Abstract
The translation of knowledge from exercise training research into the clinical management of multiple sclerosis (MS), stroke, and Parkinson’s disease (PD) requires evidence-based guidelines that are uniformly recognizable by healthcare practitioners and patients/clients. This paper synthesized resources that reported aerobic and resistance training guidelines for people with MS, stroke, and PD. Systematic searches yielded 25 eligible resources from electronic databases and websites or textbooks of major organizations. Data were extracted (exercise frequency, intensity, time, and type) and synthesized into three sets of recommendations. Exercise guidelines for MS consistently recommended 2–3 days/week of aerobic training (10–30 minutes at moderate-intensity) and 2–3 days/week of resistance training (1–3 sets of 8–15 repetition maximum (RM)). Exercise guidelines for stroke recommended 3–5 days/week of aerobic training (20–40 minutes at moderate-intensity) and 2–3 days/week of resistance training (1–3 sets between 8–15 repetitions between 30–50% 1-RM). Exercise guidelines for PD recommended 3–5 days/week of aerobic training (20–60 minutes at moderate-intensity), and 2–3 days/week of resistance training (1–3 sets of 8–12 repetitions between 40–50% of 1-RM). This harmonization of exercise guidelines provides a prescriptive basis for healthcare providers, exercise professionals, and people with MS, stroke, and PD regarding exercise programming.
Keywords: Exercise, Rehabilitation, Guidelines, Neurologic diseases
Introduction
Multiple sclerosis (MS), stroke, and Parkinson’s disease (PD) are among the most common, non-traumatic causes of mobility disability brought about by damage within the central nervous system among adults in the United States and worldwide.1–3 There are an estimated 1.1 million adults living with MS in the United States and 2.5 million adults with MS worldwide.1 There further are an estimated 6.8 million adults living with stroke,2 and nearly 1 million adults living with PD in the United States.3 MS, stroke, and PD have different causes and neurological trajectories, but result in similar and substantial personal burden based on compromised mobility and cognition, and/or symptoms such as fatigue, depression, pain, and reduced quality of life and participation.4 Such consequences require the application of rehabilitation, over-and-beyond traditional medical treatments, as an approach for managing the diseases and associated manifestations over time.
There has been substantial interest in the benefits of exercise training as a rehabilitation approach for managing the consequences of MS, stroke, and PD.4 Indeed, the quantity of literature on exercise training among these groups has expanded substantially over the past decade.4 The benefits of exercise training have been documented in Cochrane reviews of MS,5 stroke,6 and PD.7 The common benefits from exercise participation can include improvements in physiological capacity (e.g., aerobic endurance, muscular strength/endurance, walking ability), symptoms (e.g., fatigue, depression), and quality of life.4,8,9 Collectively, the evidence demonstrates that exercise training is an efficacious approach for managing the common consequences of MS, stroke, and PD, and this presents the possibility of knowledge translation through the patient-provider interaction in the context of comprehensive health care.
The promotion of exercise through the patient-provider interaction has been identified as a new avenue for addressing the problem of physical inactivity among people with MS.10 This requires that healthcare providers and exercise professionals have clear guidelines on exercise prescription for promotion of behavior change among patients/clients. Such guidelines should specify the type and dose of exercise necessary for improving outcomes and managing comorbid conditions. The guidelines further should be based on the highest level of evidence for increasing the likelihood of being translated into clinical practice.11 Of note, there are multiple existing guidelines for describing exercise prescription in MS, stroke, and PD, and this can be overwhelming and confusing for clinicians and providers who do not have substanial training in exercise behavior. This observation alone supports that consolidating and harmonizing the existing resources into a single resource, in-and-of-itself, is of value for clinicians and providers. The creation of summary guidelines for MS, stroke, and PD can serve as a beacon for clinicians in selecting and providing an appropriate prescription, and the guidelines might differ based on the degree of preparedness for exercise. Such an effort can further assist researchers in evaluating the question of exercise dosage. The question of exercise dosage is an important priority in MS,12 stroke,6 and PD.7
Currently, there is no literature review that examines and consolidates existing sets of exercise guidelines for people with MS, stroke, and PD. This paper describes a rapid review and consolidation of the literature on exercise guidelines for people with MS, stroke, and PD. The primary aims of this review were to (1) identify, report, and consolidate the existing exercise prescription guidelines for people with MS, stroke, and PD, and (2) harmonize the existing prescriptions into a set of general and advanced exercise guidelines, when possible, per disease group. The advanced exercise guidelines would differ from the general guidelines based on the degree of preparedness and experience for exercise training.
Methods
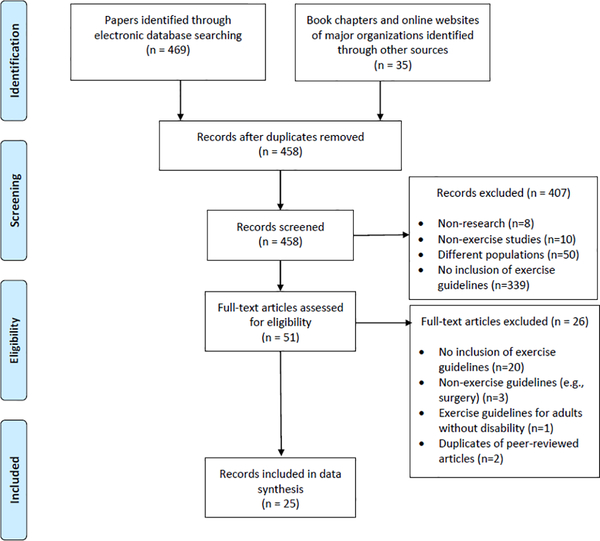
This rapid review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.13 This study also conforms to all PRISMA guidelines and reports the required information accordingly (see Supplementary Checklist). Using systematic review procedures, resources that reported exercise guidelines were identified, reviewed, synthesized, and aggregated into specific exercise recommendations for MS, stroke, and PD, separately. This was supported through the inclusion of exercise guidelines identified in books as well as online websites of major organizations related to exercise and the three groups (e.g., American College of Sports Medicine, American Physical Therapy Association, American Heart Association).
