Abstract
Social jetlag, a misalignment between sleep timing on the weekend and work week, is associated with depressive symptoms among adults across both sexes. One prior study found that later sleep timing was associated with depressive symptoms in women but not men. To date, however, no research has investigated whether the association between social jetlag and depression varies by sex among adolescents. The current study assessed self-reported sleep, depressive symptoms, and demographic information from 3,058 adolescents (48% female, mean ± SD age 15.59 ± .77 years) from the age 15 wave of the Fragile Families and Child Wellbeing Study (FFCWS). Social jetlag was calculated as the absolute value of the midpoint of sleep on the weekend minus the midpoint of sleep during the school week. Depressive symptoms were measured through a modified 5-item version of the Center for Epidemiologic Studies Depression Scale (CES-D). We assessed whether the associations between sleep duration on school nights, social jetlag, and depressive symptoms were similar between male and female adolescents using multiple linear regression. In fully adjusted models, sex moderated the association between school night TST and depressive symptoms (p < .001) and between social jetlag and depressive symptoms (p = .037). In females, but not in males, school night TST was negatively associated with depressive symptoms (p < .001), while social jetlag (p < .001) was positively and independently associated with depressive symptoms. The results indicate the importance of regular sleep timing across the week and adequate sleep duration for maintenance of optimal emotional health among female adolescents.
INTRODUCTION
Major depressive disorder is the most common type of mood disorder in the United States (Substance Abuse and Mental Health Services Administration, 2014). The average age of onset of major depression is between 11 and 14 years (Merikangas et al., 2011), indicating that depressive symptoms may emerge well before adulthood. Indeed, nearly 12% of American adolescents aged 13 to 18 have manifested clinical depression at some point in their lifetime, with 9% of these adolescents reporting severe depression-related impairment (Merikangas et al., 2011). Thus, identifying risk factors for depressive symptoms before adulthood, such as sleep behaviors, may be critical for early detection and treatment of major depressive disorder.
Over 70% of adolescents in the United States report fewer than the minimum recommended amount of 8 hours sleep per night (Wheaton et al., 2018). Furthermore, insufficient total sleep time (TST) is associated with depressive symptoms (Fernandez-Mendoza et al., 2016; Raniti et al., 2016; Roberts and Duong, 2014), with one longitudinal study finding a reciprocal relationship between short sleep and depressive symptoms across one year (Roberts and Duong, 2014). Given the high prevalence of insufficient sleep and the bidirectional association with depressive symptoms during a period in which depressive symptoms emerge (Merikangas et al., 2011), sleep health is a priority area for adolescent mental health research.
Adolescents experience a shift toward later preferred timing of daily activities (e.g., sleep), or later chronotype, compared to children and adults (Borisenkov et al., 2012; Carskadon et al., 1993; Randler et al., 2017; Roenneberg et al., 2004). During the school week, adolescents with later chronotype tend to have later bedtimes but relatively fixed early wake times due to school and other obligations (Roenneberg et al., 2003; Roepke and Duffy, 2010; Vitale et al., 2015). Late bedtimes and early wake times result in shorter TST during the school week compared to the weekend, when adolescents are “free” to wake up later. As a result, adolescents may attempt to compensate for short sleep during the school week with longer TST on the weekend (Roenneberg et al., 2003; Roepke and Duffy, 2010; Vitale et al., 2015). Later chronotypes thus tend to have a sleep interval with a later midpoint on the weekend relative to the school week (Wittmann et al., 2006). This misalignment in sleep-wake timing between the school week and the weekend is known as “social jetlag” (Wittmann et al., 2006). Adolescents experience short sleep during the school week and more social jetlag compared to adults (Touitou, 2013; Wittmann et al., 2006) due to the combination of both a shift toward later chronotype during adolescence (Borisenkov et al., 2012; Carskadon et al., 1993; Randler et al., 2017; Roenneberg et al., 2004) and early school start times (Vollmer et al., 2016; Wheaton et al., 2015). Therefore, both short school night TST and social jetlag are prevalent in adolescents.
Among adults, social jetlag is associated with negative emotional health (Lau et al., 2013; Randler and Vollmer, 2013; Yong et al., 2016). For example, adults with social jetlag self-report greater depressive symptoms (Levandovski et al., 2011; Polugrudov et al., 2016). A separate study among adolescents and young adults aged 12 to 21 failed to replicate this association (de Souza and Hidalgo, 2014); however, in that analysis, the potential moderating effect of sex was not investigated. Female adolescents are more than twice as likely to exhibit major depressive disorder or dysthymia compared to male adolescents (Avenevoli et al., 2015; Merikangas et al., 2011), suggesting potential sex differences in the etiology of depressive symptoms. Interestingly, one study found that adult females, but not males, with sleep midpoints later than 4:45 were more likely to exhibit depressive symptoms (Morita et al., 2015). As later chronotype is associated with increased social jetlag (Wittmann et al., 2006), a positive relationship may similarly exist between social jetlag and depressive symptoms in females, but not males. However, no studies have examined whether sex moderates the relationship between social jetlag and depressive symptoms in an adolescent population specifically. Female adults exhibit a shorter free-running circadian period, or tau, compared to male adults (Duffy et al., 2011). Research in adolescents is more limited but suggests a similar pattern of shorter tau in females versus males (Crowley and Eastman, 2018). Corroborating these studies, females also exhibit an earlier dim light melatonin onset (DLMO) phase and wider DLMO phase angle (relative to bedtime) than do males (Van Reen et al., 2013), indicating sex differences in the relationship of circadian phase to sleep timing behaviors. The greater prevalence of depressive symptoms and earlier circadian phase in females suggest potential sex differences in the association among sleep timing misalignment and depressive symptoms. Furthermore, it is unknown whether any relationship between social jetlag and depressive symptoms remains after accounting for TST during the school week, which is shorter in individuals with social jetlag (Touitou, 2013; Wittmann et al., 2006).
The current study had two aims: (1) to investigate the relationships between social jetlag and TST on school nights with depressive symptoms among adolescents, and (2) to determine whether these relationships are moderated by sex. We hypothesized that school night TST would be negatively associated with depressive symptoms in both sexes. Furthermore, given prior research among adults, we hypothesized that greater social jetlag would be associated with depressive symptoms in females, but not in males.
METHODS
Participants and Design
Data for the current analyses come from the Fragile Families and Child Wellbeing Study (FFCWS; www.fragilefamilies.princeton.edu). The original birth cohort consists of nearly 4,900 children born 1998–2000 in 20 U.S. cities, obtained through stratified random sampling. Non-marital births were over-sampled to obtain a sample of low socio-economic status (SES) (Wagmiller, 2010). To date, data have been collected in six waves: at birth (Reichman and Teitler, 2001) and at ages one (Noonan et al., 2010), three (Wang and Maguire-Jack, 2018), five (Hale et al., 2011), 9 (Hunt et al., 2017), and 15 (Mathew et al., 2018; Nahmod et al., 2018). The current study examines cross-sectional survey responses of 3,444 youth at age 15 and their primary caregivers (PCGs), defined as the person with whom the youth lives for “half the time” or more. Youth missing demographic, sleep, or depressive symptoms information were excluded from the current study, yielding a final analytical sample of 3,058 youth (88.8% of in-wave total and 62.4% of initial birth cohort). Families were compensated $100 for completion of the PCG questionnaire and $50 for completion of the youth questionnaire. Researchers in the FFCWS are located at multiple institutions, and approval has been obtained from each site’s Institutional Review Board.
