Abstract
Background
Persons with dementia have twice the acute hospital use as older persons without dementia. In addition to straining overburdened healthcare systems, acute hospital use impacts patient and caregiver quality of life and is associated with increased risk of adverse outcomes including death. Reducing avoidable acute hospital use in persons with dementia is thus a global healthcare priority. However, evidence regarding the impact of health service interventions as defined by the Effective Practice and Organization of Care Cochrane Group on acute hospital use is scant and inconclusive. The aim of this systematic review and meta-analysis was to synthesize available evidence on the impact of health service interventions on acute hospital use in community-dwelling persons with dementia compared to usual care.
Methods
Data Sources: MEDLINE, EMBASE, CINAHL and Cochrane CENTRAL (from 01/1995 to 08/2017). Study eligibility criteria: Randomised controlled trials measuring the impact of health service interventions on acute hospital use (proportion and mean number of emergency department visits and hospitalisations, mean number of hospital days, measured at 12 months, and at longest follow-up) in community-dwelling persons with dementia, compared to usual care. Study selection, appraisal and synthesis methods: Reviewers independently identified studies, extracted data, and assessed the risk of bias, with the Cochrane risk of bias tool. Authors of relevant trials were queried about unpublished data. Random effects model was used for meta-analyses. Effect heterogeneity was assessed through prediction intervals, and explored using sub-group analyses.
Findings
Seventeen trials provided data on 4,549 persons. Unpublished data were obtained for 13 trials, representing 65% of synthesized data. Most interventions included a case management or a self-management component. None of the outcome comparisons provided conclusive evidence supporting the hypothesis that these interventions would lead to a decrease in acute hospital use. Furthermore, prediction intervals indicated possible and important increased service use associated with these interventions, such as emergency department visits, hospital admissions, and hospital days. Subgroup analyses did not favour any type of intervention. A limitation of this study is the inclusion of any type of health service intervention, which may have increased the observed heterogeneity.
Conclusion
Despite a comprehensive systematic review and meta-analysis, including predominantly unpublished data, no health service intervention beyond usual care was found to reduce acute hospital use in community-dwelling persons with dementia. An important increase in service use may be associated with these interventions. Further research is urgently needed to identify effective interventions for this vulnerable population to limit rising acute hospital use, associated costs and adverse outcomes. Systematic review registration PROSPERO CRD42016046444.
Introduction
The World Health Organization (WHO) recognizes dementia as the global public health crisis of the 21st century [1,2]. Dementia affects 47.5 million people worldwide and this number is expected to double every 20 years [1]. The dementia population imposes a dramatic strain on healthcare systems worldwide, especially acute hospital use (Emergency Department (ED) visits and hospital admissions). It is estimated that persons with dementia have twice the acute hospital use as older persons without dementia [3–6]. Each year, approximately 40% of community-dwelling persons with dementia will visit the ED and approximately 30% will be hospitalised at least once [4–8]. Hospital care is three times more costly for this population compared to older persons without dementia [9,10]. In addition to straining already overburdened healthcare systems, acute hospital use impacts persons with dementia and their caregiver quality of life and is associated with increased risk of delirium, falls, cognitive and functional decline, 30-day readmission, long-term care admission and death [3–5].
Reducing avoidable hospitalisation and improving health services for persons with dementia are healthcare priorities, as seen in the 2017–2025 WHO action plan [11]. Various health service interventions, including memory clinics or case management, have been designed and implemented over the last two decades to improve practices and organization of care for community-dwelling persons with dementia [12–14]. However, the evidence of impact on acute hospital use is scarce and inconclusive. Previous meta-analyses have focused on case management only, and were unable to show any impact on acute hospital use [14–19]. To date, there is no comprehensive evidence synthesis or meta-analysis on the impact of health service interventions on acute hospital use in community-dwelling persons with dementia [20].
We conducted the first meta-analysis of randomised controlled trials (RCTs) measuring the impact of any type of health service intervention, as defined by the Effective Practice and Organization of Care Cochrane Group, on acute hospital use (ED visits / hospital admissions / hospital days) in community-dwelling persons with dementia compared to usual care.
Methods
This systematic review and meta-analysis were conducted and reported in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [21,22]. We followed an a priori registered protocol (PROSPERO ID: CRD42016046444) [23].
Eligibility criteria
Published articles on RCTs measuring the impact of health service interventions on acute hospital use in community-dwelling persons with dementia were included. Population: Community-dwelling persons with dementia or their caregivers or both. Intervention: Any health service intervention as defined by the Effective Practice and Organization of Care Cochrane Group (EPOC) Taxonomy 2015: “delivery arrangements”, “financial arrangements”, “governance arrangements”, or “implementation strategies” (Detailed eligibility criteria of interventions in Appendix A in S1 File) [24]. The definition of self-management applied here was the EPOC definition: “Shifting or promoting the responsibility for healthcare or disease management to the patient and/or their family.” (Detailed definition of self-management interventions in Appendix A in S1 File). Comparison: Usual care. Outcomes: Proportion or mean number of ED visits, proportion or mean number of hospital admissions, mean number of hospital days, in persons with dementia. Eligibility was restricted to interventions in high-income countries [25].
Information sources and search
We searched for publications in English or French in four databases: MEDLINE (“In-Process & Other Non-Indexed Citations”), EMBASE, CINAHL, and Cochrane Central Register of Controlled Trials (CENTRAL) from January 1995 (first publications on health service interventions for persons living with chronic diseases (5)) to August 2017. The search strategy was developed by a librarian specialized in health service interventions and meta-analysis (MG), a geriatrician (CGS), and an expert in health service interventions for persons with dementia (IV). The key concepts included in the database search were: dementia, health service intervention, community/primary care and RCT (Medline full electronic search strategy in Appendix B in S1 File). Duplicate publications were removed. The search was expanded using backward citation tracking in the reference list of included articles and recent systematic reviews on the topic [14–20] and forward citation tracking of all included studies using Scopus. Authors of relevant trials measuring impact on healthcare costs were inquired about data on acute hospital uses.
Study selection
Reviewers (CGS, MT, ML) independently assessed all records for eligibility. Disagreements were resolved by consensus or a third reviewer (IV).
Data collection, transformation and imputation
A systematic approach to data collection, transformation and imputation was followed, as recommended in the Data extraction for complex meta-analysis (DECiMAL) guide (Detailed origin, transformation or imputation of reported data in Appendix C and Tables A-E in S1 File) [26]. Two authors (CGS and ML) independently collected data on structured forms. Companion articles were used if needed, to access data on intervention details. To avoid bias due to selective inclusion of trials effect estimates, corresponding authors of included studies were contacted by email about unpublished data on outcomes at any other time point [27]. In cases of non-response, reminder emails and social media messages (ResearchGate, LinkedIn) were sent to corresponding and last authors. Transformation of data consisted of simple algebraic transformation. Data imputation consisted of weighted mean imputation of missing variance estimates. When the sample size in each group was not clearly stated, the randomised number of individuals in the text or flow chart determined the intention-to-treat population. Clustered randomised trials were identified and data adjusted on the clustering effect was collected. If unavailable, unadjusted data was collected.
Quality appraisal
Risk of bias was rated at the study level by two independent reviewers (CGS and ML), using the Cochrane Collaboration’s tool [28]. Companion articles, especially published protocols, were used to appraise quality. Blinding of participants and personnel was not assessed due to the nature of the interventions. For the six remaining individual domains, studies were classified into low, unclear or high risk of bias according to specific criteria of the tool [28]. As recommended by the Cochrane Handbook for Systematic Reviews of Interventions, studies of low quality were not excluded, but sensitivity analyses were conducted [21].
