Abstract
Several techniques exist to manage bone defects in patients: bone grafts (autograft, allograft, xenograft), use of synthetic bone substitutes, or use of the products of bone regenerative medicine. Studies generally focus on their efficacy, but few focus on their acceptance. Our objectives were to assess their theoretical acceptance among the French general population, and to identify issues justifying refusals, by mean of an open e-questionnaire. The questionnaire was submitted to a general French population, and explained these techniques in an understandable way. Participants were asked to say whether they would accept or refuse these techniques, specifying why in case of refusal (fear of the technique, ethical reasons, religious reasons). In total, 562 persons participated. Autograft and use of the products of bone regenerative medicine were the most accepted techniques (93.4% and 94.1%, respectively). Xenograft was the least accepted technique (58.2%). Most refusals were due to fear such as failure, pain, infection (autograft 8%, allograft 14.9%, xenograft 25.3%, synthetic bone substitutes 14.6%, and products of bone regenerative medicine 6.8%). Ethical reasons were mostly mentioned for allograft (6.4%) and xenograft (18.3%). Religious reasons were scarcely mentioned, only for xenograft (1.2%). Thus, acceptance of techniques does not seem to be greatly linked to sociodemographic characteristics in France. However, other countries with their own cultural, religious, and population patterns may show different levels of acceptance. This study shows that bone regenerative medicine is a promising research direction, reaching biological and also humanist quality standards, expected to improve the health of patients. Information is still the cornerstone to defuse issues about fear.
Keywords: allograft, autograft, xenograft, tissue engineering, informed consent, orthopedics, dentistry
Introduction
Infections, tumors, trauma, and surgery are some of the different possible etiologies for bone defects1. Although there are multiple solutions to handle these bone defects according to their anatomical situation and their size, autogenous bone graft is still the gold standard1–5. Indeed, this technique meets several of the characteristics of an ideal bone replacement material: it is biocompatible, osteoconductive, osteoinductive, osteogenic, logically similar to bone in its structure, porous, and mechanically resistant1,3. It avoids immunogenicity or rejection problems, and disease transmission risks1,6. Nevertheless, it shows significant disadvantages, such as the presence of a secondary operative site—the donor site—which can be a stage for supplementary comorbidities such as chronic pain or infection, for example4,7,8. Moreover, surgeons are often faced with a lack of quantity of autogenous bone.
Other techniques have been developed to manage bone defects, to try to overcome this quantity issue. Bone allografts are bone graft materials taken from another human, and bone xenografts are bone graft materials taken from another species, meaning animal tissue. However, these techniques present some biological limitations since the material involved is not osteogenic, little osteoinductive, but mainly only osteoconductive9,10. There are ethical and theological limitations as well; few studies have focused on the acceptance of these techniques by patients, and most have looked at their efficacy11. Certainly, bone is a less symbolic organ than others, such as a heart whose transplantation from an animal (a baboon) historically generated much more controversy12,13. However, a xenograft could present some difficulties for Jewish, Christian, Hindu, Muslim, or patients of other religions, as religious beliefs could conflict with specific healthcare situations14,15. Knowing that followers of Hinduism consider cows as sacred laborers, and that the sacred texts of the Jewish and Islamic religions prohibit persons of these religions from ingesting porcine products, the use of animal-derived graft material could cause ethical dilemmas that could cause religious distress for patients14,16–19. Ethical concerns about animal life may also lead to refusal11. Still, interest in xenografts persists today because scientists and surgeons observe that human tissues cannot be obtained in sufficient quantity20. The same goes for allografts, whose applications are expanding, meaning that bone banks have reported difficulties in meeting demand for more than 20 years21, and despite concerns about supply and safety1,4,11,20–24. Many authors mention a risk of virus transmission linked to allografting1,11,20,22,23,25, whereas xenografting would be less risky20,26 except for the transmission of specific zoonotic diseases11,27 such as porcine endogenous retrovirus and bovine spongiform encephalopathy1,2,20, although no evidence of this has been found after a xenotransplantation28.
Other materials that can be used for the management of bone defects are bone substitutes (hydroxyapatite, calcium sulfate, calcium phosphate ceramics, bioactive glasses, etc.)1,2,29. Each of them can be used selectively for different clinical applications concerning bone defects1, such as spine fusion30, periodontal procedures31, vertebroplasty32, management of long bone fractures33, etc. Because some of these bone substitutes are synthetically manufactured, the assumption could be made that patients would be more likely to accept their use for surgical procedures. However, bone substitutes also present some limitations, which do not make them ideal materials. Some are brittle, some resorb too fast, some do not present sufficient mechanical strength, etc.1
Hence, scientists and surgeons are working together to develop a new strategy in the management of bone defects. Sophisticated nano-implants aimed at promoting bone regeneration are currently under development, especially using polymeric substitutes as scaffolds34–36. This strategy is part of regenerative medicine. Schematically, cells from the patient are cultured in a laboratory on a sterile media (named “scaffold”), while being stimulated with growth factors. The bio-implant would then be implanted in the bone defect area to promote bone formation, resorbing as neo-bone tissue forms37,38. This technique presents real advantages: speed of bone regeneration, quality of the neo-bone tissue, biological characteristics (osteoconduction, osteoinduction, and osteogenesis), and source of the material. Indeed, the cells come from the patient him/herself, avoiding the need for an external donor and thus overcoming donor species issues38. Moreover, the bio-implants can ultimately be made of synthetic materials and the patient’s cells, avoiding the need for a secondary operative site and associated complications4.
