1. Introduction
Temporomandibular disorders (TMDs) are a heterogeneous group of orofacial pain and non-pain conditions. Approximately 5–12% of the adult U.S population suffers from painful TMD [26; 34]. There are many factors that contribute to TMD. Major risk factors such as psychological states and pain sensitivity are thought to be associated with acute TMD pain through mechanisms related to central nervous system pain processing [10; 15]. Injury is an obvious peripheral mechanism for the development of the symptom of pain. However, that obvious mechanism leading to nociceptive pain does not explain subsequent development of a pain disorder, such as TMD. In fact, injury often has a poor correlation with clinical pain disorders [49]. One reason is that pain may persist beyond the healing of the evidential damaged tissues due to other factors, which makes persistent pain disorders, such as TMD, not only multifactorial but also complex in nature [36; 49].
Most epidemiological studies that have reported an association between jaw injury and TMD are cross-sectional in design, limiting causal inference about the role of jaw injury in TMD [5; 6; 12; 16; 21; 48]. Prospective studies have shown a positive association between injury and incident TMD in participants recruited from emergency departments [5; 17; 24; 41; 42]. However, injury severity may influence who seeks emergency care as well as willingness to participate in a study, threatening internal validity due to potential selection bias. Recruitment from settings such as dental offices may focus on injuries typically treated by a dentist, such as tooth injury [18; 32; 39; 40], and not include head and neck injuries that may affect the jaw and which are more likely to present at physician offices or emergency departments. Moreover, an individual may have multiple injuries, and these may be underreported. The above situations may lend to systematically undercounting injury types. A study designed to assess incident injury and possible post-injury TMD would reduce problems related to selection bias and temporality.
The current study uses data from the OPPERA (Orofacial Pain: Prospective Evaluation and Risk Assessment) study, which we believe makes it the first to prospectively assess the association between new onset injury exposure and the incidence of first-onset TMD. In addition, the data permits exploration of the association between the type of jaw injury (intrinsic, extrinsic) and the risk of incident TMD in adults. The OPPERA study continued follow-up after the first jaw injury, providing an opportunity to explore whether the risk of TMD is influenced by the number of injuries.
2. Methods
2.1. Study Participants
OPPERA is a prospective study focusing on risk factors for incident TMD in adults. Of the 5,781 individuals who were initially screened, 2,523 individuals were excluded due to incomplete telephone screening interview (n=308), not willing to participate (n=166), traumatic injury or surgery to the face or jaw within 6 months preceding screening (n=602), receiving oral surgical, orthodontic treatment or splints (n=105), pregnant, nursing, or any significant medical conditions (n=67), <18 or >44 years of age or not living within the area (n=196), failure to attend the baseline clinical examination (n=785), or history of chronic TMD (n=92). Following these exclusions, 3,258 individuals with no history of TMD, aged 18–44 years, were enrolled at four clinical study sites within the U.S. from 2006 through 2008 [3]. Details about recruitment and eligibility are described elsewhere [45].
The institutional review boards at all participating institutions approved the study protocols and procedures and participants provided signed consent. Participants completed questionnaires on demographics, psychosocial behaviors, general health, and history of jaw injury and prior history of TMD. Participants attended a study research clinic for clinical assessments including examination by calibrated examiners trained on the Research Diagnostic Criteria protocol for clinical examination of TMD (RDC/TMD) [8]. The examiners confirmed the absence of existing TMD at enrollment using the following 2 criteria: 1) ≤4 days of pain in the prior month in the examiner-identified orofacial regions and 2) absence of a clinical RDC/TMD diagnosis of both myalgia and arthralgia [45].
At quarterly intervals after the enrollment visit, participants were sent quarterly health update questionnaires (QHUs), either by mail or online. QHUs were used to assess incident jaw injury (the study exposure). QHUs also asked about pain symptoms, the presence of which would identify individuals for further evaluation for presence of TMD (the study outcome). Depending on the date of enrollment, participants could complete quarterly updates for up to 5 years.
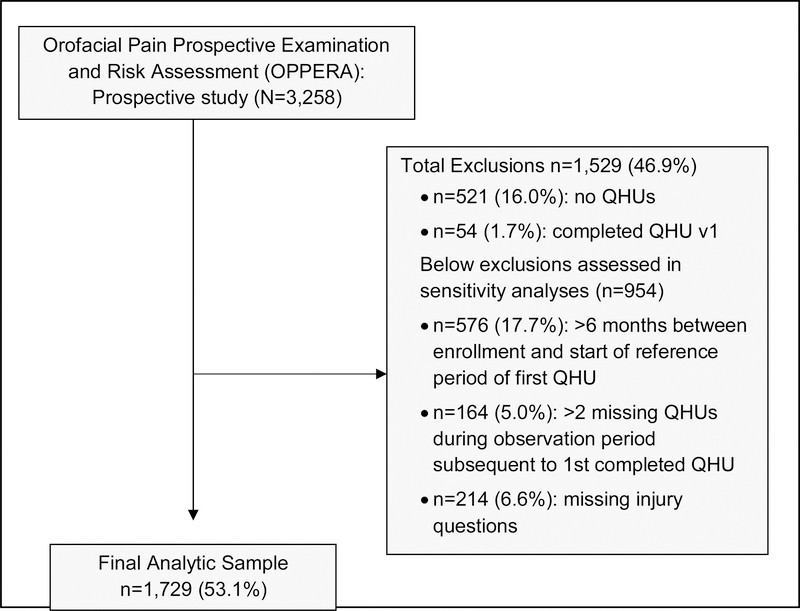
For the purpose of this analysis, participants with the following missing data were excluded: 1) complete loss to follow-up (n=521 individuals who completed no QHUs); 2) completed only the initial version of the QHU that did not contain the complete set of injury questions needed for this analysis (n=54); 3) had more than 6 months gap from enrollment until they began to provide information via QHU (n=576); 4) had more than two missing QHUs during the observation period following the completion of their first QHU (n=164); and 5) missing or mis-reporting of jaw injury questions (n=214). Individuals with many missing QHUs (more than 2 missing QHUs before and after first QHU completion) were excluded on the assumption that they would contribute uninformative time to follow-up, which could bias the true association. The final analytic sample for this analysis included 1,729 (53.1% of 3,258) individuals that had minimal missing QHUs (see Figure 1).
Figure 1.
Flowchart of participants.
2.2. Measures
2.2.1. Exposure Assessment
First jaw injury
During the possible 5-year observation period from enrollment, participants were queried at each QHU (i.e., every 3 months) whether they had experienced extrinsic events such as tooth extraction or dental treatments, oral intubation, sports injury (including falls, bumps and blows), motor vehicle accidents, accidents resulting in whiplash, and injuries to the shoulder, neck and head region. The participant was then asked whether any of these extrinsic events had caused injury to the jaw. Data were also collected on intrinsic injuries which included jaw injury attributed to yawning or prolonged mouth opening. In order to assess the association between jaw injury and the risk of clinically diagnosed TMD, we addressed the complex analysis requirements related to multiple injuries by using the first jaw injury as the time-dependent exposure of interest. “First jaw injury” was operationalized as the first positive report of any jaw injury, of either extrinsic or intrinsic type, on any QHU during the observation period.
