Abstract
Background
South Africa (SA) is an upper middle-income country with a human immunodeficiency virus (HIV) epidemic, an accelerated burden of non-communicable diseases, and a concurrent epidemic of tuberculosis. These conditions overwhelm a health system struggling under the pressure of restricted resources, including an insufficient workforce. Private practice has become more involved in the care of patients in the country but serves mainly those who are members of a Medical Aid. These Medical Aids will usually cover up to 100% of the costs for management of chronic kidney disease (CKD).
Summary
There are currently 2.3 nephrologists per million individuals, which is far lower than the global average and grossly inadequate to meet the nephrology care needs in SA. Covert chronic dialysis rationing has occurred in the public sector since the 1960s. However, the lack of formality triggered the formation of explicit rationing guidelines in one province. These guidelines have been ethically endorsed but not embraced nationally. The demand for hemodialysis (HD) has led some provinces to practicing “PD-First” programs. SA remains one of only 12 countries within Africa that perform renal transplantation, and it is the only country in Africa that relies on deceased donation for the majority of its transplants. The first kidney transplant in SA took place at the University of the Witwatersrand, Johannesburg, in 1966 and the first dialysis was performed by a general practitioner working in a town close to Johannesburg in 1957. The University of Cape Town successfully pioneered the transplantation of kidneys from HIV-positive donors to positive recipients. SA was the second country in the world to form a National Kidney Foundation as well as a renal society. Nephrology training is in place and incorporates master's and PhD programs in nephrology. Despite the numerous challenges, SA nephrologists have been among the leading researchers in nephrology from the African continent.
Keywords: Ubuntu, South Africa, History of nephrology, First dialysis, Kidney transplant, Human immunodeficiency virus, Registry data, Adolescent clinic, Nephrology training
The History of Nephrology in South Africa
Over the years, the development of nephrology has advanced mainly in the north, west, and south of the African continent. Poverty, civil strife, and government corruption – together with the high cost to healthcare of an overwhelming communicable disease profile – have left the remainder of the continent lagging [1].
In South Africa (SA) (Figure 1), presently rated as an upper middle-income country by the World Bank [2], nephrology has progressed almost pari passu with the developed world but on a much smaller scale. Apartheid influenced the decisions in relation to access to dialysis treatment for the underprivileged population and caused the concept of humanity and caring for each other (ubuntu) to be neglected [3]. The consequences of apartheid – which included discrimination in jobs, medical care, and education – are felt to this day. However, neglect for ubuntu continues unabated in the SA democratic era because restriction of access to dialysis therapy is still present. Fraud at the highest level of government has contributed to the healthcare deprivation which the SA population faces. A Judicial Commission of Inquiry into all allegations of fraud in the public sectors has been established to confirm the extent of the malfeasance.
Fig. 1.
Map of Africa and SA showing the 9 provinces in SA.
Back to the Past
The first hemodialysis (HD) acute treatment in SA was done by a general practitioner in a small town close to Johannesburg in 1957. The doctor, who had spent some time overseas and observed dialysis treatment, developed his own machine which was a derivative of the original Kolff rotating drum machine. The doctors in the old Johannesburg General Hospital performed their first acute dialysis procedure in 1958 and the Groote Schuur Hospital (GSH) doctors did their first treatment in 1959. The circumstances and outcomes of the procedures are unknown. Chronic HD clinics were established in the mid to late 1960s in Johannesburg and Cape Town, before developing in the rest of the country.
The first kidney transplantation operation in SA was performed at the University of the Witwatersrand, Johannesburg, in the old Johannesburg General Hospital in August 1966 [4]. The first transplant operation at the University of Cape Town (UCT), SA, was done in October 1967 and it was performed by Christiaan Barnard, the surgeon who very soon thereafter did the world's first human heart transplant operation at the same hospital. His kidney transplant patient lived for more than 20 years and died with a functioning graft. By 1973, the government public centers were the only units offering kidney transplantation; today the private sector has more transplant centers than the public centers (Table 1) [5]. Nevertheless, the transplant centers are presently restricted to a few major cities in SA, making the accessibility of this treatment limited and thereby condemning a proportion of patients to a lifetime of dialysis treatment.
Table 1.
