Abstract
The purpose of this study is to investigate clinical and radiographic differences between longitudinal capsulorrhaphy and inverted L-type capsulorrhaphy in patients diagnosed with hallux valgus (HV) to whom distal chevron osteotomy and HV distal soft-tissue procedure combination surgery was implemented.
A total of 36 patients and 48 feet on whom distal chevron osteotomy and HV distal soft-tissue procedure combination surgery was implemented upon diagnosis of HV were included in the study. The patients were separated into 2 groups according to capsulorrhaphy technique, as group 1 (24 feet) wherein longitudinal capsulorrhaphy was implemented and group 2 (24 feet) wherein inverted-L type capsulorrhaphy was implemented. Both groups were compared preoperatively and postoperatively in terms of American Orthopedic Foot and Ankle Society HV score, visual analogue scale (VAS) pain score, HV angle (HVA), intermetatarsal angle and complications.
Comparing the radiological data of both groups, the decrease in terms of HVA was significant in Group 2; however, no significant difference was detected in terms of other data. Postoperative hallux varus was observed 1 one patient in Group 2; however, this case was not statistically significant.
In the distal chevron osteotomy and distal soft-tissue procedure combination, applied as a HV correction surgery technique, comparing inverted L-type capsulorrhaphy with longitudinal capsulorrhaphy techniques, it was observed that inverted L-type capsulorrhaphy was more effective in correcting the HVA. However, it should be kept in mind that L-type capsulorrhaphy is also the technique wherein hallux varus complication occurred. As a result, the conclusion was reached that both techniques are applicable and effective in HV correction surgery and the choice should be made by considering the command of the surgeon on the technique.
Keywords: capsulorrhaphy, chevron osteotomy, hallux valgus
1. Introduction
HV is the most frequently observed deformity of the 1st metatarsophalangeal (MTF) joint and is more frequent in women. As the severity of HV deformity increased, quality of life was reported to deteriorate independently of sex.[1] Pain, difficulty in wearing shoes, and decrease in functional capacity are among the most frequent complaints.[2–4] In the event of such complaints, the deformity requires surgical treatment.
Radiological evaluation of HV is performed with standing anteroposterior (AP) and lateral radiographs. Angles of HV angle, intermetatarsal angle (IMA), sesamoid bone displacement and joint adherence are useful to explain the severity of the disease. HV frequency in patients diagnosed with HV was observed to increase with the age of these angles.[1,5] The deformity changes plantar muscle and fascia thickness according to the normal foot by changing the loading points on the foot, which affects the symptoms. In Lopez foot ultrasonography study, it was proved that the cross-sectional thickness of the muscles of ABH and FHB decreased and the thickness of the anterior, middle, and posterior plantar fascia increased compared to the normal foot structure.[5,6]
More than 100 different techniques were defined as HV correction treatment.[7,8] The main purpose of these surgeries is to reduce the pain in the toe and correct the deformity. Results of the combination of bone procedures and distal soft-tissue procedures are better compared to other surgical techniques and it is widely used in painful HV surgical treatment.[7–13]
The purpose of the bone procedure is to correct the IMA, whereas the purpose of the distal soft-tissue procedure is to correct the HV angle and ensure sesamoid reduction.[7] With the distal soft-tissue procedure, lateral deforming forces are reduced by loosening contracted lateral structures and 1st MTF joint reduction is achieved. In 1923, Silver[13] defined the soft-tissue procedure technique where medial eminensia is resected, lateral capsule and adductor tendon are loosened, and adductor hallucis is transposed together with medial capsular plication. Various modifications of this technique were published in the literature in subsequent years.[9,10,12,14] There are many surgical techniques in the literature described in relation to medial capsular plication. Two of these techniques are opening the capsule as inverted-L flap and resecting the capsule excess to shift the flap to the proximal phalanges proximal and suturing and opening the capsule longitudinally to resect the elongated capsule to plicate the capsule.
The purpose of this study is to compare the clinical and radiological differences in these 2 capsular plication techniques in HV-diagnosed patients on whom distal metatarsal osteotomy (Chevron osteotomy) and distal soft-tissue procedure were implemented.
2. Materials and methods
For this research, the ethics committee of the Faculty of Medicine of SANKO University was approved by decision dated February 7, 2019 and January 2019 number 05 and worked in accordance with the Helsinki Declaration Rules. All patients participating in the study were informed about the study and their written consent was obtained.
