Abstract
Context
With more studies investigating effects of high serum lipid levels, new findings are emerging regarding the damage these biomolecules may cause.
Aim
In this study we aimed to find a relation between neuropathy and hypertriglyceridemia in patients with metabolic syndrome (MS).
Material and methods
One hundred and twenty subjects (Ninety subjects with metabolic syndrome and 30 healthy controls) were included in the study. Subjects with MS were divided into three groups. HbA1C levels of the subjects were < 5.7% in group A, ≥ 5.7% - < 6.5% in group B, and ≥ 6.5% - < 8.0% in group C. Pin-Prick test and Semmes- Weinstein Monofilament were used for neurological examination. Electromyography was performed to patients with neuropathy to support the diagnosis.
Results
Neuropathy prevalence was found to be higher in the subjects with metabolic syndrome compared to control group. (9.9 %; 16.65 %; 23.31 % vs. 3.3%; in group A, group B, group C vs. healthy control group respectively) (p=0.003 for group A, p=0.0002 for group B, p=0.0002 for group C). There was an association between triglyceride levels and neuropathy in group C.
Conclusion
Patients with MS may have more neuropathy risk than we estimate.
Keywords: hypertriglyceridemia, metabolic syndrome, neuropathy
INTRODUCTION
The Metabolic Syndrome (MS) is a cluster of findings including central obesity, glucose intolerance, hyperinsulinemia, low high density lipoprotein (HDL) level, high triglyceride levels and hypertension (1), associated with a high risk of coronary heart disease (CHD) and mortality (2). Along with macrovascular complications, there is growing evidence indicating that MS, like diabetes mellitus (DM), can cause microvascular complications in patients with type 2 DM (3-5).
Neuropathy, one of the microvascular complications, is an overlooked cause of morbidity in patients with diabetes. From infections to arrhythmia, neuropathy can result with a wide range of medical conditions. Most frequent cause of neuropathy is DM (6). In patients with MS, neuropathy is not uncommon due to high glucose levels in most of the patients.
In 1999, Drory et al. observed subclinical neuropathy in patients with hypertriglyceridemia (7) and same findings were also found in another prospective study by Kassem et al.(8). Patients with metabolic syndrome have both hyperglycemia and hypertriglyceridemia, thus prone to neuropathy risk more than patients with DM. In this study we aimed to find a relation between neuropathy and hypertriglyceridemia in patients with MS.
MATERIAL AND METHODS
Between April 2012 and April 2013, ninety patients who were referred to Istanbul Medeniyet University Goztepe Training and Research Hospital and were diagnosed with metabolic syndrome according to 2009 Joint Interim Statement (JIS) definition (9) and 30 healthy control subjects were enrolled to the study. Inclusion criteria were, being older than 18 years, giving consent to participating, normal serum folate, vitamin B6 and B12 levels. Exclusion criteria included; diabetes history for more than 5 years, presence of metabolic, infectious, inflammatory and mechanic conditions that may cause neuropathy and being younger than 18 years. The study was approved by the Ethical Committee, and informed consents were obtained from the patients. Patients with metabolic syndrome were stratified into 3 groups according to their HbA1c levels as; group A (n=30): HbA1c level < 5.7%, group B (n=30): HbA1c level between ≥ 5.7% and < 6.5%, group C (n=30): HbA1c level between ≥ 6.5% and < 8.0%. Demographic, clinical and laboratory data of the patients were recorded. The patients were questioned about their diseases, their medications and alcohol use. Pin-prick test and Semmes-Weinstein Monofilament test were used to assess peripheral neuropathy. Patients with positive results in both tests were accepted as patients with neuropathy (10, 11).
Patients with neuropathy were examined with electromyography (EMG) to support the diagnosis. EMG was performed with Medelec Synergy EMG device (Oxford, London). Upper and lower extremity motor and sensory nerve conductions were studied (latency, amplitude and nerve conduction velocity). Right and left leg sural nerve velocities of each patient were recorded. Sural nerve conduction velocity lower than 40 m/s was considered to be abnormal.
