Abstract
Objective
With more teeth retained for longer in an ageing population, population‐wide periodontal treatment needs may increase. We assessed and projected periodontal treatment needs from 1997 to 2030 in Germany.
Methods
Partial‐mouth probing‐pocket depths (PPDs) from repeated waves (1997, 2005, 2014) of the nationally representative German Oral Health Studies were transformed into full‐mouth PPDs via decision‐tree‐based ensemble‐modelling. In line with German healthcare‐regulations, teeth with PPD ≥ 4 mm were regarded as needing periodontal treatment. Weighted means were interpolated cross‐sectionally by fitting spline‐curves and then regressed longitudinally 1997–2030.
Results
In 1997, younger adults (35–44 years old) had a mean of 7.4 teeth needing treatment (overall 93.8 million teeth); this decreased to 4.8 teeth (47.3 million teeth) in 2014. For 2030, we project 3.2 teeth (33.7 million teeth). In seniors, an increase was recorded (1997: 4.5 teeth, 33.5 million teeth; 2014: 7.5 teeth, 63.4 million teeth); this is expected to continue until 2030 (to 12.2 teeth, 140.8 million teeth). The cumulative number of teeth needing treatment increased from 2000 (355 million) to 2015 (365 million), and will increase further to 2030 (464 million).
Conclusions
Population‐wide periodontal treatment needs may increase until 2030, mainly in the elderly. Concepts for addressing, these growing needs are required.
Keywords: cross‐sectional study, demography, epidemiology, health services research, periodontitis
1. INTRODUCTION
Periodontal diseases, that is gingivitis and periodontitis, are among the most prevalent diseases of humankind, with severe periodontitis (defined as having probing‐pocket depths PPDs ≥ 6 mm) being the sixth most prevalent disease worldwide, affecting nearly 800 million individuals by 2016 (Kassebaum et al., 2017). Untreated periodontitis leads to tooth loss and, with it, masticatory, phonetic, aesthetic and social impairment; periodontitis is also associated with various co‐morbidities like diabetes (Tonetti, Jepsen, Jin, & Otomo‐Corgel, 2017). The direct and indirect costs of periodontitis are substantial (Righolt, Jevdjevic, Marcenes, & Listl, 2018).
In many high‐income countries, teeth are retained for longer given decreased rates of tooth loss in younger adults and seniors (Frencken et al., 2017). In parallel, populations are significantly ageing. In Germany, for example, todays’ 65‐year‐olds and older comprise 22% of the population (17.9 of 81.2 millions); in 2030, this number will be 28% (21.8 of 79.2 millions) and in 2040, even 31% (23.2 of 76.0 millions) (deStatis 2018). With more teeth retained in this growing age group, the absolute number of teeth at risk for periodontitis is increasing. Shifts in both morbidity and demography can be expected to significantly alter periodontal treatment needs. Assessing treatment needs on individual level (e.g., the mean number of teeth needing treatment in an individual) and combining these estimates with population data at different time points allows to capture both disease and population dynamics jointly. These integrated treatment needs data are relevant on multiple levels: (a) For allocating resources in both research and health services; (b) for guiding future dental education, (c) for assisting diagnostics, as knowledge on how often treatment needs are present in different age groups will improve diagnostic accuracy, (d) for dentists in developing a practice profile and business plan based on past, present and future needs for dental services.
In Germany and within the statutory insurance, which covers 89% of the population (Gesundheitsberichtserstattung 2018), treatment needs are assessed using probing‐pocket depths (PPDs) (KZBV 2017); such treatment needs should not be confused with periodontitis prevalence or extent (Holtfreter et al., 2015; Page & Eke, 2007). The German Oral Health Studies (Deutsche Mundgesundheitsstudien, DMS) are nationally representative, multi‐centre, cross‐sectional studies, conducted in 1997, 2005 and 2014, which assessed PPDs and hence can be used to assess how treatment needs have changed with time, and to also project treatment needs in the future. We aimed to assess and project periodontal treatment needs on both individual and population level from 1997 to 2030 in Germany.
2. MATERIAL AND METHODS
2.1. Data source and participants
Data from three waves of DMS were used; DMS III from 1997, DMS IV from 2005 and DMS V from 2014. DMS involve stratified multi‐stage cross‐sectional, nationwide probability samples of the civilian German population, with clinical and socio‐epidemiological examinations in different age cohorts (12 years old, 35–44 years old, 65–74 years old, and for DMS V also 75–100 years old). The sampling design, data collection protocols and data availability can be found elsewhere (Jordan & Micheelis, 2016; Micheelis & Reich, 1999; Micheelis & Schiffner, 2006).
Study participants were drawn from local residents’ registration offices in 90 randomly selected communities (sample points) using a cluster‐random sampling stratified for regions and areas of urbanization. A disproportional sample point selection was performed with 60 study sample points in the Western federal states of Germany and 30 study sample points in the Eastern states.