Type of jaw injury
First jaw injury was classified as either extrinsic or intrinsic injury based on the QHU. Individuals whose first jaw injury report included any one of the extrinsic events as described above were grouped into the extrinsic injury types, those whose first jaw injury included any of the intrinsic events as described above were grouped into the intrinsic injury types, and those whose first jaw injury included both extrinsic and intrinsic events were grouped into the “both” injury type.
Number of jaw injuries
Individuals who reported jaw injury of any type in only one QHU during the observation period were grouped into the one jaw injury category. Individuals who reported a jaw injury of any type in any QHUs subsequent to a first jaw injury were grouped into the two or more jaw injuries category.
2.2.2. Confounder Assessment
Potential confounders were measured once, at the enrollment visit and were selected for these analyses based on potential roles with the exposure and outcome. They included demographic variables such as study site, age, education (some college education or less, and college graduate or more), annual household income (<40,000 USD, ≥40,000 USD, and not stated), marital status (married or living as married, divorced, separated or widowed, and never married), and satisfaction with material standards of life and satisfaction with financial situation (each converted to tertiles of low, medium and high). Health insurance and U.S lifetime residency variables were dichotomized as yes or no. Psychological characteristics, collected at baseline, included depression and anxiety (Symptom Check List-90 revised (SCL-90-R)) [7], mood states (The Profile of Mood States-Bipolar (PMOS-Bi)) [27], physical symptoms (Comprehensive Pain and Symptom Questionnaire (CPSQ)) [37], and coping (CPQ-R) [38], and each were parameterized in their continuous form. Smoking was categorized as never smoked (less than 100 cigarettes in a lifetime), former smokers, and current smokers. Clinical measures from the baseline assessment included prior injury, prior pain, pain on jaw opening, and pain on palpation [37], each recorded as yes or no. Overuse jaw behaviors assessed from the Oral Behavior Checklist (OBC) summary score [29] were considered as a continuous measure.
2.2.3. Ascertainment of TMD cases
Quarterly Health Update questionnaires were also used to determine whether participants had experienced facial pain symptoms suggestive of TMD. From the QHU responses, significant pain symptoms (pain density) was characterized according to a pre-defined algorithm, which was comprised of three questions that assessed location and frequency of pain during the prior three-month period. Specifically, these questions queried about presence or absence of facial pain, the number of months (0–3) with at least 5 consecutive days of pain per month, and the number of days of pain in the last two weeks. The criteria for sufficient pain density for referral for study-specific clinical examination were met by either: 1) ≥5 consecutive days of orofacial pain per month for ≥2 months, and with ≥1 day of orofacial pain in the 2 weeks preceding questionnaire completion, or 2) ≥5 consecutive days of orofacial pain in the month preceding questionnaire completion, and with ≥5 days of orofacial pain in the 2 weeks preceding questionnaire completion. If a participant reported sufficient pain density, he or she was then scheduled for a clinic visit to be examined by a trained and calibrated examiner for ascertainment of first-onset of TMD [3; 8]. The test-retest reliability of the QHU status (sufficient pain density) administered at an interval of 4–8 days for 105 participants was excellent (ICC=0.83). Based on the clinical examination as the reference standard, the validity of the QHU pain screening items for identification of putative cases was as follows: the PPV=39.7%, NPV=94.4%, sensitivity=90.4% and specificity=54.1% [3]. The threshold for detection of positive symptoms with the QHU was intentionally set to be inclusive of symptomatic individuals for whom examination would exclude false positives from the QHU.
If a participant was clinically confirmed to have painful TMD using the RDC/TMD protocol and modified RDC/TMD criteria (i.e., more stringent for diagnosis, compared to the RDC/TMD, for myalgia), the participant was then considered an incident TMD case. The RDC/TMD clinical examination protocol assesses regional pain in the past 30 days, pain on palpation, and pain from jaw mobility of the masticatory muscles and/or jaw joints. Participants were classified either as myalgia (three or more of the eight muscles were positive for pain), or arthralgia (if either or both jaw joints were positive for pain). Individuals with myalgia, arthralgia, or both were considered a TMD case [3; 8]. Individuals with sufficient pain density but who did not come for a clinic visit and were not clinically examined for having TMD were considered to be non-cases. However, these individuals classified as non-cases could potentially be TMD cases who were not ascertained as they did not follow through with the clinic examination despite their positive symptoms report and could therefore potentially bias the measure of association between injury and TMD. Therefore, these individuals were assessed in a sensitivity analysis to understand the degree to which the estimate of association between injury and TMD was affected by a potential outcome misclassification, described further below.
2.3. Statistical Analysis
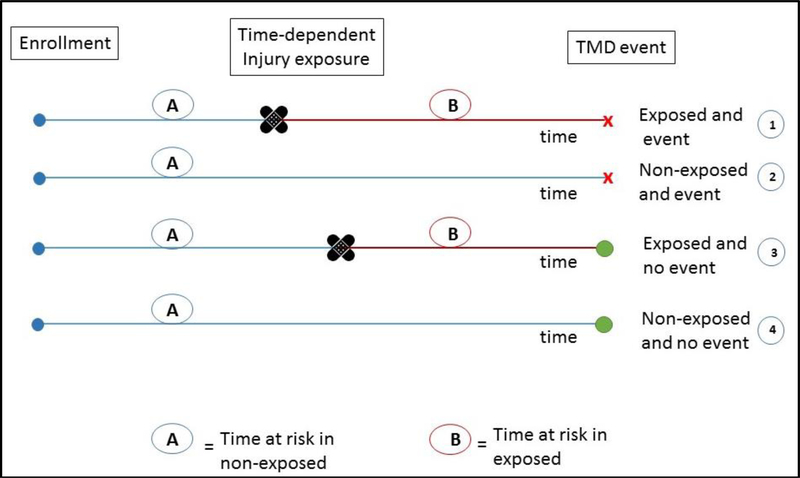
For descriptive purposes, participants with incident TMD and those without TMD were compared with respect to baseline characteristics using chi-square test or Fisher’s exact test for categorical variables in the full sample of 1,729 individuals. Independent t-test or Wilcoxon test were used to evaluate differences for continuous variables. Similarly, injured and non-injured participants were also compared on baseline characteristics. Annualized rates of TMD were calculated for both the injured and non-injured participant groups. Since participants were repeatedly assessed for jaw injury at every three-monthly QHU post-enrollment, jaw injury was treated as a time-dependent variable in a Cox model where the outcome variable is first-onset TMD. Figure 2 provides a visual description of the analytic design of the study. To estimate the associations between jaw injury and development of first-onset incident TMD Hazard Ratios (HR) and 95% Confidence Intervals (CI) were calculated for the unadjusted and the multivariable adjusted Cox regression models in a sample of 1,613 individuals that had complete information for all covariates included in the multivariable models. The ratio of two hazards, each of which represents the risk of developing TMD within a hypothetical time period that approaches zero, provides a good approximation of the incidence rate ratio. Hereafter we use the term “hazard” to characterize the general concept of risk for developing TMD within any fixed time period.
Figure 2.
Schematic showing time-dependent first jaw injury and first onset TMD within the OPPERA study design.
① Individuals exposed to first injury and develop first-onset painful TMD, contribute to time at risk in the non-exposed group and to time at risk in the exposed group.
② Individuals not exposed to injury and develop first-onset painful TMD, contribute to time at risk in the non-exposed group.
③ Individuals exposed to first injury and do not develop first-onset painful TMD, contribute to time at risk in the non-exposed group and to time at risk in the exposed group.
