Abstract
IMPORTANCE
The Advisory Committee on Immunization Practices (ACIP) recommends the tetanus, diphtheria, and acellular pertussis (Tdap) vaccine for pregnant women during each pregnancy, regardless of prior immunization status. However, safety data on repeated Tdap vaccination in pregnancy is lacking.
OBJECTIVE
To determine whether receipt of Tdap vaccine during pregnancy administered in close intervals from prior tetanus-containing vaccinations is associated with acute adverse events in mothers and adverse birth outcomes in neonates.
DESIGN, SETTING, AND PARTICIPANTS
A retrospective cohort study in 29 155 pregnant women aged 14 through 49 years from January 1,2007, through November 15,2013, using data from 7 Vaccine Safety Datalink sites in California, Colorado, Minnesota, Oregon, Washington, and Wisconsin.
EXPOSURES
Women who received Tdap in pregnancy following a prior tetanus-containing vaccine less than 2 years before, 2 to 5 years before, and more than 5 years before.
MAIN OUTCOMES AND MEASURES
Acute adverse events (fever, allergy, and local reactions) and adverse birth outcomes (small for gestational age, preterm delivery, and low birth weight) were evaluated. Women who were vaccinated with Tdap in pregnancy and had a prior tetanus-containing vaccine more than 5 years before served as controls.
RESULTS
There were no statistically significant differences in rates of medically attended acute adverse events or adverse birth outcomes related to timing since prior tetanus-containing vaccination.
| Time Since Prior Tetanus-Containing Vaccination, y |
|||
|---|---|---|---|
| Outcome | <2 | 2–5 | >5 (Control) |
| Local reactions, rate/10 000 women | 4.2 | 7.0 | 11.2 |
| Adjusted risk ratio (95% CI) | 0.49 (0.11–2.20) | 0.77 (0.31–1.95) | 1 [Reference] |
| P value | .35 | .59 | |
| Preterm delivery, % | 6.6 | 6.4 | 6.8 |
| Adjusted risk ratio (95% CI) | 1.15 (0.98–1.34) | 1.06 (0.94–1.19) | 1 [Reference] |
| P value | .08 | .33 | |
| Small for gestational age, % | 9.0 | 8.7 | 9.1 |
| Adjusted risk ratio (95% CI) | 0.99 (0.87–1.13) | 0.96 (0.87–1.06) | 1 [Reference] |
| P value | .88 | .45 | |
CONCLUSIONS AND RELEVANCE
Among women who received Tdap vaccination during pregnancy, there was no increased risk of acute adverse events or adverse birth outcomes for those who had been previously vaccinated less than 2 years before or 2 to 5 years before compared with those who had been vaccinated more than 5 years before. These findings suggest that relatively recent receipt of a prior tetanus-containing vaccination does not increase risk after Tdap vaccination in pregnancy.
Pertussis (whooping cough) is a vaccine-preventable illness that has been increasing in incidence over the past decade in the United States.1–3 Neonates and infants are at increased risk of pertussis-related hospitalization and death compared with older children and adults. Many public health strategies have been recommended to decrease the burden of pertussis in neonates and infants.4–6 Most recently, in 2012, the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommended tetanus, diphtheria, and acellular pertussis (Tdap) vaccination for all pregnant women during each pregnancy regardless of prior immunization status.6
However, few published studies have evaluated the safety of Tdap vaccine in pregnant women.7–11 In these studies, Tdap vaccination during pregnancy has not been associated with an increased risk of spontaneous abortion, stillbirth, preterm delivery, low birth weight, neonatal complications, or congenital anomalies compared with unvaccinated pregnant controls. Additionally, 1 retrospective study showed that pregnant women vaccinated with Tdap who had received a prior Tdap vaccine within 5 years had no difference in neonatal outcomes compared with women receiving their first Tdap vaccine in pregnancy.11
Most safety studies on administering repeated doses of tetanus-containing vaccines are limited to nonpregnant individuals.12–14 These studies have shown that intervals less than 5 years between tetanus-containing vaccines can be associated with increased local reactions and fever. Although these studies did not find an increased risk of Arthus reactions (severe dermal inflammation, endothelial damage, and vascular necrosis), this has been a concern with shortened intervals between tetanus vaccine doses.12–14
This study focused on determining whether there is association between receipt of Tdap vaccine during pregnancy administered in close intervals from prior tetanus-containing vaccinations and acute adverse events in mothers and adverse birth outcomes in neonates.