Search strategies
Systematic searches were conducted on April 10, 2018 to identify papers and reports on exercise guidelines for MS, stroke, and PD using three electronic databases: PubMed, CINAHL, and Google Scholar, for the period of inception date through April 2018. The electronic strategy included multiple search strings of key terms, such as exercise/physical activity, prescription/recommendation/guideline, and MS, stroke, or PD. An example of a search string is provided in Appendix I. These searches were updated in September 25, 2018 to identify papers and reports that could have potentially been published during the preparation of this paper for submission.
Textbook chapters on exercise guidelines for persons with MS, stroke, and PD were included in this paper. Three textbooks were identified, and these were published by the American College of Sports and Medicine (ACSM): ACSM’s Resources for Clinical Exercise Physiology; ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities; ACSM’s Guidelines for Exercise Testing and Prescription.14–16 The prescriptions in textbooks seemly differed from the papers, and appeared to be based on expert experience and opinion. Thus, inclusion of the textbooks in this paper is warranted for a complete and comprehensive synthesis of available guidelines.
The final search strategy involved an extensive Internet search for organizations that provided information and resources for people with MS, stroke, and PD. The organization websites were then reviewed for exercise information and guidelines. The review of organization websites was performed between June 15 and 30, 2018.
Eligibility criteria
Identified resources had to meet two or more criteria to be included in this review: (1) targeted adults with MS, stroke, or PD (aged 18 years or older); (2) reported exercise guidelines incorporating recommendations for full or partial inclusion of frequency, intensity, time, and type; (3) provided recommendations for muscular strength and/or cardiovascular endurance; (4) published in peer-reviewed journals; (5) endorsed or commissioned by prominent organizations (i.e., textbooks, reports); (6) available on organization websites; and (7) published in English. Resources were excluded based on the following criteria: (1) non-research publications (i.e., conference presentations, study protocol, dissertations); (2) no inclusion of exercise guidelines for either aerobic fitness and/or muscular strength; (3) exercise recommendations based on a single study (e.g., recommendations generated within the discussion section of a single published exercise trial).
Data extraction
The electronic search strings were created and refined with the help of a librarian. The primary analyst narrowed these searches by filters based on the inclusion and exclusion criteria of this review, including age, English language, and human subject research. After retrieving papers, the primary analyst conducted article selection/screening and data extraction processes by following a series of steps: (1) duplicate articles were excluded; (2) all articles were screened for eligibility at the abstract level; (3) remaining articles were screened in-depth at the full-text level; (4) data were systematically extracted into three spreadsheets based on diagnoses and seven sub-domains, including first author, year, exercise frequency, intensity, time and type, and special considerations; (5) data retrieved from textbooks and organization websites were coded by the same format; and (6) extracted data were cross-checked for accuracy by a second analyst.
The extracted data were aggregated into tables, and the findings were reviewed and summarized into three descriptions of exercise guidelines per disease group by a senior author. The descriptions were then reviewed by an expert review panel for consensus. The panel consisted of three researchers who had advanced knowledge with MS, stroke, and PD, and an adapted exercise specialist, a rehabilitation engineer, and a health services researcher/biostatistician with a specialization in disability outcomes research. Importantly, all members of the review panel had five or more years of experience with rehabilitation research, particularly exercise training in MS, stroke, and/or PD.
The panel reviewed, discussed, and negotiated toward agreement on a consensus provision regarding a general and, when possible (i.e., enough evidence to support it), an advanced exercise prescription. The goal of the general exercise prescription was to provide a recommendation for people who are irregularly/infrequently physically active. The advanced prescription was created to provide a recommendation for people who are regularly participating in an exercise program and/or people who seek greater benefits from exercise training.
Results
Results of the study selection process are provided in a PRISMA flowchart in Figure 1. The search strategy returned 469 papers from the electronic databases (MS, n=107; stroke, n=309; PD, n=53) that resulted in 18 eligible papers for inclusion (MS, n=817–25, Stroke, n=626–31, PD, n=432–35). There were seven additional resources from three textbooks14–16 and four organization websites (MS, n=236,37; stroke, n=138; PD, n=339–41). The list of resources that were identified and reviewed through textbooks and websites are provided in Appendix II. All three textbooks provided guidelines for MS, stroke, and PD. Some organization websites provided exercise guidelines for more than one group. For example, the American Physical Therapy Association and the National Institute for Health and Care Excellence included guidelines for both MS and PD. The Appendix II identifies the duplicate information between published studies and organization websites, when it exists. Collectively, 25 resources were included in the final review. The extracted data from individual resources are provided in Appendix III.
Figure 1.
PRISMA flow chat
These resources were consolidated into general exercise guidelines for MS, stroke, and PD, and advanced exercise guidelines for MS and stroke. The expert panels did not aggregate advanced exercise guidelines for PD based on a lack of supporting evidence. The general, aerobic exercise prescriptions are appropriate for persons who are not currently undertaking an aerobic exercise program or who are irregularly/infrequently physically active. The advanced, aerobic exercise prescriptions are appropriate for persons who are regularly undertaking a chronic, aerobic exercise program (e.g., 6 or more months and meeting the general prescription above) and who seek greater benefits from aerobic exercise training. The general, resistance exercise prescriptions are appropriate for persons who are not currently undertaking a resistance exercise program or regularly engage in resistance/strength training.
