Abstract
Purpose: The increase in cost-sharing between patients and payers has resulted in financial toxicity in cancer patients, particularly among young adult (YA) patients and survivors (<40 years of age). This study explored financial toxicity and its impact on psychological well-being, self-efficacy for coping with cancer, and cost-coping behaviors among a sample of YA cancer patients and survivors.
Methods: One hundred forty YAs completed an anonymous online survey. The Comprehensive Score for Financial Toxicity measured financial toxicity and the Cancer Behavior Inventory–Brief measured coping self-efficacy. The Patient Health Questionnaire-4 and items from the Impact of Cancer–Young Adult and the Cancer Needs Questionnaire–Young People assessed psychological well-being. A single item assessed cost-coping behaviors (i.e., skipping or delaying treatment because of its cost). Analyses included Pearson and Spearman correlation matrices and multivariate regression modeling.
Results: Worse financial toxicity was associated with lower insurance satisfaction (r = 0.52, p < 0.001), higher levels of depressive and anxiety symptoms (r = −0.42, p < 0.001), greater worry (p < 0.001), and lower self-efficacy in coping with cancer (i.e., maintaining independence and a positive attitude, r = 0.41, p < 0.001; coping and stress management, r = 0.43, p < 0.001; and managing negative effect, r = 0.20, p = 0.02). In multivariate modeling, financial toxicity related to skipping or delaying treatment and greater anxiety and depression symptomology, controlling for relevant covariates.
Conclusion: The findings suggest financial toxicity negatively impacts many facets of the YA cancer experience. There is a need to address the cost of cancer care with patients to ensure they are informed about the financial implications of treatment decisions and to support financial planning as needed.
Keywords: financial toxicity, mental health, survivorship, cost-coping behaviors
Introduction
The increase in cost-sharing between patients and payers, as seen in higher deductibles, co-insurance, co-payments, and general out-of-pocket spending requirements, has resulted in greater financial burden for patients. Combined with higher costs of medication and treatment and the potential for diminished work productivity (and subsequent loss of income), this shift in payment structure yields a unique stress, known as financial toxicity, for many cancer patients.1 Financial toxicity refers to the economic distress and burden that result from cancer treatment and its related costs.
Patient experience of cancer-related financial toxicity is widespread. A recent systematic review showed that nearly half (49%) of cancer patients experience financial toxicity, while other measures suggest up to 73% of patients experience some form of negative financial consequences as a result of their cancer.2,3 Financial toxicity is also incursive: an estimated 42% of newly diagnosed cancer patients have depleted their life savings within 2 years of diagnosis,4 and cancer patients are 2.65 times more likely to declare bankruptcy than noncancer patients, with 12%–62% reporting they are in debt because of their cancer care.3,5 Patients experiencing financial toxicity often engage in cost-coping strategies, such as skipping or delaying care or medication and forgoing mental health care,1,6 and those who face unexpected costs related to treatment are less likely to be willing and able to pay for future cancer care.7
Young adult (YA) patients and survivors (<40 years of age) are particularly susceptible to financial toxicity, as their disease and treatment may disrupt key developmental transitions that, in turn, limit their ability to complete education/training, delay or alter workforce entry and career advancement, and diminish financial well-being.8,9 YA survivors have higher out-of-pocket medical expenses,8 are more likely to be unable to afford medication,10 and experience more difficulty maintaining work/school productivity9 than their healthy peers. The risk for bankruptcy in young cancer patients is 2–5 times higher compared with older adult patients.5
While there is an emergence of literature quantifying the extent of financial effects among YAs affected by cancer, there is limited research on the psychosocial impact, despite indications of negative effects in older populations.11–16 This study explored the prevalence and predictors of self-reported financial toxicity among YA cancer patients and survivors, and its impact on psychological well-being, self-efficacy for coping with cancer (confidence or belief in one's ability to cope with cancer), and cost-coping behaviors.
Methods
This study was approved as exempt research by an Institutional Review Board committee.
