Abstract
Triangular osteosynthesis involves unilateral L5 iliac posterior instrumentation combined with an iliosacral screw fixation. The aim of this study was to describe this procedure and report the preliminary clinical results in patients with unstable sacral fractures treated with minimally invasive triangular osteosynthesis (MITO). Between 2012 and 2017, 10 patients (6 men and 3 women, mean age, 50 ± 23 years) with sacral fractures were treated with MITO and were followed up for a mean of 15.0 ± 8.5 months in our institution. Classification of sacral fracture, operative time, intraoperative bleeding, timing of full weight bearing, bone union, complications, and clinical outcomes were investigated. Two cases were classified as Denis zone 1, 2 cases as zone 2, and 6 as zone 3. Four patients had Roy-Camille type 1 fracture and 2 patients had type 2. All patients underwent MITO, which involved bilateral lumbopelvic fixation and a uni/bilateral iliosacral screw with stab incisions for percutaneous fixation or central longitudinal incision. The operative time was a mean of 182 ± 64 minutes, and the amount of intraoperative bleeding was a mean of 63 ± 74 g. Full-weight bearing was initiated at a mean of 8.2 ± 2.4 weeks. Eight fractures healed; 1 patient had pulmonary embolism and 1 had implant loosening. Based on Majeed score, 8 patients had “excellent” clinical outcomes, 1 patient had a “good” clinical outcome, and the other had a “fair” clinical outcome. MITO could be less invasive on the soft tissues and be a reliable procedure for bony union. It might provide sufficient stability to accelerate the commencement of post-operative rehabilitation, even in patients with highly unstable sacral fractures.
Keywords: lumbopelvic fixation, minimally invasive surgery, sacral fracture, triangular osteosynthesis
1. Introduction
The sacrum connects the spine and lower limbs and plays an important role in maintaining sagittal balance of the spine. The sacrum is predisposed to fracture from high-energy trauma because of its biomechanical characteristics. Unstable sacral fracture is associated with high mortality and morbidity, if it is not treated appropriately.[1–3] The goal of internal fixation is to reconstruct the fracture anatomy and achieve sufficient stability for early mobilization. It can be treated with various types of fixation (e.g., iliosacral screws, transiliac plates, transiliac rod fixation, and lumbopelvic fixation).[4–7] Although lumbopelvic fixation can achieve abundant rigidity even in multiplanar sacral fractures, it is problematic as it is a relatively invasive procedure associated with wound healing disturbance rates as high as 26%.[8,9]
Triangular osteosynthesis is a unilateral lumbopelvic instrumentation combined with a horizontal fixation using iliosacral screws or a trans-iliac plate first described by Shildhauer et al,[10] which has been reported to have enough rigidity to enable early weight bearing.[11,12] We have developed a minimally invasive technique for triangular osteosynthesis using percutaneous spinal access devices and cannulated cancellous screws.
The aim of this study was to describe the clinical results of patients with unstable sacral fractures treated with minimally invasive triangular osteosynthesis (MITO).
2. Materials and methods
2.1. Study design and patients
This study was a retrospective case review based on the database in our institution. From 2012 to 2018, 10 patients with highly unstable sacral fractures treated with MITO, who were followed up for more than 6 months, were identified as eligible for the study. Vertically displaced (AO/OTA classification type C) or multiplanar (U or H shaped) sacral fractures were defined as “highly unstable” in this study. Patients with rotational instability, which did not have vertical displacement, were not indicated for MITO. Six men and four women had been treated with MITO. The follow-up was a mean of 15.0 ± 8.5 months, and the age of patients was a mean of 50 ± 23 years.
2.2. Operative technique
Patients with vertically unstable pelvic ring fractures were initially treated with external fixation. After insertion of Schantz pins via the low route under fluoroscopic imaging, closed reduction, as described by Schweizer et al,[13] was applied with axial traction of the affected lower extremity and with manipulation through the pins. Subsequently, external fixators were connected and fastened to maintain the achieved reduction. Post-operative CT scans were essential to confirm the quality of closed reduction and to design a plan for insertion of iliosacral screws, and spinal instrumentation.