Methods
Study Population
The study protocol was reviewed and approved by institutional review boards at Emory University, the CDC, and the 7 Vaccine Safety Datalink (VSD) sites and was determined exempt from requiring participant consent. The study cohort included pregnant women enrolled in the VSD (Figure). The VSD is a collaborative project between the CDC and 9 integrated health care organizations.15 The VSD includes data on more than 9 million individuals annually (approximately 3% of the US population), with an annual birth cohort of approximately 90 000. Data are collected from standardized files prepared at each site that contain individual demographic, enrollment, immunization, hospitalization, emergency department visits, and outpatient visits. For this study, 7 VSD sites contributed data: Group Health Cooperative (Washington), Kaiser Permanente Northwest (Oregon and Washington), Kaiser Permanente Northern California, Southern California Kaiser Permanente, HealthPartners (Minnesota), Marshfield Clinic (Wisconsin), and Kaiser Permanente Colorado. These sites were chosen because they contribute pregnancy data on a yearly basis. Although the majority of the VSD data comes from the 2 California sites, and thus the western United States, the demographic characteristics of the VSD population have been shown to be generally comparable with that of the entire US population.16
Figure. Tdap Vaccinations Received During Pregnancy From January 1, 2007, Through November 15, 2013, Recorded in 7 Vaccine Safety Datalink Sites.
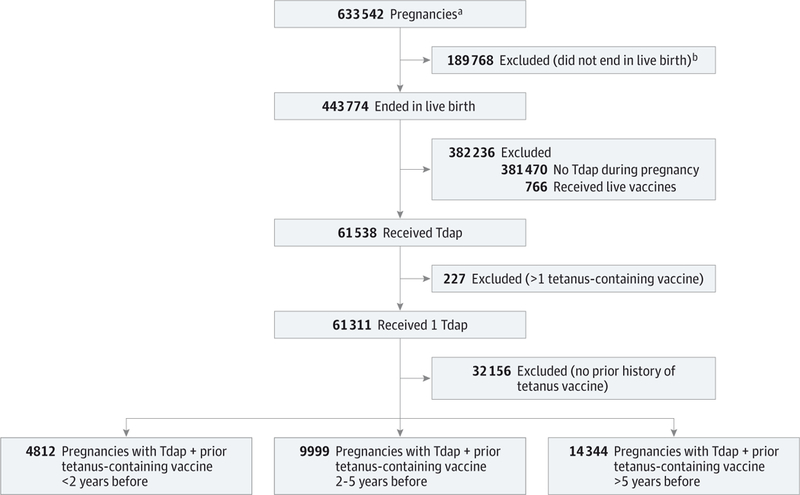
Tdap indicates tetanus, diphtheria, and acellular pertussis.
a Singleton pregnancies.
b Not live birth includes stillbirth, spontaneous abortion, therapeutic abortion, trophoblastic disease, ectopic pregnancy, and unknown outcomes.
Study Design
We conducted a retrospective cohort study among pregnant women vaccinated with Tdap by evaluating medically attended acute adverse events (occurring in outpatient, inpatient, and emergency department settings) in mothers and adverse birth outcomes in their neonates. We compared adverse events between women receiving a prior tetanus-containing vaccine less than 2 years before and 2 to 5 years before with women who had received a prior tetanus-containing vaccine more than 5 years before (controls). We chose these comparisons based on intervals used in prior studies comparing acute adverse events following multiple tetanus-containing vaccines in nonpregnant individuals.12–14 Prior vaccination status was irrespective of pregnancy status at the time of vaccination.
We identified pregnancies ending between January 1,2007, and November 15, 2013, in automated data using a validated pregnancy algorithm17 that has been used in prior VSD pregnancy studies.18,19 This pregnancy episode algorithm uses claims, administrative, and birth data from the electronic medical record to identify pregnancies, pregnancy outcomes, and gestational age at pregnancy outcome, and has been shown to be accurate within 28 days in confirming the estimated pregnancy start date for 99% of live births and in confirming the pregnancy outcome date for 96% of live births.17
We included women aged 14 through 49 years who received Tdap vaccine during pregnancy and had continuous insurance coverage from 6 months prior to pregnancy to 6 weeks postpartum with no more than a 30-day gap in enrollment. We excluded women who had no documentation of prior tetanus-containing vaccines, women who received live vaccines during pregnancy, and women with a multiple gestation pregnancy. We also excluded pregnancies with non-live birth outcomes (stillborn, spontaneous abortion, therapeutic abortion, trophoblastic disease, and ectopic pregnancy) because we did not have the resources to access medical records to confirm the timing of these outcomes in relation to vaccination, which could result in inaccurate findings. Finally, we excluded all women who received non-Tdap tetanus-containing vaccines during pregnancy (ie, tetanus diphtheria [Td]).
