Abstract
Suicide prevention is a major health care responsibility in need of new perspectives. This study reviews Zero Suicide, an emerging approach to suicide prevention that embraces the aspirational goal of zero suicides among patients treated in health care systems or organizations. Zero Suicide is gaining international momentum while at the same time evoking objections and concerns. Fundamental to Zero Suicide is a multilevel system view on suicide prevention, with three core elements: a direct approach to suicidal behaviors; continual improvement of the quality and safety of care processes; and an organizational commitment to the aspirational goal of zero suicides. The rationale and evidence for these components are clarified and discussed against the backdrop of concerns and objections that focus on possible undesired consequences of the pursuit of zero suicide, in particular for clinicians and for those who are bereaved by suicide. It is concluded that it is rational to pursue zero suicides as an aspirational goal, provided the journey toward zero suicides is undertaken in a systemic and sustained manner, in a way that professionals feel supported, empowered, and protected against blame and inappropriate guilt.
Prevention of suicide and suicidal behaviors is a major health care responsibility in need of new perspectives. Compared with other major health problems like HIV/AIDS, coronary heart disease, or leukemia, little progress has been made in reducing morbidity and mortality due to suicidal behavior (Insel, 2014). The annual US suicides number increased by 24% between 1999 and 2014 (Curtin, Warner, & Hedegaard, 2016). In the Netherlands, where 39% of all people who die by suicide were receiving specialist mental health care, this number increased by 38% between 2007 and 2015 (CBS, 2016).
While it is safe to say that health care helps to prevent many suicides, improving its quality may prevent many more. Routine care for patients at risk of suicide still is highly variable and often far from perfect. Clinical audits, root cause analyses after suicides, and service user reports show common themes directly pertaining to discontinuities and lapses in elementary care processes (Burgess, Pirkis, Morton, & Croke, 2000; Gillies, Chicop, & O'Halloran, 2015; Huisman, Robben, & Kerkhof, 2009; Renaud et al., 2014; Taylor, Hawton, Fortune, & Kapur, 2009). In clinical practice, many workers lack specific training to work with suicidal patients (e.g., Awenat et al., 2017; Castelli Dransart, Heeb, Gulfi, & Gutjahr, 2015). Ready implementation of guideline best practices and recommendations remains problematic (de Beurs et al., 2016; Cooper et al., 2013; Schmitz et al., 2012). In the face of the catastrophic impact of suicide and the lack of progress in the past decades, a transformational approach to suicide prevention in health care is warranted.
Zero Suicide is an emergent approach to suicide prevention in health care (Hampton, 2010; Hogan, 2016; Hogan & Goldstein Grumet, 2016; SPRC, 2016). Zero Suicide is driven by the aspirational view of a future in which no one dies alone and in despair by suicide as a result of excellent health care; and by the conviction that by acting upon this aspiration in a committed, systemic, and sustained manner, many and perhaps most suicides among patients in health care can be prevented. This approach is gaining momentum internationally while at the same time evoking strong concerns. With this study, we aim to clarify the background and core elements that constitute Zero Suicide as well as review its rationale and evidence base against the backdrop of the concerns and objections it has evoked. Regarding its potential to serve suicide prevention, we conclude that—under conditions—it is rational to pursue the aspirational goal of zero suicides in health care.
Background and Development
In 2011, the U.S. National Action Alliance for Suicide Prevention (NAASP; Covington et al., 2011) published a set of recommendations for health care systems based on the analysis of examples of successful suicide prevention. This analysis focused on the US Air Force multilevel suicide prevention program, which lead to a 33% reduction of suicide (Knox, Litts, Talcott, Feig, & Caine, 2003; Knox et al., 2010), and on the Henry Ford Health System Perfect Depression Care program (HFHS), which resulted in 10 consecutive quarters of no reported suicide deaths (Ahmedani, Coffey, & Coffey, 2013; Coffey, 2006, 2007; Coffey, Coffey, & Ahmedani, 2013; Hampton, 2010). Observing that profound cultural and systems change provide the underpinnings of these effective approaches, the NAASP identified three critical success factors: (1) suicide‐specific, evidence‐based practices; (2) reliably delivered by well‐managed whole systems of care that are continuously improving service access, quality, and safety; and that are (3) firmly rooted in core values reflecting a service culture that no longer accepts suicide as an outcome.
