Abstract-
Purpose
Piezosurgery is a relatively novel, precise and safe technique of ostectomy in the domain of oral and maxillofacial surgery. Our aim was to compare the inflammatory outcomes of osteotomy using piezosurgery and conventional bur in impacted mandibular third molar (IM3M) surgery.
Subjects and method
The study implemented a randomized, double-blind, crossover design. 120 sides in 60 patients were randomly allocated to the two interventions used, viz; conventional bur and piezosurgery. The primary outcome variables evaluated were facial swelling, trismus, pain, and paresthesia. Additionally, the duration of surgery and the frequency of soft tissue injuries with the use of two techniques were also evaluated.
Results
Pain, swelling, trismus, and soft tissue injuries emerged to be significantly higher with the use of bur as compared to the piezo. The duration of surgery was significantly extended in the piezo group and no significant difference was observed in the occurrence of paresthesia between the two groups.
Conclusion
The result suggests that piezosurgical osteotomy technique is superior to conventional bur in terms of the postoperative inflammatory outcomes in IM3M surgery.
Keywords: Impacted tooth, Third molar, Piezosurgery, Ostectomy, Pain, Trismus, Swelling
1. Introduction
IM3M extraction is the most routine minor oral surgical procedure practiced in clinical practice. Its surgical removal initiates a series of orchestrated inflammatory events owing to trauma to the investing bone and soft tissues.1 These are exhibited clinically as pain, swelling, trismus, and bleeding. It adversely affects the physical, psychological, and functional well-being of an individual and has direct repercussions over the postoperative quality of life.2
One of the most vital steps in the removal of impacted teeth is ostectomy, for which many techniques are in practice.3 Traditionally, rotary burs were considered a time-honored technique for ostectomy in IM3M removal. It inherently inflicts variable insult to the bone and soft tissue due to overheating, causing a greater degree of discomfort and protracted course of recovery. With the recent trends towards minimally invasive surgery, piezosurgery – a novel ostectomy technique was popularized in oral and maxillofacial surgery.4 The inserts employ micro-vibrations of the scalpel, maintained at a frequency of 24–29 kHz and amplitude alternating between 60 and 200 μm/s permitting a precise, safe and efficient ostectomy.5 The piezoelectric instrument selectively works on hard tissue, thus reducing the likelihood of inflicting iatrogenic trauma to surrounding tissues, including the mucosa and neurovascular structures.6,7 Investigators have promulgated piezosurgical devices as a safer and preferred alternative to conventional bur for ostectomies owing to favorable osseous response facilitating speedy recovery.8,9
The authors of the study hypothesize that piezosurgery is a superior alternative to conventional bur for ostectomy in IM3M in terms of improved postoperative inflammatory outcomes.
The study was deliberated to determine and compare the post-surgical inflammatory sequelae (facial swelling, trismus, pain) soft tissue injuries and neurological complications following ostectomy during removal of IM3M using a piezosurgery and conventional rotary burs, along with the assessment of the difference in operating time required.
Subjects and method- The present prospective, randomized, controlled, double-blind, crossover study was instigated on 60 systemically healthy individuals between September 2016 to Aug 2018. The study sample was derived from a patient population having asymptomatic bilateral symmetrically positioned IM3M reporting to the outpatient department of oral and maxillofacial surgery at our institute. This study confirms with the Helsinki declaration and its later amendments or comparable ethical standards. Institutional ethical committee approval from the Central Ethics Committee on Human Research (C.E.C.H.R) of Datta Meghe Institute of Medical Sciences was obtained prior to the initiation of the study.
Individuals with a presence of bilaterally asymptomatic vertical or mesioangularly oriented IM3M with similar difficulty index, depth and relationship with ramus were recruited in the study sample. Patients with the history of systemic diseases such as endocrinopathies, coagulopathies, any chronic facial pain or edema on the side of intervention, trismus, acute/chronic infections, patients on antipsychotic and anti-depressant drugs, lactating mothers or females on oral contraceptives and smokers were excluded. A detailed written informed consent was obtained from each patient.
A split-mouth design was executed and each patient was treated surgically to remove M3M using bur (control group) on one random side and piezo (study group) device on the contralateral side using a list of computer-generated randomized numbers generated for each side of the patient. The instrument was randomly selected using a coin toss, ascertaining random instrument sequence. The study design conformed with the CONSORT 2010 flow diagram for randomized trials.
