Abstract
Amputation following burn injury is rare. Previous studies describe the risk of amputation after electrical burn injuries. Therefore, we describe the distribution of amputations and evaluate risk factors for amputation following burn injury at a large regional burn center. We conducted a retrospective analysis of patients ≥17 years admitted from January 2002 to December 2015. Patients who did and did not undergo an amputation procedure were compared. A multivariate logistic regression model was used to determine the risk factors for amputation. Amputations were further categorized by extremity location and type (major, minor) for comparison. Of the 8313 patients included for analysis, 1.4% had at least one amputation (n = 119). Amputees were older (46.7 ± 17.4 years) than nonamputees (42.6 ± 16.8 years; P = .009). The majority of amputees were white (47.9%) followed by black (39.5%) when compared with nonamputees (white: 57.1%, black: 27.3%; P = .012). The most common burn etiology for amputees was flame (41.2%) followed by electrical (23.5%) and other (21.9%). Black race (odds ratio [OR]: 2.29; 95% confidence interval [CI]: 1.22–4.30; P = .010), electric (OR: 13.54; 95% CI: 6.23–29.45; P < .001) and increased %TBSA (OR: 1.03; 95% CI: 1.02–1.05; P < .001) were associated with amputation. Burn etiology, the presence of preexisting comorbidities, black race, and increased %TBSA increase the odds of post burn injury. The role of race on the risk of amputation requires further study.
Amputation is the removal of the whole or part of a limb or digit by cutting through bone or joint. An ancient surgical procedure, amputation retains its relevance in modern time to save life or remove a dead or useless limb. Trauma-related amputations are a common cause of limb loss in the United States.1 Amputation following burn injury is rare, with a reported incidence of approximately 2%, irrespective of burn etiology.2
There is paucity of data regarding amputation after burn injury. Most studies only analyze amputation following electrical injury.3–5 Electrical burns are significantly associated with an increased risk of amputation with incidence reported as high as 68%.2,6,7 Previous studies have reported that extensive thermal burns are also associated with an increased risk of amputation.8,9 Most of these studies were limited by their small sample size.
Amputation in patients with severe injury to an extremity has been shown to improve survival.8,10 Delays in amputation have been attributed to complications including infections, burn severity, and mechanism of injury. Furthermore, undergoing amputation results in additional rehabilitation needs and has long-term socioeconomic implications for patients and their families.11
While, infrequent, a better understanding of amputations following burn injury is important due to the impact on patients. To that aim, we will review the records of all burn patients admitted to a large regional burn center who underwent amputation. We will describe the distribution of amputations, determine if discharge destination is impacted by the presence of concomitant amputation, and evaluate factors associated with amputation following burn injury.
METHODS
A retrospective analysis of patients admitted to the University of North Carolina (UNC) Jaycee Burn Center surveillance registry from January 2002 to December 2015 was conducted. The UNC Jaycee Burn Center is an American Burn Association verified burn center for pediatric and adult care. The burn center is a 36-bed facility that averages over 1600 acute admissions annually.
All patients ≥17 years were included in this analysis. The medical records of subjects identified by query of the UNC Burn database were reviewed to confirm baseline demographic data and injury characteristics, including burn etiology, %TBSA burn, concomitant inhalation injury, and use of mechanical ventilation during admission. Inhalation injury diagnosis was based on history, physical examination, and/or bronchoscopic examination. International Classification of Diseases 9 (ICD-9) procedure codes (84.01, 84.05, 84.07, 84.11, 84.12, 84.15, 84.17) were used to determine type of amputation, which was recorded in the database. To examine the effect of baseline medical comorbidities on outcome, a modified Charlson Comorbidity Index (CCI)12 score was calculated for each patient. The standardized Charlson Index has been reported to accurately predict the probability of mortality within 1 year for a number of medical conditions. The score is the weighted sum of comorbid conditions. There are 17 comorbid conditions included in the score and each is assigned a weight from 1 to 6 points. The weighted sum of all comorbid conditions is the patient’s Charlson score. Data collected upon patient admission based on past medical history, medical records, and captured in the UNC Burn database were used to calculate the CCI score. Patients were excluded if clinical characteristics, including race, etiology of burn, or whether or not a concomitant inhalation injury, were present.
To evaluate the role of amputation status on discharge disposition, discharge destination was categorized into one of four mutually exclusive but ordered discharge categories: home, home with home health services (HH), skilled nursing facility (SNF), and inpatient rehabilitation (IR). These categories represent increasing levels of care at discharge and, to some degree, increasing potential intensity of rehabilitation services available to an individual.
