Abstract
Purpose:
Plantar fasciitis (PF) is characterized by the degeneration of the plantar fascia, leading to heel pain. We aimed to investigate the effectiveness of extracorporeal shock wave therapy (ESWT) and custom foot orthotics (CFO).
Method:
The study was planned as a prospective randomized controlled study. In total, 83 patients were evaluated. The patients were divided into two groups: patients treated with ESWT (group I, n=40) and patients treated with CFO (group II, n=43). Visual analogue scale (VAS) was used to evaluate pain in the morning, evening, at rest and while walking. Foot Function Index (FFI) was used to evaluate foot functions, and Foot Health Status Questionnaire (FHSQ) was used to evaluate foot health.
Results:
Both group I and group II achieved significant improvements in our evaluation parameters (morning and evening pain) at 4, 12 and 24 weeks compared with their baseline values (P<0.001), and significant improvement observed in the group II continued at 48 weeks (P<0.05); however, there was no significant difference in some parameters in the group I after treatment compared with their baseline values (P>0.05).
Conclusion:
Both treatment ESWT and CFO can use interchangebably. Neither method was superior in treating plantar fasciitis
Keywords: Plantar Fasciitis, ESWT, CFO Insoles, Foot Pain
Introduction
Plantar fasciitis (PF) is a degenerative abnormality of the plantar fascia and is one of the most common causes of heel pain[1]. The pain is excessive in the morning; it increases with long durations of standing and walking[2-4]. It is frequently reported that heel pain may be severe and may spread to the entire plantar fascia[1]. Plantar fasciitis is primarily a clinical diagnosis. Classic physical examination findings suggestive of plantar fasciitis include reproducible pain with palpation of the plantar medial aspect of the heel and pain with passive dorsiflexion of the ankle and toes (windlass test)[5]. Diagnostic imaging is not recommended for the initial evaluation of plantar fasciitis[6].
However, some diagnostic imaging techniques may be required to rule out other considerations in the differential diagnosis. This typically affects people between the age of 40 and 60 years and can be observed in both the active and the sedentary individuals[7,8]. Although its aetiology is unclear, it is more common in obese people, people who stay in standing position for a long time and in runners[9]. It is also believed that factors, such as trauma, inappropriate shoe use, decreased ankle dorsiflexion, disruption in biomechanical factors of the foot and flat-footedness contribute to PF[10]. Approximately, it occurs in 10% of the general population[7]. PF treatment may involve conservative approach or surgery. Conservative treatment is aimed at reducing pain, controlling inflammation, accelerating healing and ensuring a soft mobilization (etc walking with proper footwear) of the patient in daily life activities. Therefore, conservative treatments are often symptom-oriented, and various methods and treatment approaches are used to reduce pain, which is the most prominent symptom. Commonly used conservative methods include steroid injection[11], ultrasound therapy[12], laser therapy[13], Extracorporeal short wave therapy ESWT[14], the use of orthotic supports[15] and exercise and stretching therapy with proper footwear[16]. ESWT has been widely used as PF treatment over the last 10-15 years, and numerous clinical studies have been reported positive results on function and/or pain[17-19]. ESWT therapy consists of sound waves that are directed to affected tissues. The proposed mechanisms of action include: stimulating blood flow for a beneficial immune and inflammatory response, reinjuring tissues to stimulate healing, and shutting down the neuronal pain pathways through the pulses hitting the affected nerves[20]. Similarly night splints, orthoses and insoles have been used for many years, and many studies have reported successful results[21,22]. There are different theoretical models on the potential working mechanism of orthotic devices. The most common theory is that orthotic devices optimize the biomechanical loading of the foot, specifically to decrease excessive pronation, to off-load the plantar fascia at its origin and to recreate the heel pad[23]. Both ESWT and orthoses treatment generally have successful results in itself (etc MRI results in ESWT treatment)A literature search on the Pubmed Medline online database (http://www.ncbi.nlm.nih.gov/pubmed/) database using the key words “shock wave or ESWT, custom-made foot orthotic or CFO, Plantar fasciitis or PF”, yielded no other specific study.
However, a comparative study of both methods was not found in the literature review. Our aim is to use these two widely used methods in patients with PF and to compare their effectiveness with each other.
Material and methods
The study was planned as a prospective randomized controlled study. The study was conducted in accordance with the World Medical Association Declaration of Helsinki and the Guideline for Good Clinical Practice. The study protocol was approved by the local ethics committee and all the participants provided written informed consent. In total, 83 patients (68 females and 15 males) including 66 patients with unilateral and 17 patients with bilateral PF treated between September 2014 and July 2017 were included in the study. Participants were randomly assigned by the study biostatistician, who was not involved in the outcome measure. This randomization was achieved by assigning participants to either the programmed ESWT group (group A) or CFO group (group B) with equal probability within randomly permuted blocks of size 2, 4, and 8. [Figure 1] shows the chart containing patients’ records.
Figure 1.