Number of kidney transplants in South African public and private nephrology sectors in 2016
| Deceased donor |
Living donor |
Living donor (unrelated) |
Total | ||||
|---|---|---|---|---|---|---|---|
| C | A | C | A | C | A | ||
| Western Cape (public) | 3 | 28 | 1 | 16 | 0 | 3 | 61 |
| Western Cape (private) | 0 | 22a | 0 | 25 | 0 | 9 | 56 |
| Gauteng (public) | 3 | 25 | 0 | 25 | 0 | 0 | 32 |
| Gauteng (private) | 3b | 30c | 5 | 20 | 0 | 11 | 69 |
| KwaZulu-Natal (public) | 0 | 0 | 0 | 9 | 0 | 0 | 9 |
| KwaZulu-Natal (private) | 1 | 11 | 0 | 10 | 0 | 3 | 25 |
| Free State (public) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Free State (private) | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Total | 10 | 126 | 6 | 86 | 0 | 26 | 254 |
The kidney transplant rate for 2016 was 4.5 per million individuals. Based on data from Organ Donor Foundation, SA. Modified from the SA Registry of Davids et al. [5]. C, child recipient aged <18 years; A, adult recipient aged 18 years or older.
Includes 1 kidney-liver transplant.
Includes 1 kidney-liver transplant.
Includes 2 kidney-liver transplants and 1 kidney-pancreas transplant.
A major success for the publicity of treatment for end-stage kidney disease (ESKD) was the establishment of both the SA Renal Society (SARS) and the National Kidney Foundation of SA (NKFSA) in the same month and year, i.e., March of 1967. Both of these bodies were able to use their influence to lobby the authorities for recognition and the supply of facilities to treat patients with ESKD. SA was the second country in the world (after the USA) to form both a National Kidney Foundation and a Renal Society. Other important landmarks in the history of nephrology in SA are the formation of the SA Transplant Society (SATS) which was formally ratified and had first-time officers elected at its first congress, held in Durban, in April 1970. Also, the SA Renal Registry was first established in 1977. This was active up until 1994. It was resurrected again in 2012 and, to date, it provides information on patient numbers but, as of yet, not on diseases and outcomes [6].
Clinical Nephrology Care and Practice in SA at Present
The evolving epidemic of communicable diseases, particularly human immunodeficiency virus (HIV) and tuberculosis [7], and an ever-increasing burden of non-communicable diseases [8] fuel the increasing incidence of chronic kidney disease (CKD). This problem is compounded by limited numbers of nephrologists [9], limited resources, poor access to renal replacement therapy (RRT) [10], and a high prevalence of poverty.
Predialysis Care
The extent of CKD in SA is unknown due to the lack of large-scale epidemiological studies. There is also no registry data on predialysis CKD follow-up care. However, from what is known anecdotally, the extent of CKD is widespread. Mayosi et al. [11] demonstrated that between 1999 and 2009 the mortality per 100,000 individuals, related to nephritis or nephrosis, increased across all age groups (as did mortality from hypertension and diabetes). This is on a background of a now well-established genetic predisposition to CKD in people of African ancestry. The strongest link has been associated with APOL1 and its predisposition to hypertension and focal segmental glomerulosclerosis (either idiopathic or HIV related) [12].
SA has the world's largest HIV epidemic, with approximately 7.9 million people living with HIV [13]. Though effective antiretroviral therapy has been available since 1996, it was not until external pressure was applied to the government that SA finally launched its antiretroviral therapy roll out in 2004 [14]. SA now has the largest HIV treatment program in the world. HIV-associated renal diseases overwhelm acute, chronic, and predialysis renal services. This has placed an enormous strain on a health system already struggling under the pressure of restricted resources and compounded by a coexisting tuberculosis epidemic [15]. Renal involvement occurs due to HIV itself or/and due to the opportunistic infections frequently accompanying HIV infection (as well as the drugs used in treatment). There is also an increasing prevalence of non-communicable diseases (obesity, hypertension, and diabetes) as people are living longer on antiretroviral therapy [12].
Adolescent Nephrology Services
There is a lack of access to adolescent-friendly and transitional services for predialysis care throughout SA. HIV is currently the second leading cause of death among adolescents worldwide [16] and it contributes to renal disease and has an impact on primary caregivers [17]. Challenges are further amplified by limited access to health care, scarce RRT [10], and high rates of sexual and physical abuse [18]. Complicating their care is the fact that if an adolescent presents for the first time with an illness at 12 years, then treatment is designated to an adult hospital. In rural SA, it is not uncommon for an adult nephrologist to treat children with renal disease; there are far fewer pediatric nephrologists in SA than the adult counterpart.
