Abstract
College students with attention-deficit/hyperactivity disorder (ADHD) are at greater risk than peers for im-paired educational functioning; however, little is known regarding their longitudinal academic outcomes. This study examined: (a) differences between ADHD and control participants in academic outcomes (i.e., semester GPA, credits attempted, credits earned) over the first two years of college, and (b) factors that predict second year outcomes. A sample of 456 students (50% with ADHD; 51.8% female; 71.7% Caucasian) from 10 universities completed two annual assessments. Compared to students without ADHD, students with ADHD experience more academic difficulties that persist over two years. Motivation to study reported in year one was a significant predictor of year two GPA, suggesting the importance of providing services as early as possible to support students before they struggle.
Keywords: Attention-deficit/hyperactivity disorder, educational functioning, longitudinal analysis
Attention-deficit/hyperactivity disorder (ADHD) is characterized by developmentally deviant levels of symptoms of hyperactivity/impulsivity and/or inattention among children, adolescents and adults (DSM-5; American Psychiátric Association, 2013). Although symptoms must manifest prior to the age of 12 to meet diagnostic criteria, they typically persist into adulthood along with functional impairments across multiple domains (e.g., work, home, social, school) (Barkley, 2015; Barkley, Murphy, & Fischer, 2008; Biederman, Petty, Clarke, Lomedico & Faraone, 2011;Bramham et al., 2012; Brown, 2000; Fischer, Barkley, Smallish, & Fletcher, 2005). ADHD symptoms have been found to persist into adulthood; however, cross-sectional investigations of ADHD symptoms at different ages have demonstrated developmental differences in symptom levels and associated impairment (Barkley, 2015; Zoromski, Owens, Evans, & Brady, 2015). For example, Zoromski and colleagues (2015) reported that symptoms of hyperactivity and impulsivity decrease during childhood and into adulthood, while symptoms of inattention increase over the same time period. Further, Weyandt et al. (2003) found that college students with ADI-ID report increased levels of internal, restlessness and decreased motor activity relative to peers without ADHD. FinalIy, associations between symptoms and specific domains of impairment change between early childhood, middle childhood, and adolescence. Such changes are not surprising given increased demands on executive functioning as children and adolescents move through development (Best, Miller, & Naglieri, 2011).
As adolescents with ADHD transition into young adulthood, impairment in key areas such as educational functioning may be particularly notable for emerging adults with ADI-ID who enroll in post-secondary educational institutions. Approximately 5% of first-year college students self-report a diagnosis of ADHD (Pryor, Hurtado, DeAngelo, Palucki Blake, & Tran, 2010) and among the population of college students with disabilities, approximately 25% are diagnosed with ADHD (DuPaul, Weyandt, O’Dell, & Varejao, 2009). Unfortunately, even when emerging adults with ADHD attend college, only a small proportion (5%) reach graduation (Hechtman, 2017; Hechtman et al., 2016). Despite the increasing numbers of students with ADHD who attend college, little is known about this group regarding academic experiences and predictors for academic success in college (Weyandt et al., 2013; Wolf, Simkowitz, & Carlson, 2009). Yet, because only a minority (21%) of individuals with ADHD pursue higher education (Barkley, Fischer, Smallish, & Fletcher, 2006), those who do are likely to display unique traits that differentiate them from the rest of the ADHD population, so additional information on this particular group is needed.
Research has demonstrated that when this subgroup of emerging adults with ADHD) attends college, they are at risk for poorer academic performance (DuPaul et al., 2009; Heiligenstein, Guenther, Levy, Savino, & Fulwiler, 1999; Weyandt & DuPau1, 2006), experience more overall academic problems, and obtain lower GPAs than their peers without ADHD (Gormley, DuPaul, Weyandt, & Anastopoulos, 2016; Heiligenstein et al., 1999). One reason for this deficit may be related to the increased demands during college on executive functioning (i.e., processes such as organization and self-regulation that are necessary for cognitive control of behavior). These increased demands can potentially place a greater academic strain on these students than they had been accustomed to in their previous schooling (Brown, 2000; Weyandt et al., 2013). The novel challenges and stressors that are prevalent in the college environment may even initiate higher levels of ADHD symptom presentation and impairment and create a unique and potentially challenging environment for individuals with ADHD that warrants investigation (Fleming & McMahon, 2012).
Several factors limit conclusions based on currently available research regarding ADHD in college. First, cross-sectional, rather than longitudinal studies, currently make up the majority of the literature on academic outcomes of college ADHD populations. Although studies have shown that academic impairment in children with ADHD persists throughout childhood (Frazier, Youngstrom, Glutting, & Watkins, 2007; Loe & Feldman, 2007), few longitudinal investigations have been specifically conducted to examine academic outcomes over time for college students with ADHD. Second, there has been a paucity of research comparing this group’s academic outcomes with a non-ADHD control group to track significant differences in academic impairment. Third, of the studies that measure academic outcomes in college students with ADHI), few employ measures other than GPA. Although GPA is a major indicator of educational achievement, additional variables (e.g., credits attempted and earned, continued enrollment, study skills, symptom dimensions) that may innuence academic success warrant investigation in this population to enable analyses of trajectories over time. Without examining these extended dimensions, predictors and outcomes of academic success may be overlooked. For example, given that one of the most ubiquitous research findings for children with ADHD is that symptoms of in-attention predict academic impairment (Langberg, Dvorsky, & Evans, 2013), neglecting to include symptom dimensions (i.e., inattention and hyperactivity-impulsivity) as predictors of impairment may prevent identification of important factors related to academic success. Similarly, failure to consider comorbid conditions (e.g., depression) may hinder accurate conclusions given the documented impact of depression on GPA (Hysenbegasi, Hass & Rowland, 2005) and the increased rate of psychopathology among college students with ADHD (Anastopoulos et al., 2016). Including these additional indicators of academic functioning may also help to better explain differences in performance over time and provide a more comprehensive understanding of factors that influence the success of individuals with ADHD in the college environment.
Understanding the elements that influence academic outcomes over time for college students with ADI--ID may help provide a framework for creating and targeting interventions to bolster the success of these individuals. Increasing rates of students with ADHD are attending college (Pryor et al., 2010; Wolf et al., 2009) which necessitates research to broaden the understanding of academic outcomes over time. To address the gaps in the literature, this study examined: (a) whether differences between ADHD and control participants exist or appear over time with regard to academic outcomes (i.e., semester GPA, number of credits attempted, number of credits earned, and enrollment status) over the first two years of college, and (b) identification of factors that predict semester GPA and credits attempted and earned in the second year of college, after controlling for demographic characteristics (i.e., gender, IQ), comorbidity, medication status, and registration with disability resource center status. It was hypothesized that college students without ADHD would exhibit greater academic success (i.e., higher GPA, more credits attempted and earned) than those in the ADHD group. Additionally, it was hypothesized that year one outcomes (including symptom dimensions, as well as motivation and engagement with studying) would predict academic performance in year two (while controlling for the variance accounted for by demographic characteristics, comorbidity, medication status, and registration with disability resource center status).
Methods
Participant Description
Participants for this study were recruited as part of a larger, longitudinal study examining the long-term outcomes of college students with ADHD across three primary sites in the eastern US. The purpose of the original study was to collect annual data across the first four years of college on educational outcomes; cognitive, social, and vocational functioning; and use of support services to better understand the long-term impact of ADHD on college students. At the time of the present study, the original study was ongoing (see Gormley et al., 2015 for a more detailed description). For the purposes of this study, data from assessment years one and two were used.
At the beginning of the study in year one, participants were college students (N=456, 220= Male, 236= Female) ranging from 18 to 22 years of age (M = 18.23; SD = .52). The original sample of participants was 71.7% Caucasian, 12.3% African American, 5.5% Asian, 3.9% more than one race, and 6.6% other/not reported. Of the total sample, 228 students met research criteria for the ADHD) group and 228 students met research criteria for the Comparison group.