Materials and Methods
Data used in statistical analyses were drawn from two sources at the age 15 wave: a questionnaire administered to youth, and a separate questionnaire administered to their primary caregivers.
Youth Age 15 Questionnaire
This questionnaire was administered to youth at age 15. Teens were asked to report sleep variables including bedtime/wake time on school days and weekends, depressive symptoms, and demographic information including race/ethnicity, height, and weight (used to calculate body mass index, BMI), and number of hours spent working outside the home weekly.
Sleep Measures
Bedtime on school nights and bedtime on weekend nights were assessed through the questions, “What time do you usually go to bed on school nights? By school night we mean Sunday night through Thursday night,” and “What time do you usually go to bed on weekend nights? By weekend night we mean Friday and Saturday night,” respectively. Youth were prompted to report hour, minutes, and AM/PM for bedtimes.
Wake time on school mornings and wake time on weekend mornings were assessed through the questions, “What time do you usually wake up on school day mornings?” and “What time do you usually wake up on weekend mornings?” respectively. Youth were prompted to report hour, minutes, and AM/PM for wake times.
The following variables were calculated using bedtime and wake time measures collected from the Youth Age 15 Questionnaire. Total sleep time (TST) on school nights (TST School) was calculated as the interval between reported bedtime and wake time on school nights (Sunday through Thursday) in hours. TST on weekend nights (TST Weekend) was calculated as the interval between reported bedtime and wake time on weekend nights (Friday and Saturday) in hours. Weekly average TST was calculated through the following formula: ((TST School*5) + (TST Weekend*2)) / 7. Midpoint of sleep on school nights was calculated through the following formula: Bedtime School + (TST School*.5) (Roenneberg et al., 2003). Midpoint of sleep on weekend nights was calculated through the following formula: Bedtime Weekend + (TST Weekend*.5) (Roenneberg et al., 2003). Chronotype was calculated according to the formula created by Roenneberg et al. (2007) which uses the midpoint of sleep on weekend nights, corrected for accumulated sleep debt, to determine chronotype: sleep midpoint on weekend nights − 0.5*(TST Weekend − (5*TST School + 2*TST Weekend) / 7 (higher sleep debt-corrected sleep midpoint on weekend nights indicates later chronotype).
In primary regression models, social jetlag in hours was calculated through the following formula: | sleep midpoint on weekend nights – sleep midpoint on school nights | (Wittmann et al., 2006). We conducted a separate regression analysis using social jetlag categorized as low (≤ two hours), moderate (> two hours and ≤ four hours), and high (> four hours), as defined by Levandovski et al., 2011, to test the possibility of a non-linear relationship between social jetlag and depressive symptoms (see Supplemental Information).
Depressive Symptoms Measure
Depressive symptoms were assessed through a modified five-item version of the Center for Epidemiologic Studies Depression Scale (Perreira et al., 2005). The five-item CES-D scale has previously shown superior cross-cultural comparability to the full 20-item scale. Youth selected level of agreement with six statements expressing depressive symptoms: 1 = strongly agree, 2 = somewhat agree, 3 = somewhat disagree, and 4 = strongly disagree. The statements are as follows: “I feel I cannot shake off the blues, even with help from my family and my friends,” “I feel sad,” “I feel happy” (reverse-scored), “I feel life is not worth living,” and “I feel depressed.” A depressive symptoms score was calculated as the average of item scored and reverse scored, with greater composite score indicating greater depressive symptomology (i.e., 0 = strongly disagree, 3 = strongly agree). Youth with two or more missing depressive symptoms items were not included in the analytical sample. The coefficient alpha for the items on the scale was .76, indicating acceptable reliability.
Covariate Measures from Youth Questionnaire
Race and ethnicity consisted of four exclusive categories: “White/Caucasian” (reference); “Black/African American,” “Hispanic and/or Latino,” or a “mixed, other, or none” category.
Body mass index (BMI) percentile at age 15 was assessed using self-reported height and weight. BMI was calculated through the following formula: [weight in pounds / (height in inches2) × 703] (Keys et al., 1972) and a percentile was calculated based on 2000 CDC growth charts (Kuczmarski et al., 2002). The 50th percentile indicates the median BMI for the adolescent’s age and sex, and a percentile greater than 68% indicates the adolescent is overweight based on the World Health Organization growth reference (De Onis et al., 2007).
Number of hours of work weekly assessed the amount of time (in hours) the youth spent working for pay outside of the household.
Primary Caregiver (PCG) Questionnaire
Covariate Measures from PCG Questionnaire
Covariates for statistical analyses were additionally drawn from a questionnaire administered to PCGs: relationship to youth, PCG employment status, annual household income level, PCG highest level of education completed, number of children in household other than the youth, and whether the PCG (if a biological parent) was married or cohabiting with the youth’s other biological parent (but not if married to someone else). PCG depressive symptoms were scored through the Composite International Diagnostic Interview – Short Form (CIDI-SF), Section A (Kessler et al., 1998) and consisted of 0, does not meet criteria for major depressive disorder, and 1, meets criteria for major depressive disorder.
Statistical Analyses
Analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC). Cases were excluded from all analyses if missing any of the following: bedtime or wake time on either school or weekend nights (n = 63), more than two items from the CES-D (n = 1), and/or covariate questions (n = 322), yielding 386 excluded adolescents and a total analytic sample of N = 3,058.
Sex differences in sleep timing and TST variables were assessed through independent-groups t tests. Effect sizes (d) were interpreted based on Cohen’s cutoffs for small (d = .20), medium (d = .50), and large (d = .80) (Cohen, 1992).
Separately, three linear regression analyses were conducted to determine the interactions of TST School and social jetlag with sex on depressive symptoms. Model 1 included the following predictors: sex, TST School and its interaction with sex, and social jetlag (measured continuously) and its interaction with sex. Models 2 and 3 tested the associations of TST School and social jetlag with depressive symptoms separately within females and males, respectively. Separately, we tested the associations of TST school and categories of social jetlag (low, moderate, or high) with depressive symptoms (see Supplemental Information). Given that individuals with African ancestry exhibit shorter circadian periods compared to individuals with European ancestry (Eastman et al., 2017), we additionally ran models stratified by Black (n = 1,416) and non-Black (i.e., White/Caucasian, Hispanic and/or Latino, or mixed, other, or none; n = 1,642) race/ethnicity. Model 4 tested the three-way interactions for each sleep variable (social jetlag and TST school) with sex and Black race/ethnicity. Models 5 and 6 were similar to Model 1 except conducted only in non-Blacks or in Blacks, respectively: predictors included TST School and its interaction with sex, and social jetlag and its interaction with sex. Effect sizes (ΔR2) were interpreted based on Cohen’s cutoffs for small (ΔR2 = .01), medium (ΔR2 = .09), and large (ΔR2 = .25) (Cohen, 1992).