We identified vaccinations using electronic medical record and insurance claims data that are captured in the standardized VSD vaccine file. We defined a vaccine administered during pregnancy as one given from 7 days after the woman’s last menstrual period through 7 days before the date the pregnancy ended. We used these cutoffs to avoid misclassification of vaccines that might have been given prior to pregnancy or postpartum.10,19
Outcome Measures
We compared International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for fever, local reactions (limb pain, limb swelling, cellulitis, lymphadenitis, and Arthus reaction), and allergic reactions (allergy, urti-caria, and anaphylaxis) occurring in intervals of 0 through 3 days and 0 through 7 days following Tdap vaccine, excluding duplicate diagnoses that had been given in the previous 30 days to capture incident cases associated with a health care visit. The day of vaccination was considered day 0, and we excluded any diagnoses on day 0 occurring in the outpatient setting, as they were likely present before the vaccination. As some allergic reactions may occur on day 0 in the outpatient setting, we performed a sensitivity analysis including diagnoses of allergic reactions in the outpatient setting on the day of vaccination. We compared the risk of incident cases of Guillain-Barré syndrome in the inpatient setting, using a 1-through 42-day time window following vaccination. We also examined the following adverse birth outcomes: preterm delivery (defined as gestational age <37 weeks), low birth weight (birth weight <2500 g), and small for gestational age (weight <10th percentile for gestational age and sex).20
Statistical Methods
We compared baseline characteristics between the 3 groups of pregnant women who received Tdap vaccine. We used χ2 tests to compare categorical variables, and analysis of variance to compare continuous variables. We identified all adverse events using ICD-9-CM codes. We used log-binomial regression analysis to calculate the relative risks (RRs) for both rare and non-rare events. Akaike Information Criterion measurements are included as assessments of model fit (eTable1 in the Supplement). We adjusted for differences in gestational age at time of vaccination and VSD site (Kaiser Permanente Northern California, Southern California Kaiser Permanente, or other site) when comparing acute events. When comparing birth outcomes, we also adjusted for maternal age, length of enrollment (in months) in the health plan prior to pregnancy, risk factors for pregnancy adverse events, pregnancy complications, and prenatal care utilization, because these are likely to independently affect birth outcomes. Prenatal care utilization was assessed using the Kotelchuck Adequacy of Prenatal Care Utilization Index, which takes into account the number of prenatal care visits from the time of the first prenatal care visit until delivery.21 Comorbidities (asthma, diabetes, hypertension, and cardiovascular disease) and pregnancy complications were identified usingICD-9-CM codes. Only records that contained information on the neonate (ie, weight and gestational age) were used when analyzing birth outcomes. In addition, only vaccinations given prior to 37 weeks of gestation were included, so as to not bias the results for preterm delivery and low birth weight. All analyses were performed using SAS (SAS Institute), version 9.3.
We performed a priori power calculations based on an expected sample size of 24 000 women and determined that we had 80% or higher power to detect an RR greater than 2 for all of our birth outcomes. However, analyses for medically attended acute adverse outcomes, which are rare, were under-powered. To detect an RR greater than 2 for local reactions, 10 000 participants would be needed in each cohort; for fever, 37 000 participants; and for allergic reactions, 75 000 participants. We considered results to be statistically significant at an a error less than .05 using 2-tailed tests.
Results
From January 1, 2007, through November 15,2013, there were a total of 633 542 singleton pregnancies recorded in the VSD sites (Figure). After applying exclusion criteria, we identified 61 311 pregnancies in which a single Tdap vaccine was given. We excluded 32 156 pregnancies (52%) because there was no prior history of a tetanus-containing vaccine documented. Our final analytic data set included 29 155 pregnancies. Of these pregnancies, 4812 women (17%) had a prior tetanus-containing vaccine less than 2 years before, 9999 women (34%) 2 to 5 years before, and 14 344 women (49%) more than 5 years before (controls).