In year two, 86.6% of the sample was available for reassessment (N=395) (see Table 1 for demographic characteristics of entire sample as well as ADHD and Comparison group subsamples). Sixteen participants (3.5%) informed study personnel that they no longer wished to participate in the study. An additional 38 participants (8.3%) were unable to be reached. The demographic characteristics of the current analytic sample did not significantly differ from the original sample with regard to age, gender, race, ethnicity, number of comorbid diagnoses, highest parent education, or full scale IQ. However, individuals who dropped out of the study, or could not be reached, were less likely to take an ADID medication during their first year of college (χ2[1,420] = 3.9, p = .048) had significantly higher off-medication inattention severity scores (t[449] = −3.78, p <.001), and hyper-activity/impulsivity severity scores (t[449]=−2.77, p =.006).
Table 1.
Demographic Data and Means (Standard Deviations) for Analysis Variables
| Variable | Total Sample | ADHD Only | Comparison Only |
|---|---|---|---|
| Group (ADHD) | 51.5% | ||
| Gender (Female) | 51.8% | 52.2% | 51.3% |
| Race (non-Hispanic Caucasian) | 71.5% | 76.3% | 66.3% |
| ADHD Medication Status (% on) | 25.4% | 47.4% | |
| Disability Services (% registered) | 13.9% | 24.6% | |
| Age | 18.23 (.51) | 18.26 (.54) | 18.20 (.47) |
| Yr 1 GPA - Fall | 3.05 (.80) | 2.87 (.84) | 3.24 (.70) |
| Yr 1 GPA- spring | 2.95 (.86) | 2.80 (.90) | 3.12 (.79) |
| Yr 2 GPA - Fall | 2.90 (.88) | 2.76 (.92) | |
| Yr 2 GPA - spring | 2.91 (.90) | 2.76 (.94) | 3.07 (.83) |
| Yr 1 Credits Attempted - Fall | 14.24 (2.82) | 13.92 (2.92) | 14.54 (2.68) |
| Yr 1 Credits Attempted - Spring | 14.58 (3.18) | 14.13 (3.08) | 15.02 (3.44) |
| Yr 2 Credits Attempted - Fall | 14.01 (3.84) | 13.44 (4.15) | 14.55 (3.67) |
| Yr 2 Credits Attempted - Spring | 13.87 4.03) | 13.41 (4.34) | 14.30 (3.67) |
| Yr 1 Credits Earned Fall | 13.83 (3.08) | 13.43 (3.19) | 14.20 (2.94) |
| Yr 1 Credits Earned - Spring | 14.26 (3.38) | 13.82 (3.26) | 14.69 (3.44) |
| Yr 2 Credits Earned - Fall | 13.58 (4.11) | 12.93 (4.29) | 14.19 (3.84) |
| Yr 2 Credits Earned - Spring | 13.42 (4.40) | 12.98 (4.67) | 13.84 (4.09) |
| WASI FSIQ | 110.26 (12.07) | 110.87 (12.56) | 109.65 (11.55) |
| Highest Parent Education | 5.04 (1.43) | 5.23 (1.42) | |
| Inattention Self Rating | 10.61 (7.84) | 17.16 (4.61) | 3.67 (3.19) |
| Hyperactive/lmpulsive Self Rating | 8.87(6.60) | 13.70 (5.36) | 3.74 (2.87) |
| LASSI Anxietya | 46.83 (31.60) | 31.11 (27.41) | 62.62 (27.42) |
| LASSI Attitude | 34.06 (29.05) | 22.15 (23.71) | 46.03 (29.06) |
| LASSI Concentration | 38.08 (32.42) | 16.01 (20.99) | 60.27 (26.12) |
| LASSI Information Processing | 53.91 (29.38) | 46.94 (30.39) | 60.92 (26.62) |
| LASSI Motivation | 52.90 (32.42) | 37.28 (28.90) | 68.61 (27.90) |
| LASSI Self-Testing | 36.80 (30.09) | 27.02 (27.18) | 46.64 (29.72) |
| LASSI Selecting Main Ideas | 44.84 (31.50) | 27.93 (26.31) | 61.84 (26.82) |
| LASSI Time Management | 36.97 (31.00) | 20.88 (23.10) | 53.15 (29.51) |
| LASSI Self Testing | 43.51 (32.06) | 24.28 (24.38) | 62.84 (26.81) |
| LASSI Study Aids | 41.93 (30.30) | 37.45 (30.55) | 46.43 (29.44) |
Note. All LASSI scores are percentiles. ADHD = attention-deficit/hyperactivity disorder. GPA grade-point average. WASI = Wechsler Abbreviated Scale of Intelligence. LASSI = Learning and Study Strategies Inventory.
Screening Measures
Demographic information.
Participants provided a range of demographic information including age, gender, race (i.e., White or non-White), ethnicity (i.e., Hispanic or non-Hispanic), parent educational level, and marital status in the first year of the study.
ADHD Rating ScaleSe1f-Report Version (ADHD RS-SRV).
The ADHD RS-SRV, developed specifically for the purposes of this study, is a modified version of the ADHD RS-IV (DuPau1, Power, Anastopoulos, & Reid, 1998). The scale lists the in-attention (IN) and hyperactive-impulsive (HI) symptoms in alternating fashion, which are rated on a four-point Likert scale (0=never or rarely, 3=very often). Symptom frequency counts for both and HI are calculated by summing the number of items scored 2 or 3. The ADHD RSSRV addresses ADHD symptoms both during childhood and during the past six months, while also taking into account medication status (i.e., completed regarding symptoms on and off medication for those students receiving pharmacotherapy). Internal consistency reliability data suggest very good (.74) to excellent (.94) for the childhood and past six months reports of both IN and HI symptoms, regardless of medication status.
ADHD Rating Scale-IV: Parent Version.
The ADHD Rating Scale-IV: Parent Version was sent to parents to obtain multi-respondent diagnostic information (DuPauI et al., 1998). The scale is identical to the ADHD Rating Scale-Childhood and Past 6 Months versions; however, the wording on each item reflects that the questions are asking about the individual’s child. Parents completed the form by indicating two ratings of their child’s behavior when they were not on medication, both from the ages of 5–12 to measure childhood symptoms and in the past six months to measure current symptoms.
Semi-Structured ADHD Interview.
The Semi-Structured ADHD Interview was created for this study to address symptom presentation and impairment. The interview is based on DSM-5 adult ADHD criteria and includes nine questions about symptoms of inattention and nine questions about symptoms of hyperactivity/impulsivity to assess for symptom presence and severity (American Psychiatric Association, 2013). Additional questions explore the degree to which symptoms impair functioning as well as the age of onset of symptoms. Coefficient alphas for both the IN and HI portions of the interview were excellent (.90 and .85, respectively).
Structured Clinical Interview for DSM Disorders (SCID-I).
The SCID-I is a computer-based semi-structured interview based on the DSM-IV-TR criteria (American Psychiatric Association, 2000) that is used to test for clinically significant presentations of psychiatric disorders (First, Gibbon, Spitzer, & Williams, 2002). Because DSM-5 criteria for many non-ADHD conditions had not yet been finalized at the time these first year data were collected, DSM-IV-TR (American Psychiatric Association, 2000) guidelines were used to assess these non-ADHD conditions. Certain disorders, such as anxiety and mood disorders were routinely assessed, while others (e.g., eating disorders) were only evaluated when indicated from participants’ personal/family history. Trained graduate students in Ph.D. or Masters level clinical and school psychology programs and Ph.D. level staff conducted the SCID-I interviews. The SCID-I has adequate inter-rater reliability with kappa levels between .70 and 1.00 (First et al., 2002).
Expert panel classification.
The expert panel consisted of four PhD-level psychologists with expertise in the assessment and treatment of ADHD, including the three principal investigators of the larger longitudinal study and one consultant, who specializes in the assessment and treatment of adult ADHD. The panel utilized the data described previously to determine the eligibility for each student enrolled in the current project. Classification of ADHD or non-ADHD) Comparison for the present study was based on the unanimous decision reached by the four-member expert panel. In addition, the panel made final decisions regarding psychological classifications (e.g., anxiety or mood disorder) that may have been exclusionary or comorbid with ADHD. In instances in which the panel members came to different classifications, the entire panel discussed the case until consensus was reached.