Patients underwent definitive fixations when they became hemodynamically stable enough for surgery. Initially, iliosacral screw fixation, using 6.5 mm diameter titanium cannulated cancellous screw (MEIRA Inc, Nagoya, Japan), was performed under fluoroscopic imaging with or without navigation in a supine position, depending on the morphology and displacement of the sacrum. Iliosacral screw fixation was usually applied to the ipsilateral side of the sacrum. In cases of bilateral or transverse sacral fractures, fixation was performed bilaterally or using a trans-sacral screw method. If fractured, pubic rami were also stabilized with retrograde intra-medullary screws, using 6.5 or 5.5 mm cannulated cancellous screws. External fixators were removed at this time. In case of bilateral displaced fractures of the pubic rami, anterior subcutaneous internal fixation was an option for anterior pelvic fixation.
Thereafter, patients were placed in a prone position. Before sterilization, it was essential to confirm configuration of the L5 pedicles and obtain an iliac teardrop view under fluoroscopic imaging. Each incision was 3 cm long, and they were placed bilaterally 1 cm to 1.5 cm lateral to the lateral edge of the L5 pedicles and 2 cm medial to the posterior superior iliac spine (Fig. 1). L5 pedicle screws were inserted bilaterally with the device dedicated for percutaneous pedicle screw fixation (Medtronic Inc., LONGITUDE II, Memphis, TN) under fluoroscopic guidance. If an L5 pedicle was damaged and not suitable for screw insertion, an L4 pedicle was chosen as an alternative. The posterior superior iliac spine was exposed subperiosteally. The surgeon determined the insertion point for an iliac screw at just above and ventral to the PSIS. We did not resect the bone around the insertion point of the iliac screw. Instead, the insertion point was set ventral to the overhang of the posterior superior iliac spine to avoid irritating the skin, and this technique is similar to low profile S1 iliac trajectory.[14] The insertion point was usually within the outline of the iliac teardrop. The angle of an image intensifier was adjusted so that the insertion point was located at the center of the iliac teardrop contour. A surgeon hit in a guide wire with a hammer under fluoroscopic imaging, followed by tapping and insertion of the iliac screws (Medtronic Inc., CD Horizon Ballast, Memphis, TN) through a guide wire. Titanium rods 5.5 mm in diameter were inserted subfascially from the caudal to the cranial side, and connected rigidly with set-screws (Fig. 2).
Figure 1.
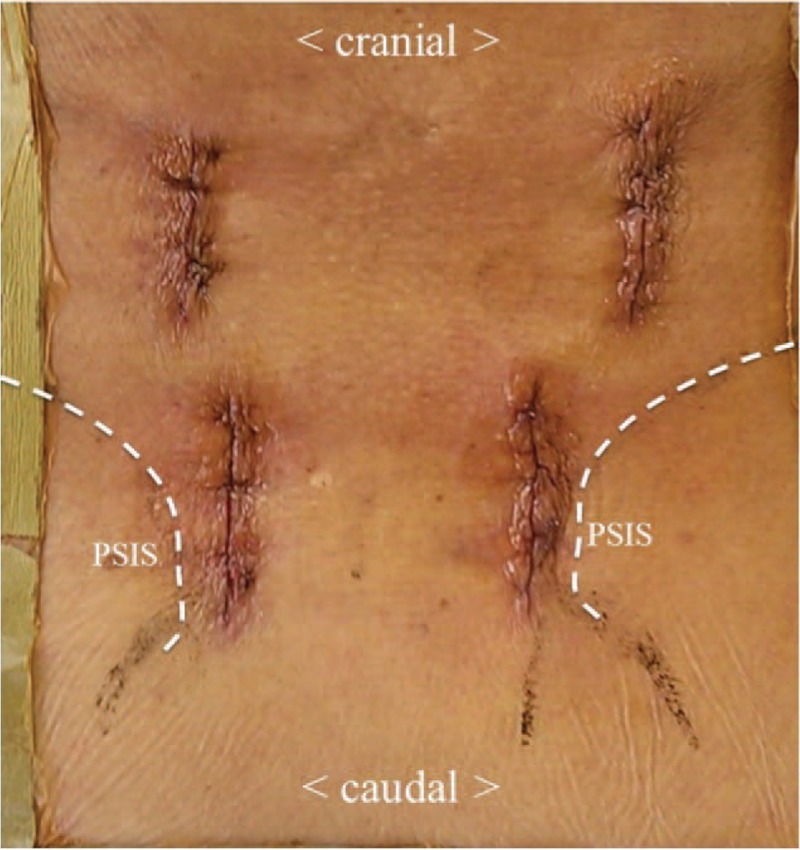
Skin incision. Each incision was 3 cm long, and they were placed bilaterally 1 cm to 1.5 cm lateral to the lateral edge of the L5 pedicles and 2 cm medial to the posterior superior iliac spine (PSIS).
