Abstract
Introduction:
Extraskeletal chondroma (EC) is a rare benign neoplasm predominantly composed of mature hyaline cartilage; it develops in the soft tissues without any connection to bone cortex, intra-articular synovium, or periosteum. To date, only few cases have been reported in the leg, mainly in the knee, thigh, and popliteal region.
Case Report:
We describe herein the case of a 42-year-old woman with a 4-year history of a slow-growing, painful swelling on the posteromedial region of her left leg. Magnetic resonance imaging showed the presence of a huge mass occupying soleus muscle, compressing, and displacing anteriorly gastrocnemius muscle. After an incisional diagnostic biopsy, a complete surgical excision of the tumor was performed. On the basis of clinicoradiological and morphological findings, a diagnosis of EC was made.
Conclusion:
This report represents a clinicoradiological and morphological analysis about a very rare huge EC arising in the posteromedial region of the leg.
Keywords: Extraskeletal chondroma, soft tissue, leg, differential diagnosis
Learning Point of the Article:
Extraskeletal chondroma is a benign neoplasm that could have atypical features simulating malignant tumors.
Introduction
Extraskeletal chondroma (EC) is a rare benign neoplasm predominantly composed of mature hyaline cartilage, which accounts for about 1.5% of all benign soft tissue tumors [1]. By definition, these neoplasms develop in the soft tissues without any connection to bone cortex, intra-articular synovium, or periosteum [1, 2]. EC usually is characterized by a slow-growing, enlarging nodule that may cause pain or tenderness, predominantly in hands and feet of male adult patients, with an excellent prognosis and sporadic malignant transformation [3, 4]. Radiological presentation of EC is usually unspecific, revealing a well-demarcated, lobulated soft tissue mass, with occasional central and peripheral calcifications with a ring-like feature [5]. However, although EC has been considered a benign tumor, a local recurrence has been reported in 15% of cases; therefore, to prevent recurrences, it is recommended to remove the entire tumor including the capsule [3, 6]. ECs arising outside hands and feet are extremely rare, even if sporadic cases in the dura, auricle, parotid gland, and fallopian tube have been signaled [7, 8]. To date, only few cases have been described in the leg, mainly in the knee, thigh, and popliteal region [9, 10]. We have thought to be of interest to report herein a huge EC case arising in the posteromedial region of the leg, discussing also clinicoradiological and morphological findings.
Case Report
A 42-year-old woman presented at our observation with a 4-year history of a slow-growing, painful swelling on the posteromedial region of her left leg (Fig. 1a). X-rays evidenced the presence of a nodular mass at the proximal third of the left leg arising from the soft tissues next to the medial aspect of tibia (Fig. 1b); multiple calcific components were also observed. Subsequent magnetic resonance imaging (MRI) showed the presence of a 13 cm × 6 cm, 3 cm × 6 cm, 1 cm capsulated mass occupying soleus muscle, compressing, and displacing anteriorly gastrocnemius muscle (Fig. 1c). Moreover, the patient underwent vascular MRI of leg arteries which showed a posterolateral dislocation of the distal part of popliteal artery and tibioperoneal trunk (Fig. 1d), without alterations in canalization. Incisional biopsy was performed to assess the nature of the lesion. After the excision, specimens were immediately fixed in a 10% buffered formalin at room temperature for 48 h, cut into several tissue slices, and embedded in paraffin tissue blocks, as elsewhere reported [11, 12]. Histologically, the bioptic samples consisted mainly of hyaline cartilage containing chondrocytes with chondrocytic lacunae; a diagnosis of a chondroma was suggested. However, to exclude the possibility of chondrosarcoma, which is a common differential diagnosis, especially when dealing with small biopsies, a surgical excision of the entire tumor, including the capsule, was performed (Fig. 2a). On the basis of radiological and histopathologic findings, a diagnosis of EC was made. At the present moment, 1 year after the surgical excision, the patient is in good general conditions and no local recurrence has been observed.
Figure 1.
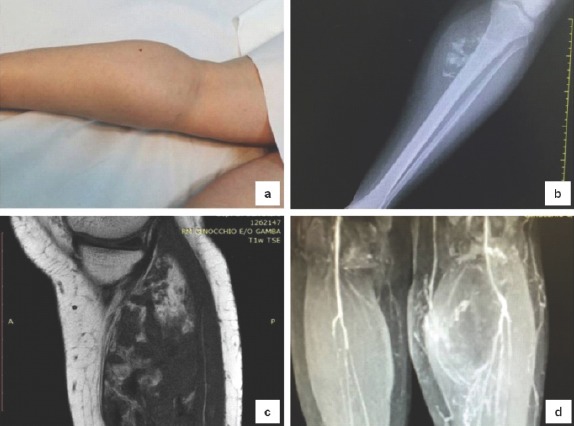
Clinical features: The lesion located in the posteromedial region of the left leg (a) pre-operative X-rays showed a nodular mass at the proximal third of the left leg (b) magnetic resonance imaging (MRI) (c) and vascular MRI (d) showed a posterolateral dislocation of the distal part of popliteal artery and tibioperoneal trunk, without alterations in canalization.