Dependent Measures
Educational data.
College GPAs were collected for each participant through a combination of registrar (423 cases=year one, 363 cases=year two) and self-report information (33 cases=year one, 56 cases= year two) from the participants’ respective college’s Registrar offices. College GPAs were calculated on a four-point scale either ranging from 0.0–4.0 or 0.0–4.3. To adjust for this discrepancy across sites, the range for college GPA was capped at 4.0 (i.e., any value equal to or above 4.0 was recorded as 4.0). GPA was recorded for each of the first four semesters of college.
Credits attempted and earned.
The number of credits attempted and credits earned per semester were collected for each participant. Credits attempted was defined as the number of credits students registered for at the start of each semester. Credits earned was defined as the number of credits participants ultimately received at the end of each semester.
Enrollment status.
Information regarding enrollment status (i.e., whether a participant was still enrolled as a student at the university they were enrolled in the previous year) was collected yearly for each participant. In addition, we identified the percentage of students in each group that had withdrawn from one or more courses, been placed on academic probation, or been suspended from college in year one. Finally, the percentage of students who transferred to another university in year two was- identified for each group.
Predictor Measures
Several previously described measures were used as predictor measures in addition to the measures listed below, including demographic information, ADHD Rating Scales, and expert panel classification.
Cognitive ability.
Two subtests (i.e., vocabulary and matrix reasoning) of the Wechsler Abbreviated Scale of Intelligence- Second Edition (WASI-II) were administered as a standardized measure of general cognitive ability (Wechsler, 2011). The two-subtests combined to form a composite full scale IQ (FSIQ-2) and provided an estimate of each participant’s cognitive ability. Adequate average reliability for an adult sample was demonstrated for the vocabulary subtest (α=.92), matrix reasoning subtest(α=.90), and FSIQ-2 (α =.94) (Wechsler, 2011).
Learning and Study Strategies Inventory, Second Edition (LASSI).
The LASSI is an 80-item measure used to collect information on students’ awareness about and use of learning and study strategies (Weinstein & Palmer, 2002). Students rate their skill, will, and self-regulation components of strategic learning on a five-point Likert Scale (a= not at all typical of me, e= very much typical of me). The LASSI is comprised of 10 subscales that measure anxiety, attitude, concentration, information processing, motivation, selecting main ideas, self-testing, study aids, test strategies, and time management. Each subscale of the LASSI has demonstrated adequate reliability, with coefficient alphas ranging from.73-.89.
Year one medication status.
Year one medication status was collected for each participant in their first year of the study. Participants provided information on whether or not they were taking medication that year, or had been taking medication for ADHD or related issues in the past.
Year one disability services registration.
Year one Disability Services Registration status was collected for participants in their first year of the study. Participants provided information on whether they were formally registered with the Office of Disability Services on their campus.
Beck Anxiety Inventory (BAI).
The BAI is a self-report measure of anxiety symptom severity in adults (Beck & Steer, 1993). The scale includes 21 items that measure symptom severity over the past week. Each item is rated on a four-point Likert scale (0=not at all, 3=severely), with higher scores indicating greater severity of anxiety symptoms. Individuals who score higher on the BAI are more likely to be experiencing more severe symptoms of an anxiety disorder. The BAI has adequate levels of internal consistency (α=.92) and concurrent validity (Beck, Epstein, Brown, & Steer, 1988).
Beck Depression Inventory-Second Edition (BDI-II).
The BDI-II measures depression symptom severity among adults, where adults report symptom severity over the past two weeks (Beck, Steer, & Brown, 1996). The scale includes 21 items, and each item provides response options rated on a four-point scale (0 = not at all, 3 = severely). Higher ratings on each question indicate greater severity of depression symptoms. The BDI-II has strong internal consistency (α = .93) and concurrent validity with other depression measures in the assessment of college students (Beck et al., 1996).
Procedure
All procedures for the larger study were initially approved by the institutional review board (IRB) at all three project sites. Participants were recruited through university disability service offices as well as via summer orientation activities, campus newspaper, social media, and campus postings soliciting participation in the project. As part of the original study, following provision of informed consent, each participant first underwent a screening process to determine group designation and eligibility for the study.
ADHD and non-ADHD comparison group status was determined via multi-method assessment procedures that included expert panel review. The first stage of this assessment included the completion of a self-report ADHD Rating Scale (DuPaul, Power, Anastopoulos, & Reid, 1998), which was modified to address current and past ADHD symptoms, in addition to medication status. If a participant’s self-report or parent-report indicated frequent displays of 4 or more symptoms of either inattention or hyperactivity-impulsivity during both childhood and the past 6 months, a semi-structured interview for adult ADHD was then administered to address full DSM-5 criteria for ADHD, which included the requirement of 5 or more symptoms of either inattention or hyperactivity-impulsivity being present. This same interview was administered to potential Comparison participants whose self- and parent-reported responses to the ADHD Rating Scale indicated the presence of 3 or fewer symptoms for both inattention and hyperactivity-impulsivity during childhood and during the past 6 months. Participants whose interview responses continued to suggest the presence of 3 or fewer symptoms from both symptom lists were deemed eligible for the Comparison group. A panel of four ADHD experts (i.e., the three principal investigators and a nationally recognized adult ADHD consultant) reviewed all potentially eligible cases. Unanimous panel agreement was required for final determination of ADHD and Comparison group status, as well as for determination of non-ADHD psychiatric comorbidity status. For detailed information regarding ADHD diagnostic results as well as the prevalence and nature of comorbidities within the present sample, the reader is referred to a related publication by our team (Anastopoulos et al, 2016).
Once eligible for the study, participants completed a variety of measures in a standardized order over a series of meetings conducted by graduate students and doctoral level staff trained on all assessment procedures (see Anastopoulos et al., 2016; Gormley et al., 2016 for detailed description). All data used in this study were collected in the first two years of four planned annual assessments following the same procedures, with the exception of the WASI-II that was administered in the first year only. For the purposes of the current study, only year one data were used for LASSI and ARS-IV scores. Demographic information was obtained through self-report ratings and archival data. Participants were provided with monetary incentives at the completion of each meeting and a report of their overall functioning for each year they participated in the study.
Statistical Analysis
For the first hypothesis (i.e., students without ADHD would exhibit greater academic success than those in the ADHD group), three 2 (group) x 4 (semester) analyses of variance (ANOVA) were conducted to examine main effects of group, time, and their interaction on semester GPA, number of credits attempted, and number of credits earned. When GPA or credit data were missing, we used last observation carried forward (LOCF). An a priori statistical power analysis using alpha level of .05 to obtain power of .80 with a moderate effect size (d = .50) indicated that 24 participants would be needed for each group. Group differences in enrollment status (enrolled, not enrolled) in the fall and spring semesters of year two were examined with chi-square analyses. For the second hypothesis (i.e., year one outcomes [symptom dimensions, motivation, engagement with studying] would predict academic performance in year two) hierarchical regression analyses were conducted with the full sample (N = 395) of participants, and each group separately. In each analysis, demographic factors (gender, IQ, race, ethnicity, parent education level, medication status, registered with disability resource center) that may be associated with educational outcomes were entered as predictors first. Next, ADHD symptom dimension scores, and presence/absence of comorbid disorder(s) were entered into the regression model. Finally, first-year LASSI scores were included in the model. A power analysis using alpha level of .05 to obtain power of .80 assuming a multiple R of .40 and inclusion of 15 predictors indicated that 131 participants were needed.
Results
Means and standard deviations for all variables including the analyses are presented in Table 1 for the analytic sample and separately for students with and without ADHD.