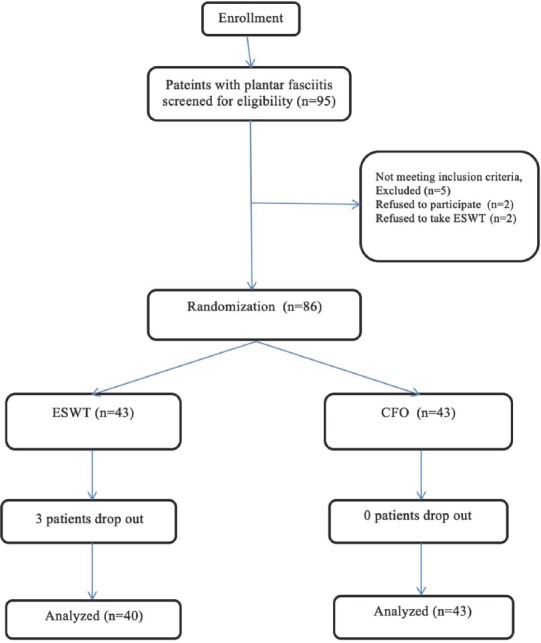
Flowchart diagram for the participants who were randomized into two groups as receiving ESWT and CFO.
PF was diagnosed using physical examination and patient history. In addition, lateral foot-ankle graphs were obtained. Patients aged 30-60 years, who had pain and sensitivity in the sole, were diagnosed with PF, experienced persistent heel pain while walking and showed abnormal foot pronation due to pain, were included in the study. Patients who had traumatic injuries in their feet in the past six months, experienced neurological heel pain, had foot bursitis, had undergone a previous surgery for PF, had walking problems due to joint problems, and those in whom the use or application of ESWT and CFO was contraindicated were excluded from the study. All patients were instructed not to use NSAID (Nonsteroidal anti-inflammatory drug) during the treatment and control periods. Information regarding the study procedure was provided to all patients.
Study groups
Patients treated with ESWT were assigned to group I (n = 40), and patients treated with CFO were assigned to group II (n = 43). In the ESWT group (group I, 40 PF), patients received three sessions of ESWT at one session per week. EMS brand (Swiss Dolor Clast®, EMS; Nyo, Switzerland) ESWT device with radial shockwave probe was used in each session delivering 2,000 pulses at 12-Hz frequency and 2.0-bars pressure. The application was performed in the supine position, where five most sensitive and painful points were determined and 400 pulses were delivered to each point. No local anaesthetic or analgesic medication was administered before or during the application. In the CFO group (group II, 43 PF), foot measurements were obtained using casting bandage and were created positive model. Then we constituted insoles with longitudinal arc support that is consist of 1-mm-thick polyethylene thermoplastic insoles were covered with soft polyphorm (Figure 2). The patients were asked to use these insoles in their shoes for at least 4 weeks during the treatment. Patients were asked to use their insoles for at least 6 hours per day. During the first week, six patients reported discomfort with the insoles. In our unit, the insoles were modified so that the patients could comfortably use the insoles. Both groups were recommended with plantar stretching exercise, gastrocnemius stretching twice a day, ten repeated for one month. All patients were controlled twice a week in outpatient clinic every other two week
Figure 2.

Illustration of the custom foot orthosis provided to the participant.
Measurement parameters
Patients were assessed in terms of pain at rest, during walking, in the morning and evening and foot functions and foot health. The same therapist was blinded and generating a random allocation sequence include using a computer software program that generates the random sequence. https://www.random.org/sequences/?min=1&max=100&col=2&format=html&rnd=new to ensure randomization. Evaluation data were obtained at pre-treatment week (0) and post-treatment weeks (4, 12, 24 and 48 weeks). To assess pain at rest, while walking, in the morning and in the evening, a 10-cm-long visual analogue scale VAS (0 indicating no pain and 10 indicating the most severe pain) was used. The Foot Function Index Revised (FFI-R) was used to evaluate foot functions[24,25]. This index examines foot insufficiency with three sub-parameters (foot pain, insufficiency and activity restriction) on a scale of 0 to 10 (0 indicating no pain and 10 indicating the most severe pain); low scores indicate better function The Turkish validity and reliability study of this index has been conducted by Yalıman et al.[23], and it was emphasized that this scale be used to evaluate foot problems. The Foot Health Status Questionnaire (FHSQ) was used to evaluate foot health. The questionnaire comprises the following sub-parameters: (FP) foot pain, (FF) foot function, (FW) footwear used, (GFH) general foot health, (GH) general health, (PA) physical activity, (SC) social capacity and (V) vigour. Each parameter is scored on a scale of 0-100; higher scores indicate better functions[26]. While two female and one male patient in the ESWT group could not complete the treatment, all the patients in the CFO group continued the study until the end of the treatment. Patients who did not complete the treatment were not followed-up, and their data were excluded from the study.
Statistical analysis
SPSS 15.0 (Chicago, USA) statistical package program for windows was used for the statistical analysis of the research data. Quantitative variables were expressed as mean ± standard deviation, whereas categorical variables were expressed as number and percentage (%). The normal distribution of the data was examined. Independent t-test was used in the paired comparison of variables in the ESWT and CFO groups with normal distribution at weeks 4, 12, 24 and 48. Mann-Whitney U-test was used for the comparison of the variables that were not normally distributed. The analysis of variance was used for the comparison of repeated measurements in the ESWT and CFO groups at weeks 0, 4, 12, 24 and 48. Chi-square (χ2) analysis was used for intergroup comparisons of qualitative variables. Hypotheses were bidirectional, and P<0.05 was considered statistically significant.
Results
During the study period, no unfavourable situation (reddening of the skin, pain, small haematomas) was observed in the ESWT and CFO groups. There was no statistically significant difference in the pre-treatment demographic characteristics and evaluation parameters between the two groups (Table 1).
Table 1.