Nevertheless, although the precision of these techniques will certainly evolve, a question remains unsolved. Do they bring a real benefit in terms of acceptance for the patient? At a time in which the autonomy of patients is advocated39, would such sophisticated techniques be accepted by patients? Are there any issues about ethics, religion, or simply fear? Surgeons have to consider cultural dispositions and patients’ choices. To highlight any potential issue, we undertook a survey among French subjects about their theoretical acceptance of the described techniques.
Material and Methods
Study Design
The study took place in the form of a voluntary internet-based open questionnaire about the theoretical acceptance of different techniques to manage bone defects: bone grafting (auto-, allo-, and xenograft), use of synthetic bone substitutes, and use of the products of bone regenerative medicine.
Ethical Approval and Recruitment
This study was submitted to the Ethical Committee of the University Hospitals of Strasbourg, France, and received the authorization n° 2018-66. The questionnaire was available from March 20th 2018 to June 1st 2018. Participants were recruited through shared social network posts and e-mails containing a link to the questionnaire. They were informed at the beginning of the questionnaire that their participation would be anonymous. Moreover, no answers could be submitted unless the participants accepted an ethical statement stipulating that, by clicking on the button “send the answers” at the end of the questionnaire, they acknowledged having been informed of the purpose of the study; having participated freely; and having understood that their participation was totally anonymous.
Study Subjects
The study was intentionally designed to reach the general French population. Thus, the only exclusion criteria were: (1) subjects under the age of 18, (2) non-French subjects, and (3) subjects who did not complete the whole questionnaire.
Questionnaire
A first version of the questionnaire was submitted to a panel of 30 randomly chosen participants to evaluate its relevance and its comprehensibility, as a pilot test. Once the panel fully understood the questions with no ambiguity in the possible answers, the study could begin. The final questionnaire was submitted through Google Forms© (Google, Mountain View, CA, USA).
The first questions focused on participant characteristics: age, sex, nationality, education level, and position regarding religion.
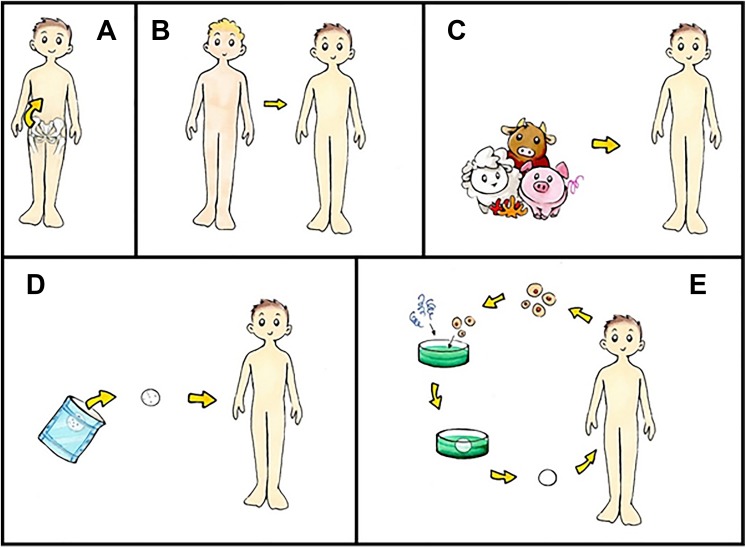
After these questions, five techniques for the management of bone defects were explained, so as to be understandable to the general population, and accompanied by a simple explanatory schematic representation (Fig. 1).
Autologous bone graft: bone material is first removed from one area of your body (usually the hip bone area) and then grafted into the area of your bone loss.
Allograft: bone material is taken from an individual of the same species (another human); it is then treated by decontamination / sterilization before being grafted into the area of your bone loss.
Xenograft: bone material is taken from an individual of a different species (an animal—coral and cattle (beef) in general); it is then treated by decontamination / sterilization before being grafted into the area of your bone loss.
Use of a synthetic bone substitute: a biocompatible, bone-miming sterile material is implanted in the area of your bone loss, before natural bone replaces it.
Use of the products of the bone regenerative medicine: your own cells are cultured in a laboratory on sterile media, stimulating them. These supports (with the cells) are then implanted in the area of your bone loss in order to accelerate the formation of the bone.
Figure 1.
Schematic representation of 5 techniques for the management of bone loss (A: autograft; B: allograft; C: xenograft; D: use of synthetic bone substitutes; E: use of the products of bone regenerative medicine).
Participants were then asked two questions:
“If necessary, would you agree to be treated with any of these techniques?” Participants were asked to give one answer for each of the five described techniques, choosing among “never,” “rather no,” “rather yes,” or “yes.” “Yes” and “rather yes” answers were considered as acceptance, while “rather no” and “never” were considered as refusal of the technique.
“What are the reasons of your possible refusal (several possible choices)?” Participants were asked to give one or more answers among “none, because I answered ‘yes’ or ‘rather yes’,” “fear of the technique (failure, side effects, pain, infection / transmission, fear of the operation),” “ethical reasons,” “religious reasons,” and “other.”
A space for free expression was then provided to participants who wanted to develop their answer.
Processing of Data and Statistical Analysis
The results were generated by Google Forms© in the form of Excel© tables. Statistical analysis was performed using Excel© and R (R Core Team (2017), Vienna, Austria. https://www.Rproject.org/). Pearson’s chi-squared test was used to assess significant differences between proportions.
Results
Acceptance or Non-Acceptance
Among all the answers, only those from French subjects (having answered “French” to the nationality question) were included. In total, 562 questionnaires were then analyzed. Participants’ characteristics are detailed in Table 1.
Table 1.