For the DMS III, 3,065 participants were included (response rate of 63.6%); for DMS IV and V, these numbers were 4,631 (63.1%) and 4,609 (50.1%), respectively. Empirical non‐responder analyses were conducted to compare the socio‐dental characteristics of responders with the target population according to gender, educational level, dental visiting patterns, and dental/prosthodontic status. Non‐response bias was found to be minimal (Supporting Information Appendix Table S1). The study was ethically approved, as were all data collection protocols. All participants completed written informed consent.
2.2. Periodontal examinations and treatment needs
The dental examinations and the socio‐scientific survey were carried out at the local sample points. To ensure reproducibility, interviewers and dental investigators were trained and calibrated by experts and multiple reliability checks were performed throughout the field phase, details can be found in Supporting Information Appendix Table S2.
Dental examinations were performed by four teams working in parallel; each team consisted of one dentist, one interviewer and one contact person. Periodontal assessment was performed according to different protocols throughout the DMS waves of which a partial‐mouth recording was the common denominator with two sites (mesio‐vestibular and mid‐vestibular) from the following index teeth: 17, 16, 11, 44, 46 and 47. If there was a missing index tooth, we registered that and considered that in full‐mouth estimations as described below. PPD was measured using a WHO probe (PCP 11.5B, HuFriedy, Tuttlingen) and was noted in 1 mm increments (hence, the threshold of treatment needs emerging was 4.0 mm in the present study, while according to German regulations it is 3.5 mm). The values were rounded mathematically. The maximum probing pressure was 0.2 N. Making contact with the tooth, the WHO periodontal probe was inserted in parallel to the tooth axis into the sulcus or pocket and the distance from the gingival margin to the sulcus base or pocket base was determined at the measurement sites per index tooth.
Our outcome parameter was the number of teeth with PPD ≥ 4 mm, these teeth are regarded in need for periodontal treatment according the German statutory healthcare, where only PPDs are used to decide periodontal treatment needs. We also determined the number of cases with ≥4 teeth with PPD ≥ 4 mm, as within the described German healthcare, these are considered “periodontitis patients”, who are managed within a systematic concept of treatment planning, pre‐treatment phase, active periodontal treatment involving scaling and root‐planing (with or without access surgery) and post‐surgical control. In cases with only 1–3 teeth with PPD ≥ 4 mm, these are not managed within such systematic concept, but using scaling and root planning only (KZBV 2017).
Further recorded clinical parameters were tooth loss, caries lesions, restorations (i.e., the components of the DMFT index), prosthodontic status, and developmental and acquired dental hard tissue defects, based on 28 teeth (third molars were excluded). A paper‐based questionnaire was completed by the subjects before the clinical examination, comprising questions on oral hygiene habits/prosthesis hygiene, utilization of dental services, questions on childhood and life course, smoking habits, and social demographics including education, income, place of residence and place of birth.
2.3. Missing data
Missing predictor variables occurred very rarely (<6% of cases). We imputed missing values using k‐nearest neighbour imputation (Andridge & Little, 2010) with k = 5 and the Euclidean distance as distance metric. Before applying k‐nearest neighbour imputation, categorical features were one‐hot encoded. Both categorical and numerical features were centred and scaled.
2.4. Prediction of full‐mouth recordings
For the transformation of partial‐mouth to full‐mouth PPD recordings, we applied a two‐staged modelling approach using extreme gradient boosting, a decision‐tree based ensemble method applicable for classification and regression (Chen & Guestrin, 2016). In the first step, we modelled patients as having or not having any teeth with PPD ≥ 4 mm (classification task). In the second step, we predicted the number of teeth with PPD ≥ 4 mm for each subject in the data set (regression task). The training data set constituted of 199 subjects, drawn for DMS V, for whom full‐mouth and partial‐mouth recordings were available. We preselected predictor variables based on domain knowledge and data availability. The following 13 variables were used: (1) Year of birth, (2) age in years, (3) sex, (4) educational level (three categories), (5) income (four categories), (6) smoking status (three categories), (7) number of missing teeth, (8) number of filled teeth, (9) number of decayed teeth, (10) number of teeth with PPD ≥ 4 mm (partial mouth, at maximum six teeth with two sites), (11) number of teeth with PPD = 4–5 mm (partial mouth), (12) number of teeth with PPD ≥ 6 mm (partial mouth), (13) number of teeth examined for partial‐mouth assessment (1 to 6, accounting for teeth missing and hence not being assessed). Model parameters were obtained by applying three‐times repeated fivefold cross‐validation for 24,000 parameter combinations (classification) and 100,000 parameter combinations (regression) using random search (Claesen & De Moor, 2015). The model parameters for classification were optimized for the area under the receiver operating characteristic curve (AUC); parameters for regression were optimized for root mean square error (RMSE). Using the best performing model parameter configuration, predictions for the number of teeth with PPD ≥ 4 mm were made for young adults (35–44 years old) and young seniors (65–74 years old). Details can be found in the appendix (Supporting Information Figures S1–S3). Based on these predictions, 95% confidence intervals were obtained by bootstrapping, using 10,000 bootstrap samples. Modelling, data preparation and visualization was done using the R package caret, and the Python packages Numpy, Pandas and Matplotlib.