Comparison of demographic characteristics between the ESWT and CFO groups.
| N=83 | ESWT (n=40) (mean±SD) (min-max) | CFO (n=43) (mean±SD) (min-max) | P |
|---|---|---|---|
| Age (year) | 48,84±9,77 (33/58) | 46,94±9,02 (31/56) | 0,822 |
| Gender, (male/female) | 7/33 | 8/35 | 0,846 |
| BMI | 27,51±1,98 | 28,34±2,36 | 0,698 |
| Duration of foot pain, (week) | 9,1±4,53 (4-15) | 9,8±4,93 (5-17) | 0,457 |
| Affected side (n (%)) | |||
| Bilateral | 8(47%) | 9(53%) | 0,837 |
| Unilateral: Right/left | 22/10 | 24/10 | |
| Employment (n (%)) | |||
| Housewife | 21 (52,5%) | 22 (51,1%) | 0,911 |
| Worker | 12 (30,0%) | 13 (30,2%) | 0,854 |
| Other | 7 (17,5%) | 8 (18,6%) | 0,713 |
MI, body mass index; SD, standard deviation.
VAS scores at rest and in the evening were found to be significant compared with pre-treatment scores (P<0.05). Moreover, VAS scores while walking and in the morning were found to be significant compared with pre-treatment scores (P<0.001). FFI scores at post-treatment weeks 4, 12, 24, and 48 were significantly improved compared with pre-treatment scores (P<0.001). The PA sub-score of FHSQ was significantly different at week 24 compared with pre-treatment score (P<0.05). There was no significant difference in FP, FF, GH and PA sub-scores at week 48 and pre-treatment scores (P>0.05). However, there were significant improvements in all other FHSQ sub-scores at weeks 4, 12, 24, and 48 compared with pre-treatment scores (P<0.001, Table 2).
Table 2.
The results and statistical comparisons of the pretreatment (week 0) and posttreatment (after 4, 12, 24 and 48 weeks) evaluation parameters in ESWT gro.
| N=40 | Baseline | 4th week | 12th week | 24th week | 48th week | P (baseline- 8th week) |
|---|---|---|---|---|---|---|
| VAS rest | 5,1±2,3* (4-8) | 3,9±1,7* (2-6) | 3,1±1,6* (1-6) | 3,7±1,5* (2-6) | 4,4±2,1* (3-6) | 0,045 |
| VAS walking | 7,2±2,3* (5-10) | 5,4±2,1* (3-8) | 5,1±2,1* (3-7) | 4,9±1,9* (3-7) | 5,5±2,1* (3-7) | <0.001 |
| VAS morning | 6,3±1,9* (5-10) | 5,1±1,7* (3-8) | 4,6±1,6* (3-7) | 4,4±1,7* (3-7) | 4,8±1,8* (4-8) | <0.001 |
| VAS evening | 7,3±2,3 (6-10) | 5,9±1,9* (4-8) | 5,4±1,8* (4-8) | 5,9±2,0* (4-9) | 6,2±2,1* (4-9) | 0,017 |
| FFI total score (34-136) | 78,3±24,5* | 65,2±20,5* | 62,8±19,9* | 62,4±19,4* | 66,4±21,1* | <0.001 |
| FHSQ, FP (0-100) | 36,1±21,5* | 54,8±19,3* | 58,8±25,3* | 51,2±18,7* | 40,4±19,3* | 0,311 |
| FHSQ, FF (0-100) | 48,6±21,7* | 71,9 ±19,8* | 74,3±24,5* | 70,5±20,8* | 54,3±19,8* | 0,421 |
| FHSQ, FW (0-100) | 34,4±16,6* | 42,8±18,7* | 44,1±18,4* | 45,6±19,1* | 43,3±18,7* | <0.001 |
| FHSQ, GFH (0-100) | 17,8±17,4 | 29,1±18,4* | 32,4±23,6* | 32,6±25,3* | 29,5±25,3* | <0.001 |
| FHSQ, GH (0-100) | 55,4±26,8 | 64,7±27,6* | 67,4±26,1* | 65,6±25,6* | 61,6±23,4* | 0,112 |
| FHSQ, PA (0-100) | 54,4±22,6 | 65,1±24,5* | 64,5±23,9* | 61,6±21,9 | 58,7±20,9 | 0,507 |
| FHSQ, SC (0-100) | 57,6±23,7 | 73,4±25,5* | 74,3±22,8* | 76,2±23,1* | 74,0±23,1* | <0.001 |
| FHSQ, V (0-100) | 41,6±19,4 | 57,0±19,7* | 55,2±18,9* | 54,7±19,3* | 52,7±18,3* | <0.001 |
VAS, Visual Analog Scale; (lower score indicating better function). FFI-R Revised Foot Function Index; (lower score indicating better function). FHSQ, Foot Health Status Questionnaire (FP Foot pain, FF Foot function, FW Footwear, GFH General foot health, GH General health, PA Physical activity, SC Social capacity and V Vigor) (higher score indicating better function).
VAS pain scores of patients in the CFO group at rest, while walking, in the morning and in the evening were significant difference at week 24 and at week 48 (P<0.001) (Table 3).
Table 3.