Figure 2.
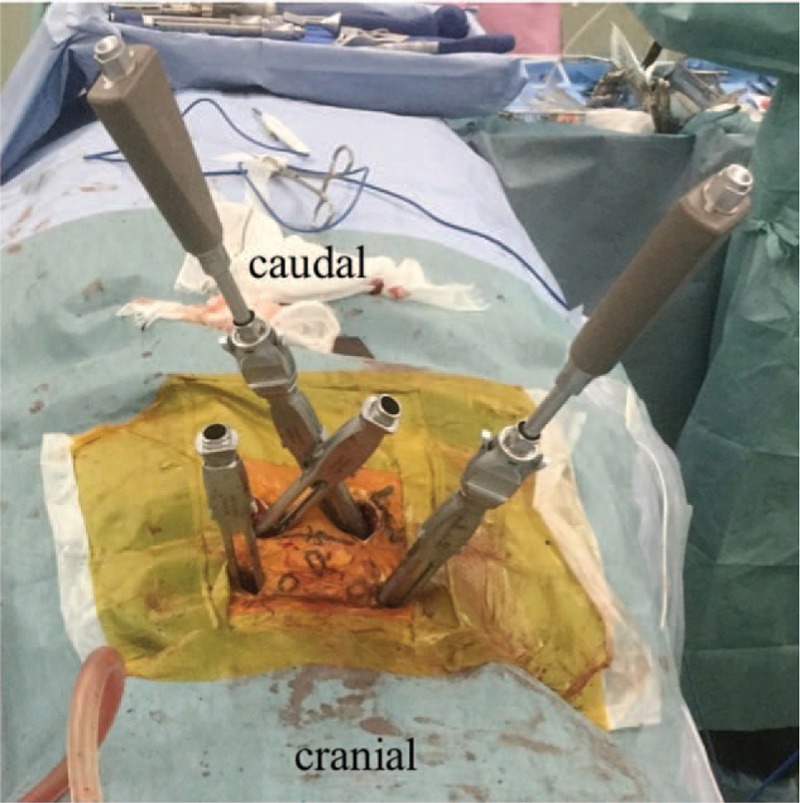
Intra-operative pictures showing percutaneous L5 pedicle and ilia screw fixation.
If a closed reduction was unsuccessful at the time of initial external fixation, iliosacral fixation was not performed with the patient in a supine position. Surgery began with the patient in a prone position. After sterilization, a 10 cm long central longitudinal incision was made. The supra-fascial layer was opened, and reduction was performed through traction of a lower extremity and manipulation with Schantz screws placed on the iliac wing and clumps. Iliosacral screw fixation was performed while maintaining reduction of the sacrum, and lumbopelvic instrumentation followed to reinforce the fixation. If decompression of the sacral spinal canal was required, it was performed after thorough MITO; however, in this case series, no patients required decompression surgery.
2.3. Post-operative management
Patients were allowed to ambulate with wheelchairs on the first post-operative day. Physical exercises that focused on strength training of the pelvis, trunk, and lower extremities were started at this point. Usually partial weight bearing was initiated 4 weeks post-surgery, and full weight bearing was permitted 8 weeks post-surgery.
Implants were removed after bony union usually between 6 months and a year post-surgery, unless patients refused due to age or preference. Implant removal surgeries were accomplished through initial incisions under general anesthesia.