Multiple Sclerosis
This rapid review of the literature and resources regarding exercise prescriptions in MS identified an opportunity for developing general and advanced guidelines for aerobic exercise training, and general guidelines for resistance exercise training. Among the resources on exercise guidelines for MS, six resources (n=6/13, 46%)18,19,21–23,37 explicitly reported severity of MS using a range of scores from the Expanded Disability Status Scale (EDSS).42 Of those, four studies described an EDSS range between 0 and 6.5 as mild to moderate. One resource22 interpreted an EDSS range between 0 and 8 as mild to moderate. Another37 interpreted moderate as an EDSS score of greater than or equal to 4. The remaining resources did not clearly specify the EDSS range for mild to moderate and rather used terms regarding functional status (e.g., high functioning MS, patients with little or no motor deficit).17,20,24 The exercise prescriptions identified for persons with mild to moderate MS (EDSS scores between 0 and 6.5) are provided in Table 1.
Table 1.
Recommended exercise prescriptions for adults with mild to moderate MS
| General aerobic exercise | Advanced aerobic exercise | General resistance exercise | |
|---|---|---|---|
| How often? | 2–3 days per week | 5 days per week | 2–3 days per week |
| How much? | Gradually increase the duration of exercise from 10–30 minutes over time. | The duration of the exercise bouts can approach 40 minutes. | The exercise bouts should range from 1– 3 sets between 8–15 repetitions of each exercise. Try to do 5–10 exercises. |
| How hard? | These activities should be performed at a moderate-intensity. Moderate-intensity of exercise is usually between 11 and 13 on the 20-point RPE scale. Alternative way of measuring moderate-intensity of exercise is 40–60% VO2peak or HRpeak |
Intensity of exercise can approach a 15 on the 20-point RPE scale. Alternative way of measuring intensity of exercise is 70% VO2peak or 80% HRpeak. |
Pick a resistance that you can finish 8–15 repetitions of the last set comfortably. |
| How to? | Some options for activity include: • Ergometry (arm, leg, or combined) • Walking (over-ground or treadmill) • Aquatics (including swimming) • Elliptical |
Some options for activity include: • Same as general guidelines • Running • Road cycling |
Resistance training activities mainly target major/large muscle groups: • Weight machines • Free weights • Elastic bands |
| Special Considerations | • Overall progression should start with either duration or frequency, and finally progress intensity per tolerability of the person. • Rest your muscles 2–4 minutes duration in between sets and muscle groups. • Rest your muscles for at least one day between strength training sessions. • Aerobic and resistance training can be performed on the same day as aerobic exercise training, depending on tolerability. • MS-specific symptoms (i.e., fatigue and heat sensitivity) should be identified and discussed before prescribing an exercise routine. |
||
RPE, rating of perceived exertion; VO2peak, peak oxygen consumption; HRpeak, peak heart rate
General, aerobic exercise prescription.
The frequency ranges between 2 and 3 days per week and should generally start with 2 days per week and progress toward 3 days per week over time. The duration of the exercise bouts ranges between 10 and 30 minutes and should gradually progress from 10 to 30 minutes over time. The intensity should be moderate and range between 11 and 13 on the 20-point rating of perceived exertion (RPE) scale, or between 40 and 60% peak oxygen consumption (VO2peak) or peak heart rate (HRpeak). The modality of exercise is listed in Table 1. The overall progression should start with increases in either duration or frequency. Progressions in intensity should be based on the tolerability of the individual with MS, only after duration and frequency are well tolerated.
Advanced, aerobic exercise prescription.
The frequency can approach 5 days per week; the duration of the exercise bouts can approach 40 minutes; the intensity can approach a 15 on the 20-point RPE scale, 70% VO2peak, or 80% HRpeak. The modality can include the same as the general guidelines but may be extended into running and road cycling. The overall progression should start with increases in either duration or frequency, followed by increases in intensity as tolerated by the individual.
General, resistance exercise prescription.
The frequency ranges between 2 and 3 days per week and should generally start with 2 days per week and progress toward 3 days per week over time. The exercise bouts should range from 1 to 3 sets between 8 to 15 repetition maximum (RM) and consist of 5 to 10 exercises. Resistance training should mainly focus on major/large muscle group, especially the lower extremities, and include those muscle groups that are the weakest and/or most functionally deficient. There should be adequate rest between sets/muscle groups of between 2 and 4 minutes. The modality of exercise is provided in Table 1. There should be a day of rest between resistance training sessions, but the sessions can be performed on the same day as aerobic exercise training, depending on tolerability.
Special considerations.
An exercise prescription for people with MS should promote a safe and individualized exercise regimen. Thus, before prescribing an exercise routine, MS-specific symptoms/characteristics (i.e., fatigue and heat sensitivity) should be identified and discussed,17–25 and the exercise prescription should include appropriate modifications. For example, individuals with high heat sensitivity should exercise in a cool environment, and a cooling fan should be readily available for the person during the exercise sessions. When individuals experience symptom exacerbation, either daily variation in symptoms or relapse, the exercise program may require modification or be temporarily discontinued until the symptoms are stable.14–16,19,25 Risk of falling should be considered for individuals with MS, and individuals with high risk of falls should perform both aerobic and strength exercises in a seated position (e.g., recumbent bike, weight machines) and under supervision.17–25
Stroke
This rapid review of the literature and resources regarding exercise prescriptions in stroke identified an opportunity for developing general and advanced guidelines for aerobic exercise training, and general guidelines for resistance exercise training. Among the resources on exercise guidelines for stroke, three resources (n=3/10, 30%)27,29,31 noted that the existing exercise recommendations for people post-stroke were mainly generated based on individuals with mild and moderate severity during subacute and chronic stages of recovery. The specific measure of severity of stroke was not provided from any of resources. The exercise prescriptions identified for mild to moderate stroke are provided in Table 2.