By putting suicide prevention in a framework of entire health care systems, the NAASP founded Zero Suicide as outlined online by the US Suicide Prevention Research Center (SPRC, 2016). Implementation of Zero Suicide best practices is recommended by the US Office of the Surgeon General (2012) and the Joint Commission (2016). The International Association of Suicide Prevention endorsed the preparation of the International Zero Suicide Declaration (IIMHL, 2016), which has inspired its implementation in Canada, Australia, New Zealand, the United Kingdom, and the Netherlands.
Concerns
In response to these developments, colleagues have argued that although laudable and appealing, the pursuit of zero suicides is irrational and inappropriate because it is unrealistic and may be distressing or upsetting to people directly involved. Coyne (2016) pointed at the absence of “extraordinary evidence” to support the “extraordinary claim” that a goal of zero suicides can be achieved and cautioned that the appealing goal of zero suicides can be misused to serve other interests (e.g., political, religious, commercial; or organizational window dressing) than suicide prevention per se. Smith et al. (2015) argued that the pursuit of zero suicides will evoke further “dysregulation” in clinicians working with people at risk of suicide. They suppose this will make matters worse with clinicians having more negative feelings about patients, using an inappropriate narrow focus on diagnosis and risk assessment, and making more ad hoc, abrupt, and inconsistent decisions. They proposed to set the more realistic goal of “suicide risk mitigation.” Erlich (2016) proposed to use the label “Envision Zero” arguing that “Zero Suicide” would enhance the already problematic guilt of those who are bereaved as a result of suicide, including clinicians and caregivers. Hawton (2016) commented that Zero Suicide has been introduced in the United Kingdom in various forms without a clear underlying strategy and that it has become a question of using the label rather than implementing a comprehensive suicide prevention program. Urging caution about the enthusiasm for Zero Suicide policies, he suggested use of words like “optimal suicide prevention” to promote action in the field.
Multilevel Systems Approach
Clearly Zero Suicide is an inspirational approach. But given the concerns and objections it has evoked: Is it also a rational approach? Is it even remotely realistic, considering the limited resources in health care and the dearth of evidence‐based treatment of suicidal behaviors? How could it be acceptable for practitioners who face a current reality of losing patients to suicide? To start answering these questions, it is important to point out that the goal of zero suicides pertains to the distinct population of people receiving health care. Furthermore, that Zero Suicide entails a multilevel systems approach to suicide prevention that considers patient safety, staff safety, and suicide prevention to be organizational responsibilities. This approach reflects Reason's (2000) “systems” view on safety that moves away from “a person approach that focuses on the errors of individuals, blaming them for forgetfulness, inattention, or moral weakness.” A systems view on safety focuses on the conditions under which individuals (in the case of suicide prevention: staff and patients) function, and tries to build protective layers to avert or prevent unsafe behaviors, or mitigate their harmful effects. No single layer is perfectly capable of preventing all accidents from happening at all times. Like slices of Swiss cheese, protective layers are lacunar. Accidents occur when the holes in the layers momentarily align. Thus, to achieve safety, multiple layers are required (Figure 1).
Figure 1.
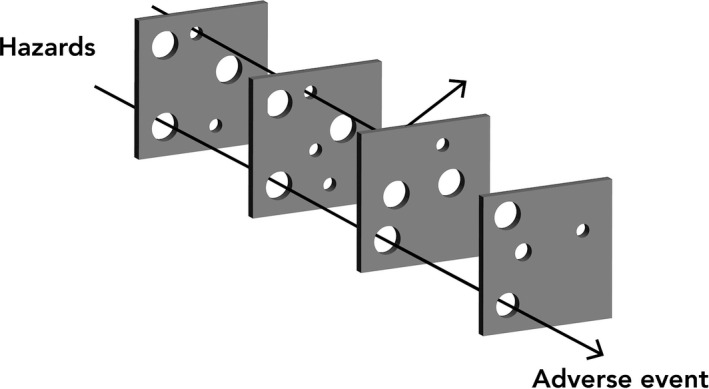
Reason's (2000) Swiss cheese model.