Covariates were selected a priori based on previous literature (Chase-Lansdale et al., 2003; Jung et al., 2017; Kim, 2014; Park et al., 2013; Schubert et al., 2017; Wang et al., 2016; Zimmerman and Katon, 2005) and were included in analyses if significantly correlated with CES-D depressive symptoms score: reported race/ethnicity, age in years, BMI percentile, number of hours of work outside of the home weekly, number of other children below the age of 18 in the household, annual household income, and PCG relationship to youth, married/cohabiting with youth’s biological parent, employment status, education level, and meeting depression criteria as indicated by the CIDI-SF, Section A (Kessler et al., 1998). Categorical covariates were dummy-coded and entered into regression models. The variance inflation factor (VIF) did not exceed 2.5 for any predictor in the regression model, indicating no multicollinearity (i.e., no predictor was strongly correlated with another predictor) (Menard, 1995).
RESULTS
The final analytical sample consisted of 3,058 youths, 88.8% of the age 15 wave (see Table 1 for sample demographic information). Among adolescents in the entire sample, the mean depressive symptoms (CES-D) score was .59 with a range of 0 to 3 (standard deviation, SD = .60); 81% of adolescents had a score ≤ 1 (indicating an average response of “disagree” with each of five depressive statements). Female adolescents (M = .66, SD = .63) reported significantly higher depressive symptoms than did males (M = .52, SD = .56), t(2946) = −6.22, p < .001, d = .23.
Table 1.
Demographic Information from Analytical Sample (N = 3,058) of Age 15 Wave of the Fragile Families and Child Wellbeing Study (FFCWS)
|
n |
% |
|
| Youth | ||
| Sexa | ||
| Female | 1478 | 48.3 |
| Male | 1580 | 51.7 |
| Race/ethnicity | ||
| Black/African American | 1416 | 46.3 |
| White/Caucasian | 535 | 17.5 |
| Hispanic and/or Latino | 737 | 24.1 |
| Other, mixed, or noneb | 370 | 12.1 |
|
Mean |
SD |
|
| Age (yrs) | 15.59 | .77 |
| Body mass indexc | 24.03 | 5.76 |
| Body mass index (percentile)cd | .68 | .28 |
| Work outside home weekly (hrs) | 1.93 | 4.67 |
| Household | ||
| Number of other children < 18 years | 1.5 | 1.4 |
|
n |
% |
|
| PCGe married or cohabiting with youth biological parent | ||
| Not married or cohabiting | 2226 | 72.8 |
| Married or cohabiting | 832 | 27.2 |
| PCG | ||
| Relationship to youth | ||
| Biological mother | 2692 | 88.0 |
| Biological father | 221 | 7.2 |
| Non-parent | 145 | 4.7 |
| Highest education level completed | ||
| Less than high school | 528 | 17.3 |
| High school or equivalent | 597 | 19.5 |
| Some college or technical school | 1334 | 43.6 |
| College graduate | 599 | 19.6 |
| Employment status | ||
| Unemployed | 896 | 29.3 |
| Employed | 2162 | 7.7 |
|
Mean |
SD |
|
| Annual household income | $62,410 | $65,498 |
| PCG major depressive disorderf | ||
| PCG does not meet criteria (score of 0) | 2529 | 82.7 |
| PCG meets criteria (score of 1) | 529 | 17.3 |
Data collected at birth.
Other category includes Asian, Central American/Caribbean, Native American/Alaska Native, and/or Native Hawaiian/Pacific Islander.
Body mass index collected at age 15.
Percentile calculated based on 2000 CDC growth charts (Kuczmarski et al., 2002).
PCG–Primary caregiver.
Based on Composite International Diagnostic Interview – Short Form (CIDI-SF), Section A (Kessler et al., 1998), describing depressive symptoms within last year.
Between-Sex Differences in Sleep Variables
Females reported significantly less sleep on school nights (M = 7.93 hrs, SD = 1.23) than did males (M = 8.02 hrs, SD = 1.24), t(3056) = −2.02 p = .044, d = −.07, driven by an earlier wake time in females compared to males (p < .001). The mean social jetlag in the entire sample was 2.80 (SD = 1.46) with no difference in between the sexes (p > .05). Furthermore, compared to males, females reported more sleep on the weekends (p = .001), driven by females going to bed earlier than males on the weekend (p = .001) and reporting earlier chronotype as indicated by the sleep midpoint on weekend nights, corrected for sleep debt (p = .001). Between-sex comparisons in additional sleep variables are in Table 2.
Table 2.
Between-Sex T-Tests in Sleep Measures (N = 3,058)
| Female | Male | Male vs. Female | ||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t (df) | d | |
| Bedtime | ||||||
| School nighta | 23:21 | 1.13 | 23:23 | 1.11 | .86 (3056) | .03 |
| Weekend nightb | 0:23 | 1.86 | 0:38 | 1.94 | 3.56*** (3056) | .13 |
| Wake time | ||||||
| School morning | 6:16 | .81 | 6:24 | .88 | 4.08*** (3055.8)e | .15 |
| Weekend morning | 9:46 | 1.77 | 9:42 | 1.91 | −1.06 (3055.8)e | −.04 |
| TST (hrs) | ||||||
| School night | 7.93 | 1.23 | 8.02 | 1.24 | 2.02* (3056) | .07 |
| Weekend night | 9.38 | 1.93 | 9.07 | 2.11 | 4.32*** (3054.4)e | .16 |
| Chronotypec | 4:33 | 1.67 | 4:47 | 1.72 | 3.78*** (3056) | .14 |
| Social jetlag (hrs)d | 2.80 | 1.46 | 2.81 | 1.46 | .26 (3056) | .01 |
Sunday-Thursday night.
Friday-Saturday night.
Midpoint of sleep on weekend nights corrected for sleep debt; measure of chronotype. Calculated as midpoint of sleep on weekend nights − .5*(TST Weekend − (5*TST School + 2*TST Weekend) / 7 (Roenneberg et al., 2004).
Calculated as | midpoint of sleep on weekend nights – midpoint of sleep on school nights | (Wittman et al., 2006).
Degrees of freedom corrected for heterogeneity of variance.
TST—total sleep time.
p < .05, two-tailed.
p < .001, two-tailed.