Summary measures
We pooled estimates for the following five outcomes at two endpoints. We pooled the estimated proportions of persons having at least one ED visit and/or at least one hospital admission, the mean number of ED visits, the mean number of hospital admissions, and the mean number of hospital days on the total sample of participants irrespective of whether participants used the corresponding service. Following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions on repeated observations on participants, we compiled data available for each outcome at 12 months and at longest follow-up for each study [21].
Synthesis
The statistical software R, and the meta and ggplot2 packages, were used to perform analyses [29]. The unit of analysis was the unique RCT. Random-effects models were employed to allow for varying effect sizes across studies due to heterogeneity of interventions and/or study populations. Risk differences, risk ratio and mean differences were calculated to determine the average relative and absolute effect of the interventions on the dichotomous and continuous outcomes. Not every cluster RCT study had published data adjusting for a potential clustering effect. Mixing unadjusted data from cluster RCTs with data from individual RCTs can lead to artificially narrow confidence intervals [30]. The Cochrane Collaboration recommends performing an “effective sample size” calculation to pool unadjusted data from cluster RCTs and individual RCTs together. As data necessary to perform this ‘effective sample size’ calculation was not available for every cluster RCT, we performed sensitivity analyses excluding unadjusted data from cluster RCTs [30]. Heterogeneity across studies was assessed by calculating the I2 statistic as well as predictions intervals. Following Cochrane recommendations, our interpretation of the I2 statistic was that over 40% may represent moderate to considerable heterogeneity [21]. Prediction intervals are another measure of heterogeneity and are easier to interpret and relate to the clinical implication of the observed heterogeneity [31]. Prediction intervals estimate a pre-specified distribution range (here: 95%) of treatment effects that can be expected in future settings. Meta-analysis results were labelled inconclusive if the range of treatment effects consistent with the prediction interval included both positive and negative clinically relevant effects.
Post hoc subgroup analyses were performed to explore heterogeneity for outcomes pooling a minimum of four studies and showing moderate to considerable heterogeneity (I2 > 40%). Criteria used to perform these subgroup analyses were the types of interventions according to the EPOC taxonomy (either the main component or one of several), country (United States vs. other), and follow-up time. The number of studies included did not allow meaningful application of meta-regression methods.
We conducted several sensitivity analyses to determine the robustness of meta-analysis results. We investigated changes in estimated pooled effects when removing: RCTs with at least one item at high risk of bias, outlying RCTs based on a graphical assessment of the corresponding forest plot, and cluster RCTs that did not properly take clustering into account. We did not generate funnel plots to identify reporting bias, because interpretation would have been questionable since most of the data in the analysis was unpublished. We conducted additional sensitivity analyses investigating changes in estimated pooled effects due to removing unpublished data provided by authors from the analyses [32].
Results
Studies characteristics
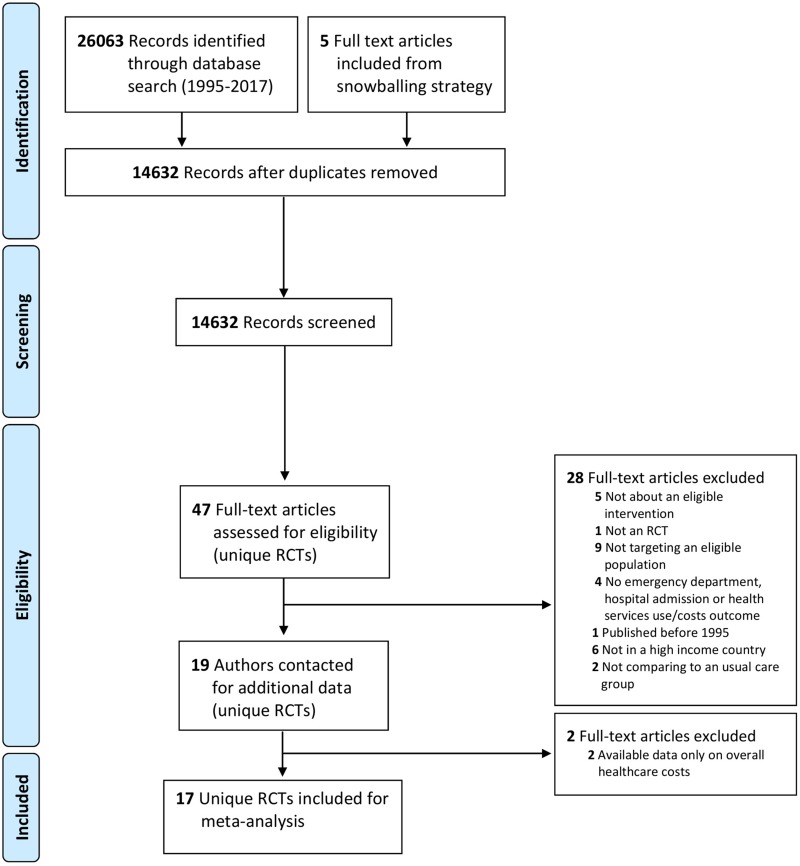
The systematic literature search resulted in 19 eligible, unique RCTs (Fig 1). Two of these were not included as the available data was only on overall healthcare costs (confirmed by study authors) [33,34]. Seventeen unique RCTs were included in the meta-analyses including four cluster RCTs (Table 1). Eight of 17 RCTs were included because unpublished data was provided by authors [13,35–41]. The published data was either only cost data or combined outcomes on use (e.g. long term care admission and hospitalisation) [13,35–41]. We obtained unpublished data for thirteen trials on five outcomes measured at two endpoints, representing 65% of overall synthesized data (Detailed origin, transformation or imputation of reported data in Appendix C and Tables A-E in S1 File).
Fig 1. Preferred reporting items for systematic reviews and meta-analysis (PRISMA) flow diagram of study selection.
Fig 1 legend: RCT, Randomised controlled trial.
Table 1. Studies characteristics.