A total of 36 patients (48 feet) on whom chevron osteotomy and distal soft tissue procedure were implemented with HV diagnosis at the Orthopaedia and Traumatology Clinic of the Faculty of Medicine of the Sanko University between June 2013 and April 2016 were included in the study. Patients who underwent osteotomy other than distal chevron osteotomy (Akin osteotomy, distal phalangs osteotomy, Mitchell osteotomy) were not included in the study. The patients were operated by the same surgeon and capsule closing technique selection was implemented consecutively. The patients were separated into 2 groups according to the implemented capsule closing technique. The group where longitudinal capsulorrhaphy was implemented (group 1) for 24 feet and the group where inverted L-type capsulorrhaphy was implemented (group 2) for 24 feet, the mean HV angle (HVA) was 32.43 ± 6.36 (21–42) and 31.08 ± 9.52 (21–52) degrees and the mean IMA was 14.61 ± 2.25 (10–18) and 13.68 ± 3.50 (10–22) degrees respectively. The HVA was not <20 (21–52) degrees in any of the patients.
Mean patient age was 45.06 ± 17.03 and mean follow-up period was 24 months.
2.1. Radiological evaluation
The HV and IMA were measured preoperatively and in the last visit through AP straight graphs of the load-bearing foot. 1st and 2nd metatarsus long axis were used in preoperative HVA and IMA measurements. Postoperative HVA and IMA measurements were performed as described by Shima et al using the correction line between the center of the distal metatarsus on which osteotomy was performed and the center of the metatarsus base, as the long axis.[15] The measurements were performed 2 times by 2 different orthopedic surgeons and the average of the 4 measurements were used for statistical evaluation. On the load-bearing foot, modified Agrawal et al's method[16] on AP straight graphs and lateral sesamoid sublocation according to the lateral cortical border of the first metatarsus head, were rated from 0 to 3 preoperatively, postoperatively, on the 3rd month and at the last visit.
2.2. Clinical assessment
American Orthopedic Foot and Ankle Society (AOFAS) HV score and VAS pain score were recorded preoperatively and at the last visit. Less than 40 degrees of dorsiflexion of the 1st MTP joint and <20 degrees of plantar flexion range of motion (ROM) restriction was defined as movement restriction. The patients were postoperatively assessed in terms of presence of avascular necrosis (AVN), nonunion, hallux varus deformity, and infection.
3. Surgical technique
Spinal anesthesia was implemented in all patients. The concerned foot was prepared for surgery. Entry was made through dorsomedial incision through the 1st MTP joint and the lateral dorsal cutaneous nerve was protected, the bunion and capsule were reached. The bunion was excised and the capsule was opened as longitudinally (Fig. 1) or as inverted L-flap (Fig. 2). The medial eminence was excised. Then, through a separate incision, a dorsal incision was opened between the 1st and 2nd metatarsus and progress was made through blunt dissection and the adductor hallucis tendon was cut and separated from the lateral sesamoid. Metatarsosesamoid ligament was freed. The lateral capsule was fully loosened. The medial was again passed and a 60-degree modified chevron osteotomy was performed per metatarsus. The osteotomy was performed 12 mm distal to the metatarsophalangeal joint (Fig. 3). The distal fragment was laterally translated by 4 to 5 mm (Fig. 4). The osteotomy line was fixed with a stud cannulated single screw in all patients (Fig. 5). In cases where longitudinal opening was made when the finger was in the corrected position, capsule plication was performed and tightly closed; however, in cases wherein inverted L-flap capsule opening was made, the excess flap was resected and the tip was sutured to the capsule piece at the distal of the 1st Proximal phalanges. Then the sutures supporting the soft-tissue surrounding the capsule anterior and posterior, were removed. Excess skin was excised and both incisions were closed. Preoperative and postoperative AP radiographs for group 1 and group 2 are shown below (Figs. 6–9).
Figure 1.