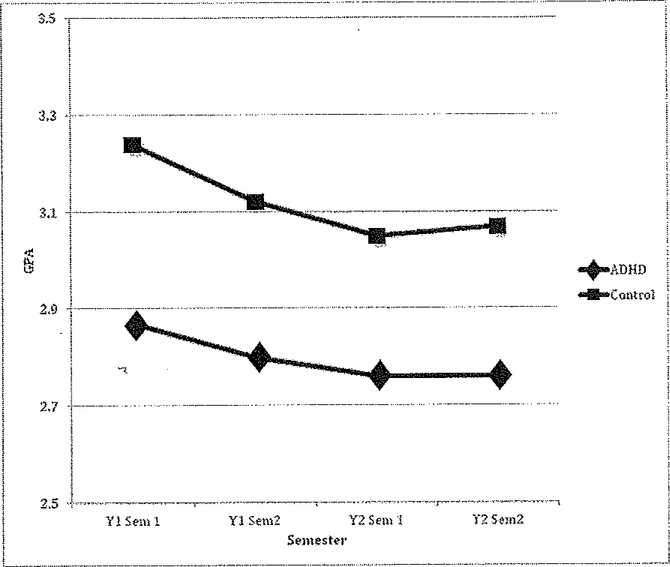
Group and Semester Differences in Academic Outcomes
The 2 (group) x 4 (semester) ANOVA for semester GPA indicated statistically significant main effects for group (F [1, 408] = 19.36, p < .001; partial eta squared = .045) and semester (F [3, 1224] 8.31, p < .01, partial eta squared = .02). The group x semester interaction was not statistically significant. Mean semester GPA was significantly higher for students without ADHD than for those with ADHD across all four semesters (see Figure 1). This group difference was small to medium in magnitude (Cohen’s d = 0.43). Trend analyses indicated that the semester effect was comprised of statistically significant linear (F [1, 408] = 14.49, p < .001) and quadratic (F [1, 408] = 5.55, p < .05) components. For both groups, semester GPA decreased in a linear fashion across the first three semesters with a plateau between the third and fourth semesters (see Figure 1).
Figure 1.
Semester GPA by ADHD vs. control group.
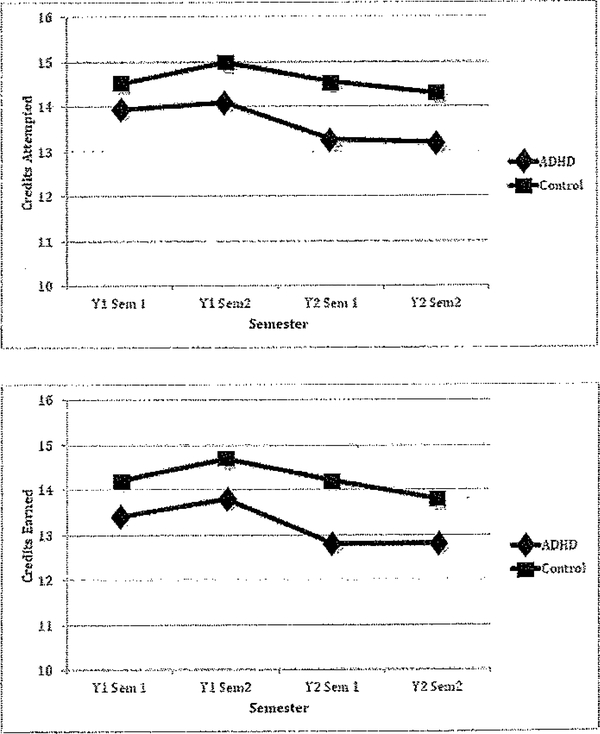
The 2 (group) x 4 (semester) ANOVA for credits attempted indicated statistically significant main effects for group (F [1, 316] = 6.98, p < .01; partial eta squared = .022) and semester (F [3, 948] = 7.12, p < .001; partial eta squared = .022). The group x semester interaction was not statistically significant. Students without ADHD attempted more credits than those with ADHD across all four semesters (see top panel, Figure 2) with this difference in the small range (Cohen’s d 0.15). The semester effect was comprised of statistically significant linear (F [1, 316] = 7.12, p <.01), quadratic (F [1, 316] = 5.98, p < .05), and cubic (F [1, 316] = 8.06, p < .01) components (see top panel, Figure 2).
Figure 2.
Credits attempted per semester by ADHD vs. control group (top). Credits earned per semester by ADHD vs. control group (bottom).
As hypothesized, similar results were obtained for semester credits earned. The 2 (group) x 4 (semester) ANOVA for credits earned indicated a statistically significant main effect for group (F [1, 316] = 7.38, p < .01; partial eta squared .023) and semester (F [3, 948] = 7.12, p < .001; partial eta squared = .022). Once again, the interaction between group and semester was not statistically significant. Students without ADHD earned significantly more credits across all four semesters relative to those with ADHD (see bottom panel, Figure 2). This group difference was small to medium in magnitude (Cohen’s d = 0.31). As was the case for credits attempted, the semester effect was comprised of significant linear (F [1, 316] = 6.94, p < .01), quadratic (F [1, 3161 5.27, p < .05), and cubic (F [1, 316] = 9.52, p < .01) trend components (see bottom panel, Figure 2).
Group Differences in College Enrollment Status
For the fall semester of year two, significantly more students with ADHD) (9.1%) were no longer enrolled in college (i.e., had dropped out) relative to non-ADHD controls (3.3%). The association between group membership and dropout rate was small (Cramer’s V = 0.12; χ2 [1] = 5.21, p < .05). In similar fashion, significantly more students with ADHD (9.8%) were not enrolled in the spring semester of year two relative to those without ADHD (2.8%). The association between group membership and dropout rate was again small (Cramer’s V = 0.14; χ2 [1] = 6.91, p < .05).
Students with ADHD were significantly more likely to withdraw from one or more courses (p = .004) in year one. A greater percentage of students with ADHD (12.1%) were placed on academic probation in year one relative to control participants (7.0%), suspended from college in year one (2.45% vs. 0.5%), or transferred to another university in year two (7.5% vs. 3.5%); however, none of these group differences were statistically significant (p values range from .06 to .11).
Prediction of Year Two Academic Outcomes
Twelve hierarchical regression analyses were conducted to examine the degree to which year one ADHD symptoms, comorbid disorders, medication status, registration with campus disability services, and study attitudes and behaviors predict year two academic functioning while controlling for demographic variables (i.e., gender, IQ, parent education level, race). When including the entire sample, the first and third stages of the regression model were statistically significant for predicting year two fall semester GPA (see Table 2) with a multiple R = .38 (adjusted R-square .09; F [20, 326] = 2.69, p < .001). Statistically significant regression weights were obtained for race (p < .05; see Table 2) and LASSI motivation (p < .001). Higher year two fall GPA was predicted by White racial status and higher scores for motivation on the LASSI in year one. Similarly, stages one and three of the regression model predicting year two spring semester GPA for all students were statistically significant (see Table 3) with a multiple R = .39 (adjusted R-square .10; F [20, 326] = 2.89, p < .001). Statistically significant regression weights were found for race (p < .01) and LASSI motivation (p < .001; see Table 3). Again, higher year two spring GPA was predicted by White racial status and higher LASSI motivation scores in year one.
Table 2.