For the purpose of suicide prevention, a variety of defenses can be derived from systematic reviews of suicide prevention strategies (Zalsman et al., 2016), practice guidelines (e.g., van Hemert, Kerkhof, de Keijser, & Verwey, 2012), and multilevel community suicide prevention approaches (van der Feltz‐Cornelis et al., 2011; Hegerl et al., 2009). In addition to effective and safe treatment, layers of defenses may involve empowerment of people at risk for suicide, including helplines, self‐help, and safety planning; collaboration with relatives and gatekeepers; and restriction of access to lethal means. In addition, protective layers on the organizational level pertain to, for example, workflow and staff capacity; the availability of clear instructions, procedures, and communication lines; levels of training and supervision of the workforce; accessibility and continuity of care; and supportive information and communications technology and electronic health records.
Core Components
Following the NAASP critical success factors, Zero Suicide core components can be described at three levels (Figure 2): at the practice level—a direct approach of identifying suicidal behavior and treating it as a distinct syndrome using specific, targeted best practices; at the process level—quality and safety improvement to provide highly accessible, reliable, and continuous care processes and routines; and at the organizational level—a safety culture with strong leadership and a system‐wide commitment to the aspirational “stretch goal” of zero suicides. These core components will be reviewed and discussed in light of available evidence.
Figure 2.
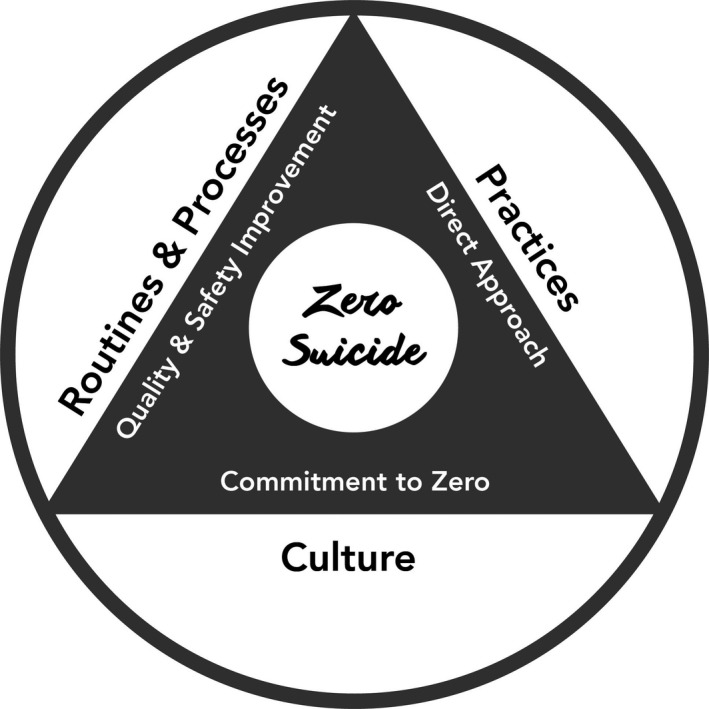
Zero Suicide core components in a health care system.
Direct Approach
Zero Suicide views suicidality as a distinct clinical process or syndrome that requires proactive detection, careful exploration, and specific interventions that directly target suicidal behaviors. This direct approach starts at the entrance of every care pathway, where all patients are screened on past and present suicidal behavior with subsequent full assessment for patients screening positive (Boudreaux & Horowitz, 2014). During treatment, screening is repeated systematically to monitor treatment effects and to capture the occurrence or recurrence of suicidal behaviors. To every patient at risk, direct interventions are offered that address suicidal thoughts and behaviors during treatment and aim at adaptive coping (e.g., dialectical behavior therapy, Linehan et al., 2006; cognitive behavior therapy, Brown et al., 2005; Collaborative Assessment and Management of Suicidality, Jobes, 2012; Attempted Suicide Short Intervention Program, Gysin‐Maillart, Schwab, Soravia, Megert, & Michel, 2016); risk mitigation by safety planning or crisis response planning (Bryan et al., 2017; Stanley & Brown, 2012); and counseling to reduce access to lethal means (e.g., Johnson, Frank, Ciocca, & Barber, 2011). These suicide‐specific interventions are offered in addition to optimal treatment of coexisting mental health problems that elevate the risk of suicide.
While Zalsman et al. (2016) stated that there is insufficient evidence to justify the cost of expensive screening procedures, Coffey (2015) showed that screening can be useful and feasible provided it is embedded in a reliable chain of care where follow‐up on screening outcomes (e.g., referral to a specialist setting) is guaranteed. The practice of addressing suicidal thoughts and behaviors directly during treatment rather than indirectly via the treatment of “underlying” mental illness or processes only is endorsed by recent strong evidence. Based on a systematic review and meta‐analysis comparing the effects of direct interventions and indirect approaches, Meerwijk et al. (2016) showed direct interventions lead to earlier effects than indirect approaches, with a 1.5 lower likelihood of patients dying by suicide or attempting suicide during treatment.