The results and statistical comparisons of the pretreatment (week 0) and posttreatment (after 4, 12, 24 and 48 weeks) evaluation parameters in CFO group.
| N=40 | Baseline | 4th week | 12th week | 24th week | 48th week | P (baseline- 48th week) |
|---|---|---|---|---|---|---|
| VAS rest | 5,4±2,2 (4-8) | 4,1±1,8 (3-6) | 3,1±1,8 (1-5) | 3,4±1,7 (2-6) | 3,7±1,9 (2-6) | <0.001 |
| VAS walking | 7.4±2,1 (5-10) | 5,3±2,0 (3-8) | 4,8±1,9(2-7) | 4,2±1,6 (2-7) | 4,1±1,7 (2-6) | <0.001 |
| VAS morning | 6,6±1,8 (5-10) | 5,2±1,8 (3-8) | 4,4±1,6 (3-7) | 3,9±1,5 (2-7) | 4,1±1,5 (3-7) | <0.001 |
| VAS evening | 7,5±2,1 (6-10) | 5,8±2,1 (4-8) | 5,0±1,8 (3-8) | 4,7±1,8 (3-7) | 4,5±1,7 (3-7) | <0.001 |
| FFI total score (34-136) | 82,5±22,9 | 63,9±21,1 | 59,3±19,7 | 55,2±18,7 | 51,8±18,1 | <0.001 |
| FHSQ, FP (0-100) | 34,4±20,4 | 56.9±20,1 | 61,8±23,4 | 60,2±20,2 | 56,2±22,1 | <0.001 |
| FHSQ, FF (0-100) | 51,3±21,3 | 74,9±17,3 | 78,1±18,1 | 80,2±17,9 | 73,0±16,9 | <0.001 |
| FHSQ, FW (0-100) | 32,7±15,4 | 43,2±20,1 | 46,8±20,8 | 47,5±20,7 | 44,7±19,8 | <0.001 |
| FHSQ, GFH (0-100) | 18,6±17,8 | 31,6±20,5 | 37,7±26,3 | 40,6±28,8 | 39,6±27,8 | <0.001 |
| FHSQ, GH (0-100) | 56,2±24,6 | 66,2±25,3 | 69,8±25,7 | 69,9±26,2 | 64,9±25,2 | 0,004 |
| FHSQ, PA (0-100) | 51,2±21,5 | 68,4±21,4 | 73,7±22,3 | 71,4±23,3 | 70,1±21,8 | <0.001 |
| FHSQ, SC (0-100) | 59,4±23,1 | 75,3±25,1 | 76,7±24,2 | 77,1±22,3 | 75,1±22,1 | <0.001 |
| FHSQ, V (0-100) | 44,4±18,6 | 57,7±21,5 | 58,9±19,3 | 59,1±20,7 | 62,8±21,6 | <0.001 |
VAS, Visual Analog Scale; (lower score indicating better function). FFI-R Revised Foot Function Index; (lower score indicating better function). FHSQ, Foot Health Status Questionnaire (FP Foot pain, FF Foot function, FW Footwear, GFH General foot health, GH General health, PA Physical activity, SC Social capacity and V Vigor) (higher score indicating better function).
In addition, there were significant differences in FFI scores at weeks 4, 12, 24, and 48 post-treatment and pre-treatment scores (P<0.001).
The GH sub-score of FHSQ was significantly different only at week 48 compared with pre-treatment score (P>0.05). All other FHSQ sub-parameter scores (FP, FF, FW, GFH, GH, PA, SC and V) were significantly different at weeks 4, 12, 24, and 48 compared with pre-treatment scores (P<0.001; Table 3).
There were no significant differences in the ESWT and CFO groups between findings at week 0 and week 4 (P>0.05). At post-treatment week 12, the PA sub-parameter of FHSQ was significantly different in favour of the CFO group (P<0.05). There was no significant difference in other parameters (P>0.05). At post-treatment week 24, there was a significant difference in evening VAS and FP, FF, GFH and PA sub-parameters of FHSQ in favour of the CFO group (P<0.05). There was no significant difference in other parameters (P>0.05). At post-treatment week 48, there was a highly significant difference in walking and evening VAS scores; FFI total scores and FP, FF and PA sub-parameters of FHSQ in favour of the CFO group (P<0.001). In addition, there was a significant difference in FP, FF and PA sub-parameters of FHSQ in favour of the CFO group (P<0.05). There was no significant difference in other parameters (P>0.05) (Table 4).
Table 4.
Comparison of the ESWT group and CFO group on the basis of the Pretreatment (0 week) and the posttreatment (after 4, 12, 24 and 48 weeks).
