Abstract
Objectives
In the United Kingdom, three people die every day awaiting an organ transplant. To address this, Scotland and England plan to follow Wales and introduce opt‐out donor consent. However, emotional barriers, myths, and misconceptions may deter potential registrants. Our objectives were to estimate the number of people who plan to opt‐out of the donor register and to test whether emotional barriers (e.g., medical mistrust) differentiated participants within this group. Finally, in an experimental manipulation, we tested whether intention to donate decreased by making emotional barriers more salient and increased following a widely used myth‐busting intervention.
Design
Mixed between–within design.
Methods
UK residents (n = 1,202) were asked whether they would choose opt‐in, deemed consent, or opt‐out/not sure if legislation changes to opt‐out. Participants also completed measures of donor intentions at baseline, following a 12‐item emotional barriers questionnaire and again, following a 9‐item myth‐busting intervention.
Results
Findings indicate that 66.1% of participants selected to opt‐in to the donor register, 24.3% selected deemed consent, and 9.4% selected opt‐out/not sure. Emotional barriers, notably fears surrounding bodily integrity, were significantly elevated in participants who selected opt‐out/not sure. Increasing the salience of emotional barriers reduced donor intentions in the opt‐out/not sure group. However, dispelling organ donation myths did not increase intention within this group.
Conclusions
If opt‐out legislation is introduced in Scotland and England, approximately 10% of participants plan to opt‐out or are not sure. Dispelling organ donation myths with facts may not be the best method of overcoming emotional barriers and increasing donor intentions for those planning to opt‐out.
Statement of contribution.
What is already known about this subject?
In the United Kingdom, three people die every day waiting for an organ transplant. Although 90% of the UK population support organ donation, only 38% are registered donors. To address this, Scotland and England have recently proposed to introduce an opt‐out system of donor consent. To date, limited research has investigated public attitudes and intentions regarding opt‐out consent laws in Scotland and England.
Emotional barriers (e.g., medical mistrust) are key factors that may deter potential registrants. However, no research has examined these barriers in relation to proposed opt‐out consent laws.
Myth‐busting is widely used around the world as part of campaigns promoting organ donation. The NHS currently use a myth‐busting feature on their webpage to dispel harmful myths about organ donation; however, there is limited evidence of the impact this has on intentions to become an organ donor.
What does this study add?
Approximately 10% of UK participants plan to opt‐out or are unsure of their decision, if the law changes to opt‐out.
Emotional barriers, notably, bodily integrity fears, are significantly elevated in people who plan to opt‐out.
Increasing the salience of emotional barriers reduced donor intentions for people who plan to opt‐out.
A myth‐busting intervention had no effect on donor intentions for people who plan to opt‐out of the donor register.
Keywords: emotions, myths, opt‐out consent, organ donation
Background
Despite widespread support for organ donation around the world, there is a critical shortage of available organs for transplantation. Approximately 6,000 people in the United Kingdom are on the waiting list for an organ transplant. However, the insufficient supply of available organs meant that in 2017, 411 people died while awaiting a life‐saving transplant (NHSBT, 2018). This illustrates the pressing need to explore factors that both promote and deter organ donor intentions and behaviours, in order to encourage donation and save lives.
The Scottish and English Governments have recently proposed to change organ donor legislation from the current opt‐in registration system to an opt‐out system. At present, individuals must actively sign up and join the organ donor register (ODR); however, the proposals for opt‐out legislation remove this requirement and, instead, follow deemed consent (Human Tissue (Authorisation) (Scotland) Bill, 2018; Organ Donation (Deemed Consent) Act, 2018). This means that individuals are automatically presumed to consent for organ donation, unless they expressly wish not to donate and actively remove themselves from the ODR, thereby opting out.
The proposals for opt‐out consent legislation have been met with some controversy. There are concerns that an opt‐out system could detrimentally impact public support for organ donation and increase mistrust in the medical system, a pivotal factor in the abolishment and revision of opt‐out consent laws in Brazil and Chile (Domínguez & Rojas, 2013). Preceding the enactment of opt‐out consent in Wales, a 24‐month nationwide communication campaign was implemented to increase public awareness and support for opt‐out consent legislation (Welsh Government, 2016). This was accompanied by comprehensive research into opt‐out consent, which assessed public attitudes and awareness, and provided baseline assessments of public donor intentions. This revealed that less than half of respondents supported proposals for opt‐out consent and 19% reported intentions to opt‐out (Welsh Government, 2012). However, following an extensive communications campaign and enactment of the law, support for opt‐out consent increased to 71%, and to date, 6% of the Welsh population have actively removed themselves from the ODR (Young, McHugh, Glendinning, & Carr‐Hill, 2017). Very little research has investigated public attitudes regarding opt‐out consent laws in Scotland and England. Therefore, given the intrinsically sensitive and complex nature of opt‐out consent, exploration of public attitudes and intentions is critical.
Aside from nationwide legislative changes (e.g., opt‐out consent systems), numerous studies have sought to develop interventions to increase support for organ donation and subsequently increase registration. A recent large‐scale investigation attempted to increase organ donor registration by manipulating anticipated regret. However, the authors found that counter to expectation, pilot studies, and existing evidence, (O'Carroll, Dryden, Hamilton‐Barclay, & Ferguson, 2011; O'Carroll, Foster, McGeechan, Sandford, & Ferguson, 2011) a brief anticipated regret manipulation led to a decrease in verified organ donor registrations (O'Carroll, Shepherd, Hayes, & Ferguson, 2016). Participants in the intervention group also completed questions assessing emotional barriers towards organ donation (e.g., medical mistrust). The authors speculated that completion of these measures led to a negative contextual cuing effect and unintentionally amplified negative attitudes towards organ donation. To test this interpretation, the present research examines whether making emotional barriers salient reduces organ donor intentions.
Previous research has shown that emotional barriers towards organ donation consistently differentiate donors and non‐donors under current opt‐in legislation (Morgan, Stephenson, Harrison, Afifi, & Long, 2008; O'Carroll, Foster, et al., 2011; Shepherd & O'Carroll, 2014a). However, as far as the authors are aware, no research has investigated the aforementioned barriers in relation to opt‐out legislation. Therefore, in this research, we also test whether emotional barriers differentiate those who plan to opt‐out of the donor register following the introduction of opt‐out consent legislation.