| Authors Publication Date |
Country | Intervention type EPOC taxonomy (main component in bold) |
Intervention duration | Type of neurocognitive disorder and severity (MMSE if available) | Sample sizea | Age, Mean (SD)b | Female No (%)b |
|---|---|---|---|---|---|---|---|
|
Callahan 2006 [42] |
United States | Teams/case management/self-management/use of information and communication technology | maximum of 12 months | AD; “moderate severity” (mean MMSE: 18) | I: 84; C: 69 |
I: 77 (6); C: 78 (6) |
I: 39 (46); C: 27 (39) |
|
Bass 2003 [43,44] |
United States | Self-management/case management | 12 months | Dementia diagnosis or a symptom code indicating memory loss; severity not reported | I:72; C:48 |
Not reported | Not reported |
|
Challis 2004 [45] |
United Kingdom | Comprehensive geriatric assessment | 6 months | MMSE lower than 24 (I: 67%; C: 54%); severity not reported | I: 129; C: 127 | I: 82 (7); C: 82 (8) |
I: 96 (74); C: 92 (72) |
|
Chien 2008 [36] |
Hong Kong | Self-management/case management | 6 months | AD (DSM IV criteria); 80% of the sample at “early (ambulatory) stage" | I: 44; C: 44 |
Total sample: 68 (7) | Total sample: 38 (43) |
|
Chien 2011 [37] |
Hong Kong | Self-management/case management | 24 months | AD (DSM IV criteria); “mild or moderate” severity (mean MMSE: I:18, C:17) | I: 46; C: 46 |
I: 68 (7); C: 67 (7) |
I: 19 (41); C: 21 (46) |
|
Duru 2009 [46,47] |
United States | Case management/self-management/use of information and communication technology/educational material and educational meetings (healthcare professionals’ education) | 18 months | AD, vascular dementia and other types of dementia; (Blessed-Roth Dementia Scale mean scores: I: 5, C: 6) | I: 238; C: 170 | I: 79 (6); C: 80 (7) |
I: 94 (55); C: 71 (56) |
|
Eloniemi-Sulkava 2009 [40] |
Finland | Teams/comprehensive geriatric assessment/case management/self-management | 24 months | AD, vascular dementia and other types of dementia; “mild”, “moderate” and “severe” dementia (mean MMSE: 14) | I: 63; C: 62 |
I: 78 (7); C: 77 (6) | I: (43) c; C: (32)c |
| Joling 2013 [38,48,49] |
Netherlands | Self-management | 12 months | Dementia diagnosis; (mean MMSE: I: 21, C: 22) | I: 96; C: 96 |
I: 73 (9); C: 77 (8) |
I: 30 (31); C: 32 (33) |
| Laakkonen 2016 [41,50] |
Finland | Self-management | 8 weeks | Dementia diagnosis; “possible”, “mild”, “moderate” and “severe” dementia (mean MMSE: I: 20, C: 22) | I: 67; C: 69 |
I: 77 (6); C: 77 (6) |
I: 25 (37); C: 26 (38) |
| Meeuwsen 2013 [51–53] |
Netherlands | Site of service delivery (memory clinic vs general practitioner)/teams | 12 months | AD, vascular dementia, other types of dementia; “very mild” and “mild” dementia (mean MMSE: 23) | I: 87; C: 88 |
I: 78 (6); C: 78 (5) |
I: 54 (62); C: 52 (59) |
| Menn 2012 [39,54,55] |
Germany | Self-management/educational material and educational meetings (healthcare professionals’ education)/shared care | 24 months | Dementia diagnosis;”mild” and “moderate” dementia (mean MMSE: I-groupB: 19, I-groupC: 19, C: 18) | I-groupB: 109 I-groupC: 110 C: 171 |
I-groupB: 79 (6); I-groupC: 81 (6); C: 81 (7) | I-groupB: (68) c; I-groupC: (71) c; C: (67) c |
| Nichols 2017 [35,56] |
United States | Self-management | 6 months | AD, Dementia diagnosis or MMSE lower than 24; severity not reported | I: 98; C: 99 |
I: 80 (8); C: 78 (9) |
I: 59 (60); C: 59 (60) |
| Rubenstein, 2007 [57] |
United States | Case management/teams | 36 months | Cognitive impairment (10-item Geriatric Postal Screening Survey); severity not reported | I: 380; C: 412 | I: 75 (6); C: 74 (6) |
I: 14 (4); C: 11 (3) |
| Samus 2014 [58,59] |
United States | Teams/case management/self-management/use of information and communication technology | 18 months | Dementia or “Cognitive Disorder Not Otherwise Specified” (DSM IV criteria); “mild”, “moderate” and “severe” dementia (mean MMSE: 19) | I: 110; C: 193 | I: 84 (6); C: 84 (6) |
I: 73 (66); C:120 (62) |
| Søgaard 2014 [60–62] |
Denmark | Self-management | 36 months | AD, mixed dementia, or Lewy body dementia; “mild” dementia (mean MMSE: 24) | I: 163; C: 167 | I: 76 (8); C: 75 (7) | I: 87 (53); C: 92 (55) |
| Thyrian 2017 [13,63,64] |
Germany | Case management/ use of information and communication technology /teams | 12 months | Positive screening for dementia (DemTect procedure); “no hint for”, “mild”, “moderate” and “severe” dementia (mean MMSE: 23) | I: 408; C: 226 | I: 81 (6); C: 80 (5) |
I: 178 (61); C: 70 (60) |
| Wray 2010 [65] |
United States | Self-management | 10 weeks | Diagnosis of dementia; "moderate-to-severe" dementia | I: 83; C: 75 |
I: 78 (7); C: 79 (8) |
Not reported |
Abbreviations: AD, Alzheimer’s Disease; DSM IV, Diagnostic and Statistical Manual of Mental Disorders IV; EPOC, Effective Practice and Organization of Care Cochrane Group; MMSE, Mini-Mental State Examination; I, Intervention Group; C, Control Group
a The numbers are the randomised numbers of participants in each group (as reported or calculated).
b Denominators are the number of participants with available baseline characteristics. They differ from the randomised numbers of participants for two trials: Thyrian 2017 and Duru 2009. In Thyrian 2017, the numbers of participants with available baseline characteristics are 291 in intervention and 116 in control groups. In Duru 2009, the numbers of participants with available baseline characteristics are 170 in intervention and 126 in control groups.
c Only percentages of female participants were reported.
Seventeen unique trials provided data on 4,549 community-dwelling persons living with dementia (study populations ranging from 88 to 792 persons, median randomisation arm size: 96) (Table 1) (13.36–65). These persons had a mean age of 77 years (standard deviation: 4) and 49% were females (proportion ranged from 4% to 74%). Twelve of the seventeen trials reported dementia severity at baseline, ranging from mild to severe: 6/12 mild, 5/12 moderate, 1/12 moderate to severe. None of the trials reported selection of participants based on risk of acute hospital use.
Health service interventions consisted of one or a combination of the following EPOC taxonomy components: case management (9/17), self-management (13/17), comprehensive geriatric assessment (2/17), educational materials/educational meetings (healthcare professional education) (2/17), use of information and communication technology (4/17), teams (6/17), shared care (1/17), site of service delivery (memory clinic) (1/17). None of the interventions involved financial or governance arrangements. Interventions were implemented and evaluated in studies conducted in the USA (7), in Europe (8) and in Hong Kong (2). Duration of interventions ranged from two to 36 months, median duration 12 months.
The sources of the data for each outcome measure included in the meta-analysis are presented in Table 2.
Table 2. Intervention types and outcomes included in the meta-analysis for each study.
| Authors Publication Date |
Intervention type EPOC taxonomy (main component in bold) |
Outcomes | ||||
|---|---|---|---|---|---|---|
| Proportion of patients with at least one ED visit | Mean number of ED visits | Proportion of patients with at least one hospital admission | Mean number of hospital admissions | Mean number of hospital days | ||
| Callahan 2006 [42] |
Teams/case management/self-management/use of information and communication technology | ✓ | ✓ | |||
| Bass 2003 [43,44] | Self-management/case management | ✓ | ✓ | |||
| Challis 2004 [45] | Comprehensive geriatric assessment | ✓ | ✓ | ✓ | ✓ | |
| Chien 2008 [36] | Self-management/case management | ✓ | ✓ | ✓ | ✓ | |
| Chien 2011 [37] | Self-management/case management | ✓ | ✓ | ✓ | ✓ | |
| Duru 2009 [46,47] | Case management/self-management/use of information and communication technology/ educational material and educational meetings (healthcare professionals’ education) | ✓ | ✓ | ✓ | ✓ | |
| Eloniemi-Sulkava 2009 [40] | Teams/comprehensive geriatric assessment/case management/self-management | ✓ | ✓ | |||
| Joling 2013 [38,48,49] | Self-management | ✓ | ✓ | |||
| Laakkonen 2016 [41,50] | Self-management | ✓ | ✓ | |||
| Menn 2012 [39,54,55] |
Self-management/educational material and educational meetings (healthcare professionals’ education)/shared care | ✓ | ✓ | ✓ | ||
| Nichols 2017 [35,56] | Self-management | ✓ | ✓ | ✓ | ✓ | ✓ |
| Rubenstein, 2007 [57] | Case management/teams | ✓ | ✓ | |||
| Samus 2014 [58,59] | Teams/case management/self-management/use of information and communication technology | ✓ | ✓ | ✓ | ✓ | ✓ |
| Søgaard 2014 [60–62] | Self-management | ✓ | ✓ | ✓ | ✓ | ✓ |
| Thyrian 2017 [13,63,64] | Case management/ use of information and communication technology /teams | ✓ | ✓ | ✓ | ✓ | ✓ |
| Wray 2010 [65] | Self-management | ✓ | ✓ | |||
Abbreviations: EPOC, Effective Practice and Organization of Care Cochrane Group.