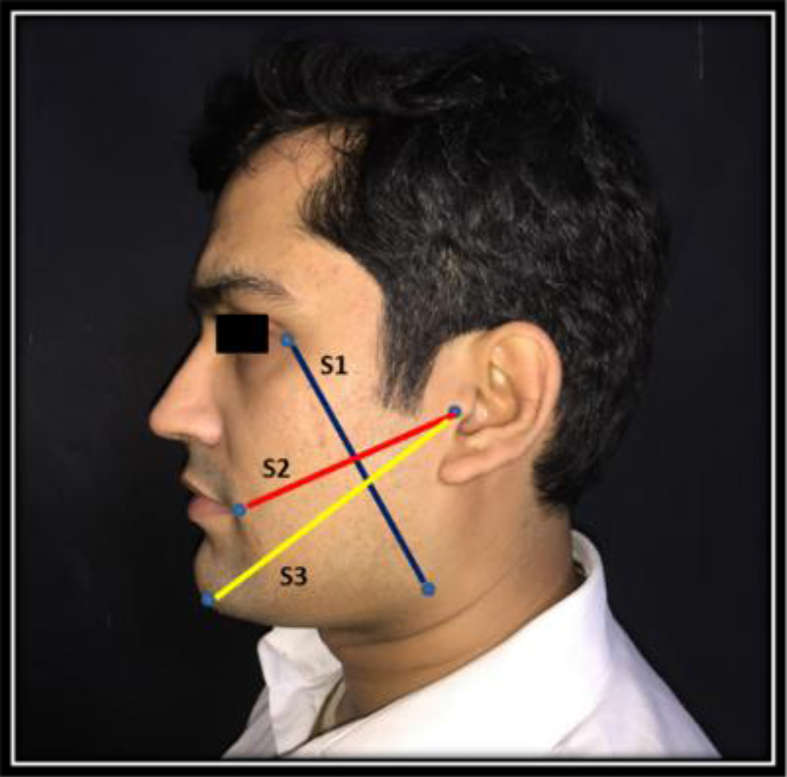
Pre-operative assessments such as facial measurements, inter-incisal mouth opening, and any sensorineural deficit/hyperesthesia/hypoesthesia/paresthesia/anesthesia were recorded as a baseline measurement and for post-surgical comparison on postoperative days 2nd and 7th. Clinical assessment of the soft tissue injuries was performed on the same day of surgery using a four-unit visual analogue scale (VAS) of 0–3, based on the color and presence of edema and bleeding; i.e., 0, normal pink, not edematous; 1, pink-red, slightly edematous; 2, red, edematous; and 3, red, edematous, bleed easily when touched.12 Facial measurements were recorded with measuring tape by taking the mean of the distance from the lateral corner of the eye (A) to angle of the mandible (B) (A-B S1), Tragus (C) to the corner of the mouth (D) (C-D=S2) and Tragus (C) to soft tissue pogonion (E) (C-E=S3)10 of facial swelling (Fig. 1). These assessments were carried out by an independent observer who was blinded to the technique used for removal of the impacted tooth.
Fig. 1.
Markings for facial swelling.
Patients were asked to rinse the oral cavity with 2% povidone-iodine solution 5 min prior to the procedure. All procedures were performed by a single surgeon under local anesthesia blockade of an inferior alveolar nerve (IAN) and long buccal nerve block using 2% lidocaine hydrochloride with 1:80,000 adrenaline. A standard ward's incision with distal extension was placed and full thickness mucoperiosteal flap was reflected to expose the impacted tooth and surrounding bone. Tooth/root sectioning, whenever required was performed on both sides. For bur group, a tungsten Carbide round bur no. 8 and straight bur no 702 mounted on a surgical straight handpiece at 22,000 rpm was used for ostectomy at the buccal and distal aspect of the tooth.
The cutting of the bone was always supplemented by copious irrigation with 0.9% NS. For a piezo group, OT7 and OT2 (Mectron®) cutting inserts were used for bone guttering around the impacted tooth. The frequency was regulated at 28–36 kHz with amplitude alternating between 30 and 60 ??m/s. The wound closure was achieved by placing 2 sutures using 3-0 black braided silk suture. The operative time was recorded using a digital stopwatch from the point of placement of incision till the commencement of sutures. Postoperatively, all the patients were prescribed Tab Amoxicillin with clavulanic acid 625 mg, 12 hourly, Tab paracetamol 650 mg 8 hourly for 5 days.