Participants’ Characteristics – Sex, Age, Education Level, and Positioning Regarding Religion.
| Characteristic | Groups | Number of participants (n) | Proportion (in %) |
|---|---|---|---|
| Sex | Female | 339 | 60.3 |
| Male | 223 | 39.7 | |
| Age | 18–25 | 226 | 40.2 |
| 26–35 | 170 | 30.3 | |
| 36–45 | 66 | 11.7 | |
| 46–60 | 55 | 9.8 | |
| More than 60 | 45 | 8 | |
| Education level | Before high school degree | 49 | 8.7 |
| High school degree | 103 | 18.3 | |
| 3 years after high school degree (bachelor) | 126 | 22.5 | |
| 5 years after high school degree (master) | 108 | 19.2 | |
| More than 5 years after high school degree | 176 | 31.3 | |
| Position regarding religion | Without religion, non-believer | 177 | 31.5 |
| Bearer of a religious cultural heritage, but non-believer | 185 | 32.9 | |
| Believer, non-practitioner | 146 | 26 | |
| Believer, practitioner | 54 | 9.6 | |
| Total | 562 | 100 | |
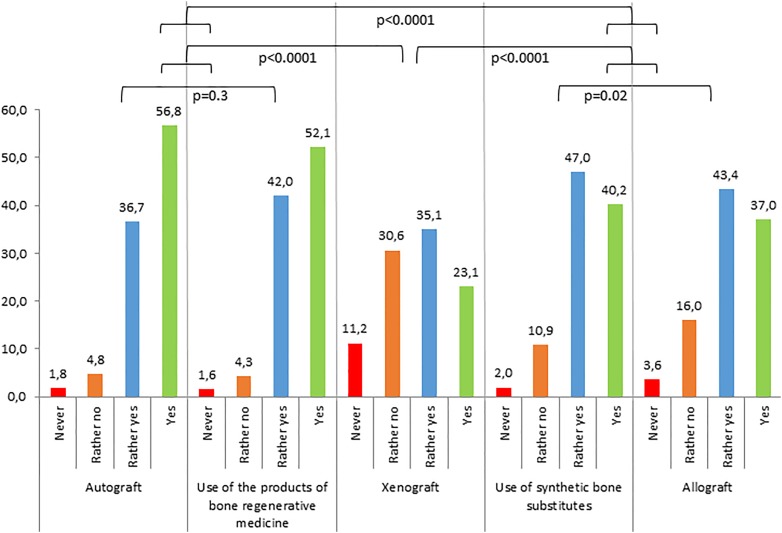
General results showed that the best theoretical acceptance rates were for autologous bone grafts (93.4%) and uses of the products of bone regenerative medicine (94.1%), with similar profiles of answers (no significant difference). All other techniques were significantly less accepted (p<0.001 for all techniques vs. autografts or products of regenerative medicine), the worst theoretical acceptance rates being for xenografts (58.2%). Overall results are showed in Fig. 2.
Figure 2.
Proportion of theoretical acceptance or non-acceptance of the techniques. General results (in %, n=562 for each technique).
The results showed very similar answers among male and female participants for all techniques, with no significant difference between the two groups (Table 2).
Table 2.
Proportion of Theoretical Acceptance or Non-Acceptance of the Techniques by Groups (in %). Significant Results in Bold.
| Characteristics | Groups Techniques | Autograft | Allograft | Xenograft | Use of synthetic bone substitutes | Use of products of regenerative medicine | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| never | rather no | rather yes | yes | never | rather no | rather yes | yes | never | rather no | rather yes | yes | never | rather no | rather yes | yes | never | rather no | rather yes | yes | ||
| General results | 1.8 | 4.8 | 36.7 | 56.8 | 3.6 | 16 | 43.4 | 37 | 11.2 | 30.6 | 35.1 | 23.1 | 2 | 10.9 | 47 | 40.2 | 1.6 | 4.3 | 42 | 52.1 | |
| Sex | Female | 2.1 | 5 | 37.5 | 55.5 | 4.4 | 16.8 | 43.4 | 35.4 | 12.7 | 32.4 | 33 | 21.8 | 2.4 | 12.1 | 47.2 | 38.3 | 1.5 | 3.8 | 45.1 | 49.6 |
| Male | 1.3 | 4.5 | 39.9 | 58.7 | 2.2 | 14.8 | 43.5 | 39.5 | 9 | 27.8 | 38.1 | 25.1 | 1.3 | 9 | 46.6 | 43 | 1.8 | 4.9 | 37.2 | 56.1 | |
| Age | 18–25 | 2.7 | 5.3 | 33.2 | 58.8 | 3.1 | 13.3 | 40.7 | 42.9 | 9.7 | 32.3 | 31.4 | 26.5 | 2.2 | 9.7 | 42.5 | 45.6 | 1.3 | 2.7 | 40.3 | 55.8 |
| 26–35 | 1.8 | 5.3 | 39.4 | 53.5 | 2.9 | 17.6 | 48.8 | 30.6 | 10 | 25.9 | 41.2 | 22.9 | 2.4 | 11.2 | 45.9 | 40.6 | 2.9 | 5.9 | 43.5 | 47.6 | |
| 36–45 | 0 | 1.5 | 45.5 | 53 | 4.5 | 12.1 | 50 | 33.3 | 15.2 | 36.4 | 31.8 | 16.7 | 1.5 | 13.6 | 54.5 | 30.3 | 0 | 7.6 | 45.5 | 47 | |
| 46–60 | 0 | 7.3 | 43.6 | 49.1 | 5.5 | 25.5 | 38.2 | 32.7 | 7.3 | 30.9 | 40 | 21.8 | 1.8 | 3.6 | 67.3 | 27.3 | 0 | 1.8 | 45.5 | 52.7 | |
| More than 60 | 2.2 | 2.2 | 22.2 | 73.3 | 2.2 | 44.4 | 17.8 | 37.8 | 22.2 | 31.1 | 28.9 | 17.8 | 0 | 20 | 37.8 | 42.2 | 2.2 | 4.4 | 35.6 | 57.8 | |
| Education level | Before high school degree | 2 | 4.1 | 24.5 | 69.4 | 4.1 | 14.3 | 49 | 32.7 | 14.3 | 42.9 | 28.6 | 14.3 | 0 | 16.3 | 49 | 34.7 | 0 | 4.1 | 38.8 | 57.1 |