For further analysis, amputations were categorized by location into upper extremity (UE) and lower extremity (LE) amputations. Amputations were also grouped into major and minor amputations. Amputations of the humerus and forearm, above-the-knee amputations, below-the-knee amputations, and foot amputations were considered major. An amputation was considered minor if it included only the fingers or toes. Additionally, characteristics of patients that underwent an amputation procedure were compared by etiology (electrical vs thermal) to assess the potential effect of burn mechanism. To further determine the effect of age on the risk of amputation, age was categorized into two groups: <65 and ≥65 years. Burn etiology was categorized into four groups: flame, scald, electrical, and other (including chemical, radiation, and additional burn types).
Baseline patient and injury characteristics were compared between groups (Amputation vs No Amputation) using Analysis of Variance for continuous variables and Pearson chi-squared test for discrete variables. To estimate the predictors of amputation, we used a multivariate logistic regression model. To determine the role of amputation on discharge destination, we first calculated the standardized mean differences (SMD) to compare covariate imbalance before and after adjustment was made using propensity score weighting.
A multiassignment propensity score, estimated via a multinomial logistic regression, was used to derive the conditional probability of assignment according to whether or not an amputation procedure was conducted given the observed prehospital variables. Inverse probability of treatment assignment weighting (IPTW) was then performed to achieve balance among the amputation and no amputation groups for selected prehospital variables. The prehospital variables included age, sex, insurance status, etiology, the presence of preexisting comorbidities, and %TBSA. The SMD was compared between the unweighted and IPTW groups to assess balance. Following IPTW and balance assessment, ordered logistic regression was used to estimate odds ratios (ORs) for discharge to a higher level of rehabilitation, with IR being the highest and home being the lowest level of rehabilitation. The regression was adjusted for in-hospital covariates (hospital length of stay [LOS], ICU [intensive care unit] LOS, mechanical ventilation) that were found to be associated with the outcome.
All analyses were performed using Stata version 15 (Statacorp, College Station, TX). The University of North Carolina Institutional Review Board approved this study.
RESULTS
There were 11,977 patients admitted from January 2002 to December 2015 with 8494 patients aged ≥17 years old. A total of 181 patients were excluded due to missing data on race (n = 58), burn etiology (n = 97), and presence of inhalation injury (n = 45). None of the patients with missing data had any amputations. The remaining 8313 patients were included for analysis. Of those, 119 (1.4%) patients underwent at least one amputation.
Table 1 shows the baseline patient characteristics of this population. The majority of patients were male, 72.5% (N = 6042), white, 57.0% (N = 4736), and <65 years, 88.7% (N = 7373). The mean age of the overall population was 42.7 ± 16.8 years. There was a male preponderance in both the amputation (83.2%) and nonamputation (72.3%) groups. Patients in the amputation group (46.7 ± 17.4 years) were significantly older than those in the nonamputation group (42.6 ± 16.8 years; P = .009). The majority of patients in both the amputation and nonamputation groups were white (47.9% vs 57.1%, respectively), followed by black (39.5% vs 27.3%, respectively; P = .012). Overall median CCI was 0. There was a greater proportion of patients who were insured in the amputation group (77.3%) when compared with those in the no amputation group (69.6%; P = .178). The most common burn etiology for amputees was flame (41.2%) followed by electrical (23.5%) and other (21.9%; P < .001). The median TBSA of patients in the amputation group was 6% (Interquartile Range [IQR] 1–8%) vs the median TBSA of 3% (IQR 1.8–23%) in the nonamputation group (P < .001). A concomitant inhalation injury was found in 17.7% of amputation patients compared with 7.5% of patients without an amputation (P < .001). Both hospital and ICU LOS were statistically significantly longer for patients who underwent amputations compared with patients without amputation. The majority of patients were discharged home, regardless of amputation status (Amputation 74.8% vs No Amputation 89.8%; P < .001). Mortality was higher for the amputation group (11.8%) than for the no amputation group (3.9%; P < .01).