Impact on acute hospital use
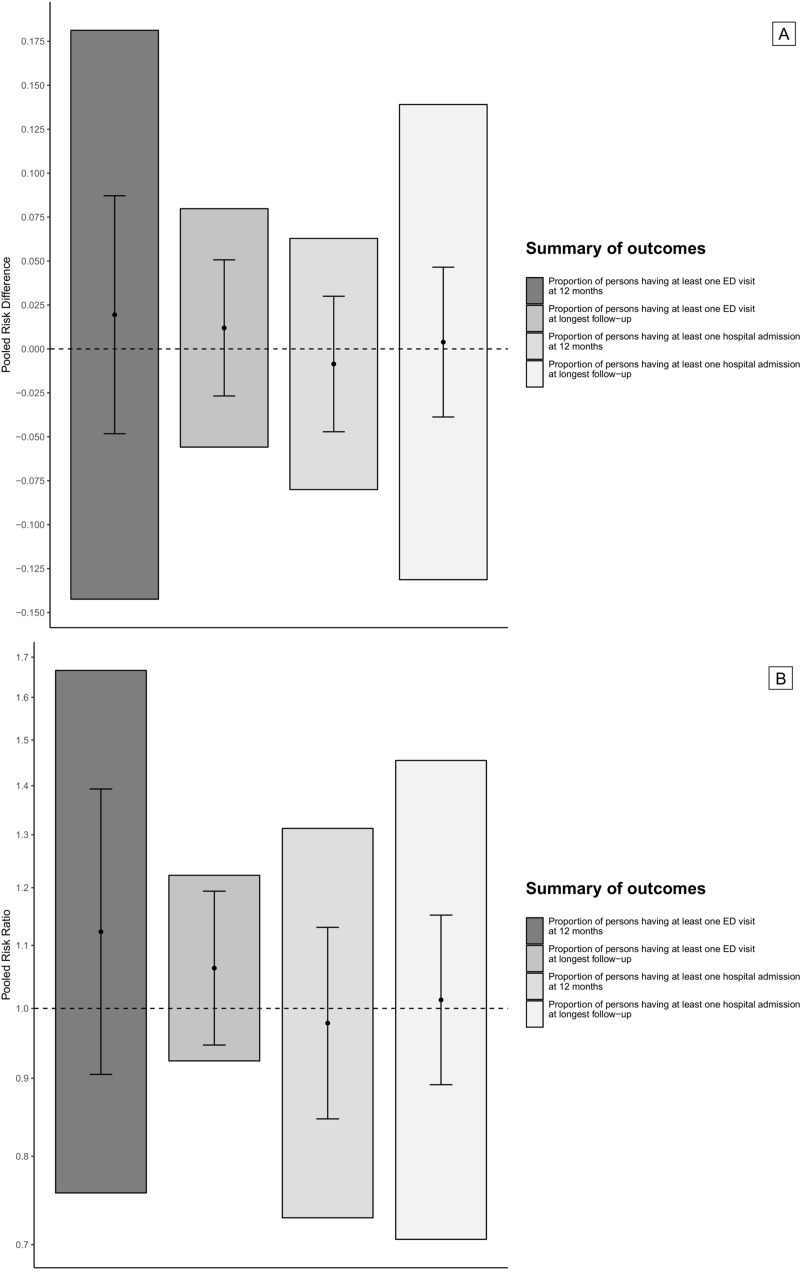
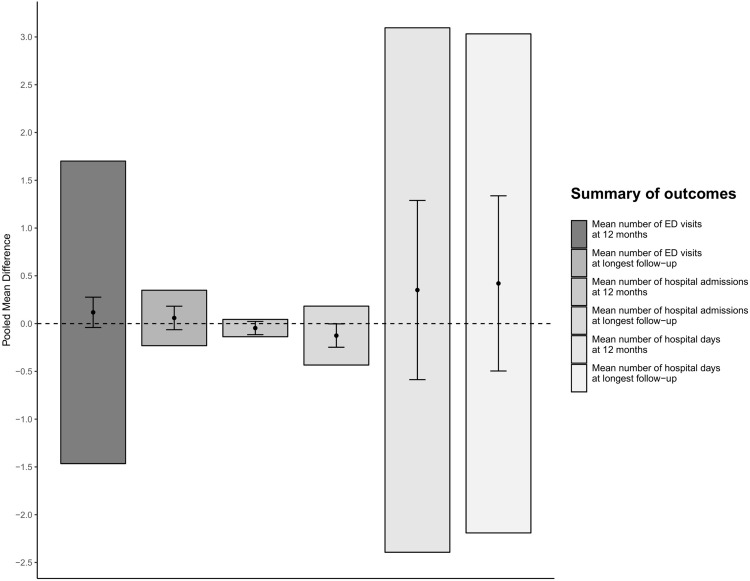
None of the considered outcome comparisons provided conclusive evidence supporting the hypothesis that health service interventions lead to a decrease in service use as measured by ED visits, hospital admission or hospital days (Figs 2 and 3 and Figs A-E in S1 File). Furthermore, in every meta-analysis, the estimated 95% prediction intervals indicated that an important increase in service use may be associated with the interventions.
Fig 2.
Pooled risk differences (2A) and pooled risk ratios (2B) for dichotomous outcomes (solid dots), 95% confidence intervals (black coloured error bars), and 95% prediction intervals (grey shaded bar plots). Fig 2 legend: ED, Emergency Department.
Fig 3. Pooled mean differences for continuous outcomes (solid dots), 95% confidence intervals (black coloured error bars), and 95% prediction intervals (grey shaded bar plots).
Fig 3 legend: ED, Emergency Department.
Post hoc subgroup analyses did not suggest any systematic dependencies of effects in relation to type of intervention, country or follow-up time.
Quality and robustness of the evidence
Four of the 17 trials were judged as having at least one area of high risk of bias (Fig F in S1 File). Eleven trials reported adequate sequence generation, 11 trials properly concealed allocation, 14 trials implemented blinding of outcome assessors, and 15 trials adequately addressed incomplete outcome data. Only eight trials published a study protocol and reported (or provided upon request) pre-specified outcomes.
Sensitivity analyses to determine the robustness of meta-analysis results did not lead to any change in estimated pooled effects that would alter the conclusions. Sensitivity analyses of the impact of unpublished data provided by authors on meta-analysis results did not suggest reporting bias.
Discussion
The results of this systematic review and meta-analysis did not establish superiority of health service interventions over usual care to reduce acute hospital use in community-dwelling persons with dementia. There was no detectable signal favouring any type of health service intervention. Overall evidence had low risk of bias. Sensitivity analyses confirmed the robustness of the results. Furthermore, for every outcome, the estimated 95% prediction intervals indicated that an important increase in service use may be associated with these interventions.