Data and patients
Data were collected as part of organizational activities of two patient organizations (Stupid Cancer and GRYT Health) to understand unmet needs of the YA patient community and inform program development, based on prior models for evaluating YA-specific cancer events run by patient organizations.17 Recruitment emails were sent to all registered attendees of a patient educational and social networking conference, inviting participation in the survey study 1 week before the event. The survey was administered using a secure, Health Insurance Portability and Accountability Act-compliant online platform, and respondents completed all survey items at one time.
Measures
Financial and insurance information
Financial toxicity was measured using the Comprehensive Score for Financial Toxicity (COST), an 11-item measure of financial distress in cancer patients.18 Respondents rate agreement on a five-point scale (from “not at all” to “very much”), and items are summed to create a single composite score, with lower scores representing worse financial outcomes as a result of cancer (greater financial toxicity). The COST assesses both the out-of-pocket expenses associated with cancer care and indirect costs, including loss of income and changes in employment. Recent work has shown the COST to be a valid and reliable measure of a clinically relevant patient-reported outcome, and in this sample, the tool showed excellent internal consistency (α = 0.90).11
Three additional items assessed perceptions of health insurance coverage: “My health insurance coverage meets my needs” (reverse coded); “I am confused about my health insurance or the insurance options available to me”; and “I am satisfied with my health insurance” (reverse coded). Answers were on a four-point Likert scale from “strongly disagree” to “strongly agree.” Items were averaged, with higher scores indicating greater concern about insurance (lower satisfaction). In this sample, internal consistency was acceptable (α = 0.76).
Psychological well-being
Assessment of psychological well-being included measures of anxiety, depression, and worry. The Patient Health Questionnaire-4 (PHQ-4) is a brief, valid four-item assessment of depressive and anxiety sysmptoms.19,20 Answers were on a four-point scale from “not at all” to “nearly every day,” with higher scores indicating higher symptomatology. Previous validation of the PHQ-4 in an online format found acceptable internal consistency for the overall tool (α = 0.83).20 Four items from the Impact of Cancer–Young Adult and the Cancer Needs Questionnaire–Young People were adapted to assess worry related to different aspects of life after cancer.21,22 Respondents rated, on a four-point Likert scale, their level of agreement with the following: “When I think about my cancer, I feel anxiety or nervousness”; “I worry about my health”; “I worry about how my cancer has affected other people in my life”; and “I worry about how my cancer affects (or will affect) my ability to do well in my job and my ability to pursue the career I want.” Higher rankings indicated higher levels of worry.
Coping self-efficacy
The Cancer Behavior Inventory–Brief is a 12-item measure of survivors' self-efficacy for coping with cancer, answered on a 0–10 scale from “not confident at all” to “totally confident I can or would be able to do this.”23,24 Domains included ability to maintain independence and a positive attitude, confidence in participating in medical care, coping and stress management, and confidence in one's ability to manage negative effect. In this sample, internal consistency for the overall tool was 0.90, with domain consistency scores ranging from 0.72 to 0.87.
Cost-coping behavior
A single item assessed whether patients ever skipped or delayed cancer care or treatment because of financial reasons (yes/no).
Statistical analysis
We used independent sample t tests and analysis of variance to examine bivariate associations between financial toxicity and demographic/clinical characteristics. A correlation matrix was generated to assess the relationship between financial toxicity and psychological and behavioral outcomes (Pearson and Spearman tests). The impact of financial toxicity on cost-coping behaviors (i.e., skipping or delaying care because of financial reasons) and psychological well-being was tested in multivariate logistic models, controlling for significant demographic and clinical variables and insurance satisfaction (for cost-coping model only).
Results
Sample
The survey was emailed to 383 YA cancer survivors; 181 clicked the link to enter the survey and 142 had complete data (response rate = 37%). Patients (n = 2) older than 40 at diagnosis were excluded, yielding a final sample of 140. Due to the anonymous nature of the survey, information on nonresponders could not be collected, and we were unable to compare responders with nonresponders.