Other salient factors thought to influence organ donor behaviour relate to people's knowledge and beliefs (Feeley, 2007). Although the general public reports an awareness of the organ donation shortage, studies have shown pervasive gaps in knowledge or misunderstandings surrounding organ donation, for example, regarding the concept of brain death (Horton & Horton, 1990). This, in turn, may contribute to the development of erroneous beliefs and myths, an important factor in reluctance to register. Further, myths and misconceptions are often exacerbated by harmful representations of organ donation, for example, through sensationalist media misrepresentations within popular entertainment TV programmes such as Grey's Anatomy (Quick, Morgan, LaVoie, & Bosch, 2014). Collectively, these factors intensify negative representations of organ donation and may contribute to the development and maintenance of misconceptions and myths that deter potential registrants.
The Organ Donation Taskforce, established by the UK Government in 2006 to identify and overcome barriers to organ donation, has reinforced the importance of correcting harmful myths and misconceptions. An independent taskforce report investigating the impact of opt‐out consent legislation in the United Kingdom, advocated for increased publicity and education to reduce harmful myths that negatively influence decisions to register as an organ donor (Organ Donation Taskforce, 2008). As a result, the NHS implemented a ‘myth busting’ feature on their website (https://www.organdonation.nhs.uk/supporting-my-decision/myth-busting/). The webpage presents common organ donation myths and misconceptions and then dispels them using corrective information and evidence. To date, limited research has explored this approach as a way of increasing organ donor intentions or registrations (Sukalla, Wagner, & Rackow, 2017). Similar methods have been used to dispel vaccine‐related myths, improve vaccination attitudes, and increase immunization rates for communicable diseases such as measles, mumps, and influenza (Hornsey, Harris, & Fielding, 2018). However, a recent study found that exposure to corrective information intended to dispel vaccination myths had a differential effect and significantly reduced intention to vaccinate in individuals with highest levels of vaccination concerns (Nyhan & Reifler, 2015). This finding supports the testing of the efficacy of similar public health interventions.
The current research
The objectives of this research were as follows: (1) to estimate the percentage of the Scottish, English, and Northern Irish population planning to opt‐out of the ODR following implementation of proposed opt‐out legislation, (2) to test whether emotional barriers (e.g., medical mistrust) differentiate those who plan to opt‐out, (3) to extend the findings of previous research (O'Carroll et al., 2016) and test whether making emotional barriers salient following exposure to an emotional barriers questionnaire reduces organ donor intentions, and finally (4) to test the efficacy of a current NHS strategy to reduce organ donation myths, by assessing the impact of a myth‐busting intervention on donor intentions. It was hypothesized that (1) participants who plan to opt‐out of the donor register will exhibit higher emotional barriers towards organ donation, (2) increasing the salience of these emotional barriers will result in decreased donor intentions, and (3) dispelling organ donation myths will increase donor intentions.
Methods
Power analysis
A G*Power calculation indicated that using ANOVA with three groups, a total sample of 969 participants would be sufficient to detect a small effect size of f = .01 at an alpha level of .05 and a power of .80 (Cohen, 1988). The target sample size was achieved, and a preliminary analysis of the first 100 responses was conducted to determine the number of responses that satisfied basic criteria for inclusion. Inclusion was defined as completion of the three primary intention measures. Of this sample, 14 responses did not satisfy the inclusion criterion. Therefore, it was necessary to increase the recruitment target to ensure sufficient responses to achieve adequate statistical power. Recruitment was continued until a final sample of 1202 responses was obtained.
Recruitment and Inclusion
Recruitment took place between the 24th of January and the 12th of March 2018. Participants were opportunistically recruited after responding to online advertisements posted on social media websites. The advertisement contained an URL link to the questionnaire which was delivered via Qualtrics, a web‐based research platform (https://www.qualtrics.com/uk/). Inclusion criteria were as follows, aged over 18 years and currently resident in either Scotland, England, or Northern Ireland.
Participants
A total of 1,202 members of the adult general public from Scotland, England, and Northern Ireland participated in this online study. The overall sample largely consisted of female participants (80.9%), with a mean age of 39.8 years (SD = 12.5). Of the overall sample, 87.8% (n = 1,055) were currently resident in Scotland, 11% (n = 132) resident in England, and 1.2% (n = 15) resident in Northern Ireland.1 The demographic characteristics of the participant groups are available in Table 1.
Table 1.
Demographic characteristics of the opt‐in, deemed consent, and combined opt‐out/not sure groups
| I would opt‐in (n = 794) | Deemed consent (n = 292) | I would opt‐out/not sure (n = 113) | |
|---|---|---|---|
| Age (SD) | 37.90 (11.90) | 43.17 (12.47) | 44.72 (13.54) |
| Gender | |||
| Male | 119 | 73 | 24 |
| Female | 665 | 217 | 88 |
| Othera . | 10 | 2 | 1 |
| Education level (%) | |||
| Lower education | 349 (43.95) | 135 (46.39) | 67 (59.29) |
| Higher educationb | 445 (56.05) | 156 (53.61) | 45 (39.82) |
| Employment status (%) | |||
| Employed | 578 (72.9) | 214 (73.8) | 76 (67.3) |
| Unemployed | 23 (2.9) | 9 (3.1) | 4 (3.5) |
| Student | 120 (15.1) | 30 (10.3) | 7 (6.2) |
| Retired | 29 (3.7) | 24 (8.3) | 15 (13.3) |
| Other | 43 (5.4) | 13 (4.5) | 11 (9.7) |
| Organ donor status (%) | |||
| Yes | 691 (87) | 137 (46.9) | 15 (13.27) |
| No | 53 (6.3) | 115 (39.45) | 92 (81.42) |
| Not sure | 50 (6.3) | 40 (13.7) | 6 (5.31) |
Four individuals from the opt‐in group identified as transgender. Nine individuals declined to state their gender, six from the opt‐in group, two from the deemed consent group, and one from the opt‐out/not sure group.
Higher education was categorized as any participant who had completed a Bachelor's degree.
