Abstract
Background
Postoperative pain is a common problem among intensive care patients. Pain management includes pain assessment and documentation, patient care, and pharmacological treatment.
Materials and methods
The study used a prospective, cross-sectional design. Nineteen intensive care nurses and 72 intensive care patients after cardiac surgery with sternotomy approach were studied. Toronto Pain Management Inventory was used to assess nurses and the 2010 Revised American Pain Society Patient Outcome Questionnaire was used to assess the patients. A research protocol was used to document pharmacological treatment data and Visual Analog Scale (VAS) pain measurements. The pharmacological therapy data was available for 72 patients, but patient satisfaction measurements were acquired from 52 patients.
Results
Postoperative pain for intensive care patients after cardiac surgery is mostly mild (68.66%). Pain intensity had a tendency to decrease over time, from a mean VAS score of 4.66 two hours after extubation to a mean VAS score of 3.12 twelve hours after extubation. Mostly opioids (100%) and nonsteroidal anti-inflammatory drugs (NSAIDs, 77.8%) were used for pharmacological treatment, and treatment was adjusted according to pain levels and patient needs. Patient satisfaction regarding pain management in the first 24 hours after surgery was high (94.2%), even though the nurses’ pain knowledge was average (X = 60.6 ± 7.3%).
Conclusions
An individualized pain management plan requires pain documentation and ensures high patient satisfaction. Pain levels after cardiac surgery with sternotomy approach are mostly mild and patient satisfaction is high.
Keywords: intensive care, postoperative pain, cardiac surgery, pain management nursing
Abstract
INTENSYVIOSIOS TERAPIJOS SKYRIAUS PACIENTŲ SKAUSMO VALDYMAS PO ŠIRDIES OPERACIJŲ SU STERNOTOMIJA
Santrauka
Įvadas. Intensyviosios priežiūros skyriaus pacientai susiduria su dažna problema – skausmu po operacijų. Skausmo valdymas apima skausmo vertinimą ir dokumentaciją, pacientų priežiūrą ir farmakologinį gydymą.
Medžiaga ir metodai. Prospektyvinio pjūvinio tyrimu ištirti 72 intensyviosios terapijos pacientai po širdies operacijų su sternotomija ir 19 intensyviosios terapijos slaugytojų. Slaugytojos vertintos naudojant Toronto skausmo valdymo metodiką. Pacientų skausmui nustatyti pasitelktas 2010 m. Amerikos skausmo draugijos pacientų klausimynas, o farmakologinio gydymo duomenų ir skausmo vizualios analogijos skalei (VAS) naudotas tyrimo protokolas. Buvo gauti 72 pacientų farmakologinio gydymo duomenys, tačiau pasitenkinimas skausmo valdymu buvo tirtas tik 52 pacientams.
Rezultatai. Intensyviosiosios terapijos skyriaus pacientų pooperaciniai skausmai po širdies operacijų dažniausiai buvo lengvi (68,66 %). Skausmo intensyvumas laikui bėgant sumažėjo nuo vidutinės VAS skalės (4,66) praėjus dviems valandoms po ekstubacijos iki vidutinio VAS balo (3,12) praėjus 12 valandų po ekstubacijos. Farmakologiniam gydymui dažniausiai naudojami opioidai (100 %) ir nesteroidiniai vaistai nuo uždegimo (NVNU, 77,8 %), o gydymas koreguojamas pagal skausmo lygį ir pacientų poreikius. Pacientų pasitenkinimas skausmo valdymu per pirmąsias 24 valandas po operacijos yra didelis (94,2 %), nors slaugytojų žinios yra vidutinės (X = 60,6 ± 7,3 %).
Išvados. Individualizuotas skausmo valdymo planas reikalauja, kad pacientų skausmas būtų dokumentuojamas, taip geriau pavyksta parinkti tinkamą skausmo mažinimo būdą ir užtikrinti didesnį pacientų pasitenkinimą. Individualizuotam skausmo valdymo planui reikalinga skausmo dokumentacija. Skausmas po širdies operacijų su sternotominiu metodu dažniausiai būna lengvas ir pacientų pasitenkinimas yra didelis.
Raktažodžiai: intensyvi priežiūra, pooperacinis skausmas, širdies chirurgija, skausmo gydymas
INTRODUCTION
Pain is more than a purely physiological phenomenon. Psychological, social, cultural, and environmental aspects all affect the pain experience (1). Postoperative pain is still a common problem among intensive care patients, especially in the surgical intensive care unit (ICU) where the patients are affected not only by surgery but also by critical illness (2).
Pain localization after heart surgery is usually in the chest and the sternum, which is directly connected to the type of surgery the patient has undergone – thoracotomy with sternotomy approach (2–4). Patient pain levels after heart surgery have been described as mild to severe, (2, 5–6) however, in Latvia it has been previously described as mild to moderate (7).
Suboptimal pain management affects patient recovery and rehabilitation, contributes to lengthier hospital stay, and increases the use of healthcare resources (8). Pain experienced during hospital stay is a traumatic memory that negatively affects health-related quality of life. Patients also experience a myriad of physical symptoms, such as weakness, fatigue, sleep disorders, and pain (9–10).
Pain management should be a multidisciplinary effort. In the current clinical setting, nurses are responsible for assessing and documenting pain, administering and titrating medication, as well as monitoring the patient, because nurses spend more time with the patient. A number of studies note the positive effect of the implementation of standardized pain assessment and documentation on patient care (8, 11–13).