The postoperative follow up was scheduled on the 2nd day and later on the 7th day. An independent observer who was blinded to the technique used for ostectomy measured the swelling, trismus, soft tissue, and nerve injury. Postoperative pain was evaluated using 10 unit Visual Analogue Scale (VAS) together with a graphics rating scale.11 Patients were asked to rate the postoperative pain till the first six postoperative days at the same time during the days and submit it on the 7th operative day.
Neurosensory evaluation of inferior alveolar and a lingual nerve was checked on 2nd and 7th operative days subjectively by asking the patient to report any prolonged hyperesthesia, hypoesthesia, paresthesia, anesthesia persisting even after weaning of local anesthetic effect. Subjective findings for neurosensorial integrity of IAN and lingual nerve were confirmed by performing objective signs such as light touch (cotton wisp) and two-point discrimination test over the ipsilateral side of the lower lip in sitting position with closed eyes and probing with an atraumatic blunt probe over the lingual gingivae and lateral border of the tongue of the ipsilateral side respectively.
Soft tissue injury was defined as any injury to the reflected flap mucosa, periosteum, muscle, tongue including thermal injury to the adjoining structures. The second surgical intervention was carried out on the contralateral side after a washout period of 21 days.
All the data was recorded and tabulated in an MS Excel sheet. Descriptive and analytical statistics were done using SPSS Version 24.0 (IBM Corporation, Chicago, USA) 2016. The normality of data was analyzed by the Shapiro-Wilk test. The independent sample t-test was used to check to mean differences between the sides. The chi-square test was used to check differences in proportions. Statistical significance was established at p < 0.05.
2. Results
There were no dropouts in the present study sample. It consisted of 42 Male and 18 Female with a mean age of the 24.90 ± 3.93 years (range 20–30 years). Each group comprised of 18 (60%) vertical and 12 (40%) mesioangular teeth. The data suggested that the operative time taken for impacted mandibular third molar surgery for bur group was lower (77.53 ± 16.94 min) compared to piezo group (108.66 ± 21.12 min) exhibiting significant statistical difference (p < 0.001). The bur group had 36.7% (n = 11) subjects who experienced soft tissue injury compared to none (n = 0) in the piezo group. Significant statistical differences (p < 0.001) existed in soft tissue injuries between the two groups.
The postoperative pain varied significantly throughout between the two sides. The mean of post-operative pain score for bur group at day 2nd was higher (5.56 ± 1.04) compared to piezo group (4.33 ± 0.75). Similar differences were also found at day 7th in bur and piezo group (3.93 ± 1.22) and (2.90 ± 0.92) respectively. A significant difference (p < 0.001) existed between the two groups (Table 1).
Table 1.
Comparison of Postoperative pain on day 2 and day 7 between the two groups.
| VAS | Groups | Mean | S.D. | P-Value |
|---|---|---|---|---|
| Day 2 | Bur | 5.56 | 1.04 | <0.001 |
| Piezo | 4.33 | 0.75 | ||
| Day 7 | Bur | 3.93 | 1.22 | 0.001 |
| Piezo | 2.90 | 0.92 |
P-value derived from paired Chi-square test, significant at p < 0.05.
The mean scores of postoperative swelling at 2nd and 7th day in the peizo group (10.22 ± 0.66 and 9.53 ± 1.03) was found to be significantly lower than the bur group 10.97 ± 0.86, 10.00 ± 0.70 respectively revealing significant difference (p < 0.001). (Table 2).
Table 2.
Comparison of postoperatively facial swelling in two groups.
| Days | Mean |
P-Value | |
|---|---|---|---|
| Peizo | Bur | ||
| Baseline (Pre-op) | 9.11 (±0.74) | ||
| Post-op Day 2 | 10.22 (±0.66) | 10.97 (±0.86) | <0.001 |
| Post-op Day 7 | 9.53 (±1.03) | 10.00 (±0.70) | |
P-value derived from paired Chi-square test.
significant at p < 0.05.