| ESWT group (Baseline) | CFO group (Baseline) | ESWT group 4th week | CFO group 4th week | ESWT group 12th week | CFO group 12th week | ESWT group 24th week | CFO group 24th week | ESWT group 48th week | CFO group 48th week | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| VAS rest | 5,1±2,3 (4-8) | 5,4±2,2 (4-8) | 3,9±1,7 (2-6) | 4,1±1,8 (3-6) | 3,1±1,6 (1-6) | 3,1±1,8 (1-5) | 3,7±1,5 (2-6) | 3,4±1,7 (2-6) | 4,4±2,1 (3-6) | 3,7±1,9 (2-6) | 0,096 |
| VAS walking | 7,2±2.3 (5-10) | 7.4±2,1 (5-10) | 5,4±2,1 (3-8) | 5,3±2,0 (3-8) | 5,1±2,1 (3-7) | 4,8±1,9 (2-7) | 4,9±1,9 (3-7) | 4,2±1,6 (2-7) | 5,5±2,1 (3-7) | 4,1±1,7 (2-6) | <0.001 |
| VAS morning | 6,3±1,9 (5-10) | 6,6±1,8 (5-10) | 5,1±1,7 (3-8) | 5,2±1,8 (3-8) | 4,6±1,6 (3-7) | 4,4±1,6 (3-7) | 4,4±1,7 (3-7) | 3,9±1,5 (2-7) | 4,8±1,8 (4-8) | 4,1±1,5 (3-7) | 0,068 |
| VAS evening | 7,3±2,3 (6-10) | 7,5±2,1 (6-10) | 5,9±1,9 (4-8) | 5,8±2,1 (4-8) | 5,4±1,8 (4-8) | 5,0±1,8 (3-8) | 5,9±2,0 (4-9) | 4,7±1,8 (3-7) | 6,2±2,1 (4-9) | 4,5±1,7 (3-7) | <0.001 |
| FFI total | 78,3± 24,5 | 82,5±22,9 | 65,2 ±20,5 | 63,9±21,1 | 62,8±19,9 | 59,3±19,7 | 62,4±19,4 | 55,2±18,7 | 66,4±21,1 | 51,8±18,1 | <0.001 |
| FHSQ, FP | 36,1±21,5 | 34,4±20,4 | 54,8±19,3 | 56.9±20,1 | 58,8±25,3 | 61,8 ±23,4 | 51,2±18,7 | 60,2±20,2 | 40,4±19,3 | 56,2±22,1 | <0.001 |
| FHSQ, FF | 48,6±21,7 | 51,3±21,3 | 71,9 ±19,8 | 74,9±17,3 | 74,3±24,5 | 78,1±18,1 | 70,5±20,8 | 80,2±17,9 | 54,3±19,8 | 73,0±16,9 | <0.001 |
| FHSQ, FW | 34,4±16,6 | 32,7±15,4 | 42,8±18,7 | 43,2±20,1 | 44,1±18,4 | 46,8±20,8 | 45,6±19,1 | 47,5±20,7 | 43,3±18,7 | 44,7±19,8 | 0,782 |
| FHSQ, GFH | 17,8±17,4 | 18,6±17,8 | 29,1±18,4 | 31,6±20,5 | 32,4±23,6 | 37,7±26,3 | 32,6±25,3 | 40,6±28,8 | 29,5±25,3 | 39,6±27,8 | 0,009 |
| FHSQ, GH | 55,4±26,8 | 56,2±24,6 | 64,7±27,6 | 66,2±25,3 | 67,4±26,1 | 69,8±25,7 | 65,6±25,6 | 69,9±26,2 | 61,6±23,4 | 64,9±25,2 | 0,184 |
| FHSQ, PA | 54,4±22,6 | 51,2±21,5 | 65,1±24,5 | 68,4±21,4 | 64,5±23,9 | 73,7±22,3 | 61,6±21,9 | 71,4±23,3 | 58,7±20,9 | 70,1±21,8 | <0.001 |
| FHSQ, SC | 57,6±23,7 | 59,4±23,1 | 73,4±25,5 | 75,3±25,1 | 74,3±22,8 | 76,7±24,2 | 76,2±23,1 | 77,1±22,3 | 74,0±23,1 | 75,1±22,1 | 0,816 |
| FHSQ, V | 41,6±19,4 | 44,4±18,6 | 57,0±19,7 | 57,7±21,5 | 55,2± 18,9 | 58,9±19,3 | 54,7±19,3 | 59,1±20,7 | 52,7±18,3 | 62,8±21,6 | 0,017 |
Discussion
In our study, we found that use of CFO was as effective as ESWT treatment. There are many conservative treatment modalities for PF because it is rather common in the general population, has a tendency to persist for months and is a disease that provokes significant disability in some of the cases[15]. Many studies have demonstrated the effectiveness of these modalities. In this study, we aimed to evaluate the effectiveness of ESWT and CFO in PF. Previous studies have focussed upon ESWT and CFO alone or have compared these to other modalities. However, to the best of our knowledge this is the first study comparing ESWT and CFO in PF. Thus, we believe that our study will guide the treatment and research of many clinicians and researchers while determining the most appropriate treatment modalities for the PF treatment.
As in similar studies, the majority of our patients were middle-aged and females[27]. Overweightness and obesity are the most common risk factors for PF[28,41]. The mean BMI in our patients was 27.51±1.98 kg/m2 in the ESWT and 28.34±2.36 kg/m2 in the CFO group, indicating that our patients are overweight or obese. Although reported both in the working and sedentary patients, the disease is more frequently observed in the working population[29]. The majority of the patients in the present study were working. The fact that there was no significant difference in the demographic, pain, clinical characteristics, foot functions and foot health data in both the groups before treatment was important for the homogeneity of the treatments. In our study, we evaluated the effectiveness of ESWT and CFO in PF short, at mid-term (4, 12, 24 weeks) and at long-term (48 weeks).
The most important finding of our study was that we found a significant improvement in the CFO group in the long-term (48 weeks) follow-up on several scales (walking and evening VAS; FFI-R total scores and FP, FF, GFH, PA and P sub-parameters of FHSQ) compared with that in the ESWT group. In the study conducted by Wrobel et al.[30] in which they evaluated the CFO use, the CFO group had significantly improved total FFI-R scores. CFO groups reported significantly lower morning and evening pain. In addition, they also reported significant improvements in the exercise program that gave to all groups, which is similar to our study in terms of pain and FFI-R. Yan W. et al.[31] conducted a study and used Eswt and CFO together, and reported more significant improvements in the pain scores; however, they also reported improvements in the groups which received only CFO and only ESWT). Riel et al.[32] compared 3 different exercises (isometric, isotonic, or walking) in 3 groups, and observed significant improvements in all groups, and reported the efficiency of exercise in relieving the pain.