Mean age at the time of the survey was 31.3 years (standard deviation [SD] = 6.5; range 19–50) and mean age at diagnosis was 24.5 years (SD = 8.2; range 3–40); 57.9% had completed treatment. The majority of the sample was female (79.3%), white (80.0%), non-Hispanic (82.1%), and at least a college graduate (76.5%). Most survey respondents were employed (69.3%) and 57.9% had employer-provided health insurance. Lymphoma was the most common diagnosis (30.0%) in the sample (Table 1).
Table 1.
Respondent Demographics and Clinical Characteristics
| Mean | SD | Range | |
|---|---|---|---|
| Age in years at diagnosis | 24.6 | 8.2 | 3–40 |
| Age in years at survey | 31.3 | 6.5 | 19–50 |
| N | % | ||
| Gender | |||
| Female | 111 | 79 | |
| Male | 21 | 15 | |
| Transgender/nonbinary | 2 | 1 | |
| Missing | 8 | 4 | |
| Race | |||
| White | 112 | 80 | |
| Asian | 8 | 6 | |
| Black | 4 | 3 | |
| More than one race | 5 | 4 | |
| Prefer not to say | 4 | 3 | |
| Missing | 6 | 4 | |
| Ethnicity | |||
| Non-Hispanic/Latinx | 115 | 82 | |
| Hispanic/Latinx | 10 | 7 | |
| Prefer not to say | 6 | 4 | |
| Missing | 9 | 6 | |
| Education | |||
| High school/vocational/some college | 27 | 19 | |
| College degree | 53 | 38 | |
| Postgraduate degree | 54 | 39 | |
| Missing | 6 | 4 | |
| Diagnosis | |||
| Leukemia | 19 | 14 | |
| Lymphoma | 42 | 30 | |
| Breast cancer | 17 | 12 | |
| Sarcoma | 13 | 9 | |
| Other | 41 | 29 | |
| Missing | 8 | 6 | |
| Employment status | |||
| Employed | 97 | 69 | |
| Not employed | 36 | 26 | |
| Missing | 7 | 5 | |
| Health insurance | |||
| Employer based | 81 | 58 | |
| Privately funded | 19 | 14 | |
| Publicly funded | 29 | 21 | |
| No insurance | 5 | 4 | |
| Missing | 6 | 4 | |
| Treatment status | |||
| Completed treatment | 81 | 58 | |
| In treatment | 13 | 9 | |
| Ongoing therapies (hormonal, etc.) | 25 | 18 | |
| Treated a chronic disease | 11 | 8 | |
| Not yet started | 2 | 1 | |
| Missing | 10 | 7 | |
SD, standard deviation.
Financial toxicity
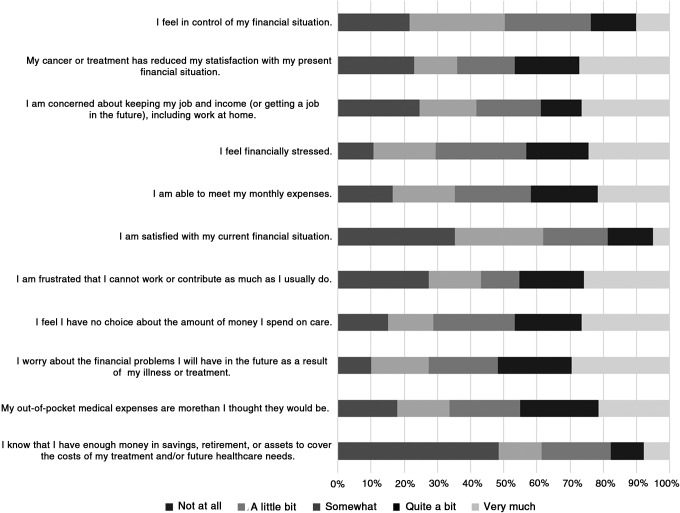
COST scores ranged from 0 to 42 (possible range = 0–44), with a mean of 18.8 (SD = 10.8) and median of 19.0, indicating worse financial outcomes than published in the literature of other cancer groups (e.g., M = 22.5, SD = 11.3; median = 21).18 Scores were normally distributed (K-S = 0.069, df = 139, p = 0.20). At the item level, 71% of respondents reported feeling financially stressed (25% “very much” so), and 73% were worried about the financial problems they will have in the future as a result of their illness (30% “very much” so). Only 18% felt they had enough money in savings, retirement, or assets to cover the costs of their treatment and/or future health care needs (Fig. 1).