Table 1. Patient demographics and clinical characteristics
| Characteristic | Overall (n = 8313) |
Amputation (n = 119) |
No amputation (n = 8194) |
P |
|---|---|---|---|---|
| Gender | .008 | |||
| M | 6042 (72.5) | 99 (83.2) | 5925 (72.3) | |
| F | 2289 (27.5) | 20 (16.8) | 2269 (27.7) | |
| Age (years), overall | 42.7 ± 16.8 | 46.7 ± 17.4 | 42.6 ± 16.8 | .009 |
| Age groups | .056 | |||
| <65 years | 7373 (88.7) | 99 (83.2) | 7274 (88.8) | |
| ≥65 years | 940 (11.3) | 20 (16.8) | 920 (11.2) | |
| Race | .012 | |||
| White | 4736 (57.0) | 57 (47.9) | 4679 (57.1) | |
| Black | 2286 (27.5) | 47 (39.5) | 2239 (27.3) | |
| Hispanic | 587 (7.0) | 10 (8.4) | 577 (7.0) | |
| Other | 704 (8.5) | 5 (4.2) | 699 (8.5) | |
| CCI, median (IQR) | 0 (0) | 0 (0–1) | 0 (0) | .030 |
| Have Insurance | 5793 (69.7) | 92 (77.3) | 5701 (69.6) | .178 |
| Unknown | 16 (0.2) | 0 (0) | 16 (0.2) | |
| Type of burn | <.001 | |||
| Flame | 4270 (51.4) | 49 (41.2) | 4221 (51.5) | |
| Scald | 2615 (31.5) | 16 (13.4) | 2599 (31.7) | |
| Electrical | 408 (4.9) | 28 (23.5) | 380 (4.6) | |
| Other | 1020 (12.2) | 26 (21.9) | 994 (12.1) | |
| TBSA, median (IQR) | 3 (1–8) | 6 (1.8–23) | 3 (1–8) | <.001 |
| Inhalation injury | 635 (7.6) | 21 (17.7) | 614 (7.5) | <.001 |
| Mechanical ventilation | 884 (10.6) | 43 (36.1) | 841 (10.3) | <.001 |
| Unknown | 250 (3.0) | 3 (2.5) | 247 (3.0) | |
| Hospital LOS, median (IQR) | 7 (2–13) | 36 (19–70) | 7 (2–13) | <.001 |
| ICU LOS, median (IQR) | 0 (0–1) | 5 (0–36) | 0 (0–1) | <.001 |
| Disposition | <.001 | |||
| Home | 7449 (89.6) | 89 (74.8) | 7360 (89.8) | |
| HH | 451(5.4) | 11 (9.2) | 440 (5.4) | |
| SNF | 76 (0.9) | 5 (4.2) | 71 (0.9) | |
| IR | 337 (4.1) | 14 (11.8) | 323 (3.9) | |
| Mortality | 337 (4.1) | 14 (11.8) | 323 (3.9) | <.001 |
CCI, Charlson Comorbidity Index; HH, home with home health care; ICU, intensive care unit; IQR, interquartile range; IR, inpatient rehab; LOS, length of stay; SNF, skilled nursing facility.
Distribution of Amputations
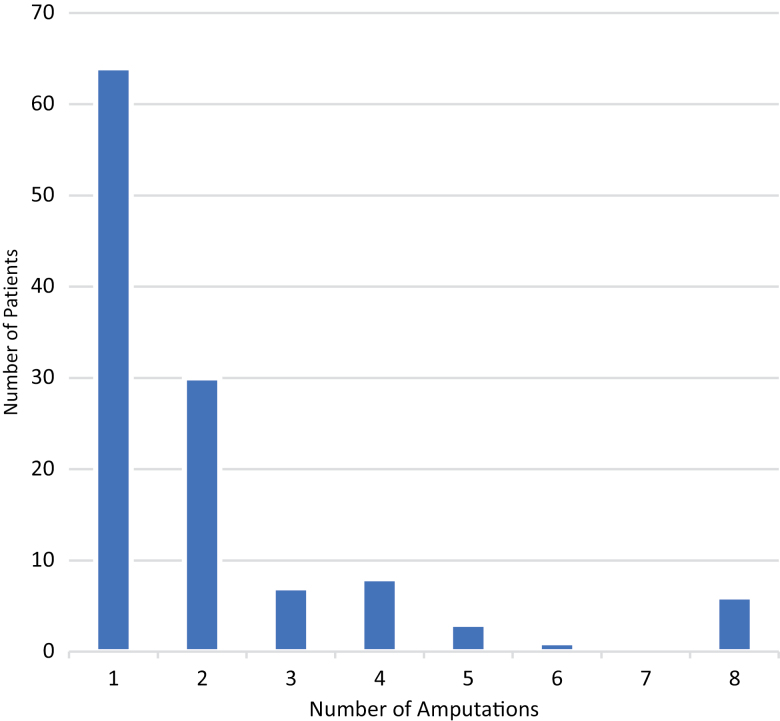
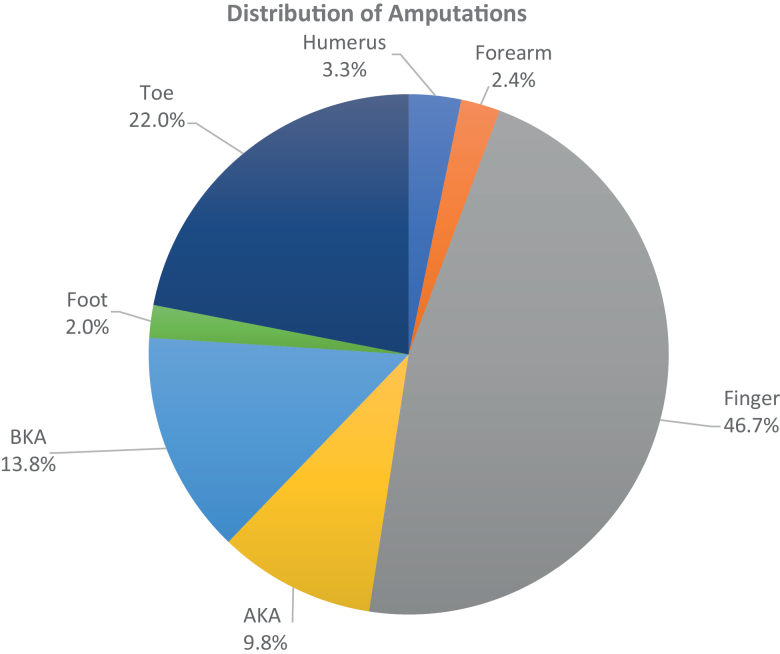
There was a total of 246 amputations for 119 patients. Figure 1 shows the number of patients who underwent amputations grouped by the number of amputation procedures. The majority of patients received only one amputation (n = 64), followed by two amputations (n = 30). Those patients who underwent four or more amputations often had multiple digits removed. The distribution of amputations according to location is seen in Figure 2. The majority of amputations were of fingers (46.7%) and toes (22.0%).