Among the 29 155 pregnancies ending from 2007 through 2013, the majority of Tdap vaccinations were administered from 2010 through 2013 (98.1%), and most were administered in 2013 (54.0%). In the overall cohort, Tdap was most often administered in the third trimester (67.4%). Fewer women received the vaccine in the second trimester (27.5%) and the first trimester (5.1%). Maternal age, length of enrollment, and gestational age at Tdap vaccination were significantly different in the 3 study groups (P = <.001) (Table 1). In addition, most pregnant women who received a prior tetanus-containing vaccine less than 2 years before (94%) and 2 to 5 years before (85%) their current Tdap vaccine had previously received Tdap (as opposed to a non-Tdap tetanus-containing vaccine) vs only 17% of controls (P <.001).
Table 1.
Selected Demographic Characteristics of Pregnant Women Who Received Tdap During Pregnancy by Vaccination Status Recorded in the Vaccine Safety Datalink Sites From January 1, 2007, Through November 15, 2013
| No. (%) |
||||
|---|---|---|---|---|
| Time Since Prior Tetanus-Containing Vaccination, y |
||||
| Variable | <2 (n = 4812) |
2–5 (n = 9999) |
>5 (Control) (n = 14 344) |
P Value |
| Maternal age, mean (range), y | 30.5 (15–49) | 30.7 (14–49) | 28.8 (14–48) | <.001 |
| Enrollment prior to pregnancy, mean (range), mo | 49.8 (6.0–99.9) | 62.4 (6.0–100.5) | 63.9 (6.0–99.8) | <.001 |
| Gestational age at Tdap, mean (range), wk | 30 (1–39) | 30 (1–41) | 27 (1–40) | <.001 |
| Adequate prenatal carea | 3629 (75) | 7324 (73) | 10 542 (73) | .01 |
| Other vaccines in pregnancy | 3012 (63) | 6179 (62) | 8996 (63) | .33 |
| Maternal comorbidityb | 1383 (29) | 2956 (30) | 4394 (31) | .03 |
| Pregnancy complicationc | 2514(52) | 5230 (52) | 7565 (53) | .74 |
| Prior tetanus vaccine Tdapd | 4542 (94) | 8511 (85) | 2477 (17) | <.001 |
Abbreviation: Tdap, tetanus, diphtheria, and acellular pertussis.
Adequate or adequate plus prenatal care based on Kotelchuck Adequacy of Prenatal Care Utilization Index.
Presence of hypertension in pregnancy, diabetes, cardiovascular disease, or asthma.
Includes any of the following diagnoses: fetal abnormality affecting maternal management, fetal or placental problems affecting maternal management, polyhydramnios, oligohydramnios, premature rupture of membranes, amnionitis, antepartum hemorrhage, placental abruption, placenta previa, or antepartum complications.
Compared with non-Tdap tetanus vaccines (ie, tetanus diphtheria; tetanus toxoid; diphtheria and tetanus toxoids and acellular pertussis, etc).
Acute Outcomes
Overall, acute adverse events after vaccination were rare (eTables 2–3 in the Supplement). There were no statistically significant differences in fever, allergic reactions, or local reactions among women who had received their prior tetanus-containing vaccine less than 2 years before and 2 to 5 years before compared with controls (Table 2). Fever beginning 0 through 3 days after vaccination occurred at a rate (per 10 000 women) of 2.1 in those who received Tdap and had a prior tetanus-containing vaccine less than 2 years before compared with 3.5 among controls (adjusted RR, 0.66 [95% CI, 0.07–5.77]; P = .70). Allergic reactions beginning 0 through 3 days after vaccination occurred at a rate (per 10 000 women) of 2.1 in women who received Tdap and had a prior tetanus-containing vaccine less than 2 years before (adjusted RR, 1.55 [95% CI, 0.13–18.45]; P = .73) and 1.0 in those receiving it 2 to 5 years before (adjusted RR, 0.71 [95% CI, 0.06–8.13]; P = .78) compared with 1.4 among controls. Local reactions beginning 0 through 3 days after vaccination occurred at a rate (per 10 000 women) of 4.2 in women who received Tdap and had a prior tetanus-containing vaccine less than 2 years before (adjusted RR, 0.49 [95% CI, 0.112.20]; P = .35) and 7.0 in those receiving it 2 to 5 years before (adjusted RR, 0.77 [95% CI, 0.31–1.95]; P = .59) compared with 11.2 among controls. There was no increased risk of allergic reactions based on the sensitivity analysis including outpatient diagnoses occurring on day 0 (eTable 4 in the Supplement). There were no cases of anaphylaxis, Arthus reactions, or Guillain-Barré syndrome following vaccination.