FIG. 1.
Item-level Comprehensive Score for Financial Toxicity responses.
Respondents who were unemployed (t[130] = 2.4, p = 0.02), had public health insurance (F[3,129] = 4.3, p < 0.01), did not have a college degree (t[131] = 2.3, p = 0.02), and were still being treated for cancer (i.e., active treatment, ongoing maintenance therapy, or chronic disease; t[127] = 2.2, p = 0.03) reported greater financial toxicity than their counterparts. Worse financial toxicity was associated with lower insurance satisfaction (r = −0.52, p < 0.001). Sarcoma patients had worse financial toxicity than leukemia patients (p = 0.01), but there were no other significant difference in COST scores between diagnostic groups. Current age, age at diagnosis, race, ethnicity, relationship status, and gender were not associated with COST scores (all p's > 0.05).
Financial toxicity and psychological well-being
Worse financial toxicity was associated with higher levels of depressive and anxiety symptoms (r = −0.42, p < 0.001), and greater cancer-related worry across all items assessed (all p's < 0.05) (Table 2).
Table 2.
Correlation with Comprehensive Score for Financial Toxicity
| Worry | Self-efficacy | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| PHQ-4 | When I think about my cancer, I feel anxiety or nervousness | About health | About how my cancer has affected other people in my life | About how my cancer affects my ability to do well in my job and my ability to pursue the career I want | Maintaining independence and a positive attitude | Coping and stress management | Participating in medical care | Managing negative affect | |
| N | 138 | 131 | 135 | 134 | 126 | 123 | 109 | 132 | 122 |
| r/ρa | −0.42** | −0.41** | −0.40** | −0.27* | −0.56** | 0.40** | 0.43** | 0.14 | 0.20* |
Pearson r correlation coefficient used for interval-level responses; Spearman ρ correlation coefficient used for ordinal-level responses.
p < 0.05.
p < 0.001.
PHQ-4, Patient Health Questionnaire-4.
Financial toxicity and coping self-efficacy
Greater financial toxicity was related to lower confidence in managing cancer-related issues across the domains of maintaining independence and a positive attitude (r = 0.41, p < 0.001), coping and stress management (r = 0.43, p < 0.001), and managing negative affect (r = 0.20, p = 0.02). Financial toxicity was not associated with confidence in taking an active role in one's medical care (r = 0.14, p = 0.11) (Table 2).
Financial toxicity and cost-coping behaviors
Seventeen percent of respondents reported skipping or delaying cancer care or treatment because of financial reasons. This behavior correlated with experiencing greater financial toxicity as a result of cancer (M = 20.5, SD = 10.6), compared to those in the sample who did not engage in cost-coping strategies (M = 10.9, SD = 10.7.6; t[137] = 4.2, p < 0.001). Respondents who skipped or delayed care because of financial reasons also had lower satisfaction with their insurance (t[123] = 2.7, p = 0.007).
Multivariate modeling
Controlling for education, employment status, treatment status, and insurance satisfaction, financial toxicity predicted likelihood of using cost-coping strategies, with a one-point decrease in COST scores (worse financial outcome) yielding a 9% increase in the odds of skipping or delaying treatment (Wald[1] = 6.03, p = 0.01, 95% confidence interval eβ: 0.85–0.98). Financial toxicity was also predictive of depressive and anxiety symptoms, above and beyond the same covariates (β = −0.12, t[123] = −4.8, p < 0.001). The model explained a significant proportion of the variation in anxiety and depression scores (R2 = 0.18, F[4,123] = 7.1, p < 0.001).
