Abstract
Dietary diversity is a key component of infant and young child feeding (IYCF) as well as adult health. In Tajikistan, a predominantly rural, former Soviet country in Central Asia, we conducted formative research to identify barriers to dietary diversity and strategies for nutrition behaviour change. In Spring, 2016, mixed‐methods data collection took place across 13 villages in all five regions, collecting collaborative mapping; structured assessments of stores and markets; home visits for dietary recalls; food storage, preparation, and meal observations; focus groups with pregnant women, mothers of young children, fathers, and mothers‐in‐law; and in‐depth expert interviews with local nutrition and health influentials. Overall, maternal diet was adequate in terms of diversity (only 13% reported <5/10 food groups in the past 24 hr); however, only 42% of index children 6–24 months met WHO guidelines for diversity, and only 34% met minimum acceptable diet criteria. In addition to issues of poverty and food scarcity, qualitative data reveal many behavioural barriers to timely introduction of diverse complementary foods. Women's strategies focused on gradual introduction of household diet components, without regard for diversity or nutrition. Foods such as meat were seen as costly and thus inappropriate for IYCF, and food taboos (i.e., fresh vegetables) further reduced diversity. Infant food preparation methods such as grinding were seen as impractical, and many foods were withheld until children develop teeth. Possible nutrition education strategies include point‐of‐purchase campaigns to improve availability and appeal of IYCF‐friendly foods, as well as influencing other key household members through mosques, schools, and health care providers.
Keywords: Central Asia, dietary diversity, IYCF, poverty, undernutrition
Key messages.
As in many low‐resource countries, infants in Tajikistan are at risk for undernutrition, due in part to delayed introduction of diverse complementary foods.
Cost and availability of foods play a role in limiting dietary diversity, but in most households where IYCF is suboptimal, adult household members report adequate diversity.
Although infant health is highly prioritized within the household, child nutritional activities focus on satiety and gradual socialization to the family diet, rather than strategic planning for optimal infant nutrition.
Nutritional education for behaviour change should leverage multiple family members and utilize multiple channels, including schools, mosques, health care providers, and point‐of‐purchase communication.
1. INTRODUCTION
Diversity is one cornerstone of healthful diet across the life course, with diets lacking diversity contributing to micronutrient deficiency and undernutrition (Ruel, 2003). In developing countries, poor dietary diversity is often tied to low socio‐economic status, with reliance on starchy diets with little meat‐based protein, fresh fruits, or vegetables (Ruel, 2003). Dietary diversity plays a role in the health of women of reproductive age, preconception and fetal development, and infant and child growth (Begin & Aguayo, 2017; Krasevec, An, Kumapley, Begin, & Frongillo, 2017; Krebs‐Smith, Smiciklas‐Wright, Guthrie, & Krebs‐Smith, 1987). It is also key to reducing obesity‐related chronic disease burden in adulthood and combating detrimental effects of the global nutrition transition.
Tajikistan is a small mountainous former Soviet country in Central Asia, with diverse climate and food environments. Multiple ethnic and language groups live in rural villages within a predominantly Muslim, Persian culture. Despite economic progress since independence in 1991 and the subsequent civil war, it remains among the poorest Commonwealth of Independent States countries, with significant unemployment and labour migration to Russia. Undernutrition in Tajikistan remains significant, with the first Tajikistan Demographic Health Survey (DHS) in 2012 finding that 26% of children <5 were stunted from chronic malnutrition, 10% were wasted (indicating acute malnutrition), and 12% were underweight. Micronutrient deficiency is widespread (Statistical Agency under the President of the Republic of Tajikistan [SA], Ministry of Health [Tajikistan], and ICF International, 2013). Prevalence of anaemia among both children 6–59 months and reproductive age women is 26%, and median urinary iodine content levels are 87.5 μg/l among children <5 and 75.0 μg/l among reproductive age women, far below the threshold of 100 μg/l (Ministry of Health Republic of Tajikistan, 2018). Most Tajik children breastfeed, but only 34% of infants <6 months old receive exclusive breastfeeding, only 49% begin complementary foods at 6 months, and only 20% of children 6–23 months receive recommended food diversity and meal frequency (Statistical Agency under the President of the Republic of Tajikistan [SA], Ministry of Health [Tajikistan], and ICF International, 2013). Interventions addressing maternal and child undernutrition in Tajikistan include promotion of exclusive breastfeeding and optimal infant and young child feeding (IYCF), micronutrient supplementation programme (semi‐annual Vitamin A campaign for children <5, iron/folic acid supplementation for pregnant women, and multiple micronutrient powders [“sprinkles”] for children 6–23 months), treatment of acutely malnourished children, and universal salt iodization.
Along with addressing economic and geographic access to diverse foods, a key strategy for nutrition behaviour change is education (Mayen et al., 2016; Sanghvi, Seider, Baker, & Jimerson, 2017). Soviet‐era gains in universal secondary education have not been fully recovered since the civil war; in 2012, only 51% of females age 20–24 had completed secondary school (Statistical Agency under the President of the Republic of Tajikistan [SA], Ministry of Health [Tajikistan], and ICF International, 2013). In villages, girls' schooling is often restricted by demands at home; additionally, Tajik curriculum offers little reproductive health or nutrition education. Tajik women typically move as “young brides” to their husband's village and family home, where their prenatal and post‐natal diets are shaped by multigenerational household dynamics and seasonal agrarian economics. Given Tajikistan's traditional household and community culture, interventions for women must not only deliver specific micronutrients but also leverage key interpersonal relationships to build long‐term sustainable change in household‐level dietary attitudes and behaviours. The emerging nutrition transition and obesity burden in traditional cultures also present compelling rationale for development of culturally based nutrition education interventions for reproductive age women.
In 2015–2016, UNICEF Tajikistan partnering with the Tajikistan Ministry of Health and Social Protection (MoHSP) and Drexel University undertook formative research to explore factors influencing nutrition across diverse geographic settings and ethnic and cultural groups. The research objectives were to describe current IYCF and maternal nutrition practices; identify positive and negative socio‐cultural, economic, gender, and contextual influences; and recommend strategies to improve maternal and child nutrition.