Table 2.
Recommended exercise prescriptions for adults with mild to moderate post-stroke
| General aerobic exercise | Advanced aerobic exercise | General resistance exercise | |
|---|---|---|---|
| How often? | 3–5 days per week | 5–7 days per week | 2–3 days per week |
| How much? | Gradually increase the duration of exercise from 20–40 minutes over time. The duration can be obtained through multiple 10-minute bouts across the day. |
The duration of the exercise bouts can approach 60 minutes. | The exercise bouts should range from 1–3 sets between 10–15 repetitions of each exercise. Try to do 8–10 exercises. |
| How hard? | These activities should be performed at a moderate-intensity. Moderate-intensity of exercise is usually between 12 and 13 on the 20-point RPE scale. Alternative way of measuring moderate-intensity of exercise is 40–59% HRR. |
Intensity of exercise can approach between 14 and 16 on the 20-point RPE scale. Alternative way of measuring intensity of exercise is 60–80% HRR. |
Pick a resistance between 30–50% and up to 50–80% of 1-RM. |
| How to? | Some options for activity include: • Ergometry (arm, leg, or combined) • Walking (over-ground or treadmill) • Aquatics (including swimming) • Recumbent stepping |
Some options for activity include: • Same as general guidelines • Elliptical |
Resistance training activities mainly target major/large muscle groups: • Weight machines • Free weights • Elastic bands |
| Special Considerations | • Overall progression should start with either duration or frequency, and finally progress intensity per tolerability of the person. • Rest your muscles 2–4 minutes duration in between sets and muscle groups. • Rest your muscles for at least one day between strength training sessions. • Aerobic and resistance training can be performed on the same day as aerobic exercise training, depending on tolerability. • Cardiovascular risk factors should be screened before prescribing an exercise routine. • Heart rate and blood pressure monitoring should be carried out. |
||
RPE, rating of perceived exertion; HRR, heart rate reserve; 1-RM, one-repetition maximum
General, aerobic exercise prescription.
The frequency ranges between 3 and 5 days per week and should generally start with 3 days per week and progress toward 5 days per week over time. The duration of the exercise bouts ranges between 20 and 40 minutes, with a gradual progression from 20 to 40 minutes as tolerated. If a duration of 20 to 40 minutes of continuous exercises cannot be achieved in a single bout, the duration can be obtained through multiple 10-minute bouts across the day. The intensity should be moderate and range between 12 and 13 on the 20-point RPE scale and 40 to 59% heart rate reserve (HRR). The modality of exercise is provided in Table 2. The overall progression should start with either duration or frequency, and finally progress intensity per tolerability of the person.
Advanced, aerobic exercise prescription.
The frequency ranges between 5 and 7 days per week; the duration of the exercise bouts can approach 60 minutes; the intensity can approach between 14 and 16 on the 20-point RPE scale and between 60 and 80% HRR. The modality can include the same as above in the general guidelines but may be extended into elliptical training. The overall progression should start with either duration or frequency, then finally progress intensity per tolerability of the person.
General, resistance exercise prescription.
The frequency ranges between 2 and 3 days per week and should generally start with 2 days per week and progress toward 3 days per week over time. At the early stages of the program, resistance training should target major muscle groups and include 8 to 10 exercises with 1 to 3 sets between 10 and 15 RM per exercise, performed at 30 to 50% one-repetition maximum (1-RM). At later stages, the training intensity can be set within 50 to 80% 1-RM as tolerated. The modality is listed in Table 2. There should be a day of rest between resistance training sessions, but the sessions can be performed on the same day as aerobic exercise training, depending on tolerability.
Special considerations.
An exercise prescription for people post-stroke should promote a safe and continuous exercise regimen. People post-stroke should undergo thorough screening for cardiovascular risk factors that may pose safety concerns. Ideally, heart rate monitoring should be undertaken and occasional blood pressure monitoring should be carried out.29,43 Regarding risk of falls or balance concerns, people post-stroke might perform both aerobic and strength exercises in seated position (e.g., recumbent bike, weight machines, and a body weight support system can be used in conjunction with the treadmill).26–31 With an emphasis on the benefit and volume of aerobic training, lifestyle physical activity is encouraged through short bouts of indoor/outdoor walking that might be complemented with activity monitors (e.g., pedometer, accelerometer) for motivating and self-managing behavior change among participants.27
Parkinson’s Disease
This rapid review of the literature and resources regarding exercise prescriptions in PD identified an opportunity for developing general guidelines for both aerobic exercise training and resistance exercise training. Among the resources on exercise guidelines for PD, three resources (n=3/10, 30%)33–35 clearly described the range of severity of PD in terms of the Hoehn and Yahr scale.44 The remaining resources14–16,32,39–41 did not provide a specific measure of severity. The exercise prescriptions identified for mild to moderate PD (Hoehn and Yahr scale 1–3), are provided in Table 3.
Table 3.