Quality and Safety Improvement
The second component of Zero Suicide is quality and safety improvement leading to the provision of reliable, continuous, and evidence‐based care. This involves the implementation of guidelines and best practices; service redesign involving service users; increasing service access (face to face and online); proactive planning of critical components of care (i.e., intake, screening, assessment, indication, medication, psychosocial therapies); collaboration between staff and patients’ relatives; and organizing continuity of care at critical phases (i.e., transfers, postdischarge). In addition, patients’ no‐show or withdrawal from care is actively responded to. Critical process indicator data are monitored and used to improve workflows, patient safety, and treatment outcomes (Ahmedani et al., 2013). Since quality and safety of care rest on the competence and the confidence of the people who deliver it, all workers are trained to acquire the necessary competences and skills to work with suicidal patients.
Recent quantitative evidence underscores the importance of guideline implementation and the quality of organizations for suicide prevention within health care services. In a national before‐and‐after analysis, While et al. (2012) showed reductions in suicide rates among persons in care in the United Kingdom associated with the implementation of seven, of a total of nine, selected service guideline recommendations. Kapur et al. (2016) demonstrated a 20 to 30% reduction of suicide rates in all mental health services in England associated with each of 16 specific service improvements and implementation of guideline recommendations pertaining to community services, staff training, guideline implementation, and policies aimed at minimizing the effects of discontinuities in care. In addition, this study demonstrated the importance of the organizational factors. As an example, low nonmedical staff turnover in an organization enhanced the preventive effects of implemented suicide prevention best practices. Thus, suicide prevention outcomes in mental health services are related to both the nature of interventions offered and the quality of the organization with which they are offered.
Safety Culture Aimed at Zero Suicides
The third component is a safety culture with a system‐wide commitment to the “stretch goal” of zero suicides within organizations. This means a transformation of a mindset of resigned acceptance of suicide into a mindset of active prevention of suicide as an outcome of treatment. Instead of asking how not to have more suicides than usual, a Zero Suicide organization challenges itself to have no suicides at all. In this respect, Zero Suicide is a member of the “zero accident vision” family of safety approaches in organizations and industries that require very high levels of safety, like aviation, construction, and the automotive industry (Zwetsloot et al., 2013). Zero Suicide is in accordance with expert views on the imperative to improve patient safety (e.g., Berwick et al., 2013; Dixon‐Woods et al., 2014; Leape et al., 2009) that express the need for cultural change, clear goal setting, and the abandoning of blame as an instrument to secure safety.
Transformational approaches aiming at zero preventable harm in very large health care organizations have shown improvement of quality and reduction of mortality and costs within a decade after implementation (Nanji, Ferris, Torchiana, & Meyer, 2013). As an example, Ascension Health, the third largest US health care provider, reported a 21% reduction of mortality among their patients within 3 years of initiation of their “journey towards zero preventable injuries or deaths” (Hilliard et al., 2012; Pryor, Hendrich, Henkel, Beckmann, & Tersigni, 2011). Likewise, within 2 years the Nationwide Children's Hospital Zero Hero program resulted in an 83% reduction of serious safety events, a 53% reduction of preventable harm, a 25% reduction in mortality rate, and a 22% reduction in estimated harm‐related hospital costs (Brilli et al., 2013). These examples illustrate that this level of ambition serves well to rapidly improve and enhance patient safety as well as staff safety: “zero” strategies lead not to more litigation, but less.
Discussion
As presented, Zero Suicide aims for a cultural paradigm shift in health care organizations from resigned acceptance of suicide to active prevention of suicides. It draws health care suicide prevention into the realms of safety science, with an assertive stance toward quality improvement and a commitment to patient and staff safety. Zero Suicide is driven by aspiration, but its core components are rational. Although the available evidence is encouraging, it is clear that there are many unresolved questions and that the evidence base should be strengthened. With Coffey (2006) reporting significant positive financial effects, there is still not enough quantitative evidence to conclude that the costs of Zero Suicide implementation are outweighed by its benefits. Equally important is the question of how Zero Suicide would develop in organizations with a less defined leadership culture and organizational structure than the US Air Force and HFHS. Thus, program evaluation and implementation studies in different health care settings and systems that include health economic analyses are an important next step.