Figure 1.
Distribution of patients based on number of postburn amputation procedures.
Figure 2.
Distribution of amputation location. AKA, above-the-knee amputation; BKA, below-the-knee amputation.
Amputations were compared by extremity location (Table 2) and type (Table 3). Men were more likely to undergo an amputation for any given extremity location (UE: 68.2%, LE: 91.7%, both UE and LE: 100%) when compared with women (UE: 31.8%, LE: 8.3%, both UE and LE: 0%; P = .005). All amputation locations were similar in regard to age, race, CCI, etiology, %TBSA, and mortality. Patient characteristics were similar regardless of amputation type, except in regard to the presence of comorbidities and mortality. The median CCI of patients who underwent both major and minor amputations (CCI: 2, IQR: 0–5.5) was greater than the median CCI of those who only underwent a major (CCI: 0, IQR: 0–1) or minor amputation (CCI: 0, IQR: 0; P = .037). The mortality rate was found to be higher in patients who underwent a major amputation (21.6%) when compared with those who underwent a minor amputation (4.9%) and to those who underwent both major and minor amputations (0%; P = .015).
Table 2. Comparison of amputation patients by amputation location
| Characteristic | UE (n = 44) |
LE (n = 72) |
Both (n = 3) |
P |
|---|---|---|---|---|
| Gender | .005 | |||
| M | 30 (68.2) | 66 (91.7) | 3 (100.0) | |
| F | 14 (31.8) | 6 (8.3) | 0 (0) | |
| Age (years), Overall | 43.3 ± 17.9 | 48.9 ± 17.1 | 42.3 ± 6.7 | .211 |
| Race | .459 | |||
| White | 25 (56.8) | 30 (41.7) | 2 (66.7) | |
| Black | 13 (29.6) | 33 (45.8) | 1 (33.3) | |
| Hispanic | 3 (6.8) | 7 (9.7) | 0 (0) | |
| Other | 3 (6.8) | 2 (2.8) | 0 (0) | |
| CCI, median (IQR) | 0 (0) | 0 (0–1) | 0 (0) | .319 |
| Have Insurance | 33 (75.0) | 56 (77.8) | 3 (100.0) | .918 |
| Type of burn | .259 | |||
| Flame | 21 (47.7) | 28 (38.9) | 0 (0) | |
| Scald | 3 (6.8) | 13 (18.1) | 0 (0) | |
| Electrical | 10 (22.7) | 15 (20.8) | 2 (66.7) | |
| Other | 10 (22.7) | 16 (22.2) | 1 (33.3) | |
| TBSA, median (IQR) | 6 (1.5–26) | 5 (1.5–22) | 15.8 (2–29.5) | .537 |
| Discharge destination | .672 | |||
| Home | 35 (79.6) | 51 (70.8) | 3 (100.0) | |
| HH | 2 (4.6) | 9 (12.5) | 0 (0) | |
| SNF | 1 (2.3) | 4 (5.6) | 0 (0) | |
| IR | 6 (13.6) | 8 (11.1) | 0 (0) | |
| Mortality | 6 (13.6) | 8 (11.1) | 0 (0) | .844 |
CCI, Charlson Comorbidity Index; HH, home with home health care; IQR, interquartile range; IR, inpatient rehab; LE, lower extremity; SNF, skilled nursing facility; UE, upper extremity.