Discussion
This survey found that financial toxicity has a negative association with many facets of the YA cancer experience, including survivors' psychological well-being and confidence in coping with cancer. Financial toxicity also correlated with cost-coping strategies such that those experiencing more negative financial effects due to cancer were more likely to skip or delay treatment and care.
Zafar and Abernethy25,26 and Gordon et al.,2 Yabroff et al.,27 and Sharp et al.28 characterized financial toxicity as being both objective and subjective in nature, and these experiences are illustrated in our findings. The objective experience of financial toxicity refers to the financial burden that can be measured (e.g., out-of-pocket dollars spent, percent of income spent on health care, and lost wages), while subjective experiences relate to the impact on psychosocial well-being and quality of life and include patient decisions about treatment, medication adherence, and other cost-coping practices (e.g., forgoing nutrition or not paying bills to afford treatment).25,26 Importantly, this subjective experience of financial toxicity can have a significant and snowballing effect on survivors' adjustment after a cancer diagnosis, including into long-term survivorship. In our sample, financial toxicity was shown to have a negative relationship with YA survivors' confidence in their ability to maintain independence and normal activities, cope with physical changes relating to their disease, and manage negative effect. Experiencing financial toxicity increased the likelihood of respondents choosing to delay or skip treatment because of financial reasons and was related to negative psychological well-being, including increased depressive and anxiety symptoms and cancer-related worry. Findings are consistent with the limited literature of the psychosocial and quality-of-life impact of financial toxicity in other cancer groups.29,30
There is a clear need to address the cost of cancer care with patients to ensure they are informed about the financial implications of treatment decisions and to support financial planning, as needed. This is particularly true for YA patients who are at greater risk of financial stress following cancer compared to older patients, while also having less financial knowledge, capability, and management skills.31,32 The American Society for Clinical Oncology recommended oncologists integrate cost-considerations into their treatment plans and address financial issues directly with patients, viewing these discussions as a key component of quality care.33 Presently though, evidence suggests such discussions are limited, and there is discord between patient and provider perceptions of cost communication.34,35 Irwin et al. found that while 94% of their sample of 134 breast cancer patients expected that oncologists would discuss costs of care, only 14% reported having a discussion with their providers.36 Another evaluation of oncologist-patient conversations across 677 visits revealed that the topic of treatment costs only occurred in 22% of visits and had a median duration of 33 seconds, which were initiated by patients 41% of the time.37 In these conversations, cost-lowering strategies were discussed 38% of the time and included discussions about switching to lower-cost therapy/diagnostic test, changing logistics of the intervention, and facilitating copay assistance.37
Notably, patients have reported a preference to have discussions with financial counselors, as opposed to physicians, social workers, or nurses38; and many are interested in education to improve their financial literacy.39 This may be especially important for YAs, who may have limited prior experience with financial decision making and planning. Financial toxicity interventions have used financial counselors, patient navigators, and social workers to deliver support, along with the use of support groups and transportation vouchers.40
Yezefski et al. provided financial navigation training to staff at hospitals and cancer care clinics and demonstrated a reduction in patient out-of-pocket spending and reduced institution financial losses.41 Shankaran et al. partnered with the Consumer Education and Training Services (www.centsprogram.org) and the Patient Advocate Foundation (www.paf.org) to develop a patient-centered financial education and counseling intervention, including assistance with budgeting, retirement planning, and managing medical bills; the program showed decreases in anxiety about cancer-related costs over a 6-month period.42
Recent work has focused on web-based and smartphone applications designed to provide patients with tailored financial assistance or connect them with existing financial assistance programs specific to their needs. Pilot testing has indicated high usability and acceptability of these digital platforms, with preliminary success in matching patients with appropriate resources.43,44 Other intervention-based research has explored decision-making aids and support services for selecting insurance plans and the efficacy of patient financial assistance programs for prescription drugs, with both showing modest promise.45–47
None of the aforementioned interventions addressed the unique needs of YA patients and survivors, although YAs have expressed interest in such targeted programming.48 Patient-centered interventions must incorporate preferences and feedback from the target population to guide intervention design and content (e.g., language used and topics covered). When designing interventions for YAs, it is important for researchers to consider the developmental age of the targeted audience, including their development of financial capability and how their concerns relate to life stage tasks (e.g., impact of late and long-term treatment effects on YAs' ability to attend school or work). Topics of particular relevance to a YA audience may include accessing and funding higher education; managing student loans, credit cards, and medical debt; financing family building and fertility challenges; navigating and selecting insurance plans; saving money for home, car, and other large purchases; applying for disability benefits, supplemental nutrition assistance, and other forms of government assistance; and understanding the indirect costs of cancer and the impact of cancer on mental health. YAs also have different levels of financial knowledge, experience, skill, and behaviors than older adults and may benefit from targeted educational and skills building intervention components.