Clinics that use pain management protocols have noted an increase in staff education regarding pain management and sedation, and more efficient use of analgesic and sedative medications (14). Benefits of routine pain assessment are a lower incidence of pain, lower pain levels, and decreased use of sedative and analgesic medications. Benefits also include a shorter length of stay in an ICU as well as better patient clinical outcomes and more intensive staff education regarding pain management (13–16).
Although pain should be documented along with received medication, it is often done inconsistently or inadequately (17–18). Pain assessment and documentation practices depend on the competence and knowledge of the healthcare team (15, 19).
In the context of pharmacological treatment of pain, multimodal analgesia is becoming more and more widespread. It includes a combination of different pharmacological agents to decrease the need for opioids and their adverse effects. However, for multimodal analgesia to be carried out in an ICU, a multidisciplinary approach to pain management is needed (14).
Recommendations for postoperative pain management after thoracotomy, including thoracotomy with sternotomy approach, include opioids, NSAIDs or specifically paracetamol (acetaminophen), as well as pregabalin, gabapentin and intravenous ketamine. Recommendations after coronary artery bypass surgeries are similar, except that only paracetamol is recommended from NSAIDs (20).
Several organizational factors, such as a lack of personnel and excess workload, disrupt the efficiency and effectiveness of pain management. Overworked members of staff experience lack of time, which not only prevents them from carrying out their duties in full, but also negatively affects their communication with the patients. A lack of communication has a negative impact on the quality of healthcare in many contexts (8, 21). It is necessary to gather data on patient outcomes and patient satisfaction, and especially on pain management to evaluate the quality of care (1, 22).
Patient satisfaction with pain management is not directly connected with patient pain levels. Patient satisfaction can be high even if they experience high pain levels and patients admit that they are satisfied with the way healthcare workers discuss their pain and listen to their needs. It is not uncommon that nurses primarily educate patients about pain and discuss their pain management (6, 23–24).
Patient satisfaction is affected not only by the effectiveness of pharmacological treatment. Communication and the attitude of healthcare workers is also an important factor (1, 4, 22). The relationship between the patient and the healthcare team is one of the reasons why patients can be satisfied with pain management even if their pain level is high (25).
In summary, pain in intensive care patients after heart surgery continues to be undermanaged and patient satisfaction with pain management is not only affected by the efficacy of pharmacological treatment, but also by the skills and knowledge of the healthcare team. Therefore, the objective of the study was to identify pain management practices and describe patient satisfaction measurements for intensive care patients after cardiac surgery with sternotomy approach at a university hospital in Riga, Latvia.
MATERIALS AND METHODS
Design and objectives
A prospective, cross-sectional design was used to examine the following research objectives: (1) describe knowledge and competence of intensive care nurses, (2) assess postoperative pain for intensive care patients after cardiac surgery with sternotomy approach, (3) gather data about pharmacological treatment options and usage, and (4) assess patient satisfaction measurements regarding pain management in the first 24 hours after surgery. The hypothesis is that satisfaction with pain management is higher if an individualized pain management plan is used depending on patients’ pain levels.
The sample
The data was collected from a convenience sample of consenting nurses and patients in one cardiac surgery ICU at a university hospital in Riga, Latvia. Out of 30 nurses currently working at the ICU, 21 nurses were eligible. The exclusion criteria were as follows: non-participation in patient care (head nurse), a prolonged leave, and weekend-only working schedule. Nineteen nurses returned the questionnaire and 15 questionnaires were filled out fully and therefore eligible for data analysis.
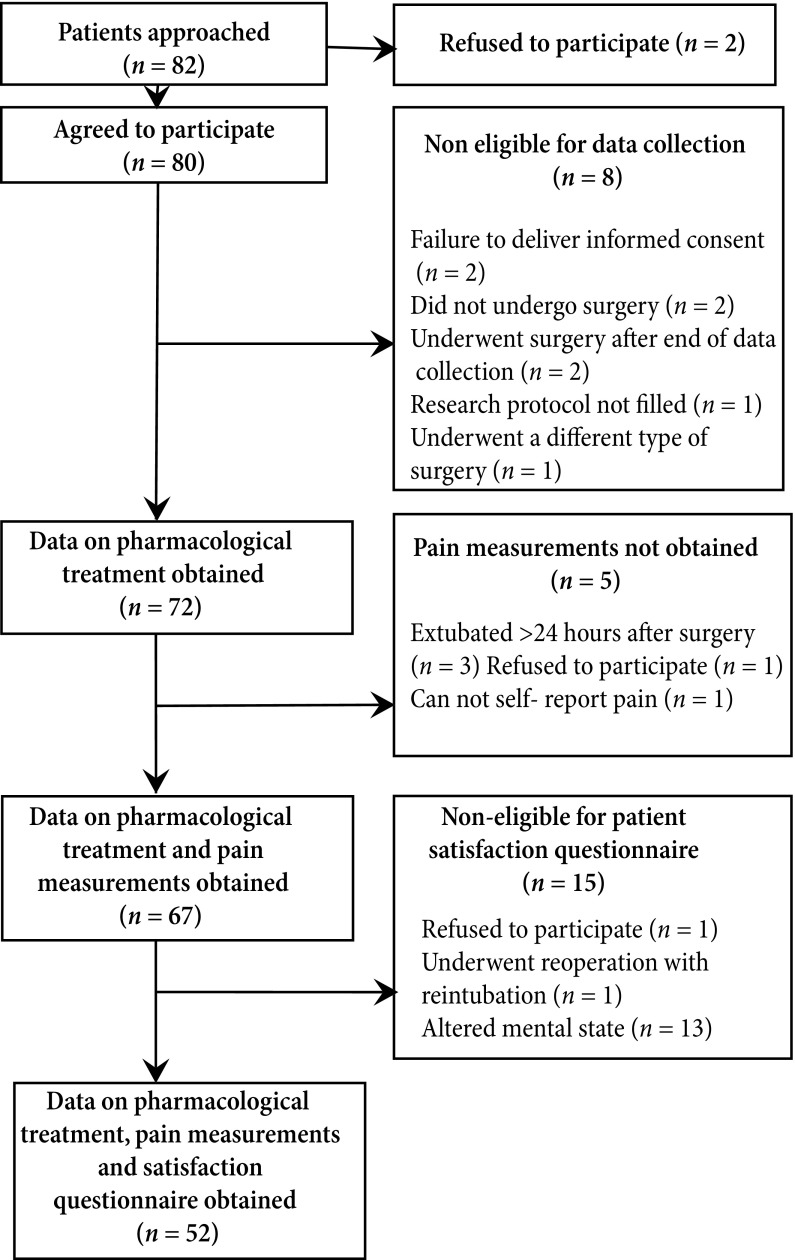
From the patient pool, 2 of the 82 patients initially approached refused to participate. Of the 80 participants 66.7% (n = 48) were males and 33.3% (n = 24) were females. Due to several exclusion criteria, the data about pharmacological treatment was gathered from 72 patients, the data about pharmacological treatment and pain measurements were gathered from 67 patients, and patient satisfaction questionnaire was completed by 52 patients (see Fig. 1).