Table 2.
Acute Outcomes Following Tdap Vaccination in Pregnancy By Interval Since Prior Tetanus-Containing Vaccination
| Time Since Prior Tetanus-Containing Vaccination, y |
Relative Risk (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <2 (n = 4812) |
2–5 (n = 9999) |
>5 (Control) (n = 14 344) |
<2 y vs Control |
2–5 y vs Control |
||||||
| Outcome | No. of Patients |
Ratea | No. of Patients |
Ratea | No. of Patients |
Ratea | Unadjustedb | Adjustedb,c | Unadjustedd | Adjustedc,d |
| Fever | ||||||||||
| 0–3 d | 1 | 2.1 | 0 | 0 | 5 | 3.5 | 0.60 (0.07–5.10) | 0.66 (0.07–5.77) | ||
| 0–7 d | 3 | 6.2 | 1 | 1.0 | 6 | 4.2 | 1.49 (0.37–5.96) | 1.61 (0.39–6.66) | 0.24 (0.03–1.99) | 0.21 (0.03–1.80) |
| Allergic Reaction | ||||||||||
| 0–3 d | 1 | 2.1 | 1 | 1.0 | 2 | 1.4 | 1.49 (0.14–16.4) | 1.55 (0.13–18.45) | 0.72 (0.07–7.91) | 0.71 (0.06–8.13) |
| 0–7 d | 2 | 4.2 | 4 | 4.0 | 5 | 3.5 | 1.19 (0.23–6.14) | 1.32 (0.24–7.17) | 1.15 (0.31–4.27) | 1.23 (0.32–4.80) |
| Local Reaction | ||||||||||
| 0–3 d | 2 | 4.2 | 7 | 7.0 | 16 | 11.2 | 0.37 (0.09–1.62) | 0.49 (0.11–2.20) | 0.63 (0.26–1.53) | 0.77 (0.31–1.95) |
| 0–7 d | 6 | 12.5 | 17 | 17.0 | 22 | 15.3 | 0.81 (0.33–2.00) | 1.01 (0.40–2.56) | 1.11 (0.59–2.09) | 1.28 (0.66–2.47) |
Abbreviation: Tdap, tetanus, diphtheria, and acellular pertussis.
Rate per10 000 women.
Tdap + prior tetanus less than 2years before compared with Tdap + prior tetanus more than 5years before.
Adjusting for Vaccine Safety Datalink site and gestational age at vaccination in weeks.
Tdap + prior tetanus 2 to 5years before compared with Tdap + prior tetanus more than 5 years before.
Birth Outcomes
There were no statistically significant differences in adverse birth outcomes among women who had received their prior tetanus-containing vaccine less than 2 years before and 2 to 5 years before compared with controls (Table 3). Preterm delivery occurred in 6.6% of women who received Tdap and had a prior tetanus-containing vaccine less than 2 years before (adjusted RR, 1.15 [95% CI, 0.98–1.34]; P = .08) and 6.4% of those receiving it 2 to 5 years before (adjusted RR, 1.06 [95% CI, 0.94–1.19]; P = .33) compared with 6.8% of controls. Low-birth-weight delivery occurred in 4.7% of women who received Tdap and had a prior tetanus-containing vaccine less than 2 years before (adjusted RR, 1.10 [95% CI, 0.92–1.32]; P = .31) and4.7% of those receiving it2to5 years before (adjusted RR, 1.03 [95% CI, 0.89–1.18]; P = .72) compared with 5.1% of controls. Small for gestational age delivery occurred in 9.0% of women who received Tdap and had a prior tetanus-containing vaccine less than 2 years before (adjusted RR, 0.99 [95% CI, 0.87–1.13]; P = .88) and 8.7% of those receiving it2to5 years before (adjusted RR, 0.96 [95% CI, 0.87–1.06]; P = .45) compared with 9.1% of controls.
Table 3.