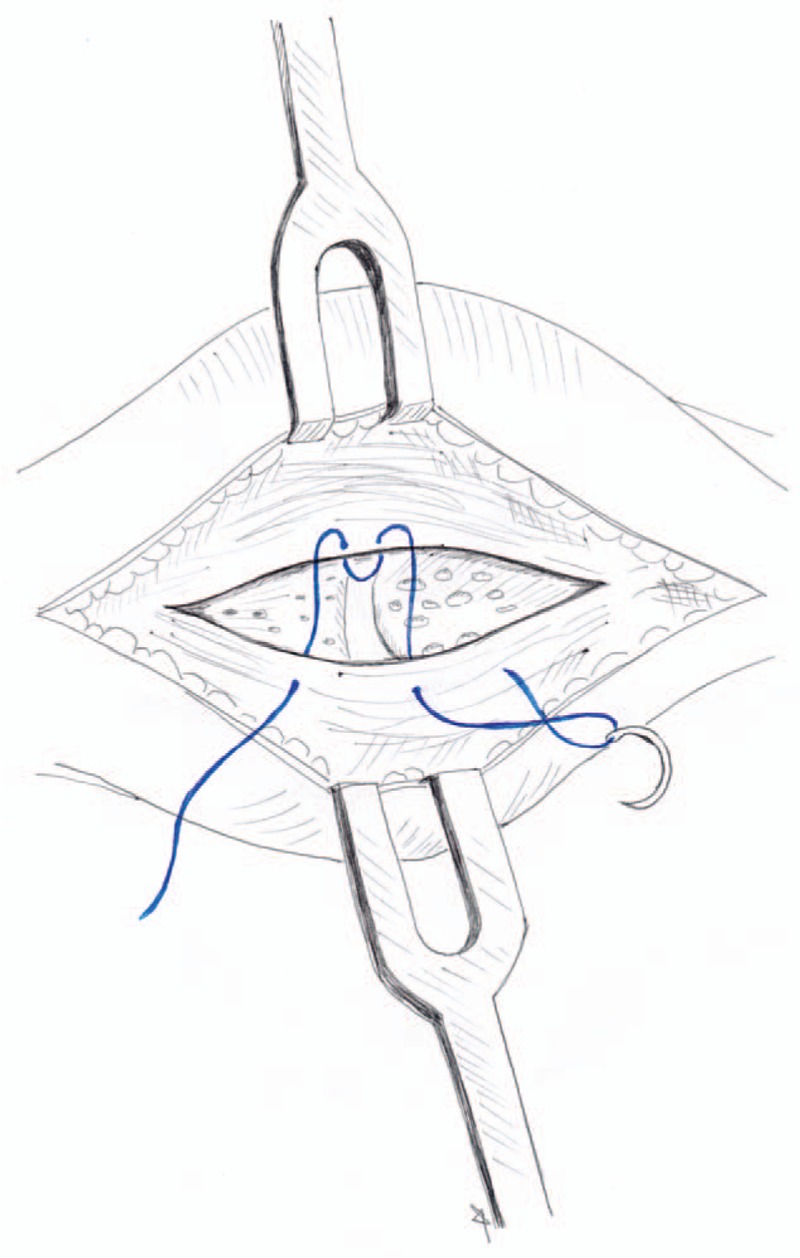
Longitidunal type capsule opening.
Figure 2.
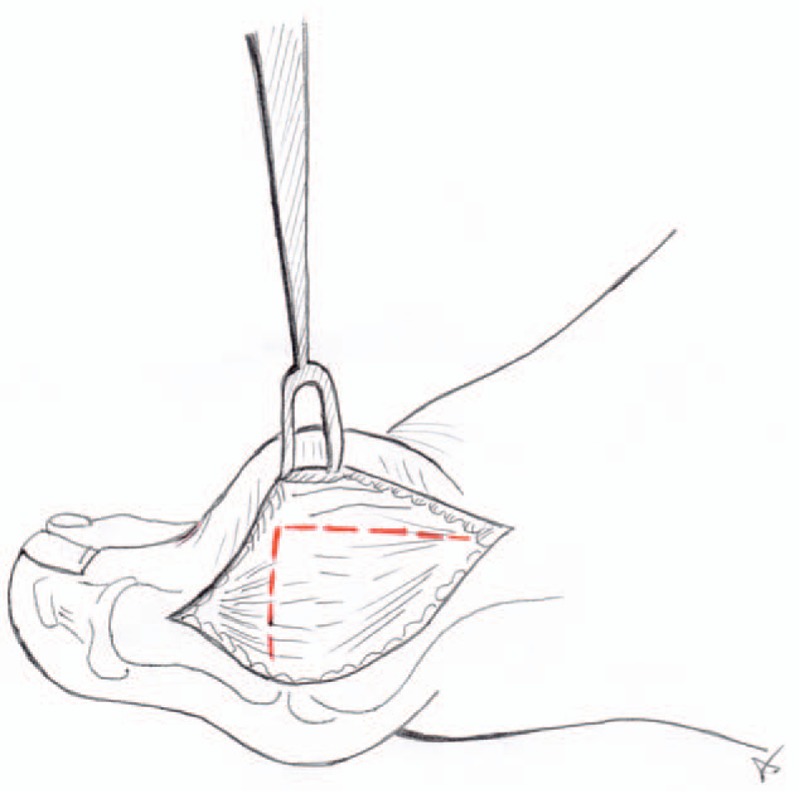
Inverte L type capsule opening.