2.5. Cross‐sectional imputation
In the three waves of the DMS, subject data were available for age cohorts 35–44 years and 65–74 years. We computed the weighted mean age for each age cohort and DMS wave, and both the mean number of teeth and cases with periodontal treatment need. For age groups not sampled by the DMS, we interpolated cross‐sectionally by fitting a piecewise cubic polynomial spline (Akima, 1970). A boundary condition of zero was set for 12‐year‐olds.
2.6. Longitudinal imputation
We modelled the non‐linear pattern of the mean number of teeth and cases with periodontal treatment need per age group longitudinally for the period 1997 to 2030 by applying log‐linearization and then fitting a linear regression model (for teeth) and a quadratic regression model (for cases). Thereafter, we applied exponentiation to reproduce the non‐linear pattern. The fit of this imputation (based on partial‐mouth recordings) was reasonable (Supporting Information Figure S4). Note that we aimed to assess population‐level treatment needs; edentate individuals were hence included.
2.7. Population‐level estimates
Number of teeth and cases for each age group and year were combined with recorded (1997–2015) and predicted population estimates (2020–2030) to determine the overall absolute number (Statistisches Bundesamt 2012). We used the so‐called G1‐L1‐W2 scenario prediction model, assuming that fertility will remain nearly constant at the level of 1.4 children per woman (G1), that life expectancy will moderate increase to 84.8 years for men and 88.8 for women until 2060 (L1), and that until 2021 the migration balance decreases to 200,000 persons per year, and remains constant thereafter (W2) (deStatis 2015). An alternative prediction model (V2A), accounting for the recently increased birth rates (to 1.5 children) and higher migration into Germany (W2015), was additionally used, but yielded very similar overall results (see Supporting Information Figures S5 and S6).
3. RESULTS
The characteristics of the three waves of the DMS are displayed in Table 1. The mean number of teeth with periodontal treatment needs has decreased steadily in adults (35–44 years old) between 1997 (7.36 teeth) and 2014 (4.76 teeth). Projected on all individuals in this age group, a decrease from 93.8 million teeth in 1997 to 47.3 million teeth in 2014 was noted. We expect a further decrease in the mean number of teeth in need of treatment in 2030 (to 3.15) (Figure 1a,b), which means a decrease to 33.7 million teeth in all individuals of this age group (Table 2). In contrast, seniors bear an increasing number of teeth per individual (1997: 4.54, 2014: 7.52 teeth) (Figure 1a,b). Projected to all individuals in this age group, an increase from 33.5 million teeth in 1997 to 63.4 million teeth in 2014 was estimated (Table 2). We expect a further increase in the mean number of teeth in need of treatment in 2030 (to 12.23), which means an increase to 140.9 million teeth in all individuals of this age group (Figure 1a,b, Table 2). Thus, treatment needs have decreased in those aged 51 years or below, and increased in groups older than that; this development is expected to continue to 2030. The cumulative number of teeth in need of treatment has increased from 2000 (355.2 million) to 2015 (364.5 million), and is expected to increase further to 2030 (464.4 million) (Figure 1c).
Table 1.
Mean number of teeth with periodontal treatment needs (PPD ≥ 4 mm) per individual
| Strata | Age group | Category/Level | DMS III (1997) | DMS IV (2005) | DMS V (2014) |
|---|---|---|---|---|---|
| All | 35 to 44‐years‐olds | ‐ | 7.36 | 6.34 | 4.76 |
| 65 to 74‐years‐olds | ‐ | 4.54 | 5.99 | 7.52 | |
| Educational level | 35 to 44‐years‐olds | ||||
| Low | 8.57 | 8.24 | 6.04 | ||
| Medium | 7.10 | 7.21 | 4.6 | ||
| High | 6.35 | 4.48 | 3.36 | ||
| 65 to 74‐years‐olds | |||||
| Low | 3.92 | 5.34 | 7.21 | ||
| Medium | 4.84 | 6.84 | 7.37 | ||
| High | 7.04 | 8.17 | 8.48 | ||
| Sex | 35 to 44‐years‐olds | Male | 8.59 | 7.72 | 5.26 |
| Female | 6.20 | 5.60 | 3.46 | ||
| 65 to 74‐years‐olds | Male | 5.12 | 6.80 | 8.62 | |
| Female | 3.81 | 5.17 | 6.69 | ||
| Smoking | 35 to 44‐years‐olds | ||||
| Never smoker | 5.98 | 5.15 | 3.45 | ||
| Former smoker | 7.01 | 6.53 | 4.42 | ||
| Current smoker | 8.98 | 8.26 | 5.59 | ||
| 65 to 74‐years‐olds | |||||
| Never smoker | 4.34 | 5.78 | 7.79 | ||
| Former smoker | 4.99 | 6.63 | 7.69 | ||
| Current smoker | 3.42 | 5.77 | 6.38 |
Estimates are based on imputed full‐mouth numbers of teeth. Edentate individuals are included.