④ Individuals not exposed to injury and do not develop first-onset painful TMD, contribute to time at risk in the non-exposed group.
Potential confounding variables were evaluated in multivariable models based on their associations with injury and TMD, as well as biologic plausibility. Hazard ratios (95% Confidence Intervals) between first injury and incident TMD after adjusting for each covariate separately are provided in supplemental table 2s. Potential confounders were considered if their addition to the base (i.e., unadjusted) model (model-1) changed the HR by a nominal threshold of ≥10%. Although arbitrary, this threshold has precedents in the epidemiologic literature [25; 28; 31] because it represents a degree of confounding that could meaningfully alter interpretations concerning the influence of the predictor variable on the outcome. In order to explore for effect modification, categorical predictors measured at baseline (education, income, health insurance, marital status, satisfaction with material and financial status and smoking) were assessed for whether the stratum specific HR estimates were significantly different from each other. For continuous measures, the p-value for interaction was assessed by adding the cross-product term between the continuous predictor and injury to the model. All tests for effect modification were conducted at alpha=0.1 in order to reduce probability of type II error and find a true interaction if one exists. For model-2, we also included study site, because OPPERA is a multi-site study and site-specific variation is expected. Likewise, age, gender and race were used in model-2 to be consistent with the approach used in other OPPERA study findings. Estimates were also computed from a fully adjusted model (model-3) that included, in addition to the variables in model-2, clinically relevant covariates of depression, anxiety, physical symptoms, positive and negative mood, coping, oral behaviors, prior pain, financial and material satisfaction, and smoking.
In order to compare whether hazard of TMD differs by type of injuries, we used the Woolf test, a type of Wald test that compares the HR from two different sub-groups. The Woolf test was also used to determine whether the HR for TMD significantly differed in those who reported one injury compared to those reporting two or more injuries. A two-sided p-value of 0.05 was used to evaluate statistical significance for all tests other than the interaction analysis (alpha=0.1). All data analysis was performed using SAS 9.4 (SAS Institute, Cary, N.C.).
2.3.1. Sensitivity analysis
Three types of sensitivity analyses were undertaken to evaluate potential bias associated with errors in ascertainment of TMD, missing QHUs, and missing injury information on available QHUs. The first type of sensitivity analysis assessed potential biases due to errors in ascertainment of TMD incidence in relation to a non-examined participant with a positive QHU within the n=1,729 analytical sample. Bair et al. previously described a multiple imputation procedure in which the estimated parameter of examiner-verifier TMD, based on baseline predictors, was applied to participants with positive QHUs who were not followed by an examination [3]. The same imputation procedure for case classification was conducted here, but it was restricted to our analytical sample of n=1,729, replicated 100 times, and combined with data on injury. A summary HR and 95% CI of the association between injury and incident TMD were estimated by combining the 100 sets using the “mianalyze” procedure in SAS as described previously by Bair et al. (2013).
The second type of sensitivity analysis assessed potential biases due to missing QHUs within the n=1,729 analytical sample: 32.9% had missing QHUs before the first available QHU due to delay in the study procedures and 21.7% had missing QHUs after the first available QHU during the remaining observation period. Within our sample of 1,729 individuals, 25% reported an injury, which corresponded to 5% of 18,049 QHUs. Consequently, sensitivity analysis was carried out whereby positive injury report was randomly assigned to 5% of the missing QHUs and missing injury reports. In order to address possible under-reporting of injury episodes, the assignment proportion was doubled to 10% of the missing QHUs and missing injury reports in order to create an upper bound of the estimate. Following 100 imputation replications, the HR and 95%CI were computed using the Cox time-dependent regression model.
The third type of sensitivity analysis assessed potential biases due to exclusion of individuals with excessively missing QHUs. There were 1,729 OPPERA enrollees included in the complete-case dataset used for the primary analysis (Figure 1). Excluded were 954 individuals who provided only partial follow-up information about injury using the same injury questionnaire completed by subjects in the complete-case dataset, 521 who provided no follow-up data and 54 individuals who completed an earlier version of the injury questionnaire. Partial data from the largest of those excluded groups was used for the imputation procedures described above, producing hazard ratios and 95% CIs were for the n=2,683 subjects used in sensitivity analysis.
3. Results
3.1. Participant Characteristics at enrollment
Compared to participants who did not develop TMD, participants who developed TMD were more likely to be African-American, older (mean=29.1 years), lifetime U.S. residents, divorced, separated or widowed, with some college education or less, current smokers, and less satisfied with material and financial standards in life (all p<0.05). Incident TMD cases also reported prior pain, pain from palpation in the neck and body, somatic symptoms, more jaw overuse behaviors, higher depression, anxiety, and negative moods states at baseline (all p<0.01), compared to non-cases (Table 1). This Table 1, based on subject compliance with QHUs, comes to the same conclusions as the previously published table 1, which included everyone, in the OPPERA Act II publications [10; 35; 46]. We further compared baseline characteristics by jaw injury (Supplemental table 1s). Compared to non-injured participants, injured participants were more likely to be African-American, older, divorced, separated or widowed and with some college education or less (all p<0.01). Injured participants were also more likely to be current smokers, less satisfied with material standards in life, with no health insurance and reported facial pain prior to enrollment. They also had more depression, anxiety, and negative moods states (all p<0.01) (Table 1s). In summary, the predictors for incident TMD and for incident injury overlapped substantially.
Table 1.
Characteristics of Participants by TMD Incidence (n=1,729).