Procedure and measures
Ethical approval for this study was obtained from the University of Stirling General University Ethics Panel. The study was delivered in the format of an online questionnaire via Qualtrics. Participants responded to online advertisements for the research, containing a link to the questionnaire. Following the presentation of study information and eligibility criteria, participants provided informed consent by selecting an electronic check box. Participants initially completed questions measuring demographic information, followed by measures assessing organ donor status and previous organ or blood donation experience. Participants were then asked about their awareness of the current organ donor consent system and the proposed legislative changes in Scotland and England (opt‐out system).
The main dependent variable was anticipated organ donor status following the introduction of an opt‐out organ donor system. Participants were initially presented with information regarding the proposed legislative changes (available as Appendix S1) and asked, ‘If the organ donation laws in your country change to an opt‐out system, what would your choice be?’ The potential responses were as follows; (1) I would opt‐in (I want to be an organ donor), (2) I have no objection to donating my organs (deemed consent to be an organ donor), (3) I would opt‐out (I do not want to be an organ donor), and (4) not sure.
Organ donation myths
The organ donation myths used in the myth‐correcting intervention were adapted from a myth‐busting webpage used by NHS Blood and Transplant https://www.organdonation.nhs.uk/supporting-my-decision/myth-busting/. The webpage presents 14 common myths and misconceptions surrounding organ donation and provides corrective information to refute and dispel each myth. Nine myths were reviewed and selected for the intervention. Information that may have primed a response from participants, for example, appeals for readers to ‘leave a lasting legacy and join the donor register’ were omitted. Within the current study, participants were presented with each of the nine statements and asked to select whether they believed the statement to be ‘true’ or ‘false’. Regardless of the response, participants were then presented with the correct answer and corrective information to serve as a myth‐correcting intervention. Participants’ responses to the true or false statements were also used as a measure of organ donation knowledge, with higher scores indicating greater organ donation knowledge (lower belief in myths). The nine myths and counterevidence used in the intervention are available as Appendix S2. An example is provided in Figure 1.
Figure 1.
Example myth and corrective information presented during the myth‐correcting intervention.
Experimental manipulation
The order of the experimental manipulation was counterbalanced to control for potential order effects. Participants were randomly allocated via Qualtrics to receive either the emotional barriers questionnaire followed by the myth‐busting intervention or, alternatively, completed the myth‐busting intervention followed by measures of emotional barriers. The study procedure is illustrated in Figure 2.
Figure 2.
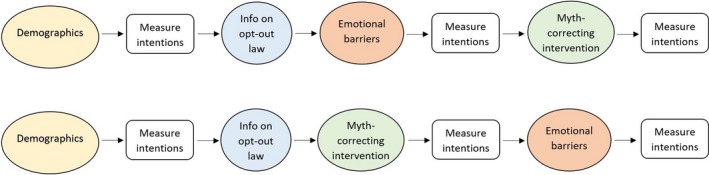
Study procedure diagram. [Colour figure can be viewed at wileyonlinelibrary.com]
Dependent variables
Emotional barriers
Emotional barriers towards organ donation were measured using an adapted version of the attitudes towards organ donation scale (Morgan et al., 2008). In their original research, Morgan et al. (2008) examined various factors thought to impact beliefs surrounding organ donation. It was found that visceral ‘non‐cognitive’ emotional beliefs, for example, feelings of disgust regarding organ donation, play the greatest role in predicting organ donor behaviours in comparison with cognitive‐rational factors, such as one's knowledge surrounding organ donation.
The present study used a 12‐item scale, which measured four affective attitudes towards organ donation, bodily integrity, medical mistrust, the ick factor, and the jinx factor. Responses were scored on a 7‐point Likert scale ranging from 1 ‘strongly disagree’ to 7 ‘strongly agree’. Given that the process of registering as an organ donor is now predominantly completed online without the requirement to physically sign a donor card, the wording in three of the questions was modified. The phrase ‘signing an organ donor card’ was amended to ‘register as an organ donor’.
Bodily integrity
This concerns the belief that the body should remain whole after death. Bodily integrity was measured by two items (α = .74). An example item is, ‘Removing organs from the body just isn't right’. Higher scores are indicative of greater bodily integrity concerns.
Jinx factor
This relates to fears and superstitions that misfortune will arise following organ donor registration. The jinx factor was measured by three items. An example item is, ‘Organ donors may not be resurrected because they don't have all of their parts’. Higher scores indicate a stronger feeling that it is bad luck to talk about death or register as an organ donor. The reliability of the 3‐item jinx factor scale was low (α = .50). Deletion of question 2 from this scale, ‘The surest way to bring about my own death is to make plans for it like registering as an organ donor’ increased the reliability of the scale to α = .60.2
Ick factor
This represents an aversion to the concept of organ donation and is associated with concerns regarding mutilation of the body during the donation process. The ick factor was measured by three items (α = .78). An example item is, ‘The idea of organ donation is somewhat disgusting’. Higher scores indicate greater feelings of revulsion at the idea of organ donation.
Medical mistrust
This represents fears regarding the medical profession in relation to organ donation. Medical mistrust was measured by four items (α = .70). An example item is, ‘If I register as an organ donor, doctors might take my organs before I'm actually dead’. Higher scores indicate stronger medical mistrust.
Organ donor intention
Intentions regarding organ donation were measured at three time points throughout this study (baseline, post‐myth busting, and post‐emotional barriers questionnaire) using the following question, ‘I intend to donate my organs after death’. Responses were scored on a 7‐point Likert scale ranging from 1 ‘strongly disagree’ to 7 ‘strongly agree’. Higher scores are indicative of greater intentions to donate.
Data preparation and analysis
Analyses were conducted using SPSS version 23. Participants were initially grouped based on their response to the following question, ‘If the organ donation laws in your country change to an opt‐out system, what would your choice be?’