2. RESEARCH DESIGN AND METHODS
Complex nutrition behaviours, including child feeding, are best understood and modified using theory that considers multiple levels of influence. The Social–Ecological Model (Bronfenbrenner, 1992; Figure 1) takes into account interconnected influences of family, peers, community, and society on behaviour and successful behaviour change. Social ecology, “the study of influence of the social context on behavior” (Sallis, Owen, & Fisher, 2008), is a form of meta‐model or meta‐theory, because each model level encompasses theories of change for that particular level. Higher levels may facilitate or constrain change at lower levels, suggesting that interventions for planned change should address all levels to be effective. Thus, individuals' behaviours cannot be understood without examining peer networks, family and household relationships, community influences, and resources and societal norms.
Figure 1.
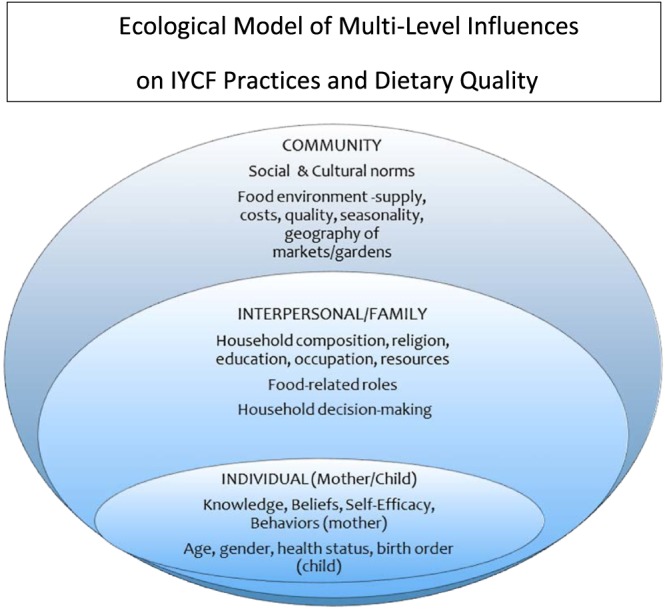
Ecological model of multilevel influences on IYCF practices and dietary quality
The mixed‐methods approach utilized structured methods to measure quantitative elements of diet, food access, and household environments, and qualitative methods to explore more nuanced aspects of culture, social roles and relationships, and beliefs and attitudes. The benefits of a mixed‐methods approach to understanding diet in diverse populations are substantial. Diets are composed not just of individual nutrients but of foods, combinations of foods in meals, and patterns of eating events across time. Similarly, individuals obtain, prepare, and consume foods in social units of households, families, and communities. A quantitative analysis based on analysing micronutrients or other dietary elements decomposes eating events to understand, and perhaps prioritize, specific nutrients among multiple nutritional problems stemming from poor diet. However, a qualitative approach recomposes those elements into a food culture within the lives of children, mothers, and households, and to understand the drivers and intervention points to change quantitative outcomes. The concurrent design examined quantitative and qualitative data simultaneously to provide cross‐sectional explanatory evidence (Creswell, Klassen, Plano‐Clark, & Smith, 2011). By prioritizing the collection of both quantitative and qualitative data and conducting a mixed‐methods analysis, the process of “meta‐inference” can triangulate and validate or also expand on seemingly contradictory findings from any individual data source.
2.1. Data sources and data collection
Expert interviews with Tajik regional and national maternal and child health leaders and nutrition‐focused experts from development partners informed fieldwork design and methods. After analysing national data on geographic patterns of food production and availability, undernutrition, and cultural practices, a purposive sample of 13 representative districts and villages, across all five regions of Tajikistan, were selected for village‐level in‐depth data collection. In Spring, 2016, after a week‐long training, teams of MoHSP data collectors undertook multiday field visits to each village to engage in a predetermined village‐level sampling strategy and set of data collection activities. An introductory transect walk with participatory mapping with key residents gave teams spatial‐ethnographic understandings of village food environments and publically introduced the study to residents. Structured market and store assessments of food availability and pricing were collected using a comprehensive, culturally based tool (Byker Shanks, Jilcott Pitts, & Gustafson, 2015). Age and gender appropriate data collectors conducted four focus groups: with young women expecting their first child, mothers of children <24 months, fathers of young children, and mothers‐in‐law living with young children. Up to four in‐depth interviews were conducted with key informants, including health care workers, religious leaders, women's council heads, and local political leaders.
In each village, four diverse households were purposively selected for the 2‐day household data collection, and within households with multiple mothers and children, one child age 6–23 months was selected to serve as the “index child,” with his or her mother and father (if present) serving as the “index mother and father.” Households' selection sought diversity of factors shaping dietary behaviour, including index child age and gender, maternal age and parity, and household size, composition, and socio‐economic status. Data collection included structured observations of sanitation, meal preparation, and (as permitted) mealtime behaviours; 24‐hr and 7‐day food recalls for an index child age 0–24 months, the child's mother, and the household; and an in‐depth semistructured interview with the child's mother.
Thus, across the 13 selected villages, the final data for analysis included information from 52 focus groups (13 villages with four groups per village), 52 households (four per village), and 38 in‐depth interviews (two to four per village, depending on whether villages had specific types of leaders), as well as data from village mapping and market assessments. Sampling and data collection were successful in every village, and our final completed data collection matched the planned sampling strategy and sample size for the overall data collection effort, which was designed a priori, based on Tajikistan's geographic and cultural diversity, available resources, and goals for thematic saturation and understanding of key elements of IYCF.
Households received culturally appropriate gifts (cooking oil and soap), and focus group participants received refreshments and nutrition education materials. All participants provided verbal informed consent. The research was approved by Drexel University's Institutional Review Board, UNICEF Tajikistan, and the Tajikistan MoHSP. Data, including audio recordings, notes and questionnaires, maps, and photographs, were transmitted to Drexel for translation and analysis.
2.2. Data and measures used
For this paper, structured questionnaire, 24‐hr dietary recall, and qualitative in‐depth interview and focus group data are incorporated to explore correlates of dietary diversity and potential leverage points for intervention. Mothers' Minimum Dietary Diversity‐Women (MDD‐W; FAO and FHI360, 2016) scores counted prior day intake from 10 food groups (grains/roots/tubers, pulses, nuts/seeds, dairy, flesh foods, eggs, dark green leafy vegetables, other Vitamin A‐rich fruits and vegetables, other vegetables, and other fruits) with scores ≥5/10 considered adequate diversity. For children, we used the WHO Infant feeding guidelines (WHO, 2008) of exclusive breastfeeding before 6 months and continued breastfeeding at months 12–15. For children 6–23 months, we calculated “minimum dietary diversity” as ≥4 foods from seven groups (grains/roots/tubers, legumes/nuts, dairy, flesh foods, eggs, vitamin A‐rich fruits and vegetables, and other fruits and vegetables), “minimum meal frequency” adjusted for age and breastfeeding status (two meals for infants 6–8 months, three meals for breastfed children 9–23 months, and four meals for non‐breastfed children 9–23 months), and “minimum acceptable diet” (MAD), a 0/1 indicator based on achieving both minimum dietary diversity and meal frequency, and, for non‐breastfed children, receipt of milk.