Recommended exercise prescriptions for adults with mild to moderate PD
| General aerobic exercise | General resistance exercise | |
|---|---|---|
| How often? | 3–5 days per week | 2–3 days per week |
| How much? | Gradually increase the duration of exercise from 20 to 60 minutes over time. | The exercise bouts should range from 1 to 3 sets of 8 to 12 repetitions of each exercise. |
| How hard? | These activities should be performed at a moderate-intensity. Moderate-intensity of exercise is usually 13 on the 20-point RPE scale. Alternative way of measuring moderate-intensity of exercise is 60–80% HRpeak or 40–60% HRR/VO2R. |
Pick a resistance between 40–50% and up to 60–80% of 1-RM. |
| How to? | Some options for activity include: • Ergometry (arm, leg, or combined) • Walking (over-ground or treadmill) • Aquatics (including swimming) |
Resistance training activities mainly target major/large muscle groups: • Weight machines • Free weights • Elastic bands |
| Special Considerations | • Overall progression should start with either duration or frequency, and finally progress intensity per tolerability of the person. • Rest your muscles 2–4 minutes duration in between sets and muscle groups. • Rest your muscles for at least one day between strength training sessions. • Aerobic and resistance training can be performed on the same day as aerobic exercise training, depending on tolerability. • The exercise training should be undertaken during medication cycles or in an “on” state. |
|
RPE, rating of perceived exertion; HRpeak, peak heart rate; HRR, heart rate reserve; VO2R, oxygen uptake reserve; 1-RM, one-repetition maximum
General, aerobic exercise prescription.
The frequency ranges between 3 and 5 days per week and should generally start with 3 days per week and progress toward 5 days per week over time. The duration of the exercise bouts ranges between 20 and 30 minutes, with an upward range of 60 minutes, and should gradually progress from 20 to 60 minutes over time. The intensity should be moderate with a target of 13 on the 20-point RPE scale, and range of between 60 and 80% HRpeak or 40 and 60% HRR/oxygen uptake reserve (VO2R). The modality of exercise is described in Table 3. The overall progression should start with either duration or frequency, and finally progress intensity per tolerability of the person.
General, resistance exercise prescription.
The frequency ranges between 2 and 3 days per week and should generally start with 2 days per week and progress toward 3 days per week over time. The exercise bouts should range between 1 and 3 sets of 8 to 12 repetitions, between 40 to 50% 1-RM and up to 60 to 80% 1-RM. Training should include 8 to 10 exercises per set targeting major/large muscle groups that are important for everyday function (e.g., walking or climbing steps). The modality of exercise is included in Table 3. There should be a day of rest between resistance training sessions, but the sessions can be performed on the same day as aerobic exercise training, depending on tolerability.
Special considerations.
An exercise prescription for people with PD should implement effective exercise regimen in a safe environment. The exercise training should be undertaken during medication cycles or in an “on” state. The exercise further should include visual and auditory cues that promote movement coordination. Supervised exercise training is recommended for safety. This is particularly good for individuals with high risk of falls and balance concerns, and persons with more advanced PD might perform all exercises in a seated position (e.g., recumbent bike, weight machines)32–35 or using body weight support during treadmill walking.
Discussion
This rapid review consolidated and harmonized the existing resources on prescriptive guidelines for exercise training among people with MS, stroke, and PD into a single, convenient resource for healthcare providers, fitness professionals, and researchers. This review provided a general exercise prescription for MS, stroke, and PD as a translational method of highest level of rehabilitation research into clinical practice. This review further provided advanced prescriptions of aerobic exercise for people with MS and post-stroke, who are currently undertaking regular exercise, but seek greater demand for promoting physiological adaptation. The exercise guidelines were identified and harmonized across peer-reviewed journals, book chapters, and organization websites. These resources were harmonized into general exercise prescription recommendations for MS, stroke, and PD, and advanced exercise prescriptions for MS and stroke. Further discussion was provided on the implications and applications of the resulting exercise prescriptions, as well as existing gaps in knowledge.
Multiple sclerosis.
Aerobic and strength exercise guidelines for people with mild to moderate MS were relatively consistent across the resources. This consistency may be associated with the wealth of evidence that has been generated in this population.9 Indeed, a recent scoping review of exercise literature reported that clinical trials of exercise and physical activity were most prevalent in MS compared with stroke and PD,4 and these studies are often the basis for generating exercise recommendations. The literature we summarized consistently indicated that moderate-intensity aerobic training should be performed 2 to 3 days per week in 10- to 40-minute bouts. By achieving these guidelines, people with MS can potentially improve their cardiovascular fitness, mobility and symptoms of fatigue and depression.21,22 This should be complemented by 2 to 3 days of weekly resistance training, from which anticipated benefits could include: improved strength, balance, mobility, performance of activities of daily living, and symptoms of fatigue.45
However, there was one inconsistency among the resources. Some resources recommended that aerobic exercise can be performed on the same day as resistance exercise,22 whereas others recommended aerobic and resistance training should be conducted on separate days.14,18,19,21,24,25 To that end, further research is required to explore whether combining or isolating aerobic and strength training is appropriate and necessary for individuals with MS and further elicits a difference in training adaptations and benefits.
Stroke.