Figure 3.

Localization of chevron osteotomy.
Figure 4.
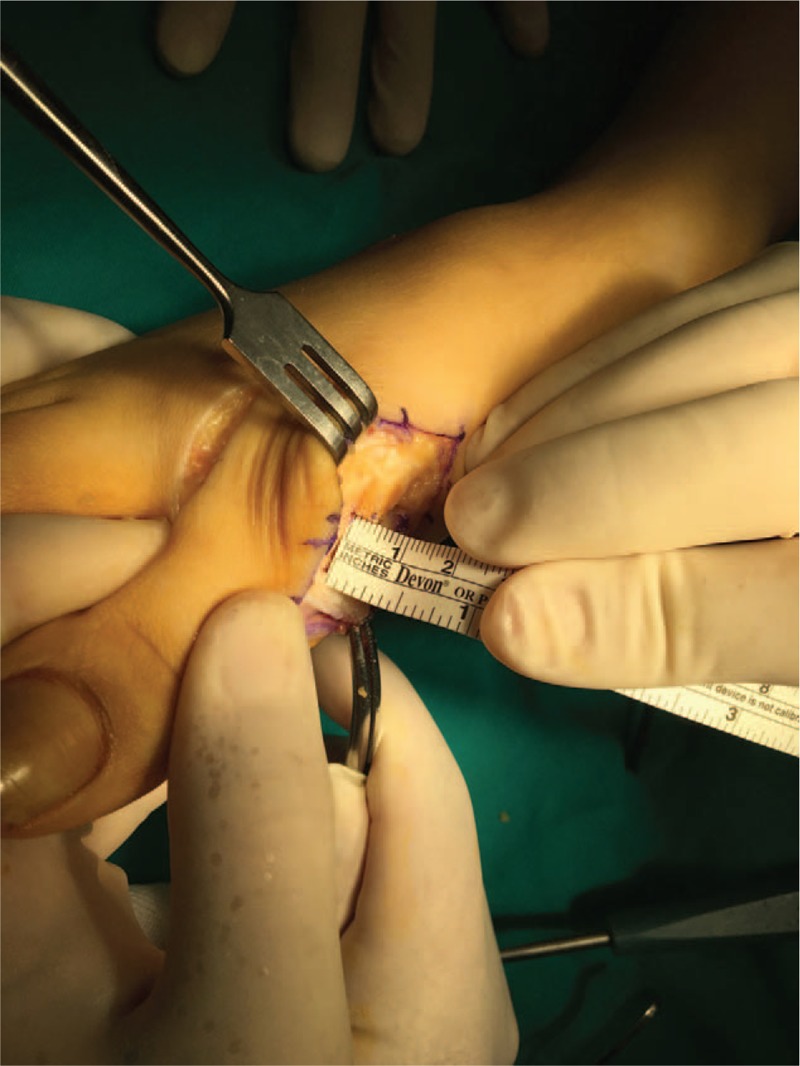
Lateralization amount of distal fragment.
Figure 5.

View of fixed Chevron osteotomy.
Figure 6.

Left foot preoperative x-ray.
Figure 9.

Right foot postoperative x-ray.
Figure 7.

Left foot postoperative x-ray.
Figure 8.

Right foot preoperative x-ray.
4. Postoperative care
Two-centimeter-thick gauze was placed between the 1st and 2nd toes. This gauze was replaced with inter-toe silicon roll when the sutures were removed on the 15th day and used for 6 weeks. The patient was postoperatively mobilized on the first day by stepping on heel. Carrying full load was permitted at the end of the 3rd week and ROM movements were permitted after week 2.