| High school degree (HSD) | 1.9 | 4.9 | 43.7 | 49.5 | 4.9 | 18.4 | 41.7 | 35 | 16.5 | 31.1 | 34 | 18.4 | 3.9 | 18.4 | 49.5 | 28.2 | 3.9 | 1.9 | 43.7 | 50.5 | |
| 3 years after HSD | 0 | 4.8 | 38.1 | 57.1 | 3.2 | 8.7 | 45.2 | 42.9 | 11.9 | 35.7 | 31 | 21.4 | 0 | 10.3 | 53.2 | 36.5 | 0.8 | 6.3 | 50 | 42.9 | |
| 5 years after HSD | 1.9 | 2.8 | 36.1 | 59.3 | 2.8 | 20.4 | 40.7 | 36.1 | 11.1 | 34.3 | 28.7 | 25.9 | 0 | 8.3 | 46.3 | 45.4 | 0 | 6.5 | 42.6 | 50.9 | |
| More than 5 years after HSD | 2.8 | 6.3 | 35.2 | 55.7 | 3.4 | 17.6 | 43.2 | 35.8 | 6.8 | 21 | 44.3 | 27.8 | 4 | 6.8 | 40.9 | 48.3 | 2.3 | 2.8 | 35.8 | 59.1 | |
| Position regarding religion | Without religion, non-believer | 1.7 | 5.1 | 35.6 | 57.6 | 2.3 | 14.7 | 48 | 35 | 8.5 | 24.3 | 39.5 | 27.7 | 0.6 | 6.8 | 48 | 44.6 | 1.1 | 4 | 41.8 | 53.1 |
| Bearer of a religious cultural heritage, but non-believer | 1.7 | 4.3 | 35.7 | 57.8 | 4.3 | 13 | 43.8 | 38.9 | 10.8 | 28.1 | 36.2 | 24.9 | 2.2 | 11.4 | 44.9 | 41.6 | 2.7 | 3.2 | 40 | 54.1 | |
| Believer, non-practitioner | 0.6 | 6.2 | 43.2 | 50 | 3.4 | 21.9 | 40.4 | 34.2 | 14.4 | 39 | 32.9 | 13.7 | 4.1 | 15.1 | 52.7 | 28.1 | 1.4 | 5.5 | 47.3 | 45.9 | |
| Believer, practitioner | 1.1 | 1.9 | 25.9 | 68.5 | 5.6 | 14.8 | 35.2 | 44.4 | 13 | 37 | 22.2 | 27.8 | 0 | 11.1 | 35.2 | 53.7 | 0 | 5.6 | 35.2 | 59.3 | |
| Chi2 tests between techniques: vs. Allograft | p<0.0001 | ||||||||||||||||||||
| vs. Xenograft | p<0.0001 | p<0.0001 | |||||||||||||||||||
| vs. Synthetic bone substitutes | p<0.0001 | p=0.02 | p<0.0001 | ||||||||||||||||||
| vs. Products of regenerative medicine | p=0.3 | p<0.0001 | p<0.0001 | p<0.0001 | |||||||||||||||||
Age did not show a significant impact on the good theoretical acceptance of autograft or use of the products of bone regenerative medicine, nor on the less good acceptance of allograft, synthetic bone substitute, or even xenograft (Table 2).
Education level did not seem to have an impact on the answers of the participants, except for the use of synthetic bone substitutes and for xenograft, although the theoretical acceptance rate for this technique still was the worst. A higher education level led to more acceptance for the use of synthetic bone substitutes (83.7% for the “before high school” group, 77.7% for the “high school degree” group, 89.7% for the “bachelor” group, 91.7% for the “master” group, and finally 89.2% for the “more than 5 years after high school degree” group, p<0.05) and for xenograft, (42.9% for the “before high school” group, 52.4% for the “high school degree” group and the “bachelor” group, 54.6% for the “master” group, and finally 72.1% for the “more than 5 years after high school degree” group, p<0.0005) (Table 2).
When focusing on position regarding religion, the answers seemed to follow the same scheme. Indeed, there was no remarkable difference between the different groups concerning the different techniques, except for the use of synthetic bone substitutes and for xenograft, whose acceptance was still the worst. Believers seemed to be more reluctant regarding xenograft than non-believers (67.2% of acceptance for the “without religion, non-believer” group, 61.1% for the “bearer of a religious cultural heritage, but non-believer” group, 46.6% for the “believer, non-practitioner” group, and finally 50% for the “believer, practitioner” group, p<0.005) (Table 2), although religious reasons were rarely invoked as refusal reasons (1.2% of all participants, corresponding to 2.6% of refusals) (Table 3).
Table 3.