Responses were as follows: opt‐in, deemed consent, opt‐out, and not sure. Of the total sample, 1,199 participants answered this question. Because of the low numbers reporting opt‐out intentions and to ensure adequate cell sizes for analysis, the response variables opt‐out and not sure were collapsed and the analysis conducted with a three‐group comparison (opt‐in, deemed consent, and opt‐out/not sure).3
Differences in demographic characteristics between participant groups were assessed using chi‐squared tests and one‐way ANOVAs. To test for differences in responses to the myth‐correcting intervention, a one‐way ANOVA was conducted. This was followed up using a Games–Howell post‐hoc test. A repeated measures ANOVA was then conducted to compare differences in donor intentions across experimental conditions (baseline, post‐myth busting, and post‐emotional barriers questionnaires) for participants in different groups. A series of post‐hoc paired samples t‐tests were run to further explore these results. To investigate the impact of exposure to emotional barriers on participants’ donor intentions between the different groups, a multivariate analysis of variance (MANOVA) was conducted. This was followed up using univariate ANOVAS on each of the emotional barriers. Group‐level differences were explored using a Games–Howell post‐hoc test, used to correct for a violation of the assumption of homogeneity.
Partial η2 effect sizes were generated throughout the analysis; for interpretation, the square root of these values was calculated to enable interpretation of effect size r. According to Cohen (1988), an r of .1 represents criteria for a ‘small’ effect size, .3 represents a ‘medium’ effect size, and .5 represents a ‘large’ effect size.
There was a small amount of missing data for study dependent variables, anticipated organ donor status (0.25%), organ donation myths (0.23%), and the emotional barriers questionnaire (0.55%). As a result, listwise deletion was implemented throughout the analysis.
Results
Demographic characteristic comparisons
Descriptive data of participant characteristics can be found below, in Table 1. Comparisons between the participant groups (opt‐in, deemed consent and opt‐out/not sure) revealed significant differences in age, F (2, 1133) = 28.34, p < .001; and gender, x 2 (8, n = 1,199) = 18.44, p = .018. Significant differences were also found in education, x 2 (2, n = 1,197) = 9.97, p = .007; and employment status, x 2 (8, n = 1,196) = 33.68, p = <.001.
To explore differences in baseline intention between male and female participants, an independent samples t‐test was conducted. Baseline intention was significantly higher in female participants (M = 5.77, SD = 2.08) in comparison with male participants (M = 5.37, SD = 2.13), t(1187) = −2.52, p = .01.
Anticipated organ donor status following the introduction of opt‐out consent
Frequency counts indicated that 66.1% (n = 794) of participants selected to ‘opt‐in’ to the ODR following the proposed law change. 24.3% (n = 292) of participants selected ‘deemed consent to be an organ donor’, 4.2% (n = 50) of participants selected to ‘opt‐out’, and 5.2% (n = 63) of participants selected ‘not sure’.
Organ donation myths
Participant responses from the organ donation knowledge test are shown in Table 2. To test for potential differences in scores between participants in the opt‐in, deemed consent, and opt‐out/not sure groups, a one‐way ANOVA was conducted. To control for a violation of homogeneity of variances, a Welch ANOVA was implemented. Significant differences were found between participants’ scores in the opt‐in (M score = 7.61, SD = 1.02), deemed consent, (M score = 7.52, SD = 1.04), and opt‐out/not sure group (M score = 7.05, SD = 1.36), Welch's F(2, 261.6) = 9.22, p < .001. A Games–Howell post‐hoc analysis revealed that participants in the opt‐in and deemed consent group had significantly higher scores in comparison with participants in the opt‐out/not sure group at p < .001 and p = .003, respectively. Higher scores indicate greater knowledge of organ donation (lower belief in myths).
Table 2.
Percentage responses to organ donation myths for the opt‐in, deemed consent, and combined opt‐out/not sure group (all answers are false)
| Statement | Group | N | Response % | |
|---|---|---|---|---|
| True | False | |||
| 1. Doctors might not do their best to save someone's life if they know they are on the NHS Organ Donor Register | I would opt‐in | 793 | 2.6 | 97.4 |
| I have no objection to donating my organs (deemed consent for organ donation) | 292 | 4.1 | 95.9 | |
| I would opt‐out/not sure | 112 | 21.4 | 78.6 | |
| 2. People could still be alive when their organs are removeda | I would opt‐in | 793 | 44 | 56 |
| I have no objection to donating my organs (deemed consent for organ donation) | 291 | 42.6 | 57.4 | |
| I would opt‐out/not sure | 113 | 47.8 | 52.2 | |
| 3. Organ donation is against many religious beliefs | I would opt‐in | 793 | 59.3 | 40.7 |
| I have no objection to donating my organs (deemed consent for organ donation) | 291 | 63.2 | 36.8 | |
| I would opt‐out/not sure | 113 | 68.1 | 31.9 | |
| 4. Organ Donation leaves the body disfigured and afterwards, people won't be able to have an open‐casket funeral | I would opt‐in | 791 | 1.5 | 98.5 |
| I have no objection to donating my organs (deemed consent for organ donation) | 291 | 1.7 | 98.3 | |
| I would opt‐out/not sure | 113 | 7.1 | 92.9 | |
| 5. There is an age limit for organ donation | I would opt‐in | 793 | 18.4 | 81.6 |
| I have no objection to donating my organs (deemed consent for organ donation) | 290 | 21.0 | 79.0 | |
| I would opt‐out/not sure | 113 | 18.6 | 81.4 | |
| 6. The NHS only need adult organ donors | I would opt‐in | 791 | 0.1 | 99.9 |
| I have no objection to donating my organs (deemed consent for organ donation) | 292 | 0.3 | 99.7 | |
| I would opt‐out/not sure | 113 | 0 | 100 | |
| 7. There are enough organs available for the people waiting for an organ transplant | I would opt‐in | 791 | 1.0 | 99.0 |
| I have no objection to donating my organs (deemed consent for organ donation) | 292 | 1.0 | 99.0 | |
| I would opt‐out/not sure | 113 | 0.0 | 100 | |
| 8. People who have medical conditions can't donate | I would opt‐in | 790 | 6.7 | 93.3 |
| I have no objection to donating my organs (deemed consent for organ donation) | 292 | 8.9 | 91.1 | |
| I would opt‐out/not sure | 112 | 18.8 | 81.3 | |
| 9. Donated organs can be bought and sold | I would opt‐in | 793 | 5.0 | 95.0 |
| I have no objection to donating my organs (deemed consent for organ donation) | 292 | 5.1 | 94.9 | |
| I would opt‐out/not sure | 113 | 12.4 | 87.6 | |
NHS = National Health Service.