Figure 2.
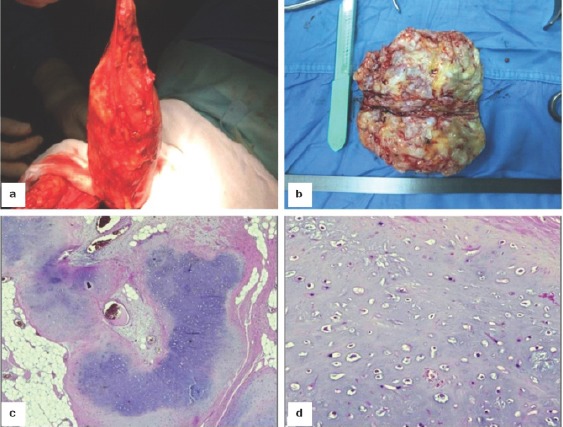
Surgical and histological images: En bloc excision of the tumor (a) gross examination of a well-circumscribed, nodular, white-gray, stiff mass (b) microscopic findings ×120 (c) and ×200 (d) showing that the lesion consisted in a multinodular growth with lobules of hyaline cartilage with a low cellularity and bland-looking chondrocytes (hematoxylin/eosin stain).
Pathological findings
Gross examination revealed a well-circumscribed, gray-white, nodular mass of 13 cm in greatest diameter (Fig. 2b). Histological examination showed an encapsulated lesion with multinodular growth, composed of the lobules of hyaline cartilage surrounded by mature adipose tissue (Fig. 2c). The tumor had low cellularity and consisted of bland-looking chondrocytes within lacunar spaces with no evidence of cytologic atypia, mitotic figures, or necrosis (Fig. 2d).
Immunohistochemistry
The tumor cells showed reactivity for S100, while the Ki67 index was <1%, confirming the benign nature.
Discussion
Ecs are benign cartilaginous tumors composed of mature chondrocytes associated with hyaline cartilage matrix that develops in soft tissues, without bone or joint involvement; usually, ECs are located in fingers, hands, toes, and feet [1, 2, 3, 4]. Less common locations include the forearms, the chest and abdominal wall, lung, fallopian tube, and other visceral organs [7, 8]. These tumors are described as well-circumscribed ovoid or lobulated shape, gray-white in color; histologically, EC is composed of hyaline cartilage arranged in lobules associated with fibrosis, ossification, and myxoid areas [3, 4]. A minor subset of ECs displays a preponderance of chondroblasts resembling osseous chondroblastoma with focal or diffuse calcifications [13]. The neoplastic chondrocytes may demonstrate mild nuclear atypia and visible nucleoli; mitotic figures are rarely observed. By immunohistochemistry, a typical positive stain for the S-100 protein as well as vimentin has been documented; generally, the grow fraction is low as documented by a quite absence of Ki 67 positivity (<3%) [14]. In the present case, the tumor was unusually located in the posteromedial region of the left leg, occupying the space between soleus and gastrocnemius muscles, as elsewhere reported in occasional sporadic cases. Another intriguing finding observed is the size of the tumor; in fact, our patient presented a huge swelling tumor measuring 13 cm × 6 cm, 3 cm ×6 cm,1 cm in size, while most of ECs present in literature are <3 cm [1, 2, 3, 4]. The differential diagnosis of EC is broad and includes other benign cartilaginous tumors such as calcifying aponeurotic fibroma (CAF) and tumoral calcinosis (TC), as well as malignant cartilage-forming tumors such as extraskeletal well-differentiated chondrosarcoma, cutaneous metastases of chondrosarcoma, or chondroblastic osteosarcoma. In detail, CAF contains cartilaginous foci in a dense fibromatous background, but it mainly occurs in hands and feet of children, [14]. Moreover, this lesion is not well-circumscribed and tends to infiltrate the surrounding soft tissues. TC also may mimic EC, especially when extensive calcifications are present, but the cartilage is lacking and a dense histiocytic infiltration is usually encountered. Taking into consideration the large size and location of our EC case, the most important differential clinicoradiological diagnoses were extraskeletal chondrosarcoma and extraskeletal chondroblastic osteosarcoma. In fact, both these tumors tend to reach large size, are usually located in deep soft tissues involving large muscles and joints of extremities [14]. However, the present case exhibited well-circumscribed margins, greatly in contrast with the infiltrative growth of the above-mentioned malignant counterparts. Finally, the low cellularity, as well as the absence of significant nuclear atypia/pleomorphism together with the low KI67 index, was strongly consistent with the benign nature of the lesion.