Pain is the most important problem in patients with PF. Thus, VAS has been used as an evaluation scale in almost all studies of PF[33-35]. In our study, we evaluated VAS at four different time points in during daily life activities (at rest, while walking, in the morning and in the evening) in order to evaluate pain. As in other studies, we found significant improvements in both the ESWT and CFO groups in the short-, mid- and long-term follow-up compared with pre-treatment. FFI has been used in almost all studies to evaluate foot functions in the conservative treatment of patients with PF[21], [36]. We used FFI-R in our study and found significant improvements in FFI-R scores in both the ESWT and CFO groups in the short-, mid- and long-term follow-up compared with pre-treatment. We also used the FHSQ sub-parameters to assess foot health and found significant improvements in all parameters in the CFO group in the short-, mid- and long-term follow-up compared to pre-treatment. However, although we found significant improvement in short and mid-term follow-up in the ESWT group, we did not find a significant improvement in some parameters in long-term follow-up.
Several methods have been used in the conservative treatment of PF[11-16]. However, there is no consensus on the most successful conservative treatment[8,37,42]. In addition to the studies reporting that the combination of corticosteroid injection with exercise is the most efficient treatment, there are also some publications reporting that platelet rich plasma is more efficient than steroid injection in the long term[46-47].
ESWT was approved by the US Food and Drug Administration in 2000 for use in patients diagnosed with PF.[33]. It is emphasized that ESWT is commonly preferred over other treatment methods because it is non-invasive, because it is well tolerated by the patients and because it has less side effects[34]. Although many studies have reported that ESWT is an effective treatment for patients with PF[13,15,35], studies reporting that ESWT is ineffective or is minimally effective are rare[36]. On the basis of the results of our study, we found that ESWT is an effective treatment modality in relieving pain, improving foot functions and maintaining and improving foot health in the treatment of PF. Since insoles are thought to reduce the stress on the fascia during standing and walking, ready-made or custom-made insoles are recommended for people stand for long periods (>8 hours). The results of studies regarding the use of insoles markedly differ[37,43-45]. Although studies have demonstrated the effectiveness of custom-made insoles[20,38,39], the short-term or mild effectiveness of the use of insoles have also been reported (3 months)[40]. In our study, we used custom-made insoles produced by obtaining patient-specific measurements. The insoles (CFO) were readily accepted by our patients because the insole could be easily adhered to the footwear and relieved pain due to PF among these patients from the first use, which delivered the most important result in this study. Based on the short-, mid-, and long-term follow-up patients in the CFO group in our study, we found that CFO was a highly effective treatment method for relieving pain, improving foot functions and maintaining and improving foot health.
In conclusion, we found that ESWT and CFO were effective modalities in reducing foot pain, improving foot functions and maintaining foot health in the treatment of PF. Moreover, when we compared the two methods with each other, there was no superiority between the two methods in terms of short and mid-term effects. However, CFO was more effective than ESWT in reducing pain, improving foot functions and maintaining foot health at long-term.
Limitations
There are a few limitations of this treatment for one in our study, we did not use the control group with ESWT and CFO comparable to each other. Another one both ESWT and CFO groups did not fully recover from the pain despite reduced pain. Another one the use of more subjective measures that are evaluated by the patient together with objective measurements in our study. The studies in which the Eswt sessions are longer might provide more objective data.
Footnotes
None of the authors received any type of financial support that could be considered potential conflict of interest regarding the manuscript or its submission.
Edited by: G. Lyritis
References
- 1.Lemont H, Ammirati KM, Usen N. Plantar fasciitis:a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–37. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 2.Yüzer S, Sever S, Gürçay E, Ünlü E, Çakcı A. Topuk Dikeni Tedavisinde Lazer Tedavisi ve Steroid Enjeksiyonunun Etkinliğinin Karşılaştırılması. Türkiye Fiziksel Tıp ve Rehabilitasyon Dergisi. 2006;52(2):68–71. [Google Scholar]
- 3.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;20:2159–66. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 4.Landorf KB. Plantar heel pain and plantar fasciitis. BMJ Clin Evid. 2015;25:1111. [PMC free article] [PubMed] [Google Scholar]
- 5.Neufeld SK, Cerrato R. Plantar fasciitis:evaluation and treatment. J Am Acad Orthop Surg. 2008;16(6):338–46. doi: 10.5435/00124635-200806000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Levy JC, Mizel MS, Clifford PD, Temple HT. Value of radiographs in the initial evaluation of nontraumatic adult heel pain. Foot Ankle Int. 2006;27(6):427–430. doi: 10.1177/107110070602700607. [DOI] [PubMed] [Google Scholar]