Hierarchical Regression Analysis Summary for Year One Variables Predicting Year Two Fall GPA in Combined Samnle
| Step and Predictor Variable | B | SEB | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Step 1: | .046* | ||||
| Year one medication status | −.11 | .10 | −.07 | ||
| Disability services | −.20 | .12 | −.09 | ||
| Gender | −.16 | .08 | −.10 | ||
| Race | −.23 | .10 | −.14* | ||
| Ethnicity | .16 | .15 | .06 | ||
| WASI IQ | .002 | .003 | .03 | ||
| Parent Education | .05 | .03 | .10 | ||
| Step 2: | .063* | .017 | |||
| Year one medication status | .01 | .12 | .01 | ||
| Disability services | −.12 | .12 | −.06 | ||
| Gender | −.20 | .09 | −.13* | ||
| Race | −.23 | .10 | −.14* | ||
| Ethnicity | .16 | .15 | .06 | ||
| WASI IQ | .002 | .003 | .03 | ||
| Parent Education | .05 | .03 | .09 | ||
| Year one ARS Inattention | −.01 | .01 | −.11 | ||
| Year one ARS Hyp-Impulsivity | −.002 | .01 | −.02 | ||
| Comorbid disorder | −.09 | .10 | −.04 | ||
| Step 3: | .141*** | .08** | |||
| Year one medication status | .12 | .11 | .07 | ||
| Disability services | −.09 | .12 | −.04 | ||
| Gender | −.12 | .09 | −.08 | ||
| Race | −.25 | .10 | −.15* | ||
| Ethnicity | .14 | .14 | .05 | ||
| WASI IQ | .00 | .004 | −.005 | ||
| Parent Education | .04 | .03 | .07 | ||
| Year one ARS Inattention | −.002 | .01 | −.02 | ||
| Year one ARS Hyp-Impulsivity | −.008 | .01 | −.07 | ||
| Comorbid disorder | −.05 | .10 | −.03 | ||
| LASSI Anxiety | −.001 | .002 | −.03 | ||
| LASSI Attitude | .004 | .002 | .15 | ||
| LASSI Concentration | −.001 | .003 | −.03 | ||
| LASSI Information Processing | −.002 | .002 | −.09 | ||
| LASSI Motivation | .01 | .002 | |||
| LASSI Self-Testing | −.001 | .002 | −.04 | ||
| LASSI Selecting Main Ideas | .000 | .002 | −.02 | ||
| LASSI Study Aids | −.001 | .002 | −.04 | ||
| LASSI Time Management | −.002 | .002 | −.08 | ||
| LASSI Test Strategies | −.002 | .003 | −.09 | ||
Note. GPA= grade-point average. WASI = Wechsler Abbreviated Scale of Intelligence. ARS = ADHD Rating Scale. LASSI = Learning and Study Strategies Inventory.
p< .05.
p < .01.
p< .001.
Table 3.
Hierarchical Regression Analysis Summary for Year One Variables Predicting Year Spring Fall GPA in Combined Sample
| Step and Predictor Variable | B | SEB | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Step 1: | .061* | ||||
| Year one medication status | −.23 | .10 | −.13* | ||
| Disability services | −.24 | .13 | −.11 | ||
| Gender | −.15 | .09 | −.09 | ||
| Race | −.22 | .11 | −.12* | ||
| Ethnicity | .22 | .15 | .08 | ||
| WASI IQ | .002 | .004 | .03 | ||
| Parent Education | .08 | .03 | .13* | ||
| Step 2: | .075* | .014 | |||
| Year one medication status | −.15 | .12 | −.08 | ||
| Disability services | −.18 | .13 | −.08 | ||
| Gender | −.18 | .09 | −.11* | ||
| Race | −.23 | .11 | − .13* | ||
| Ethnicity | .22 | .15 | .08 | ||
| WASI IQ | .002 | .004 | .03 | ||
| Parent Education | .07 | .03 | −.13* | ||
| Year one ARS Inattention | −.01 | .01 | −.12 | ||
| Year one ARS Hyp-lmpulsivity | .01 | .01 | .08 | ||
| Comorbid disorder | −.15 | .10 | − .04 | ||
| Step 3: | .151*** | .075** | |||
| Year one medication status | −.04 | .12 | −.02 | ||
| Disability services | −.16 | .13 | |||
| Gender | −.08 | .09 | −.05 | ||
| Race | −.25 | .10 | −.14* | ||
| Ethnicity | .17 | .15 | .06 | ||
| WASI IQ | .001 | .004 | .01 | ||
| Parent Education | .06 | .03 | .11 | ||
| Year one ARS Inattention | −.01 | .01 | −.06 | ||
| Year one ARS Hyp-Impulsivity | .004 | .01 | .03 | ||
| Comorbid disorder | −.11 | .11 | − .07 | ||
| LAS SI Anxiety | .000 | .002 | −.02 | ||
| LASSI Attitude | .003 | .002 | .13 | ||
| LASSI Concentration | −.005 | .003 | −.21 | ||
| LASSI Information Processing | −.003 | .002 | −.10 | ||
| LASSI Motivation | .008 | .002 | .33*** | ||
| LASSI Self-Testing | .002 | .002 | .07 | ||
| LASSI Selecting Main Ideas | .003 | .003 | .12 | ||
| LASSI Study Aids | −.001 | .002 | −.02 | ||
| LASSI Time Management | .000 | .002 | −.02 | ||
| LASSI Test Strategies | −.002 | .003 | −.08 | ||
Note. GPA = grade-point average. WASI = Wechsler Abbreviated Scale of Intelligence. ARS = ADHD Rating Scale. LASSI = Learning and Study Strategies Inventory,
< .05.
p < .01
p < .001
Hierarchical regression analyses conducted only with students in the ADHD group failed to reach statistical significance for both year two fall and spring semester GPA. However, the full model predicting year two spring GPA approached significance for this group with a multiple R = .42 (adjusted R-square = .06; F [20, 145] 1.52, p = .082). A statistically significant regression weight was found for LASSI self-testing and LASSI information processing (both ps < .05) such that higher year two spring GPA was predicted by higher LASSI self-testing scores and lower LASSI information processing scores.
Among students in the comparison group, the third stage of the hierarchical regression analysis for year two fall semester GPA was statistically significant (see Table 4) with a multiple R = .46 (adjusted R-square = .11; F [20, 160] = 2.10, p < .01). Statistically significant regression weights were found for race (p < .05), LASSI attitude (p < .05), and LASSI motivation (p < .001). Higher GPA was predicted by White racial status and higher scores for attitude and motivation on the LASSI in year one. Similarly, only the third stage of the hierarchical regression analysis for year two spring semester GPA was statistically significant (see Table 5) with a multiple R = .44 (adjusted R-square = .09; F [20, 160] = 1.91, p < .05). The only statistically significant predictor was year one LASSI motivation such that higher scores predieted higher year two spring semester GPA.
Table 4.
Hierarchical Regression Analysis Summary for Year One Variables Predicting Year Two Fall GPA in Comparison Students
| Step and Predictor Variable | B | SEB | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Step 1: | .076 | ||||
| Year one medication status | −.52 | .38 | −.10 | ||
| Disability services | .13 | .34 | .03 | ||
| Gender | −.16 | .11 | −.11 | ||
| Race | −.24 | .13 | −.15 | ||
| Ethnicity | .13 | .21 | .05 | ||
| WASI IQ | .003 | .01 | .04 | ||
| Parent Education | .08 | .04 | .15 | ||
| Step 2: | .078 | .003 | |||
| Year one medication status | −.53 | .39 | −.10 | ||
| Disability services | .15 | .35 | .03 | ||
| Gender | −.16 | .12 | −.11 | ||
| Race | −.26 | .14 | −.16 | ||
| Ethnicity | .14 | .21 | .05 | ||
| WASI IQ | .003 | .01 | .04 | ||
| Parent Education | .08 | .04 | .15 | ||
| Year one ARS Inattention | .01 | .02 | .05 | ||
| Year one ARS Hyp-Impulsivity | −.01 | .02 | −.05 | ||
| Comorbid disorder | −.05 | .15 | −.02 | ||
| Step 3: | .208** | .129** | |||
| Year one medication status | −.13 | .39 | −.03 | ||
| Disability services | .22 | .35 | .05 | ||
| Gender | −.08 | .12 | −.05 | ||
| Race | −.31 | .13 | −.19* | ||
| Ethnicity | .13 | .21 | .05 | ||
| WASI IQ | −.001 | .01 | −.01 | ||
| Parent Education | .07 | .04 | .13 | ||
| Year one ARS Inattention | .03 | .03 | .13 | ||
| Year one ARS Hyp-Impulsivity | −.01 | .02 | −.04 | ||
| Comorbid disorder | −.02 | .15 | −.01 | ||
| LASSI Anxiety | .001 | .003 | .02 | ||
| LASSI Attitude | .01 | .003 | .23* | ||
| LASSI Concentration | −.004 | .004 | −.15 | ||
| LASSI Information Processing | −.002 | .003 | −.06 | ||
| LASSI Motivation | .01 | .003 | 43*** | ||
| LASSI Self-Testing | −.01 | .003 | −.18 | ||
| LASSI Selecting Main Ideas | .000 | .003 | −.02 | ||
| LASSI Study Aids | −.001 | .002 | −.03 | ||
| LASSI Time Management | .000 | .003 | −.01 | ||
| LASSI Test Strategies | −.003 | .004 | −.11 | ||
Note. GPA = grade-point average. WASI = Wechsler Abbreviated Scale of Intelligence. ARS = ADHD Rating Scale. LASSI = Learning and Study Strategies Inventory.
p < .05
p < .01
p < .001
Table 5.