The high percentage of incorrect responses may result from ambiguity in this question regarding the potential to donate organs as a living donor.
Emotional barriers: Hypothesis 1
A multivariate analysis of variance (MANOVA) was conducted to investigate the differences between the participant groups (opt‐in, deemed consent, and opt‐out/not sure) on measures of emotional barriers towards organ donation (bodily integrity, medical mistrust, ick, and jinx). A statistically significant difference between the groups on the combined dependent variables was found, F(8, 2304) = 49.98, p < .001; Pillai's V = .296; r = .38. Mean emotional barriers scores for each of the groups are graphically represented in Figure 3.
Figure 3.
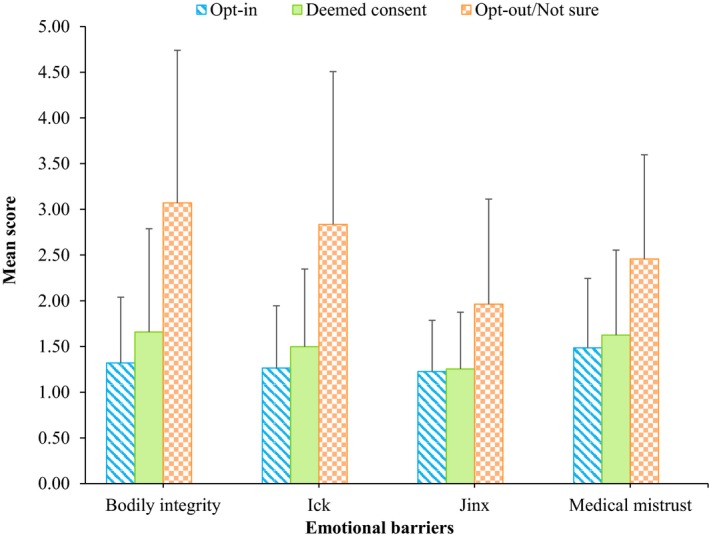
Bar graph showing mean emotional barriers scores of the three participant groups. Error bars are SDs. [Colour figure can be viewed at wileyonlinelibrary.com]
To ascertain which of the outcome variables are contributing to the significant MANOVA, a series of univariate ANOVAs on each of the emotional barriers were conducted. To differentiate group‐level differences, a Games–Howell post‐hoc test was conducted. This post‐hoc test was selected to correct for a violation of homogeneity of variances.
Bodily integrity
ANOVAs revealed a statistically significant difference in bodily integrity scores between the groups, F (2, 1154) = 158.73, p < .001; r = .46. Post‐hoc analysis revealed significant differences across all group comparisons. Bodily integrity scores were highest in the opt‐out/not sure group, in comparison with both the opt‐in and the deemed consent groups. These differences were all significant at p < .001. Higher scores are indicative of greater bodily integrity concerns.
Ick factor
A statistically significant difference in ick factor scores between the groups was found, F (2, 1154) = 155.39, p < .001; r = .46. Post‐hoc analysis revealed significant differences across all group comparisons. Ick factor scores were highest in the opt‐out/not sure group, in comparison with the opt‐in and deemed consent groups. These differences were all significant at p < .001. Higher scores indicate greater feelings of revulsion at the idea of organ donation.
Jinx factor
A statistically significant difference in jinx factor scores between the groups was also found, F (2, 1154) = 60.34, p < .001; r = .31. Post‐hoc analysis revealed that participants in the opt‐out/not sure group had significantly higher jinx factor scores than both those who plan to opt‐in and those who would follow deemed consent; opt‐out/not sure > opt‐in and deemed consent, both at p < .001. Higher scores indicate stronger feelings that it is bad luck to talk about death or becoming an organ donor. No significant differences in jinx factor scores were found between those in the opt‐in versus those in the deemed consent group, p = .766.
Medical mistrust
ANOVAs revealed a statistically significant difference in medical mistrust scores between the groups, F (2, 1154) = 57.11, p < .001; r = .30. Post‐hoc analysis revealed that participants in the opt‐out/not sure group had significantly higher medical mistrust scores than both the opt‐in and deemed consent groups; opt‐out/not sure > opt‐in and deemed consent, both at p < .001. Higher scores indicate stronger medical mistrust. No significant differences in medical mistrust scores were found between those in the opt‐in versus those in the deemed consent group, p = .060.
To investigate differences in emotional barriers between male and female participants, a series of independent samples t‐test was conducted. Bodily integrity scores were significantly higher (indicative of greater bodily integrity concerns) in male participants (M = 1.75, SD = 1.20) in comparison with female participants (M = 1.54, SD = 1.07), t(291.74) = 2.38, p = .02. No such differences between the remaining emotional barriers (medical mistrust, ick, and jinx) were found.
Experimental manipulation: Hypotheses 2 and 3
A repeated measures ANOVA was run to investigate differences in donor intentions as a function of time point (baseline, post‐myth busting, and post‐emotional barriers questionnaire) and group (opt‐in, deemed consent, and opt‐out/not sure). Mauchly's test of sphericity indicated that the assumption of sphericity was violated, (2) = 96.38, p < .001. As estimated epsilon was greater than 0.75, a Huynh–Feldt correction was applied. A main effect of group was found, F (2, 1196) = 159.83, p < .001, r = .46. Donor intentions significantly differed between participant groups. There was a significant main effect of time, F (1.86, 2227.01) = 3.71, p = .027, r = .05. Intention to donate organs significantly differed between baseline, post‐myth busting, and post‐emotional barriers questionnaires. A significant interaction between time point and group was also found, F (3.72, 2227.01) = 2.90, p = .024, r = .07, ε =.93. A graphical representation of intention over the three time points for each group is displayed in Figure 4.
Figure 4.