Figure 1.
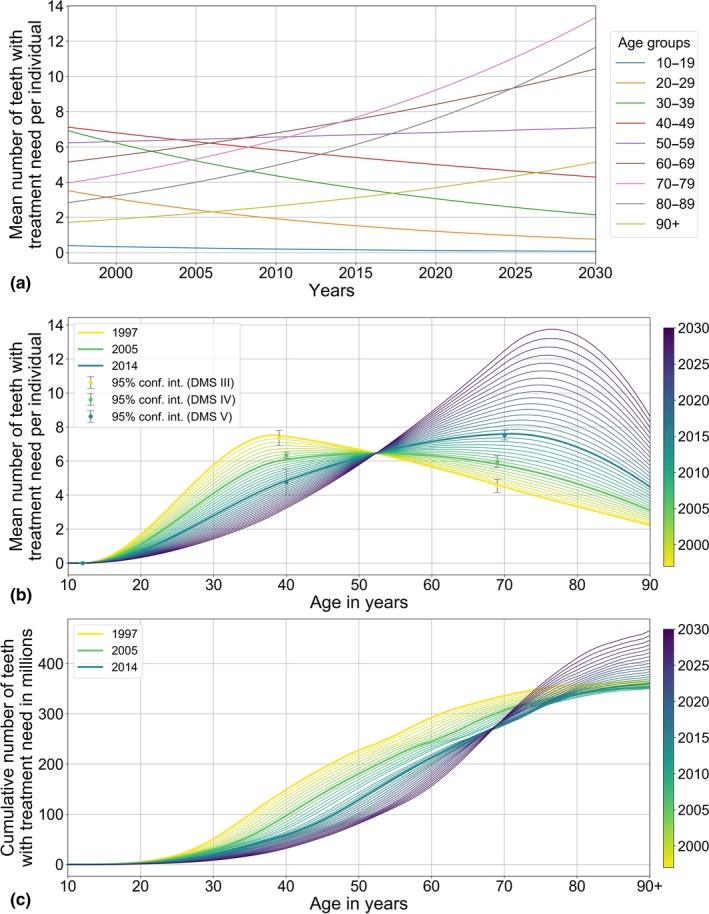
Number of teeth in need for periodontal treatment (PPD ≥ 4 mm). Estimates are based on imputed full‐mouth numbers of teeth. Edentate individuals are included. (a) Mean number of teeth with treatment need in different age groups between 1997 and 2030. (b) Mean number of teeth with treatment need at different ages in different years between 1997 and 2030. (c) The cumulative number of teeth (in millions) with treatment need between 1997 and 2030
Table 2.
Mean number of teeth with periodontal treatment needs (PPD ≥ 4 mm) and cases (individuals >3 teeth with PPD ≥ 4 mm) in the different waves of the DMS, and projected until 2030
| DMS | Age group | Individuals in million | Teeth per individual | Teeth in million | Cases (%) | Cases in million |
|---|---|---|---|---|---|---|
| DMS III (1997) | 35 to 44‐years‐old | 12.745 | 7.36 | 93.8 | 74 | 9.432 |
| 65 to 74‐years‐old | 7.390 | 4.54 | 33.5 | 56 | 4.138 | |
| DMS IV (2005) | 35 to 44‐years‐old | 13.881 | 6.34 | 88.0 | 65 | 9.023 |
| 65 to 74‐years‐old | 9.134 | 5.96 | 54.4 | 67 | 6.120 | |
| DMS V (2014) | 35 to 44‐years‐old | 9.943 | 4.76 | 47.3 | 37 | 3.679 |
| 65 to 74‐years‐old | 8.435 | 7.52 | 63.4 | 80 | 6.748 | |
| 2030 | 35 to 44‐years‐old | 10.690 | 3.15 | 33.7 | 22 | 2.352 |
| 65 to 74‐years‐old | 11.520 | 12.23 | 140.9 | 76 | 8.758 |
Estimates are based on imputed full‐mouth numbers of teeth. Edentate individuals are included.