A similar trend was observed in the mean scores of postoperative trismus on 2nd and 7th day. In the peizo group (34.18 ± 3.3 and 38.40 ± 3.7) was found to be significantly less than the bur group (30.27 ± 3.5 and 35.51 ± 4.1) on the 2nd and 7th postoperative days respectively exhibiting significant difference (p < 0.001)(Table 3). Postoperatively, none of the subjects reported with hypoesthesia, anesthesia, hyperesthesia or paresthesia in the two groups.
Table 3.
Comparison of postoperative trismus between the two groups.
| Days | Mean |
P-Value | |
|---|---|---|---|
| Peizo | Bur | ||
| Baseline (Pre-op) | 42.20 ± 1.24 | ||
| Post-op Day 2 | 34.18 ± 3.3 | 30.27 ± 3.5 | <0.001 |
| Post-op Day 7 | 38.40 ± 3.7 | 35.51 ± 4.1 | |
P-value derived from paired Chi-square test.
significant at p < 0.05.
3. Discussion
Pain, trismus, and swelling are immediate and direct sequelae of IM3M removal procedure which adversely affects the postoperative quality of life of an individual. Numerous therapeutic protocols have been into practice to reduce the inflammatory outcomes which include the use of various medications, non-pharmacological applications, improved instrumentations for ostectomy, flap designs and wound closure techniques.13 The latest addition to the inventory of armamentarium is the piezoelectric surgery, an innovative osteotomy technique employing the micro-vibrations of the inserts at an ultrasonic frequency to selectively perform precise osteotomies, sparing the soft tissues and neurovascular structures. The present study was aimed to compare piezosurgery with bur for ostectomy in terms of evaluation of pain, swelling, trismus, paresthesia and soft tissue injuries during IM3M removal.
In the present study, we selected a homogenous sample having asymptomatic bilateral symmetrically oriented IM3M having similar angulations, depth, relationship with ramus and similar difficulty scores taking into account the fact that, age and position of the tooth can influence postoperative outcomes.
The operative time has a bearing on the postoperative outcomes. Extended surgeries or increased duration of surgery is proportional to the complications like decreased patient compliance, fatigue, trauma due to retraction of soft tissue injuries and increased postoperative pain. In the present study, the operative time was significantly less with bur as compared to piezo. This can be partly attributed to the slower micrometric cutting action and partly to a definite, albeit, small learning curve.14 The extended operative time was requisite especially in earlier cases, it gradually reduced as the operator gained experience. However, due to reduced noise and vibrations, it is preferred by the patients in spite of increased operating time.15 The outcomes of our study are in lieu of the results of studies published earlier.9,16,17
The magnitude of pain, swelling, and trismus are critically influenced by the synthesis of various mediators of inflammation, prostaglandin E2, and bradykinin. Postoperative pain was measured with VAS, at the same time during day 1 to day 7 postoperatively. In comparison, a significant difference was noted in mean pain scores, with pain being experienced more on the side where bur was used. Lesser pain experienced with piezo can be attributed to its mineralized tissue-specific, micrometric and precise cutting which causes less tissue damage sparing the soft tissues, and neurovascular structures.8,18,19
Facial swelling is a direct result of surgical trauma to the investing tissues of 3M region. The onset is gradual and attains peak at the conclusion of 24–48 h and even can last up to 7 days.11,20 It was measured on both sides by a sum of linear measurements obtained from predetermined fixed points on 2nd and 7th postoperative days. The results showed that there was significantly decreased swelling on the piezo side compared to bur with statistically significant differences on both the days.
Trismus is proportional to pain and swelling. Subjects experiencing a marked reduction of mouth opening during the early postoperative days is due to inflammatory tissue reaction and the pain perceived. Trismus was calculated by measuring interincisal opening on the 2nd and 7th days. The results showed that, after the surgical procedure, range of mouth opening (inter-incisal distance) was significantly greater in a piezo group compared to the bur group on postoperative days 2nd and 7th.
Due to its selective affinity of cutting in highly mineralized structures such as bone and tooth, there is a nominal risk of neurological complications with the use of piezosurgery for ostectomy in IM3M surgery.21 There was no occurrence of postoperative paresthesia or anesthesia or dysesthesia or hyperesthesia in any of the cases with the use of either of the ostectomy techniques.