2.2.1. Quantitative data analysis
Structured data were abstracted from interview instruments, with validation from translated and transcribed audio recordings, and entered into SPSS for analysis. Frequency distributions of key variables are reported in Tables 1 and 2, including mothers' interview responses regarding household characteristics, food procurement, preparation, and eating attitudes and practices, as well as previous day diets for themselves and index children. In Table 3, cross‐tabulations are presented for the index child's dietary diversity and MAD and mother's MDD‐W by key household and maternal characteristics, with marginally and statistically significant associations (P < 0.10, <0.05, and <0.01) identified by the chi‐square statistic.
Table 1.
Household characteristics and influences on IYCF (n = 52 households)
| N | % | |
|---|---|---|
| Region of Tajikistan | ||
| Sugd (three villages) | 12 | 23 |
| Khatlon–Kulob zone (two villages) | 8 | 15 |
| Khatlon–Kurgan Tube zone (three villages) | 12 | 23 |
| RRS (two villages) | 8 | 15 |
| GABO (two villages) | 8 | 15 |
| Dushanbe (one neighbourhood) | 4 | 8 |
| Ethnic background | ||
| Tajik | 37 | 71 |
| Uzbek | 6 | 11 |
| Pamir | 4 | 8 |
| Kyrgyz | 5 | 10 |
| Household size (adults and children) | ||
| 4–6 | 21 | 40 |
| 7–10 | 20 | 39 |
| 11–21 | 11 | 21 |
| Head of household | ||
| Index child's paternal grand father | 36 | 69 |
| Other | 16 | 31 |
| Household resources | ||
| Owns livestock | 40 | 77 |
| Grows food | 47 | 90 |
| Owns car or truck | 27 | 53 |
| Owns television | 44 | 85 |
| Owns radio | 9 | 17 |
| Household educational attainment | ||
| Head of household–Attended University | 21 | 40 |
| Index mother–Attended University | 8 | 15 |
| Index father away in labour migration | 13 | 25 |
| Number of rooms in home | ||
| 2–3 | 17 | 32 |
| 4–5 | 27 | 52 |
| Mother's age | ||
| 19–22 | 16 | 31 |
| 23–27 | 21 | 40 |
| 28–43 | 15 | 29 |
| Index child's age | ||
| 1–5 months | 14 | 27 |
| 6–11 months | 19 | 37 |
| 12–24 months | 19 | 37 |
| Mother's no. of children (including index child) | ||
| 1 | 20 | 38 |
| 2–5 | 32 | 62 |
| Index child is male | 26 | 50 |
| Primary food shopper | ||
| Index child's paternal grand father | 16 | 31 |
| Index child's paternal grand mother | 5 | 10 |
| Other, multiple shoppers | 31 | 59 |
| Primary decision maker on purchases | ||
| Index child's paternal grand mother | 23 | 44 |
| Other, multiple decision makers | 29 | 56 |
| Primary meal planner | ||
| Index child's paternal grand mother | 29 | 56 |
| Other, multiple decision makers | 23 | 44 |
| Family names foods they cannot afford | 35 | 67 |
| Family has seasonal food scarcity | 31 | 60 |
| Family borrows or asks for food | 18 | 35 |
| Who makes decisions on child feeding? | ||
| Child's mother (self) | 34 | 65 |
| Child's paternal grand mother | 13 | 25 |
| Other (both parents, etc.) | 5 | 10 |
| Who should make final decisions? | ||
| Child's mother (self) | 40 | 77 |
| Child's paternal grand mother | 4 | 8 |
| Other (both parents, etc.) | 8 | 15 |
| Who should have priority if food is limited? | ||
| Pregnant/lactating women | 14 | 28 |
| Children | 23 | 49 |
| Elders, adults | 3 | 7 |
| Other answer (share equally, etc.) | 8 | 16 |
| Who advises mother on child feeding? | ||
| Own mother | 31 | 60 |
| Mother in law | 37 | 71 |
| Doctors or health workers | 23 | 44 |
Table 2.
Mother and index child's 24‐hr dietary diversity and nutritional adequacy
| N | % | |
|---|---|---|
| Mother's diet (n = 52) | ||
| MDD‐W number of food groups | ||
| 1–4 | 7 | 13 |
| 5–6 | 21 | 40 |
| 7–8 | 14 | 27 |
| 9–10 | 10 | 20 |
| One or more servings in past day | ||
| Starchy staples | 52 | 100 |
| All dairy products | 47 | 90 |
| Beans and peas | 18 | 35 |
| Nuts and seeds | 18 | 35 |
| Flesh foods | 32 | 62 |
| Eggs | 18 | 35 |
| Vitamin A‐rich dark green leafy vegetables | 41 | 79 |
| Other Vitamin A‐rich fruits and vegetables | 43 | 83 |
| Other vegetables | 48 | 92 |
| Other fruits | 21 | 40 |
| Index child's diet | ||
| Exclusive breastfeeding (0–5 months, n = 14) | 8 | 57 |
| Continued breastfeeding at 1 year (12–15 months, n = 9) | 8 | 89 |
| Introduction of complementary foods (6–8 months, n = 9) | 5 | 55 |
| Minimum dietary diversity (≥4 groups; 6–23 months, n = 38) | 16 | 42 |
| (6–8 months, n = 9) | 0 | 0 |
| (9–11 months, n = 10) | 3 | 30 |
| (12–23 months, n = 19) | 13 | 68 |
| Minimum meal frequency (6–23 months, n = 38) | 25 | 66 |
| (6–8 months, n = 9) | 5 | 56 |
| (9–11 months, n = 10) | 5 | 50 |
| (12–23 months, n = 19) | 15 | 79 |
| Minimum acceptable diet (6–23 months, n = 38) | 13 | 34 |
| (6–8 months, n = 9) | 0 | 0 |
| (9–11 months, n = 10) | 3 | 30 |
| (12–23 months, n = 19) | 10 | 53 |
Table 3.