Between-Sex Associations of TST School and Social Jetlag with Depressive Symptoms Score
The full model including the entire sample, N = 3058 (Model 1) investigated the associations of TST School (TST on school nights), social jetlag, and their sex interactions with depressive symptoms score (see Table 3) and explained 5.8% of the variance in depressive symptoms score. There were significant interactions between sex and TST School (b = .07, ΔR2 = .011, p < .001) and between sex and social jetlag (b = .03, ΔR2 = .003, p = .037) on depressive symptoms.
Table 3.
Regression Models Predicting Depressive Symptoms (CES-D Scorea) from TST School and Social Jetlag (N = 3058)
| UNADJUSTED |
ADJUSTEDe |
|||||
|---|---|---|---|---|---|---|
| b | 95% CIb | ΔR2 | b | 95% CIb | ΔR2 | |
| Overall (Model 1) | ||||||
| TST school (hrs)c | −.08*** | −.10, −.05 | .024 | −.08*** | −.11, −.06 | .030 |
| Sex (female=ref) | −.13*** | −.17, −.09 | .012 | −.13*** | −.17, −.09 | .012 |
| TST school (hrs)c * Sex | .07*** | .03, .10 | .010 | .07*** | .04, .10 | .011 |
| Social jetlag (hrs)cd | .05*** | .02, .07 | .012 | .04*** | .02, .06 | .010 |
| Social jetlag (hrs)cd * Sex | −.03* | −.06, .003 | .003 | −.03* | −.06, .002 | .003 |
| Females (Model 2) | ||||||
| TST schoolc (hrs) | −.08*** | −.10, −.05 | .022 | −.08*** | −.11, −.06 | .027 |
| Social jetlagcd (hrs) | .05*** | .02, .07 | .011 | .04*** | .02, .06 | .009 |
| Males (Model 3) | ||||||
| TST schoolc (hrs) | −.01 | −.03, .01 | <.001 | −.01 | −.03, .01 | .001 |
| Social jetlagcd (hrs) | .01 | −.01, .03 | .001 | .01 | −.01, .03 | .001 |
CES-D subscale range: 0=low depressive symptoms; 3=high depressive symptoms (Perreira et al., 2005).
95% confidence interval for unstandardized coefficient, b.
Mean-centered.
Calculated as | midpoint of sleep on weekend nights – midpoint of sleep on school nights | (Wittmann et al., 2006).
Adjusted for reported race/ethnicity, age in years, body mass index percentile, number of other children below the age of 18 in the household, number of hours youth works outside home weekly, annual household income, youth relationship to primary caregiver (PCG), PCG married/cohabiting with youth’s biological parent, PCG employment status, PCG education level, and PCG meeting clinical depression criteria for past year.
ref=reference group; TST—total sleep time.
p < .01, two-tailed.
p < .001, two-tailed.
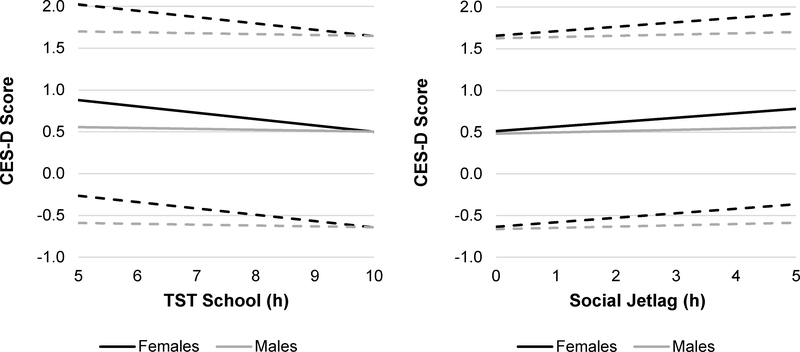
Post-hoc analyses were conducted to investigate the associations of TST School and social jetlag with depressive symptoms within each sex separately. Model 2 (in females only) explained 7% of the variance in depressive symptoms score and showed that TST School was negatively associated with depressive symptoms (b = −.08, ΔR2 = .027, p < .001); thus, females with shorter TST School reported more depressive symptoms. Social jetlag was positively associated with depressive symptoms in females (b = .04, ΔR2 = .009, p < .001), indicating females with greater social jetlag expressed more depressive symptoms. Model 3 (in males only) explained 3.1% of the variance in depressive symptoms score and found no association between TST School and depressive symptoms or between social jetlag and depressive symptoms (p > .05). The results indicated that females with short sleep during the school week and with greater social jetlag, but not males, expressed more depressive symptoms. See Figure 1 for a depiction of the associations of TST School and social jetlag with depressive symptoms within each sex.
Figure 1.
According to Model 1, the interactions between school night total sleep time (TST School) and sex (b = .07, ΔR2 = .011, p < .001), and between social jetlag (|midpoint of sleep on weekend nights – midpoint of sleep on school nights|; Wittman, 2006) and sex (b = −.03, ΔR2 = .003, p = .037), on depressive symptoms (Center for Epidemiologic Studies Depression Scale; CES-D) score (Perreira, 2005) in adolescents (n = 3,058) were significant. In females (black lines), TST School (left panel; b = −.08, ΔR2 = .027, p < .001) and greater social jetlag (right panel; b = .04, ΔR2 = .009, p < .001) were associated with higher depressive symptoms score. In males (gray lines), neither TST School nor social jetlag (p > .05), were associated with higher depressive symptoms score according to Model 3. Note. Dashed lines represent 95% confidence interval around the mean.
Stratification by Black Race/Ethnicity
Model 4 tested the three-way interactions of each sleep variable (social jetlag and TST School) with sex and Black race/ethnicity and explained 5.9% of the variance in depressive symptoms score. The interaction between social jetlag, Black race/ethnicity, and sex was significant (b = .07, ΔR2 = .008, p = .011); there was no significant interaction between TST School, Black race/ethnicity, and sex (p > .05).
Models 5 (in non-Blacks) and 6 (in Blacks) examined interactions between sleep variables and sex, stratified by Black race/ethnicity, with the following predictors: TST School and its interaction with sex, and social jetlag and its interaction with sex. Model 5 in non-Blacks explained 7.0% of the variance in depressive symptoms and indicated a significant interaction between social jetlag and sex on depressive symptoms (b = −.07, ΔR2 = .014, p < .001). Post-hoc analyses in non-Blacks were conducted to investigate the associations of TST School and social jetlag with depressive symptoms within each sex separately. A model in non-Black females explained 9.1% of the variance in depressive symptoms and indicated a significant positive association between social jetlag and depressive symptoms (b = .06, ΔR2 = .014, p = .001). A model in non-Black males explained 4.6% of the variance in depressive symptoms and indicated no significant association between social jetlag and depressive symptoms (p > .05). Model 6 in Black adolescents (male and female) explained 5.4% of the variance in depressive symptoms and indicated no significant interaction between social jetlag and sex on depressive symptoms (p > .05). According to Model 6, social jetlag was not significantly associated with depressive symptoms (p > .05) in Black adolescents (both male and female).