Measures
Toronto Pain Management Inventory
The Toronto Pain Management Inventory was used to assess the expertise and competence of intensive care nurses (21). The Toronto Pain Management Inventory is composed of a demographical part and 23 questions on a visual analogue scale (VAS), rated from 0 to 100. The questions examine the expertise of nurses in pain management, including analgesia, patient experience, and response to pain and professional issues. Items also examine evidence-based knowledge and common beliefs not based on scientific evidence. Individual VAS scores are summed for a total score of 0 to 2300, which is then converted to a percentage. The possible values range from 0 (least knowledge) to 2300 or 100% (most knowledge) (21). The instrument was translated into Latvian and adapted for use in this study. Permission for use was obtained from the author.
2010 Revised American Pain Society Patient Outcome Questionnaire
The 2010 Revised American Pain Society Patient Outcome Questionnaire (26) was used to assess patient satisfaction with pain management in the first 24 hours after surgery. It is composed of 12 questions, and of these, four questions contain four subquestions each. It measures the following aspects of patient satisfaction with pain management: (1) pain severity and relief; (2) impact of pain on activity, sleep, and negative emotions; (3) side effects of treatment; (4) usefulness of information on pain treatment; (5) ability to participate in pain treatment decisions, and (6) the use of non-pharmacological strategies. Answers are given on a visual analogue scale. In this study, the questions were analysed individually. The instrument was translated into Latvian and adapted for use in this study.
Research protocol
A research protocol was developed and used to gather data about pharmacological treatment, patient pain level after surgery, and usage of patient positioning for pain relief. The research protocol covered 24 hours after surgery and nurse participants were asked to register every analgesic medication that the patients received. Nurse participants were also asked to assess patient pain level 2 hours, 4 hours, 6 hours, and 12 hours after extubation. Instances of patient positioning with the aim of pain relief were also registered in the research protocol.
Fig. 1.
Patient participation flow chart
Procedure
Ethical approval was received from the Ethics Committee of Riga Stradiņš University and Pauls Stradiņš Clinical University Hospital in January 2017. Written informed consent was obtained from patient participants and verbal consent was obtained from nurse participants. The research protocol was filled out from the moment of a patient’s arrival in the ICU after surgery to 12 hours after extubation. The patient questionnaire was completed 24 hours after extubation and surgery or before the patient’s transfer to a surgical care unit. Before the questionnaire was filled out, patients were assessed with the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) to assess delirium and altered mental state (27). If CAM-ICU was positive (delirium present), patients were excluded from the questionnaire. Nurse assessment was carried out independently, before the collection of the patient data was started. During the study, nurse-patient pairs were registered. Nurse-conducted measurements were not independent of each patient, because usually the same nurse was assigned to more than one patient during the study. All data was collected by the principal researcher from 5 February to 16 April 2018.
Statistical analysis
Descriptive statistics were tabulated and analysed. Spearman correlation coefficient was used to assess associations between patient satisfaction measurements and contributing factors. Pearson correlation coefficient was used to assess associations between the pain levels registered in the research protocol and patient self-assessment of their lowest and highest pain levels. T-tests were also used to assess associations between different factors.
Results
Nurses’ knowledge on pain
The Toronto Pain Management Inventory (21) was used to assess the nurses’ knowledge regarding pain management. Nineteen nurse participants returned the questionnaire and 15 questionnaires were eligible for data analysis. The nurse sample was very diverse with regard to the age and work experience. Nurses’ age ranged from 23 years to 59 years (X = 36 ± 13.3), general work experience ranged from 1.5 years to 40 years (X = 15 ± 13.37), and work experience in the ICU – from 0.5 years to 37 years (X = 10 ± 10.6). Nine nurses had a bachelor’s degree in nursing, but only six nurses had received education about pain management.
The Toronto Pain Management Inventory scores could be calculated for 15 nurses. The results ranged from 50% to 78% (N = 60.6 ± 7.3%), which can be described as average knowledge. Due to the small sample size and several inadequately filled questionnaires, the results could not be analysed question by question. During the study, each of the participating nurses cared for one to 13 patients.
Pharmacological treatment
The data on pharmacological treatment could be gathered from 72 patients. During analysis, the data was split into two groups – medication used before extubation and medication used after extubation (Table 1).
Table 1.