Proportion of Refusal for Each Reason Regarding Each Technique (in % of All Respondents, n=562).
| Reasons Techniques |
Fear of the technique | Ethical reasons | Religious reasons | Other |
|---|---|---|---|---|
| Autograft | 8.0 | 0.2 | 0 | 0.9 |
| Allograft | 14.9 | 6.4 | 0 | 1.6 |
| Xenograft | 25.3 | 18.3 | 1.2 | 2.3 |
| Use of synthetic bone substitutes | 14.6 | 0.7 | 0 | 1.2 |
| Use of products of regenerative medicine | 6.8 | 1.1 | 0 | 0.9 |
Refusal Reasons
Overwhelmingly, refusals were due to some kind of fear of the technique, such as failure, side effects, pain, infection / transmission, or fear of the operation (8.0% of respondents for autograft, 14.9% for allograft, 25.3% for xenograft, 14.6% for the use of synthetic bone substitutes, and 6.8% for the use of the products of bone regenerative medicine, p<0.0001 for fear versus any other refusal reason, whatever the technique) (Table 3). Ethical reasons were mostly mentioned for allograft and xenograft procedures (6.4% and 18.3%, respectively) and very rarely for the use of synthetic bone substitutes or products of regenerative medicine (0.7% and 1.1%, respectively). Religious reasons were only mentioned regarding xenograft, and for a small proportion of patients (1.2%) (Table 3).
Among participants who wanted to develop their answer, 13 told their personal medical story, 15 clarified their fears (pain, infection, graft rejection, etc.), four mentioned animal wellbeing and the impossibility for animals to give their consent, three expressed their concern about the danger of using stem cells, one pointed out that these techniques are not natural enough, and one wondered how a human being could give his/her own biological tissue, highlighting the risk that these tissues could be commercialized.
Discussion
The design of the survey can be critiqued insofar as complications, comorbidity, and success rates were not given to participants. Indeed, we tried to keep a simple structure without information overload, to keep the questionnaire understandable for all participants. Moreover, we aimed at focusing on the treatments’ principles and their potential intrinsic barriers. These two specific points are the reason for dealing with “theoretical acceptance,” or “agreement in principle.” When exposed to the same choice in a real situation of demand of care, answers could be slightly different due to the psychological burden of being in need of treatment, and also through benefiting from more detailed information about each technique from a medical team.
Strength of faith could have been assessed using specific questionnaires such as the Santa Clara Strength of Religious Faith Questionnaire40,41 or the Revised Religious Fundamentalism Scale42. However, this approach would have been too long for participants and not well adapted to this survey, as these questionnaires are very focused on religion, while religion was not the main field of this study, and is a very sensitive subject in French population. Indeed, designing a questionnaire asking about the nature of people’s religion is rarely legally authorized, as it is considered as sensitive data by French government and ethics committees.
In our study, young people (18 to 35) and people with a high education level are overrepresented compared with other groups. This may be due to two reasons: (1) the mode of diffusion of the questionnaire, through shared social network posts (favoring young people) and professional mailing (favoring people with a high educational level), and (2) interest in the subject (favoring people with a high education level) even though the questionnaire was designed to be accessible to anyone. However, the analysis by groups (age, education) shows that differences in the answers are minimal. Facing a population that no longer responds to postal mail, added to the impossibility of conducting this survey by telephone (needing time to reflect, helping with comprehension using visual aids) and in order to directly reach a population interested in the subject, we chose to use shared social network posts. Consequently, and in an assumed manner, our population sample is not randomized because it is not randomizable. Nevertheless, our sample is consistent with the population of French internet users (age, education level)43.
No European, Oceanian, African, or North American studies focusing on patients’ acceptance are available to date. Still, our results are congruous with the results of the few studies on this subject in Chile and Turkey, regarding acceptance of autograft, allograft, and use of synthetic bone substitutes, but with a larger number of participants. Indeed, in the studies of Fernández et al.11 (100 concerned Chilean participants, as they were attending care offering bone graft and/or bone substitutes procedures) and Güngörmüş et al.16 (203 concerned Turkish participants, attending the same type of care), autograft was, respectively, accepted by more than 75% and 88.7% of participants, use of alloplastic material by more than 80% and 65%, and allograft by 40% with 21% more who would accept it but only at last resort and 53.2% in the second study (Table 4). When focusing on xenograft, there are large differences among studies. While we found a global acceptance of 58.2%, this rate was 55% in the Fernández et al. study11, 60.1% for bovine-derived xenografts in the Güngörmüş et al. study16, and only 7.4% for porcine-derived xenografts in the same study16 (Table 4). The low acceptance rate for porcine-derived xenografts was largely attributed to religious reasons (84.6% of refusals) and rarely to a fear of any infection (3.7%)16. Having noted these differences in relation to religion, we examined the distribution of religions in these different countries. The major difference in these studies is their location: the Fernández et al. study was led in Chile, whereas the Güngörmüş et al. one was in Turkey. Chile has a very important Christian population with 88% Catholics and 11% Protestants44, while Turkey is composed of 99% Muslims, with small Christian (Greek Orthodox and Catholic) and Jewish minorities45. France is composed of 68% Christians, 25% of the population with no religion, 6% Muslims, and 1% Jews46, leading to cultural differences between these countries. Christianity is more permissive about use of animal or human products than other religions such as Islam or Hinduism for example47, and our results regarding xenograft acceptance are close to the results of the study led in Chile. French laws do not allow the design of surveys which ask about the type of the religion of people. As a result, it is difficult to really discuss how the type of religion practiced influences responses. However, data that were gathered in the literature could allow speculation that acceptance of some techniques could be linked to cultural and religious parameters (almost 70% of our sample is at least “bearer of a religious cultural heritage”), and that no study could be transposed from one country to another unless they present the same pattern of population. For example, the USA—where no such studies are available—has 76% Christians, 15% of the population with no religion, 1.2% Jews, and 0.6% Muslims18, and is thus close to France in this specific aspect, and has a quite similar Human Development Index (HDI) (0.924 for the USA, 0.897 for France48), and so could show results that would be similar to those presented in our study. HDI is an index between 0 and 1, calculated by taking into account specific dimensions of human development such as a having a long and healthy life, being knowledgeable, and having a decent standard of living.