2.4. Evaluations
We investigated the following parameters: mechanism of injury, classification of the sacral fracture (Denis's classification for longitudinal fractures), Roy-Camilles classification for transverse sacral fractures, initial treatment at time of injury, time from injury to definitive surgeries, fixation method, type of incision, addition of anterior fixation, operative time, amount of bleeding, timing of partial and full weight bearing, bone union, complications, nerve injury assessed by Gibbons classification,[15] removal of implants, and clinical outcomes (evaluated by Majeed score).
2.5. Statistical analysis
Data were analyzed using SPSS 17.0 (IBM, Armonk, NY). Data are presented as mean ± standard deviation (SD) or actual number.
3. Results
Four cases sustained injury after falling from height, 3 after traffic accidents, and 3 after crush incidents. Based on AO/OTA classification, the patients group contained 5 cases of C1, 3 cases of C2. Remaining 3 patients had U-shaped fractures, which were hard to be classified into AO/OTA fracture types. There were 2 cases of Denis zone 1, 2 cases of zone 2, and 6 case of zone 3. All sacral fractures with a transverse fracture line were classified as zone 3. Of the 6 patients with transverse fractures, 4 had Roy-Camille type 1 fracture, and 2 had type 2. Six patients underwent initial external fixation. One patient had been stabilized with a pelvic binder. All patients underwent MITO: bilateral lumbopelvic fixation and iliosacral screw fixation and they underwent definitive surgeries a mean of 8 ± 4 days after injury. Six patients had stab incisions for percutaneous fixation, and 4 patients had central longitudinal incisions. Anterior fixation was performed in addition to MITO in 5 patients with displaced pubic rami fractures. Operative time was a mean of 182 ± 64 minutes, and the intraoperative bleeding amount was a mean of 63 ± 74 g. Partial weight bearing was initiated at a mean of 4.4 ± 1.6 weeks and full-weight bearing was permitted at a mean of 8.2 ± 2.4 weeks. All fractures were healed. There were 2 complications, including 1 asymptomatic pulmonary embolism and 1 loose pedicle screw after bone union. No patients had wound-related complications, infections, or implant failures requiring revision surgeries. Four patients had nerve injuries due to sacral fractures. The Gibbons classification was 3 in 2 patients, and 2 in 2 patients. Two patients with a Gibbons classification of 3 improved to 2, and 2 patients with a Gibbons classification of 2 maintained a score of 2 at final follow up. Only 4 patients had their implants removed between 6 months and a year after surgery, while we had offered all patients to remove implants. The other 6 patients did not wish to have their implants removed because they had experienced no irritation or discomfort from the implants, or because of their advanced age. Based on Majeed functional assessment system, 8 patients had an “excellent” clinical outcome, 1 patient had a “good” clinical outcome, and the final patient had a “fair” clinical outcome.
4. Case presentation
A 26-year-old man was injured after being crushed by a heavy board. On admission, the radiograph (Fig. 3 A) and the CT scan (Fig. 3 B) showed a crescent fracture on the right and a vertically-displaced sacral fracture on the left. Concomitant injuries were hepatic injury and rupture of the bladder. Following a massive transfusion, the patient was rushed to the operation theater. After insertion of half pins, closed reduction was performed through the pins and traction of the affected limb was performed (Fig. 3 C). A CT scan was taken subsequently for evaluation of initial reduction and planning of the definitive fixation (Fig. 3 D). Ten days after injury, definitive fixation was performed. The posterior pelvic ring was stabilized with MITO, and the anterior ring was fixed with subcutaneous internal fixation (Fig. 3 E). Post-operative CT images showed appropriate insertion of a trans-sacral screw (Fig. 3 F) and iliac screws, which were not bulging from the surface of the posterior superior iliac crests (Fig. 3 G). At 12 months post-injury, implants were removed and the patient had returned to his original occupation without any pain on motion (Fig. 3 H). His clinical outcome as assessed by Majeed evaluation was “excellent”.
Figure 3.