Conclusion
In this case, we demonstrated that chondroma can have atypical position, like the posteromedial region of the left leg, and can be significantly bigger than what commonly reported in literature. These findings should be taken in consideration in the differential diagnosis with extraskeletal chondrosarcoma and extraskeletal chondroblastic osteosarcoma.
Clinical Message.
Chondroma is a benign lesion that sometimes could have atypical features simulating malignant tumors. Thus, it is important to know these elements to reach the correct diagnosis when the lesion has this uncommon presentation.
Biography


Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Kedhaier A, Maala R, Ennouri N, Regaya N. Soft tissue chondroma of the hand:A report of five cases. Acta Orthop Belg. 2007;73:458–61. [PubMed] [Google Scholar]
- 2.Bahnassy M, Abdul-Khalik H. Soft tissue chondroma:A case report and literature review. Oman Med J. 2009;24:296–9. doi: 10.5001/omj.2009.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahlin DC, Salvador AH. Cartilaginous tumors of the soft tissues of the hands and feet. Mayo Clin Proc. 1974;49:721–6. [PubMed] [Google Scholar]
- 4.Chung EB, Enzinger FM. Chondroma of soft parts. Cancer. 1978;41:1414–24. doi: 10.1002/1097-0142(197804)41:4<1414::aid-cncr2820410429>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Hondar Wu HT, Chen W, Lee O, Chang CY. Imaging and pathological correlation of soft-tissue chondroma:A serial five-case study and literature review. Clin Imaging. 2006;30:32–6. doi: 10.1016/j.clinimag.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 6.Cho SJ, Horvai A. Chondro-osseous lesions of soft tissue. Surg Pathol Clin. 2015;8:419–44. doi: 10.1016/j.path.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Bergmann M, Pinz W, Blasius S, Lentschig M, Ostertag H, Neubauer U, et al. Chondroid tumors arising from the meninges –Report of 2 cases and review of the literature. Clin Neuropathol. 2004;23:149–53. [PubMed] [Google Scholar]
- 8.Varras M, Akrivis Ch, Tsoukalos G, Plis Ch, Karadaglis S, Ladopoulos I, et al. Tubal ectopic pregnancy associated with an extraskeletal chondroma of the fallopian tube:Case report. Clin Exp Obstet Gynecol. 2008;35:83–5. [PubMed] [Google Scholar]
- 9.Singh AP, Dhammi IK, Jain AK, Bhatt S. Extraskeletal juxtaarticular chondroma of the knee. Acta Orthop Traumatol Turc. 2011;45:130–4. doi: 10.3944/AOTT.2011.2419. [DOI] [PubMed] [Google Scholar]
- 10.Mao BY. Extraskeletal chondroma in the popliteal region:A Case report. Chin Med Sci J. 2015;30:270–2. doi: 10.1016/s1001-9294(16)30012-8. [DOI] [PubMed] [Google Scholar]
- 11.Ieni A, Barresi V, Branca G, Giuffrè G, Rosa MA, Tuccari G, et al. Immunoexpression of lactoferrin in bone metastases and corresponding primary carcinomas. Oncol Lett. 2013;5:1536–40. doi: 10.3892/ol.2013.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ieni A, Barresi V, Grosso M, Rosa MA, Tuccari G. Immunolocalization of lactoferrin in cartilage-forming neoplasms. J Orthop Sci. 2009;14:732–7. doi: 10.1007/s00776-009-1396-x. [DOI] [PubMed] [Google Scholar]
- 13.Isayama T, Iwasaki H, Kikuchi M. Chondroblastomalike extraskeletal chondroma. Clin Orthop Relat Res. 1991;268:214–7. [PubMed] [Google Scholar]
- 14.Goldblum JR, Folpe AL, Weiss SW. Enzinger and Weiss's Soft Tissue Tumors. 6th ed. Philadelphia, PA: Saunders-Elsevier; 2014. Cartilaginous and Osseous Soft Tissue Tumors; pp. 918–22. [Google Scholar]