| TMD Incidence | |||
|---|---|---|---|
| Characteristic | Yes (n=175) | No (n=1,554) | p-value* |
| n (%) | |||
| Study site | |||
| Chapel Hill, NC | 20 (11.4) | 413 (26.6) | <0.01 |
| Buffalo, NY | 45 (25.7) | 384 (24.7) | |
| Gainesville, FL | 67 (38.3) | 424 (27.3) | |
| Baltimore, MD | 43 (24.6) | 333 (21.4) | |
| Gender | |||
| Males | 61 (34.9) | 621 (39.9) | 0.20 |
| Females | 114 (65.1) | 933 (60.0) | |
| Race | |||
| White | 92 (52.6) | 841 (54.1) | <0.01 |
| Black/African American | 61 (34.8) | 398 (25.6) | |
| Other | 22(12.6) | 315 (20.3) | |
| Life time residency in U.S | |||
| Yes | 161 (92.5) | 1,257 (82.5) | <0.01 |
| No | 13 (7.5) | 266 (17.5) | |
| Missing | 1 | 31 | |
| Education | |||
| Some college or less | 112 (65.5) | 822 (53.9) | <0.01 |
| College graduate or more | 59 (34.5) | 704 (46.1) | |
| Missing | 4 | 28 | |
| Family annual household Income | |||
| <40,000 USD | 71 (50.4) | 499 (41.6) | 0.07 |
| ≥40,000 USD | 70 (49.7) | 700 (58.4) | |
| Not Stated | 34 | 355 | |
| Covered by health insurance | |||
| Yes | 143 (84.6) | 1,256 (83.8) | 0.80 |
| No | 26 (15.4) | 243 (16.2) | |
| Missing | 6 | 55 | |
| Rating of satisfaction financial situation | |||
| Low (0–3) | 65 (37.8) | 431 (28.2) | 0.03 |
| Mid (4–6) | 62 (36.1) | 606 (39.7) | |
| High (7–10) | 45 (26.2) | 490 (32.1) | |
| Missing | 3 | 27 | |
| Rating of satisfaction material situation | |||
| Low (0–5) | 60 (35.1) | 392 (25.7) | <0.01 |
| Mid (6–8) | 84 (49.1) | 701 (46.0) | |
| High (9–10) | 27 (15.8) | 430 (28.2) | |
| Missing | 4 | 31 | |
| Marital Status | |||
| Married/ Living as married | 35 (20.0) | 294 (19.2) | 0.02 |
| Divorced/ Separated/ Widowed | 23 (13.1) | 105 (6.8) | |
| Never Married | 116 (66.3) | 1,126 (73.4) | |
| Refused to state | 1 (0.6) | 10 (0.7) | |
| Missing | 0 | 19 | |
| Smoking | |||
| Current | 35 (20.8) | 212 (13.9) | <0.01 |
| Former | 25 (14.9) | 114 (7.5) | |
| Never | 108 (64.3) | 1,201 (78.7) | |
| Missing | 7 | 27 | |
| Injury/event prior to 6 mo before enrollment | |||
| Yes | 14 (9.0) | 107 (7.3) | 0.40 |
| No | 141 (91.0) | 1,359 (92.7) | |
| Missing | 20 | 88 | |
| Facial pain prior to enrollment | |||
| Yes | 44 (25.4) | 208 (13.5) | <0.01 |
| No | 129 (74.6) | 1,331 (86.5) | |
| Missing | 2 | 15 | |
| Pain from palpation (body) | |||
| None | 64 (36.8) | 787 (50.6) | <0.01 |
| Any | 110 (63.2) | 767 (49.4) | |
| Missing | 1 | 0 | |
| Pain from palpation (neck) | |||
| None | 97 (55.8) | 1,100 (70.8) | <0.01 |
| Any | 77 (44.3) | 454 (29.2) | |
| Missing | 1 | 0 | |
| mean (±sd) | |||
| Age | 29.1 (8.8) | 26.8 (7.7) | <0.01 |
| Oral Behavior Checklist sum score | 23.9 (10.0) | 20.1 (8.5) | <0.01 |
| Missing | 0 | 29 | |
| SCL 90R Depression (Median (IQR)) | 0.4 (0.7) | 0.2 (0.4) | <0.01† |
| Missing | 0 | 3 | |
| SCL 90R Anxiety (Median (IQR)) | 0.1 (0.4) | 0.1 (0.2) | <0.01† |
| Missing | 0 | 3 | |
| Physical sxs: PILL | 99.8 (26.4) | 87.6 (20.0) | <0.01 |
| Missing | 0 | 2 | |
| PCS coping (Median (IQR)) | 9.0 (16.0) | 7.0 (12.0) | 0.20† |
| Missing | 0 | 1 | |
| Mood state (POMS) | |||
| Bi: Positive Affect | 85.0 (15.5) | 88.2 (15.3) | <0.01 |
| Missing | 0 | 11 | |
| Bi: Negative Affect | 52.8 (16.0) | 48.9 (15.4) | <0.01 |
| Missing | 0 | 11 | |
χ2 test for categorical variables and t-test for continuous variables
Fisher’s exact test for categorical variables and Wilcoxon-test for continuous variables
sd: standard deviation
3.2. Rate of TMD incidence by injury, type of injury and number of injuries
During a median of 2.8 years of follow-up, 175 incident TMD cases were ascertained in 1,729 participants (4429.50 person-years). The rate of TMD incidence was 5.37 per 100 person-years (95%CI=4.19–6.87) among those who experienced a jaw injury and was 3.44 per 100 person-years (95%CI=2.8–4.14) among those who did not experience any jaw injuries during the observation period (Table 2). The above rates were computed using person-years from enrollment until incident TMD for both injured and non-injured groups and did not account for time-dependent aspect of injury. Rates of TMD incidence reported below also did not consider time-dependent aspect of injury.
Table 2.
Absolute incident rates of TMD characterized by any jaw injury, types of first jaw injury and number of jaw injuries. Observed rates derived using person-years from enrollment to incident TMD for both injured and non-injured groups and does not account for time-varying aspect of injury (n=1,729).
| Jaw Injury | Non-cases n=1,554 | Incident TMD cases n=175 | Person-yrs | Incident rate% of people per annum (95% CI) |
|---|---|---|---|---|
| No Injury (ref) | 1,183 (76.1) | 112 (64.0) | 3,255.7 | 3.44 (2.86–4.14) |
| Any Injury | 371 (23.9) | 63 (36.0) | 1,173.8 | 5.37 (4.19–6.87) |
| Type of First Jaw Injury | ||||
| No Injury (ref) | 1,183 (76.1) | 112 (64.0) | 3,255.7 | 3.44 (2.86–4.14) |
| Extrinsic Injury only | 64 (4.1) | 9 (5.1) | 215.8 | 4.17 (2.17–8.02) |
| Intrinsic Injury only | 295 (19.0) | 51 (29.1) | 916.2 | 5.57 (4.23–7.32) |
| Both intrinsic and extrinsic injury | 12 (0.8) | 3 (1.7) | 41.8 | n/c |
| Number of Jaw Injuries | ||||
| No Injury (ref) | 1,183 (76.1) | 112 (64.0) | 3,255.7 | 3.44 (2.86–4.14) |
| One injury | 238 (15.3) | 42 (24.0) | 726.9 | 5.78 (4.27–7.82) |
| Two or more injuries | 133 (8.6) | 21 (12.0) | 446.8 | 4.70 (3.06–7.21) |
n/c estimates were not computed due to small sample size
According to types of injuries, rate of TMD incidence among those whose first jaw injury was of the extrinsic type was 4.17 per 100 person-years (95%CI=2.17–8.02) and among those whose first jaw injury was of the intrinsic type was 5.57 per 100 person-years (95%CI=4.23–7.32) (Table 2).
On stratifying by number of jaw injuries into single injury (n=280) and two or more injuries (n=154), the incidence rate of TMD, defined as the number of TMD cases divided by the number of person-years from enrollment to TMD or last quarterly visit, was 5.78 per 100 person-years (95%CI=4.27–7.82) and 4.70 per 100 person-years (95%CI=3.06–7.21), respectively (Table 2).
3.3. Association between time-dependent first jaw injury and incident TMD
Using jaw injury as a time-dependent covariate in the unadjusted Cox regression model-1 (n=1,613), injury was associated with an approximate four-fold increase in hazard of painful TMD (Table 3: HR=4.00, 95% CI=2.86–5.60). In subsequent multivariable modeling, none of the potential confounding variables changed the unadjusted association by 10% or more. Model-2 which adjusted for study site and demographics likewise signified four-fold greater incidence of TMD associated with jaw injury (HR=3.98, 95% CI=2.81–5.63). In the fully adjusted model-3 that adjusted for all clinically relevant covariates the association was attenuated only marginally (HR=3.67 (95% CI=2.57–5.24), see Table 3. For comparison but not shown in Table 3, in models that include the complete sample of n=1,729, the unadjusted association between first injury and incident TMD was HR=4.02 (95%CI=2.92–5.55), and the study site and demographic adjusted model was HR=3.94 (95%CI=2.82–5.50)
Table 3.