These results are of particular interest to policy makers, persons living with dementia, their caregivers, and healthcare professionals. There is no cure or disease-modifying treatment for dementia and no promising advances in the near future [66]. Improving healthcare delivery remains essential to limit rising acute hospital use and associated costs, improve quality of life of patients and their caregivers, and prevent adverse outcomes for persons living with dementia. The absence of evidence for an impact on acute hospital use of any type of health service intervention is thus highly concerning. The possibility that these interventions may increase acute hospital use is not to be disregarded.
Non-intended effects of health service interventions, such as increase in service use (ED visits, hospital admissions, and hospital days) have previously been witnessed in several contexts, such as self-management interventions. These non-intended effects were associated with either beneficial or adverse outcomes. Some health service interventions, like self-management interventions for caregivers, have led to non-intended beneficial outcomes: increased service use due to increased caregiver awareness of symptoms, diagnosis procedures and treatment options [38,60]. Some health service interventions, such as self-management in patients with chronic obstructive pulmonary disease (COPD), have led to non-intended adverse outcomes. A decreased service use due to patient overconfidence in self-management led to higher mortality [67].
It is essential to better characterize acute hospital use and inappropriate use, so that beneficial and adverse non-intended outcomes can be sorted out. In the trials included in this systematic review and meta-analysis, only total acute hospital use was measured. However, community-dwelling persons with dementia would have a much greater chance of potentially avoidable hospitalizations (74%) or ED visits (51%), than persons without dementia [5]. Definitions and measures of potentially avoidable acute hospital use such as Ambulatory-Care Sensitive Conditions (ACSC) hospital admissions have recently been questioned for inaccuracy in community-dwelling persons living with dementia [68]. Developing accurate measures of potentially avoidable service use in community-dwelling persons living with dementia is essential [68].
Two main reasons could explain the inconclusive results of this evidence synthesis. First, the included RCTs might not have detected an effect because of lack of statistical power. Lack of power could be a consequence of inappropriate specification of the target population. These RCTs did not exclusively consider high-risk populations for acute hospital use. Targeting high-risk populations may be necessary to show measurable reductions in acute hospital use due to health service interventions. To our knowledge, no screening tool is available to identify community-dwelling persons with dementia with high-risk of acute hospital use, so its development is essential [69].
Second, there might be a gap between the focus of the interventions and the actual causes of acute hospital use [20,70]. The interventions may not have effectively addressed the causes of acute hospital use of community-dwelling persons with dementia [20,70,71]. Only a few types of interventions were tested in the 17 trials, mainly case management and self-management. Case management would have been effective if the reasons for acute hospital use were care fragmentation. However, care fragmentation was not identified as a major determinant of crises leading to acute hospital use [70,72]. Since behavioural and psychological symptoms of dementia are not leading causes of hospital admissions, increasing self-management skills for patients and caregivers would not have been effective [3,71].
The literature suggests that physical conditions are a leading cause of acute hospital use in persons with dementia. Most admissions are due to accidents and injuries arising from falls, urinary tract and respiratory infections, or complications of chronic diseases [3,70–72]. Improving access to primary health care and training home-care staff on early detection and appropriate management of the common causes of acute hospital use could reduce avoidable acute hospital use [68,73].
Caregiver availability and caregiver health are other important determinants of acute hospital use. Indeed, caregiver stress, burden, mental health and sudden absence (hospital admission or death) are identified as major drivers of crises [70–72,74]. Offering timely support to caregivers through respite care or temporary home care could reduce avoidable acute hospital use [20].
During the final year of life, nearly 80% of community-dwelling persons with dementia are hospitalized [5]. Some of these hospitalizations may not be the choice of patients and caregivers, who may have preferred to obtain end-of-life care at home [75]. Palliative care in older persons with advanced illness has been shown to double the chances of dying at home [76]. Interventions emphasizing a palliative care approach with discussion of advanced directives and preferences for end-of-life care might reduce undesired acute hospital use.
Strengths and limits
Our study has strengths as well as potential limitations. This is the first systematic review and meta-analysis on the impact of any type of health service interventions on acute hospital use in community-dwelling persons with dementia, and the first to include predominantly unpublished data provided by the authors of included randomised controlled trials. Two main challenges were encountered when retrieving data for this synthesis: i) some evidence was published as cost-effectiveness analysis; ii) outcomes were measured in different ways. We gathered data pro-actively by contacting authors of identified trials, and used a systematic approach for data transformation and imputation. These strategies dramatically increased the range of synthesised evidence and were likely to have decreased potential publication bias impact on our effect estimates [77,78].
Acknowledging the complexity of acute hospital use prevention in this vulnerable population, we included any type of health service intervention as defined and classified in the Cochrane EPOC taxonomy [24]. This is a common approach in Cochrane reviews [79], but might have increased the observed heterogeneity. We computed prediction intervals and performed sub-group analyses to explain possible sources of effect heterogeneity. We used prediction intervals to conservatively interpret the range of expected treatment effects in future studies rather than an average effect composed by a set of different underlying effects. Our sub-group analyses were based on limited descriptions provided in the articles, which limited our understanding of heterogeneity [80]. For example, usual care and primary care access might vary widely between countries, regions, or subpopulations and were rarely described in the studies. Likewise, intervention descriptions were sometimes too limited to classify interventions according to the EPOC taxonomy. We thus looked for protocols and companion articles and performed independent data extraction to reduce subjectivity.
Conclusion, policy implications and future research
With the data available, it was not possible to establish superiority of any health service intervention beyond usual care to reduce acute hospital use in community-dwelling persons with dementia. In fact, our evidence synthesis findings do not rule out the possibility that the studied health service interventions may be associated with an important increase in service use.
We have no recommendations for health service interventions to be implemented. However, we can propose a research agenda focused on: 1) development of accurate measures of potentially avoidable acute hospital use by community-dwelling persons with dementia; 2) identifying the causes and determinants of potentially avoidable acute hospital use; 3) development of a validated screening tool to target high-risk population; 4) co-design of health service interventions with patients and caregivers that address the causes of avoidable acute hospital use; and 5) rigorous testing of the impact of these co-designed interventions in high-risk community-dwelling persons with dementia.
Supporting information
S1 file legend:
Appendix A: Detailed eligibility criteria of intervention.
Appendix B: Medline full electronic search strategy.
Appendix C: Detailed origin, transformation or imputation of reported data.
Table A: Origin, transformation or imputation of data for proportions of persons having at least one Emergency Department visit.
Table B: Origin, transformation or imputation of data for mean number of Emergency Department visit.
Table C: Origin, transformation or imputation of data for proportions of persons having at least one hospital admission.
Table D: Origin, transformation or imputation of data for mean number of hospital admission.
Table E: Origin, transformation or imputation of data for mean number of hospital days.
Fig A. Proportion of persons having at least one Emergency Department visit (Risk Ratio and Risk Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; RD, Risk Difference; RR, Risk Ratio.
Fig B. Proportion of persons having at least one hospital admission (Risk Ratio and Risk Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; RD, Risk Difference; RR, Risk Ratio.