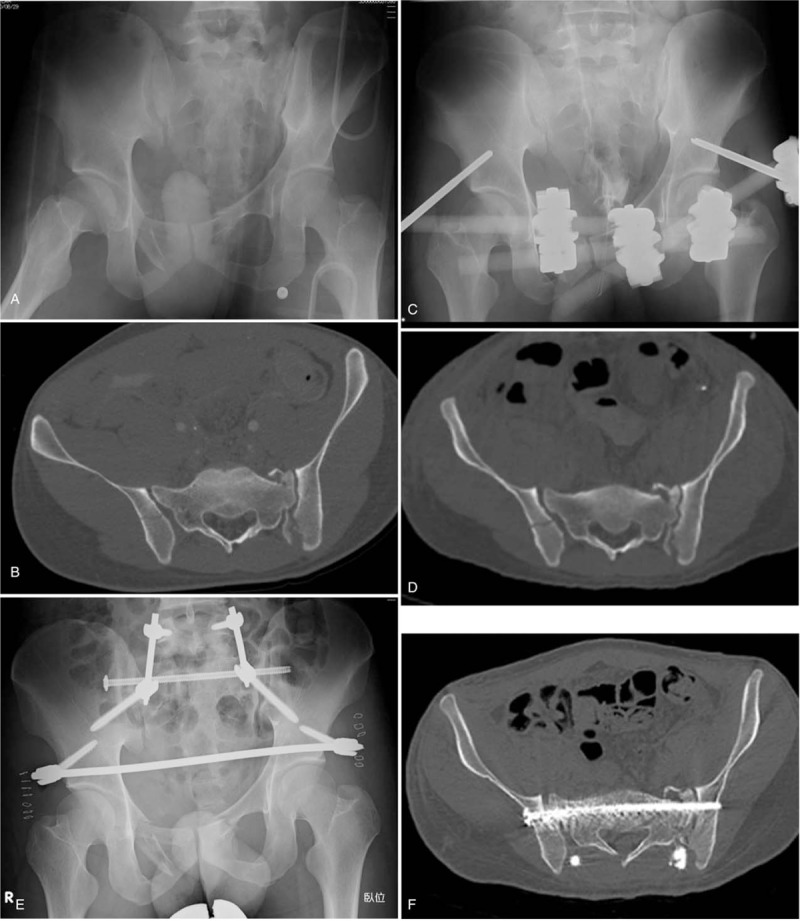
Male, 26-years-old, crush injury. A. Radiograph on admission showing a vertically displaced sacral fracture on left. B. Axial CT view of S1 on admission showing a crescent fracture on right. C. Radiograph taken after external fixation. D. Axial CT view of S1 after external fixation. The sacral fracture on the left side is reduced. E. Post-operative radiograph: posterior pelvic ring was stabilized by MITO, and anterior subcutaneous internal fixation was applied. F. Post-operative axial CT view of S1 showing appropriate insertion of a trans-sacral screw. G. Iliac screws are not bulging from the surface of posterior superior iliac crests. CT = computed tomography, MITO = minimally invasive triangular osteosynthesis. H. Radiograph at 12 months post-injury. Implants were removed.
Figure 3 (Continued).
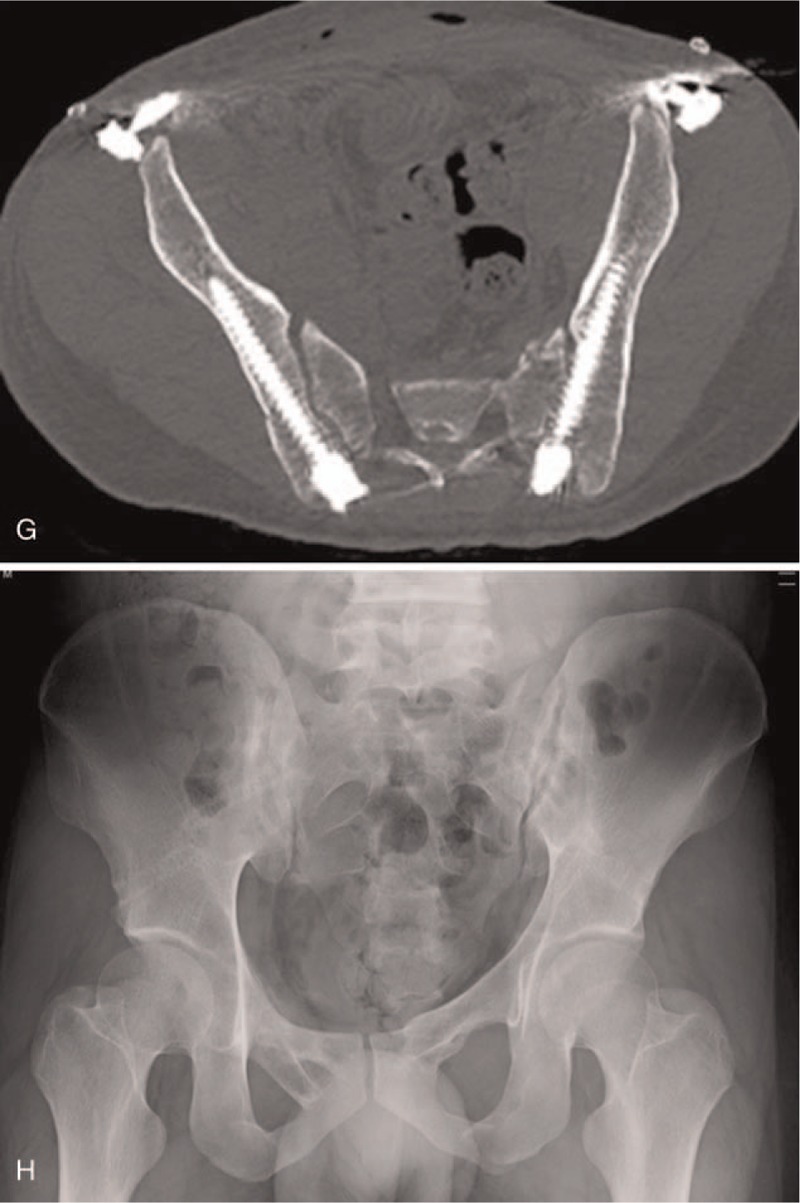
Male, 26-years-old, crush injury. A. Radiograph on admission showing a vertically displaced sacral fracture on left. B. Axial CT view of S1 on admission showing a crescent fracture on right. C. Radiograph taken after external fixation. D. Axial CT view of S1 after external fixation. The sacral fracture on the left side is reduced. E. Post-operative radiograph: posterior pelvic ring was stabilized by MITO, and anterior subcutaneous internal fixation was applied. F. Post-operative axial CT view of S1 showing appropriate insertion of a trans-sacral screw. G. Iliac screws are not bulging from the surface of posterior superior iliac crests. CT = computed tomography, MITO = minimally invasive triangular osteosynthesis. H. Radiograph at 12 months post-injury. Implants were removed.
5. Discussion