None of the subjects had an occurrence of soft tissue injury in the peizo group, however, the bur group had 36.7% (n = 11) subjects who sustained injuries during the procedure. Selective cutting of mineralized structures, salvaging soft tissues including neurovascular structures act as the unique advantage of using piezo, thereby not inflicting any injury to soft tissues. In contrast, burs inflict thermal insults due to overheating and furthermore have marked potential to cause iatrogenic inadvertent soft tissue injury during the surgical procedure.22 Apart from high cost, the shortcomings of piezosurgery are extended operating time, as a result of the slow cutting rate and the high possibility of breaking the surgical inserts.9,23
Piezoelectric surgery is a relatively novel technique of osteotomy employing micro-vibrations at ultrasonic frequency generating its distinctive microstreaming and cavitation features. The microstreaming is created by an uninterrupted whirling movement of fluids generated by a small vibrating insert that facilitates mechanical dislodgement of debris. The cavitational phenomenon, activated by an implosion of gas bullae onto blood vessels during ostectomy, yield an essential hemostatic effect enhancing visualization of the operative field to perform efficient bone cutting when compared to bur.6
Volumetric analysis was desirable for the assessment of postoperative facial swelling. Also, anxiety levels and postoperative quality of life assessment would have imparted an impactful conclusion to the study conducted and can be considered as limitations of the study. Furthermore, the present study did not take into consideration the breakage of cutting inserts which could incur and escalate the cost of treatment and may pose a financial burden. Future studies should be engaged at multicentric levels considering the aforementioned recommendations.
4. Conclusion
Piezosurgery is a novel and superior alternative in surgical removal of third molars as it is more efficient in terms of pain, swelling, trismus, and soft tissue injuries. However, it is more time consuming but the operative time is reduced after a definite, albeit small learning curve.
Contributor Information
Chirag Patil, Email: chiragpatil1275@gmail.com.
Anendd Jadhav, Email: anendd.j@gmail.com.
Rajanikanth K, Email: rajanikanthmalviya@gmail.com.
Nitin Bhola, Email: drnitinbhola@gmail.com.
Rajiv M. Borle, Email: vcdmimsdu@gmail.com.
Apoorva Mishra, Email: drmishraapoorva@gmail.com.
References
- 1.Eshghpour M., Nejat A.H. Dry socket following surgical removal of the impacted third molar in an Iranian population: incidence and risk factors. Niger J Clin Pract. 2013 Dec;16(4):496–500. doi: 10.4103/1119-3077.116897. [DOI] [PubMed] [Google Scholar]
- 2.Preti G., Martinasso G., et al. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007 Apr;78(4):716–722. doi: 10.1902/jop.2007.060285. [DOI] [PubMed] [Google Scholar]
- 3.Praveen G., Rajesh P., et al. Comparison of morbidity following the removal of mandibular third molar by lingual split, surgical bur and simplified split bone technique. Indian J Dent Res. 2007 Jan 1;18(1):15. doi: 10.4103/0970-9290.30916. [DOI] [PubMed] [Google Scholar]
- 4.Sortino F., Pedullà E., Masoli V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: comparison of postoperative recovery. J Oral Maxillofac Surg. 2008 Dec;66(12):2444–2448. doi: 10.1016/j.joms.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Eggers G., Klein J., et al. Piezosurgery: an ultrasound device for cutting bone and its use and limitations in maxillofacial surgery. Br J Oral Maxillofac Surg. 2004 Oct;42(5):451–453. doi: 10.1016/j.bjoms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Vercellotti T. Technological characteristics and clinical indications of piezoelectric bone surgery. Minerva Stomatol. 2004 May;53(5):207–214. [PubMed] [Google Scholar]
- 7.Robiony M., Polini F., Costa F., Vercellotti T., Politi M. Piezoelectric bone cutting in multipiece maxillary osteotomies. J Oral Maxillofac Surg. 2004 Jun;62(6):759–761. doi: 10.1016/j.joms.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Tasveer Fatima D.T.F. Piezoelectric ostectomy: a new technique for impacted third molar surgery. IOSR J Dental Med Sci (IOSR-JDMS. 2015 Sep;14:103–107. 9 Ver. IV (Sep. 2015) [Google Scholar]