The prevalence of cases in need of periodontal treatment in adults (35–44 years old) has decreased steadily between 1997 (74%) and 2014 (37%) (Figure 2a,b), or 9.4 million cases in 1997 and 3.7 million cases in 2014 (Table 2). We expect a further decrease in the prevalence of cases in need of periodontal treatment in 2030 (to 22%), which means a decrease to 2.4 million cases in this age group. In contrast, the prevalence of cases in seniors has increased (1997: 56% 2014: 80%) (Figure 2a,b). Projected on all individuals in this age group, this was an increase from 4.1 million cases in 1997 to 6.8 million in 2014 (Table 2). We expect a minimal decrease to 76% in 2030 (or 8.8 million cases). The cumulative number of cases in need of treatment has decreased from 2000 (39.2 million) to 2015 (34.9 million), and is expected to decrease further to 2030 (30.9 million) (Figure 2c).
Figure 2.
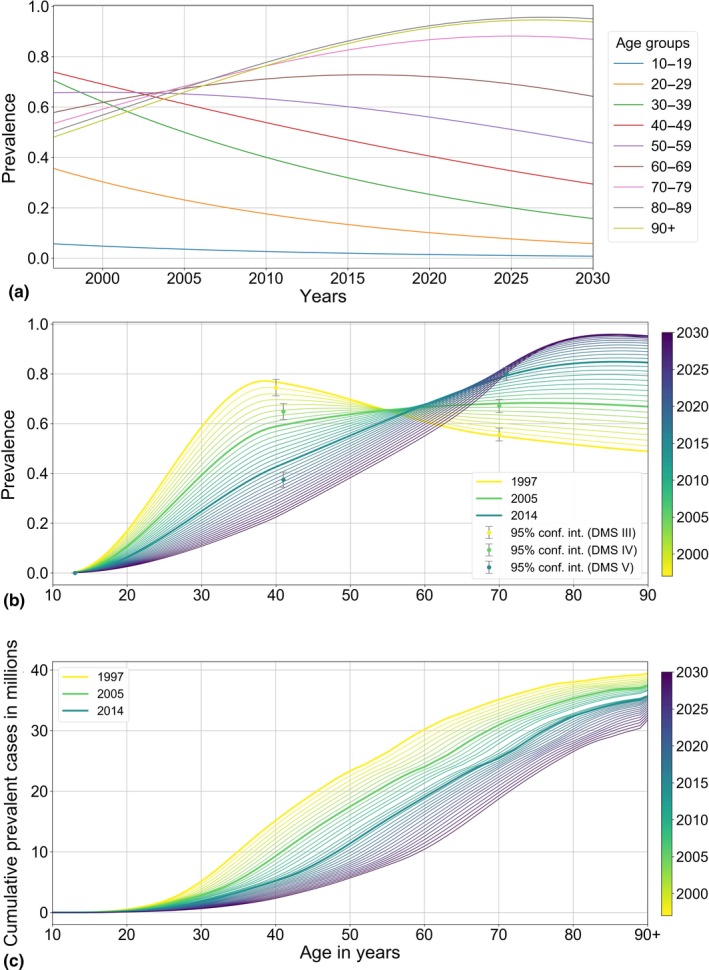
Prevalence and prevalent cases in need for periodontal treatment (>3 teeth with PPD ≥ 4 mm). Estimates are based on imputed full‐mouth numbers of teeth. Edentate individuals are included. (a) Prevalence in different age groups between 1997 and 2030. (b) Prevalence at different ages in different years between 1997 and 2030. (c) The cumulative number of prevalent cases (in millions) between 1997 and 2030
4. DISCUSSION
In Germany, as in many high‐income countries, populations are rapidly ageing; individuals aged 60 years or above are the only growing age group, while younger age groups shrink (deStatis 2018). Combining these population data with epidemiological data allows to quantify and contrast overall treatment needs in a country over time. The data from the present study will inform dental services planning in Germany.
Based on our findings, periodontal treatment needs have dramatically decreased in the younger age group, and will have nearly halved by 2030 compared to 1997. This younger group seems to benefit from various underlying trends; for example, these individuals have a higher education (deStatis 2017), enter adulthood with substantially fewer restorations (Jordan & Micheelis, 2016), they smoke less often (deStatis 2017), show a higher oral health awareness and better oral hygiene, and many attend the dentist more regularly (Jordan & Micheelis, 2016). In parallel, the growing group of elderly retains an increasing number of teeth at risk for periodontal disease. Based on our results, the mean number of teeth with PPD ≥ 4 mm in seniors (aged 65–74 years) in Germany has nearly doubled since 1997 and is expected to nearly triple in total until 2030. This increase in the number of teeth with PPD ≥ 4 mm in the elderly has also been observed in the SHIP studies, where the 75 + ‐year‐old subjects had 1.5 teeth with treatment needs in 1997–2001, and 2.5 teeth in 2008–2012 (Schutzhold et al., 2015). Given the described demographic shifts, the population‐level number of teeth with periodontal treatment needs in this age group in Germany will nearly quadruple. The cumulative number of teeth (i.e., the sum of teeth with treatment needs in the whole German population) in Germany has increased by 25% between 1997 and 2014, and will increase further until 2030 (by then 29% compared with 1997). In parallel, the number of adult cases with treatment needs has nearly halved since 1997 and will halve once more until 2030; the contrary is the case in the elderly, where a large part shows treatment needs already today. Given that the total number of cases with treatment needs is not expected to increase, a smaller number of individuals will carry an increasing burden in the future.