Statistical analysis was performed using SPSS for Windows 15.0. Chi-square test was used for categorical data comparison. One-way ANOVA was used for normal distributed data and p<0.05 was considered as statistically significant.
RESULTS
A hundred and eighty six patients were screened and 66 patients were excluded according to exclusion criteria. Table 1 shows demographic characteristics of the patients. Mean body mass index of the groups were 26.77 for healthy controls, 32.01 for group A, 31.67 for group B and 33.38 for group C. There were no patients with neuropathy in healthy controls. Neuropathy prevalence was found 10 % in group A, 16.67 % in group B and 23.33 % in group C with p values 0.003, 0.0002 and 0.0002 respectively. Right and left leg sural nerve velocities of each patient are shown in Table 2. In group A, three patients were found to have neuropathy and EMG results of these patients confirmed the diagnosis. In group B, five patients had neuropathy and with EMG, four patients’ neuropathy diagnosis was confirmed, in one patient sural nerve response was not achieved. In group C there were seven patients with neuropathy and EMG results have found sensory neuropathy in 6 of these patients, in one patient sural nerve response was not achieved. Although, higher HbA1C levels found to be related with higher neuropathy prevalence, this difference was not statistically significant (p=0.31 for group A vs. group B; p=0.36 for group B vs. group C).
Table 1.
Demographic and clinical data
| Control group n=30 | Group A n=30 | Group B n=30 | Group C n=30 | |
| Age (Years) | 48.96 ± 11.16 | 49.60 ± 13.02 | 50.13 ± 11.74 | 49.73 ± 9.51 |
| Sex | Male:13 | Male:14 | Male:15 | Male:15 |
| Female:17 | Female:16 | Female:15 | Female:15 | |
| BMI (kg/m2) | 26.77 ± 2.53 | 32.01 ± 4.97 | 31.67 ± 4.29 | 33.38 ± 5.83 |
| WC(cm) | 84.60±6.34 | 103.73±7.68 | 102.96±9.47 | 111.03±12.02 |
| SBP (mm/Hg) | 120.50 ± 8.94 | 128.40 ± 18.43 | 129.27 ± 8.88 | 128.17 ± 13.74 |
| DBP(mm/Hg) | 77.00 ± 6.51 | 81.23 ± 9.87 | 77.00 ± 6.27 | 79.00 ± 5.93 |
| Triglyceride (mg/dL) | 112.57 ± 50.76 | 158.5 ± 65.90 | 143.43 ± 74.38 | 160.73 ± 58.40 |
| Total cholesterol (mg/dL) | 166 ± 23.72 | 182 ± 45.53 | 225 ± 64.56 | 195 ± 54.92 |
| Subjects with Neuropathy (n;%) | None | 3; 10 | 5; 16.67 | 7; 23.33 |
| Mean Diabetes Duration (months) | N/A | N/A | 19.23±14.96 | 22.26±17.53 |
BMI: Body Mass Index, WC: Waist Circumference, SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, N/A: not applicable Control group: Healthy subjects (n=30)
Group A: Subjects with metabolic syndrome HbA1c levels <% 5.7 (n=30)
Group B: Subjects with metabolic syndrome HbA1c levels between ≥% 5.7, <% 6.5 (n=30)
Group C: Subjects with metabolic syndrome HbA1c levels between ≥% 6.5, <% 8.0 (n=30).
Table 2.
Electromyography results of right sural nerve
| Amplitude (microV) | Conduction Velocity (m/s) | |
| Group A, patient 1 | 3.42 | 39.5 |
| Group A, patient 2 | 3.92 | 36.3 |
| Group A, patient 3 | 3.46 | 37.6 |
| Group B, patient 1 | 4.58 | 32.8 |
| Group B, patient 2 | 4.54 | 34.9 |
| Group B, patient 3 | 3.98 | 36.2 |
| Group B, patient 4 | Response not achieved | Response not achieved |
| Group B, patient 5 | 4.12 | 35.9 |
| Group C, patient 1 | 4.92 | 31.7 |
| Group C, patient 2 | 4.36 | 34.3 |
| Group C, patient 3 | 3.52 | 32.4 |
| Group C, patient 4 | 4.46 | 31.6 |
| Group C, patient 5 | 4.68 | 33.8 |
| Group C, patient 6 | 4.54 | 34.9 |
| Group C, patient 7 | Response not achieved | Response not achieved |
MicroV: microvolt
M/s: meters/second.