Lumbopelvic fixation for highly unstable fractures, even in case of multi-planar instabilities, has been reported to be a reliable method for fracture heeling.[7,8] Although the clinical importance of using additional iliosacral screws to short-segment lumbopelvic fixation remains unclear, there are several reports that support the efficacy of triangular osteosynthesis.[10,11,16–19] Sagi et al[16] reported the largest case series of triangular osteosynthesis with favorable clinical results. In that study, 6 out of 40 cases had asymmetric tilting of the L5 vertebral body with distraction of the L5/S1 facet joint, and 2 cases had implant failures. These problems may have stemmed from the unilateral nature of the original triangular osteosynthesis. A biomechanical study conducted by Toogood et al[17] suggested that the construct of an iliac screw connected to the contralateral S1 screw, which acted as a proxy for a L5 pedicle screw, had superior rotational stability than that of an iliac screw connected to an ipsilateral S1 screw. Mouhsine et al[18] reported a case series involving a modification of triangular osteosynthesis in which bilateral fixations from L4 to the ilium were connected with a transverse rod. We believe in the superiority of a bilateral construct in terms of stability of the fixation and prevention of complications resulting from a unilateral configuration.
MITO procedure is outstanding as it includes bilateral lumbopelvic fixation in addition to the iliosacral screw, and the procedure can be performed percutaneously all the way through. The original report on triangular osteosynthesis[10] described a distraction fixation technique performed between a lumbar pedicle screw and an iliac screw. We did not adopt this concept because we were concerned that it may generate excess stress on implants, and result in loosening of screws or even implant failures. As a result, we did not have any patients with tilting of the L5 vertebral body with distraction of the L5/S1 facet joint, nonunion, or implant failures before fracture healing, suggesting sufficient stability for active rehabilitation and bone union of the sacrum.