Associations between time-varying first jaw injury, type of first jaw injury, number of jaw injuries with incident TMD using Cox models (n=1,613).
| Jaw Injury | Total n=1,613 | Incident TMD cases n=163 | Hazard Ratio* (95% Confidence Interval) | ||
|---|---|---|---|---|---|
| Model-1 | Model-2** | Model-3 *** | |||
| No Injury (ref) | 1,215 (75.33) | 106 (65.0) | 1.0 | 1.0 | 1.0 |
| First Injury | 398 (24.7) | 57 (35.0) | 4.00 (2.86–5.60) | 3.98 (2.81–5.63) | 3.67 (2.57, 5.24) |
| Type of First Jaw Injury | |||||
| No Injury (ref) | 1,215 (75.33) | 106 (65.0) | 1.0 | 1.0 | 1.0 |
| Extrinsic Injury only | 69 (4.28) | 9 (5.52) | 3.95 (1.98–7.89) | 4.26 (2.11–8.62) | 4.04 (1.96, 8.31) |
| Intrinsic Injury only | 316 (19.59) | 45 (27.61) | 3.85 (2.68–5.53) | 3.80 (2.62–5.50) | 3.47 (2.37, 5.07) |
| Both intrinsic and extrinsic injurya | 15 (0.93) | 3 (1.84) | n/c | n/c | n/c |
| p-valueb | 0.94 | 0.76 | 0.69 | ||
| Number of Jaw Injuries | |||||
| No Injury (ref) | 1,215 (75.33) | 106 (65.03) | 1.0 | 1.0 | 1.0 |
| One injury | 261 (16.18) | 39 (23.93) | 5.27 (3.60–7.73) | 5.93 (3.99–8.79) | 6.01 (4.02–8.99) |
| Two or more injuries | 137 (8.49) | 18 (11.04) | 2.65 (1.60–4.40) | 2.34 (1.40–3.93) | 1.94 (1.14–3.30) |
| p-valuec | 0.02 | <0.01 | <0.01 | ||
Hazard ratio considers when during post-enrollment first injury occurred, and therefore least biases the true association due to the unexposed between enrollment and first jaw injury and correctly contributes to the hazards of the unexposed group
Adjusted for study site, age, gender, and race
Adjusted for study site, age, gender, race, depression, anxiety, physical symptoms, positive and negative mood, coping, and smoking n/c estimates were not computed due to small sample size.
Not part of Woolf test analysis
Woolf test for heterogeneity comparing extrinsic only and intrinsic only injuries
Woolf test for heterogeneity comparing one injury and two or more injuries
Next, the HRs for incident TMD were evaluated for extrinsic and intrinsic injury. Compared to those who did not experience jaw injury during the observation period, those with extrinsic injury experienced a four-fold increase in the HR of TMD in the study site and demographic adjusted model (HR=4.26, 95%CI=2.11–8.62). Results for intrinsic injury was similar (HR=3.80, 95%CI=2.62–5.50) (Table 3). Comparing extrinsic and intrinsic injury was statistically non-significant (Woolf test p=0.76) (Table 3). Those who had experienced both forms of injures are not shown in Table 3 since the number of individuals with both extrinsic and intrinsic forms of injuries were too small for separate analysis (n=15). In Table 4, we present (for descriptive purposes) specific first jaw injury types (frequencies and percentages). Among the TMD incident cases (n=175), intrinsic injuries were the predominant types (29.1%), and these included yawn injuries which were the most frequent (13.1%), followed by injuries due to sustained opening (11.4%), and injuries due to both yawning and sustained opening (4.6%). Only a small percentage of incident TMD cases had extrinsic injuries (5.1%), which included either sport injuries, dental injuries, head injuries, or motor vehicle injuries exclusively, or a combination of whiplash, motor vehicle, sports, head, and shoulder-neck injuries. Additional descriptive analyses on types of injuries by injury are found in Supplementary Table 3s.
Table 4.
Frequency (percent) of type of jaw injury presented by TMD case status (n=1,729).
| Type of Injury | Total n=1,729 | Incident TMD cases n=175 | TMD non-cases n=1,554 |
|---|---|---|---|
| n (%) | |||
| No Injury | 1,295 (74.9) | 112 (64.0) | 1,183 (76.1) |
| Intrinsic injuries only | 346 (20.0) | 51 (29.1) | 295 (19.0) |
| Yawning only | 158 (9.1) | 23 (13.1) | 135 (8.7) |
| Sustained mouth opening only | 132 (7.6) | 20 (11.4) | 112 (7.2) |
| Yawning and Sustained mouth opening | 56 (3.2) | 8 (4.6) | 48 (3.0) |
| Extrinsic injuries only | 73 (4.2) | 9 (5.1) | 64 (4.1) |
| Undefined | 27 (1.6) | 2 (1.1) | 25 (1.6) |
| Sports only | 18 (1.0) | 1 (0.6) | 17 (1.1) |
| Dental Treatment only | 9 (0.5) | 1 (0.6) | 8 (0.5) |
| Head only | 8 (0.4) | 1 (0.6) | 7 (0.4) |
| Shoulder-neck only | 1 (0.1) | 0 | 1 (0.1) |
| Motor Vehicle Accident only | 1 (0.1) | 1 (0.6) | 0 |
| Sports and Oral intubation | 1 (0.1) | 0 | 1 (0.1) |
| Dental treatment and Sports | 1 (0.1) | 0 | 1 (0.1) |
| Dental treatment and Oral intubation | 1 (0.1) | 0 | 1 (0.1) |
| Motor Vehicle Accident and Head | 1 (0.1) | 0 | 1 (0.1) |
| Motor Vehicle Accident and Sports | 1 (0.1) | 0 | 1 (0.1) |
| Motor Vehicle Accident and Whiplash | 1 (0.1) | 1 (0.6) | 0 |
| Whiplash, Sports, Shoulder-Neck and Head | 2 (0.1) | 1 (0.6) | 1 (0.1) |
| Motor Vehicle Accident, Sports, Shoulder-Neck and Head | 1 (0.1) | 1 (0.6) | 0 |
| Both Intrinsic and Extrinsic Injury | 15 (0.9) | 3 (1.7) | 12 (0.8) |
| Sustained mouth opening, Yawn and Undefined extrinsic | 2 (0.1) | 0 | 1 (0.1) |
| Sustained mouth opening and Undefined extrinsic | 1 (0.1) | 0 | 1 (0.1) |
| Yawn and Undefined extrinsic | 1 (0.1) | 0 | 1 (0.1) |
| Yawn and Shoulder-neck | 3 (0.2) | 1 (0.6) | 2 (0.1) |
| Yawn and Sports | 1 (0.1) | 0 | 1 (0.1) |
| Sustained mouth opening and Oral Intubation | 1 (0.1) | 0 | 1 (0.1) |
| Yawn and Dental Treatment | 1 (0.1) | 1 (0.6) | 0 |
| Sustained mouth opening and Dental Treatment | 1 (0.1) | 0 | 1 (0.1) |
| Sustained mouth opening, Yawn and Dental Treatment | 2 (0.1) | 0 | 2 (0.1) |
| Sustained mouth opening, Whiplash and Shoulder-neck | 2 (0.1) | 1 (0.6) | 1 (0.1) |
Undefined: individuals did not report any traumatic events but reported jaw injury.
Listed combinations under both intrinsic and extrinsic injury were presented in the observed sample.