5. Statistical analysis
As the age, HVA, and IMA variables between both groups showed normal distribution, significance test (independent groups t test) was used to compare the difference between the 2 means; and as VAS pain score and AOFAS scores did not have normal distribution, they were compared with the Mann-Whitney U test. Inter-group sesamoid rotation degrees were evaluated with the χ2 test. P < .05 was accepted as statistically significant.
6. Result
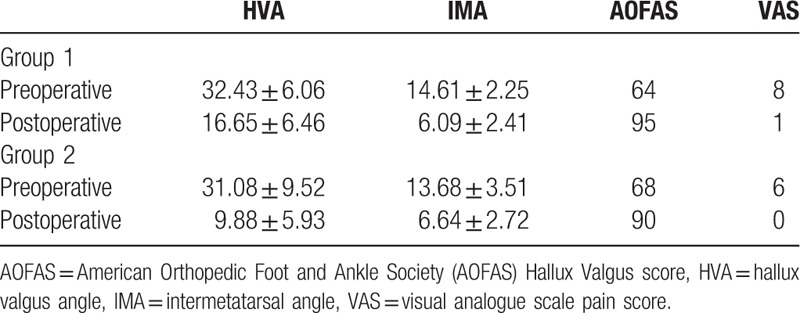
Postoperative HVA and IMA improved in both groups. In Group 1, HVA improved from 32.43 ± 6.06 degrees (between 21 and 42 degrees) to 16.65 ± 6.46 degrees (between 7 and 23 degrees P < .001) and IMA improved from 14.61 ± 2.25 degrees (between 10 and 18 degrees) to 6.09 ± 2.41 degrees (between 3 and 10 degrees P < .001). In Group, 2 HVA improved from 31.08 ± 9.52 degrees (between 21 and 52 degrees) to 9.88 ± 5.93 degrees (between 3 and 25 degrees) and IMA improved from 13.68 ± 3.51 degrees (between 10 and 22 degrees) to 6.64 ± 2.72 degrees (between 3 and 9 degrees P = .001). Comparing the degree of HVA improvement for both groups, a statistically significant difference was observed to the advantage of group 2, the HVA mean improvement percentage difference was 47.80 ± 19.40 in Group 1 and 67.42 ± 18.5 in Group 2 (P = .001). Postoperative improvement was achieved in both groups in terms of AOFAS and VAS pain score. In Group 1, AOFAS and VAS pain score improved respectively from 64 (between 45 and 84) to 95 (between 53 and 100) and from 8 (between 0 and 10) to 1 (between 0 and 9) (P < .001), and in Group 2 from 68 (between 42 and 87) to 90 (between 46 and 100) and from 6 (between 0 and 10) to 0 (between 0 and 6) (P < .001). Evaluating in terms of AOFAS and VAS pain score, no statistically significant difference was found between the 2 groups (Table 1).
Table 1.
Comparision of radiological and clinical differences between groups.
Comparing the mean degree of lateral sesamoid position postoperatively on the 3rd month and at the last visit, no statistically significant difference was found. In Group 1, lateral sesamoid position was 3 (between 2 and 4) in the preoperative evaluation and was 1 (between 0 and 3; P = .0001) at the postoperative 3rd month and 1 (between 1 and 2; P = .0001) at the last visit. In Group 2, lateral sesamoid position was 2 (between 1 and 4) in the preoperative evaluation and was 1 (between 0 and 3; P = .0001) at the postoperative 3rd month and 1 (between 1 and 2; P = .0001) at the last visit. In terms of sesamoid sublocation, there was no statistically significant between the 2 groups at the postoperative 3rd month and the last visit.
Movement restriction in dorsiflexion and plantar flexion was postoperatively observed in 1 case in both group 1 and group 2, whereas movement restriction in plantar flexion was observed in 2 groups and dorsiflexion restriction was not observed in both groups.
Hallux varus was postoperatively observed in one case in group 2 and was not observed in group 1. There was no movement restriction in the case with the hallux varus complication, but corrective surgery was implemented because of difficulty in wearing shoes. Lateral cutaneous nerve damage, AVN, nonunion, malunion, or infection complications was not detected in any of the cases.