Nutritional adequacy of index child and mother, by individual, household, and village characteristics (n = 52)
| Minimum dietary diversity of child 6–24 months 16/38 42% | Minimal acceptable diet for child 6–24 months 13/38 34% | MDD‐W ≥ 5 for mother 45/52 87% | |
|---|---|---|---|
| Household characteristics | |||
| Mother's age | |||
| 19–22 (n = 16) | 46% | 27% | 94% |
| 23–43 (n = 36) | 41% | 37% | 83% |
| MDD‐W for mother | |||
| 5–10 (n = 45) | 44% | 38% | — |
| 1–4 (n = 7) | 33% | 17% | — |
| Mother's no. of children (including index child) | |||
| 1 (n = 20) | 31% | 31% | 85% |
| 2–5 (n = 32) | 50% | 36% | 88% |
| Index child gender | |||
| Male (n = 26) | 42% | 37% | 88% |
| Female (n = 26) | 42% | 32% | 85% |
| Head of household | |||
| Father in law (n = 36) | 42% | 35% | 89% |
| Other (n = 16) | 42% | 33% | 81% |
| Household resources | |||
| Garden and livestock | |||
| Yes (n = 36) | 35% | 31% | 94%** |
| No (n = 16) | 58% | 42% | 69% |
| Transportation | |||
| Has car or truck (n = 27) | 47% | 33% | 93% |
| No car or truck (n = 24) | 41% | 36% | 79% |
| Education level of household head | |||
| University (n = 21) | 44% | 31% | 86% |
| Household head–secondary or less (n = 31) | 41% | 36% | 87% |
| Index father in labour migration | |||
| Yes, away (n = 13) | 46% | 46% | 100% |
| No, present (n = 39) | 41% | 30% | 82% |
| Village market environment | |||
| Adequate access (n = 32) | 44% | 35% | 97%*** |
| Poor access (n = 20) | 40% | 33% | 70% |
| Family reports seasonal food scarcity | |||
| Yes (n = 31) | 29%* | 24% | 84% |
| No (n = 21) | 59% | 47% | 91% |
| Family asks others for food when needed | |||
| Yes (n = 18) | 46% | 39% | 72%** |
| No (n = 35) | 40% | 32% | 94% |
| Family says they have enough food | |||
| Yes (n = 45) | 44% | 38% | 93%*** |
| No (n = 6) | 40% | 20% | 33% |
| Mother's sources of child feeding info | |||
| Her mother in law | |||
| Yes (n = 37) | 50% | 42% | 92%* |
| No (n = 15) | 29% | 21% | 73% |
| Her own mother | |||
| Yes (n = 31) | 39% | 30% | 90% |
| No (n = 21) | 47% | 40% | 81% |
| Health care provider | |||
| Yes (n = 23) | 25% | 19%* | 91% |
| No (n = 29) | 55%* | 46% | 83% |
P < 0.10,
P < 0.05,
P < 0.01.
2.2.2. Qualitative data analysis
Qualitative transcripts were read by multiple team members, and memos were used to identify key themes. Subsequently, key text was abstracted and highlighted to correspond with themes.
To contextualize findings from structured data, qualitative analyses are presented, which focus on key thematic content about dietary diversity. A single household “case study” is used to illustrate semistructured interview responses from one mother. Then theme‐specific content is presented, extracted from all village‐level focus group discussions with mothers of young children.
3. RESULTS
3.1. Household sociodemographic and nutrition characteristics
Table 1 provides information on the village and household sample. Data collection took place across all five regions and one neighbourhood in the capital, Dushanbe. Purposive sampling prioritized selecting three villages in two regions, to capture diverse cultures and areas with documented nutrition disparities. Interviews were conducted in Tajik, Uzbek, Pamir, and Kyrgyz languages, with Russian used to facilitate understanding with participants speaking local dialects.
Household size ranged from 4 to 21 members, in rural households with many married sons, daughters‐in‐law, and children. Sixty‐nine percent of mothers lived in households headed by their fathers‐in‐law. Almost all households grew food in gardens and orchards, 77% kept livestock (typically chickens and cows), and 53% owned a means of transportation. Televisions were almost universal (85%) but radios far less common (17%). Forty percent of household heads, but only 15% of index mothers, had attended university. One quarter of fathers were absent, typically in labour migration to Russia. Home sizes were modest, with four room homes very common. Mothers' ages ranged from 19 to 43, and one third were first time mothers. By design, index child gender was balanced.
Fathers‐in‐law were the most common food shopper, either alone or with other family members (i.e., mothers‐in‐law or adult sons). Mothers‐in‐law were most often the decision maker regarding food purchases and meal planning. Where the index mother and her spouse were heads of household, shopping was typically done by the mother herself.
Two thirds of respondents named foods their household could not routinely afford (most commonly meat, followed by fruits and vegetables). Sixty percent of households experienced seasonal scarcity, either due to geographic conditions, such as road freezing and reduced village food access, or because their own economic and agricultural resources were reduced in winter and early spring. Thirty‐five percent of households borrowed food from neighbours or family to manage periodic scarcity, ranging from occasional shortages to households heavily dependent on charitable gifts.
Most mothers (65%) reported making decisions regarding their child's feeding. In 25% of homes, mothers‐in‐law decided how index children were fed, and in 10% of families, others, such as husbands or fathers‐in‐law, had roles. However, when asked who should be the final decision maker, 77% felt the child's mother should have final say, and only 8% viewed mothers‐in‐law as appropriate decision makers.
Respondents were asked to imagine if food was limited, who should receive priority. Most commonly, respondents felt children (49%) or lactating mothers (28%) should receive priority. Less commonly, women felt that elders deserved priority, usually due to their frailty, or that all household members receive equal portions. When asked about child feeding advice, 71% sought advice from their mothers‐in‐law, slightly fewer (60%) received information from their own mothers, and only 44% from health care providers.
3.2. Mother and index child nutrition
Table 2 displays the previous day's dietary quality of mothers and index children. Only 13% of mothers had MDD‐W scores of ≤4; however, an additional 40% ate from only 5–6 groups. Starchy staples (bread) and dairy products (yogourt and milk) were common foods, with legumes, nuts, eggs, and non‐Vitamin A fruits less common.
Of 14 index children <6 months, 57% were exclusively breastfed, whereas the rest typically received breast milk and formula, cow's milk, water or other liquids, and solid or semi‐solid foods. Common foods included dairy (yogourt and cheese), cereals and starches (porridge and bread soaked in tea), vegetables, potatoes, and other white vegetables and tubers. Among children 12–15 months, 89% receive breast milk.