In analyses of individuals who experienced single verses multiple injuries during the follow-up period, compared to those with no injury, the HR for incident TMD among those who experienced only one injury was significantly greater HR=5.93, 95%CI=3.99–8.79 than those who experienced two or more injuries (HR=2.34, 95%CI=1.40–3.93), based on the Woolf test (p<0.01; Table 3).
3.4. Sensitivity analysis
The first sensitivity analysis assessed potential biases due to errors in ascertainment of TMD incidence due to the non-examined positive QHU in the sample of 1,729 individuals. Incident case status was imputed for individuals with positive QHUs and without clinical examination resulting in 248 incident TMD cases, of which 40.7% had experienced an injury and 59.3% had not. The strength of association between injury and incident TMD from the multiple imputation procedure for the multivariable adjusted model (HR=4.01, 95%CI=2.82–5.64) was similar to that from the initial analysis with 175 incident TMD cases for the multivariable adjusted model (HR=3.94, 95%CI=2.82–5.50, Table 4s).
The second sensitivity analysis assessed potential bias due to missing QHUs before the first injury within the 1,729 individuals. Assigning “yes” for injury randomly to a probabilistic sample of 5% and 10% of missing QHUs and missing injury reports in a multiple imputation procedure revealed a HR=3.34 (95%CI=2.37–4.72) and HR=2.94 (95%CI=2.08–4.16), respectively, in the multivariable adjusted model (Table 5s).
The third sensitivity analysis assessed potential bias due to excluding participants with excessively missing QHUs or missing injury reports. Adding 954 individuals to the analytical sample of 1,729 individuals, for a total sample of 2,683, increased the estimate slightly to HR=4.72 (95%CI=3.58–6.22) in the multivariable adjusted model. Assigning “yes” randomly to a probabilistic sample of 5% and 10% of missing QHUs and missing injury reports, in a multiple imputation procedure, revealed an HR=3.30 (95%CI=2.47–4.41) and HR=2.67 (95%CI=1.99–3.59), respectively, in the multivariable model (Table 6s).
4. Discussion
In this prospective cohort study of TMD incidence, subjects who reported experiencing jaw injury had four times the hazard of developing TMD as their non-injured counterparts. While four-fifths of injuries were intrinsic, the rate of TMD increased to a similar degree whether injury was intrinsic or extrinsic. Paradoxically, the rate of TMD in people who experienced a single jaw injury was significantly higher than the rate of TMD in people who had two or more injuries.
In comparison to our study that assessed jaw injury reported from a wide variety of traumatic events, most previous studies of TMD assessed injuries from either motor vehicle accidents, whiplash, or third molar tooth extractions [18–20; 22; 23]. An exception was a case-control study investigating lifetime history of multiple types of trauma which found TMD cases had twice the odds of having experienced facial trauma than controls and a four-fold greater odds for third molar removal [19]. Because of their design, case-control studies inherently have potential for attribution bias: over-reporting of injury as an attributed cause of their pain. In contrast, the current study represents the first prospective study that we know of in which first jaw injury was enumerated prior to ascertainment of first-onset TMD, and a 4-fold increased risk of incident TMD was found. However, within the three-monthly assessment of both injury and pain symptoms, we are unable to assess the sequencing of the injury and pain symptoms. Furthermore, it is possible that within the QHU an individual may attribute injury to an event because pain symptoms were pre-existing before the traumatic event.
Studies on extrinsic vs. intrinsic types of jaw injuries and TMD are scarce. Among individuals with chronic painful TMD compared to non-TMD, a broad evaluation of injury types found that the strongest association was due to prolonged mouth opening (OR=8.3, 95%CI=4.5–15.2), followed by injury due to yawning (OR=7.3, 95%CI=4.2–12.7) and extrinsic injury of any type (OR=4.2, 95%CI=2.8–6.5) after adjusting for study site and demographics [37]. However, given the cross-sectional design, it is possible that sensitization in individuals with chronic painful TMD contributes to increased pain sensitivity attributing to injury. It is also possible that individuals with chronic painful TMD undergo muscle changes, such as presence of persistent guarding behaviors or loss of normal elasticity, that make them more vulnerable to injury from jaw movements and behaviors [33], thereby leading to an increase in jaw injury due to yawning and prolonged mouth opening. While the above-cited estimates suggest that types of injury to the jaw may differ in their impact on the jaw, we found no evidence of that in this study.
In addition, with regard to the effect of number of jaw injuries on risk of TMD, our results indicate that the impact of a single injury on development of first-onset TMD was significantly higher than the impact of the first injury in those who had two or more injuries. However, this finding only considered the effect of the first injury on the risk of TMD and does not take into account the cumulative effects of multiple injuries. It is possible that those with a single injury could have had a more severe form of injury, whereas individuals who experienced multiple injuries did not experience such a severe first injury that would have led to development of sufficient symptoms for a TMD diagnosis.
Multiple factors contribute to TMD, where major risk factors such as psychological states and pain sensitivity are well established. For example, in the OPPERA prospective study, multiple risk factors have been associated with incident TMD, including somatic symptoms, e.g., aches, soreness and tightness (HR=1.44, 95%CI=1.29–1.60) [10], smoking (HR=1.74, 95%CI=1.22–2.47) [44] and sleep disturbance (HR=1.73, 95%CI=1.14–2.62) [43]. In comparison to the other risk factors, the present study and the published literature on injury and TMD provide evidence that injury has a strong, positive association with painful TMD onset. The clinical implications of this finding are consistent with existing literature suggesting that patients should be monitored carefully following injury[11]. While some studies have indicated early intervention to be effective in preventing individuals with acute TMD progressing to chronic TMD [9; 13], use of early intervention has not been evaluated with regard to injury as a risk factor among other risk factors in the progression from acute to chronic TMD. Instead, injury represents a specific situation where early monitoring of signs and symptoms of TMD post-injury may permit identifying an earlier stage where treatment might have its best potential to prevent first-onset TMD.
This study has a number of strengths. The prospective design allows determination of temporality of the association between exposure to jaw injury and subsequent incidence of TMD. This is a unique aspect not found in the existing literature on injury and TMD, which has been primarily limited to cross-sectional study designs. Secondly, we addressed potential confounding and bias that could undermine internal validity. Though confounding was assessed using a conventional and well-established epidemiological approach, we recognize that other methods exist for managing complex variable sets and their interrelationships [14; 47], some of which have been used in the published OPPERA study findings [4]. While prior studies have adjusted for psychological factors [1; 2], in this study, these variables did not meet a prior threshold of 10% or more change in the magnitude of association between the unadjusted model-1 and the multivariable models. Moreover, in comparison to the fully adjusted model-3, model-2 permits better generalizability because it was estimated using the larger sample of n=1,729 and, with far fewer covariates, is more parsimonious. While the different models reflect theoretically important tradeoffs between greater generalizability, on the one hand, and less bias due to confounding, on the other, the consistent finding across models was that injury was associated with a nearly four-fold greater incidence rate of TMD. Thirdly, potential bias related to missing injury information was found not to markedly change the estimate of association between injury and TMD.
Other strengths of this study were due to the methods of data collection. TMD is often experienced as intermittent episodes, and the repeated assessments at follow-up allowed us to capture the disease phenomenon more judiciously in comparison to studies with only a single follow-up assessment. Trained and calibrated examiners used a validated clinical examination protocol (RDC/TMD) to adjudicate first-onset incident TMD cases, decreasing the potential for outcome misclassification. Lastly, the sociodemographic characteristics of the large cohort of individuals, with no prior history of TMD, recruited across four study sites closely mirrors the socio-demographic distribution of the U.S 2000 decennial census, [45]. While the sample in this study had some loss of generalizability due to missing data, sensitivity analysis suggests results are internally valid to gauge injury-TMD associations.