Types of medication and frequency of administration before extubation
| Type | Dosage and administration | Amount administered | n | % | |
|---|---|---|---|---|---|
| Opiods | Fentanyl | 0.5 mg/50 ml, continuous intravenous infusion | 0.13–0.14 µg/kg/h | 2 | 2.8 |
| 0.2–0.33 µg/kg/h | 58 | 80.6 | |||
| 0.25 µg/kg/h | 1 | 1.4 | |||
| 0.3–0.5 µg/kg/h | 11 | 15.3 | |||
| NSAIDs | Paracetamol (acetaminophen) | 1000 mg/100 ml, intravenous infusion | 1000 mg | 54 | 75.0 |
| 2000 mg | 1 | 1.4 | |||
| 500 mg | 1 | 1.4 | |||
| Ketorolac tromethamine | 30 mg, intravenous injection | 30 mg | 7 | 9.7 |
Fentanyl was used in 100% of the cases and paracetamol (acetaminophen) was used in 77.8% of the patients. The medications were administered solely via the intravenous route. The post-extubation range of medications used increased as different routes of administration became possible.
Post-extubation fentanyl infusion was ceased in four cases, most likely due to opioid side effects, and replaced with a lidocaine infusion. Metamizole was used in four cases when pain did not subside after the use of ketorolac tromethamine. Similarly, a combination of metamizole and carbamazepine was also used in cases when ketorolac tromethamine did not alleviate the pain.
Table 2.
Types of medication and frequency of post-extubation administration
| Type | Dosage and administration | Amount administered | n | % | |
|---|---|---|---|---|---|
| Opioids | Fentanyl | 0.5 mg/50 ml, continuous intravenous infusion | 0.08 μg/kg/h | 1 | 1.4 |
| 0.1–0.17 μg/kg/h | 7 | 9.7 | |||
| 0.2–0.34 μg/kg/h | 52 | 72.2 | |||
| 0.3–0.37 μg/kg/h | 9 | 12.5 | |||
| 0.1 mg, fractioned intravenous injection | 0.1 mg | 1 | 2.8 | ||
| Promedol | 20 mg, intravenous injection | 20 mg | 1 | 1.4 | |
| NSAIDs | Paracetamol (acetaminophen) | 1000 mg/100 ml, intravenous infusion | 1000 mg | 20 | 27.8 |
| 500 mg | 2 | 2.8 | |||
| Ketorolac tromethamine | 30 mg, intravenous or intramuscular injection | 30 mg | 27 | 37.5 | |
| 60 mg | 5 | 6.9 | |||
| Lornoxicam | 8 mg, intravenous injection | 8 mg | 2 | 2.8 | |
| Others | Lidocaine | 400 mg/40 ml, continuous intravenous infusion | 1.0–1.16 mg/kg/h | 4 | 5.6 |
| Gabapentin | 300 mg, orally | 300 mg | 2 | 2.8 | |
| Pregabalin | 75 mg, orally | 75 mg | 3 | 4.2 | |
| “Skudexa” | 75 mg tramadol/25 mg dexketoprofen, orally | 75 mg/25 mg | 2 | 2.8 | |
| Metamizole | 500 mg/ml, intravenous injection | 2000 mg | 4 | 5.6 | |
| Metamizole with carbamazepine | Metamizole i/v, carbamazepine orally | 2000 mg (metamizole), 200 mg (carbamazepine) | 2 | 2.8 | |
| Carbamazepine | 200 mg, orally | 200 mg | 2 | 2.8 | |
| Carbmazepine with amitriptyline | Carbamazepine 200 mg, amitriptyline 10 mg | 200 mg (carbamazepine), 10 mg (amitriptyline) | 1 | 1.4 |
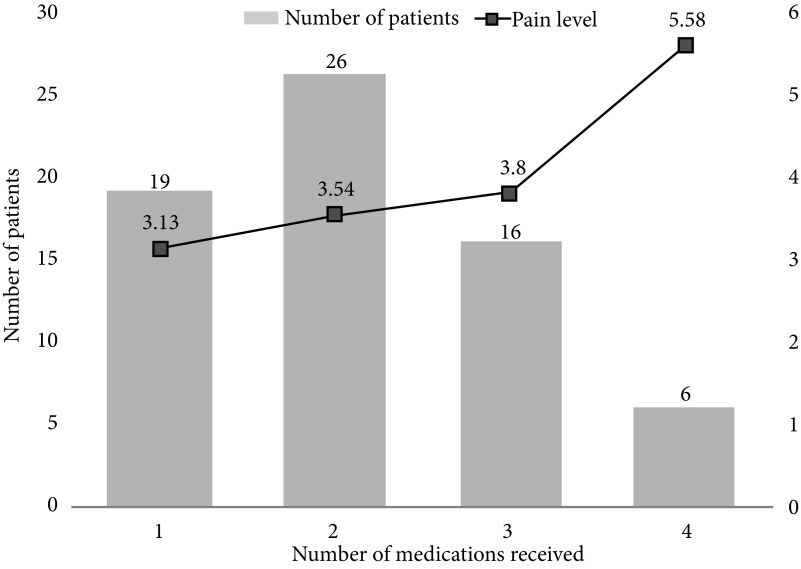
Both pre- and post-extubation, a continuous intravenous infusion of either fentanyl or lidocaine was administered for baseline pain treatment in all patients. The administration of other medications, specifically in bolus injections, was used for breakthrough pain treatment (see Fig. 2).
Patient pain levels
Patient pain level measurements were obtained from 67 patients. As two patients underwent reoperation with reintubation, only one measurement of four could be obtained. For the remaining 65 patients, the pain level was obtained at 2, 4, 6, and 12 hours after extubation. In 27.7% of cases (n = 18), pain level was measured more than four times due to the nurses’ initiative.