Although our sample averaged worse financial toxicity than previously reported in the literature18 and over 80% felt they did not have enough money in savings, retirement, or assets to cover the costs of their treatment, only 17% of the sample reported skipping or delaying treatment as a result of financial distress. This juxtaposition in findings is likely multifactorial in nature. It may reflect respondents' insurance coverage such that most had enough coverage to pay their medical bills, despite experiencing other financial toxicity effects. Respondents' assessment of financial toxicity may have related to issues other than their ability to pay for treatment and/or reflected a prioritization of health over other competing financial pressures. We did not assess if other sacrifices were made as a result of paying treatment costs or if there were related ramifications such as job lock (the inability to freely leave a job for fear of losing benefits such as health care).
This study is limited by the lack of gender, racial/ethnic, and educational diversity in the sample, which limits generalizability. Notably, the sample was highly educated, suggesting that results may have underestimated the extent of financial toxicity in YAs' with lower educational attainment and earning potential. The diversity of diagnoses in the sample prevented meaningful analysis of the impact of diagnosis or treatment on financial toxicity, and future work should identify specific patient subgroups at increased risk for high treatment costs. Because the survey was anonymous, we were unable to compare responders to nonresponders. Our response rate of 37% is also lower than we had expected, but comparable to that reported in the literature of emailed online cancer survey studies.49,50 Due to the cross-sectional design, we were unable to make inferences about causality or explore temporal relationships between financial toxicity and outcomes of interest, and we did not collect data on patient's objective experience of financial toxicity (e.g., measuring income or estimating annual health care costs). Despite these limitations, understanding the impact of financial toxicity in this underserved patient population is critical to improve comprehensive cancer care services.
Future research should examine financial relationships in larger, more diverse samples of YAs, with more specific assessment of patients' financial knowledge, priorities, and decision-making processes; strategies to manage medical expenses amidst other financial pressures; and support needs with respect to budgeting and financial planning. It would be useful to evaluate how YA patients may use and benefit from existing evidence-based resources and interventions, or how to best adapt them for the unique needs of the YA cancer population.