Adverse Birth Outcomes Following Tdap Vaccination in Pregnancy by Interval Since Prior Tetanus-Containing Vaccination
| No. (%) |
|||||||
|---|---|---|---|---|---|---|---|
| Time Since Prior Tetanus-Containing Vaccination, y |
Relative Risk (95% CI) |
||||||
| Outcome | <2 (n = 3313) |
2–5 (n = 7226) |
>5 (Control) (n = 10 633) |
<2 y vs Control |
2–5 y vs Contro |
||
| Unadjusteda | Adjusteda,b | Unadjustedc | Adjustedb,c | ||||
| Preterm deliveryd | 218 (6.6) | 460 (6.4) | 723 (6.8) | 0.97 (0.84–1.12) | 1.15 (0.98–1.34) | 0.94 (0.84–1.05) | 1.06 (0.94–1.19) |
| Low birth weighte | 156 (4.7) | 342 (4.7) | 543 (5.1) | 0.92 (0.78–1.10) | 1.10 (0.92–1.32) | 0.93 (0.81–1.06) | 1.03 (0.89–1.18) |
| Small for gestational agef | 298 (9.0) | 629 (8.7) | 996 (9.1) | 0.99 (0.87–1.12) | 0.99 (0.87–1.13) | 0.96 (0.87–1.05) | 0.96 (0.87–1.06) |
Abbreviation: Tdap, tetanus, diphtheria, and acellular pertussis.
Tdap + prior tetanus less than 2 years before compared with Tdap + prior tetanus more than 5 years before.
Adjusting for gestational age at Tdap vaccination in weeks, Vaccine Safety Datalink site, length of enrollment (in months), prenatal care utilization index, maternal comorbidity, pregnancy complication, and maternal age.
Tdap + prior tetanus 2 to 5 years before compared with Tdap + prior tetanus more than 5 years before.
Gestational age of less than 37 weeks.
Birth weight of less than 2500 g.
Weight of less than the 10th percentile for gestational age and sex.
Discussion
To our knowledge, this is the first study to evaluate medically attended acute adverse outcomes in mothers following Tdap vaccine in pregnancy looking specifically at intervals since receipt of prior tetanus-containing vaccinations. We did not find any differences in acute events in the mothers or adverse birth outcomes in neonates when comparing women who were vaccinated with Tdap during pregnancy regardless of the length of time since a prior tetanus-containing vaccine. Our findings should reassure patients and clinicians who might be hesitant to give Tdap vaccine to pregnant women who recently received a Tdap or other tetanus-containing vaccination.
Our findings are similar to another retrospective cohort study evaluating women receiving Tdap in pregnancy who had a prior pregnancy with Tdap vaccine administered within 5 years compared with multiparous women with no prior Tdap vaccine in pregnancy.11 This study found no difference in gestational age at delivery, stillbirth, major malformations, neonatal care admissions, ventilation requirements, and neonatal death, whereas ours focused on preterm delivery, small for gestational age, and low birth weight. The prior study did note a small increase in average birth weight of neonates of women receiving multiple Tdap vaccines. Our study did not compare actual birth weights, but rather compared the presence of low-birth-weight (<2500 g) delivery, and did not find a statistically significant difference.
Our findings contrast with some studies in other populations that suggest an increased risk of adverse events when tetanus-containing vaccines are given at short intervals, most of which evaluated differences in solicited adverse events.12–14 In 2006, a clinical trial of 7156 children found that Tdap vaccine was well tolerated when given at intervals as short as 18 months since prior tetanus-containing vaccines; however, there was an increase in solicited injection site swelling and erythema in participants who received a tetanus-containing vaccine more recently.12 A VSD retrospective cohort study of 436 828 Td vaccinations demonstrated that medically attended local reactions, including cellulitis, were more common among persons who received a Td-containing vaccine within the last 5 years compared with a longer interval.13 Another study assessed safety in 4524 Tdap-vaccinated health care workers during a pertussis outbreak in New England.14 Overall, there was no difference in the rates of solicited moderate or severe injection site reactions, but there was an increase in redness, swelling, and subjective fever among patients who had received their prior Td-containing vaccine less than 2 years earlier. Among 20 pregnant women included in that study, only 1 person reported severe swelling and 2 reported feeling feverish without documented fever. All symptoms in these pregnant women resolved without treatment, and all neonates were born at term with normal newborn evaluations. None of the pregnant women had received a prior tetanus-containing vaccine 2 years before their Tdap vaccination.
One explanation of the apparent paucity of acute adverse events with short tetanus vaccination intervals in our study could be related to shifts in immunological responses that occur during pregnancy.22 These include shifts in humoraland cellular-mediated immunity and natural killer cells that occur to protect the fetus from harm. Among other changes, there may be less inflammation that occurs in response to vaccinations, which may result in fewer adverse events following multiple tetanus-containing vaccinations given in close proximity. Another explanation could be that we relied exclusively on medically attended adverse events, which are rare, whereas the majority of prior studies included solicited adverse events. Therefore, milder reactions that do not come to medical care might not have been included.