Table 3.
Comparison of amputation patients by amputation type
| Characteristic | Major (n = 51) |
Minor (n = 61) |
Both (n = 7) |
P |
|---|---|---|---|---|
| Gender | .692 | |||
| M | 44 (86.3) | 49 (80.3) | 6 (85.7) | |
| F | 7 (13.7) | 12 (19.7) | 1 (14.3) | |
| Age, Overall | 50.6 ± 18.7 | 44.0 ± 16.1 | 41.0 ± 13.2 | .090 |
| Race | .080 | |||
| White | 27 (52.9) | 28 (45.9) | 2 (28.6) | |
| Black | 22 (42.1) | 20 (32.8) | 5 (71.4) | |
| Hispanic | 1 (2.0) | 9 (14.8) | 0 (0) | |
| Other | 1 (2.0) | 4 (6.6) | 0 (0) | |
| CCI, median (IQR) | 0 (0–1) | 0 (0) | 2 (0–5.5) | .037 |
| Type of burn | .067 | |||
| Flame | 30 (58.8) | 17 (27.9) | 2 (28.6) | |
| Scald | 4 (7.8) | 11 (18.0) | 1 (14.3) | |
| Electrical | 9 (17.7) | 17 (27.9) | 2 (28.6) | |
| Other | 8 (15.7) | 16 (26.2) | 2 (28.6) | |
| TBSA, median (IQR) | 13.5 (3.5–34) | 2.5 (1–9.5) | 9.8 (1.5–13) | .063 |
| Mortality | 11 (21.6) | 3 (4.9) | 0 (0) | .015 |
CCI = Charlson Comorbidity Index; IQR, interquartile range.
Amputations were compared by etiology (electrical vs thermal) in Table 4. The majority of amputations were due to electrical burns (n = 65). Men were more likely to undergo an amputation due to a thermal burn than an electrical burn (96.4% vs 78.5%, respectively; P = .033). Patients who underwent an amputation due to an electrical burn (49.2 ± 17.2 years) were significantly older than patients who had a thermal burn (36.1 ± 13.2 years; P = .001). The majority of patients to experience an amputation due to either an electrical or thermal burn were white (46.2% vs 53.6%), followed by black (43.1% vs 28.6%; P = .033). Median TBSA was greater for electrical burns (12.5%, IQR: 3–34.5%) than for thermal burns (4%, IQR: 1–22%; P = .050).
Table 4.
Comparing patient characteristics for electrical and thermal burns in patients who underwent an amputation procedure
| Characteristic | Electrical (n = 65) |
Thermal (n = 28) |
P |
|---|---|---|---|
| Gender | .033 | ||
| M | 51 (78.5) | 27 (96.4) | |
| F | 14 (21.5) | 1 (3.6) | |
| Age (years), Overall | 49.2 ± 17.2 | 36.1 ± 13.2 | .001 |
| Race | .033 | ||
| White | 30 (46.2) | 15 (53.6) | |
| Black | 28 (43.1) | 8 (28.6) | |
| Hispanic | 2 (3.1) | 5 (17.9) | |
| Other | 5 (7.7) | 0 (0) | |
| CCI, median (IQR) | 0 (0–1) | 0 (0) | .036 |
| TBSA, median (IQR) | 12.5 (3–34.5) | 4 (1–22) | .050 |
CCI, Charlson Comorbidity Index; IQR, interquartile range.
A multivariate logistic regression model was then performed (Table 5). Black patients (OR: 2.29, 95% confidence interval [CI]: 1.22–4.30) were more than twice as likely to undergo an amputation when compared with white patients (P = .010). Odds of amputation was also increased for each additional point increase in CCI (OR: 1.29, 95% CI: 1.05–1.59; P = .015). Electrical (OR: 13.54, 95% CI: 6.23–29.45; P < .001) and other (OR: 4.24, 95% CI: 1.84–9.81; P = .001) burns were associated with increased odds of amputation. For each percentage increase in TBSA, there was a 3% increased odd of undergoing an amputation (OR: 1.03, 95% CI: 1.02–1.05; P < .001).