Hierarchical Regression Analysis Summary for Year One Variable Predicting Two Spring GPA in Comparison Students
| Step and Predictor Variable | B | SEB | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Step 1: | .075 | ||||
| Year one medication status | |||||
| Disability services | −.63 | .35 | −.13 | ||
| Gender | −.17 | .12 | −.11 | ||
| Race | −.16 | .14 | −.10 | ||
| Ethnicity | .15 | .22 | .06 | ||
| WASI IQ | .01 | .01 | .09 | ||
| Parent Education | .07 | .04 | .12 | ||
| Step 2: | .077 | .003 | |||
| Year one medication status | −.76 | .40 | |||
| Disability services | −.63 | .36 | −.13 | ||
| Gender | |||||
| Race | .17 | .14 | −.10 | ||
| Ethnicity | .16 | .22 | .06 | ||
| WASI IQ | .01 | .01 | .09 | ||
| Parent Education | .07 | .12 | |||
| Year one ARS Inattention | .001 | .02 | .002 | ||
| Year one ARS Hyp-Impulsivity | .01 | .02 | .05 | ||
| Comorbid disorder | −.02 | .16 | −.01 | .192 * | |
| Year one medication status | −.36 | .41 | −.07 | ||
| Disability services | −.53 | .37 | −.11 | ||
| Gender | −.07 | .13 | −.05 | ||
| Race | −.22 | .14 | −.13 | ||
| Ethnicity | .13 | .21 | .05 | ||
| WASI IQ | .002 | .01 | .04 | ||
| Parent Education | .06 | .04 | .11 | ||
| Year one ARS Inattention | .03 | .03 | .11 | ||
| Year one ARS Hyp-Impulsivity | .01 | .02 | .02 | ||
| Comorbid disorder | .01 | .16 | .003 | ||
| LASSI Anxiety | .000 | .003 | −.02 | ||
| LASSI Attitude | .01 | .003 | .17 | ||
| LASSI Concentration | −.01 | .004 | −.18 | ||
| LASSI Information Processing | .000 | .003 | −.01 | ||
| LASSI Motivation | .01 | .003 | .42 ** | ||
| LASSI Self-Testing | −.003 | .003 | −.11 | ||
| LASSI Selecting Main Ideas | .002 | .004 | .06 | ||
| LASSI study Aids | .000 | .002 | −.02 | ||
| LASSI Time Management | .001 | .003 | .03 | ||
| LASSI Test Strategies | −.003 | .004 | −.12 | ||
Note. GPA = grade-point average. WASI = Wechsler Abbreviated Scale of Intelligence. ARS = ADHD Rating Scale. LASSI = Learning and Study Strategies Inventory
< .05.
p < .01.
p < .001.
The first stage of the hierarchical regression analysis for year two credits attempted by the entire sample was statistically significant with multiple R = .25 (adjusted R-square = .04; F [7, 283] = 2.75, p < .01). The two subsequent regression stages did not contribute significantly more variance to the prediction model. The only significant predictor was WASI IQ (p < .05). Interestingly, lower IQ predicted higher number of credits attempted in year two. In similar fashion, only the first stage of the prediction model for year two credits earned was statistically significant with multiple R = .24 (adjusted R-square = .04; F [7, 283] = 2.52, p < .05). The only significant predictor was WASI IQ (p < .01) although there was a nonsignificant trend for first year medication status (p = .064). Again, higher IQ predicted lower number of credits earned in year two.
Among students in the ADHD group alone, only the first stage of the hierarchical regression analysis for year two credits attempted was statistically significant with multiple R = .32 (adjusted R-square = .06; F [7, 130] = 2.19, p < .05). Similar to the combined sample, the only significant predictor was WASI IQ (p < .01) such that lower IQ again predicted a higher number of credits attempted in year two. Only the first stage of the prediction model for year two credits earned was statistically significant with multiple R = .32 (adjusted R-square = .06; F [7, 1301 = 2.17, p < .05). Again, the only significant predictor was WASI IQ (p < .01) with higher IQ predicting a lower number of credits earned.
Finally, among only students in the comparison group, hierarchical regression analyses for both year two credits attempted and credits earned failed to reach statistical significance.
Discussion
In accordance with the research literature (e.g., Weyandt & DuPaul, 2006), it was hypothesized that college students with ADI--ID would fare worse than college students without ADHD on measures of academic success. The results of this study were generally in line with this hypothesis. Specifically, students with ADI-ID earned lower GPAs than those in the control group; this difference was small to medium in magnitude. This disparity in GPA persisted across the first two years of college even as GPA for both groups declined through the fall of the second year of college, reaching a plateau in the spring of the second year. This main effect of ADHD status on GPA aligns with the hypothesis and previous work suggesting that college students with ADHD tend to obtain significantly lower GPAs than their peers without ADHD (Gormley et al., 2016), as well as with the larger body of literature indicating that younger students with ADHD experience academic impairment in school (e.g., Biederman et al., 2011). The small to medium effect size obtained in this study (.40) is smaller than the (d = .71) effect size reported in the Frazier and colleagues (2007) meta-analysis of children with ADHD. This difference may be indicative of the fact that college students with ADHD are an educationally more successful subgroup of the ADHD population.
Although the GPA trajectories were similar for the two groups, differences in enrollment status were observed over the first two years of college. Participants in the ADHD group were more likely to withdraw from one or more courses in year one and were approximately three times more likely to be listed as non-enrolled (e.g., as a result of dropout) in year two. This finding that college students with ADHD experience greater difficulties in maintaining their enrollment status is not surprising given the current literature suggesting that individuals with ADHD are less likely to attend college than their non-ADHD peers (Hechtman, 2017) and when they do enroll, are less likely to earn a degree (Barkley, Fischer, Smallish, & Fletcher, 2002; Hechtman et al., 2016).
In addition to enrolling in fewer courses, students with ADHD also completed fewer credits. Specifically, college students with ADHD completed, on average, one less academic credit per semester than individuals in the control group. This group difference was consistent across the first two years of college. For both credits earned peaked in the spring of the first year and then declined in the second year. Although speculative, it is possible students may face increased time pressures (e.g., employment) or that courses may become more difficult in the second year of college. It is also possible that college students with ADHD may be responding to advice from academic advisors to enroll in fewer credits. In general, these findings are consistent with the research hypotheses and the larger body of literature indicating that college students with ADHD are at risk for poorer academic outcomes than students without this disorder (e.g., Advokat et al., 2011; Lewandowski, Gathje, Lovett, & Gordon, 2013).
Several variables including motivation, IQ, comorbidity, medication status, and registration with disability services were further examined as potential predictors of academic outcomes. Different variables in year one predicted GPA and credit status in year two. For analyses that included the entire sample or comparison students only, student race and the LASSI subscale for motivation emerged as predictors of GPA, with first-year motivation being the strongest predictor of year two GPA. GPA prediction models for the ADHD subsample were not statistically significant, perhaps due to limited statistical power. Alternatively, WASI IQ in year one was the only significant predictor of the number of credits that students attempted and earned in the second year of college for analyses including the entire sample or the subsample of students with ADHD. Interestingly, higher IQ predicted lower number of credits attempted and earned. It may be the case that students with higher IQs selected fewer but more difficult courses than students with lower IQs. Surprisingly, given the importance of symptom dimensions in predicting outcomes for children with ADHD (e.g., Langberg, Dvorsky, & Evans, 2013), symptom ratings did not emerge as a significant predictor of academic outcomes for college students in any of the analyses. It is possible that other predictors (e.g., medication status) are correlated with symptom ratings and account for similar variance in academic functioning. Overall, these findings are consistent with the study’s prediction that college students without ADHD experience greater academic success in the first two years of college than students with ADHD.