Lumbopelvic fixation, represented by the Galvestone technique, is a relatively invasive surgery. Wound-related complications and/or infection, resulting from the high invasiveness of the surgery and poor soft-tissue condition around the sacrum, are serious concerns for surgeons. Infection rates following lumbopelvic fixation have been reported to be 9% to 26%.[9,18] Although there are only a few reports about local infection rates following triangular osteosynthesis and its modifications, reports suggest rates of 6% to 14%,[16,18,19] which is a similar rate to that of ordinary lumbopelvic fixation. This infection rate is high and needs improvement. Percutaneous lumbopelvic fixation for sacral fractures could be a possible solution for this situation.[20–22] Williams et al[21] reported the results of a percutaneous technique of lumbopelvic stabilization for sacral fractures with spinopelvic dissociation patterns. In that study, 1 out of 17 patients experienced infection, and the patient was treated successfully without the need for implant removal. Koshimune et al[22] compared conventional open surgery with minimally invasive spinopelvic fixation for bilateral unstable sacral fractures. Infection occurred in 3 of 8 patients who underwent the conventional method, and in none of the 8 patients who underwent the minimally invasive method. They also reported that the minimally invasive procedure helped to shorten the operative time and reduce intra-operative bleeding. In our series, none of the ten patients had wound-related complications and infections. This may be explained by the fact that we did not detach the paraspinal muscles because reduction was accomplished anteriorly as a primary external fixation or posteriorly with clamps on the supra-fascial layer at the definite surgery. If decompression of the sacral spinal canal was required, minimal exposure of the paraspinal muscles can be addressed using a midline longitudinal incision. Regarding operative time and intra-operative bleeding, the results in our series were comparable to the previous reports of percutaneous lumbopelvic fixation,[21,22] despite the addition of an iliosacral screw to posterior lumbopelvic fixation.
Triangular osteosynthesis is advantageous for post-operative rehabilitation. Most authors who have advocated triangular osteosynthesis[10,16,18,19] allowed early weight bearing for patients after surgery to promote success. We kept patients from weight bearing for 4 weeks after surgery, and permitted full weight bearing 8 weeks after surgery. We deemed this interval of non-weight bearing to be beneficial for pain-free post-operative rehabilitation. Nonetheless, this restriction seems not to be the major reason for a favorable result in our case series, and might be unnecessary for patients who do not have severe post-operative pain. We would consider an earlier start to rehabilitation in the future.
In the original article of triangular osteosynthesis,[11] implant removal was performed in case of patients’ request. The other authors[16,18,19] advocated to remove implants routinely at a minimum of 6 months post-operatively, and we followed this protocol, because we believe implant removal would improve mobility of the sacroiliac joint and prevent adjacent segment diseases in lumbar spine.
Despite the insights provided by this study, there are some limitations to consider. These include its retrospective nature, small sample size, and a lack of control group. Regardless of these limitations, however, we believe that the present study provides some novel perspectives on clinical practice, suggesting that MITO could have advantages in being less invasive on the soft tissues and in gaining an abundant stability.
6. Conclusions
MITO could be less invasive on the soft tissues and be a reliable procedure for bony union. It might provide sufficient stability to allow acceleration of the commencement of post-operative rehabilitation, even in patients with highly unstable sacral fractures.
Author contributions
Conceptualization: Shozo Kanezaki, Masashi Miyazaki.
Data curation: Naoki Notani, Tomonori Sakamoto.
Investigation: Toshinubu Ishihara, Tomonori Sakamoto, Takashi Sone.
Methodology: Masashi Kataoka.
Supervision: Masashi Kataoka, Hiroshi Tsumura.
Writing – original draft: Shozo Kanezaki.
Writing – review & editing: Masashi Miyazaki.
Masashi Miyazaki orcid: 0000-0003-0001-5336.
Footnotes
Abbreviation: MITO = minimally invasive triangular osteosynthesis.
This study received approval from our institution's Ethical Committee. All procedures were performed in accordance with the ethical standards of this committee, as well as with the 1964 Helsinki Declaration and its later amendments.