Table 5.
Multivariate logistic regression estimating risk of amputation
| Adjusted OR, 95% CI | P | |
|---|---|---|
| Gender (male reference) | 0.50 (0.21–1.23) | .133 |
| Age (years) | 0.99 (0.97–1.02) | .477 |
| Age Group (<65 reference) | 1.35 (0.39–4.64) | .633 |
| Race (white reference) | ||
| Black | 2.29 (1.22–4.30) | .010 |
| Hispanic | 1.56 (0.59–4.10) | .371 |
| Other | 0.28 (0.04–2.11) | .217 |
| CCI | 1.29 (1.05–1.59) | .015 |
| Etiology (flame reference) | ||
| Scald | 0.66 (0.21–2.04) | .733 |
| Electric | 13.54 (6.23–29.45) | <.001 |
| Other | 4.24 (1.84–9.81) | .001 |
| TBSA | 1.03 (1.02–1.05) | <.001 |
| Inhalation injury | 1.51 (0.67–3.41) | .317 |
CCI, Charlson Comorbidity Index; CI, confidence interval; OR, odds ratio.
IPTW was performed for age, gender, insurance status, race, CCI, TBSA, type of burn, presence of inhalation injury, and intubation status. The SMD was calculated and balance was achieved. An ordered logistic regression was performed on the IPTW-adjusted sample (Table 6). Although the presence of an amputation did increase a patient’s odds of being discharged to a higher level of rehabilitation, it was not significant (OR: 1.82, 95% CI: 0.46–7.15; P = .390).
Table 6.
Ordered logistic regression estimating odds of discharge to higher level of care
| Adjusted OR, 95% CI | P | |
|---|---|---|
| Amputation | 1.82 (0.46–7.15) | .390 |
| Gender (male reference) | 0.41 (0.16–1.10) | .076 |
| Age (years) | 1.05 (1.02–1.08) | .003 |
| Have insurance | 2.58 (1.51–4.41) | .001 |
| Race (white reference) | ||
| Black | 0.75 (0.32–1.75) | .500 |
| Hispanic | 0.20 (0.06–0.73) | .015 |
| Other | 1.25 (0.25–6.27) | .790 |
| CCI | 1.32 (0.99–1.76) | .061 |
| Etiology (flame reference) | ||
| Scald | 2.07 (0.67–6.37) | .204 |
| Electric | 7.03 (1.84–26.85) | .004 |
| Other | 2.44 (0.92–6.46) | .072 |
| TBSA | 1.09 (1.06–1.12) | <.001 |
| Inhalation injury | 1.20 (0.81–1.78) | .370 |
| Mechanical Ventilation | 2.40 (0.58–9.90) | .227 |
CCI, Charlson Comorbidity Index; CI, confidence interval; OR, odds ratio.
Discharge to home is lowest level of care, while discharge to inpatient rehab is highest level of care.
DISCUSSION
In this study, we show that the majority of amputations are related to electrical injury rather than thermal burns. Additionally, the presence of an amputation was not a significant determinant of a patient’s discharge destination. Furthermore, upon multivariate logistic regression, independent risk factors for amputations after controlling for pertinent covariates were electrical burns, burn size, the presence of comorbidities, and nonwhite race.
Our finding that electrical burns was associated with increased risk of amputation is in line with prior studies.2,3,8,13–15 Between 75.8% and 82.8% of burn-related amputations were attributable to electrical burns.3,16 Furthermore, Soto et al described that electrical burns increased the likelihood of amputation by 13.8 times.2 The majority of these patients are working males.13,17 This could be explained by the fact that more men had occupational exposure to electricity than women. According to the Bureau of Labor and Statistics, only 20.3% of employees in the utilities industry and 9.1% of employees in construction are women.18 Contact or chemical burn were found to increase the odds of amputation as compared with thermal burns by 3-fold.
Previous case series have demonstrated the potential difficulties in rehabilitating burn-injured patients who have undergone amputations.9,19,20 Kennedy et al, in a series of 27 burn-injured amputees, noted difficulties in rehabilitation following discharge relating to poor quality of skin coverage, reported skin breakdown, and secondary joint and wound contracture over the amputation stump.8 To our knowledge, there are no previous studies that examine the determinants of discharge destination in this cohort. Similar to our findings, other studies have demonstrated increased likelihood of discharge to a higher level of rehabilitative services for patients with increasing age,21–23 more severe burns, and for those who are insured.24 In conjunction with previous findings, we noted that minorities are less likely to be discharged to a higher level of care.