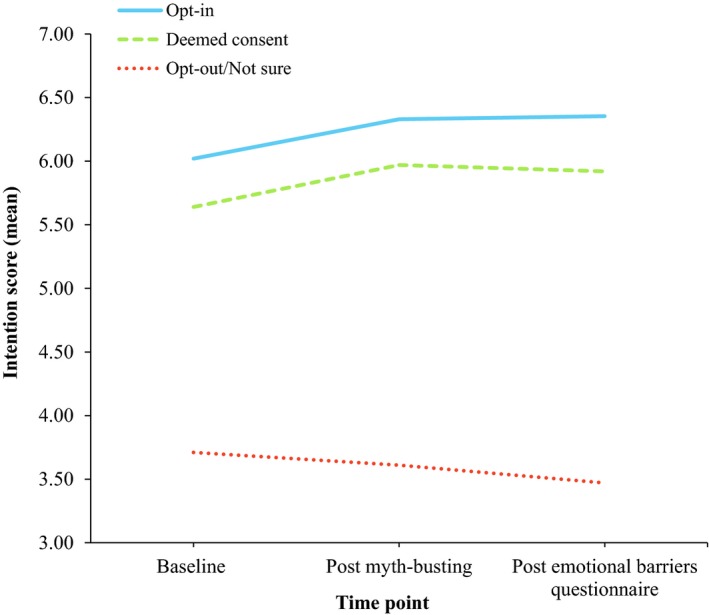
Line graph showing the mean intention to donate organs (7‐point scale) over baseline, post‐myth busting, and post‐emotional barriers time points, across the three participant groups. [Colour figure can be viewed at wileyonlinelibrary.com]
Effect of increasing the salience of emotional barriers on organ donor intentions: Hypothesis 2
To determine whether increasing the salience of emotional barriers reduced participants’ intentions to donate organs, post‐hoc paired samples t‐tests were conducted. For participants in the opt‐in group, exposure to the emotional barriers questionnaire significantly increased intention in comparison with baseline t(793) = −4.47, p < .001. For participants in the deemed consent group, exposure to the emotional barriers questionnaire also significantly increased intention in comparison with baseline, t(291) = −2.77, p = .006. However, for participants in the combined opt‐out/not sure group, exposure to the emotional barriers questionnaire decreased intention (M = 3.47, SD = 1.80), in comparison with baseline (M = 3.71, SD = 1.88), t(112) = 1.81, p = .07.
Effect of dispelling myths on organ donor intentions: Hypothesis 3
To determine whether correcting myths would increase participants’ intentions to donate organs, post‐hoc paired samples t‐tests were conducted. For participants who selected to opt‐in to the ODR, dispelling myths significantly increased intention in comparison with baseline, t(793) = −4.86, p < .001. For participants who selected deemed consent for organ donation, dispelling myths also significantly increased intention in comparison with baseline, t(291) = −3.65, p < .001. However, for the combined opt‐out/not sure participant group, dispelling myths had no significant effect on intention (M = 3.61, SD = 1.83) in comparison with baseline (M = 3.71, SD = 1.88).
Supplementary analysis of registered donors and non‐donors
A supplementary analysis was then conducted to investigate differences between participants who were currently registered organ donors and who selected opt‐in or deemed consent, n = 828 (Group 1), versus those who were not registered as organ donors but who also selected to opt‐in or follow deemed consent, n = 168 (Group 2).
An independent samples t‐test found a significant difference in baseline donor intention: Group 1 had higher baseline intentions (M = 6.13, SD = 2.01) in comparison with Group 2 (M = 4.97, SD = 1.63) t(994) = −6.99, p < .001.
A series of independent samples t‐tests were then conducted to test for differences in emotional barriers. Group 2 had significantly higher emotional barrier scores than participants in Group 1; these differences were all significant at p < .001. Means and standard deviations for each of the emotional barriers are provided in Table 3.
Table 3.
Means and standard deviations for emotional barrier scores in registered donors and non‐donors who plan to opt‐in or follow deemed consent
| Group 1: Registered donor opt‐in or deemed consent (n = 828) | Group 2: Non‐donor opt‐in or deemed consent (n = 168) | |
|---|---|---|
| Bodily integrity (SD) | 1.30 (0.71) | 1.92 (1.22) |
| Ick factor (SD) | 1.25 (0.66) | 1.63 (0.91) |
| Jinx factor (SD) | 1.20 (0.53) | 1.41 (0.76) |
| Medical mistrust (SD) | 1.46 (0.71) | 1.78 (1.06) |
Higher scores are indicative of greater emotional barriers towards organ donation.
Discussion
Intent to opt‐out
This study investigated the percentage of the population planning to opt‐out of the donor register if the organ donation laws change to an opt‐out system in Scotland and England. Approximately 10% of respondents plan to actively opt‐out of the organ donor register or are unsure of their decision if the law changes to opt‐out. Notably, this figure is less than baseline assessments recorded in Wales during 2012, whereby 19% of the population indicated an intent to actively opt‐out of the donor register (Welsh Government, 2012). This may suggest greater preliminary support for opt‐out legislation in Scotland and England. It should be noted that support for organ donation may be overinflated among our respondents as over 70% reported being registered as donors, in comparison with the 38% UK average (NHSBT, 2018).
Do emotional barriers differentiate participants who plan to opt‐out?
The present research found that individuals who intend to remove themselves from the ODR if opt‐out consent is introduced had significantly higher negative emotional barriers towards organ donation, in comparison with participants who plan to opt‐in or follow deemed consent. In particular, bodily integrity concerns were most prominent within this group. Fears that the physical integrity of the body may be violated as a consequence of organ donation have recurrently emerged within both quantitative and qualitative literature as a key barrier to organ donor registration in opt‐in countries (Morgan et al., 2008; Newton, 2011; Shepherd & O'Carroll, 2014b). The findings from this research confirm that bodily integrity concerns are also important barriers in relation to opt‐out consent legislation. Previous qualitative research examining the public opinions of opt‐out donor consent has emphasized bodily integrity concerns in the following quote, ‘So if they will take away my kidneys, will I be resurrected with them missing?’ (Lauri, 2009) Concerns that, after organ donation, the body would be regarded as incomplete are intrinsically difficult to dispel and overcome. This fear may also be exacerbated by misconceptions surrounding religion and organ donation. Notably, more than half of the respondents in this study believed that organ donation was against most religious beliefs.