Touching on the issue of the preventability of suicide, the goal and label “Zero Suicide” evokes skepticism and strong concerns. This can be understood in that Zero Suicide is in essence a cultural intervention that affects values, habits, and interests. The current pessimism about the preventability of some suicides provides consolation for society, for health care systems, and for the bereaved, including clinicians. The “promise” of Zero Suicide, its presumption that most if not all suicides can be prevented by excellent health care, offsets a coping style of learned helplessness in health care that is fueled by shame, guilt, and fear of blame (Awenat et al., 2017). In this respect, the concerns expressed by Hawton (2016) and Smith et al. (2015) are justified. Haphazard use of the “Zero Suicide” label without the implementation of its core components and its system approach would be inappropriate and unjust. This would add to already problematic levels of dysregulation in “sick” health care systems (Reason, Carthey, & De Leval, 2001) that are prone to remain unsafe due to a tendency to blame frontline workers and deny systemic errors. The pursuit of zero suicides among patients in health care is only rational in an integral manner that involves practices, processes, and organizational culture across entire health care systems.
Most if not all health care workers would agree to have the mindset that no patient should die alone and in despair by suicide. To overcome reluctance to adopt zero suicides as an aspirational goal, it is of paramount importance that health care leaders empower staff to learn and improve in a genuinely blame‐free working environment: patient safety and staff safety go hand in hand. Still, in some contexts, the words “Zero Suicide” may be too bold or too provocative to be engaging. Perhaps in these instances, suicide prevention may initially be better served with an approach called the “Zero Suicide Mindset,” “Towards Zero Suicide,” or “Every Life Counts.”
Irrespective of labels or semantics, health care suicide prevention is about creating safeguards with patients and their relatives that promote their recovery, that help them have a life worth living, and protect them from self‐harm when they are unable to protect themselves. It will be a long road to achieve this always, for each and every one of our patients. Setting out on this journey, we feel that the goal of zero suicides provides the clarity to direct us, the ambition to help us make strides, and the confidence to encourage us as we proceed along the way. Thus, it is rational to pursue the aspirational goal of zero suicides in health care.
References
- Ahmedani, B. K. , Coffey, J. , & Coffey, C. E. (2013). Collecting mortality data to drive real‐time improvement in suicide prevention. The American Journal of Managed Care, 19, 386–390. [PubMed] [Google Scholar]
- Awenat, Y. , Peters, S. , Shaw‐Nunez, E. , Gooding, P. , Pratt, D. , & Haddock, G. (2017). Staff experiences and perceptions of working with in‐patients who are suicidal: Qualitative analysis. The British Journal of Psychiatry. Advance online publication. 10.1192/bjp.bp.116.191817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick, D. , Bibby, J. , Bisognano, M. , Callaghan, I. , Dalton, D. , Dixon‐Woods, M. , et al. (2013). A promise to learn–A commitment to act: Improving the safety of patients in England. Report of the National Advisory Group on the Safety of Patients in England. Retrieved June 22, 2016, from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/226703/Berwick_Report.pdf
- de Beurs, D. P. , de Groot, M. H. , de Keijser, J. , van Duijn, E. , de Winter, R. F. , & Kerkhof, A. J. (2016). Evaluation of benefit to patients of training mental health professionals in suicide guidelines: Cluster randomised trial. The British Journal of Psychiatry, 208, 477–483. [DOI] [PubMed] [Google Scholar]