Acknowledgment
This article was funded, in part, through the NIH/NCI Cancer Center Support Grant P30 CA008748. The authors thank Stupid Cancer and GRYT Health for their collaboration in data collection. Neither Stupid Cancer nor GRYT Health was involved in data analysis, and they did not influence findings in any way.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient's experience. Oncologist. 2013;18(4):381–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gordon LG, Merollini KM, Lowe A, Chan RJ. A systematic review of financial toxicity among cancer survivors: we can't pay the co-pay. Patient. 2017;10(3):295–309 [DOI] [PubMed] [Google Scholar]
- 3. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109(2):pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or debt? National estimates of financial toxicity in persons with newly-diagnosed cancer. Am J Med. 2018;131(10):1187–99.e5 [DOI] [PubMed] [Google Scholar]
- 5. Ramsey S, Blough D, Kirchhoff A, et al. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood). 2013;32(6):1143–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Knight TG, Deal AM, Dusetzina SB, et al. Financial toxicity in adults with cancer: adverse outcomes and noncompliance. J Oncol Pract. 2018:Jop1800120 [DOI] [PubMed] [Google Scholar]
- 7. Chino F, Peppercorn JM, Rushing C, et al. Out-of-pocket costs, financial distress, and underinsurance in cancer care. JAMA Oncol. 2017;3(11):1582–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guy GP, Jr, Yabroff KR, Ekwueme DU, et al. Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Aff (Millwood). 2014;33(6):1024–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaul S, Avila JC, Mehta HB, et al. Cost-related medication nonadherence among adolescent and young adult cancer survivors. Cancer. 2017;123(14):2726–34 [DOI] [PubMed] [Google Scholar]
- 11. de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer. 2017;123(3):476–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Delgado-Guay M, Ferrer J, Rieber AG, et al. Financial distress and its associations with physical and emotional symptoms and quality of life among advanced cancer patients. Oncologist. 2015;20(9):1092–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors' quality of life. J Oncol Pract. 2014;10(5):332–8 [DOI] [PubMed] [Google Scholar]
- 14. Jones SMW, Walker R, Fujii M, et al. Financial difficulty, worry about affording care, and benefit finding in long-term survivors of cancer. Psychooncology. 2018;27(4):1320–6 [DOI] [PubMed] [Google Scholar]
- 15. Tran G, Zafar SY. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6(9):166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zafar SY, McNeil RB, Thomas CM, et al. Population-based assessment of cancer survivors' financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zebrack B, Kwak M, Sundstrom L. First descents, an adventure program for young adults with cancer: who benefits? Support Care Cancer. 2017;25(12):3665–73 [DOI] [PubMed] [Google Scholar]
- 18. de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer. 2014;120(20):3245–53 [DOI] [PubMed] [Google Scholar]
- 19. Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–21 [DOI] [PubMed] [Google Scholar]
- 20. Cano-Vindel A, Munoz-Navarro R, Medrano LA, et al. A computerized version of the Patient Health Questionnaire-4 as an ultra-brief screening tool to detect emotional disorders in primary care. J Affect Disord. 2018;234:247–55 [DOI] [PubMed] [Google Scholar]
- 21. Husson O, Zebrack BJ. Psychometric evaluation of an adolescent and young adult module of the impact of cancer instrument. J Adolesc Young Adult Oncol. 2017;6(1):159–70 [DOI] [PubMed] [Google Scholar]
- 22. Clinton-McHarg T, Carey M, Sanson-Fisher R, et al. Preliminary development and psychometric evaluation of an unmet needs measure for adolescents and young adults with cancer: the Cancer Needs Questionnaire-Young People (CNQ-YP). Health Qual Life Outcomes. 2012;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Merluzzi TV, Nairn RC, Hegde K, et al. Self-efficacy for coping with cancer: revision of the Cancer Behavior Inventory (version 2.0). Psychooncology. 2001;10(3):206–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Heitzmann CA, Merluzzi TV, Jean-Pierre P, et al. Assessing self-efficacy for coping with cancer: development and psychometric analysis of the brief version of the Cancer Behavior Inventory (CBI-B). Psychooncology. 2011;20(3):302–12 [DOI] [PubMed] [Google Scholar]
- 25. Zafar SY, Abernethy AP. Financial toxicity, Part II: how can we help with the burden of treatment-related costs? Oncology. 2013;27(4):253–4 [PubMed] [Google Scholar]
- 26. Zafar SY, Abernethy AP. Financial toxicity, part I: a new name for a growing problem. Oncology. 2013;27(2):80–1 [PMC free article] [PubMed] [Google Scholar]