Comorbidities have been previously shown to play an important role in patient outcomes following burn injury.25,26 We demonstrated that for every point increase in CCI score, the odds of amputation increased 29%. Additionally, we noted that those patients who underwent both major and minor amputation procedures had a higher median CCI than those who underwent either one alone. No studies could be found that evaluated the role that the presence of preexisting comorbidities may play in amputation following burn injury. We know, however, that the presence of preexisting diabetes mellitus or indeed peripheral vascular occlusive diseases predispose to amputations in the absence of burn injury.27,28 Both of these medical conditions are accounted for in the CCI score and may explain the association we found. Active management of comorbidities may help attenuate amputation rates further in the burn population.
In our study, we also found black race to be associated with an increased risk of amputation. To our knowledge, this is the first paper describing a racial difference in amputation after burn injury. Previous studies have evaluated racial disparities in outcomes for burn-injured patients.29–31 Using the National Burn Repository, Chen et al evaluated for racial disparities after burn injury for six different racial and ethnic groups (white, black, Hispanic, Asian, Native American, and other). They found that black patients had the highest mortality and the highest percentage of people without insurance. Satahoo et al found that black race was an independent risk factor for deep vein thrombosis development after burn injury. It has also been shown that older blacks have a greater odd of amputation following traumatic lower extremity fractures.32 A larger comparative study is needed to evaluate for potential racial disparities in regards to amputations following burn injury.
Li et al evaluated a population of 82 amputees and noted that extent of injury at the initial insult was one of the most important risk factors for amputation.17 We found that risk of amputation increased by 3% for every percentage increase in TBSA. The TBSA in our amputation group, however, was much lower than that reported in other studies.2,3,8,17 The majority of amputations in our study cohort were minor, which may explain the lower overall %TBSA.
Limitations of this study include those inherent to the retrospective design of the study. Additionally, the findings of this single-institution study may not be generalizable. Other factors that would affect whether or not a patient would undergo amputation, including the specific location of burn injuries (ie, hand, torso, extremity), as well as depth and degree of burns, and knowledge of the reason for amputation, were not available in this database. A larger nationwide study is important to further elucidate the risk factors for amputation following burn injury.
CONCLUSIONS
Factors associated with increased risk of amputation following burn injury are electrical burns and other type of burns, the presence of preexisting comorbidities, black race, and increased %TBSA. The role of comorbidities and race on the risk of amputation requires further study.
Funding: Research reported in this manuscript was supported by the National Institutes of Health under award NIH Grant number 5T32GM008450-23.
REFERENCES
- 1. Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89:422–9. [DOI] [PubMed] [Google Scholar]
- 2. Soto CA, Albornoz CR, Peña V, Arriagada C, Hurtado JP, Villegas J. Prognostic factors for amputation in severe burn patients. Burns 2013;39:126–9. [DOI] [PubMed] [Google Scholar]
- 3. Tarim A, Ezer A. Electrical burn is still a major risk factor for amputations. Burns 2013;39:354–7. [DOI] [PubMed] [Google Scholar]
- 4. Hsueh YY, Chen CL, Pan SC. Analysis of factors influencing limb amputation in high-voltage electrically injured patients. Burns 2011;37:673–7. [DOI] [PubMed] [Google Scholar]
- 5. Luz DP, Millan LS, Alessi MS et al. Electrical burns: a retrospective analysis across a 5-year period. Burns 2009;35:1015–019. [DOI] [PubMed] [Google Scholar]
- 6. Yowler CJ, Mozingo DW, Ryan JB, Pruitt BA Jr. Factors contributing to delayed extremity amputation in burn patients. J Trauma 1998;45:522–6. [DOI] [PubMed] [Google Scholar]
- 7. Tapking C, Hundeshagen G, Popp D et al. The frequency and reason for amputations in electrically burned pediatric patients. J Burn Care Res 2019;40:107–11. [DOI] [PubMed] [Google Scholar]
- 8. Viscardi PJ, Polk HC Jr. Outcome of amputations in patients with major burns. Burns 1995;21:526–9. [DOI] [PubMed] [Google Scholar]
- 9. Kennedy PJ, Young WM, Deva AK, Haertsch PA. Burns and amputations: a 24-year experience. J Burn Care Res 2006;27:183–8. [DOI] [PubMed] [Google Scholar]
- 10. Williams ZF, Bools LM, Adams A, Clancy TV, Hope WW. Early versus delayed amputation in the setting of severe lower extremity trauma. Am Surg 2015;81:564–8. [PubMed] [Google Scholar]
- 11. Carrougher GJ, McMullen K, Mandell SP et al. Impact of burn-related amputations on return to work: findings from the burn injury model system national database. J Burn Care Res 2019;40:21–8. [DOI] [PubMed] [Google Scholar]
- 12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- 13. Aghakhani K, Heidari M, Tabatabaee SM, Abdolkarimi L. Effect of current pathway on mortality and morbidity in electrical burn patients. Burns 2015;41:172–6. [DOI] [PubMed] [Google Scholar]
- 14. Jang KU, Joo SY, Jo JH, Seo HC. Burn and amputations: a retrospective analysis 379 amputation out of 19,958 burns in 10-year. Int J Phys Med Rehabil 2018;6:2. [Google Scholar]
- 15. Ghavami Y, Mobayen MR, Vaghardoost R. Electrical burn injury: a five-year survey of 682 patients. Trauma Mon 2014;19:e18748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Özalp B, Calavul A. Amputations in burn patients with a special emphasis on pediatric patients. Erciyes Med J 2017;39:7–11. [Google Scholar]
- 17. Li Q, Wang LF, Chen Q, Wang SJ, Li F, Ba T. Amputations in the burn unit: a retrospective analysis of 82 patients across 12 years. Burns 2017;43:1449–54. [DOI] [PubMed] [Google Scholar]
- 18. U.S. Bureau of Labor and Statistics. Labor force statistics from the current population survey: employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity; accessed 22 Aug. 2018; available from https://www.bls.gov/cps/cpsaat18.htm.