- Boudreaux, E. D. , & Horowitz, L. M. (2014). Suicide risk screening and assessment: Designing instruments with dissemination in mind. American Journal of Preventive Medicine, 47, 163–169. [DOI] [PubMed] [Google Scholar]
- Brilli, R. J. , McClead, R. E. , Crandall, W. V. , Stoverock, L. , Berry, J. C. , Wheeler, T. A. , et al. (2013). A comprehensive patient safety program can significantly reduce preventable harm, associated costs, and hospital mortality. The Journal of Pediatrics, 163, 1638–1645. [DOI] [PubMed] [Google Scholar]
- Brown, G. K. , Ten Have, T. , Henriques, G. R. , Xie, S. X. , Hollander, J. E. , & Beck, A. T. (2005). Cognitive therapy for the prevention of suicide attempts: A randomized controlled trial. JAMA, 294, 563–570. [DOI] [PubMed] [Google Scholar]
- Bryan, C. J. , Mintz, J. , Clemans, T. A. , Leeson, B. , Burch, T. S. , Williams, S. R. , et al. (2017). Effect of crisis response planning vs. contracts for safety on suicide risk in US Army soldiers: A randomized clinical trial. Journal of Affective Disorders, 212, 64–72. [DOI] [PubMed] [Google Scholar]
- Burgess, P. , Pirkis, J. , Morton, J. , & Croke, E. (2000). Lessons from a comprehensive clinical audit of users of psychiatric services who committed suicide. Psychiatric Services, 51, 1555–1560. [DOI] [PubMed] [Google Scholar]
- Castelli Dransart, D. A. , Heeb, J. L. , Gulfi, A. , & Gutjahr, E. M. (2015). Stress reactions after a patient suicide and their relations to the profile of mental health professionals. BMC Psychiatry, 15, 265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centraal Bureau voor de Statistiek . (2016). Statline Overledenen, zelfdoding. Retreived June 22, 2016, from http://statline.cbs.nl/Statweb/search/?LA=NL&Q=zelfdoding
- Coffey, C. E. (2006). Pursuing perfect depression care. Psychiatric Services, 57, 1524–1526. [DOI] [PubMed] [Google Scholar]
- Coffey, C. E. (2007). Building a system of perfect depression care in behavioral health. Joint Commission Journal on Quality and Patient Safety, 33, 193–199. [DOI] [PubMed] [Google Scholar]
- Coffey, M. J. (2015). Perfect depression care spread: The traction of zero suicides. Journal of Clinical Outcomes Management, 22(3), 123–129. [Google Scholar]
- Coffey, C. E. , Coffey, M. J. , & Ahmedani, B. K. (2013). An update on perfect depression care. Psychiatric Services, 64, 396. [DOI] [PubMed] [Google Scholar]
- Cooper, J. , Steeg, S. , Bennewith, O. , Lowe, M. , Gunnell, D. , House, A. , et al. (2013). Are hospital services for self‐harm getting better? An observational study examining management, service provision and temporal trends in England British Medical Journal Open, 3, e003444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covington, D. , Hogan, M. , Abreu, J. , Berman, A. , Breux, P. , Coffey, E. , et al. (2011). Suicide care in systems framework. National Action Alliance: Clinical Care & Intervention Task Force Retrieved January 9, 2013, from http://actionallianceforsuicideprevention.org/sites/actionallianceforsuicideprevention.org/files/taskforces/ClinicalCareInterventionReport.pdf.
- Coyne, J. (2016). An open‐minded, skeptical look at the success of “zero suicides”: Any evidence beyond the rhetoric? Retrieved November 15, 2016, from http://blogs.plos.org/mindthebrain/2016/10/28/an-open-minded-skeptical-look-at-the-success-of-zero-suicides-any-evidence-beyond-the-rhetoric/
- Curtin, S. C. , Warner, M. , & Hedegaard, H. (2016). Increase in suicide in the United States, 1999‐2014. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Retreived from https://www.cdc.gov/nchs/products/databriefs/db241.htm.