Fig C. Mean number of Emergency Department visit (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig D. Mean number of hospital admission (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig E. Mean number of hospital days (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig F. Quality Appraisal using the Cochrane Risk of Bias Tool. a Random sequence generation (selection bias). b Allocation concealment (selection bias). c Blinding of participant and personnel (performance bias). d Blinding of outcome assessment. e Incomplete outcome data (attrition bias). f Selective reporting (reporting bias). g Other bias. h Questions marks, uncertain risk of bias; + signs, low risk of bias;—signs, high risk of bias.
References.
(DOCX)
(DOCX)
Acknowledgments
Our thanks to Muriel Guériton, specialized librarian, for the literature search; Rebecca Rupp, Genevieve Arsenault-Lapierre, Nadia O’Brien for their editorial assistance; and to Alvaro Guillen-Cuevas for his assistance in designing the figures.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Claire Godard-Sebillotte received support through a Doctoral Research Award from the Canadian Institutes of Health Research: Vanier Canada Graduate Scholarship (Vanier CGS). The work of Mélanie Le Berre, Muriel Guériton and Rebecca Rupp was funded through a research grant from the Canadian Institutes of Health Research: The Canadian Consortium for Neurodegeneration and Aging (CCNA). “Assessing care models implemented in primary health care for persons with Alzheimer’s disease and related disorders”. 2014-2019. Tibor Schuster received funding through a Tier II Canada Research Chair from the Canadian Institutes of Health Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. The epidemiology and impact of dementia: current state and future trends 2015. Geneva, Switzerland: World Health Organization; 2015. http://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_epidemiology.pdf?ua=1. Accessed August 5, 2015. [Google Scholar]
- 2.World Health Organization. Dementia: a public health priority. Geneva, Switzerland: World Health Organization; 2012. https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHO-Dementia-English.pdf. Accessed October 5, 2017. [Google Scholar]
- 3.Prince M, Comas-Herrera A, Knapp M, et al. World Alzheimer Report 2016 Improving healthcare for people living with dementia coverage, Quality and costs now and in the future. London, UK: Alzheimer’s Disease International; 2016. https://www.alz.co.uk/research/world-report-2016. Accessed November 1, 2016. [Google Scholar]
- 4.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency Department Use Among Older Adults With Dementia. Alzheimer Dis Assoc Disord. 2016;30: 35–40. 10.1097/WAD.0000000000000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feng Z, Coots LA, Kaganova Y, Wiener JM. Hospital and ED use among medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff Millwood. 2014;33: 683–690. 10.1377/hlthaff.2013.1179 [DOI] [PubMed] [Google Scholar]
- 6.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA. 2012;307: 165–172. 10.1001/jama.2011.1964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudolph JL, Zanin NM, Jones RN, Marcantonio ER, Fong TG, Yang FM, et al. Hospitalization in community-dwelling persons with Alzheimer’s disease: frequency and causes. J Am Geriatr Soc. 2010;58: 1542–1548. 10.1111/j.1532-5415.2010.02924.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao Y, Kuo T-C, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8: 108 10.1186/1472-6963-8-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alzheimer’s Association. 2017 Alzheimer’s Disease Facts and Figures. Alzheimers Dement. 2017: 325–373. [Google Scholar]
- 10.Lin P-J, Zhong Y, Fillit HM, Chen E, Neumann PJ. Medicare Expenditures of Individuals with Alzheimer’s Disease and Related Dementias or Mild Cognitive Impairment Before and After Diagnosis. J Am Geriatr Soc. 2016;64: 1549–1557. 10.1111/jgs.14227 [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. WHO | Global action plan on the public health response to dementia 2017–2025. Geneva, Switzerland: World Health Organization; 2017. http://www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/. Accessed Feb 6, 2018. [Google Scholar]
- 12.Callahan CM. Alzheimer’s Disease: Individuals, Dyads, Communities, and Costs. J Am Geriatr Soc. 2017;65: 892–895. 10.1111/jgs.14808 [DOI] [PubMed] [Google Scholar]
- 13.Thyrian JR, Hertel J, Wucherer D, et al. Effectiveness and Safety of Dementia Care Management in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74(10):996–1004. 10.1001/jamapsychiatry.2017.2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reilly S, Miranda-Castillo C, Malouf R, Hoe J, Toot S, Challis D, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1: CD008345 10.1002/14651858.CD008345.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanassov V, Vedel I, Pluye P. Case management for dementia in primary health care: a systematic mixed studies review based on the diffusion of innovation model. Clin Interv Aging. 2014;9: 915–928. 10.2147/CIA.S64723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khanassov V, Vedel I, Pluye P. Barriers to implementation of case management for patients with dementia: a systematic mixed studies review. Ann Fam Med. 2014;12: 456–465. 10.1370/afm.1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pimouguet C, Lavaud T, Dartigues JF, Helmer C. Dementia case management effectiveness on health care costs and resource utilization: a systematic review of randomized controlled trials. J Nutr Health Aging. 2010;14: 669–676. [DOI] [PubMed] [Google Scholar]
- 18.Somme D, Trouve H, Dramé M, Gagnon D, Couturier Y, Saint-Jean O. Analysis of case management programs for patients with dementia: a systematic review. Alzheimers Dement J Alzheimers Assoc. 2012;8: 426–436. [DOI] [PubMed] [Google Scholar]
- 19.Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28: 889–902. 10.1002/gps.3906 [DOI] [PubMed] [Google Scholar]
- 20.Phelan EA, Debnam KJ, Anderson LA, Owens SB. A systematic review of intervention studies to prevent hospitalizations of community-dwelling older adults with dementia. Med Care. 2015;53: 207–213. 10.1097/MLR.0000000000000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Chichester, England: The Cochrane Collaboration, 2011. [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151: W65–94. [DOI] [PubMed] [Google Scholar]
- 23.Godard-Sebillotte C, Le Berre M, Trottier M, et al. Interventions aimed at improving care for persons with neurocognitive disorders and reducing emergency and hospital use: a systematic mixed studies review. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016046444 (accessed 28 Aug 2017).
- 24.Effective Practice and Organisation of Care (EPOC). EPOC Taxonomy; 2015. https://epoc.cochrane.org/epoc-taxonomy. Accessed September 5, 2017.
- 25.World Bank Country and Lending Groups–World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed Jul 25, 2016.