Pain levels can be described as mostly mild and tend to lower over time, with a mean VAS score of 4.33 two hours post-extubation to a mean VAS score of 3.12 twelve hours post-extubation. However, 2 hours post-extubation most of the patients had moderate pain (46.3%, n = 29, scale range 5–7), but 4 hours, 6 hours, and 12 hours after extubation most patients had mild pain (scale range 1–4). The incidence of severe pain also lowered over time, from seven cases (10.5%) 2 hours post-extubation to two cases (3.1%) 12 hours post-extubation. Over time, the number of patients not feeling any pain also increased, the maximum being eight cases (12.3%) at 12 hours post-extubation (see Table 3).
Table 3.
Mean VAS (visual analogue scale) scores and distribution
| Time of measurement | n | Mean (SD) | No pain VAS = 0 n (%) | Mild pain VAS = 1–4 n (%) | Moderate pain VAS = 5–7 n (%) | Severe pain VAS = 8–10 n (%) |
|---|---|---|---|---|---|---|
| 2 hours post–extubation | 67 | 4.33 ± 2.39 | 5 (7.5) | 26 (38.8) | 29 (46.3) | 7 (10.5) |
| 4 hours post–extubation | 65 | 3.66 ± 2.26 | 5 (7.7) | 38 (58.5) | 17 (26.1) | 5 (7.7) |
| 6 hours post–extubation | 65 | 3.45 ± 2.05 | 3 (4.6) | 47 (72.3) | 13 (20.0) | 2 (3.1) |
| 12 hours post–extubation | 65 | 3.12 ± 2.18 | 8 (12.3) | 41 (63.1) | 14 (21.5) | 2 (3.1) |
Fig. 2.
Number of medications received based on pain level (mean VAS)
Individual pain levels were calculated and tabulated including all available pain level measurements. Individual mean VAS scores ranged from no pain (2.98%, n = 2) and mild pain (68.66%, n = 46), to moderate pain (28.36%, n = 19) and severe pain (1.49%, n = 1). However, it should be noted that the patient experiencing severe pain had several drug intolerances and sensitivities, therefore only fentanyl could be used for pharmacological treatment (Table 4).
Table 4.
Individual mean VAS (visual analogue scale) scores and distribution
| Pain level | n (%) | Mean (SD) | Min | Max |
|---|---|---|---|---|
| No pain VAS = 0–0.4 | 2 (2.98) | 0 | 0 | 0 |
| Mild pain VAS = 0.5–4.5 | 46 (68.66) | 2.87 ± 1.07 | 0.75 | 4.25 |
| Moderate pain VAS = 4.5–7.4 | 19 (28.36) | 5.72 ± 0.96 | 4.6 | 7.4 |
| Severe pain VAS = 7.5–10 | 1 (1.49) | 8 | 8 | 8 |
For several patients (n = 52) who also completed the 2010 American Pain Society Patient Outcome Questionnaire, the pain levels registered in the research protocol could be compared to the self-reported lowest and highest pain levels. For the lowest pain level, a mean VAS score of 2.31 was recorded in the research protocol (scale range 0–7) and the self-reported mean VAS score was 1.99 (scale range 0–9). For the highest pain level, the results were a mean VAS score of 4.94 in the research protocol (scale range 0–10) and a self-reported mean VAS score of 5.77 (scale range 0–10). Differences in the measurements can be explained by a reduced sample size and the last pain level registered in the research protocol being at 12 hours post-extubation and self-reported pain levels registered after a longer period. However, there is a moderate positive correlation between the lowest registered and the lowest self-reported pain level (r = 0.548, p < 0.0005), and between the highest registered and the highest self-reported pain level (r = 0.424, p = 0.002).
Effects of patient positioning on pain
Instances of patient positioning as a method of pain relief were also registered in the research protocol. Patient positioning was done in 31.3% of cases (n = 21). In two cases, the effect could not be evaluated due to lacking pain measurements. The positioning process has been described as painful in several studies (28), however, a change of position can act as pain relief. In 13 cases of this study pain levels decreased after positioning and did not change in six cases. Positioning was found to decrease the pain level from score 1 to score 5. In most cases (n = 8), the pain level decreased by 1 on VAS.
Patient satisfaction measurements
Patient satisfaction measurements could be obtained from 52 patients. The 2010 American Pain Society Patient Outcome Questionnaire was completed 24 hours after extubation or before the transfer of a patient to a surgical care unit. The questions on the use of non-pharmacological techniques were not analysed because they were not used during this study. The question on activities outside the bed was not analysed either because all patients participating in the study were under bed-rest orders. The remaining questions were analysed and tabulated (see Appendix 1).
Appendix.