Our findings have implications on various levels. First, periodontal treatment needs will be increasingly age‐specific; nearly all individuals aged 65–80 years will show some periodontal treatment needs by 2030, while few adult subjects (35–44 years old) will. Periodontal management concepts including disease detection (screening) and treatment should account for that. Second, in the elderly, the treatment needs per patient will increase (we estimate, in mean, 12 teeth with treatment needs in those aged 65–74 years; this number will be even higher in those aged >75 years). Considering that the 75‐year‐olds in 2030 are the 42‐year‐olds of 1997, who showed 11.7 filled and 3.9 missing teeth at that age already (Jordan & Micheelis, 2016), managing these patients will be complex and involve periodontal, restorative and treatments. In the very old, a substantial number of individuals will additionally require long‐term care; providing conventional dental and periodontal treatment will be a challenge for these individuals. Nevertheless, managing dental diseases in this group will remain mandatory when considering possible co‐morbidities and sequels of poor oral health due to missing teeth, untreated carious lesions, ill‐fitting dentures and periodontitis, like diabetes, malnutrition or pneumonia (Schwendicke, Stolpe, & Müller, 2017; Tonetti, Bottenberg et al., 2017). Third, the estimated needs and the resulting demand will need to be addressed by the future dental workforce. Pregraduate curricula of periodontology and postgraduate specialization programs may need to be adopted in scope and breadth accordingly. Also, long‐term systematic management of periodontal disease should be implemented within the statutory insurance (currently, supportive periodontal therapy is not covered). Moreover, it should be considered that PPD may not be the only relevant measure to estimate treatment needs; in elderly populations, periodontal attachment loss has been shown to be experienced through recession rather than pocketing (Schutzhold et al., 2015), and ageing has not necessarily been found to come with increased PPDs (but often with increased attachment loss) (Renvert, Persson, & Persson, 2013).
This study and the underlying data have a number of strengths. First, a novel approach of cross‐sectionally and longitudinally imputing data allowed to identify trends across age groups and cohorts, and thus helps to understand patterns of disease dynamics and resulting treatment needs which have so far not been described. Second, by combining data on periodontitis with data on population, we were able to more comprehensively evaluate the combined effects of disease and population dynamics. Third, nationally representative data were used.
Several limitations apply, too. First, we used partial‐mouth recordings to transform them into full‐mouth data, as only full‐mouth data are useful for estimating treatment needs in a way that allows health services planning. Transformation was based on a subsample of the DMS V, where 199 patients had been examined full‐mouth. We used Extreme Gradient Boosting to determine this transformation, and validated our findings against simple transformations (Jordan & Micheelis, 2016). Our transformation might not hold perfectly true for the samples in the DMS III and IV, and we were unable to validate our estimates here. However, it was reassuring to find the trends—reduced treatment need in younger and increased need in older individuals—to be reflected by data from another large German study (Schutzhold et al., 2015). Second, our projection to 2030 can only limitedly account for unknown secular health trends and how these will change in the future. For example, the DMS found self‐efficacy, oral hygiene and dental services utilization in seniors to increase or improve with time, for example. Also, the improved periodontal health in younger adults may well continue into older age at some point, compensating for the fact that more units are at risk there. In this case, elderly would have more teeth, which remain nevertheless healthier than in the past. The Jönköping studies, which find that—similar to Germany—the number of retained teeth has considerably increased over the last three decades in the 70‐ to 80‐year‐olds, report such trend reversal in the elderly population (Norderyd et al., 2015). Also, our projection approach built on only one covariate, the year of birth of an individual (in different age groups), assuming past changes in the number of teeth per individual continuing to some degree in the future. An alternative would have been to use a multivariate regression model for prediction. We have done so in a previous study to predict tooth loss in 2030, but found that a model based on a reasonable set of socio‐economic and health‐related predictors does not necessarily account for large parts of the observed variance, while the year of birth and the age of the individuals were the covariates with the most predictive power. Additional analyses performed on the present data using multivariable linear regression modelling (see Supporting Information Appendix Table S3, Figure S7) confirmed this; the explanatory value of all used variables remained limited at 22%. Third, our data do not allow to monitor the severity of the disease; no stratification into teeth with moderate (PPD = 4–5 mm) or severe (PPD ≥ 6 mm) periodontitis was made, with teeth with PPD ≥ 6 mm possibly requiring surgical treatment more often. Also, it was not possible to stratify treatment needs into different treatment phases (active/supportive treatment). However, as surgical treatment is very rarely provided under the statutory insurance and supportive therapy is not at all covered, such stratification was not needed for the purpose of our study. Last, we once more highlight that our study evaluated treatment needs under the perspectives of German healthcare, that is solely based on PPDs. Of course, PPD do not necessarily reflect attachment loss; in case of overgrowth it overestimates, while in the elderly PPD plateaus and thus underestimates (Billings et al., 2018; Schutzhold et al., 2015). In many settings, attachment loss rather than PPD may be used to decide on treatment needs and resulting demands, and even in Germany, periodontal therapy may be provided to teeth not falling into our case definition outside of the statutory insurance setting (i.e., patients would pay privately for such therapy). Also, the proportion of treated cases remains unclear. For example, in a treated case, a PPD of 4 mm may reflect an acceptable endpoint of treatment which does not generate further treatment need. While it was not possible to capture this aspect, future evaluations should attempt to consider this when assessing treatment needs.