In summary, the results indicate a negative association between TST School and depressive symptoms in both Black and non-Black females (b = −.08, ΔR2 = .027, p < .001), a positive association between social jetlag and depressive symptoms in non-Black females only (b = .06, ΔR2 = .014, p = .001), and no significant associations between either social jetlag or TST School and depressive symptoms in males (Blacks and non-Blacks).
DISCUSSION
The findings from the current study indicate that in female adolescents, greater social jetlag and shorter TST during the school week were independently associated with higher depressive symptoms. However, in males, neither social jetlag nor school night TST were associated with depressive symptoms. Furthermore, the amount of social jetlag did not differ between male and female adolescents; school night TST was significantly higher in males. Together, these findings indicate that differences in amounts of TST and of social jetlag between males and females do not account for between-sex differences in adolescent depressive symptoms. Rather, the associations of school night TST and social jetlag with depressive symptoms differ between the sexes; that is, female adolescents exhibit greater vulnerability to experiencing depressive symptoms accompanying short school night TST and social jetlag. Thus, male and female adolescents may have different risk factors and require different treatment for depressive symptoms.
Our findings indicate significant, albeit small, differences in TST and sleep timing between male and female adolescents. Compared to males, females have a 5.4-minute shorter school night TST (d = .07) driven by an earlier school day wake time (d = .15) and 19-minute longer weekend night TST (d = .16) driven by a 14-minute earlier chronotype (d = .14) and earlier weekend night bed time (d = .13). Although they have a similar bedtime during the school week to their male counterparts, females wake up earlier on school mornings, obtaining less school night sleep and compensating by going to bed earlier on the weekend and obtaining more weekend night sleep, in comparison to males. Previous research supports our findings of shorter TST on school nights for female versus male adolescents (Jiang et al., 2015; Ming et al., 2016; Ojio et al., 2016) but more research is needed on between-sex differences in adolescent TST on the weekend. The 5.4-minute shorter TST School in females compared to males may seem like a modest difference but translates to a 27-minute reduction in sleep duration across one week. Moreover, research suggests that even a 4-minute increase in TST per night is linked to improved self-reported mental health and fewer emotional problems in adolescents (Chan et al., 2017). Our findings of between-sex differences in sleep duration and timing highlight that female adolescents may be more vulnerable to experiencing sleep insufficiency during the school week than males. Future studies should replicate these sex differences in adolescent sleep duration and timing and determine whether these constitute meaningful differences with regard to emotional health.
We found a mean social jetlag of 2.80 hours in this large sample of adolescents, with no between-sex differences (2.80 in females and 2.81 in males). Population-level studies of social jetlag in adolescents demonstrate average social jetlag levels around 2.50 (Haynie et al., 2018; Vollmer et al., 2017), similar to the current sample. These levels of social jetlag in adolescents contrast sharply with population-level studies in adults, which find the majority of adults having social jetlag ≤ 1 hours (Islam et al., 2018; Koopman et al., 2017; Parsons et al., 2015), translating to about 250% greater social jetlag in adolescents versus adults. As social jetlag increases with later chronotype (Wittmann et al., 2006) and adolescents tend to have later chronotype than adults (Borisenkov et al., 2012; Carskadon et al., 1993; Randler et al., 2017; Roenneberg et al., 2004), it is unsurprising that adolescents would have greater levels of social jetlag. The evidence indicates that adolescents are a critical population with respect to targeted interventions to lengthen sleep during the school week, decrease social jetlag, and improve associated health outcomes.
Corroborating previous research, we found that females self-reported greater depressive symptoms compared to male adolescents (Avenevoli et al., 2015; Frost et al., 2015; Merikangas et al., 2011; Salk et al., 2016). Though the effect size for the between-sex difference was small (d = .23), the mean CES-D depressive symptoms score for female adolescents was .66, nearly 27% higher than males (mean score .52). Furthermore, the vast majority of our sample (81%) scored ≤ 1 on the CES-D, which ranges from 0, “strongly disagree,” to 3, “strongly agree” (with depressive statements). Therefore, the level of depressive symptomology was relatively low in our sample. Given that the CES-D does not have a clinical cutoff for depression (Perreira et al., 2005), we cannot conclude, however, that levels of clinical depression meaningfully differed between male and female adolescents in our sample. Moreover, some research suggests females are more likely to self-report depressive symptoms than males, even when clinician-scored depressive symptoms do not differ between the sexes (Compas et al., 1997; Frank et al., 1988; Perugi et al., 1990). Nevertheless, these between-sex differences emphasize the need to address the potential greater prevalence of depressive symptoms in females when implementing interventions for depression in adolescents.
In females, TST during the school week was negatively associated with self-reported depressive symptoms. The results are consistent with studies indicating an association between short sleep and depression in adolescents (Fernandez-Mendoza et al., 2016; Raniti et al., 2016). Contrary to our expectations, males did not exhibit an association between school night TST and depressive symptoms. Previous studies have indicated sex differences in the cortisol stress response to sleep loss which may explain the observed sex differences in the current study. For example, adult women exhibit greater cortisol awakening response (CAR) to sleep loss (Eek et al., 2012; Vargas et al., 2017), while adult men exhibit lower CAR after sleep loss (Vargas et al., 2017). Individuals who ruminate before sleep exhibit elevated CAR, indicating that CAR may be a marker of psychological stress (Schlotz et al., 2004). Thus, females, but not males, may experience elevated CAR in response to sleep loss, which is linked to greater psychological stress. There is only one study examining CAR in response to sleep loss in adolescents which suggests short sleep duration is associated with lower CAR in males but no association in females (Pesonen et al., 2014). More research is needed regarding the association between sleep insufficiency and CAR in male and female adolescents. These sex differences, along with the findings from the current study, indicate that females may be more vulnerable to experiencing depressive symptoms with insufficient sleep than males.
Interestingly, we found that beyond TST during the school week, social jetlag was positively associated with depressive symptoms in female but not male adolescents. Poor sleep quality is associated with depressive symptoms in females but not males (van Zundert et al., 2013); the current study corroborates the notion that poor sleep health (i.e., social jetlag) affects mood to a greater degree in females than males. Alternatively, given the cross-sectional nature of the current study, it is plausible that females who have later sleep timing on the weekend relative to the school week (i.e., higher social jetlag) exhibit behaviors which are simultaneously associated with later weekend sleep timing and with depressive symptoms. For example, adolescent females tend to ruminate (i.e., dwell on negative thoughts) more than males (Rood et al., 2009); and the association between rumination and depressive symptoms is stronger among adult females than males (Polanco-Roman et al., 2016). Females who exhibit a delayed bedtime on the weekend (relative to the school week) and thus, greater social jetlag, may also ruminate near bedtime on the weekend more than males with a delayed bedtime on the weekend. These bedtime behaviors may result in simultaneous delayed bedtime, social jetlag, and depressive symptoms for females rather than social jetlag causing depressive symptoms per se. Sex differences in rumination near bedtime may be explained by differences in online social media use. Female adolescents are more likely to make technology-based social comparisons than males, and the association between technology-based social comparisons and depressive symptoms is stronger in females than males (Nesi and Prinstein, 2015). Indeed, having an electronic device (such as a mobile phone) in the bedroom or internet use in the hour before bedtime predicts greater social jetlag, and these behaviors are more prevalent in female adolescents (Nesi and Prinstein, 2015; Spilková et al., 2017). Females may be more likely to use social media and delay bedtime on weekend nights (when they are free to stay up later) rather than during the school week. Therefore, in female adolescents, social jetlag may increase the risk for depressive symptoms, be a consequence of depressive symptoms, or have a reciprocal relationship. Future empirical work should determine whether the contributors to social jetlag (e.g., use of social media before bedtime) differ between male and female adolescents.