- 9.Goyal Manoj, Marya k., Jhamb a., et al. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a piezotome or a conventional handpiece: a prospective study. Br J Oral Maxillofac Surg. 2012;50(6):556–561. doi: 10.1016/j.bjoms.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Arakji H., Shokry M., Aboelsaad N. Comparison of piezosurgery and conventional rotary instruments for removal of impacted mandibular third molars: a randomized controlled clinical and radiographic trial. Int J Dentistry. 2016;2016 doi: 10.1155/2016/8169356. 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartuli F.N., Luciani F., Caddeo F., et al. Piezosurgery vs High-Speed Rotary Handpiece: a comparison between the two techniques in the impacted third molar surgery. Oral Implantol (Rome) 2013;6(1):5–10. [PMC free article] [PubMed] [Google Scholar]
- 12.Sivolella S., Berengo M., et al. Osteotomy for lower third molar germectomy: randomized prospective crossover clinical study comparing piezosurgery and conventional rotatory osteotomy. J Oral Maxillofac Surg. 2011 Jun;69(6):e15–23. doi: 10.1016/j.joms.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 13.Graziani F., D'Aiuto F., et al. Perioperative dexamethasone reduces post-surgical sequelae of wisdom tooth removal. A split-mouth randomized double-masked clinical trial. Int J Oral Maxillofac Surg. 2006 Mar;35(3):241–246. doi: 10.1016/j.ijom.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Beziat J.-L., Bera J.-C., et al. Ultrasonic osteotomy as a new technique in craniomaxillofacial surgery. Int J Oral Maxillofac Surg. 2007 Jun;36(6):493–500. doi: 10.1016/j.ijom.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Stübinger S., Kuttenberger J., Filippi A., Sader R., Zeilhofer H.-F. Intraoral piezosurgery: preliminary results of a new technique. J Oral Maxillofac Surg. 2005 Sep;63(9):1283–1287. doi: 10.1016/j.joms.2005.05.304. [DOI] [PubMed] [Google Scholar]
- 16.Piersanti L., Dilorenzo M., Monaco G., Marchetti C. Piezosurgery or conventional rotatory instruments for inferior third molar extractions? J Oral Maxillofac Surg. 2014;72(9):1647–1652. doi: 10.1016/j.joms.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 17.Mantovani E., Arduino P.G., et al. A split-mouth randomized clinical trial to evaluate the performance of piezosurgery compared with a traditional technique in lower wisdom tooth removal. J Oral Maxillofac Surg. 2014 Oct;72(10):1890–1897. doi: 10.1016/j.joms.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Bhati B., Kukreja P., Kumar S., Rathi V.C., Singh K. Piezosurgery versus rotatory osteotomy in mandibular impacted third molar extraction. Ann Maxillofac Surg. 2017;7(1):5–10. doi: 10.4103/ams.ams_38_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rullo R., Addabbo F., Papaccio G. Piezoelectric device vs. conventional rotative instruments in impacted third molar surgery: relationships between surgical difficulty and postoperative pain with histological evaluations. J Cranio-Maxillo-Fac Surg. 2013 Mar;41(2) doi: 10.1016/j.jcms.2012.07.007. e33-3. [DOI] [PubMed] [Google Scholar]
- 20.Troedhan A., Kurrek A. Ultrasonic piezotome surgery: is it a benefit for our patients and does it extend surgery time? A retrospective comparative study on the removal of 100 impacted mandibular 3rd molars. Open J Stomatol. 2011 Dec 7;01:179. [Google Scholar]
- 21.Itro A., Lupo G., Marra A., et al. The piezoelectric osteotomy technique compared to the one with rotary instruments in the surgery of included third molars. A clinical study. Minerva Stomatol. 2012 Jun;61(6):247–253. [PubMed] [Google Scholar]
- 22.Chang H.-H., Lee M.-S., Hsu Y.-C., Tsai S.-J., Lin C.-P. Comparison of clinical parameters and environmental noise levels between regular surgery and piezosurgery for extraction of impacted third molars. J Formos Med Assoc. 2015 Oct;114(10):929–935. doi: 10.1016/j.jfma.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Al-Moraissi E.A., Elmansi Y.A., Al-Sharaee Y.A. Does the piezoelectric surgical technique produce fewer postoperative sequelae after lower third molar surgery than conventional rotary instruments? A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016 Mar;45(3):383–391. doi: 10.1016/j.ijom.2015.10.005. [DOI] [PubMed] [Google Scholar]