- 27. Yabroff KR, Dowling EC, Guy GP Jr., et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22(4):745–55 [DOI] [PubMed] [Google Scholar]
- 29. De Souza JA, Aschebrook-Kilfoy B, Grogan R, et al. Grading financial toxicity based upon its impact on health-related quality of life (HRQol). J Clin Oncol. 2016;34(3_Suppl):16 [Google Scholar]
- 30. De Souza JA, Yap BJ, Hlubocky FJ, Daugherty C. Relationship between the cancer-specific comprehensive score for financial toxicity (COST), patient-reported outcome, and health-related quality of life (HRQOL) in patients with advanced cancers. J Clin Oncol. 2014;32(31_Suppl):222 [Google Scholar]
- 31. Serido J, Shim S, Tang C. A developmental model of financial capability: a framework for promoting a successful transition to adulthood. Int J Behav Dev. 2013;37:287–97 [Google Scholar]
- 32. de Bassa Scheresberg C. Financial literacy and financial behavior among young adults: evidence and implications. Numeracy. 2013;6(2):Article 5 [Google Scholar]
- 33. Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27(23):3868–74 [DOI] [PubMed] [Google Scholar]
- 34. Bestvina CM, Zullig LL, Rushing C, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract. 2014;10(3):162–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jagsi R, Ward KC, Abrahamse PH, et al. Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer. 2018;124:3668–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Irwin B, Kimmick G, Altomare I, et al. Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist. 2014;19(11):1135–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hunter WG, Zafar SY, Hesson A, et al. Discussing health care expenses in the oncology clinic: analysis of cost conversations in outpatient encounters. J Oncol Pract. 2017;13(11):e944–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Proussaloglou E, Yap BJ, O'Connor J, et al. Preferred cost communicator and financial distress (FD) in patients with cancer. J Clin Oncol. 2016;34(7_Suppl):26 [Google Scholar]
- 39. Shankaran V, Linden H, Steelquist J, et al. Development of a financial literacy course for patients with newly diagnosed cancer. Am J Manag Care. 2017;23(3 Suppl):S58–64 [PubMed] [Google Scholar]
- 40. De Souza JA, Proussaloglou E, Nicholson L, Wang Y. Evaluating financial toxicity (FT) interventions. J Clin Oncol. 2017;35(15_Suppl):e21673 [Google Scholar]
- 41. Yezefski T, Steelquist J, Watabayashi K, et al. Impact of trained oncology financial navigators on patient out-of-pocket spending. Am J Manag Care. 2018;24(5 Suppl):S74–9 [PubMed] [Google Scholar]
- 42. Shankaran V, Leahy T, Steelquist J, et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract. 2018;14(2):e122–9 [DOI] [PubMed] [Google Scholar]
- 43. Nicolla J, Friedman F, Manners I, Zafar Y. Empowering patients to self-identify financial assistance programs using an online application. J Clin Oncol. 2017;35(8_Suppl):428034060 [Google Scholar]
- 44. Zafar Y, Manners I, Nicolla J, et al. Bridging the financial assistance gap: a pilot study of a patient-facing app to identify drug financial assistance programs. J Clin Oncol. 2017;35(15_Suppl):e18296 [Google Scholar]
- 45. Politi MC, Kuzemchak MD, Liu J, et al. Show me my health plans: using a decision aid to improve decisions in the federal health insurance marketplace. MDM Policy Pract. 2016;1 [Epub ahead of print]; DOI: 10.1177/2381468316679998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhao J, Mir N, Ackermann N, et al. Dissemination of a web-based tool for supporting health insurance plan decisions (show me health plans): cross-sectional observational study. J Med Internet Res. 2018;20(6):e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zullig L, Wolf S, Vlastelica L, et al. The role of patient financial assistance programs in reducing costs for cancer patients. J Manag Care Spec Pharm. 23(4):407–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pannier ST, Warner EL, Fowler B, et al. Age-specific patient navigation preferences among adolescents and young adults with cancer. J Cancer Educ. 2017; [Epub ahead of print]; DOI: 10.1007/s13187-017-1294-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Feigelson HS, McMullen CK, Madrid S, et al. Optimizing patient-reported outcome and risk factor reporting from cancer survivors: a randomized trial of four different survey methods among colorectal cancer survivors. J Cancer Surviv. 2017;11(3):393–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kelvin JF, Thom B, Benedict C, et al. Cancer and fertility program improves patient satisfaction with information received. J Clin Oncol. 2016;34(15):1780–6 [DOI] [PMC free article] [PubMed] [Google Scholar]