5. CONCLUSIONS
Based on the present study, periodontal treatment needs have moderately declined in younger adults since 1997 and are expected to decline further in the future. In individuals aged >51 years, treatment needs have increased and may continue to do so. Given the demographic population shift, population‐wide cumulative treatment needs may increase until 2030. Health services and workforce planning should address these increasing needs (in oftentimes highly vulnerable populations) in Germany in the future.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflict of interests in connection with this article.
6.
Clinical Relevance.
Scientific rationale for the study: Evaluating time trends and projecting future treatment needs are relevant for clinicians and resource allocation. We assessed treatment needs in Germany, capturing both disease and population dynamics over time using nationally representative data.
Principal findings: In younger adults, periodontal treatment needs have moderately declined since 1997 and are expected to decline further in the future. In individuals aged >51 years, treatment needs may increase substantially. Given the demographic population shift, a higher overall population‐level treatment need is expected in the future.
Practical implications: Health services and workforce planning should address the increasing periodontal treatment needs in Germany.
Supporting information
ACKNOWLEDGEMENTS
The study was coordinated by Kantar Health GmbH, Munich (Germany) after a call for tenders published in the information system for European public procurement on May 31, 2013 (2013‐073518). We hereby acknowledge the contributions of the field and research staff of the “DMS V Surveillance Investigators’ Group”.
Schwendicke F, Krois J, Kocher T, Hoffmann T, Micheelis W, Jordan RA. More teeth in more elderly: Periodontal treatment needs in Germany 1997–2030. J Clin Periodontol. 2018;45:1400–1407. 10.1111/jcpe.13020
Funding information
The German Oral Health Studies are financed by the German dental profession via the German Dental Association (Bundeszahnärztekammer – Arbeitsgemeinschaft der Deutschen Zahnärztekammern – (BZÄK) e. V.) and the National Association of Statutory Health Insurance Dentists (Kassenzahnärztliche Bundesvereinigung (KZBV) KdöR). However, the writing group is solely responsible for the contents of this paper.
REFERENCES
- Akima, H. (1970). A new method of interpolation and smooth curve fitting based on local procedures. Journal of the ACM, 17, 589–602. 10.1145/321607.321609 [DOI] [Google Scholar]
- Andridge, R. R. , & Little, R. J. (2010). A review of hot deck imputation for survey non‐response. International Statistical Review, 78, 40–64. 10.1111/j.1751-5823.2010.00103.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings, M. , Holtfreter, B. , Papapanou, P. N. , Mitnik, G. L. , Kocher, T. , & Dye, B. A. (2018). Age‐dependent distribution of periodontitis in two countries: Findings from NHANES 2009 to 2014 and SHIP‐TREND 2008 to 2012. Journal of Clinical Periodontology, 45(Suppl 20), S130–S148. 10.1111/jcpe.12944 [DOI] [PubMed] [Google Scholar]
- Chen, T. , & Guestrin, C. (2016). XGBoost: A scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, pp. 785–794. San Francisco, CA: ACM. [Google Scholar]
- Claesen, M. , & De Moor, B. (2015). Hyperparameter search in machine learning. Retrieved from https://arxiv.org/pdf/1502.02127v2.pdf
- Frencken, J. E. , Sharma, P. , Stenhouse, L. , Green, D. , Laverty, D. , & Dietrich, T. (2017). Global epidemiology of dental caries and severe periodontitis – A comprehensive review. Journal of Clinical Periodontology, 44(Suppl 18), S94–S105. 10.1111/jcpe.12677 [DOI] [PubMed] [Google Scholar]
- Gesundheitsberichtserstattung (2018). Versicherungsverhältnisses in der Krankenversicherung. Retrieved from http://www.gbe-bund.de