Table 4.
Acceptance of Techniques in Different Studies (in % of Respondents of Each Study).
| Country of the study | France [present study] | Chile11 | Turkey16 |
|---|---|---|---|
| Number of respondents | 562 | 100 | 203 |
| Autograft | 93.4 | 75 | 88.7 |
| Allograft | 80.4 | 40 (+21 only in last resort) |
53.2 |
| Xenograft | 58.2 | 55 | 60.1 (bovine- derived products) 7.4 (porcine- derived products) |
| Use of synthetic bone substitutes | 87.2 | 80 | 65 |
| Use of products of regenerative medicine | 94.1 | - | - |
The next step of such an investigation would be a qualitative survey. Indeed, refusals for ethical reasons are mentioned (1.1% for the use of products of bone regenerative medicine, 6.4% for allograft, and 18.3% for xenograft), and it would be interesting to explore these specific reasons. Some are given in the free comments of our study, such as questions inherent to the use of stem cells. Some have already been raised in the literature, such as the question about the moral status that is given to the nonhuman from whom the organs are taken22. Furthermore, and even if it is rarely mentioned in the free comments, it is easy to imagine that an increase in vegan lifestyles and the proportion of people concerned about animal wellbeing could play a role in the non-acceptance of xenograft as a refusal for ethical reasons. This point appeared in a previous study by Fernández et al.11, in which 12% of participants refused xenograft because “it is wrong to use animals for human benefit,” and in the study by Güngörmüş et al.16, in which refusal of a bovine-derived xenograft because it is “animal-derived” (not for religious reasons) comprised three-quarters of refusals overall. According to Jenkins et al.18, vegan people would predominantly prefer allogeneic products over xenogeneic products even if they are less effective and even if their costs are higher.
However, even if some patients do belong to a certain religion or cultural group, they may not necessarily share the same beliefs or values as the leaders or other members of that group18. Physicians have to navigate in respecting patients’ autonomy by remaining flexible and open-minded. They have to seek the patients’ best interest in its multiple forms, providing detailed information about the pros and cons of every possible therapeutic decision available in their situation, telling patients what they think is the best option, listening to patients regarding what they want to do, and dealing with the science that tells patients what they can do49. That is always a moral exercise, because all patients should be treated on an individual basis, especially in matters involving consent18.
Finally, if the use of the products of bone regenerative medicine is a technique awaited by surgeons to overcome the biological, comorbidity, and quality problems that can still be found in other techniques, our study is the first to show that it could also limit ethical issues, despite the development of living scaffolds (embedded with cells) in laboratories38, which could have made people more wary. Indeed, if it seems possible to deal with fears regarding the technique by giving detailed explanations and reassuring the patient, it is nevertheless rather unlikely to change his/her ethical and religious opinions in a short period. This point places bone regenerative medicine within the biological as well as the humanist quality standards that are expected to improve the health of patients.
Conclusions
For a patient suffering from a bone defect several techniques exist, each having advantages and disadvantages: autograft, allograft, xenograft, use of synthetic bone substitutes, and use of the products of bone regenerative medicine. While many studies focused on their efficacy, few have focused on their acceptance by patients, since ethical, religious, and fear issues could be involved. In France, almost no theoretical refusals are due to religious issues, and few are due to ethical reasons, mainly concerning allografts and xenografts. Acceptance of techniques does not seem to be greatly linked to population characteristics in France. Bone regenerative medicine is a promising way of treating patients, and this study shows that it could overcome some acceptance issues. However, and although autograft and use of the products of bone regenerative medicine are widely well accepted, some patients still feel some fear regarding these techniques. In fact, fear represents the main issue for patients who would theoretically refuse some of the techniques. Therefore, and even more so at a time in which patients’ autonomy has to be respected and included in the therapeutic approach, physicians should defuse these issues by explaining, reassuring, and informing patients. That is precisely the deepest essence of consent.
Footnotes
Author Contribution: Dr Damien Offner and Dr Gabriel Fernandez de Grado contributed equally to this work.