In 2014, the Western Cape Province of SA approved a UCT application submitted toward “innovative solutions for new possibilities and bold solutions to better patient care” aimed at creating an adolescent-centric service in nephrology. The approach involved young-patient input to help design a service that would be utilized for and cater to the medical and psychosocial needs of the patients and their families. Furthermore, this service presently provides a training platform where adult nephrologists can learn approaches to young patients. It also plays a fundamental role in the transition of pediatric patients to adult nephrology services.
Rationing of RRT in SA
SA has one of the highest Gini coefficients in the world [19]. In 2016, the SA renal registry reported a population of 55.91 million being serviced in a 2-tiered health system. The registry describes a private sector serving approximately 16% of the population while the remaining 84% are serviced by an under-resourced public health system (Table 2) [5]. The rate of dialysis in the private sector is on a par with the best in the world but the rate among the poor majority lags regretfully [20]. Public sector medical care, including dialysis, is free for those who cannot afford it. However, due to the high expense of RRT, dialysis is rationed. Covert rationing in the public sector has occurred since the 1960s, with no clear policy guiding the selection process [20]. This lack of formality triggered a response from nephrologists in the Western Cape. Formal guidelines were developed that involved wide consultation with relevant stake holders and were based on the patient's ability to be transplanted. The guidelines are explicit, they have been accepted by the local provincial government, and they have withstood the scrutiny of the Human Rights Commission [20, 21]. They have been ethically endorsed and strictly adhered to and can be defended morally and legally. However, the Western Cape Province is the only province that has officially adopted this priority-setting policy. Of all patients presenting to GSH in the Western Cape Province between 2008 and 2012, 53.9% were not selected for the program [22]. The selection criteria therefore force tragic choices and additional challenges. If a non-selected patient is not able to afford the alternative, which is private medical care, then a palliative care plan needs to be implemented.
Table 2.
Number of RRT patients by province and sector in SA in 2016
| Eastern Cape | Free State | Gauteng | KwaZulu- Natal | Limpopo | Mpumalanga | North West | Northern Cape | Western Cape | All | |
|---|---|---|---|---|---|---|---|---|---|---|
| Publicsector | 299 | 235 | 957 | 431 | 141 | 10 | 162 | 64 | 876 | 3,175 |
| Privatesector | 746 | 342 | 2,298 | 1,591 | 268 | 265 | 303 | 82 | 1,187 | 7,082 |
| Total | 1,045 | 577 | 3,255 | 2,022 | 409 | 275 | 465 | 146 | 2,063 | 10,257 |
Modified from the SA Registry of Davids et al. [5].
HD and Peritoneal Dialysis Services in SA
SA performs 85% of the peritoneal dialysis (PD) in Africa, with the public sector being the highest provider [23]. In 2016, there were 3,175 patients on dialysis in the public sector in SA, 881 (27.8%) of whom were on PD. This is compared to 426 of a total 7,081 patients (6.0%) who were offered PD in the private sector [5]. PD should be an ideal form of RRT as it is more suitable for those living in rural areas and it can reduce the HD demand. This demand has led some provinces to practice “PD-First” unless there are compelling medical, physical, or psychosocial factors precluding PD. In a study from UCT describing outcomes of a PD-First program, patient survival was not inferior to the survival in countries with a similar GDP or other PD-First programs, or developed countries reporting PD registry data. This can be partially attributed to the strict dialysis selection criteria previously described [24]. However due to high rates of poverty and a lack of formal housing, electricity, and sanitation as well as limited or no home visits (because of a threat to staff safety), PD has a unique set of challenges in SA [24].
Cost comparisons between CAPD and HD are complex [25, 26]. Currently in SA the cost of PD is either greater than or similar to that of HD [27]. There is lack of regulation of PD fluid costs compounded by the lack of larger PD numbers which can bring down the cost of fluid seen in other countries [1]. Reuse of dialyzers also significantly reduces HD costs in some regions.
