocates, and other necessary allied health professionals that can assist in ensuring medication adherence and monitor patient symptoms. In addition, the role of a social worker in conducting a post-discharge follow-up may prove to be valuable in integrating patients back into everyday life within the community in which they reside. There are also unmeasured factors that could explain the pattern seen within 30-day readmission rates such as provider behavior with patient engagement and patient behavior in adherence with discharge guidelines.
4.1. Limitations
The study strength is driven by is methodology. We used multilevel Poisson regressions to adjust for biases and nesting effects of the data. Our modeling consists of a comprehensive community and hospital level variables driven primary for the literature. It is the first study to examine community diversities influence on each 30-day readmission rate individually. Another major strength to our study is our unique definition of community. Using HRR as a community measure accurately examines patient utilization pattern. We are able to control for patient characteristics for each HRR using community level factors aggregated to the HRR level. A major limitation of this study is that the study is an observational study, thus, ausation cannot be determined. However, the observed effects of variance provide critical information regarding the patterns of 30-day readmissions within the CMS program [48]. Another limitation is that the study uses cross-sectional analysis, thereby limiting patterns to a section of time rather than through time.
Lastly, in this study, the definition of a community can be argued, as we define community by HRRs. HRRs do cross state lines, making it difficult to assess other non-observed variable impacts on hospital performance in the 30-day readmission program. In summary, this study provides a comprehensive examination of community diversity on hospital performance in the 30-day readmission program.
4.2. Conclusion
Our results show that after accounting for community and hospital characteristics, a large amount of variance in the 30-day readmission program is explained. Hospitals must address key hospital and community factors in order to increase profit and decrease re-hospitalization for this aging population. Insight to the populations they serve is imperative as patient factors have a strong influence on readmissions. Strategic strategy for success must focus on not only hospitals, but also on the communities they serve. Future research is needed to examine and identify the key reasons for such health care disparity.
Acknowledgments
We would like to acknowledge and thank our respective institutions.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Kripalani S, Theobald C, Anctil B, et al. Reducing hospital readmission: current strategies and future directions. Annu Rev Med. 2014October21;65:471–485. PubMed PMID: PMC4104507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].DeVore AD, Hammill BG, Hardy NC, et al. Has public reporting of hospital readmission rates affected patient outcomes? Analysis of medicare claims data. J Am Coll Cardiol. 2016March1;67(8):963–972. PubMed PMID: 26916487. [DOI] [PubMed] [Google Scholar]
- [3].Park L, Andrade D, Mastey A, et al. Institution specific risk factors for 30 day readmission at a community hospital: a retrospective observational study. BMC Health Serv Res. 2014;14(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wan TT, Ortiz J, Du A, et al. Contextual, organizational and ecological effects on the variations in hospital readmissions of rural medicare beneficiaries in eight southeastern states. Health Care Manag Sci. 2017March;20(1):94–104. PubMed PMID: 26373554; PubMed Central PMCID: PMCPMC4792779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].McIlvennan CK, Eapen ZJ, Allen LA.. Hospital readmissions reduction program. Circulation. 2015May19;131(20):1796–1803. PubMed PMID: 25986448; PubMed Central PMCID: PMCPMC4439931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Glied S, Jackson A.. The future of the affordable care act and insurance coverage. Am J Public Health. 2017;107(4):538–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bronstein LR, Gould P, Berkowitz SA, et al. Impact of a social work care coordination intervention on hospital readmission: a randomized controlled trial. Soc Work. 2015July;60(3):248–255. PubMed PMID: 26173366. [DOI] [PubMed] [Google Scholar]
- [8].Centers for medicare and medicaid services. Hospital-acquired condition reduction program (HACRP) 2017. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HAC-Reduction-Program.html [DOI] [PubMed]
- [9].Henke RM, Karaca Z, Lin H, et al. Patient factors contributing to variation in same-hospital readmission rate. Med Care Res Rev. 2015June;72(3):338–358. PubMed PMID: 25824244. [DOI] [PubMed] [Google Scholar]