In regard to the introduction of complementary foods, 55% of children aged 6–8 months received ≥1 serving of food in the prior 24 hr, but none received foods from ≥4 food groups. Of 38 index children aged 6–23 months, only 42% met this minimum dietary diversity guideline (30% of those 9–11 months and 68% of those 12–23 months). Common foods were milk, grains, tubers, fruits, and vegetables.
Meal frequency was also inadequate by WHO standards for some children; only 66% received the age‐specific recommended number of feedings. Only 56% of those 6–8 months and 50% of those 9–11 months received age‐specific recommended minimum number of feedings; this improved to 79% for children 12–23 months. When indicators for dietary diversity and meal frequency were combined for the WHO MAD score, 34% of the children 6–23 months met age‐specific criteria, with no infants 6–8 months, and 30% aged 9–11 months and 53% aged 12–23 months having MAD.
3.3. Characteristics associated with dietary diversity
Table 3 explores relationships between socio‐demographic and household characteristics and behaviours, and index child dietary diversity and adequacy and mothers' dietary diversity. Although the study focused intensively on a relatively small number of households, some statistically significant differences are seen, as well as trends to be further explored in larger samples.
For index children 6–23 months, there are no significant differences in dietary diversity or MAD by most maternal and household characteristics, although children in families reporting seasonal food scarcity have a trend towards poorer dietary diversity (P < 0.10). Moreover, children whose mothers report relying on health care providers for feeding advice are less likely to have adequate diversity or MAD scores (P < 0.10).
There was a moderately positive correlation between dietary diversity scores for mothers and children (0.43, P < 0.01; data not shown). For mothers, multiple factors, mostly related to food supply or scarcity at the household and village level, are associated with inadequate dietary diversity. Mothers in households without gardens and livestock are significantly less likely to have MDD‐W scores of 5 or higher (P < 0.05), and those in villages without adequate food access are also less likely to have adequate scores (P < 0.01). Household food insecurity is also strongly associated with poor diversity; women reporting having insufficient food (P < 0.001) and asking others for food (P < 0.05) are more likely to have poor diversity scores. Finally, women who discuss their child's feeding with their mothers‐in‐law are more likely to have adequate dietary diversity themselves.
Figure 2 is helpful to further illustrate the relationship between maternal and index child dietary diversity, among children 6–24 months (n = 36). Adequate dietary diversity for both mother and index child was reported by 37% of households. In only 5% (two households) was the mother's dietary diversity poor, whereas the child had adequate diversity, suggesting that this is a rare occurrence, perhaps due to mother's temporary illness or other unique factors. In the remaining 58%, inadequate dietary diversity was reported for the index child. In most of those instances, the mother's diet was adequate in terms of diversity. In only 11% of households did both mother and child have inadequate diversity. Stated differently, 84% of women with children aged 6–23 months had adequate diversity in their own diet, but in the majority of cases, the diversity of their child's diet was inadequate. Given that there also appears to be an age‐related gradient of adequate diversity shown in Table 2 (0% aged 6–9 months, 30% aged 9–11 months, and 68% 12–23 months), this suggests a phenomenon of “delayed” diversity.
Figure 2.
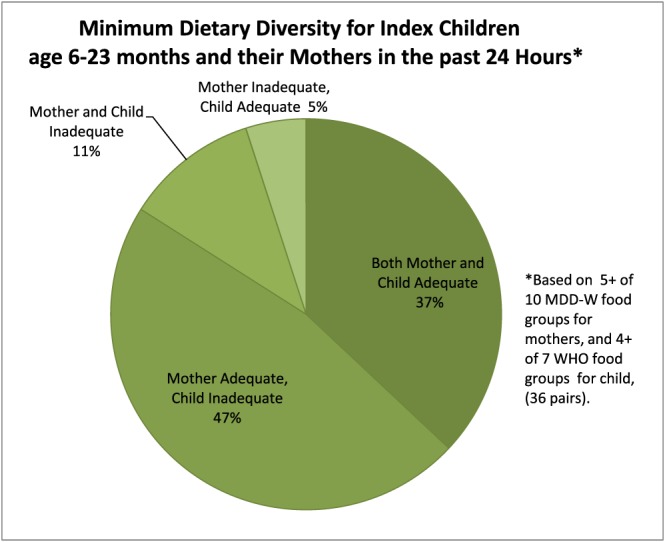
Minimum dietary diversity for index children age 6–23 months and their mothers in the past 24 hr, based on 5+ of 10 MDD‐W food groups for mothers, and 4+ of 7 WHO food groups for child (36 pairs)
3.4. Insights from qualitative data
In order to contextualize delayed dietary diversity, we first present a case study of a typical household, from a rural village in the south‐eastern corner of Sughd. The 9‐month‐old index child was the fourth child of a woman in her thirties, who managed her household, while her university‐educated husband participated in labour migration. After exclusive breastfeeding until 7 months, the mother reports
When she was about 7 months old, I understood she was not getting full from my breast milk, so … I breast feed her 3–4 times in the day, and then I offer her food additionally. Like the bullion with potato puree, things like this, liquid foods. She wakes up 3–4 times per night, she is only breast fed.
The child's 7‐day recall included occasional carrots, egg, and pureed beans and peas, but no meat, fruit, or fruit juice. The mother remarked, when reporting on the lack of fruits in her infant's diet, “we don't have any fruits to eat ourselves!” The mother viewed mashed potatoes, soup from beans, and semolina porridge with cow's milk as healthy first foods.
In this household, food costs and access may compound poor understanding of child dietary diversity, as the mother reported food hardship and household poverty, as well as seasonal scarcity “especially when the roads are frozen in winter.” However, the household gardened and raised livestock and had sufficient food by both observation, and the mother's MDD‐W score of 7. She had good general knowledge and reported substantial access to child nutrition advice, including regular health care and receipt of nutritional supplements (“sprinkles”), educational TV, and advice from her mother, mother‐in‐law, and other village women. As she did all her cooking, she could add more frequent pulses and vegetables, meat, and other foods to child's diet; occasionally purchase or preserve small amounts of fruits or juices; and take other infant‐specific strategies.
3.5. Timing of complementary foods introduction
Data from focus groups with mothers of young children offer further insights. In these groups, a chart displaying age‐specific recommended foods was used to stimulate discussions. Although some respondents knew that introduction of complementary foods should begin as early as 6 months, in general, mothers were more conservative.
I don't feed at all to 8‐month‐old. Maybe some of these girls (other participants) do.
We don't really give them most of the foods here (referring to chart). We mostly feed breast milk.