Renal Transplantation Services in SA
SA remains one of only 12 countries within Africa that perform renal transplantation and the only country in Africa that relies on deceased donation for the majority of its transplants [28]. Transplantation plays a key role in the public sector as it turns over the rationed spaces for HD. Despite the known benefits, sub-Saharan Africa falls into the lowest quartile of transplantation rates worldwide [29]. Religious restrictions to donation, declining numbers of deceased donors, and long waiting lists have limited transplantation rates. The lack of donor availability prompted the transplantation of kidneys from HIV-positive donors to positive recipients pioneered at UCT, thereby increasing the pool of donor kidneys [30]. The program has shown success with outcomes similar to those of non-HIV patients [30] and better than those of extended criteria donor transplantation [31].
Cost of RRT in SA
In SA the cost of sustaining 1 person on dialysis per annum is approximately ZAR 200 000 per year (USD 13,900). This cost can be conceptualized within the constraints of allocated health budgets. In the 2015/2016 financial year, Statistics SA reported a government allocation to health care per person of ZAR 3,332 for those without medical aid (i.e., USD 231) [32]. Compare this to the USA (with an allocation in 2016 of USD 10,348), Switzerland (USD 7,919), or Australia (USD 4,708) [33]. Dialysis consumes a large proportion of any health budget. Due to their high cost, chronic renal replacement programs in many low- and low middle-income countries are unable to be sustained. This supports introduction of the practice of rationing of dialysis so that at least a few may be treated and not die.
Nephrology Clinical Training in SA
Workforce shortage remains a critical factor impeding the growth of nephrology service provision in SA [34]. There are currently 130 registered nephrologists in SA; this is 2.3 nephrologists per million individuals, which is far lower than the global average [35]. In SA, to qualify to be trained in nephrology, the trainee is required to first have obtained a postgraduate fellowship, e.g., fellow of the College of Physicians (FCP) or equivalent in internal medicine. The International Society of Nephrology (ISN) Global Kidney Health Atlas (GKHA) has, however, shown that the structure of nephrology training for African nephrologists is not uniform. Although most are required to be trained as nephrologists after completing general internal medicine training, there are others who proceeded to nephrology training after obtaining a basic undergraduate medical qualification.
In SA, the duration of nephrology training (after general internal medicine) is usually 2 years. During this time, a trainee is expected to become knowledgeable and competent in various aspects of clinical care of the patient with kidney disease. This training includes care of the ICU AKI patient, treatment of various complications of CKD, treatment of various forms of glomerular diseases, dialysis care for ESRD patients, and competence in performance of various procedures such as renal biopsy and catheter insertion (tunneled and no-tunneled).
Challenges in Improving Clinical Nephrology Training in SA
SA does have the facilities for the diagnosis and treatment of patients in all of the recognized academic centers. Therefore, in these centers, nephrology services (including pathology, predialysis care, in-centre dialysis programs, and transplant programs) are usually available to aid with the provision for training of fellows in nephrology.
Because the training centers are few, SA consequently has a relative “low nephrology workforce.” This can be seen by observing that the concentration and saturation of nephrology services (including private practice) is to be found within the very large cities of SA, where the academic centers are to be found. In fact, many parts of SA have a low or nonexistent nephrology workforce (with figures approaching that reported by the ISN-GKHA). Unwillingness of qualified nephrologists to move away from the big cities, together with the fear of a lack of opportunities in the smaller more rural areas, is another reason for the relative shortage of a workforce in SA.
The government provision for increasing nephrology training is inadequate. At the GSH-UCT in Cape Town, only 1 salaried slot is available for an SA to be trained every 2 years. Whatever remaining slots are available are usually taken up by supernumerary trainees from sub-Saharan African countries. Thus, from this single center, only 5 nephrologists are able to join the nephrology workforce in SA every decade. There is therefore an urgent need at various tiers of government (national and provincial) to improve funding for training.