- 19. Prasad JK, Bowden ML, McDonald K, Thomson PD. Rehabilitation of burned patients with bilateral above-knee amputations. Burns 1990;16:297–301. [DOI] [PubMed] [Google Scholar]
- 20. Ward RS, Hayes-Lundy C, Schnebly WA, Reddy R, Saffle JR. Rehabilitation of burn patients with concomitant limb amputation: case reports. Burns 1990;16:390–2. [DOI] [PubMed] [Google Scholar]
- 21. Pham TN, Carrougher GJ, Martinez E et al. Predictors of discharge disposition in older adults with burns: a study of the burn model systems. J Burn Care Res 2015;36:607–12. [DOI] [PubMed] [Google Scholar]
- 22. Pham TN, Kramer CB, Wang J et al. Epidemiology and outcomes of older adults with burn injury: an analysis of the national burn repository. J Burn Care Res 2009;30:30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Klein MB, Lezotte DC, Heltshe S et al. Functional and psychosocial outcomes of older adults after burn injury: results from a multicenter database of severe burn injury. J Burn Care Res 2011;32:66–78. [DOI] [PubMed] [Google Scholar]
- 24. Nygaard RM, Gayken JR, Endorf FW. Influence of insurance status on hospital length of stay and discharge location in burn patients. Am Surg 2018;84:924–9. [PubMed] [Google Scholar]
- 25. Knowlin L, Stanford L, Moore D, Cairns B, Charles A. The measured effect magnitude of co-morbidities on burn injury mortality. Burns 2016;42:1433–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Heng JS, Clancy O, Atkins J et al. Revised baux score and updated charlson comorbidity index are independently associated with mortality in burns intensive care patients. Burns 2015;41:1420–7. [DOI] [PubMed] [Google Scholar]
- 27. Swaminathan A, Vemulapalli S, Patel MR, Jones WS. Lower extremity amputation in peripheral artery disease: improving patient outcomes. Vasc Health Risk Manag 2014;10:417–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Resnick HE, Valsania P, Phillips CL. Diabetes mellitus and nontraumatic lower extremity amputation in black and white Americans: the National Health and Nutrition Examination Survey Epidemiologic Follow-up Study, 1971-1992. Arch Intern Med 1999;159:2470–5. [DOI] [PubMed] [Google Scholar]
- 29. Chen JH, Nosanov LB, Carney BC. Patient and social characteristics contributing to disparities in outcomes after burn injury: application of database research to minority health in the burn population. Am J Surg 2018;216:863–8. [DOI] [PubMed] [Google Scholar]
- 30. Satahoo SS, Parikh PP, Naranjo D et al. Are burn patients really at risk for thrombotic events? J Burn Care Res 2015;36:100–4. [DOI] [PubMed] [Google Scholar]
- 31. Bedri H, Romanowski KS, Liao J et al. A national study of the effect of race, socioeconomic status, and gender on burn outcomes. J Burn Care Res 2017;38:161–8. [DOI] [PubMed] [Google Scholar]
- 32. Weber DJ, Shoham DA, Luke A, Reed RL, II, Luchette FA. Racial odds for amputation ratio in traumatic lower extremity fractures. J Trauma 2011;71:1732–6. [DOI] [PubMed] [Google Scholar]