Table 3 shows the treatment modalities of the patients according to their groups. Only one patient in this study was on insulin treatment.
Table 3.
Treatment modalities according to groups
| Only diet | Single OAD (metformin) | Dual OAD | ≥3 OAD | Insulin | |
| Group 2 | 27/30 | 3/30 | - | - | |
| % | 89.1(%) | (10.9%) | |||
| Group 3 | 9/30 | 16/30 | 5/30 | - | - |
| % | (29.9%) | (53.3%) | (16.6%) | ||
| Group 4 | 17/30 | 12/30 | - | 1/30 | |
| % | (56.7%) | (39.9%) | (3.33%) |
OAD: Oral antidiabetics.
Mean total cholesterol levels were 166 for healthy controls, 182 for group A, 225 for group B and 195 for group C. No significant difference was observed between cholesterol levels of the groups. Mean triglyceride levels of the groups are shown in Figure 1. A significant association between neuropathy and triglyceride levels was found only in group C (p=0.01).
Figure 1.
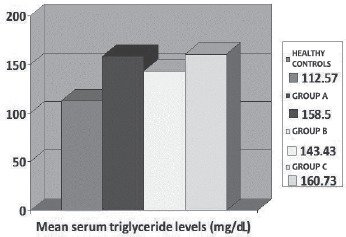
Mean serum triglyceride levels of the groups.
DISCUSSION
Study results show increasing neuropathy prevalence with increasing HbA1c levels. In another study by Young et al. in patients with diabetes less than 5 years (12), neuropathy prevalence was 21 %, our study result correlates with this finding.
In this study we found that about 10 percent of patients with MS and with normal HbA1C levels and 16% of patients with MS and pre-diabetes have neuropathy. In an analysis from NHANES study showed, peripheral neuropathy risk was 11 % higher in patients with prediabetes compared to patients with no diabetes (13).
In our study an association was found between high triglyceride levels of patients with the highest Hba1c levels and neuropathy. Same correlation was found in another study by Hughes et al. which suggests that neuropathy linked to hypertriglyceridemia can be more painful (14). In another study by Smith (15) et al. hypertriglyceridemia was found as one of the risk factors for neuropathy. Metabolic syndrome consists of both diabetes and hypertriglyceridemia; the results of our study and the other studies mentioned may reveal that patients with metabolic syndrome may be at double “jeopardy” for neuropathy.
There can be several mechanisms that may explain this finding. One of which is oxidative stress. Increased triglyceride levels may harm neurons by inflammatory pathways. In a study by Rosenson et al. with fenofibrate treatment in subjects with hypertriglyceridemia, amelioration in inflammatory markers was observed (16). Another explanation to these findings may be that hypertriglyceridemia itself can cause damage to neurons, particularly their conduction ability. In a study by Lupachyk et al. a niacin derivative “acipimox” was given to rats with hypertriglyceridemia and improvement in neuropathy and reduction in triglyceride levels were observed with this agent (17).
There are several limitations of this study. First of all, our sample size is relatively small and positive findings are limited. Secondly, diagnosis of peripheral neuropathy is not at ease and the non-invasive methods are still not highly sensitive (18).
Our results may provide additional data for a possible relationship between hypertriglyceridemia and neuropathy. Because MS is an increasing epidemic, neuropathy risk of these patients due to both hyperglycemia and hypertriglyceridemia should be sought further with more prospective studies in order to decrease morbidity and even mortality due to relevant complications.
Conflict of interest
The authors declare that they have no conflict of interest concerning this article.