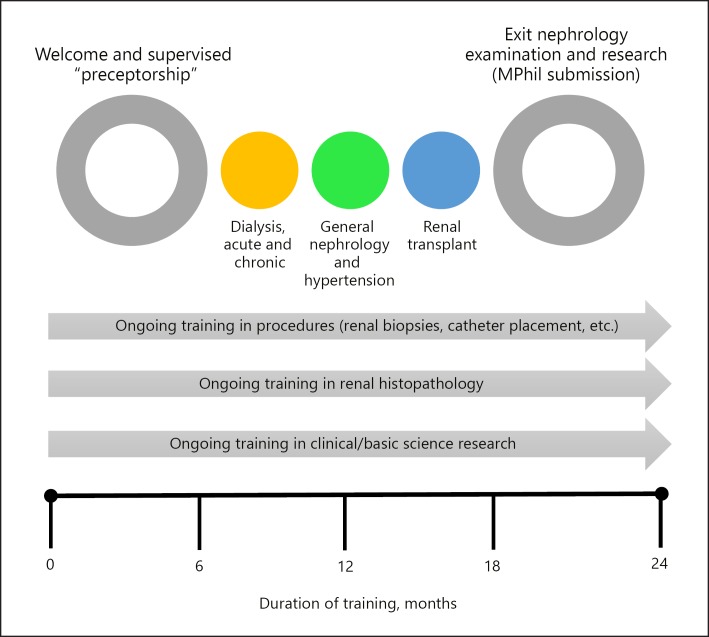
Another challenge in nephrology training in other parts of Africa is the lack of a structured training program in nephrology. In fact, to ensure that an adequate program is in place at the training centers (host centers), the ISN Fellowship Committee requires that the program in the host center be set out prior to ISN approval for the fellowship. Therefore, most accepted host centers have established formal, structured working modules. An example of the program used at the GSH is illustrated in Figure 2. This has worked well and it has made the process of transition to a higher level of education easy, especially for those arriving from African countries where the level of infrastructure may not be as developed as in SA.
Fig. 2.
Structure of nephrology training at the UCT.
Nephrology Research Training in SA
The Health Professionals Council of SA and the College of Medicine of SA introduced a research component (MMed and MPhil) as part of the postgraduate fellowship training in SA. The proximity and affiliation to institutional research organizations (e.g., human genetics, molecular laboratories, bio-banking facilities, etc). and readily available and functional research ethics committees have helped with the capacity to teach methods in research and improve the quality of the postgraduate qualifications. A few trainees, after successfully completing the College of Medicine of SA examinations in nephrology, are able to further extend their studies and graduate with PhD degrees.
In other parts of Africa, there is a limited capacity for research training in nephrology [36]. Due to a depleted workforce in several regions, many potential trainees often cannot spend time on research, as they are overwhelmed by the necessity of providing primary healthcare for their population. The poor salaries on offer also compel many to go into clinical practice to earn money to support their families. The limited capacity for research also becomes evident when one looks at the participation in global kidney disease observational studies and clinical trials. Very few African sites are able to take part, often because of a lack of expertise in this area [37]. Other barriers to nephrology research in Africa include the absence of ethics committees in some institutions, a lack of utility for processing and storage of samples, and a lack of expertise in methodological approaches for various forms of research.
SA nephrologists have been among the leading researchers in Nephrology from the African continent. Many have represented the continent at important ISN, ASN, and ERA-EDTA functions. Because of their research standing they have served as reviewers for – and as editorial board members of – leading medical and nephrology journals. They are therefore well placed to offer teaching in research and advice on the various aspects of information gathering, publication of data, and interaction with research ethics committees.
Conclusion
Despite the many challenges, SA remains at the apex of provision of comprehensive care for patients with kidney diseases when compared to other countries in the continent. It remains critically important to continue to train nephrologists in order to improve the numbers of the workforce locally as well as in other countries on the continent. Another major goal in SA must be to provide dialysis to all of its population that require it.
SA has the will to continue to provide leadership for the next generation of nephrologists in SA and on the continent.
Disclosure Statement
The authors have no conflict of interests to disclose.
Acknowledgement
Most of the information described under Back to the Past was provided by Prof. A.M. Meyers, Honorary Professor, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, and Chairperson of the NKFSA.