The aerobic and strength exercise guidelines for people with mild to moderate stroke during the subacute and chronic phase were relatively consistent across the identified resources. People post-stroke should generally aim to achieve 10- to 40- minutes of moderate-intensity aerobic exercise, 3 to 5 days per week. These guidelines were relatively higher in frequency and duration compared to those reported for MS and PD, and likely represent the inverse relationship between aerobic training and the lowered risk of further cardiovascular events, such as a subsequent stroke, within this population.46 Other benefits from aerobic training include improved aerobic capacity, walking endurance, cognition, and reduced cardiovascular risk factors (e.g., blood pressure and cholesterol).28,47 With regard to resistance exercises, people post-stroke should train 2 to 3 days each week (1 to 3 sets of 8 to 10 repetitions, between 30–50% 1-RM) to increase muscular strength and reduce the energetic demand of daily activities.47–49 Of note, the panel observed that there were far fewer recommendations for strength training. This may be due to the previously questioned safety or detrimental effects (e.g., exacerbated spasticity) of resistance training within this population. However, current reports have demonstrated that there is no evidence to suggest resistance training is unsafe for this population, even within the early stages of post-rehabilitation discharge (3 months).50
Of note, the panel had one interesting observation regarding aerobic training in stroke. Some resources (n=4/8; 50%) recommended that aerobic training should be performed up to 5 days a week15,27–29 whereas others recommended a maximum of 7 days a week (n= 2/8; 25%).26,30 Earlier resources appeared to report the latter. As there has been a large growth in randomized controlled exercise trials in stroke over recent years,4 the expert panel’s decision was aligned with more current resources, which may have had a larger pool of evidence from which to recommend a lesser volume of 5 days per week of training.
Parkinson’s disease.
Based on the available resources, the exercise guidelines for people with mild to moderate PD should be 3 to 5 days of weekly moderate-intensity aerobic exercise performed between 20 to 30 minutes per bout. An additional 2 to 3 days of weekly resistance training were recommended with 1 to 3 sets of 8 to 12 repetitions, between 40 to 50% 1-RM and up to 60 to 80% 1-RM. Anticipated benefits may include reductions in tremor and bradykinesia51 enhanced balance, gait, and improved quality of life.7,52,53 However, PD seemingly had the least consistent recommendations for guiding aerobic and resistance exercise training.
Generalizability of the guidelines
The guidelines can only be generalized amongst a sub-population of MS, stroke, and PD, particularly those who have mild to moderate severity. Across the resources on exercise guidelines for MS, severity is mainly described using an EDSS and the ranges are relatively consistent. The expert panel decided that the consolidated guidelines are appropriate for people with mild to moderate MS, who may have a significant disease progression but still are ambulatory with constant bilateral assistance (i.e., EDSS ranges between 0 and 6.5).
None of the resources for stroke clearly defined a standard measure of severity, but generally agreed that the guidelines are appropriate for mild through moderate severity. If it is interpreted based on MS, this would imply persons who walk independently or walk with an assistive device.
The exercise guidelines for PD consistently indicated that these prescriptions are appropriate for people with mild to moderate PD based on Hoehn and Yahr scale scores. The expert panel agreed and defined that our consolidated exercise guidelines are appropriate for people with mild to moderate PD, who are classified as having Hoehn and Yahr scale scores between 1 and 3.
Notable Trends
There are two trends identified from our expert panel regarding exercise recommendations for people with MS, post-stroke, and PD: 1) overlap and uniqueness in exercise recommendations between disease types; and 2) recommendations of high intensity interval training (HIIT) across the diseases. The expert panel noted that the exercise prescriptions for MS, stroke, and PD seemingly overlapped in many aspects. For example, exercise guidelines for both MS and PD recommended 2 to 3 days of weekly aerobic training. Across all groups, moderate intensity aerobic exercise was recommended in conjunction with 2 to 3 days of weekly resistance training. These similarities between the exercise prescriptions across the groups appear to be influenced by the similar consequences of MS, stroke, and PD (i.e., mobility disability) and the needs of participant populations. Despite the similarities in exercise recommendations across the groups, specific exercise recommendations were provided, as these highlight the uniqueness of prescriptions for MS, stroke, and PD. For example, aerobic training recommendations for people post-stroke emphasize substantially higher frequency and longer duration compared with the other groups with importance of cardiorespiratory health. MS, stroke, and PD further have unique characteristics (as described in the special consideration section) (e.g., fatigue/heat sensitivity for MS, medication ‘on/off’ timing for PD) that should be considered when designing/prescribing exercise programs to maximize the benefits and ensure the safety of participants.
The expert panel noted a recent trend for recommendation of HIIT among people with MS and post-stroke. Indeed, two resources suggested one weekly session of high intensity training up to 90% of VO2peak can be prescribed for people with MS.19,21 This was supported by a recent systematic review that demonstrated HIIT was a safe and effective means for increasing fitness in people with higher functioning MS.54 Regarding people with stable, chronic stroke, one resource acknowledged that HIIT can elicit greater training effects and should be performed when safe and well tolerated.28 Benefits from HIIT for people post-stroke may include improved functional, cardiovascular, and neuroplastic outcomes.55–57 This recommendation was not observed within the resultant PD exercise resources, and may reflect a less mature knowledge base.
Study Limitations
This review had some limitations. These guidelines may not be suitable for people with more severe mobility impairments, as this was a limitation of the reviewed sources and a limitation of the exercise trials themselves. The existing recommendations in the literature and on organization websites were not tailored based on the severity of the disease or an individual’s physiological or psychological profile. Future studies are warranted that consider providing precise exercise recommendations based on individual level characteristics, such as behavioral factors and preferences.
Conclusions
This is the first paper to harmonize the existing exercise guidelines for people with MS, stroke, and PD. The guidelines provide clinicians and exercise professionals with greater clarity in prescribing specific exercise programs among patients/clients with MS, stroke, and PD. The consolidation of the existing guidelines into a single convenient resource might facilitate easy translation of knowledge into practice for practitioners, and this is important for possibly addressing the high rate of physical inactivity in MS, stroke, and PD. The guidelines further serve as a foundation for conducting future research on identifying if the exercise prescriptions optimize outcomes within in these populations. Overall, the guidelines should advance the prescription of exercise training in MS, stroke, and PD.