Ethical Approval: The study was approved by the Ethical Committee of the University Hospitals of Strasbourg, France, and received the authorization n° 2018-66.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Internet informed consent was obtained from the participants at the end of the e-questionnaire for their anonymized information to be published in this article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Damien Offner  https://orcid.org/0000-0003-0982-7031
https://orcid.org/0000-0003-0982-7031
References
- 1. Fernandez de Grado G, Keller L, Idoux-Gillet Y, Wagner Q, Musset AM, Benkirane-Jessel N, Bornert F, Offner D. Bone substitutes: a review of their characteristics, clinical use, and perspectives for large bone defects management. J Tissue Eng. 2018;9:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Campana V, Milano G, Pagano E, Barba M, Cicione C, Salonna G, Lattanzi W, Logroscino G. Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci Mater Med. 2014;25(10):2445–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Faour O, Dimitriou R, Cousins CA, Giannoudis PV. The use of bone graft substitutes in large cancellous voids: any specific needs? Injury. 2011;42(Suppl 2):S87–S90. [DOI] [PubMed] [Google Scholar]
- 4. Offner D, Wagner Q, Keller L, Idoux-Gillet Y, Benkirane-Jessel N, Musset AM. Complications d’une autogreffe osseuse, et comparaison avec une allogreffe osseuse ou l’utilisation de BMPs (Bone Morphogenetic Proteins): une revue systématique de la littérature. Le Journal de l’Orthopédie. 2017;18(65):3032–3043. [Google Scholar]
- 5. Athanasiou VT, Papachristou DJ, Panagopoulos A, Saridis A, Scopa CD, Megas P. Histological comparison of autograft, allograft-DBM, xenograft, and synthetic grafts in a trabecular bone defect: an experimental study in rabbits. Med Sci Monit. 2010;16(1):BR24–BR31. [PubMed] [Google Scholar]
- 6. Tilkeridis K, Touzopoulos P, Ververidis A, Christodoulou S, Kazakos K, Drosos GI. Use of demineralized bone matrix in spinal fusion. World J Orthop. 2014;5(1):30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Flierl MA, Smith WR, Mauffrey C, Irgit K, Williams AE, Ross E, Peacher G, Hak DJ, Stahel PF. Outcomes and complication rates of different bone grafting modalities in long bone fracture nonunions: a retrospective cohort study in 182 patients. J Orthop Surg Res. 2013;8:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011;42(Suppl 2):S3–S15. [DOI] [PubMed] [Google Scholar]
- 9. Oryan A, Alidadi S, Moshiri A, Maffulli N. Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res. 2014;9(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brydone AS, Meek D, Maclaine S. Bone grafting, orthopaedic biomaterials, and the clinical need for bone engineering. Proc Inst Mech Eng H. 2010;224(12):1329–1343. [DOI] [PubMed] [Google Scholar]
- 11. Fernández RF, Bucci C, Navarro P, Beltrán V, Borie E. Bone grafts utilized in dentistry: an analysis of patients’ preferences. BMC Med Ethics. 2015;16(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McCarthy CR. Ethical aspects of animal-to-human xenografts. ILAR J. 1995;37(1):3–9. [DOI] [PubMed] [Google Scholar]
- 13. Annas GJ. Baby fae: the “anything goes” school of human experimentation. Hastings Cent Rep. 1985;15(1):15–17. [PubMed] [Google Scholar]
- 14. Easterbrook C, Maddern G. Porcine and bovine surgical products. Jewish, Muslim, and Hindu perspectives. Arch Surg. 2008;143(4):366–370. [DOI] [PubMed] [Google Scholar]
- 15. De Vries R, Oerlemans A, Trommelmans L, Dierickx K, Gordijn B. Ethical aspects of tissue engineering: a review. Tissue Eng Part B Rev. 2008;14(4):367–375. [DOI] [PubMed] [Google Scholar]
- 16. Güngörmüş Z, Güngörmüş M. Effect of religious belief on selecting of graft materials used in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2017;75(1):2347–2353. [DOI] [PubMed] [Google Scholar]
- 17. Goyal D, Goyal A, Brittberg M. Consideration of religious sentiments while selecting a biological product for knee arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1577–1586. [DOI] [PubMed] [Google Scholar]
- 18. Jenkins ED, Yip M, Melman L, Frisella MM, Matthews BD. Informed consent: cultural and religious issues associated with the use of allogeneic and xenogeneic mesh products. J Am Coll Surg. 2010;210(4):402–410. [DOI] [PubMed] [Google Scholar]
- 19. Sattar SP, Shakeel AM, Majeed F, Petty F. Inert medication ingredients causing nonadherence due to religious beliefs. Ann Pharmacother. 2004;38(4):621–624. [DOI] [PubMed] [Google Scholar]
- 20. Zhong R, Platt JL. Current status of animal-to-human transplantation. Expert Opin Biol Ther. 2005;5(11):1415–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Norman-Taylor FH, Santori N, Villar RN. The trouble with bone allograft. BMJ. 1997;315(7107):498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nelson JL. Moral sensibilities and moral standing: caplan on xenograft “donors”. Bioethics. 1993;7(4):315–322. [DOI] [PubMed] [Google Scholar]
- 23. Zimmermann G, Moghaddam A. Allograft bone matrix versus synthetic bone graft substitutes. Injury. 2011;42(suppl 2):S16–S21. [DOI] [PubMed] [Google Scholar]
- 24. Mroz TE, Joyce MJ, Steinmetz MP, Lieberman IH, Wang JC. Musculoskeletal allograft risks and recalls in the United States. J Am Acad Orthop Surg. 2008;16(10):559–565. [DOI] [PubMed] [Google Scholar]
- 25. Robertson A, Nutton RW, Keating JF. Current trends in the use of tendon allografts in orthopaedic surgery. J Bone Joint Surg Br. 2006;88(8):988–992. [DOI] [PubMed] [Google Scholar]