- 26.Pedder H, Sarri G, Keeney E, Nunes V, Dias S. Data extraction for complex meta-analysis (DECiMAL) guide. Syst Rev. 2016;5: 212 10.1186/s13643-016-0368-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Page MJ, McKenzie JE, Kirkham J, Dwan K, Kramer S, Green S, et al. Bias due to selective inclusion and reporting of outcomes and analyses in systematic reviews of randomised trials of healthcare interventions. Cochrane Database Syst Rev. 2014; MR000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.R Core Team. R: A language and environment for statistical computing. [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2017. Available: https://www.R-project.org/ [Google Scholar]
- 30.Richardson M, Garner P, Donegan S. Cluster Randomised Trials in Cochrane Reviews: Evaluation of Methodological and Reporting Practice. PloS One. 2016;11: e0151818 10.1371/journal.pone.0151818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.IntHout J, Ioannidis JPA, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6: e010247 10.1136/bmjopen-2015-010247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mullan RJ, Flynn DN, Carlberg B, Tleyjeh IM, Kamath CC, LaBella ML, et al. Systematic reviewers commonly contact study authors but do so with limited rigor. J Clin Epidemiol. 2009;62: 138–142. 10.1016/j.jclinepi.2008.08.002 [DOI] [PubMed] [Google Scholar]
- 33.Newcomer R, Miller R, Clay T, Fox P. Effects of the Medicare Alzheimer’s disease demonstration on Medicare expenditures. Health Care Financ Rev. 1999;20: 45–65. [PMC free article] [PubMed] [Google Scholar]
- 34.Wishart L, Macerollo J, Loney P, King A, Beaumont L, Browne G, et al. “Special steps”: an effective visiting/walking program for persons with cognitive impairment. Can J Nurs Res Rev. 2000;31: 57–71. [PubMed] [Google Scholar]
- 35.Nichols LO, Martindale-Adams J, Zhu CW, Kaplan EK, Zuber JK, Waters TM. Impact of the REACH II and REACH VA Dementia Caregiver Interventions on Healthcare Costs. J Am Geriatr Soc. 2017;65: 931–936. 10.1111/jgs.14716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chien WT, Lee YM. A disease management program for families of persons in Hong Kong with dementia. Psychiatr Serv. 2008;59: 433–436. 10.1176/ps.2008.59.4.433 [DOI] [PubMed] [Google Scholar]
- 37.Chien WT, Lee IYM. Randomized controlled trial of a dementia care programme for families of home-resided older people with dementia. J Adv Nurs. 2011;67: 774–787. 10.1111/j.1365-2648.2010.05537.x [DOI] [PubMed] [Google Scholar]
- 38.Joling KJ, Bosmans JE, van Marwijk HWJ, van der Horst HE, Scheltens P, MacNeil Vroomen JL, et al. The cost-effectiveness of a family meetings intervention to prevent depression and anxiety in family caregivers of patients with dementia: a randomized trial. Trials. 2013;14: 305 10.1186/1745-6215-14-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Menn P, Holle R, Kunz S, Donath C, Lauterberg J, Leidl R, et al. Dementia care in the general practice setting: a cluster randomized trial on the effectiveness and cost impact of three management strategies. Value Health. 2012;15: 851–859. 10.1016/j.jval.2012.06.007 [DOI] [PubMed] [Google Scholar]
- 40.Eloniemi-Sulkava U, Saarenheimo M, Laakkonen M-L, Pietilä M, Savikko N, Kautiainen H, et al. Family care as collaboration: effectiveness of a multicomponent support program for elderly couples with dementia. Randomized controlled intervention study. J Am Geriatr Soc. 2009;57: 2200–2208. 10.1111/j.1532-5415.2009.02564.x [DOI] [PubMed] [Google Scholar]
- 41.Laakkonen M-L, Kautiainen H, Hölttä E, Savikko N, Tilvis RS, Strandberg TE, et al. Effects of Self-Management Groups for People with Dementia and Their Spouses-Randomized Controlled Trial. J Am Geriatr Soc. 2016;64: 752–760. 10.1111/jgs.14055 [DOI] [PubMed] [Google Scholar]
- 42.Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, Perkins AJ, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295: 2148–2157. 10.1001/jama.295.18.2148 [DOI] [PubMed] [Google Scholar]
- 43.Clark PA, Bass DM, Looman WJ, McCarthy CA, Eckert S. Outcomes for patients with dementia from the Cleveland Alzheimer’s Managed Care Demonstration. Aging Ment Health. 2004;8: 40–51. 10.1080/13607860310001613329 [DOI] [PubMed] [Google Scholar]
- 44.Bass DM, Clark PA, Looman WJ, McCarthy CA, Eckert S. The Cleveland Alzheimer’s managed care demonstration: outcomes after 12 months of implementation. Gerontologist. 2003;43: 73–85. 10.1093/geront/43.1.73 [DOI] [PubMed] [Google Scholar]
- 45.Challis D, Clarkson P, Williamson J, Hughes J, Venables D, Burns A, et al. The value of specialist clinical assessment of older people prior to entry to care homes. Age Ageing. 2004;33: 25–34. 10.1093/ageing/afh007 [DOI] [PubMed] [Google Scholar]
- 46.Duru OK, Ettner SL, Vassar SD, Chodosh J, Vickrey BG. Cost evaluation of a coordinated care management intervention for dementia. Am J Manag Care. 2009;15: 521–528. [PMC free article] [PubMed] [Google Scholar]
- 47.Vickrey BG, Mittman BS, Connor KI, Pearson ML, Della Penna RD, Ganiats TG, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145: 713–726. [DOI] [PubMed] [Google Scholar]
- 48.Joling KJ, van Hout HPJ, Scheltens P, Vernooij-Dassen M, van den Berg B, Bosmans J, et al. (Cost)-effectiveness of family meetings on indicated prevention of anxiety and depressive symptoms and disorders of primary family caregivers of patients with dementia: design of a randomized controlled trial. BMC Geriatr. 2008;8: 2 10.1186/1471-2318-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Joling KJ, van Marwijk HWJ, Smit F, van der Horst HE, Scheltens P, van de Ven PM, et al. Does a family meetings intervention prevent depression and anxiety in family caregivers of dementia patients? A randomized trial. PloS One. 2012;7: e30936 10.1371/journal.pone.0030936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laakkonen M-L, Savikko N, Hölttä E, Tilvis R, Strandberg T, Kautiainen H, et al. Self-management groups for people with dementia and their spousal caregivers. A randomized, controlled trial. Baseline findings and feasibility. Eur Geriatr Med. 2013;4: 389–393. [Google Scholar]
- 51.Meeuwsen E, Melis R, van der Aa G, Golüke-Willemse G, de Leest B, van Raak F, et al. Cost-effectiveness of one year dementia follow-up care by memory clinics or general practitioners: economic evaluation of a randomised controlled trial. PloS One. 2013;8: e79797 10.1371/journal.pone.0079797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meeuwsen EJ, German P, Melis RJF, Adang EM, Golüke-Willemse GA, Krabbe PF, et al. Cost-effectiveness of post-diagnosis treatment in dementia coordinated by Multidisciplinary Memory Clinics in comparison to treatment coordinated by general practitioners: an example of a pragmatic trial. J Nutr Health Aging. 2009;13: 242–248. [DOI] [PubMed] [Google Scholar]
- 53.Meeuwsen EJ, Melis RJF, Van Der Aa GCHM, Golüke-Willemse GAM, De Leest BJM, Van Raak FHJM, et al. Effectiveness of dementia follow-up care by memory clinics or general practitioners: randomised controlled trial. BMJ. 2012;344: e3086 10.1136/bmj.e3086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schwarzkopf L, Menn P, Kunz S, Holle R, Lauterberg J, Marx P, et al. Costs of care for dementia patients in community setting: an analysis for mild and moderate disease stage. Value Health. 2011;14: 827–835. 10.1016/j.jval.2011.04.005 [DOI] [PubMed] [Google Scholar]
- 55.Holle R, Grässel E, Ruckdäschel S, Wunder S, Mehlig H, Marx P, et al. Dementia care initiative in primary practice: study protocol of a cluster randomized trial on dementia management in a general practice setting. BMC Health Serv Res. 2009;9: 91 10.1186/1472-6963-9-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145: 727–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rubenstein LZ, Alessi CA, Josephson KR, Trinidad Hoyl M, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc. 2007;55: 166–174. 10.1111/j.1532-5415.2007.01044.x [DOI] [PubMed] [Google Scholar]