We found that the moderating influence of sex on the association between social jetlag and depressive symptoms was present only in non-Black adolescents. The disparity between Blacks and non-Blacks in these associations may be explained by differences in the length of the free-running circadian period; in individuals of European ancestry, but not of African ancestry, females exhibit shorter circadian period compared to males (Eastman et al., 2017). It is possible that differences in circadian period between non-Black males and females results in between-sex differences in the associations between social jetlag and emotional health in this population which do not exist in Blacks. Future studies should probe the interactions between sleep deficiency, sex, and race/ethnicity on other domains of emotional health.
Our findings indicate that shorter school night TST and greater social jetlag are associated with an increased risk for depressive symptoms in female but not male adolescents. The current study indicates that female youth with later chronotype who must conform to early school schedules are particularly at risk for social jetlag (Touitou, 2013; Wittmann et al., 2006) and, potentially, depressive symptoms; social jetlag is not associated with depressive symptoms in male adolescents. Future studies should target short school night TST and social jetlag to identify and subsequently treat female adolescents at risk for depressive symptoms. The risk of depressive symptoms may be reduced through lengthening sleep on school nights (e.g., going to bed earlier or delaying school start times). Lengthening sleep on school nights may in turn reduce the amount of sleep debt across the week, resulting in lower levels of social jetlag and further reducing the risk of depressive symptoms.
Limitations of the current study include a cross-sectional study design, restricting our ability to determine temporal order of sleep patterns and depressive symptoms. As mentioned, research demonstrates a reciprocal relationship between short sleep and depressive symptoms (Roberts and Duong, 2014); social jetlag may cause depressive symptoms or may result from other factors, such as greater rumination near bedtime in female adolescents (Polanco-Roman et al., 2016; Rood et al., 2009). Future longitudinal research should determine whether sleep behaviors precede, follow, or have a reciprocal relationship with depressive symptoms in adolescents of both sexes. Furthermore, the depressive symptoms scale employed in the current study (CES-D) does not have a clinical cutoff for major depressive disorder (Perreira et al., 2005). However, due to the large sample size, we were able to identify associations of small effect size according to Cohen’s guidelines (Cohen, 1992) among school night TST and depressive symptoms (ΔR2 = .027) and between social jetlag and depressive symptoms (ΔR2 = .009) in females. Additionally, we calculated TST as the elapsed time between self-reported bedtime and wake time. However, sleep latency may be longer on school days due to adolescents going to bed before their biological night; thus, it is likely that we overestimated TST, particularly on school nights. Finally, we used survey sleep data, which may be prone to self-report bias, particularly in individuals with poor emotional health (Baillet et al., 2016). Strengths of the current study are its large sample size and the inclusion of demographic and household covariates in regression models (e.g., race and ethnicity, income) which may have been confounding variables (Xing et al., 2011).
In conclusion, we found that shorter sleep duration during the school week and greater social jetlag were associated with depressive symptoms in females, but not males, in a large national sample of adolescents. Though effect sizes were small, our findings indicate female adolescents may be more vulnerable to experiencing negative emotional health accompanying short sleep and social jetlag than are males. Our findings may help explain the nearly twofold greater prevalence of depression in female compared to male adolescents (Avenevoli et al., 2015; Merikangas et al., 2011). Future experimental and longitudinal research should determine whether increasing sleep duration during the school week and decreasing social jetlag reduces depressive symptoms in female adolescents.
Supplementary Material
Acknowledgments
DECLARATION OF INTEREST STATEMENT
The authors have indicated no financial conflicts of interest relevant to the current study. Dr. Lauren Hale receives an honorarium from the National Sleep Foundation for serving as Editor-in-Chief of the journal Sleep Health. Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD073352 (to LH), R01HD36916, R01HD39135, and R01HD40421, as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- Avenevoli S, Swendsen J, He JP, Burstein M, and Merikangas KR (2015) Major depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 54:37–44.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillet M, Cosin C, Schweitzer P, Pérès K, Catheline G, Swendsen J, and Mayo W (2016) Mood influences the concordance of subjective and objective measures of sleep duration in older adults. Front Aging Neurosci 8:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borisenkov MF, Fradkova LI, and Kolomeichuk SN (2012) Factors affecting chronotype of adolescents in the north according to multiple regression analysis. Chronobiol Int 29:1418–1419. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Vieira C, and Acebo C (1993) Association between puberty and delayed phase preference. Sleep 16:258–262. [DOI] [PubMed] [Google Scholar]
- Chan NY, Zhang J, Yu MWM, Lam SP, Li SX, Kong APS, Li AM, and Wing YK (2017) Impact of a modest delay in school start time in Hong Kong school adolescents. Sleep Med 30:164–170. [DOI] [PubMed] [Google Scholar]
- Chase-Lansdale PL, Moffitt RA, Lohman BJ, Cherlin AJ, Coley RL, Pittman LD, Roff J, and Votruba-Drzal E (2003) Mothers’ transitions from welfare to work and the well-being of preschoolers and adolescents. Science (80- ) 299:1548–1552. [DOI] [PubMed] [Google Scholar]
- Cohen J (1992) A power primer. Psychol Bull 112:155–159. [DOI] [PubMed] [Google Scholar]
- Compas BE, Oppedisano G, Connor JK, Gerhardt CA, Hinden BR, Achenbach TM, and Hammen C (1997) Gender differences in depressive symptoms in adolescence: Comparison of national samples of clinically referred and nonreferred youths. J Consult Clin Psychol 65:617–626. [DOI] [PubMed] [Google Scholar]