Results of 2010 Revised American Pain Society Patient Outcome Questionnaire
| Measurement | Min | Max | Mean | SD |
|---|---|---|---|---|
| Least pain in 24 hours | 0 | 9 | 1.98 | 1.92 |
| Worst pain in 24 hours | 1 | 10 | 5.77 | 2.31 |
| Estimate of percentage of time in severe pain, % | 0 | 100 | 8.35 | 2.92 |
| Pain relief in the first 24 hours, % | 10 | 100 | 76.92 | 26.68 |
| Pain interfered/prevented activities in bed | 0 | 10 | 4.69 | 3.37 |
| Pain interfered/prevented falling asleep | 0 | 10 | 1.69 | 2.69 |
| Pain interfered/prevented sleeping | 0 | 10 | 2.02 | 2.86 |
| How much the pain caused you to feel anxious | 0 | 9 | 1.21 | 2.29 |
| How much the pain caused you to feel depressed | 0 | 10 | 1.10 | 2.28 |
| How much the pain caused you to feel frightened | 0 | 10 | 1.49 | 2.68 |
| How much the pain caused you to feel helpless | 0 | 10 | 2.48 | 3.79 |
| Severity of nausea | 0 | 10 | 1.65 | 3.22 |
| Severity of drowsiness | 0 | 10 | 4.23 | 2.93 |
| Severity of itching | 0 | 4 | 0.17 | 0.73 |
| Severity of dizziness | 0 | 10 | 0.60 | 1.78 |
| Were you allowed to participate in decisions about pain treatment? | 0 | 10 | 8.35 | 2.92 |
| How helpful was the information about pain treatment, if received? * | 1 | 10 | 9.02 | 2.08 |
* 43 out of 52 patients received information about pain treatment
The least pain or the lowest pain level experienced was mild at 1.98 mean VAS score, but the worst pain or the highest pain level experienced was moderate at 5.77 mean VAS score. As for the percentage of time in severe pain, 40.4% of the patients (n = 21) did not experience severe pain at all during the first 24 hours. The pain relief was also high in the sample, with no patients experiencing zero pain relief and the majority of the patients (61.5%, n = 32) experiencing pain relief in the 80–100% range. Only 7.7% of (n = 4) the patients received mild pain relief in the 10–20% range.
Pain mostly interfered with activities in bed and for 9.6% of the patients (n = 5) pain prevented them from doing any activity. However, in 17.3% of cases (n = 9), the patients experienced no interference of pain in doing activities in bed. Pain did not interfere with falling asleep for 61.5% of the patients (n = 32) and sleeping was undisturbed for 57.7% of the patients (n = 30). For one patient, pain had completely prevented them from falling asleep and sleeping.
As for pain negatively affecting the mood and emotions, patients on average experienced it minimally: 67.3% of the patients (n = 35) did not feel anxious, 65.4% of the patients (n = 34) did not feel depressed, and 61.5% of patients (n = 32) did not feel frightened. The most negatively experienced emotion in the sample was helplessness, with 13.5% of patients (n = 7) feeling completely helpless.
The prevalence of medication side effects was also minimal. The least common side effects were itching and nausea, which were experienced by only 5.8% of the patients (n = 3). The most commonly experienced side effect was drowsiness experienced by 69.2% of the patients (n = 36). The majority of the patients also received information about their pain management (n = 43) and noted that the information was useful and that they could participate in decision making.
On average, patient satisfaction was high throughout the sample (Table 5).
Table 5.
Measurements of patient satisfaction
| Measurement | n | Mean | % | SD |
|---|---|---|---|---|
| Dissatisfied VAS = 1–4 | 1 | 4 | 1.9 | – |
| Satisfied VAS = 5–7 | 2 | 5.5 | 2.8 | 0.71 |
| Very satisfied VAS = 8–10 | 49 | 9.24 | 94.2 | 0.80 |
| Total | 52 | 9 | 100 | 1.28 |
In the sample, only one patient was dissatisfied and rated their satisfaction with a score of 4 (scale range 0–10). Most of the patients (94.2%, n = 49), were very satisfied with a 9.24 mean VAS score. Fewer than half, or 44.2% of the patients (n = 23) rated their satisfaction with a score of 10 (extremely satisfied). Due to high overall satisfaction in the sample, the hypothesis of the study can be neither affirmed or denied. There is a moderate positive correlation between patient satisfaction and pain relief (rs = 0.466, p = 0.001) and a moderate negative correlation between patient satisfaction and emotion subscale measurements and the percentage of time in severe pain (rs = –0.509, p > 0.0005).
DISCUSSION
The data acquired in the study show that pain management after cardiac surgery is guideline-based and efficient. Recommendations for thoracotomy, also thoracotomy with sternotomy approach, include opioids, NSAIDs, or, specifically, paracetamol (acetaminophen) as well as gabapentin, pregabalin, and intravenous ketamine (20). Before extubation, only the intravenous route of administration is used, and mostly a combination of an opioid (fentanyl) and a NSAID (paracetamol) is administered. Both baseline and breakthrough pain are treated: baseline pain with a continuous infusion and breakthrough pain with different types of medications and routes of administration (29).
Post-extubation, the use of pharmacological treatments increases, including the guideline recommended gabapentin and pregabalin. An increased use of medications also shows that patient needs regarding pain management are considered (20). A rare use of other opioid medications might be a sign of a relatively low general pain level.
Pain management should have an individualized approach according to the pain level (15). Based on this study, an individualized approach is also used in the cardiac surgery ICU in Riga, Latvia. Patients with a higher pain level also receive more pain medication, although in other studies it has been noted that patients do not receive more medication even if their pain level is high (21). A general low level of pain and the rare incidence of medication side effects are a sign of pain management being adequate and safe, according to patient safety practices (8).
Even if patients in the sample have experienced pain more often (97.02% of cases) than in other studies, 80–82% accordingly, the pain level is relatively low and decreases over time (6, 8). Previous data from the cardiac surgery ICU in Riga, Latvia was from 4.94 mean VAS score 2 hours post-extubation to 3.98 mean VAS score 24 hours post-extubation (7). The pain level is slightly lower in this study with a 4.33 mean VAS score 2 hours post-extubation and 3.12 mean VAS score 12 hours post-extubation. The pain level, as well as the incidence of severe pain, tends to lower over time on average.
A sign of effective pain management is also the high pain relief (76.9%) and low incidence of severe pain (8.35%). Overall, the pain level on VAS score was lower by 2 points in comparison to other studies (5), although that may be due to the small sample size. Severe pain was experienced by 1.49% of patients and moderate pain was experienced by 28.36% of patients, though in other studies severe pain has been noted in 3.3–39% of cases and moderate pain in 24.1–47% of cases (6, 24).