- 58.Samus QM, Johnston D, Black BS, Hess E, Lyman C, Vavilikolanu A, et al. A multidimensional home-based care coordination intervention for elders with memory disorders: the Maximizing Independence at Home (MIND) pilot randomized trial. Am J Geriatr Psychiatry. 2014;22: 398–414. 10.1016/j.jagp.2013.12.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Amjad H, Wong SK, Roth DL, et al. Health Services Utilization in Older Adults with Dementia Receiving Care Coordination: The MIND at Home Trial [published online January 12, 2017]. Health Serv Res 10.1111/1475-6773.12647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Søgaard R, Sørensen J, Waldorff FB, Eckermann A, Buss DV, Waldemar G. Cost analysis of early psychosocial intervention in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2014;37: 141–153. 10.1159/000355368 [DOI] [PubMed] [Google Scholar]
- 61.Søgaard R, Sørensen J, Waldorff FB, Eckermann A, Buss DV, Phung KTT, et al. Early psychosocial intervention in Alzheimer’s disease: cost utility evaluation alongside the Danish Alzheimer’s Intervention Study (DAISY). BMJ Open. 2014;4: e004105 10.1136/bmjopen-2013-004105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Waldemar G, Waldorff FB, Buss DV, Eckermann A, Keiding N, Rishøj S, et al. The Danish Alzheimer intervention study: rationale, study design and baseline characteristics of the cohort. Neuroepidemiology. 2011;36: 52–61. 10.1159/000322942 [DOI] [PubMed] [Google Scholar]
- 63.Thyrian JR, Fiß T, Dreier A, Böwing G, Angelow A, Lueke S, et al. Life- and person-centred help in Mecklenburg-Western Pomerania, Germany (DelpHi): study protocol for a randomised controlled trial. Trials. 2012;13: 56 10.1186/1745-6215-13-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dreier A, Thyrian JR, Eichler T, Hoffmann W. Qualifications for nurses for the care of patients with dementia and support to their caregivers: A pilot evaluation of the dementia care management curriculum. Nurse Educ Today. 2016;36: 310–317. 10.1016/j.nedt.2015.07.024 [DOI] [PubMed] [Google Scholar]
- 65.Wray LO, Shulan MD, Toseland RW, Freeman KE, Vásquez BE, Gao J. The effect of telephone support groups on costs of care for veterans with dementia. Gerontologist. 2010;50: 623–631. 10.1093/geront/gnq040 [DOI] [PubMed] [Google Scholar]
- 66.Shah H, Albanese E, Duggan C, Rudan I, Langa KM, Carrillo MC, et al. Research priorities to reduce the global burden of dementia by 2025. Lancet Neurol. 2016;15: 1285–1294. 10.1016/S1474-4422(16)30235-6 [DOI] [PubMed] [Google Scholar]
- 67.Nici L, Bontly TD, Zuwallack R, Gross N. Self-management in chronic obstructive pulmonary disease. Time for a paradigm shift? Ann Am Thorac Soc. 2014;11: 101–107. 10.1513/AnnalsATS.201306-150FR [DOI] [PubMed] [Google Scholar]
- 68.Amjad H, Carmichael D, Austin AM, Chang C-H, Bynum JPW. Continuity of Care and Health Care Utilization in Older Adults With Dementia in Fee-for-Service Medicare. JAMA Intern Med. 2016;176: 1371–1378. 10.1001/jamainternmed.2016.3553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Costa A, Harkness K, Haughton D, Heckman G, S McKelvie R. Risk of emergency department use among community-dwelling older adults: A review of risk factors and screening methods. Clin Pract. 2014;11: 763–776. [Google Scholar]
- 70.Toot S, Devine M, Akporobaro A, Orrell M. Causes of hospital admission for people with dementia: a systematic review and meta-analysis. J Am Med Dir Assoc. 2013;14: 463–470. 10.1016/j.jamda.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 71.Sloane PD, Schifeling CH, Beeber AS, Ward KT, Reed D, Gwyther LP, et al. New or Worsening Symptoms and Signs in Community-Dwelling Persons with Dementia: Incidence and Relation to Use of Acute Medical Services. J Am Geriatr Soc. 2017;65: 808–814. 10.1111/jgs.14672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ledgerd R, Hoe J, Hoare Z, Devine M, Toot S, Challis D, et al. Identifying the causes, prevention and management of crises in dementia. An online survey of stakeholders. Int J Geriatr Psychiatry. 2016;31: 638–647. 10.1002/gps.4371 [DOI] [PubMed] [Google Scholar]
- 73.Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev. 2011;68: 131–155. 10.1177/1077558710379422 [DOI] [PubMed] [Google Scholar]
- 74.Toot S, Hoe J, Ledgerd R, Burnell K, Devine M, Orrell M. Causes of crises and appropriate interventions: the views of people with dementia, carers and healthcare professionals. Aging Ment Health. 2013;17: 328–335. 10.1080/13607863.2012.732037 [DOI] [PubMed] [Google Scholar]
- 75.Hanson LC, Zimmerman S, Song M-K, Lin F-C, Rosemond C, Carey TS, et al. Effect of the Goals of Care Intervention for Advanced Dementia: A Randomized Clinical Trial. JAMA Intern Med. 2017;177: 24–31. 10.1001/jamainternmed.2016.7031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013; CD007760 10.1002/14651858.CD007760.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dwan K, Gamble C, Williamson PR, Kirkham JJ, Reporting Bias Group. Systematic review of the empirical evidence of study publication bias and outcome reporting bias—an updated review. PloS One. 2013;8: e66844 10.1371/journal.pone.0066844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chan A-W, Hróbjartsson A, Haahr MT, Gøtzsche PC, Altman DG. Empirical evidence for selective reporting of outcomes in randomized trials: comparison of protocols to published articles. JAMA. 2004;291: 2457–2465. 10.1001/jama.291.20.2457 [DOI] [PubMed] [Google Scholar]
- 79.Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;3: CD006560 10.1002/14651858.CD006560.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lin JS, Whitlock EP, Eckstrom E, Fu R, Perdue LA, Beil TL, et al. Challenges in synthesizing and interpreting the evidence from a systematic review of multifactorial interventions to prevent functional decline in older adults. J Am Geriatr Soc. 2012;60: 2157–2166. 10.1111/j.1532-5415.2012.04214.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
S1 file legend:
Appendix A: Detailed eligibility criteria of intervention.
Appendix B: Medline full electronic search strategy.
Appendix C: Detailed origin, transformation or imputation of reported data.
Table A: Origin, transformation or imputation of data for proportions of persons having at least one Emergency Department visit.
Table B: Origin, transformation or imputation of data for mean number of Emergency Department visit.
Table C: Origin, transformation or imputation of data for proportions of persons having at least one hospital admission.
Table D: Origin, transformation or imputation of data for mean number of hospital admission.
Table E: Origin, transformation or imputation of data for mean number of hospital days.
Fig A. Proportion of persons having at least one Emergency Department visit (Risk Ratio and Risk Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; RD, Risk Difference; RR, Risk Ratio.
Fig B. Proportion of persons having at least one hospital admission (Risk Ratio and Risk Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; RD, Risk Difference; RR, Risk Ratio.
Fig C. Mean number of Emergency Department visit (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig D. Mean number of hospital admission (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig E. Mean number of hospital days (Mean Difference). A. At 12 months. B. At the longest follow-up. Abbreviations: CI, Confidence Interval; MD, Mean Difference; SD, Standard Deviation.
Fig F. Quality Appraisal using the Cochrane Risk of Bias Tool. a Random sequence generation (selection bias). b Allocation concealment (selection bias). c Blinding of participant and personnel (performance bias). d Blinding of outcome assessment. e Incomplete outcome data (attrition bias). f Selective reporting (reporting bias). g Other bias. h Questions marks, uncertain risk of bias; + signs, low risk of bias;—signs, high risk of bias.
References.
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.