- 26. Laurencin CT, El-Amin SF. Xenotransplantation in orthopaedic surgery. J Am Acad Orthop Surg. 2008;16(1):4–8. [DOI] [PubMed] [Google Scholar]
- 27. Oryan A, Alidadi S, Moshiri A. Current concerns regarding healing of bone defects. Hard Tissue. 2013;2(2):13. [Google Scholar]
- 28. Paradis K, Langford G, Long Z, Heneine W, Sandstrom P, Switzer WM, Chapman LE, Lockey C, Inions D, Otto E. Search for cross-species transmission of porcine endogenous retrovirus in patients treated with living pig tissue. Science. 1999;285(5431):1236–1241. [DOI] [PubMed] [Google Scholar]
- 29. Greenwald AS, Boden SD, Goldberg VM, Khan Y, Laurencin CT, Rosier RN. Bone-graft substitutes: facts, fictions and applications. J Bone Joint Surg Am. 2001;83(A-Suppl 2 Pt 2):98–103. [DOI] [PubMed] [Google Scholar]
- 30. Gupta A, Kukkar N, Sharif K, Main BJ, Albers CE, El-Amin III SF. Bone graft substitutes for spine fusion: a brief review. World J Orthop. 2015;6(6):449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rickert D, Huddleston Slater JJR, Meijer HJA, Vissink A, Raghoebar GM. Maxillary sinus lift with solely autogenous bone compared to a combination of autogenous bone and growth factors or (solely) bone substitutes. A systematic review. Int J Oral Maxillofac Surg. 2012;41(2):160–167. [DOI] [PubMed] [Google Scholar]
- 32. Garfin SR, Yuan HA, Reily MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26(14):1511–1515. [DOI] [PubMed] [Google Scholar]
- 33. Russell TA, Leighton RK; on behalf of the Alpha-BSM Tibial Plateau Fracture Study Group. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am. 2008;90(10):2057–2061. [DOI] [PubMed] [Google Scholar]
- 34. Offner D, Wagner Q, Idoux-Gillet Y, Ferrandon A, Schwinte P, Musset AM, Benkirane-Jessel N, Keller L. Hybrid collagen sponges and stem cells as a new combined scaffold able to induce the re-organization of endothelial cells into clustered networks. Biomed Mater Eng. 2017;28(Suppl 1):S185–S192. [DOI] [PubMed] [Google Scholar]
- 35. Wagner Q, Idoux-Gillet Y, Offner D, Saleem I, Satyanarayana Somavarapu S, Schwinté P, Benkirane-Jessel N, Keller L. Advanced nanostructured medical device combining mesenchymal cells and VEGF nanoparticles for enhanced engineered tissue vascularization. Nanomedicine (Lond). 2016;11(18):2419–2430. [DOI] [PubMed] [Google Scholar]
- 36. Guerrero J, Catros S, Derkaoui SM, Lalande C, Siadous R, Bareille R, Thébaud N, Bordenave L, Chassande O, Le Visage C, Letourneur D, et al. Cell interactions between human progenitor-derived endothelial cells and human mesenchymal stem cells in a three-dimensional macroporous polysaccharide-based scaffold promote osteogenesis. Acta Biomater. 2013;9(9):8200–8213. [DOI] [PubMed] [Google Scholar]
- 37. Hench LL, Polak JM. Third-generation biomedical materials. Science. 2002;295(5557):1014–1017. [DOI] [PubMed] [Google Scholar]
- 38. Offner D, Keller L, Wagner Q, Benkirane-Jessel N, Musset AM. Réflexions éthiques autour de la recherche en ingénierie tissulaire osseuse. Ethique et Santé. 2018;15(4):257–263. [Google Scholar]
- 39. Loi n° 2002-303 du 4 mars 2002 relative aux droits des malades et à la qualité du système de santé. 2002. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000000227015&categorieLien=id (accessed October 30th 2018). [PubMed]
- 40. Cummings JP, Carson CS, Shrestha S, Kunik ME, Armento ME, Stanley MA, Amspoker AB. Santa Clara strength of religious faith questionnaire: psychometric analysis in older adults. Aging Ment Health. 2015;19(1):86–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Plante TG, Boccaccini MT. The Santa Clara strength of religious faith questionnaire. Pastoral Psychol. 1997;45(5):375–387. [Google Scholar]
- 42. Altemeyer B, Hunsberger B. A revised religious fundamentalism scale: the short and sweet of it. Int J Psychol Relig. 2004;14(1):47–54. [Google Scholar]
- 43. Bigot R, Croutte P, Daudey E; for the CREDOC (Research Centre for the Study and Observation of Living Conditions). La diffusion des technologies de l’information et de la communication dans la société française (2013). www.credoc.fr/download/pdf/Rapp/R297.pdf (accessed November 16th 2018).
- 44. Ministère français de l’Europe et des Affaires Etrangères. Présentation du Chili. 2018. https://www.diplomatie.gouv.fr/fr/dossiers-pays/chili/presentation-du-chili/article/presentation-du-chili (accessed October 30th 2018).
- 45. Ministère français de l’Europe et des Affaires Etrangères. Présentation de la Turquie. 2018. https://www.diplomatie.gouv.fr/fr/dossiers-pays/turquie/presentation-de-la-turquie/ (accessed October 30th 2018).
- 46. Machelon JP. (sous la direction de), pour le Ministère français de l’Intérieur et de l’aménagement du territoire Rapport de la Commission de réflexion juridique sur les relations des cultes avec les pouvoirs publics, 2006. http://www.ladocumentationfrancaise.fr/var/storage/rapports-publics/064000727.pdf (accessed October 30th 2018)
- 47. Eriksson A, Burcharth J, Rosenberg J. Animal derived products may conflict with religious patients’ beliefs. BMC Med Ethics. 2013;14:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Palmarès – indicateur de développement humain (IDH). 2017. https://www.populationdata.net/palmares/idh/ (accessed October 30th 2018)
- 49. Curkin FA, Roach CJ, Bhat-Gorawara R, Lantos JD, Chin MH. When patients choose faith over medicine. Physician perspectives on religiously related conflict in the medical encounter. Arch Intern Med. 2005;165(1):88–91. [DOI] [PubMed] [Google Scholar]