However, there are some limitations to this study. First, false negative case classification due to absence of a clinical examination was possible in those reporting sub-threshold pain symptoms and thereby not scheduled for a clinic visit. Nevertheless, as Bair et al reported, the QHU was reliable for pain density reporting and appropriately sensitive with minimal false negatives for case classification [3]. Second, false negative case classification due to timing of the clinical examination was possible in those with positive QHU pain density reports. Due to the fluctuating nature of TMD with intermittent episodes of pain and remission, the previously reported pain symptoms could have remitted and therefore were not reproducible on clinical examination. Of the 478 positive QHUs accompanied by examination within the full sample of 2,737 individuals with at least one QHU, 243 (50.8%) examinations were negative for TMD. Had these individuals with remitted pain symptoms been assessed closer to the time of the symptom report on the QHU, they may have qualified as an onset case. Nevertheless, the sensitivity analysis indicated that imputing for incident-case status for individuals with positive QHU but without clinical examination did not change the estimate of the association between injury and TMD.
Third, although information on a number of lifestyle, behavior, and general health factors were systematically collected to assess for potential confounding, there may be residual confounding by unmeasured factors such as fear-avoidance, a known risk factor for pain and that could change an individuals’ vulnerability to injury, or litigation, that has mixed (and even bi-directional) effects on pain following injury. However, most injury in this study was “intrinsic”, creating no potential for litigation [30]. Finally, we excluded a number of individuals based on either complete loss to follow-up, partial loss to follow-up, and missing injury reports. Yet, including the 954 individuals with excessively missing QHUs and further assuming 5% and 10% of the missing QHUs and QHUs with missing information on injury were positive for injury, multiple imputation did not markedly change the measure of association between injury and TMD from our initial analysis on the n=1,729 sample.
In conclusion, in this cohort of adults a positive and a strong association between first jaw injury and incidence of first-onset TMD was observed regardless of whether the injury was extrinsic or intrinsic. Given the increased risk of developing incident painful TMD after jaw injury, it appears prudent to monitor individuals who experience either intrinsic or extrinsic injury, especially if early identification and treatment of TMD symptoms is associated with less painful and shorter episodes of TMD.
Supplementary Material
Acknowledgements
This work was supported by the National Institutes of Health and National Institutes of Dental and Craniofacial Research (grant number U01-DE017018 and P01-NS045685), NIH/NIDCR training grant (T32-DE023526), and funding from Department of Oral Diagnostic Sciences, School of Dental Medicine, University at Buffalo, New York. The OPPERA program also acknowledges resources specifically provided for this project by the participating institutions: Battelle Memorial Institute; University at Buffalo; University of Florida; University of Maryland; University of North Carolina at Chapel Hill.
Footnotes
Conflict of interest statement
The authors have no conflict of interest to declare.
REFERENCES
- [1].Aggarwal VR, Macfarlane GJ, Farragher TM, McBeth J. Risk factors for onset of chronic oro-facial pain--results of the North Cheshire oro-facial pain prospective population study. Pain 2010;149(2):354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Aggarwal VR, McBeth J, Zakrzewska JM, Lunt M, Macfarlane GJ. Are reports of mechanical dysfunction in chronic oro-facial pain related to somatisation? A population based study. European journal of pain 2008;12(4):501–507. [DOI] [PubMed] [Google Scholar]
- [3].Bair E, Brownstein NC, Ohrbach R, Greenspan JD, Dubner R, Fillingim RB, Maixner W, Smith SB, Diatchenko L, Gonzalez Y, Gordon SM, Lim PF, Ribeiro-Dasilva M, Dampier D, Knott C, Slade GD. Study protocol, sample characteristics, and loss to follow-up: the OPPERA prospective cohort study. J Pain 2013;14(12 Suppl):T2–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bair E, Ohrbach R, Fillingim RB, Greenspan JD, Dubner R, Diatchenko L, Helgeson E, Knott C, Maixner W, Slade GD. Multivariable modeling of phenotypic risk factors for first-onset TMD: the OPPERA prospective cohort study. The journal of pain : official journal of the American Pain Society 2013;14(12 Suppl):T102–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bergman H, Andersson F, Isberg A. Incidence of temporomandibular joint changes after whiplash trauma: a prospective study using MR imaging. AJR Am J Roentgenol 1998;171(5):1237–1243. [DOI] [PubMed] [Google Scholar]
- [6].Caroll LJ, Ferrari R, Cassidy JD. Reduced or painful jaw movement after collision-related injuries: A population based study. J Am Dent Assoc 2007;138(1):86–93. [DOI] [PubMed] [Google Scholar]
- [7].Derogatis LR. SCL-90-R : symptom checklist-90-R : administration, scoring & procedures manual. Minneapolis, Minne: National Computer Systems, Inc., 1994. [Google Scholar]
- [8].Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. Journal of craniomandibular disorders : facial & oral pain 1992;6(4):301–355. [PubMed] [Google Scholar]
- [9].Epker J, Gatchel RJ, Ellis E 3rd. A model for predicting chronic TMD: practical application in clinical settings. J Am Dent Assoc 1999;130(10):1470–1475. [DOI] [PubMed] [Google Scholar]
- [10].Fillingim RB, Ohrbach R, Greenspan JD, Knott C, Diatchenko L, Dubner R, Bair E, Baraian C, Mack N, Slade GD, Maixner W. Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain 2013;14(12 Suppl):T75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Fricton J, Eli B, Gupta A, Johnson N. Preventing chronic pain after acute jaw sprain or strain. J Am Dent Assoc 2016;147(12):979–986. [DOI] [PubMed] [Google Scholar]
- [12].Garcia R Jr., Arrington JA. The relationship between cervical whiplash and temporomandibular joint injuries: an MRI study. Cranio 1996;14(3):233–239. [DOI] [PubMed] [Google Scholar]
- [13].Gatchel RJ, Stowell AW, Wildenstein L, Riggs R, Ellis E 3rd. Efficacy of an early intervention for patients with acute temporomandibular disorder-related pain: a one-year outcome study. J Am Dent Assoc 2006;137(3):339–347. [DOI] [PubMed] [Google Scholar]
- [14].Greenland S Modeling and variable selection in epidemiologic analysis. Am J Public Health 1989;79(3):340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Greenspan JD, Slade GD, Bair E, Dubner R, Fillingim RB, Ohrbach R, Knott C, Diatchenko L, Liu Q, Maixner W. Pain sensitivity and autonomic factors associated with development of TMD: the OPPERA prospective cohort study. J Pain 2013;14(12 Suppl):T63–74 e61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Häggman-Henrikson B, Osterlund C, Eriksson PO. Endurance during chewing in whiplash-associated disorders and TMD. J Dent Res 2004;83(12):946–950. [DOI] [PubMed] [Google Scholar]