Our study has some limitations. We had limited power for the acute adverse events analysis. However, the rates of acute adverse events were generally not more common in pregnant women who had more recent tetanus-containing vaccinations. We also excluded women with no prior documented tetanus-containing vaccination, which comprised 52% of the Tdap-vaccinated cohort, to reduce misclassification. Although it is unlikely that these women never received a tetanus-containing vaccine in the past, this exclusion allowed for more conservative estimates of risk as the cohorts were not diluted with women that were potentially previously unvaccinated. There is the potential for some confounding due to differences in the type of vaccine received because the majority of the women in our study who were vaccinated with tetanus-containing vaccines less than 2 years before received Tdap and those vaccinated more than 5 years before had previously received Td. Additionally, we did not review medical charts to validate the adverse events, which would correct for any potential overestimation of the rates of acute reactions following Tdap in pregnancy. Although this is important, we would expect any resulting misclassification bias to be nondifferential, and not to affect our overall results. Finally, the VSD population is an insured population, and these findings may not be generalizable to the entire US population. However, demographic characteristics of the VSD population, including race, ethnicity, income, and education, have been shown to be generally comparable with the population of the United States.16
Future studies are needed to determine if there are differences in other important adverse pregnancy outcomes, such as stillbirth and spontaneous abortion, when Tdap is given in pregnancy in close intervals from prior tetanus-containing vaccines.
Conclusions
Among women who received Tdap vaccination during pregnancy, there was no increased risk of acute adverse events or adverse birth outcomes for those who had been previously vaccinated less than 2 years before or 2 to 5 years before compared with those who had been vaccinated more than 5 years before. These findings suggest that relatively recent receipt of a prior tetanus-containing vaccination does not increase risk after Tdap vaccination in pregnancy.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported by the Centers for Disease Control and Prevention and grant T32AI074492 from the National Institute of Allergy and Infectious Diseases (Dr Sukumaran).
Role of the Funder/Sponsor: The funders of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation or review of the manuscript; and decision to submit the manuscript for publication. The manuscript was approved by the Centers for Disease Control and Prevention clearance process.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Sukumaran reports receiving research support from the National Institutes of Health. Dr Naleway reports receiving research support from GlaxoSmithKline and Pfizer. Dr Klein reports receiving research support from GlaxoSmithKline, Sanofi Pasteur, Merck, Pfizer, Nuron Biotech, MedImmune, Novartis, and Protein Science. The Vaccine Safety Datalink Project is funded by the Centers for Disease Control and Prevention.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official policy or position of the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, or the National Institutes of Health.
Contributor Information
Lakshmi Sukumaran, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia; Department of Pediatrics, Emory University School of Medicine, Atlanta, Georgia.
Natalie L. McCarthy, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia.
Elyse O. Kharbanda, HealthPartners Institute for Education and Research, Minneapolis,Minnesota.
Michael M. McNeil, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia.
Allison L. Naleway, The Center for Health Research, Kaiser Permanente Northwest, Portland, Oregon.
Nicola P. Klein, Kaiser Permanente Vaccine Study Center, Oakland, California.
Michael L. Jackson, Group Health, Research Institute, Seattle,Washington.
Simon J. Hambidge, Department of Ambulatory Care Services, Denver, Health, Denver, Colorado; Institute for Health Research, Kaiser Permanente Colorado,Denver; Department of Pediatrics, University of Colorado, Denver.
Marlene M. Lugg, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena.
Rongxia Li, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia.
Eric S. Weintraub, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia.
Robert A. Bednarczyk, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Jennifer P. King, Marshfield Clinic Research Foundation, Marshfield,Wisconsin.
Frank DeStefano, Immunization Safety Office, Centers for Disease Control and Prevention, Atlanta, Georgia.
Walter A. Orenstein, Emory Vaccine Center, Emory University, Atlanta, Georgia.
Saad B. Omer, Rollins School of Public Health, Emory University, Atlanta, Georgia; Emory Vaccine Center, Emory University, Atlanta, Georgia.