I myself did not feed my kids until they were a year and a half. After that I started slowly giving porridge and purees. They are only breast fed.
Starting from the 2nd year. (Do you not feed anything else besides breast milk?) We do give them light food such as soup broth, starting at a year and a half.
Two years and up. Above two and two and a half. From the time the baby starts talking and can say “food.”
3.6. Mother–infant motivators and barriers to dietary diversity
When viewed in a behavioural framework, influences on delayed diversity stem from few recognized benefits but also significant perceived barriers to offering infants diverse foods. In terms of benefits, the social/developmental value of feeding was cited more frequently than its nutritional value, with the first birthday an important milestone.
Whatever food we eat, we give of bit to our babies too. The purpose being they should get used to it. We don't give them much, starting around 1 year old, little, little portions so it sits in their behavior.
An additional perceived benefit to complementary foods was child satiety, as mentioned by the case study respondent. Thus, some saw the primary role of complementary foods as addressing inadequate breast milk supply (both before and after 6 months), rather than providing dietary diversity at developmentally appropriate stages.
Participants identified multiple barriers related to child development, digestion, and health. For many women, recommended steps to prepare foods for infants were impractical, and many foods were reserved until children could chew them directly from the family meal. Thus, the most important developmental milestone for complementary feeding was development of teeth.
I don't give plov (pilaf) to my child. How can you feed a one year old with plov? It's still early. It depends on whether the child has teeth or not. We can give carrots from plov if not the rice from plov. Some children have teeth before they are one year old.
Here it shows ground meat (for a one year old). If I find that meat, I would it give it as is, baby would eat it with teeth. We don't have a grinder, and we don't have time to do this.
Chicken is expensive, we don't feed it. Babies can't digest them at 8 months, they have no teeth.
Other food beliefs focused on food textures as well as digestion difficulty, often translated as “hard.”
We boil lentils, so that the taste comes out, and give them the liquid, but not the lentils, because they are hard.
(What don't you give them?) Foods that are heavier. We don't give salad. We don't give rice pilav.
We don't give them cold (foods) so they don't get a cold.
(Why don't you feed chicken to 8 month old babies?) Because it's hard. (What happens if it's hard?) They will have a stomach ache.
Additional foods viewed as difficult for infants to digest included butter and related fried foods, egg whites, salads, and many fresh fruits and vegetables. Some respondents described specific illness episodes blamed on dangerous nature of fresh produce, although one woman recognized that preparation and sanitation played a role.
When my baby used to crawl and ate persimmons from under the tree. Baby started throwing up and … whatever the baby ate, went to the lungs.
We once gave a watermelon to my daughter which led us all the way to the doctor.
And we live in a village where kids might go to the garden and pick a cucumber and eat it without even washing off those chemicals. We should wash and peel then feed those types of things.
In contrast, participants were not aware of IYCF recommendations to avoid cow's milk prior to 9 months (Michaelson et al., 2003) or to avoid other iron‐depleting foods such as black tea. Heavily sweetening foods were seen as a good approach to increasing a food's appeal.
In the mornings place (cow's milk) on the stove and let it boil, boil, boil. Then we throw a candy in it, with bread, and they eat it.
3.7. Additional household and village level barriers
In addition to child development and preparation logistics, diverse foods were not appropriate due to complexity and cost. Especially if items were costly or scarce for adult household members, then it was unnecessary to prioritize their inclusion in infant diets. Equity with older children was also an issue.
She can't give meat (to a 9–11 month old) It is expensive!
I don't have anything to hide to give one and hide from the others.
Cost was tied to village‐level availability as well.
It depends on what the village has; you feed that to the baby.
And of course we feed our babies all the foods here but it depends on their availability. We feed them these when we have those products.
Most participants saw infant foods as a subset of the usual household diet. When asked about buying IYCF foods, what came to mind was formula or other commercial infant foods, rather than healthful common foods.
Very few buy special foods for the kids. They do sell it in the markets, but once we start giving regular food we don't buy them. Few people buy it, but mostly they feed whatever they eat.
Even those recognizing the value of foods from the graphic viewed them as idealized, rather than essential, for development.
(The foods that you mentioned, why do you give them?) Because they are useful, they have vitamins in them. You have to give these things for the development of the baby. (What if you do not have them?) Well then you raise them with Shirchoy (milk with tea) or with cookies.
4. DISCUSSION
The results of our formative research on IFYC feeding in Tajikistan reveal multilevel factors that reduce young children's dietary quality and diversity and may influence the stunting and malnutrition seen in national data. Findings suggest not only specific problematic feeding behaviours but also potential avenues for intervention.
4.1. Maternal knowledge and practices
Although patterns vary widely by region, culture, and economics, many Tajik households build diets around one main cooked meal of stew or soup including starches, vegetables, and meat (as available), with bread and tea. Therefore, an infant's path to complementary foods is understood as gradual introduction of components of this household diet, with early foods limited to broth, followed by mashed starches such as potatoes. Similarly, because sweetened tea and bread or cookies are common elements across the day, infants are offered these as first foods.
Within this restricted adult diet, IYCF diversity is further challenged because many foods, as prepared for adults, are withheld due to concerns such as texture. Therefore, available foods offering nutrients for infants, including meats and vegetables, are avoided due to their “hard” consistency and belief that they are too difficult to digest.
Children's diets appear to be rarely planned, and few households purchase foods exclusively for them (e.g., fortified baby cereals). IYCF food purchases are often limited to formula, which is used as a supplemental food, even when a child is breastfed. Use of liquids other than breast milk reduces thirst, and sweetened liquids add calories, reducing both hunger and thirst and jeopardizing infants' demand for, and production of, breast milk. Cow's milk is not recommended by WHO before 9 months, (Michaelson, 2003) in part because it interferes with iron absorption, and black tea can reduce iron absorption from plant‐based sources. Thus, anaemia, for example, may have dual causes if a child's early diet contains harmful components, such as black tea and cow's milk, but is also slow to include diverse iron‐rich foods.
We found that 81% of infants with inadequate diets live in households with sufficient food to provide a minimally diverse diet for adults. In these homes, nutrition education strategies should focus on accelerating introduction of specifically prepared versions of diverse household‐available foods and procuring small amounts of foods especially for IYCF.