- [17].Heise AP, Laskin DM, Gervin AS. Incidence of temporomandibular joint symptoms following whiplash injury. J Oral Maxillofac Surg 1992;50(8):825–828. [DOI] [PubMed] [Google Scholar]
- [18].Huang GJ, Drangsholt MT, Rue TC, Cruikshank DC, Hobson KA. Age and third molar extraction as risk factors for temporomandibular disorder. J Dent Res 2008;87(3):283–287. [DOI] [PubMed] [Google Scholar]
- [19].Huang GJ, LeResche L, Critchlow CW, Martin MD, Drangsholt MT. Risk factors for diagnostic subgroups of painful temporomandibular disorders (TMD). J Dent Res 2002;81(4):284–288. [DOI] [PubMed] [Google Scholar]
- [20].Huang GJ, Rue TC. Third-molar extraction as a risk factor for temporomandibular disorder. J Am Dent Assoc 2006;137(11):1547–1554. [DOI] [PubMed] [Google Scholar]
- [21].Klobas L, Tegelberg A, Axelsson S. Symptoms and signs of temporomandibular disorders in individuals with chronic whiplash-associated disorders. Swed Dent J 2004;28(1):29–36. [PubMed] [Google Scholar]
- [22].Kolbinson DA, Epstein JB, Senthilselvan A, Burgess JA. A comparison of TMD patients with or without prior motor vehicle accident involvement: treatment and outcomes. J Orofac Pain 1997;11(4):337–345. [PubMed] [Google Scholar]
- [23].Kolbinson DA, Epstein JB, Senthilselvan A, Burgess JA. Effect of impact and injury characteristics on post-motor vehicle accident temporomandibular disorders. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics 1998;85(6):665–673. [DOI] [PubMed] [Google Scholar]
- [24].Kronn E The incidence of TMJ dysfunction in patients who have suffered a cervical whiplash injury following a traffic accident. J Orofac Pain 1993;7(2):209–213. [PubMed] [Google Scholar]
- [25].Lee PH. Is a cutoff of 10% appropriate for the change-in-estimate criterion of confounder identification? J Epidemiol 2014;24(2):161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 1993;124(10):115–121. [DOI] [PubMed] [Google Scholar]
- [27].Lorr M, Heuchert JWP, McNair DM. Profile of Mood States: Bipolar Form. San Diego, CA: Educational and Industrial Testing Service,, 1998. [Google Scholar]
- [28].Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol 1993;138(11):923–936. [DOI] [PubMed] [Google Scholar]
- [29].Markiewicz MR, Ohrbach R, McCall WD Jr. Oral behaviors checklist: reliability of performance in targeted waking-state behaviors. Journal of orofacial pain 2006;20(4):306–316. [PubMed] [Google Scholar]
- [30].McLean SA, Ulirsch JC, Slade GD, Soward AC, Swor RA, Peak DA, Jones JS, Rathlev NK, Lee DC, Domeier RM, Hendry PL, Bortsov AV, Bair E. Incidence and predictors of neck and widespread pain after motor vehicle collision among US litigants and nonlitigants. Pain 2014;155(2):309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989;129(1):125–137. [DOI] [PubMed] [Google Scholar]
- [32].Miller VJ, Bodner L. The long-term effect of oromaxillofacial trauma on the function of the temporomandibular joint. Journal of oral rehabilitation 1999;26(9):749–751. [DOI] [PubMed] [Google Scholar]
- [33].Moseley GL, Arntz A. The context of a noxious stimulus affects the pain it evokes. Pain 2007;133(1–3):64–71. [DOI] [PubMed] [Google Scholar]
- [34].NIH/NIDCR. Facial Pain, Vol. 2016: National Institues of Health, 2014. [Google Scholar]
- [35].Ohrbach R, Bair E, Fillingim RB, Gonzalez Y, Gordon SM, Lim PF, Ribeiro-Dasilva M, Diatchenko L, Dubner R, Greenspan JD, Knott C, Maixner W, Smith SB, Slade GD. Clinical orofacial characteristics associated with risk of first-onset TMD: the OPPERA prospective cohort study. J Pain 2013;14(12 Suppl):T33–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ohrbach R, Dworkin SF. The Evolution of TMD Diagnosis: Past, Present, Future. J Dent Res 2016;95(10):1093–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Ohrbach R, Fillingim RB, Mulkey F, Gonzalez Y, Gordon S, Gremillion H, Lim PF, Ribeiro-Dasilva M, Greenspan JD, Knott C, Maixner W, Slade G. Clinical findings and pain symptoms as potential risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain 2011;12(11 Suppl):T27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Riley JL 3rd, Robinson ME. CSQ: five factors or fiction? Clin J Pain 1997;13(2):156–162. [DOI] [PubMed] [Google Scholar]
- [39].Rusanen J, Pirttiniemi P, Tervonen O, Raustia A. MRI of TMJ in patients with severe skeletal malocclusion following surgical/orthodontic treatment. Cranio : the journal of craniomandibular practice 2008;26(3):182–190. [DOI] [PubMed] [Google Scholar]
- [40].Sahebi S, Moazami F, Afsa M, Nabavi Zade MR. Effect of lengthy root canal therapy sessions on temporomandibular joint and masticatory muscles. Journal of dental research, dental clinics, dental prospects 2010;4(3):95–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Salè H, Hedman L, Isberg A. Accuracy of patients’ recall of temporomandibular joint pain and dysfunction after experienceing whiplash trauma: a prospective study. J Am Dent Assoc 2010;141:879–886. [DOI] [PubMed] [Google Scholar]
- [42].Salé H, Isberg A. Delayed temporomandibular joint pain and dysfunction induced by whiplash trauma A controlled prospective study. JADA 2007;138(8):1084–1091. [DOI] [PubMed] [Google Scholar]
- [43].Sanders AE, Essick GK, Fillingim R, Knott C, Ohrbach R, Greenspan JD, Diatchenko L, Maixner W, Dubner R, Bair E, Miller VE, Slade GD. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. Journal of dental research 2013;92(7 Suppl):70S–77S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Sanders AE, Slade GD, Bair E, Fillingim RB, Knott C, Dubner R, Greenspan JD, Maixner W, Ohrbach R. General health status and incidence of first-onset temporomandibular disorder: the OPPERA prospective cohort study. The journal of pain : official journal of the American Pain Society 2013;14(12 Suppl):T51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Slade GD, Bair E, By K, Mulkey F, Baraian C, Rothwell R, Reynolds M, Miller V, Gonzalez Y, Gordon S, Ribeiro-Dasilva M, Lim PF, Greenspan JD, Dubner R, Fillingim RB, Diatchenko L, Maixner W, Dampier D, Knott C, Ohrbach R. Study methods, recruitment, sociodemographic findings, and demographic representativeness in the OPPERA study. J Pain 2011;12(11 Suppl):T12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Slade GD, Bair E, Greenspan JD, Dubner R, Fillingim RB, Diatchenko L, Maixner W, Knott C, Ohrbach R. Signs and symptoms of first-onset TMD and sociodemographic predictors of its development: the OPPERA prospective cohort study. J Pain 2013;14(12 Suppl):T20–32 e21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Tibshirani R The lasso method for variable selection in the Cox model. Stat Med 1997;16(4):385–395. [DOI] [PubMed] [Google Scholar]
- [48].Visscher C, Hofman N, Lousberg R,MN Is temporomandibular pain in chronic whiplash-associated disorders part of a more widespread pain syndrome? Clin J Pain 2005;21(4):353–357. [DOI] [PubMed] [Google Scholar]
- [49].Wall PD. On the relation of injury to pain. The John J. Bonica lecture. Pain 1979;6(3):253–264. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.