- Holtfreter, B. , Albandar Jasim, M. , Dietrich, T. , Dye Bruce, A. , Eaton Kenneth, A. , Eke Paul, I. , … Kocher, T. (2015). Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies. Journal of Clinical Periodontology, 42, 407–412. 10.1111/jcpe.12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan, R. A. , & Micheelis, W. (2016). Fünfte Deutsche Mundgesundheitsstudie. Köln, Germany: Deutscher Zahnärzte Verlag, Institut der Deutschen Zahnärzte. [Google Scholar]
- Kassebaum, N. J. , Smith, A. G. C. , Bernabé, E. , Fleming, T. D. , Reynolds, A. E. , Vos, T. , … Yonemoto, N. (2017). Global, regional, and national prevalence, incidence, and disability‐adjusted life years for oral conditions for 195 countries, 1990–2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. Journal of Dental Research, 96, 380–387. 10.1177/0022034517693566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- KZBV (2017). Catalogue of Fees [Gebührenverzeichnisse] 2017. Berlin, Germany: KZBV. [Google Scholar]
- Micheelis, W. , & Reich, E. (1999). Dritte Deutsche Mundgesundheitsstudie. Retrieved from www3.idz-koeln.de/idzpubl3.nsf/…/$FILE/dms-III-zusammenf.pdf
- Micheelis, W. , & Schiffner, U. (2006). Vierte Deutsche Mundgesundheits‐Studie (DMS IV) In: Institut der Deutschen Zahnärzte (Eds.), IDZ Materialreihe. Köln, Germany: Deutscher Ärzteverlag. [Google Scholar]
- Norderyd, O. , Koch, G. , Papias, A. , Kohler, A. A. , Helkimo, A. N. , Brahm, C. O. , … Frisk, F. (2015). Oral health of individuals aged 3–80 years in Jonkoping, Sweden during 40 years (1973–2013). II. Review of clinical and radiographic findings. Swedish Dental Journal, 39, 69–86. [PubMed] [Google Scholar]
- Page, R. C. , & Eke, P. I. (2007). Case definitions for use in population‐based surveillance of periodontitis. Journal of Periodontology, 78, 1387–1399. 10.1902/jop.2007.060264 [DOI] [PubMed] [Google Scholar]
- Renvert, S. , Persson, R. E. , & Persson, G. R. (2013). Tooth loss and periodontitis in older individuals: Results from the Swedish National Study on Aging and Care. Journal of Periodontology, 84, 1134–1144. 10.1902/jop.2012.120378 [DOI] [PubMed] [Google Scholar]
- Righolt, A. J. , Jevdjevic, M. , Marcenes, W. , & Listl, S. (2018). Global‐, regional‐, and country‐level economic impacts of dental diseases in 2015. Journal of Dental Research, 97, 501–507. 10.1177/0022034517750572 [DOI] [PubMed] [Google Scholar]
- Schutzhold, S. , Kocher, T. , Biffar, R. , Hoffmann, T. , Schmidt, C. O. , Micheelis, W. , … Holtfreter, B. (2015). Changes in prevalence of periodontitis in two German population‐based studies. Journal of Clinical Periodontology, 42, 121–130. 10.1111/jcpe.12352 [DOI] [PubMed] [Google Scholar]
- Schwendicke, F. , Stolpe, M. , & Müller, F. (2017). Professional oral healthcare for preventing nursing home‐acquired pneumonia: A cost‐effectiveness and value of information analysis. Journal of Clinical Periodontology, 44, 1236–1244. 10.1111/jcpe.12775 [DOI] [PubMed] [Google Scholar]
- deStatis (2015). Population projection. Retrieved from https://www.destatis.de/EN/FactsFigures/SocietyState/Population/PopulationProjection/PopulationProjection.html
- deStatis (2017). Rauchgewohnheiten der Bevölkerung.Retrieved from https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Gesundheitszustand/Rauchgewohnheiten5239004179004.pdf.
- deStatis (2018). Bevölkerungspyramide. Retrieved from https://service.destatis.de/bevoelkerungspyramide/#!y=2040
- Statistisches Bundesamt (2012). Online‐Datenbank: Fortschreibung des Bevölkerungsstandes (Stand: 31.05.2012). Retrieved from www.destatis.de
- Tonetti, M. S. , Bottenberg, P. , Conrads, G. , Eickholz, P. , Heasman, P. , Huysmans, M. C. , … Paris, S. (2017). Dental caries and periodontal diseases in the ageing population: Call to action to protect and enhance oral health and well‐being as an essential component of healthy ageing – Consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. Journal of Clinical Periodontology, 44(Suppl 18), S135–S144. 10.1111/jcpe.12681 [DOI] [PubMed] [Google Scholar]
- Tonetti, M. S. , Jepsen, S. , Jin, L. , & Otomo‐Corgel, J. (2017). Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. Journal of Clinical Periodontology, 44, 456–462. 10.1111/jcpe.12732 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