7. Discussion
Symptoms of the HV disease require correction using surgical methods when they reduce the quality of daily life and the pain symptom stands out. More than 100 different techniques have been defined for this surgery. In their study, Park et al[17] achieved successful results in moderate and severe HV cases with chevron osteotomy and distal soft-tissue procedure combination surgery. Chevron osteotomy and distal soft-tissue procedure combination was also implemented in our study.
Silver is the person who pioneered lateral capsule and adductor tendon loosening medial exostectomy and medial capsulorrhaphy in HV surgery.[13] The main purpose of this surgical technique is to loosen contracted lateral joint structures (adductor hallusis, lateral joint capsule, transverse metatarsal ligament) and plicate the medial capsule to ensure alignment between proximal phalanx metatarsus. Capsulorrhaphy is an important part of this procedure. Many techniques have been defined in the literature for capsulorrhaphy. Longitudinal and inverted L-type capsulorrhaphy are the most frequently used ones.[18] After lateral contracted structures are loosened, in the inverted L-type capsulorrhaphy technique, the capsule is sutured to the joint capsule at the proximal of the proximal phalanges, while in the longitudinal capsulorrhaphy technique, plication is performed after excess capsule is removed.
There are insufficient studies in the literature on the clinical and radiological effects of the capsulorrhaphy technique as a result of HV surgery. There are cadaver studies concerning the movement restriction of capsulorrhaphy techniques on the 1st MTF joint[19,20]; however, there are no studies in the literature on the comparison of the clinical and radiological results of different techniques. In the cadaver study conducted by Hua et al, the inverted L-type capsulorrhaphy technique and the Y-type capsulorrhaphy technique were compared and it was observed that the L-type capsulorrhaphy technique caused significantly higher 1st MTF joint movement restriction. Researchers asserted that this situation was caused by the sutures stretching the capsule.[19] The fact that this study was a cadaver study and the fact that the cadavers on which capsulorrhaphy was implemented had no HV deformity were the weaknesses of the study. In our study, movement restriction in dorsiflexion and plantar flexion was observed in 1 case in both group 1 and group 2, whereas movement restriction in plantar flexion was observed in 2 groups and dorsiflexion restriction was not observed in both groups and no statistically significant difference was observed between both capsulorrhaphy techniques in terms of impact on 1st MTF joint movement.
The purpose of this study is to compare the clinical and radiological differences of 2 different capsulorrhaphy techniques on patients diagnosed with HV, on whom the same surgical procedures were implemented by the same surgeon. As a result, it was statistically shown that the inverted L-type capsulorrhaphy technique was more effective compared to the longitudinal capsulorrhaphy technique in correcting HVA. Considering that the single hallux varus complication occurred with the L-type capsulorrhaphy technique, it was considered that more care should be taken during the 1st MTF joint correction and over-correction should be avoided. Although more effective improvement in HVA was observed in with the inverted L-type capsulorrhaphy technique in the radiological comparison, acceptable improvement was achieved also with the longitudinal capsulorrhaphy technique. As a conclusion, it is considered that both capsulorrhaphy techniques are effective in HV surgery and that the choice should be made in accordance with the experience of the surgeon and that however, if the inverted L-type capsulorrhaphy technique is to be implemented, care should be taken in terms of hallux varus complication and overcorrection should be avoided during surgery.
Author contributions
Conceptualization: Gökhan Bülent Sever.
Data curation: Gökhan Bülent Sever, Faruk Aykanat, Cenk Cankuş.
Formal analysis: Gökhan Bülent Sever.
Funding acquisition: Gökhan Bülent Sever.
Investigation: Gökhan Bülent Sever.
Methodology: Gökhan Bülent Sever, Cenk Cankuş.
Project administration: Gökhan Bülent Sever.
Resources: Gökhan Bülent Sever.
Software: Gökhan Bülent Sever.
Supervision: Gökhan Bülent Sever.
Validation: Gökhan Bülent Sever.
Visualization: Gökhan Bülent Sever.
Writing – original draft: Gökhan Bülent Sever.
Writing – review & editing: Gökhan Bülent Sever.
Gökhan Bülent Sever orcid: 0000-0002-3096-5968.