- Dixon‐Woods, M. , Baker, R. , Charles, K. , Dawson, J. , Jerzembek, G. , Martin, G. , et al. (2014). Culture and behaviour in the English National Health Service: Overview of lessons from a large multi‐method study. BMJ Quality & Safety, 23, 106–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlich, M. D. (2016). Envisioning zero suicide. Psychiatric Services, 67, 255. [DOI] [PubMed] [Google Scholar]
- van der Feltz‐Cornelis, C. M. , Sarchiapone, M. , Postuvan, V. , Volker, D. , Roskar, S. , Roskar, S. , et al. (2011). Best practice elements of multilevel suicide prevention strategies: A review of systematic reviews. Crisis, 32, 319–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies, D. , Chicop, D. , & O'Halloran, P. (2015). Root cause analyses of suicides of mental health clients. Crisis, 36, 316–324. [DOI] [PubMed] [Google Scholar]
- Gysin‐Maillart, A. , Schwab, S. , Soravia, L. , Megert, M. , & Michel, K. (2016). A novel brief therapy for patients who attempt suicide: A 24‐months follow‐up randomized controlled study of the attempted suicide short intervention program (ASSIP). PLoS Medicine, 13(3), e1001968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampton, T. (2010). Depression care effort brings dramatic drop in large HMO population's suicide rate. JAMA, 303, 1903–1905. [DOI] [PubMed] [Google Scholar]
- Hawton, K. (2016). Submission to the U.K. Parliament suicide inquiry. Retrieved March 3, 2017, from http://data.parliament.uk/WrittenEvidence/CommitteeEvidence.svc/EvidenceDocument/Health/Suicide%20Prevention/written/36847.html
- Hegerl, U. , Wittenburg, L. , Arensman, E. , Van Audenhove, C. , Coyne, J. C. , McDaid, D. , et al. (2009). Optimizing suicide prevention programs and their implementation in Europe (OSPI Europe): An evidence‐based multi‐level approach. BMC Public Health, 9, 428 10.1186/1471-2458-9-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hemert, A. , Kerkhof, A. , de Keijser, J. , & Verwey, B. (2012). Multidisciplinaire richtlijn voor diagnostiek en behandeling van suïcidaal gedrag. Utrecht: Nederlandse Vereniging voor Psychiatrie/Nederlands Instituut voor Psychologen/Trimbos Instituut. [Google Scholar]
- Hilliard, M. A. , Sczudlo, R. , Scafidi, L. , Cady, R. , Villard, A. , & Shah, R. (2012). Our journey to zero: Reducing serious safety events by over 70% through high‐reliability techniques and workforce engagement. Journal of Healthcare Risk Management, 32(2), 4–18. [DOI] [PubMed] [Google Scholar]
- Hogan, M. F. (2016). Better suicide screening and prevention are possible. JAMA Psychiatry, 73, 1111–1112. [DOI] [PubMed] [Google Scholar]
- Hogan, M. F. , & Goldstein Grumet, J. (2016). Suicide prevention: An emerging priority for health care. Health Affairs, 35, 1084–1090. [DOI] [PubMed] [Google Scholar]
- Huisman, A. , Robben, P. B. , & Kerkhof, A. J. (2009). An examination of the Dutch Health Care Inspectorate's supervision system for suicides of mental health care users. Psychiatric Services, 60, 80–85. [DOI] [PubMed] [Google Scholar]
- IIMHL . (2016) The international zero suicide declaration. Retrieved June 3, 2016, from https://zerosuicide.org/2016/01/30/international-declaration/.
- Insel, T. (2014). State of the NIMH–mental illness: The view from 2014. Oral presentation. NIMH Alliance for Research Progress.
- Jobes, D. A. (2012). The Collaborative Assessment and Management of Suicidality (CAMS): An evolving evidence‐based clinical approach to suicidal risk. Suicide and Life‐Threatening Behavior, 42, 640–653. [DOI] [PubMed] [Google Scholar]
- Johnson, R. M. , Frank, E. M. , Ciocca, M. , & Barber, C. W. (2011). Training mental healthcare providers to reduce at‐risk patients’ access to lethal means of suicide: Evaluation of the CALM project. Archives of Suicide Research, 15, 259–264. [DOI] [PubMed] [Google Scholar]
- Joint Commission . (2016). Detecting and treating suicide ideation in all settings. Oak Brook, IL: Sentinel Event Alert; Retrieved June 3, 2016, from http://www.jointcommission.org/assets/1/18/SEA_56_Suicide.pdf [PubMed] [Google Scholar]
- Kapur, N. , Ibrahim, S. , While, D. , Baird, A. , Rodway, C. , Hunt, I. M. , et al. (2016). Mental health service changes, organisational factors, and patient suicide in England in 1997–2012: A before‐and‐after study. The Lancet Psychiatry, 3, 526–534. [DOI] [PubMed] [Google Scholar]