Strengths and Limitations
The current study adds a longitudinal perspective to the literature describing the educational outcomes of college students with ADHD. The longitudinal design of the present study allows for an examination of patterns over the first two years of college, which are critical for identifying points of intervention to bolster later success. Additionally, the large and heterogeneous sample comprised of students from several colleges and universities, included a non-ADHD Comparison group. The current study also controlled for demographic variables (e.g., IQ) such that the findings explicate the degree to which year one variables impact year two academic functioning above and beyond factors typically associated with educational success.
Findings from this study should also be interpreted in light of its limitations. First, study skills data were collected via self-report, so students may have been biased in reporting on their own study habits. Second, descriptive analyses demonstrated possible multicollinearity evidenced by significant correlations among the LASSI subscales. However, inspection of both the VIF and Tolerance variables indicated that all variables were within the accepted limits of below 4 and above 0.1, respectively (Field, 2009). Thus, the assumption of multicollinearity was not violated; however, a cautious interpretation of analyses including the LASSI subscales as predictors is still warranted.
Several characteristics of the sample also represent limitations to the current study. Participants were first-year college students and recruited from four-year east coast universities. Thus, results may not generalize to other college populations, such as students in community colleges with broader age ranges. Participants with ADHD as well as non-White participants were more likely than those without ADHD to drop out of the study between year one and year two. Among dropouts, students with a higher level of hyperactivity-impulsivity symptoms while on medication were overrepresented. Further, the “last observation carried forward” method of observation may have biased the results, potentially overestimating student GPA and credits attempted/completed.
Implications and Future Directions
Clinicians and educators working with college students can use findings from the current study to recognize that students with ADHD are at a heightened risk of negative academic outcomes (i.e., fewer credits completed and lower GPAs) within their first two years of college, which in turn can impact their chances of graduation and subsequent professional success. Although a matter for additional empirical study especially given the possible limitations of typical support strategies such as educational accommodations (Lewandowski, et al., 2013; Miller, Lewandowski, & Antshel, 2013), it is assumed that college students with ADHD may benefit from academic counseling, coaching, and other supports to ensure that they are prepared to graduate. Given the fact that college students with ADHD tend to lag behind their peers in credit completion, disability service providers can help students with ADHD plan for the possibility of needing to make up credits (e.g., by taking summer courses or an extra semester) so they remain on-track with a realistic time frame to graduation.
Based on findings demonstrating that good study habits and motivation to study are predictive of GPA, college-based practitioners should consider offering services that help students improve their study skills and increase their academic self-efficacy and motivation to study. Time effects found in the present study show the importance of providing services early on in college. Similar to students who do not have ADHD, students with ADHI) may benefit most from receiving services at the beginning of their college career as well as during the transition from high school to college. This may be accomplished through screening to identify incoming college students with ADHD who are at the highest risk of academic difficulties or dropping out to target that group as early as possible. Based on the present findings, symptom dimensions may not be as useful an indicator of risk for academic difficulties relative to measures that tap motivation and attitude towards studying. It may be especially important to provide supports for non-White students with ADHD) and students with poor study skills, as these individuals face heightened academic risks compared to the general population of college students with ADHD. College-based clinicians may wish to build in opportunities for students to learn about services that are available to them, as these services may not be well known.
In the future, researchers can build upon the current study by seeking to determine what strategies are most effective in working with students with ADHD from the beginning of college. This may include programs that help students transition from high school to college or coaching for study skills. Researchers can also continue to examine patterns across all four years of college, or differential patterns for a more diverse sample of students. Trajectory analyses can help determine the key time point for intervention, which, based on findings of the current study, appears to be as early as possible in a student’s college career. There is also a need to examine post-college outcomes for college students with ADHD to understand the long-term effects of students’ early college experiences.
Conclusion
This is the first study to examine the trajectory of educational outcomes for college students with ADHD in comparison to their peers without ADHD. As hypothesized, findings revealed that students with ADHD experience more academic difficulties, including having lower GPAs, attempting and earning fewer credits, and being more likely to drop out of school, than students without ADHD from the very beginning of college. These patterns were shown to persist as students with ADHD continued through their second year of college. Study skills and habits, particularly related to motivation, reported in year one were found to be important predictors of year two outcomes, suggesting that providing services that may presumably boost motivation as early as possible in college is essential, to target students before they begin to struggle. These longitudinal findings are preliminary, representing only the first two years of this four-year study. Subsequent studies will more fully address the longitudinal trajectories of these students over the later college years. The implication of these preliminary results is that universities should be encouraged to offer programs to enhance student study skills and increase academic motivation. These findings can be incorporated into clinical practice by professionals working with college students with ADHD and future research is warranted to examine the most effective strategies for supporting this population’s educational success.
About the Authors
George J. DuPaul received his B .A. degree in psychology from Wesleyan University and Ph.D. in school psychology from the University of Rhode Island. He has extensive experience providing consultative support regarding ADHD to families, school personnel, and health care professionals. He is currently a professor in the School Psychology program of Lehigh University. His research interests include assessment and treatment of A_DHD from early childhood to the college population. He can be reached by email at gjd3@lehigh.edu.
Melanie K. Franklin is a Ph.D. student in school psychology at Lehigh University in Bethlehem PA. She received her B.A. degree in psychology from Muhlenberg College and her M.Ed. degree in Human Development from Lehigh University. Melanie’s research interests include treatment of ADHD, factors that impact treatment adherence in youth and emerging adults, and pediatric school psychology. She can be reached by email at mkf213@1ehigh.edu.
Brittany Pollack received her B.A. degree in Psychology and B.S. degree in Family Science from the University of Maryland, College Park. She received her Ph.D. in School Psychology from Lehigh University in August 2017. Her early career experience includes working as a school psychologist in the Philadelphia area. Her research interests include ADHD and associated academic, social, and emotional functioning. She can be reached by email at brittanypollack12@ gmail.com.
Kristen F. Stack received her B.A. degree in Psychology from Cornell University and her M.Ed. in Human Development from Lehigh University, where she is currently working toward a Ph.D in School Psychology. She has experience providing assessment and intervention for students with disabilities, including ADHD and LD. Her research interests include educational resilience and academic motivation. She can be reached by email at ksf43@1ehigh.edu.
Aliza Jaffe is a Ph.D. student in School Psychology at Lehigh University in Bethlehem, PA. She received her B.A. degree in Psychology and Education Studies at Washington University in St. Louis, and she received her M.Ed. degree in Human Development from Lehigh University. Aliza’s research interests include determining predictors of academic and socioemotional functioning in children and adolescents with ADHD, as well as care coordination within pediatric psychology. She can be reached by email at arj215@1ehigh.edu.
Matthew J. Gormley received his B.A. degree in psychology from the State University of New York, College at Geneseo and Ph.D. in school psychology from Lehigh University. He is currently an Assistant Professor in the Educational Psychology department at the University of Nebraska-Lincoln. He is interested in the development and application of individualized and continuous supports across major (e.g., secondary to post-secondary) and minor transitions (e.g., second to third grade) within, to, and from academic settings. Additionally, he is interested in the intersections and collaborations between families, schools, and healthcare settings. He can be reached by email at mgorm_ley2@unl.edu.