A number of studies note the positive effect of standardized pain assessment and documentation on pain management (8, 11–13). At the start of this study, no pain documentation was available or used in the cardiac surgery ICU and hospital. However, after the end of the study, a pain documentation form was successfully introduced and is now being used routinely. The intensity of patient care can be described as high, as shown by the administration of medications according to patient pain level and the usage of positioning as a form of pain relief.
Pain can intensify sleep disorders and negative emotions, which can also influence patient satisfaction (9–10), as can also be seen in this study. Patients experienced pain preventing them from doing activities in bed (4.69 VAS) and sleeping (2.02 VAS). The patient emotional state, which has been affected negatively, can be explained not only by pain, but also by the stay in the ICU in general. Studies have found that pain is a traumatic memory for 38% of intensive care patients (10). The most commonly experienced negative emotion in this sample was helplessness, but it also was of low intensity (2.48 VAS) The patient emotional state should be taken into account and extra care should be taken while carrying out early patient rehabilitation with activities in and out of bed in an ICU. Pre-emptive pain relief administration before procedures is recommended with both pharmacological and non-pharmacological techniques (15).
Other studies have found that a lack of time is a factor contributing to suboptimal pain management. The nurses noted that they did not have time to listen to patient concerns and their descriptions of pain, to give information, and to include them in decision making regarding pain management (8). However, in this study, most patients received information about their pain management (82.7%) and found it to be useful (9.02 VAS). The patients were also included in decision making (8.35 VAS), which shows that the nurses actively participated in patient care and spent enough time on communication.
Even though the nurses’ knowledge regarding pain management was average (60.6%), as is also shown in other studies (21), patient satisfaction was high. While analysing nurse-patient pairs, it was found that patients were satisfied with each nurse, with no correlation with the nurses’ work experience, knowledge, or other factors. Other studies have also found that 93% of patients were satisfied with nurses’ role in pain management and care (25).
Patient satisfaction measures in other studies differed from 50% in 2013 to 70.4% in 2003 (23–24). However, in this study it was significantly higher at 98.1%. It can be explained by a small sample size and different cultural aspects. Nonetheless, it has been proven that patients could be satisfied with their pain management, even if they experienced high pain levels (22).
The pain management approach includes analgesic medications, pain assessment and documentation, non-pharmacological techniques, and communication with the patient (14). Although such factors as pain relief, incidence of severe pain and the impact of pain on emotions can affect patient satisfaction, it was very high in this study (9 VAS). It shows that pain management was individualized to each patient depending on their needs and the pain level, with the use of both pharmacological and non-pharmacological techniques. A low pain level and high satisfaction indicate that pain management was qualitative, effective, and safe.
The limitations of this study were a small sample size and the data being collected by a single researcher. Further research is needed to draw specific conclusions and attribute them to entire populations and not just to the sample in this study.
CONCLUSIONS
Postoperative pain after cardiac surgery was mostly mild and pain management was guideline-based with the administration of fentanyl and paracetamol (acetaminophen). Patient satisfaction with pain management in the first 24 hours after surgery was high, even though the nurses’ knowledge was average, which directs attention to the communication and the attitude as factors affecting patient satisfaction. Pain documentation and routine pain assessment is needed and patient pain levels and needs must be taken into account to ensure an individualized pain management plan, which is the cornerstone in successful pain relief and high patient satisfaction.
Baiba Vilīte, Eva Strīķe, Katrīna Rutka, Roberts Leibuss
References
- Sherwood G, Adams-McNeill J, Starck PL, Nieto B, Thompson CJ. Qualitative assessment of hospitalized patients’ satisfaction with pain management. Res Nurs Health. 2000. December; 23(6): 486–95. [DOI] [PubMed] [Google Scholar]
- Gélinas C, Fillion L, Puntillo KA, Viens C, Fortier M. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care. 2006. July; 15(4): 420–7. [PubMed] [Google Scholar]
- Bjørnnes AK, Rustøen T, Lie I, Watt-Watson J, Leegaard M. Pain characteristics and analgesic intake before and following cardiac surgery. Eur J Cardiovasc Nurs. 2016. February; 15(1): 47–54. Epub 2014 Sep 5. [DOI] [PubMed] [Google Scholar]
- Leegaard M, Fagermoen MS. Women’s descriptions of postoperative pain and pain management after discharge from cardiac surgery. J Clin Nurs. 2008. August; 17(15): 2051–60. [DOI] [PubMed] [Google Scholar]
- Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013. April; 118(4): 934–44. [DOI] [PubMed] [Google Scholar]
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003. August; 97(2): 534–40. [DOI] [PubMed] [Google Scholar]
- Bērziņš A, Arkliņa B, Strīķe E. Acute post-operative pain impact on outcome of patients after heart surgery. Proceedings of RSU Scientific Conference 2017, April 6–7; Riga, Latvia: p. 111–2. [Google Scholar]