References
- 1.Swanepoel CR, Wearne N, Okpechi IG. Nephrology in Africa—not yet uhuru. Nat Rev Nephrol. 2013 Oct;9((10)):610–22. doi: 10.1038/nrneph.2013.168. [DOI] [PubMed] [Google Scholar]
- 2.World Bank Open Data http://data.worldbank.org/indicator. [Google Scholar]
- 3.Moosa MR, Kidd M. The dangers of rationing dialysis treatment: the dilemma facing a developing country. Kidney Int. 2006 Sep;70((6)):1107–14. doi: 10.1038/sj.ki.5001750. [DOI] [PubMed] [Google Scholar]
- 4.Fabian J, Maher H, Bentley A, Gaylard P, Crymble K, Rossi B, Aucamp L, Gottlich E, Loveland J, Botha JR, et al. Favourable outcomes for the first 10 years of kidney and pancreas transplantation at Wits Donald Gordon Medical Centre, Johannesburg, South Africa. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2016;106((2)):172–176. doi: 10.7196/SAMJ.2016.v106i2.10190. [DOI] [PubMed] [Google Scholar]
- 5.Davids MR, Jardine T, Marais N, Jacobs JC. South African Renal Registry Annual Report 2016. Afr J Nephrol. 2018;21((1)):61–72. [Google Scholar]
- 6.Davids MR, Eastwood JB, Selwood NH, Arogundade FA, Ashuntantang G, Benghanem Gharbi M, et al. A renal registry for Africa: first steps. Clin Kidney J. 2016 Feb;9((1)):162–7. doi: 10.1093/ckj/sfv122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanifer JW, Jing B, Tolan S, Helmke N, Mukerjee R, Naicker S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014 Mar;2((3)):e174–81. doi: 10.1016/S2214-109X(14)70002-6. [DOI] [PubMed] [Google Scholar]
- 8.Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet. 2009 Sep;374((9693)):934–47. doi: 10.1016/S0140-6736(09)61087-4. [DOI] [PubMed] [Google Scholar]
- 9.Sharif MU, Elsayed ME, Stack AG. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J. 2016 Feb;9((1)):11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015 May;385((9981)):1975–82. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 11.Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM, Lancet South Africa team Health in South Africa: changes and challenges since 2009. Lancet. 2012 Dec;380((9858)):2029–43. doi: 10.1016/S0140-6736(12)61814-5. [DOI] [PubMed] [Google Scholar]
- 12.Swanepoel CR, Atta MG, D'Agati VD, Estrella MM, Fogo AB, Naicker S, et al. Conference Participants Kidney disease in the setting of HIV infection: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2018 Mar;93((3)):545–59. doi: 10.1016/j.kint.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.THE FIFTH SOUTH AFRICAN NATIONAL HIV PREVALENCE, INCIDENCE, BEHAVIOUR AND COMMUNICATION SURVEY, 2017 (SABSSM V1) http://www.hsrc.ac.za/uploads/pageContent/9234/SABSSMV_Impact_Assessment_Summary_ZA_ADS_cleared_PDFA4.pdf 2017. [Google Scholar]
- 14.Swanepoel CR, Wearne N, Duffield MS, Okpechi IG. The evolution of our knowledge of HIV-associated kidney disease in Africa. Am J Kidney Dis. 2012 Oct;60((4)):668–78. doi: 10.1053/j.ajkd.2012.04.034. [DOI] [PubMed] [Google Scholar]
- 15.Moosa MR, Meyers AM, Gottlich E, Naicker S. An effective approach to chronic kidney disease in South Africa. S Afr Med J. 2016 Jan;106((2)):156–9. doi: 10.7196/SAMJ.2016.v106i2.9928. [DOI] [PubMed] [Google Scholar]
- 16.W.H.O. Health of the Worlds Adolescents; A second chance in the second decade. http://wwwwhoint/adolescent/second-decade Retrieved June, 05: 2016. [Google Scholar]
- 17.UNAIDS Fact sheet. Global statistics. http://wwwunaidsorg/en/resources/campaigns/2014/2014gapreport/factsheet Retrieved June, 05: 2016. [Google Scholar]
- 18.Preventing child maltreatment: a guide to taking action and generating evidence https://www.who.int/violence_injury_prevention/publications/violence/child_maltreatment/en/ [Google Scholar]
- 19.The World Bank in South Africa https://www.worldbank.org/en/country/southafrica/overview. [Google Scholar]
- 20.Moosa MR, Wearne N. Invited Commentary Should We Be Rationing Dialysis in South Africa in the 21st Century? Perit Dial Int. 2018 Mar-Apr;38((2)):84–8. doi: 10.3747/pdi.2017.00179. [DOI] [PubMed] [Google Scholar]