Arthur D. Anastopoulos received his B.A. in Child Study from Tufts University, his M.A. in General/Experimental Psychology from Wake Forest University, and his Ph.D. in Clinical Psychology from Purdue University. He has extensive experience providing clinical services and consultation to children, adolescents, and adults with ADHD. He is currently a professor in the Department of Human Development and Family Studies at the University of North Carolina at Greensboro. His research interests include the assessment and treatment of ADHD and its associated features across the life span, with a current focus on emerging adults with ADHD attending college. He can be reached by email at ada@uncg.edu.
Lisa Weyandt received her B.S. degree in Human Development and Family Studies from Penn State University and Ph.D. in school psychology from the University of Rhode Island. She is currently a professor in the Department of Psychology and George and Anne Ryan Institute of Neuroscience at the University of Rhode Island. Her research interests include assessment and treatment of ADI--ID in children, adolescents and college students. She can be reached by email at lisaweyandt@uri.edu.
References
- Advokat C , Lane SM , & Luo C (2011). College students with and without ADHD: Comparison of self-report of medication usage, study habits, and academic achievement. Journal of Attention Disorders, 15, 656–666. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Anastopoulos AD, DuPaul GJ, & Weyandt LL, Morrissey-Kane E, Sommer JL, Rhoads LH, Gudmundsdottir BG (2016). Rates and patterns of comorbidity among first-year college students with ADHD. Journal of Clinical Child & Adolescent Psychology. Advance online publication. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (2015). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York, NY: Guilford Press. [Google Scholar]
- Barkley RA, Fischer M, Smallish L, & Fletcher K (2002). The persistence of attention-deficit/ hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology, 111, 279–289. [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, & Fletcher K (2006). Young adult follow-up of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 192–202. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, & Fischer M (2008). ADHD in adults: What the science says. New York, NY: Guilford Press. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893–897. [DOI] [PubMed] [Google Scholar]
- Beck AT, & steer RA (1993). Beck Anxiety lnventory manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck AT, steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Best JR, Miller PH, & Naglieri JA (2011). Relations between executive function and academic achievement from ages 5 to 17 in a large, representative national sample. Learning and Individual Differences, 21, 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Clarke A, Lomedico A , & Faraone SV (2011). Predictors of persistent ADHD: An Il-year follow-up study. Journal of Psychiatric Research, 45, 150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramham J, Murphy DGM, Xenitidis K, Asherson P, Hopkin G, & Young S (2012). Adults with attention deficit hyperactivity disorder: An investigation of age-related differences in behavioural symptoms, neuropsychological function and co-morbidity. Psychological Medicine, 42, 2225–2234. [DOI] [PubMed] [Google Scholar]
- Brown TE (2000). Attention-deficit disorders and comorbidities in children, adolescents, and adults. Washington, DC: American Psychiatric Press. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD , & Reid R (1998). ADHD rating scale-IV: Check-lists, norms, and clinical interpretation. New York: Guilford Press. [Google Scholar]
- DuPau1 GJ, Weyandt LL, O’Dell SM, & Varejao M (2009). College students with ADHD: Current status and future directions. Journal of Attention Disorders, 13, 234–250. [DOI] [PubMed] [Google Scholar]
- Field AP (2009). Discovering statistics using SPSS (3rd ed.). London: Sage Publications. [Google Scholar]
- First MB, Gibbon M, Spitzer RL , & Williams JBW (2002). User’s guide for the structured clinical interview for DSM-IV-TR Axis I disorders-research version (SCID-I for DSM-IV-TR, November 2002 Revision). New York, NY: Biometrics Research. [Google Scholar]
- Fischer M, Barkley RA, Smallish L , & Fletcher K (2005). Executive functioning in hyperactive children as young adults: Attention, inhibition, response perseveration, and the impact of comorbidity. Developmental Neuropsychology, 27, 107–133. [DOI] [PubMed] [Google Scholar]
- Fleming AP, & McMahon RJ (2012). Developmental context and treatment principles for ADHD among college students. Clinical Child and Family Psychology Review, 15, 303–329. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Glutting JJ, & Watkins MW (2007). ADHD and achievement: Meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. Journal of Learning Disabilities, 40, 49–65. [DOI] [PubMed] [Google Scholar]
- Gormley MJ, DuPau1 GJ, Weyandt LL & Anastopoulos AD (2016). First-year GPA and academic service use among college students with and without ADHD. Journal of Attention Disorders. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormley MJ, Pinho T , Pollack B, Puzino K, Franklin M„ Busch C, DuPau1 GJ, Weyandt LL , & Anastopoulos AD (2015). Impact of study skills and parent education on first-year GPA among college students with and without ADHD: A moderated mediation model. Journal of Attention Disorders. Advance online publication [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hechtman L (2017). Attention deficit hyperactivity disorder: Adult outcome and its predictors. New York: Oxford University Press. [Google Scholar]
- Hechtman L, Swanson JM, Sibley MH , Stehli A, Owens EB, Mitchell JT,...Nich01s JQ (2016). Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 945952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiligenstein E, Guenther G, Levy A , Savino F , & Fulwiler J (1999). Psychological and academic functioning in college students with attention deficit hyperactivity disorder. Journal of American College Health, 47, 181–185. [DOI] [PubMed] [Google Scholar]
- Hysenbegasi A, Hass SL, & Rowland CR (2005). The impact of depression on the academic productivity of university students. The Journal of Mental Health Policy and Economics, 8, 145–151. [PubMed] [Google Scholar]
- Langberg JM, Dvorsky MR , & Evans SW (2013). What specific facets of executive function are associated with academic functioning in youth with attention-deficit/hyperactivity disorder? Journal of Abnormal Child Psychology, 41, 1145–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowski L, Gathje RA , Lovett BJ, & Gordon M (2013). Test-taking skills in college students with and without ADHD. Journal of Psychoeducational Assessment, 31, 41–52. [Google Scholar]
- Loe 1, & Feldman H (2007). Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology, 32, 643–654. [DOI] [PubMed] [Google Scholar]
- Miller LA, Lewandowski LJ, & Antshel KM (2015). Effects of extended time for college students with and without ADHD. Journal of Attention Disorders, 19, 678–686. [DOI] [PubMed] [Google Scholar]
- Pryor J,H, Hurtado S, DeAngelo L, PaluckiBlake L , & Tran S (2010). The American freshman: National norms fall 2010. Los Angeles: Higher Education Research Institute, UCLA. [Google Scholar]
- Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, & Bissada NN (2002). Criterion validity, severity cut scores, and test-retest reliability of the Beck Depression Inventory-II in a counseling center sample. Journal of Counseling Psychology, 49, 381–385. [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence-second edition manual. Bloomington, Pearson. [Google Scholar]
- Weinstein CE, & Palmer DR (2002). Learning and Study Strategies Inventory-second edition: User manual. Clearwater, FL: H&H Publishing Company, Inc. [Google Scholar]
- Weyandt LL, & DuPau1 GJ (2006). ADHD in college students. Journal of Attention Disorders,10, 9–19 [DOI] [PubMed] [Google Scholar]
- Weyandt LL, DuPau1 GJ, Verdi G., Rossi JS, Swentosky AJ, Vilardo B .Carson KM (2013). The performance of college students with ADHD: Neuropsychological, academic, and psychosocial functioning. Journal of Psychopathology, and Behavioral Assessment, 35, 421–435. [Google Scholar]
- Weyandt L, Iwaszuk W, Twaites K, Greenlaw C, Schepman S, Fouts H, Tramblay N, & Olerton M (2003). The Internal Restlessness Scale. Performance of college students with and without ADHD. Journal of Learning Disabilities, 36, 382–389. [DOI] [PubMed] [Google Scholar]
- wolf LE, Simkowitz e, & Carlson H (2009). College students with attention-deficit/hyperactivity disorder. Current Psychiatry Reports, 11, 415–421. [DOI] [PubMed] [Google Scholar]
- Zoromski AK, Owens JS, Evans SW, & Brady CE (2015). Identifying ADHD symptoms most associated with impairment in early childhood, middle childhood, and adolescence using teacher report. Journal of Abnormal Child Psychology, 43, 1243–1255. [DOI] [PubMed] [Google Scholar]