Experimental manipulation
This research also examined the effect of increasing the salience of emotional barriers and a brief NHS myth‐correcting intervention on participants’ intention to donate organs. Based on previous research (O'Carroll et al., 2016), it was hypothesized that increasing the salience of emotional barriers towards organ donation, by completing an emotional barriers questionnaire, would decrease intention to donate organs after death. We observed a differential effect and found that counter to expectation; exposure to emotional barriers significantly increased intention to donate for both the opt‐in and deemed consent groups. However, for participants in the opt‐out/not sure group, increasing the salience of emotional barriers slightly reduced intention, although this did not reach threshold for significance. Therefore, for participants inclined to opt‐out of the donor register, increasing the salience of emotional barriers may have amplified negative barriers towards organ donation.
A brief NHS myth‐correcting intervention was found to significantly increase intention to donate for participants who plan to opt‐in or select deemed consent. However, for participants in the opt‐out/not sure group, the group one would be most hoping to influence, and dispelling myths had no significant effect on intention to donate. This finding is consistent with extant literature on the use of corrective factual information to dispel antivaccination myths. Such interventions are reported in the literature to be either ineffective or detrimental towards vaccination intentions (Hornsey et al., 2018; Nyhan & Reifler, 2015). Moreover, this effect is reported to be amplified for individuals with more negative attitudes and heightened vaccination concerns (Nyhan, Reifler, Richey, & Freed, 2014).
Although corrective information provides the reader with rational evidence to refute harmful myths, information provision was not sufficient to change donor intentions for those inclined to opt‐out. Notably, participants who plan to opt‐out exhibited significantly higher negative emotional barriers towards organ donation. Extensive research has shown that emotions and affective attitudes play the greatest role in predicting organ donor behaviours (Morgan et al., 2008; O'Carroll, Foster, et al., 2011). However, the myth‐busting intervention targeted facts rather than feelings. Adopting a dual‐process perspective (Strack & Deutsch, 2004), interventions that target ‘facts’ may have a limited impact on donor intentions that are driven by ‘feelings’ (emotional barriers). This may explain why the act of presenting corrective rational evidence was not sufficient to dispel deep‐set myths and, subsequently, influence intention. Moreover, the potential persuasiveness of information increases following readers perceptions of credibility (Henkel & Mattson, 2011). Although the myths and counterevidence within this manipulation were derived from the NHS, participants were not explicitly made aware of this. Consequently, the credibility and thus the effectiveness of the intervention may have been undermined. The present research also found female participants to have higher baseline donor intentions than males. This finding reinforces that of previous research from O'Carroll et al. (2016), which found female participants more likely to register as organ donors in comparison with males.
Implications and future directions
As media campaigns designed to dispel harmful myths about organ donation are common within organ donation campaigns, rigorous evaluations of their efficacy and mechanisms of effect are essential. This is crucial, as such campaigns could potentially have deleterious effects on intentions towards health‐related behaviours for those with heightened negative attitudes (Nyhan et al., 2014). Research has shown that emotions play the biggest role in predicting organ donor behaviours (Morgan et al., 2008). However, the myth‐busting intervention currently used by the NHS targets facts rather than feelings. Previous research has found narrative communication campaigns that employ fictional testimonies to refute organ donation myths, to be more effective at increasing donor consent in comparison with corrective statistical based information (Weber, Martin, & Corrigan, 2006). Interventions that target feelings and emotions may be more effective at overcoming deep‐set emotional beliefs and increasing donor intentions. Future studies are required to test this.
Limitations
Potential limitations of this research concern the generalizability of the findings to the UK general public. The use of volunteer sampling enabled the recruitment of a large sample; however, there may have been a selection bias among respondents, as over 70% of participants self‐reported being registered as organ donors. This is significantly higher than the 38% of the U.K. population currently on the ODR (NHSBT, 2018). Therefore, support for organ donation may have been over‐represented in this sample. Additionally, the study sample primarily consisted of people living in Scotland, and only a small percentage of respondents reported to be living in England and Northern Ireland. This again may reduce the generalizability of the findings to populations outside of Scotland. Moreover, this study relied on self‐report measures of organ donor intentions. This was essential, as opt‐out legislation has not yet been introduced in Scotland and England. Therefore, the use of self‐report intention measures provides an important estimate of the nation's probable behaviour. Following the introduction of opt‐out consent legislation, future studies should test whether the findings are replicated in between‐group analyses using verified measures of organ donor behaviour.
Conclusions
Approximately 10% of participants plan to opt‐out of the organ donor register or are unsure of their decision if opt‐out consent legislation is introduced. Emotional barriers towards organ donation were significantly higher in participants inclined to opt‐out of the register. Therefore, before the implementation of planned opt‐out legislation, rigorous evaluation of interventions to counter these potential barriers is imperative. Moreover, dispelling organ donation myths using corrective factual information may not be the best means of increasing donor intentions for those most likely to opt‐out, as it is using facts to challenge feelings. Public health campaigns designed to target emotional beliefs regarding donor intentions require rigorous evaluation.
Conflict of interest
All authors declare no conflict of interest.
Supporting information
Appendix S1. Information presented to participants regarding proposed changes to organ donor laws.
Appendix S2. Myths and counterevidence used in the myth‐correcting intervention.
Footnotes
The analysis was repeated with only the participants from Scotland, and the same results were obtained. These results are available on request from the authors.
Data analysis was repeated with question 2 of the jinx factor subscale removed. The same results were obtained; therefore, all three items from the jinx subscales were retained.
The analysis was rerun with a four‐group comparison (opt‐in, deemed consent, opt‐out, and not sure). In this analysis, very similar results were found, with the not sure responses falling between opt‐out and deemed consent. These results are available on request from the authors.
References
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Domínguez, J. , & Rojas, J. (2013). Presumed consent legislation failed to improve organ donation in Chile. Transplantation Proceedings, 45(4), 1316–1317. 10.1016/j.transproceed.2013.01.008 [DOI] [PubMed] [Google Scholar]
- Feeley, T. H. (2007). College students’ knowledge, attitudes, and behaviors regarding organ donation: An integrated review of the literature. Journal of Applied Social Psychology, 37(2), 243–271. 10.1111/j.0021-9029.2007.00159.x [DOI] [Google Scholar]
- Henkel, L. A. , & Mattson, M. E. (2011). Reading is believing: The truth effect and source credibility. Consciousness and Cognition, 20(4), 1705–1721. 10.1016/j.concog.2011.08.018 [DOI] [PubMed] [Google Scholar]
- Hornsey, M. J. , Harris, E. A. , & Fielding, K. S. (2018). The psychological roots of anti‐vaccination attitudes: A 24‐nation investigation. Health Psychology, 37(4), 307 http://psycnet.apa.org/doi/10.1037/hea0000586 [DOI] [PubMed] [Google Scholar]
- Horton, R. L. , & Horton, P. J. (1990). Knowledge regarding organ donation: Identifying and overcoming barriers to organ donation. Social Science and Medicine, 31(7), 791–800. 10.1016/0277-9536(90)90174-Q [DOI] [PubMed] [Google Scholar]
- Human Tissue (Authorisation) (Scotland) Bill (2018). Retrieved from http://www.parliament.scot/Human%20Tissue%20(Authorisation)%20(Scotland)%20Bill/SPBill32S052018.pdf.