- 21.Moosa MR, Maree JD, Chirehwa MT, Benatar SR. Use of the ‘accountability for reasonableness’ approach to improve fairness in accessing dialysis in a middle-income country. PLoS One. 2016 Oct;11((10)):e0164201. doi: 10.1371/journal.pone.0164201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilonzo KG, Jones ES, Okpechi IG, Wearne N, Barday Z, Swanepoel CR, et al. Disparities in dialysis allocation: an audit from the new South Africa. PLoS One. 2017 Apr;12((4)):e0176041. doi: 10.1371/journal.pone.0176041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abu-Aisha H, Elamin S. Peritoneal dialysis in Africa. Perit Dial Int. 2010 Jan-Feb;30((1)):23–8. doi: 10.3747/pdi.2008.00226. [DOI] [PubMed] [Google Scholar]
- 24.Davidson B, Crombie K, Manning K, Rayner B, Wearne N. Outcomes and Challenges of a PD-First Program, a South-African Perspective. Perit Dial Int. 2018 May-Jun;38((3)):179–86. doi: 10.3747/pdi.2017.00182. [DOI] [PubMed] [Google Scholar]
- 25.Karopadi AN, Mason G, Rettore E, Ronco C. Cost of peritoneal dialysis and haemodialysis across the world. Nephrol Dial Transplant. 2013 Oct;28((10)):2553–69. doi: 10.1093/ndt/gft214. [DOI] [PubMed] [Google Scholar]
- 26.Sennfält K, Magnusson M, Carlsson P. Comparison of hemodialysis and peritoneal dialysis—a cost-utility analysis. Perit Dial Int. 2002 Jan-Feb;22((1)):39–47. [PubMed] [Google Scholar]
- 27.Wearne N, Kilonzo K, Effa E, Davidson B, Nourse P, Ekrikpo U, et al. Continuous ambulatory peritoneal dialysis: perspectives on patient selection in low- to middle-income countries. Int J Nephrol Renovasc Dis. 2017 Jan;10:1–9. doi: 10.2147/IJNRD.S104208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bello AK, Levin A, Tonelli M, Okpechi IG, Feehally J, Harris D, et al. Assessment of Global Kidney Health Care Status. JAMA. 2017 May;317((18)):1864–81. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia GG, Harden P, Chapman J. The global role of kidney transplantation. Curr Opin Nephrol Hypertens. 2012 May;21((3)):229–34. doi: 10.1097/MNH.0b013e328352586d. [DOI] [PubMed] [Google Scholar]
- 30.Muller E, Barday Z, Mendelson M, Kahn D. HIV-positive-to-HIV-positive kidney transplantation—results at 3 to 5 years. N Engl J Med. 2015 Feb;372((7)):613–20. doi: 10.1056/NEJMoa1408896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stock PG, Barin B, Murphy B, Hanto D, Diego JM, Light J, et al. Outcomes of kidney transplantation in HIV-infected recipients. N Engl J Med. 2010 Nov;363((21)):2004–14. doi: 10.1056/NEJMoa1001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Public Healthcare How much per person? http://www.statssa.gov.za/?p=10548. [Google Scholar]
- 33.Health Spending https://data.oecd.org/healthres/health-spending.htm. [Google Scholar]
- 34.Barsoum RS, Khalil SS, Arogundade FA. Fifty years of dialysis in Africa: challenges and progress. Am J Kidney Dis. 2015 Mar;65((3)):502–12. doi: 10.1053/j.ajkd.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Osman MA, Alrukhaimi M, Ashuntantang GE, Bellorin-Font E, Benghanem Gharbi M, Braam B, et al. Global nephrology workforce: gaps and opportunities toward a sustainable kidney care system. Kidney Int Suppl (2011) 2018 Feb;8((2)):52–63. doi: 10.1016/j.kisu.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Okpechi IG, Alrukhaimi M, Ashuntantang GE, Bellorin-Font E, Benghanem Gharbi M, Braam B, et al. Global capacity for clinical research in nephrology: a survey by the International Society of Nephrology. Kidney Int Suppl (2011) 2018 Feb;8((2)):82–9. doi: 10.1016/j.kisu.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okpechi IG, Swanepoel CR, Venter F. Access to medications and conducting clinical trials in LMICs. Nat Rev Nephrol. 2015 Mar;11((3)):189–94. doi: 10.1038/nrneph.2015.6. [DOI] [PubMed] [Google Scholar]