- 7.Martin RL, Davenport TE, Reischl SF, Mcpoil TG, Matheson JW, Wukich DK, et al. Heel pain-plantar fasciitis:revision. J Orthop Sports Phys Ther. 2014;44(11):A1–33. doi: 10.2519/jospt.2014.0303. [DOI] [PubMed] [Google Scholar]
- 8.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of running injuries. Br J Sports Med. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ribeiro AP, Sacco IC, Dinato RC, João SM. Relationships between static foot alignment and dynamic plantar loads in runners with acute and chronic stages of plantar fasciitis:a cross-sectional study. Braz J Phys Ther. 2016;20(1):87–95. doi: 10.1590/bjpt-rbf.2014.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Özkut AT, Özkan NK, Uluçay Ç, Ertaş M, Eren A. İnatçıplantar fasiitisli olgularda ekstrakorporal şok dalga litotripsi sonuçlarımız. Göztepe Tıp Dergisi. 2011;26(3):123–7. [Google Scholar]
- 11.Rastegar S, Mahdavi SB, Hoseinzadeh B, Badiei S. Comparison of dry needling and steroid injection in the treatment of plantar fasciitis:a single-blind randomized clinical trial. Int Orthop. 2018;42(1):109–16. doi: 10.1007/s00264-017-3681-1. [DOI] [PubMed] [Google Scholar]
- 12.Gurcay E, Kara M, Karaahmet OZ, Ata AM, Onat ŞŞ, Özçakar L. Shall We Inject Superficial or Deep to the Plantar Fascia?An Ultrasound Study of the Treatment of Chronic Plantar Fasciitis. J Foot Ankle Surg. 2017;56(4):783–7. doi: 10.1053/j.jfas.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Cinar E, Saxena S, Uygur F. Low-level laser therapy in the management of plantar fasciitis:a randomized controlled trial. Lasers Med Sci. 2018;33(5):949–58. doi: 10.1007/s10103-017-2423-3. [DOI] [PubMed] [Google Scholar]
- 14.Yin M, Chen N, Huang Q, Marla AS, Ma J, Ye J, Mo W. New and Accurate Predictive Model for the Efficacy of Extracorporeal Shock Wave Therapy in Managing Patients With Chronic Plantar Fasciitis. Arch Phys Med Rehabil. 2017;98(12):2371–77. doi: 10.1016/j.apmr.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Cinar E, Saxena S, Uygur F. Combination Therapy Versus Exercise and Orthotic Support in the Management of Pain in Plantar Fasciitis:A Randomized Controlled Trial. Foot Ankle Int. 2018;39(4):406–14. doi: 10.1177/1071100717747590. [DOI] [PubMed] [Google Scholar]
- 16.Engkananuwat P, Kanlayanaphotporn R, Purepong N. Effectiveness of the Simultaneous Stretching of the Achilles Tendon and Plantar Fascia in Individuals With Plantar Fasciitis. Foot Ankle Int. 2018;39(1):75–82. doi: 10.1177/1071100717732762. [DOI] [PubMed] [Google Scholar]
- 17.Makia M, Ikoma K, Kido M, Hara Y, Sawada K, Ohashi S, Kubo T. Magnetic resonance imaging findings of chronic plantar fasciitis before and after extracorporeal shock wave therapy. Foot (Edinb) 2017;33:25–28. doi: 10.1016/j.foot.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Ulusoy A, Cerrahoglu L, Orguc S. Magnetic Resonance Imaging and Clinical Outcomes of Laser Therapy, Ultrasound Therapy, and Extracorporeal Shock Wave Therapy for Treatment of Plantar Fasciitis:A Randomized Controlled Trial. J Foot Ankle Surg. 2017;56(4):762–7. doi: 10.1053/j.jfas.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Roca B, Mendoza MA, Roca M. Comparison of extracorporeal shock wave therapy with botulinum toxin type A in the treatment of plantar fasciitis. Disabil Rehabil. 2016;38(21):2114–21. doi: 10.3109/09638288.2015.1114036. [DOI] [PubMed] [Google Scholar]
- 20.Van der Worp H, van den Akker-Scheek I, van Schie H, et al. ESWT for tendinopathy:technology and clinical implications. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1451–8. doi: 10.1007/s00167-012-2009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wrobel JS, Fleischer AE, Crews RT, Jarrett B, Najafi B. A randomized controlled trial of custom foot orthoses for the treatment of plantar heel pain. J Am Podiatr Med Assoc. 2015;105(4):281–94. doi: 10.7547/13-122.1. [DOI] [PubMed] [Google Scholar]
- 22.Drake M, Bittenbender C, Boyles RE. The short-term effects of treating plantar fasciitis with a temporary custom foot orthosis and stretching. J Orthop Sports Phys Ther. 2011;41(4):221–231. doi: 10.2519/jospt.2011.3348. [DOI] [PubMed] [Google Scholar]
- 23.Kogler GF, Solomonidis SE, Paul JP. Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Clin Biomech. 1996;11(5):243–252. doi: 10.1016/0268-0033(96)00019-8. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira LM, Alves CM, Mizuzaki J. [Portuguese adaptation of “The Foot Function Index”] [Article in Portuguese] Rev Bras Reum Suppl. 2002;42:56–8. [Google Scholar]
- 25.Yalıman A, Şen Eİ, Eskiyurt N, Budiman-Mak E. Ayak Fonksiyon İndeksi'nin Plantar Fasiitli Hastalarda Türkçe'ye Çeviri ve Adaptasyonu. Turk J Phys Med Rehab. 2014;60(3):212–22. [Google Scholar]
- 26.Ferreira AF, Laurindo IM, Rodrigues PT, Ferraz MB, Kowalski SC, Tanaka C. Brazilian version of the foot health status questionnaire (FHSQ-BR):cross-cultural adaptation and evaluation of measurement properties. Clinics. 2008;63(5):595–600. doi: 10.1590/S1807-59322008000500005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scher DL, Belmont PJ, Jr, Bear R, Mountcastle SB, Justin D, Owens MB. The incidence of plantar fasciitis in the United States military. J Bone JointSurg Am. 2009;91(12):2867–72. doi: 10.2106/JBJS.I.00257. [DOI] [PubMed] [Google Scholar]