However, the positive correlation between mother and child diversity suggests that economics may influence behaviours in all households. Diversifying infants' diet may be economically feasible for most families, and most mothers, when asked about hypothetical shortage, prioritized children's needs. However, especially in larger households with many children and multiple food decision‐makers, modifying household‐level practices to prioritize foods for infants over others may be less successful than addressing overall household dietary diversity and improving nutritional status for all family members. In addition to educating mothers about “why” a high‐quality, diverse diet (rather than simple satiety) is critical in IYCF, education could focus on “how” to economically diversify diets, by increasing use of nonmeat proteins and Vitamin A‐rich vegetables, as well as food storage or preservation methods to overcome seasonal scarcity.
4.2. Household dynamics
There are multiple actors involved in procuring, preparing, and offering foods to infants and young children in Tajik households, and therefore, behaviour change efforts must be strategically designed to reach a range of audiences. In typical households, mothers‐in‐law play key roles as meal planners, and fathers‐in‐law are often involved in purchasing foods. Fathers of young children often have views on child feeding as well. Women's own mothers, although not always living nearby, have considerable influence as sources of information and advice. All of these persons appear to be key influencers (and intervention targets) for IYCF behaviours. For example, given the central role of the man in Islamic culture, and important family‐related teachings transferred from religious leaders to older and younger men, strategies for improving child nutrition at the household level could use these gender‐specific channels.
School‐age children also represent an untapped communication channel into homes. Several sources reported a lack of nutrition and health education curriculum in schools. This is an important area for multisectoral partnership, given the importance of schools to bring new information into homes and families. As well, the growing burden of overweight and obesity in Tajikistan underscores the need for school‐age children to understand healthy food choices.
4.3. Village
Public health interventions promoting dietary diversity will have limited impact unless they are nested within an ecological approach addressing food access, availability, and price. Although major towns have large bazaars, rural villages typically only have small stores with limited offerings, especially during winter and early spring. Families with transportation can access larger markets with favourable pricing and variety; thus, poor families are doubly disadvantaged, as they pay higher prices for limited foods at village stores. Policies aimed at supporting and improving healthful food access and affordability in smaller village shops could improve dietary diversity among all households and especially address access barriers experienced by lower income families (Global Panel on Agriculture and Food Systems for Nutrition, 2014).
The village food environment is also a key location for behaviour change opportunities. Similar to “baby‐friendly” birth setting campaigns promoting breastfeeding (World Health Organization & UNICEF, 2009), partnerships between nutrition, health, and economic sectors could assist remote village stores with creating “nutrition friendly” point‐of‐purchase educational and promotional campaigns with signage and pricing, strategies proven widely effective across cultures and settings (Hartmann‐Boyce et al., 2018; Liu, Stephenson, Houlihan, & Gustafson, 2017). Given the extreme scarcity of key foods in some villages, even a modest increase in accessibility and appeal of healthful foods offers important return on investment. If nutrition sector stakeholders provided campaigns with free signage and educational advertising, with pictures to reduce reading burden, this might encourage shopkeepers to prominently display healthful foods, rather than soft drinks, snack foods, or currently marketed “western” foods.
It is also worth investigating whether village shopkeepers and food suppliers could play a health advocate role to promote infant feeding behaviours. We also saw evidence that women seeking nutritional advice from health care providers were significantly less likely to report infant MAD, but because our data are cross‐sectional, we cannot determine if this negative association indicates that providers are unsuccessful at improving behaviour, or if perhaps women facing IYCF barriers are more actively seeking guidance. Overall, this supports the value of broader interventions aimed at all community influences on IYCF. In terms of mass communication, television has potential as a highly influential medium, as most mothers reported learning child advice on television. Unfortunately, radio was rarely used, reducing its utility as a low‐cost medium for behaviour change communication.
4.4. Limitations and priorities for future research
These formative research findings do not provide conclusive answers but rather identify promising areas and questions for future exploration. The strategic sample of villages was broadly representative of Tajikistan's diversity geography, climate, and cultures but was not intended for between‐region comparisons. Late spring was chosen to capture the most food‐insecure time for rural households, prior to growing season, when winter food stores may be depleted and household funds are absorbed by seasonal costs for planting, but findings would likely vary by season.
Additionally, because of tremendous scope of topics of interest, not all areas could be fully explored (despite the large quantity of data collected). Respondents were generous with their time and energy, but participant time burden, especially for young mothers, was substantial. During home visits, households tolerated multiple data collectors inspecting food stores and sanitation areas and observing cooking and meals. The private nature of home life, and sensitive issues involved in child‐rearing, household relationships, and economic insecurity, further increased burden. Although informed consent and ethical training reduced coercion, and participants were generally open with responses, findings may be conservative in capturing negative attitudes, beliefs, or practices. Finally, although well‐validated methods for dietary recall collection were used, and 24‐hr recalls are generally known to be less subject to inaccuracies than recalls based on longer periods of time, there is still the possibility of bias in 24‐hr recall data (National Cancer Institute, 2018).
However, despite the modest sample size, findings are similar to patterns seen in the 2012 Tajikistan DHS (e.g., 55% vs. 49% rates of complementary food introduction) and other large analyses (Lavado, Seitz, & Thiebaud, 2017), strengthening the utility of these findings for expanding the limited peer‐reviewed evidence base regarding IYCF in rural Central Asian societies. More broadly, the mixed‐methods design and results provide tools to inform possible IYCF research approaches, which have been predominantly separating strands of either structured DHS‐based analyses or qualitative work (e.g., Campbell et al., 2018; Hackett, Mukta, Jalal, & Sellen, 2015). Many areas for intervention were identified, as well as specific topics for additional research. For example, for previously unrecognized beliefs or behaviours identified in this qualitative research, structured questions in broader surveys could determine their prevalence more widely, or their correlates in specific regions or subgroups.
5. CONCLUSIONS
This work highlights not only challenges but also positive elements of the infant and young child nutrition situation in Tajikistan. Although severely challenged by both economic hardships and lack of detailed nutrition knowledge, many families highly valued the health of their mothers and young children. Thus, there are many positive aspects of family support and cultural values regarding IYCF that can be leveraged for behaviour change. However, extensive education appears necessary to expand the prevalent understanding of IYCF needs, beyond satisfying immediate demands of perceived hunger or thirst, to meeting age‐specific nutritional recommendations.
Successful behaviour change depends on new behaviours being feasible within household and village food environments. Some households and villages are clearly limited by food scarcity due to poverty and food distribution issues. Strategies that emphasize small, economically feasible changes to children's diets may be the most successful in further reducing stunting and malnutrition.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
ACK led the design of the data collection activities and instruments, together with BJM and BL. Data collector training for field work was co‐led by ACK and BJM, together with SG, CC, RA, YS, and SA. YS and SA led the conceptualization and planning of the research, and coordinated all in‐country aspects of the sample development and recruitment, data collection and transmittal. RA, MI and JM translated and interpreted instruments, audio‐recordings, and other forms of data. LB led the literature review, management of data, and preparation of final products and reports. AK led the writing of the manuscript, with all authors reviewing and approving the manuscript in final form.