References
- 1.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 2.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 3.Szalat A, Raz I. Metabolic syndrome and microangiopathy. Isr Med Assoc J. 2006;8:424–425. [PubMed] [Google Scholar]
- 4.Shimajiri Y, Tsunoda K, Furuta M, Kadoya Y, Yamada S, Nanjo K, Sanke T. Prevalence of metabolic syndrome in Japanese type 2 diabetic patients and its significance for chronic vascular complications. Diabetes Res Clin Pract. 2008;79:310–317. doi: 10.1016/j.diabres.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 5.Isomaaa B, Henricsson M, Almgren P, Tuomi T, Taskinen MR, Groop L. The metabolic syndrome influences the risk of chronic complications in patients with type II diabetes. Diabetologica. 2001;44:1148–54. doi: 10.1007/s001250100615. [DOI] [PubMed] [Google Scholar]
- 6.Backonja M, Beydoun A, Edwards KR, Schwartz SL, Fonseca V, Hes M, LaMoreaux L, Garofalo E. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA. 1998;280(21):1831–1836. doi: 10.1001/jama.280.21.1831. [DOI] [PubMed] [Google Scholar]
- 7.Drory VE, Groozman GB, Rubinstein A, Koreczyn A. Hypertriglyceridemia maycausea subclinical peripheral neuropathy. Electromyography and clinical neurophysiology. 1999;39(1):39–41. [PubMed] [Google Scholar]
- 8.Kassem HS, Azar ST, Zantout MS, Sawaya RA. Hypertriglyceridemia and peripheral neuropathy in neurologically asymptomatic patients. Neuroendocrinology letters. 2005;26(6):775–779. [PubMed] [Google Scholar]
- 9.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 10.Sosenko JM, Sparling YH, Hu DS, Welty T, Howard BV, Lee E, Robbings DC. Use of the Semmes-Weinstein monofilament in the Strong Heart Study. Diabetes Care. 1999;22:1715–1721. doi: 10.2337/diacare.22.10.1715. [DOI] [PubMed] [Google Scholar]
- 11.Forouzandeh F, Aziz Ahari A, Abolhasani F, Larijani B. Comparison of different screening tests for detecting diabetic foot neuropathy. Acta Neurologica Scandinavica. 2005;112(6):409–413. doi: 10.1111/j.1600-0404.2005.00494.x. [DOI] [PubMed] [Google Scholar]
- 12.Young MJ, Boulton AJM, MacLeod AF, Williams DRR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia. 1993;36(2):150–154. doi: 10.1007/BF00400697. [DOI] [PubMed] [Google Scholar]
- 13.Katon Jodie G, Reiber Gayle E., Nelson Karin M. Peripheral Neuropathy Defined by Monofilament Insensitivity and Diabetes Status NHANES 1999–2004. Diabetes care. 2013;36(6):1604–1606. doi: 10.2337/dc12-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hughes RAC, Umapathi T, Gray IA, Gregson NA, Noori M, Pannala AS, Swan AV. A controlled investigation of the cause of chronic idiopathic axonal polyneuropathy. Brain. 2004;127(8):1723–1730. doi: 10.1093/brain/awh192. [DOI] [PubMed] [Google Scholar]
- 15.Smith A. Gordon, Robinson Singleton J. Obesity and hyperlipidemia are risk factors for early diabetic neuropathy. Journal of Diabetes and its Complications. 2013;27(5):436–442. doi: 10.1016/j.jdiacomp.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenson RS, Wolff DA, Huskin AL, Helenowski IB, Rademaker AW. Fenofibrate therapy ameliorates fasting and postprandial lipoproteinemia, oxidative stress, and the inflammatory response in subjects with hypertriglyceridemia and the metabolic syndrome. Diabetes Care. 2007;30(8):1945–1951. doi: 10.2337/dc07-0015. [DOI] [PubMed] [Google Scholar]
- 17.Lupachyk S, Watcho P, Hasanova N, Julius U, Obrosova IG. Triglyceride, nonesterified fatty acids, and prediabetic neuropathy: role for oxidative–nitrosative stress. Free Radical Biology and Medicine. 2012;52(8):1255–1263. doi: 10.1016/j.freeradbiomed.2012.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horowitz SH. Criteria for the diagnosis of peripheral neuropathies. Occupational and environmental medicine. 2002;59(7):425–426. doi: 10.1136/oem.59.7.425. [DOI] [PMC free article] [PubMed] [Google Scholar]