- Crowley SJ and Eastman CI (2018) Free-running circadian period in adolescents and adults. J Sleep Res 27:e12678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy JF, Cain SW, Chang A-M, Phillips AJK, Munch MY, Gronfier C, Wyatt JK, Dijk D-J, Wright KP, and Czeisler CA (2011) Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Natl Acad Sci 108:15602–15608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastman CI, Tomaka VA, and Crowley SJ (2017) Sex and ancestry determine the free-running circadian period. J Sleep Res 26:547–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eek F, Karlson B, Garde AH, Hansen åse M, and Ørbæk P (2012) Cortisol, sleep, and recovery - Some gender differences but no straight associations. Psychoneuroendocrinology 37:56–64. [DOI] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Calhoun S, Vgontzas A, Li Y, Gaines J, Liao D, and Bixler E (2016) Insomnia phenotypes based on objective sleep duration in adolescents: Depression risk and differential behavioral profiles. Brain Sci 6:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Carpenter L, and Kupfer DJ (1988) Sex differences in recurrent depression: are there any that are significant? Am J Psychiatry 145:41–45. [DOI] [PubMed] [Google Scholar]
- Frost A, Hoyt LT, Levy A, and Adam EK (2015) Daily life with depressive symptoms: Gender differences in adolescents ‘ everyday emotional experiences. J Adolesc 43:132–141. [DOI] [PubMed] [Google Scholar]
- Hale L, Berger LM, LeBourgeois MK, and Brooks-Gunn J (2011) A longitudinal study of preschoolers’ language-based bedtime routines, sleep duration, and well-being. J Fam Psychol 25:423–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynie DL, Lewin D, Luk JW, Lipsky LM, O’Brien F, Iannotti RJ, Liu D, and Simons-Morton BG (2018) Beyond Sleep Duration: Bidirectional Associations Among Chronotype, Social Jetlag, and Drinking Behaviors in a Longitudinal Sample of US High School Students. Sleep 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt TKA, Slack KS, and Berger LM (2017) Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse Negl 67:391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam Z, Akter S, Kochi T, Hu H, Eguchi M, Yamaguchi M, Kuwahara K, Kabe I, and Mizoue T (2018) Association of social jetlag with metabolic syndrome among Japanese working population: the Furukawa Nutrition and Health Study. Sleep Med 51:53–58. [DOI] [PubMed] [Google Scholar]
- Jiang X, Hardy LL, Baur LA, Ding D, Wang L, and Shi H (2015) Sleep duration, schedule and quality among urban Chinese children and adolescents: Associations with routine afterschool activities. PLoS One 10:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung SJ, Woo HT, Cho S, Park K, Jeong S, Lee YJ, Kang D, and Shin A (2017) Association between body size, weight change and depression: systematic review and meta-analysis. Br J Psychiatry 211:14–21. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, and Wittchen H-U (1998) The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF). Int J Methods Psychiatr Res 7:171–185. [Google Scholar]
- Keys A, Fidanza F, Karvonen MJ, Kimura N, and Taylor HL (1972) Indices of relative weight and obesity. J Chronic Dis 25:329–343. [DOI] [PubMed] [Google Scholar]
- Kim M (2014) Racial/ethnic disparities in depression and its theoretical perspectives. Psychiatr Q 85:1–8. [DOI] [PubMed] [Google Scholar]
- Koopman ADM, Rauh SP, van ’t Riet E, Groeneveld L, van der Heijden AA, Elders PJ, Dekker JM, Nijpels G, Beulens JW, and Rutters F (2017) The Association between Social Jetlag, the Metabolic Syndrome, and Type 2 Diabetes Mellitus in the General Population: The New Hoorn Study. J Biol Rhythms 32:359–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, and Johnson CL (2002) 2000 CDC growth charts for the United States: methods and development. Vital Heal Stat 11:1–190. [PubMed] [Google Scholar]
- Lau EYY, Wong ML, Ng ECW, Hui CCH, Cheung SF, and Mok DSY (2013) “Social jetlag” in morning-type college students living on campus: Implications for physical and psychological well-being. Chronobiol Int 30:910–918. [DOI] [PubMed] [Google Scholar]
- Levandovski R, Dantas G, Fernandes LC, Caumo W, Torres I, Roenneberg T, Hidalgo MPL, and Allebrandt KV (2011) Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol Int 28:771–778. [DOI] [PubMed] [Google Scholar]
- Mathew G, Li X, Hale L, and Chang A-M (2018) Sleep duration and social jetlag are independently associated with anxious symptoms in adolescents. In press. Chronobiol Int. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menard S (1995) Quantitative Applications in the Social Sciences: Applied Logistic Regression Analysis, Sage Publications, Thousand Oaks, CA. [Google Scholar]
- Merikangas K, Jian-ping H, Burstein M, Swanson S, Avenevoli S, Lihong C, Benjet C, Georgiades K, and Swendsen J (2011) Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Study-Adolescent Supplement. J Am Acad Child Adolesc Psychiatry 49:980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ming X, Radhakrishnan V, Kang L, and Pecor K (2016) Gender, headaches, and sleep health in high school students. J Women’s Heal 25:930–935. [DOI] [PubMed] [Google Scholar]
- Morita Y, Sasai-Sakuma T, Asaoka S, and Inoue Y (2015) The impact of a delayed sleep-wake schedule on depression is greater in women--A web-based cross-sectional study in Japanese young adults. Chronobiol Int 32:952–958. [DOI] [PubMed] [Google Scholar]
- Nahmod NG, Lee S, Master L, Chang A, Hale L, and Buxton OM (2018) Later high school start times associated with longer actigraphic sleep duration in adolescents. Sleep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesi J and Prinstein MJ (2015) Using social media for social comparison and feedback-seeking: Gender and popularity moderate associations with depressive symptoms. J Abnorm Child Psychol 43:1427–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan K, Carroll A, Reichman NE, and Corman H (2010) Mental illness as a risk factor for uninsurance among mothers of infants. Matern Child Health J 14:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojio Y, Nishida A, Shimodera S, Togo F, and Sasaki T (2016) Sleep duration associated with the lowest risk of depression/anxiety in adolescents. Sleep 1555–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, and Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Heal Organ 85:812–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park AL, Fuhrer R, and Quesnel-Vallée A (2013) Parents’ education and the risk of major depression in early adulthood. Soc Psychiatry Psychiatr Epidemiol 48:1829–1839. [DOI] [PubMed] [Google Scholar]
- Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, and Caspi A (2015) Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes 39:842–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira KM, Deeb-Sossa N, Harris KM, and Bollen K (2005) What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces 83:1567–1602. [Google Scholar]
- Perugi G, Musetti L, Simonini E, Piagentini F, Cassano GB, and Akiskal HS (1990) Gender-Mediated Clinical Features of Depressive Illness the Importance of Temperamental Differences. Br J Psychiatry 157:835–841. [DOI] [PubMed] [Google Scholar]
- Pesonen A, Martikainen S, Kajantie E, Heinonen K, Wehkalampi K, Lahti J, Strandberg T, and Räikkönen K (2014) The associations between adolescent sleep, diurnal cortisol patterns and cortisol reactivity to dexamethasone. Psychoneuroendocrinology 49:150–160. [DOI] [PubMed] [Google Scholar]