REFERENCES
- 1.Cherry JD. Epidemic pertussis in 2012—the resurgence of a vaccine-preventable disease. N Engl J Med. 2012;367(9):785–787. [DOI] [PubMed] [Google Scholar]
- 2.Winter K, Glaser C, Watt J, Harriman K; Centers for Disease Control and Prevention (CDC). Pertussis epidemic—California, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(48):1129–1132. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers of Disease Control and Prevention. Pertussis outbreak trends. http://www.cdc.gov/pertussis/outbreaks/trends.html. Accessed May 20, 2015. [Google Scholar]
- 4.Murphy TV, Slade BA, Broder KR, et al. Prevention of pertussis, tetanus, and diphtheria among pregnant and postpartum women and their infants recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57(RR-4):1–51. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices(ACIP),2011.MMWR Morb Mortal Wkly Rep. 2011;60(41):1424–1426. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2013;62(7):131–135. [PMC free article] [PubMed] [Google Scholar]
- 7.Shakib JH, Korgenski K, Sheng X, Varner MW, Pavia AT, Byington CL. Tetanus, diphtheria, acellular pertussis vaccine during pregnancy: pregnancy and infant health outcomes. J Pediatr. 2013;163(5): 1422–1426.e1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munoz FM, Bond NH, Maccato M, et al. Safety and immunogenicity of tetanus diphtheria and acellular pertussis (Tdap) immunization during pregnancy in mothers and infants: a randomized clinical trial. JAMA. 2014;311(17):1760–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donegan K, King B, Bryan P. Safety of pertussis vaccination in pregnant women in the United Kingdom: observational study. BMJ. 2014;349:g4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kharbanda EO, Vazquez-Benitez G, Lipkind HS, et al. Evaluation of the association of maternal pertussis vaccination with obstetric events and birth outcomes. JAMA. 2014;312(18):1897–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan JL, Baggari SR, McIntire DD, Sheffield JS. Pregnancy outcomes after antepartum tetanus, diphtheria, and acellular pertussis vaccination. Obstet Gynecol. 2015;125(6):1433–1438. [DOI] [PubMed] [Google Scholar]
- 12.Halperin SA, Sweet L, Baxendale D, et al. How soon after a prior tetanus-diphtheria vaccination can one give adult formulation tetanus-diphtheria-acellular pertussis vaccine? Pediatr Infect Dis J. 2006;25(3):195–200. [DOI] [PubMed] [Google Scholar]
- 13.Jackson LA, Yu O, Belongia EA, et al. Frequency of medically attended adverse events following tetanus and diphtheria toxoid vaccine in adolescents and young adults: a Vaccine Safety Datalink study. BMC Infect Dis. 2009;9:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Talbot EA, Brown KH, Kirkland KB, Baughman AL, Halperin SA, Broder KR. The safety of immunizing with tetanus-diphtheria-acellular pertussis vaccine (Tdap) less than 2 years following previous tetanus vaccination: Experience during a mass vaccination campaign of health care personnel during a respiratory illness outbreak. Vaccine. 2010;28(50):8001–8007 [DOI] [PubMed] [Google Scholar]
- 15.McNeil MM, Gee J, Weintraub ES, et al. The Vaccine Safety Datalink: successes and challenges monitoring vaccine safety. Vaccine. 2014;32(42): 5390–5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sukumaran L, McCarthy NL, Li R, Weintraub ES, Jacobsen SJ, Hambidge SJ, et al. Demographic characteristics of members of the Vaccine Safety Datalink(VSD): a comparison with the United States population. Vaccine. 2015;33(36):4446–4450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naleway AL, Gold R, Kurosky S, et al. Identifying pregnancy episodes, outcomes, and mother-infant pairs in the Vaccine Safety Datalink. Vaccine. 2013; 31(27):2898–2903. [DOI] [PubMed] [Google Scholar]
- 18.Nordin JD, Kharbanda EO, Benitez GV, et al. Maternal safety of trivalent inactivated influenza vaccine in pregnant women. Obstet Gynecol. 2013; 121(3):519–525. [DOI] [PubMed] [Google Scholar]
- 19.Kharbanda EO, Vazquez-Benitez G, Lipkind H, Naleway A, Lee G, Nordin JD; Vaccine Safety Datalink Team. Inactivated influenza vaccine during pregnancy and risks for adverse obstetric events. Obstet Gynecol. 2013;122(3):659–66 . [DOI] [PubMed] [Google Scholar]
- 20.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kotelchuck M The Adequacy of Prenatal Care Utilization Index: its US distribution and association with low birth weight. Am J Public Health. 1994;84 (9):1486–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Szekeres-Bartho J Immunological relationship between the mother and the fetus. Int Rev Immunol. 2002;21(6):471–495. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