Supplementary Material
Acknowledgments
FUNDING
The contents of this publication were developed under a grant, RERC RecTech from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90REGE0002). The NIDILRR is a Center within the Administration for Community Living, Department of Health and Human Services. The contents of this manuscript do not necessarily represent the policy of these groups and you should not assume endorsement by the U.S. Federal Government.
Footnotes
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
- 1.National Multiple Sclerosis Society. MS prevalence. 2017; https://www.nationalmssociety.org/About-the-Society/MS-Prevalence.
- 2.Benjamin EJ, Virani SS, Callaway CW, et al. : Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:67–492. [DOI] [PubMed] [Google Scholar]
- 3.Marras C, Beck J, Bower J, et al. : Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018;4:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai B, Young H-J, Bickel CS, et al. : Current trends in exercise intervention research, technology, and behavioral change strategies for people with disabilities: a scoping review. Am J Phys Med Rehabil. 2017;96:748–61. [DOI] [PubMed] [Google Scholar]
- 5.Rietberg MB, Brooks D, Uitdehaag BM, et al. : Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;25:CD003980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2016;3:CD003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehrholz J, Kugler J, Storch A, et al. : Treadmill training for patients with Parkinson’s disease. Cochrane Database Syst Rev. 2015:1:CD0007830. [DOI] [PubMed] [Google Scholar]
- 8.Motl RW, Pilutti LA: The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8:487–97. [DOI] [PubMed] [Google Scholar]
- 9.Motl RW, Sandroff BM, Kwakkel G, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16:848–56. [DOI] [PubMed] [Google Scholar]
- 10.Motl RW, Barstow EA, Blaylock S, et al. : Promotion of Exercise in Multiple Sclerosis Through Health Care Providers. Exerc Sport Sci Rev. 2018;46:105–11. [DOI] [PubMed] [Google Scholar]
- 11.Sudsawad P: Knowledge translation: introduction to models, strategies and measures Vol 4: Southwest Educational Development Laboratory, National Center for the Dissemination of Disability Research; Austin, TX; 2007. [Google Scholar]
- 12.Motl RW, Learmonth YC, Pilutti LA, et al. : Top 10 research questions related to physical activity and multiple sclerosis. Res Q Exerc Sport. 2015;86:117–29. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. : Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. [DOI] [PubMed] [Google Scholar]
- 14.Myers J, Herbert WG, Humphrey RH. ACSM’s resources for clinical exercise physiology: musculoskeletal, neuromuscular, neoplastic, immunologic, and hematologic conditions. Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 15.Durstine JL, Moore G, Painter P, et al. : ACSM’s Exercise Management for Persons With Chronic Diseases and Disabilities. Champaign, IL: Human Kinetics; 2009. [Google Scholar]
- 16.Riebe D, Ehrman JK, Liguori G, et al. : ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 17.Brown TR, Kraft GH: Exercise and rehabilitation for individuals with multiple sclerosis. Phys Med Rehabil Clin N Am. 2005;16:513–55. [DOI] [PubMed] [Google Scholar]
- 18.Dalgas U, Ingemann-Hansen T, Stenager E: Physical Exercise and MS Recommendations. Int MS J. 2009;16:5–11. [PubMed] [Google Scholar]
- 19.Dalgas U, Stenager E, Ingemann-Hansen T: Multiple sclerosis and physical exercise: recommendations for the application of resistance-, endurance- and combined training. Mult Scler. 2008;14:35–53. [DOI] [PubMed] [Google Scholar]
- 20.Petajan JH, White AT: Recommendations for physical activity in patients with multiple sclerosis. Sports Med. 1999;27:179–91. [DOI] [PubMed] [Google Scholar]
- 21.Halabchi F, Alizadeh Z, Sahraian MA, et al. : Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017;17:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. : Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–28. [DOI] [PubMed] [Google Scholar]
- 23.Sandoval AE: Exercise in multiple sclerosis. Phys Med Rehabil Clin N Am. 2013;24:605–18. [DOI] [PubMed] [Google Scholar]
- 24.White LJ, Dressendorfer RH: Exercise and multiple sclerosis. Sports Med. 2004;34:1077–100. [DOI] [PubMed] [Google Scholar]
- 25.Ronai P, LaFontain T, Bollinger L: Exercise guidelines for persons with multiple sclerosis. Strength Conditioning J. 2011;33:30–3. [Google Scholar]
- 26.Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors. Circulation. 2004;109:2031–41. [DOI] [PubMed] [Google Scholar]
- 27.Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors. Stroke. 2014;45:2532–53. [DOI] [PubMed] [Google Scholar]
- 28.Billinger SA, Boyne P, Coughenour E, et al. : Does aerobic exercise and the FITT principle fit into stroke recovery? Curr Neurol Neurosci Rep. 2015;15:519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pang MY, Charlesworth SA, Lau RW, et al. : Using aerobic exercise to improve health outcomes and quality of life in stroke: evidence-based exercise prescription recommendations. Cerebrovasc Dis. 2013;35:7–22. [DOI] [PubMed] [Google Scholar]
- 30.Lindsay P, Bayley M, Hellings C, et al. : Canadian best practice recommendations for stroke care (updated 2008). CMAJ. 2008;179:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hebert D, Lindsay MP, McIntyre A, et al. : Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11:459–84. [DOI] [PubMed] [Google Scholar]
- 32.Olanow CW, Watts RL, Koller WC: An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology. 2001;56:1–88. [DOI] [PubMed] [Google Scholar]
- 33.McGraw SM, Hoover DL, Shirey MP: Exercise guidelines for patients with Parkinson’s disease: An overview for the home health care professional. Home Health Care Manag Pract. 2014;26:167–74. [Google Scholar]
- 34.Gallo PM, Garber CE: Parkinson’s disease: a comprehensive approach to exercise prescription for the health fitness professional. ACSM’s Health Fitness J. 2011;15:8–17. [Google Scholar]
- 35.Salgado S, Williams N, Kotian R, et al. : An evidence-based exercise regimen for patients with mild to moderate Parkinson’s disease. Brain Sci. 2013;3:87–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Physical Therapy Association. Patient education fact sheets: multiple sclerosis and exercise; http://www.neuropt.org/special-interest-groups/degenerative-diseases/patient-education-fact-sheets.