- Yin HH, Tse MM, Wong FK. Systematic review of the predisposing, enabling, and reinforcing factors which influence nursing administration of opioids in the postoperative period. Jpn J Nurs Sci. 2015 October; 12(4): 259–75. Epub 2015. March 17. [DOI] [PubMed] [Google Scholar]
- Choi J, Hoffman LA, Schulz R, Tate JA, Donahoe MP, Ren D, Given BA, Sherwood PR. Self-reported physical symptoms in intensive care unit (ICU) survivors: pilot exploration over four months post-ICU discharge. J Pain Symptom Manage. 2014. February; 47(2): 257–70. Epub 2013. July 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schelling G, Richter M, Roozendaal B, Rothenhäusler HB, Krauseneck T, Stoll C, Nollert G, Schmidt M, Kapfhammer HP. Exposure to high stress in the intensive care unit may have negative effects on health-related quality-of-life outcomes after cardiac surgery. Crit Care Med. 2003. July; 31(7): 1971–80. [DOI] [PubMed] [Google Scholar]
- Gélinas C, Arbour C, Michaud C, Vaillant F, Desjardins S. Implementation of the critical-care pain observation tool on pain assessment/management nursing practices in an intensive care unit with nonverbal critically ill adults: a before and after study. Int J Nurs Stud. 2011. December; 48(12): 1495–504. Epub 2011. May 6. [DOI] [PubMed] [Google Scholar]
- Topolovec-Vranic J, Canzian S, Innis J, Pollmann-Mudryj MA, McFarlan AW, Baker AJ. Patient satisfaction and documentation of pain assessments and management after implementing the adult nonverbal pain scale. Am J Crit Care. 2010. July; 19(4): 345–54. [DOI] [PubMed] [Google Scholar]
- van Gulik L, Ahlers SJ, Brkić Z, Belitser SV, van Boven WJ, van Dongen EP, Knibbe CA, Bruins P. Improved analgesia after the realisation of a pain management programme in ICU patients after cardiac surgery. Eur J Anaesthesiol. 2010. October; 27(10): 900–5. [DOI] [PubMed] [Google Scholar]
- Bantel C, Laycock H, Ward S, Halmshaw C, Nagy I. Pain in intensive care: a personalised healthcare approach. J Intensive Care. 2013; 14(4): 312–8. [Google Scholar]
- Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R. American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013. January; 41(1): 263–306. [DOI] [PubMed] [Google Scholar]
- Chanques G, Jaber S, Barbotte E, Violet S, Sebbane M, Perrigault PF, Mann C, Lefrant JY, Eledjam JJ. Impact of systematic evaluation of pain and agitation in an intensive care unit. Crit Care Med. 2006. June; 34(6): 1691–9. [DOI] [PubMed] [Google Scholar]
- Gélinas C, Fortier M, Viens C, Fillion L, Puntillo K. Pain assessment and management in critically ill intubated patients: a retrospective study. Am J Crit Care. 2004. March; 13(2): 126–35. [PubMed] [Google Scholar]
- Rose L, Smith O, Gélinas C, Haslam L, Dale C, Luk E, Burry L, McGillion M, Mehta S, Watt-Watson J. Critical care nurses’ pain assessment and management practices: A survey in Canada. Am J Crit Care. 2012. July; 21(4): 251–9. [DOI] [PubMed] [Google Scholar]
- Abdalrahim MS, Majali SA, Stomberg MW, Bergbom I. The effect of postoperative pain management program on improving nurses’ knowledge and attitudes toward pain. Nurse Educ Pract. 2011. July; 11(4): 250–5. Epub 2010. December 24. [DOI] [PubMed] [Google Scholar]
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, Griffith S, Manworren R, McCarberg B, Montgomery R, Murphy J, Perkal MF, Suresh S, Sluka K, Strassels S, Thirlby R, Viscusi E, Walco GA, Warner L, Weisman SJ, Wu CL. Management of Postoperative Pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016. February; 17(2): 131–57. [DOI] [PubMed] [Google Scholar]
- Watt-Watson J, Stevens B, Garfinkel P, Streiner D, Gallop R. Relationship between nurses’ pain knowledge and pain management outcomes for their postoperative cardiac patients. J Adv Nurs. 2001. November; 36(4): 535–45. [DOI] [PubMed] [Google Scholar]
- Farooq F, Khan R, Ahmed A. Assessment of patient satisfaction with acute pain management service: Monitoring quality of care in clinical setting. Indian J Anaesth. 2016. April; 60(4): 248–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips S, Gift M, Gelot S, Duong M, Tapp H. Assessing the relationship between the level of pain control and patient satisfaction. J Pain Res. 2013. September 9; 6: 683–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung JW, Lui JC. Postoperative pain management: study of patients’ level of pain and satisfaction with health care providers’ responsiveness to their reports of pain. Nurs Health Sci. 2003. March; 5(1): 13–21. [DOI] [PubMed] [Google Scholar]
- Dawson R, Spross JA, Jablonski ES, Hoyer DR, Sellers DE, Solomon MZ. Probing the paradox of patients’ satisfaction with inadequate pain management. J Pain Symptom Manage. 2002. March; 23(3): 211–20. [DOI] [PubMed] [Google Scholar]
- Gordon DB, Polomano RC, Pellino TA, Turk DC, McCracken LM, Sherwood G, Paice JA, Wallace MS, Strassels SA, Farrar JT. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010. November; 11(11): 1172–86. Epub 2010. April 18. [DOI] [PubMed] [Google Scholar]
- Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001. July; 29(7): 1370–9. [DOI] [PubMed] [Google Scholar]
- Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, Wild LR. Patients’ perceptions and responses to procedural pain: results from Thunder Project II. Am J Crit Care. 2001. July; 10(4): 238–51. [PubMed] [Google Scholar]
- Svendsen KB, Andersen S, Arnason S, Arnér S, Breivik H, Heiskanen T, Kalso E, Kongsgaard UE, Sjogren P, Strang P, Bach FW, Jensen TS. Breakthrough pain in malignant and nonmalignant diseases: a review of prevalence, characteristics and mechanisms. Eur J Pain. 2005. April; 9(2): 195–206. [DOI] [PubMed] [Google Scholar]