ACKNOWLEDGMENTS
The authors acknowledge the contributions of the individuals and households who participated in the study, and generously provided their time and insights. We also thank the Tajikistan Ministry of Health and Social Protection, and its staff, for assisting in study design, data collection, and logistics. Funding for the research was provided by UNICEF Tajikistan, under a long‐term agreement for services with Drexel University. Dr. Maqsood was supported by the Fulbright Foreign Student Program.
Klassen AC, Milliron BJ, Suehiro Y, et al. “Then you raise them with Shirchoy or cookies”: Understanding influences on delayed dietary diversity among children in Tajikistan. Matern Child Nutr. 2019;15:e12694 10.1111/mcn.12694
REFERENCES
- Begin, F. , & Aguayo, V. M. (2017). First foods: Why improving young children's diets matter. Maternal & Child Nutrition, 13(S2), e12528 10.1111/mcn.12528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1992). Ecological systems theory In Vasta R. (Ed.), Six theories of child development: Revised formulations and current issues. London, England: Jessica Kingsley Publishers. [Google Scholar]
- Byker Shanks, C. , Jilcott Pitts, S. , & Gustafson, A. (2015). Development and validation of a farmers' market audit tool in rural and urban communities. Health Promotion Practice, 16(6), 859–866. 10.1177/1524839915597899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, R. K. , Aguayo, V. , Kang, Y. , Dzed, L. , Joshi, V. , Waid, J. , … West, K. P. Jr. (2018). Infant and young child feeding practices and nutritional status in Bhutan. Maternal & Child Nutrition, 14(3), e12580 10.1111/mcn.12580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell, J. , Klassen, A. C. , Plano‐Clark, V. , & Smith, K. C. (2011). Best practices for mixed methods research in the health sciences. Bethesda: Office of behavioral and social sciences In National institutes of health. [Google Scholar]
- FAO and FHI360 (2016). Minimum dietary diversity for women: A guide to measurement. Rome: FAO. [Google Scholar]
- Global Panel on Agriculture and Food Systems for Nutrition (2014). How can agriculture and food system policies improve nutrition? In Technical brief. London, UK: Global Panel on Agriculture and Food Systems for Nutrition. [Google Scholar]
- Hackett, K. M. , Mukta, U. S. , Jalal, C. S. , & Sellen, D. W. (2015). Knowledge, attitudes and perceptions on infant and young child nutrition and feeding among adolescent girls and young mothers in rural Bangladesh. Maternal & Child Nutrition, 11(2), 173–189. 10.1111/mcn.12007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann‐Boyce, J. , Bianchi, F. , Piernas, C. , Riches, S. P. , Frie, K. , Nourse, R. , & Jebb, S. A. (2018). Grocery store interventions to change food purchasing behaviors: A systematic review of randomized controlled trials. The American Journal of Clinical Nutrition, 107(6), 1004–1016. 10.1093/ajcn/nqy045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasevec, J. , An, X. , Kumapley, R. , Begin, F. , & Frongillo, E. A. (2017). Diet quality and risk of stunting among infants and young children in low‐ and middle‐income countries. Maternal & Child Nutrition, 13(S2), e12430 10.1111/mcn.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs‐Smith, S. M. , Smiciklas‐Wright, H. , Guthrie, H. A. , & Krebs‐Smith, J. (1987). The effects of variety in food choices on dietary quality. Journal of the American Dietetic Association, 87(7), 897–903. [PubMed] [Google Scholar]
- Lavado, R. , Seitz, W. , & Thiebaud, A. (2017). Childhood stunting in Tajikistan: Quantifying the association with wash In Food security, health and care practices. Washington, D.C.: World Bank Group. [Google Scholar]
- Liu, E. , Stephenson, T. , Houlihan, J. , & Gustafson, A. (2017). Marketing strategies to encourage rural residents of high‐obesity counties to buy fruits and vegetables in grocery stores. Preventing Chronic Disease, 14, 170109 10.5888/pcd14.170109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayen, A. L. , Mestral, C. D. , Zamora, G. , Paccaud, F. , Marques‐Vidal, P. , Bovet, P. , & Stringhini, S. (2016). Interventions promoting healthy eating as a tool for reducing social inequalities in diet in low‐ and middle‐income countries: A systematic review. International Journal for Equity in Health, 15(2), 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaelson, K. F. , Weaver, L. , Branca, F. , & Robertson, A. (2003). Feeding and nutrition of infants and young children. Guidelines for the WHO European Region, with emphasis on the former Soviet countries. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Ministry of Health Republic of Tajikistan (2018). Micronutrient status survey in Tajikistan, 2016. Dushanbe: Ministry of Health. [Google Scholar]
- National Cancer Institute . Dietary assessment primer. 2018. (https://dietassessmentprimer.cancer.gov/) [Accessed on: July 19, 2018].
- Ruel, M. T. (2003). Operationalizing dietary diversity: A review of measurement issues and research priorities. The Journal of Nutrition, 133, 3911S–3926S. 10.1093/jn/133.11.3911S [DOI] [PubMed] [Google Scholar]
- Sallis, J. F. , Owen, N. , & Fisher, E. B. (2008). Ecological models of health behavior. Health Behavior and Health Education: Theory, Research, and Practice, 4, 465–486. [Google Scholar]
- Sanghvi, T. , Seider, R. , Baker, J. , & Jimerson, A. (2017). Using behavior change approaches to improve complementary feeding practices. Maternal & Child Nutrition, 13(S2), e12406 10.1111/mcn.12406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistical Agency under the President of the Republic of Tajikistan [SA], Ministry of Health [Tajikistan], and ICF International (2013). Tajikistan demographic and healthy survey 2012. Dushanbe, Tajikistan, and Calverton, Maryland, USA: SA, MOH, and ICF International. [Google Scholar]
- World Health Organization (WHO 1) . (2008). Indicators for assessing infant and young child feeding practices, part 1: Definition. Geneva, Switzerland.
- World Health Organization, UNICEF . (2009) Baby‐friendly hospital initiative. Revised, updated and expanded for integrated care. Geneva, Switzerland. [PubMed] [Google Scholar]