- [10].Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015November;175(11):1803–1812. PubMed PMID: 26368317; PubMed Central PMCID: PMCPMC4991542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Nuckols TK. County-level variation in readmission rates: implications for the hospital readmission reduction program‘s potential to succeed. Health Serv Res. 2015February;50(1):12–19. PubMed PMID: 25630850; PubMed Central PMCID: PMCPMC4319868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen M, Grabowski DC. Hospital readmissions reduction program: intended and unintended effects. Med Care Res Rev. 2017December1:1077558717744611.PubMed PMID: 29199504 DOI: 10.1177/1077558717744611. [DOI] [PubMed] [Google Scholar]
- [13].Hebert PL, Howell EA, Wong ES, et al. Methods for measuring racial differences in hospitals outcomes attributable to disparities in use of high-quality hospital care. Health Serv Res. 2017April;52(2):826–848. PubMed PMID: 27256878; PubMed Central PMCID: PMCPMC5346505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Aseltine RH Jr., Yan J, Gruss CB, et al. Connecticut hospital readmissions related to chest pain and heart failure: differences by race, ethnicity, and payer. Conn Med. 2015February;79(2):69–76. PubMed PMID: 26244203. [PubMed] [Google Scholar]
- [15].Moore CD, Gao K, Shulan M. Racial, income, and marital status disparities in hospital readmissions within a veterans-integrated health care network. Eval Health Prof. 2015;38(4):491–507. [DOI] [PubMed] [Google Scholar]
- [16].Herrin J, St Andre J, Kenward K, et al. Community factors and hospital readmission rates. Health Serv Res. 2015February;50(1):20–39. PubMed PMID: 24712374; PubMed Central PMCID: PMCPMC4319869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Martsolf GR, Barrett ML, Weiss AJ, et al. Impact of race/ethnicity and socioeconomic status on risk-adjusted readmission rates: implications for the hospital readmissions reduction program. Inquiry. 2016;53:0046958016667596. [Google Scholar]
- [18].Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011February16;305(7):675–681. PubMed PMID: 21325183; PubMed Central PMCID: PMCPMC3332042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].McHugh MD, Carthon JM, Kang XL. Medicare readmissions policies and racial and ethnic health disparities: a cautionary tale. Policy Polit Nurs Pract. 2010November;11(4):309–316. PubMed PMID: 21531966; PubMed Central PMCID: PMCPMC3105322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Rodriguez F, Joynt KE, Lopez L, et al. Readmission rates for hispanic medicare beneficiaries with heart failure and acute myocardial infarction. Am Heart J. 2011August;162(2):254–261 e3. PubMed PMID: 21835285. [DOI] [PubMed] [Google Scholar]
- [21].Thompson MP, Kaplan CM, Cao Y, et al. Reliability of 30 day readmission measures used in the hospital readmission reduction program. Health Serv Res. 2016;51(6):2095–2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].American Hospital Association A diversity and cultural proficiency assessment tool for leaders. Washington, DC: American Hospital Association; 2004. [Google Scholar]
- [23].Theil H. The information approach to demand analysis. Econometrica. 1965;33(1):67–87. [Google Scholar]
- [24].Gorelick R, Bertram SM. Multi-way multi-group segregation and diversity indices. PLoS One. 2010;5(6):e10912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Geronimus AT. Understanding and eliminating racial inequalities in women‘s health in the USA: the role of the weathering conceptual framework. J Am Med Womens Assoc (1972). 2001;56(4):133–6, 149–50. [PubMed] [Google Scholar]
- [26].Hatch SL. Conceptualizing and identifying cumulative adversity and protective resources: implications for understanding health inequalities. J Gerontol B Psychol Sci Soc Sci. 2005;60(Special_Issue_2):S130–S134. [DOI] [PubMed] [Google Scholar]
- [27].National Academies of Sciences Engineering and Medicine Accounting for social risk factors in medicare payment: criteria, factors, and methods. Washington DC, USA: National Academies Press; 2016. [PubMed] [Google Scholar]
- [28].Marmot M, Friel S, Bell R, et al. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. [DOI] [PubMed] [Google Scholar]
- [29].Wennberg JE. The dartmouth atlas of health care in the USA (incl. Diskette). Chicago, IL: American Hospital Association; 1996. [Google Scholar]
- [30].Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. 2001;55: 693–700. 2001-10-0100:00:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Look KA, Kim NH, Arora P. Effects of the affordable care act‘s dependent coverage mandate on private health insurance coverage in urban and rural areas. J Rural Health. 2017January;33(1):5–11. PubMed PMID: 27079801. [DOI] [PubMed] [Google Scholar]
- [32].Hasnain-Wynia R, Kang R, Landrum MB, et al. Racial and ethnic disparities within and between hospitals for inpatient quality of care: an examination of patient-level hospital quality alliance measures. J Health Care Poor Underserved. 2010;21(2):629–648. PubMed PMID: 105203715 Language: English. Entry Date: 20100625. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- [33].Colby SL, Ortman JM. Projections of the size and composition of the US population: 2014 to 2060: population estimates and projections. Washington, DC, USA: Census Bureau; 2017.