Footnotes
Abbreviations: AOFAS = American Orthopedic Foot and Ankle Society Score, HV = hallux valgus, HVA = hallux valgus angle, IMA = intermetatarsal angle, MTF = metatarsofalangial, ROM = range of motion, VAS = visual analogue scale.
The authors report no conflicts of interest.
References
- [1].Lopez DL, Calejo Gonzalez L, Losa Iglesias ME, et al. Quality of life impact related to foot health in a sample of older people with hallux valgus. Aging Dis 2016;7:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mann RA, Coughlin MJ. Hallux valgus-etiology, anatomy, treatment and surgical considerations. Clin Orthop Relat Res 1981;31–41. [PubMed] [Google Scholar]
- [3].Kato T, Watanabe S. The etiology of hallux valgus in Japan. Clin Orthop Relat Res 1981;78–81. [PubMed] [Google Scholar]
- [4].Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in general population: a systematic review and meta-analysis. J Foot Ankle Res 2010;3:21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rodríguez-Sanz D, Tovaruela-Carrión N, López-López D, et al. Foot disorders in the elderly: a mini-review. Dis Mon 2018;64:64–91. [DOI] [PubMed] [Google Scholar]
- [6].Lobo CC, Marin AG, Sanz DR, et al. Ultrasound evaluation of intrinsic plantar muscles and fascia in hallux valgus. Medicine (Baltimore) 2016;95:5243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen YJ, Hsu RW, Shin HN, et al. Distal chevron osteotomy with intra-articular lateral soft tissue release for treatment of moderate to severe hallux valgus deformity. J Formos Med Assoc 1996;95:776–81. [PubMed] [Google Scholar]
- [8].Easley ME, Trnka HJ. Current concepts review: hallux valgus part 2: operative treatment. Foot Ankle Int 2007;28:748–58. [DOI] [PubMed] [Google Scholar]
- [9].Mann RA, Pfeffinger L. Hallux valgus repair. DuVries modified McBride procedure. Clin Orthop Relat Res 1991;272:213–8. [PubMed] [Google Scholar]
- [10].DuVries H. Surgery of the foot. Static deformities of the forefoot. 2nd ed 1965;St. Louis: The C.V. Mosby Company, 379–467. [Google Scholar]
- [11].Sammarco GJ, Conti SF. Proximal Chevron metatarsal osteotomy: single incision technique. Foot Ankle 1993;14:44–7. [DOI] [PubMed] [Google Scholar]
- [12].Johnson JE, Clanton TO, Baxter DE, et al. Comparison of Chevron osteotomy and modified McBride bunionectomy for correction of mild to moderate hallux valgus deformity. Foot Ankle 1991;12:61–8. [DOI] [PubMed] [Google Scholar]
- [13].Silver D. The operative treatment of halluks valgus. J Bone Joint Surg Am 1923;5-39:225–32. [Google Scholar]
- [14].Pfeffinger LL. The modified McBride procedure. Orthopaedics 1990;13:979–84. [DOI] [PubMed] [Google Scholar]
- [15].Shima H, Okuda R, Yasuda T, et al. Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am 2009;91:1369–76. [DOI] [PubMed] [Google Scholar]
- [16].Agrawal Y, Desai A, Mehta J. lateral sesamoid position in hallux valgus:correlation with the conventional radiological assessment. Foot Ankle Surg 2011;17:308–11. [DOI] [PubMed] [Google Scholar]
- [17].Park YB, Lee KB, Kim SK, et al. Comparison of distal soft tissue procedures combined with a distal chevron osteotomy for moderate to severe hallux valgus: first web space versus transarticular approach. J Bone Joint Surg Am 2013;95:e158. [DOI] [PubMed] [Google Scholar]
- [18].Disorders of the hallux, Soft tissue procedures, Campbell's Operative Orthopaedics, twelfth edition volume four p: 3809–18. [Google Scholar]
- [19].Xu C, LI M, Wang C, et al. Range of motion of the first metatarsophalangial joint after different capsulorrhaphies. J Am Podiatr Med Assoc 2017. [DOI] [PubMed] [Google Scholar]
- [20].Orozco-Villasenor SL, Monzo Planella M, Martin Oliva X, et al. Propuesta de una capsulorrafia como parte del tratamientoquirurgico del hallux valgus: estudio en cadaver. Acta Ortoipedica Mexicana 2017;3:118–22. [PubMed] [Google Scholar]