- Knox, K. L. , Litts, D. A. , Talcott, G. W. , Feig, J. C. , & Caine, E. D. (2003). Risk of suicide and related adverse outcomes after exposure to a suicide prevention program in the US Air Force: Cohort study. BMJ, 327, 1376–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox, K. L. , Pflanz, S. , Talcott, G. W. , Campise, R. L. , Lavigne, J. E. , Bajorska, A. , et al. (2010). The US Air Force suicide prevention program: Implications for public health policy. American Journal of Public Health, 100, 2457–2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leape, L. , Berwick, D. , Clancy, C. , Conway, J. , Gluck, P. , Guest, J. , et al. (2009). Transforming healthcare: A safety imperative. Quality and Safety in Health Care, 18, 424–428. [DOI] [PubMed] [Google Scholar]
- Linehan, M. M. , Comtois, K. A. , Murray, A. M. , Brown, M. Z. , Gallop, R. J. , Heard, H. L. , et al. (2006). Two‐year randomized controlled trial and follow‐up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry, 63, 757–766. [DOI] [PubMed] [Google Scholar]
- Meerwijk, E. L. , Parekh, A. , Oquendo, M. A. , Allen, I. E. , Franck, L. S. , & Lee, K. A. (2016). Direct versus indirect psychosocial and behavioural interventions to prevent suicide and suicide attempts: A systematic review and meta‐analysis. The Lancet Psychiatry, 3, 544–554. [DOI] [PubMed] [Google Scholar]
- Nanji, K. C. , Ferris, T. G. , Torchiana, D. F. , & Meyer, G. S. (2013). Overarching goals: A strategy for improving healthcare quality and safety? BMJ Quality & Safety, 22(3), 187–193. [DOI] [PubMed] [Google Scholar]
- office of the surgeon general, national action alliance for suicide prevention . (2012). National strategy for suicide prevention: Goals and objectives for action. Washington, DC: Department of Health and Human Services; Retrieved June 3, 2016, from https://www.surgeongeneral.gov/library/reports/national-strategy-suicide-prevention/index.html [PubMed] [Google Scholar]
- Pryor, D. , Hendrich, A. , Henkel, R. J. , Beckmann, J. K. , & Tersigni, A. R. (2011). The quality ‘journey’ at Ascension Health: How we've prevented at least 1,500 avoidable deaths a year—And aim to do even better. Health Affairs, 30, 604–611. [DOI] [PubMed] [Google Scholar]
- Reason, J. (2000). Human error: Models and management. BMJ, 320, 768–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reason, J. T. , Carthey, J. , & De Leval, M. R. (2001). Diagnosing “vulnerable system syndrome”: An essential prerequisite to effective risk management. Quality in Health Care, 10(Suppl 2), ii21–ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renaud, J. , Séguin, M. , Lesage, A. D. , Marquette, C. , Choo, B. , & Turecki, G. (2014). Service use and unmet needs in youth suicide: A study of trajectories. Canadian Journal of Psychiatry, 59, 523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz, W. M. Jr , Allen, M. H. , Feldman, B. N. , Gutin, N. J. , Jahn, D. R. , Kleespies, P. M. , et al. (2012). Preventing suicide through improved training in suicide risk assessment and care: An American Association of Suicidology Task Force report addressing serious gaps in U.S. mental health training. Suicide and Life‐Threatening Behavior, 42, 292–304. [DOI] [PubMed] [Google Scholar]
- Smith, M. J. , Bouch, J. , Bradstreet, S. , Lakey, T. , Nightingale, A. , & O'Connor, R. C. (2015). Health services, suicide, and self‐harm: Patient distress and system anxiety. The Lancet Psychiatry, 2, 275–280. [DOI] [PubMed] [Google Scholar]
- Stanley, B. , & Brown, G. K. (2012). Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256–264. [Google Scholar]
- Suicide Prevention Resource Centre , (2016). Zero Suicide in health and behavioral health care. Retrieved June 3 2016 from http://zerosuicide.sprc.org/
- Taylor, T. L. , Hawton, K. , Fortune, S. , & Kapur, N. (2009). Attitudes towards clinical services among people who self‐harm: Systematic review. The British Journal of Psychiatry, 194(2), 104–110. [DOI] [PubMed] [Google Scholar]
- While, D. , Bickley, H. , Roscoe, A. , Windfuhr, K. , Rahman, S. , Shaw, J. , et al. (2012). Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: A cross‐sectional and before‐and‐after observational study. The Lancet, 379, 1005–1012. [DOI] [PubMed] [Google Scholar]
- Zalsman, G. , Hawton, K. , Wasserman, D. , van Heeringen, K. , Arensman, E. , Sarchiapone, M. , et al. (2016). Suicide prevention strategies revisited: 10‐year systematic review. The Lancet Psychiatry, 7, 646–659. [DOI] [PubMed] [Google Scholar]
- Zwetsloot, G. I. , Aaltonen, M. , Wybo, J. L. , Saari, J. , Kines, P. , & De Beeck, R. O. (2013). The case for research into the zero accident vision. Safety Science, 58, 41–48. [Google Scholar]