- [34].Iceland J. The multigroup entropy index (also known as Theil’s H or the information theory index). University of Maryland, MD: US Census Bureau; 2006;31 Retrieved July. 2004. [Google Scholar]
- [35].Sosunov EA, Egorova NN, Lin HM, et al. The impact of hospital size on cms hospital profiling. Med Care. 2016April;54(4):373–379. PubMed PMID: 26683782; eng. [DOI] [PubMed] [Google Scholar]
- [36].Hamadi H, Apatu E, Spaulding A. Does hospital ownership influence hospital referral region health rankings in the USA. Int J Health Plann Manage. 2018January;33(1):e168–e180. . PubMed PMID: 28731547; eng. [DOI] [PubMed] [Google Scholar]
- [37].Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007;167(12):1233–1239. [DOI] [PubMed] [Google Scholar]
- [38].Chen AS, Revere L, Ratanatawan A, et al. A comparative analysis of academic and nonacademic hospitals on outcome measures and patient satisfaction. Am J Med Qual. 2018September23:1062860618800586 PubMed PMID: 30246541; eng DOI: 10.1177/1062860618800586 [DOI] [PubMed] [Google Scholar]
- [39].Lingsma HF, Bottle A, Middleton S, et al. Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res. 2018;18(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Stata Corp LP Stata statistical software release 14. College Station, TX: Stata Press Publication; 2014. [Google Scholar]
- [41].Lindenauer PK, Bernheim SM, Grady JN, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. J Hosp Med. 2010;5(6):E12–8. PubMed PMID: 20665626 Jul-Aug. [DOI] [PubMed] [Google Scholar]
- [42].Prentice DA, Miller DT. When small effects are impressive. Psychol Bull. 1992;112(1):160. [Google Scholar]
- [43].Jindal RP, Gauri DK, Singh G, et al. Factors influencing hospital readmission penalties: are they really under hospitals‘ control? Decis Support Syst. 2018;110:58–70. . [Google Scholar]
- [44].Artetxe A, Beristain A, Graña M. Predictive models for hospital readmission risk: A systematic review of methods. Comput Methods Programs Biomed. 2018October01;164:49–64. [DOI] [PubMed] [Google Scholar]
- [45].Danner OK, Matthews LR, Wilson KL, et al. Healthcare outcome disparities in trauma care. West J Emerg Med. 2012;13(3):217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Katz MH. Future of the safety net under health reform. JAMA. 2010;304(6):679–680. [DOI] [PubMed] [Google Scholar]
- [47].Neuhausen K, Davis AC, Needleman J, et al. Disproportionate-share hospital payment reductions may threaten the financial stability of safety-net hospitals. Health Affairs. 2014June01;33(6):988–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Altmann J. Observational study of behavior: sampling methods. Behav. 1974;49(3):227–267. PubMed PMID: 4597405. [DOI] [PubMed] [Google Scholar]