- Lauri, M. A. (2009). Metaphors of organ donation, social representations of the body and the opt‐out system. British Journal of Health Psychology, 14(4), 647–666. 10.1348/135910708X397160 [DOI] [PubMed] [Google Scholar]
- Morgan, S. E. , Stephenson, M. T. , Harrison, T. R. , Afifi, W. A. , & Long, S. D. (2008). Facts versus feelings’ how rational is the decision to become an organ donor? Journal of Health Psychology, 13(5), 644–658. 10.1177/1359105308090936 [DOI] [PubMed] [Google Scholar]
- Newton, J. D. (2011). How does the general public view posthumous organ donation? A meta‐synthesis of the qualitative literature. BMC Public Health, 11, 791 10.1186/1471-2458-11-791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHSBT (2018). Organ donation and transplantation: Activity report 2017/18. Retrieved from https://nhsbtdbe.blob.core.windows.net/umbraco-assets/1848/transplant-activity-report-2017-2018.pdf
- Nyhan, B. , & Reifler, J. (2015). Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine, 33(3), 459–464. 10.1016/j.vaccine.2014.11.017 [DOI] [PubMed] [Google Scholar]
- Nyhan, B. , Reifler, J. , Richey, S. , & Freed, G. L. (2014). Effective messages in vaccine promotion: A randomized trial. Pediatrics, 133(4), e835–e842. 10.1542/peds.2013-2365 [DOI] [PubMed] [Google Scholar]
- O'Carroll, R. E. , Dryden, J. , Hamilton‐Barclay, T. , & Ferguson, E. (2011). Anticipated regret and organ donor registration—A pilot study. Health Psychology, 30(5), 661 http://psycnet.apa.org/doi/10.1037/a0024182 [DOI] [PubMed] [Google Scholar]
- O'Carroll, R. E. , Foster, C. , McGeechan, G. , Sandford, K. , & Ferguson, E. (2011). The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychology, 30(2), 236 http://psycnet.apa.org/doi/10.1037/a0022379 [DOI] [PubMed] [Google Scholar]
- O'Carroll, R. E. , Shepherd, L. , Hayes, P. C. , & Ferguson, E. (2016). Anticipated regret and organ donor registration: A randomized controlled trial. Health Psychology, 35(11), 1169 10.1037/hea0000363 [DOI] [PubMed] [Google Scholar]
- Organ Donation (Deemed Consent) Act (2018). Retrieved from https://publications.parliament.uk/pa/bills/cbill/2017-2019/0268/180268.pdf.
- Organ Donation Taskforce (2008). The potential impact of an opt out system for organ donation in the UK. Retrieved from https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4250/thepotentialimpactofanoptoutsystemfororgandonationintheuk.pdf
- Quick, B. L. , Morgan, S. E. , LaVoie, N. R. , & Bosch, D. (2014). Grey's Anatomy viewing and organ donation attitude formation: Examining mediators bridging this relationship among African Americans, Caucasians, and Latinos. Communication Research, 41(5), 690–716. 10.1177/0093650213475476 [DOI] [Google Scholar]
- Shepherd, L. , & O'Carroll, R. E. (2014a). Do affective attitudes predict organ donor registration? A prospective study. Journal of Health Psychology, 19(10), 1329–1333. 10.1177/1359105313488984 [DOI] [PubMed] [Google Scholar]
- Shepherd, L. , & O'Carroll, R. E. (2014b). When do next‐of‐kin opt‐in? Anticipated regret, affective attitudes and donating deceased family member's organs. Journal of Health Psychology, 19(12), 1508–1517. 10.1177/1359105313493814 [DOI] [PubMed] [Google Scholar]
- Strack, F. , & Deutsch, R. (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8(3), 220–247. 10.1207/s15327957pspr0803_1 [DOI] [PubMed] [Google Scholar]
- Sukalla, F. , Wagner, A. J. , & Rackow, I. (2017). Dispelling fears and myths of organ donation: How narratives that include information reduce ambivalence and reactance. International Journal of Communication, 11, 5027–5047. http://ijoc.org/index.php/ijoc/article/view/6662/2210 [Google Scholar]
- Weber, K. , Martin, M. M. , & Corrigan, M. (2006). Creating persuasive messages advocating organ donation. Communication Quarterly, 54(1), 67–87. 10.1080/01463370500270413 [DOI] [Google Scholar]
- Welsh Government (2012). Public attitudes to organ donation: Baseline survey Cardiff, UK: Welsh Government; Retrieved from https://gov.wales/docs/caecd/research/121019organdonationen.pdf. [Google Scholar]
- Welsh Government (2016). Human Transplantation (Wales) Act 2013: Report laid before the National Assembly for Wales under Section 2.(3). Welsh Government. Retrieved from http://www.assembly.wales/laid%20documents/gen-ld9964%20-%20human%20transplantation%20(wales)%20act%202013%20report%20laid%20before%20the%20national%20assembly%20for%20wales/gen-ld9964-e.pdf.
- Young, V. , McHugh, S. , Glendinning, R. , & Carr‐Hill, R. (2017). Evaluation of the Human Transplantation (Wales) Act: Impact evaluation report. Retrieved from https://gov.wales/docs/caecd/research/2017/171130-evaluation-human-transplantation-wales-act-impact-en.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Information presented to participants regarding proposed changes to organ donor laws.
Appendix S2. Myths and counterevidence used in the myth‐correcting intervention.