- 37.National Institute for Health and Care Excellence. Multiple sclerosis in adults: management 2014; https://www.nice.org.uk/guidance/CG186/chapter/1-Recommendations#ms-symptom-management-and-rehabilitation-2.
- 38.National Clinical Guideline Centre UK. Stroke rehabilitation in adults. 2013; https://www.nice.org.uk/guidance/cg162.
- 39.American Physical Therapy Association: Patient education fact sheets: Parkinson’s disease and exercise; http://www.neuropt.org/special-interest-groups/degenerative-diseases/patient-education-fact-sheets.
- 40.American Parkinson Disease Association. Be Active & Beyond - A guide to exercise and wellness for people with parkinson’s disease. 2018; https://www.apdaparkinson.org/uploads/files/Be-Active-Book_For-Web-90o.pdf
- 41.Davis Phinney Foundation for Parkinson’s. Exercise. 2018; https://www.davisphinneyfoundation.org/living-well/exercise/
- 42.Kurtzke JF: Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444. [DOI] [PubMed] [Google Scholar]
- 43.MacKay-Lyons MJ, Macko R, et al. : Cardiovascular fitness and adaptations to aerobic training after stroke. Physiotherapy Canada. 2006;58:103–13. [Google Scholar]
- 44.Hoehn MM, Yahr MD: Parkinsonism: Onset, progression and mortality. Neurology. 2001. [PubMed] [Google Scholar]
- 45.Kjolhede T, Vissing K, de Place L, et al. : Neuromuscular adaptations to long-term progressive resistance training translates to improved functional capacity for people with multiple sclerosis and is maintained at follow-up. Mult Scler. 2015;21:599–611. [DOI] [PubMed] [Google Scholar]
- 46.Chaturvedi S, Nahab F: Exercise for stroke prevention. Neurology. 2017;88:342. [DOI] [PubMed] [Google Scholar]
- 47.Han P, Zhang W, Kang L, et al. : Clinical Evidence of Exercise Benefits for Stroke. Adv Exp Med Biol; 2017:1000:131–51. [DOI] [PubMed] [Google Scholar]
- 48.Williams MA, Haskell WL, Ades PA, et al. : Resistance exercise in individuals with and without cardiovascular disease: 2007 update. Circulation. 2007;116:572–84. [DOI] [PubMed] [Google Scholar]
- 49.Pollock ML, Franklin BA, Balady GJ, et al. : Resistance exercise in individuals with and without cardiovascular disease. Circulation. 2000;101:828–33. [DOI] [PubMed] [Google Scholar]
- 50.Salter K, Musovic A: In the first 3 months after stroke is progressive resistance training safe and does it improve activity? A systematic review. Top Stroke Rehabil. 2016;23:366–75. [DOI] [PubMed] [Google Scholar]
- 51.Ridgel AL, Peacock CA, Fickes EJ, et al. : Active-assisted cycling improves tremor and bradykinesia in Parkinson’s disease. Arch Phys Med Rehabil. 2012;93:2049–54. [DOI] [PubMed] [Google Scholar]
- 52.Herman T, Giladi N, Gruendlinger L, et al. : Six weeks of intensive treadmill training improves gait and quality of life in patients with Parkinson’s disease: a pilot study. Arch Phys Med Rehabil. 2007;88:1154–8. [DOI] [PubMed] [Google Scholar]
- 53.Cakit BD, Saracoglu M, Genc H, et al. : The effects of incremental speed-dependent treadmill training on postural instability and fear of falling in Parkinson’s disease. Clin Rehabil. 2007;21:698–705. [DOI] [PubMed] [Google Scholar]
- 54.Campbell E, Coulter EH, Paul L: High intensity interval training for people with Multiple Sclerosis: a systematic review. Mult Scler Relat Disord. 2018;24:55–63. [DOI] [PubMed] [Google Scholar]
- 55.Crozier J, Roig M, Eng JJ, et al. High-Intensity Interval Training After Stroke: An Opportunity to Promote Functional Recovery, Cardiovascular Health, and Neuroplasticity. Neurorehabil Neural Repair. 2018;32:543–56. [DOI] [PubMed] [Google Scholar]
- 56.Outermans JC, van Peppen RPS, Wittink H, et al. : Effects of a high-intensity task-oriented training on gait performance early after stroke: A pilot study. Clin Rehabil. 2010;24:979–87. [DOI] [PubMed] [Google Scholar]
- 57.Rose D, Paris T, Crews E, et al. : Feasibility and effectiveness of circuit training in acute stroke rehabilitation. Neurorehabil Neural Repair. 2011;25:140–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.