- Polanco-Roman L, Gomez J, Miranda R, and Jeglic E (2016) Stress-related symptoms and suicidal ideation: The roles of rumination and depressive symptoms vary by gender. Cognit Ther Res 40:606–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polugrudov AS, Panev AS, Smirnov VV., Paderin NM, Borisenkov MF, and Popov SV. (2016) Wrist temperature and cortisol awakening response in humans with social jetlag in the North. Chronobiol Int 33:802–809. [DOI] [PubMed] [Google Scholar]
- Randler C and Vollmer C (2013) Aggression in young adults — a matter of short sleep and social jetlag? Psychol Rep 113:754–765. [DOI] [PubMed] [Google Scholar]
- Randler C, Faßl C, and Kalb N (2017) From lark to owl: Developmental changes in morningness-eveningness from new-borns to early adulthood. Sci Rep 7:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raniti MB, Allen NB, Schwartz O, Waloszek JM, Byrne ML, Woods MJ, Bei B, Nicholas CL, and Trinder J (2016) Sleep duration and sleep quality: Associations with depressive symptoms across adolescence. Behav Sleep Med 2002:1–18. [DOI] [PubMed] [Google Scholar]
- Van Reen E, Sharkey KM, Roane BM, Barker D, Seifer R, Raffray T, Bond TL, and Carskadon MA (2013) Sex of college students moderates associations among bedtime, time in bed, and circadian phase angle. J Biol Rhythms 28:425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichman NE and Teitler J (2001) Fragile Families: Sample and design. Child Youth Serv Rev 23:303–326. [Google Scholar]
- Roberts RE and Duong HT (2014) The prospective association between sleep deprivation and depression among adolescents. Sleep 30–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T, Wirz-Justice A, and Merrow M (2003) Life between clocks: Daily temporal patterns of human chronotypes. J Biol Rhythm 18:80–90. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, and Merrow M (2004) A marker for the end of adolescence. Curr Biol 14:1038–1039. [DOI] [PubMed] [Google Scholar]
- Roepke SE and Duffy JF (2010) Differential impact of chronotype on weekday and weekend sleep timing and duration. Nat Sci Sleep 2:213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rood L, Roelofs J, Bögels SM, Nolen-Hoeksema S, and Schouten E (2009) The influence of emotion-focused rumination and distraction on depressive symptoms in non-clinical youth: A meta-analytic review. Clin Psychol Rev 29:607–616. [DOI] [PubMed] [Google Scholar]
- Salk RH, Petersen JL, Abramson LY, and Hyde JS (2016) The contemporary face of gender differences and similarities in depression throughout adolescence: Development and chronicity. J Affect Disord 205:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlotz W, Hellhammer J, Schulz P, and Stone AA (2004) Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med 66:207–214. [DOI] [PubMed] [Google Scholar]
- Schubert KO, Clark SR, Van LK, Collinson JL, and Baune BT (2017) Depressive symptom trajectories in late adolescence and early adulthood: a systematic review. Aust N Z J Psychiatry 51:477–499. [DOI] [PubMed] [Google Scholar]
- de Souza CM and Hidalgo MPL (2014) Midpoint of sleep on school days is associated with depression among adolescents. Chronobiol Int 31:199–205. [DOI] [PubMed] [Google Scholar]
- Spilková J, Chomynová P, and Csémy L (2017) Predictors of excessive use of social media and excessive online gaming in Czech teenagers. J Behav Addict 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2014) Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, Rockville, MD. [PubMed] [Google Scholar]
- Touitou Y (2013) Adolescent sleep misalignment: A chronic jet lag and a matter of public health. J Physiol Paris 107:323–326. [DOI] [PubMed] [Google Scholar]
- Vargas I, Mayer S, and Lopez-Duran N (2017) The cortisol awakening response and depressive symptomatology: The moderating role of sleep and gender. Stress Heal 33:199–210. [DOI] [PubMed] [Google Scholar]
- Vitale JA, Roveda E, Montaruli A, Galasso L, Weydahl A, Caumo A, and Carandente F (2015) Chronotype influences activity circadian rhythm and sleep: differences in sleep quality between weekdays and weekend. Chronobiol Int 32:405–415. [DOI] [PubMed] [Google Scholar]
- Vollmer C, Jankowski KS, Díaz-Morales JF, Itzek-Greulich H, Wüst-Ackermann P, and Randler C (2016) Morningness–eveningness correlates with sleep time, quality, and hygiene in secondary school students: A multilevel analysis. Sleep Med 30:151–159. [DOI] [PubMed] [Google Scholar]
- Vollmer C, Jankowski KS, Díaz-Morales JF, Itzek-Greulich H, Wüst-Ackermann P, and Randler C (2017) Morningness–eveningness correlates with sleep time, quality, and hygiene in secondary school students: a multilevel analysis. Sleep Med 30:151–159. [DOI] [PubMed] [Google Scholar]
- Wagmiller RLJ (2010) How representative are the Fragile Study families? A comparison of the early childhood longitudinal study-birth cohort and Fragile Families samples. Princet Univ Woodrow Wilson Sch Public Int Aff Cent Res Child Wellbeing, Work Pap 1–28. [Google Scholar]
- Wang X and Maguire-Jack K (2018) Family and environmental influences on child behavioral health: the role of neighborhood disorder and adverse childhood experiences. J Dev Behav Pediatr 39:28–36. [DOI] [PubMed] [Google Scholar]
- Wang L, Feng Z, Yang G, Yang Y, Wang K, Dai Q, Zhao M, Hu C, Zhang R, Liu K, et al. (2016) Depressive symptoms among children and adolescents in western china: an epidemiological survey of prevalence and correlates. Psychiatry Res 246:267–274. [DOI] [PubMed] [Google Scholar]
- Wheaton AG, Ferro GA, and Croft JB (2015) School start times for middle school and high school students – United States, 2011–12 school year. MMWR Morb Mortal Wkly Rep 64:809–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton AG, Jones SE, Cooper AC, and Croft JB (2018) Short sleep duration among middle school and high school students — United States, 2015. MMWR Morb Mortal Wkly Rep 67:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittmann M, Dinich J, Merrow M, and Roenneberg T (2006) Social jetlag: Misalignment of biological and social time. Chronobiol Int 23:497–509. [DOI] [PubMed] [Google Scholar]
- Xing G, Lin C-Y, and Xing C (2011) A comparison of approaches to control for confounding factors by regression models. Hum Hered 72:194–205. [DOI] [PubMed] [Google Scholar]
- Yong M, Fischer D, Germann C, Lang S, Vetter C, and Oberlinner C (2016) Are chronotype, social jetlag and sleep duration associated with health measured by Work Ability Index? Chronobiol Int 33:721–729. [DOI] [PubMed] [Google Scholar]
- Zimmerman FJ and Katon W (2005) Socioeconomic status, depression disparities, and financial strain: what lies behind the income-depression relationship? Health Econ 14:1197–1215. [DOI] [PubMed] [Google Scholar]
- van Zundert RMP, van Roekel E, Engels RCME, and Scholte RHJ (2013) Reciprocal associations between adolescents’ night-time sleep and daytime affect and the role of gender and depressive symptoms. J Youth Adolesc 44:556–569. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.