- 28.Thing J, Maruthappu M, Rogers J. Diagnosis and management of plantar fasciitis in primary care. Br J Gen Pract. 2012;62(601):443–4. doi: 10.3399/bjgp12X653769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernández-Mijares A, Solá-Izquierdo E, Ballester-Mechó F, Marí-Herrero MT, Gilabert-Molés JV, Gimeno-Clemente N, Morales-Suárez-Varela M. Obesity and overweight prevalences in rural and urban populations in East Spain and its association with undiagnosed hypertension and Diabetes Mellitus: a crosssectional population-based survey. BMC Res Notes. 2009;2:151. doi: 10.1186/1756-0500-2-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wrobel JS, Fleischer AE, Crews RT, Jarrett B, Najafi B. A randomized controlled trial of custom foot orthoses for the treatment of plantar heel pain. J Am Podiatr Med Assoc. 2015;105(4):281–94. doi: 10.7547/13-122.1. [DOI] [PubMed] [Google Scholar]
- 31.Yan W, Sun S, Li X. herapeutic effect of extracorporeal shock wave combined with orthopaedic insole on plantar fasciitis. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2014;39(12):1326–30. doi: 10.11817/j.issn.1672-7347.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 32.Riel H, Vicenzino B, Jensen MB, Olesen JL, Holden S, Rathleff MS. The effect of isometric exercise on pain in individuals with plantar fasciopathy:A randomized crossover trial. Scand J Med Sci Sports. 2018;28(12):2643–2650. doi: 10.1111/sms.13296. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed M, Ehab M. Endoscopic plantar fasciotomy versus extracorporeal shock wave therapy for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg. 2010;130(11):1343–7. doi: 10.1007/s00402-009-1034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.James L, Jeffrey C, Steven R, Robert M, John M, John V, Lowell S, Howard Z, Richard B, Jeffrey B. The diagnosis and treatment of heel pain:A clinical practice guideline-revision. J Foot Ankle Surg. 2010;49(3):1–19. doi: 10.1053/j.jfas.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 35.David S, Ben P, Lee H, Rachel C. The effectiveness of manual stretching in the treatment of plantar heel pain:a systematic review. J Foot Surg. 2011;4(1):19–31. doi: 10.1186/1757-1146-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wheeler PC. The addition of a tension night splint to a structured home rehabilitation programme in patients with chronic plantar fasciitis does not lead to significant additional benefits in either pain, function or flexibility:a single-blinded randomised controlled trial. BMJ Open Sport & Exercise Medicine. 2017;3(1):e000234. doi: 10.1136/bmjsem-2017-000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gill LH. Plantar fasciitis: diagnosis and conservative management. Journal of the American Academy of Orthopaedic Surgeons. 1997;5(2):109–517. doi: 10.5435/00124635-199703000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Herney JE. From the Foot and Drug Aministration: shock wave for heel pain. JAMA. 2000;284:2711. doi: 10.1001/jama.284.21.2711-jfd00010-2-1. [DOI] [PubMed] [Google Scholar]
- 39.Vulpiani MC, Trischitta D, Travato P, Vetrano M, Ferreti A. Extracorporeal shockwave therapy (ESWT) in Achilles tendinopathy. A long-term follow-up observational study. J. Sports Med. Phys. Fitness. 2009;49(2):171–6. [PubMed] [Google Scholar]
- 40.Akinoğlu B, Köse N, Kirdi N, Yakut Y. Comparison of the Acute Effect of Radial Shock Wave Therapy and Ultrasound Therapy in the Treatment of Plantar Fasciitis: A Randomized Controlled Study. Pain Medicine. 2017;18(12):2443–52. doi: 10.1093/pm/pnx113. [DOI] [PubMed] [Google Scholar]
- 41.Rompe JD, Küllme K, Vogel J, Eckardt U, Wahlmann P, Eysel, et al. Orthopäde. 1997;26:215. doi: 10.1007/s001320050088. [DOI] [PubMed] [Google Scholar]
- 42.Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database of Systematic Reviews. 2003;3:CD000416. doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 43.Fong, Daniel Tik-Pui, Pang Kai-Yip, Chung Mandy Man-Ling, Hung Aaron See-Long, Chan Kai-Ming. Evaluation of combined prescription of rocker sole shoes and custom-made foot orthoses for the treatment of plantar fasciitis. Clinical Biomechanics. 2012;27(10):1072–7. doi: 10.1016/j.clinbiomech.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 44.Rasenberg N, Fuit E, Poppe AJA, Kruijsen-Terpstra KJ, Gorter MS, Rathleff PLJ, et al. The STAP-study:The (cost) effectiveness of custom made orthotic insoles in the treatment for plantar fasciopathy in general practice and sports medicine: design of a randomized controlled trial. BMC Musculoskeletal Disorders. 2016;17(1):31. doi: 10.1186/s12891-016-0889-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis. Arch Intern Med. 2006;166(12):1305–10. doi: 10.1001/archinte.166.12.1305. [DOI] [PubMed] [Google Scholar]
- 46.Johannsen FE, Herzog RB, Malmgaard-Clausen NM, Hoegberget-Kalisz M, Magnusson SP, Kjaer M. Corticosteroid injection is the best treatment in plantar fasciitis if combined with controlled training. Knee Surg Sports Traumatol Arthrosc. 2018:1–8. doi: 10.1007/s00167-018-5234-6. [DOI] [PubMed] [Google Scholar]
- 47.Shetty SH, Dhond A, Arora M, Deore S. Platelet-Rich Plasma Has Better Long-Term Results Than Corticosteroids or Placebo for Chronic Plantar Fasciitis:Randomized Control Trial. J Foot Ankle Surg. 2018 Nov 15; doi: 10.1053/j.jfas.2018.07.006. pii:S1067-2516(18)30282-5. [DOI] [PubMed] [Google Scholar]