Compliance with ethical standards
Shozo Kanezaki, Masashi Miyazaki, Naoki Notani, Toshinobu Ishihara, Tomonori Sakamoto, Takashi Sone, Masashi Kataoka, and Hiroshi Tsumura declare that they have no conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- [1].Latenser BA, Gentilello LM, Tarver AA, et al. Improved outcome with early fixation of skeletally unstable pelvic fractures. J Trauma 1991;31:28–31. [DOI] [PubMed] [Google Scholar]
- [2].Lykomitros VA, Papavasiliou KA, Alzeer ZM, et al. Management of traumatic sacral fractures: a retrospective case-series study and review of the literature. Injury 2010;41:266–72. [DOI] [PubMed] [Google Scholar]
- [3].Park YS, Baek SW, Kim HS, et al. Management of sacral fractures associated with spinal or pelvic ring injury. J Trauma Acute Care Surg 2012;73:239–42. [DOI] [PubMed] [Google Scholar]
- [4].Nork SE, Jones CB, Harding SP, et al. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 2001;15:238–46. [DOI] [PubMed] [Google Scholar]
- [5].Griffin DR, Starr AJ, Reinert CM, et al. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma 2003;17:399–405. [DOI] [PubMed] [Google Scholar]
- [6].Suzuki T, Hak DJ, Ziran BH, et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury 2009;40:405–9. [DOI] [PubMed] [Google Scholar]
- [7].Jones CB, Sietsema DL, Hoffmann MF. Can lumbopelvic fixation salvage unstable complex sacral fractures? Clin Orthop Relat Res 2012;470:2132–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tan GQ, He JL, Fu BS, et al. Lumbopelvic fixation for multiplanar sacral fractures with spinopelvic instability. Injury 2012;43:1318–25. [DOI] [PubMed] [Google Scholar]
- [9].Bellabarba C, Schildhauer TA, Vaccaro AR, et al. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976) 2006;31:S80–8. [DOI] [PubMed] [Google Scholar]
- [10].Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma 1998;12:307–14. [DOI] [PubMed] [Google Scholar]
- [11].Schildhauer TA, Ledoux WR, Chapman JR, et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma 2003;17:22–31. [DOI] [PubMed] [Google Scholar]
- [12].Min KS, Zamorano DP, Wahba GM, et al. Comparison of two-transsacral-screw fixation versus triangular osteosynthesis for transforaminal sacral fractures. Orthopedics 2014;37:e754–60. [DOI] [PubMed] [Google Scholar]
- [13].Schweitzer D, Zylberberg A, Cordova M, et al. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury 2008;39:869–74. [DOI] [PubMed] [Google Scholar]
- [14].Nakamichi K, Watanabe H, Kataoka T, et al. Lumbopelvic fixation by low profile S1-iliac trajectory (LSIT). J Spine Res 2013;4:1505–8. Japanese. [Google Scholar]
- [15].Gibbons KJ, Soloniuk DS, Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg 1990;72:889–93. [DOI] [PubMed] [Google Scholar]
- [16].Sagi HC, Militano U, Caron T, et al. A comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma 2009;23:313–9. [DOI] [PubMed] [Google Scholar]
- [17].Toogood P, McDonald E, Pekmezci M. A biomechanical comparison of ipsilateral and contralateral pedicle screw placement for modified triangular osteosynthesis in unstable pelvic fractures. J Orthop Trauma 2013;27:515–20. [DOI] [PubMed] [Google Scholar]
- [18].Mouhsine E, Wettstein M, Schizas C, et al. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J 2006;15:857–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hu X, Pei F, Wang G, et al. Application triangular osteosynthesis for vertical unstable sacral fractures. Eur Spine J 2013;22:503–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Martin CT, Witham TF, Kebaish KM. Sacropelvic fixation: two case reports of a new percutaneous technique. Spine (Phila Pa 1976) 2011;36:E618–21. [DOI] [PubMed] [Google Scholar]
- [21].Williams SK, Quinnan SM. Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns. J Orthop Trauma 2016;30:e318–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Koshimune K, Ito Y, Sugimoto Y, et al. Minimally invasive spinopelvic fixation for unstable bilateral sacral fractures. Clin Spine Surg 2016;29:124–7. [DOI] [PubMed] [Google Scholar]


