Summary
Burns are considered an important preventable fraction of injuries in low and middle-income countries, and are still a leading cause of death in Iran. This study investigates features of burns in Sina Hospital’s Burn Centre in East Azerbaijan Province in order to calculate survival and mortality rates as well as factors affecting mortality in this centre. In this cross-sectional study, demographic characteristics of patients such as age, sex, cause of burns, type of burns, length of stay (LOS) in the hospital, total body surface area (TBSA), anatomic distribution of burn, mortality rate and final status of patients at the time of discharge from hospital (recovery, death) were investigated. The total mortality rate was 6.84%. Hot liquid burns and gas cylinder explosion burns were among the most common. Burns on multiple regions of the body (45.9%) and pelvic and lower limb burns (22%) constituted the next most common injury. In the TBSA index, compared to reference categories (extent of burn less than 50 percent), the categories of 50-59, 60-69, 70-79, 80-89 and over 90 percent indicated lowest survival based on the Log-Rank test. Hazard ratio for burns greater than 10% was 15.33 fold. Total body surface area burned of over 10% constantly increases the instantaneous risk of mortality therefore there is a need to enhance the quality of care provided to burn victims.
Keywords: body surface area, burns, injuries, mortality rate
Abstract
Les brûlures sont considérées comme des accidents hautement évitables dans les pays à IDH bas et moyen. Elles restent une cause majeure de décès en Iran. Cette étude détaille les caractéristiques des brûlés hospitalisés dans le CTB de l’hôpital Sina (province iranienne d’est Azerbaïdjan) afin d’en évaluer la mortalité et les facteurs l’influençant. Dans cette étude transversale, nous avons analysé l’âge et le sexe des patients, la cause de la brûlure, la surface atteinte et la localisation, la durée d’hospitalisation et la mortalité. Celle – ci était de 6,84%, elle était plus élevée au-delà de 50% SCT brûlée (Log Rank). Le risque de mortalité est multiplié par 15,33 au-delà de 10% de SCT, limite de surface nécessitant donc des soins spécifiques. Les 2 causes les plus fréquentes étaient les ébouillantements et les explosions de gaz. Les atteintes disséminées (45,9%) ainsi que celles de la région pelviennes et des membres inférieurs (22%) prédominaient.
Introduction
Burns are the fourth leading traumatic event in the world after traffic accidents, falls and violence among individuals.1 They involve threats such as a decrease in quality of life, increasing disability and death.2 According to the World Health Organization (WHO), every year more than 300,000 people die from fire-related burns worldwide, with the highest deaths from burning occurring in Southeast Asia and the Middle East.3 Currently, 90% of burns occur in moderate- and low-income countries due to a lack of facilities and failings in the management of this event.4 In our country 24,000-28,000 burn victims need hospitalization annually.5 In Iran, the annual mortality rate for burns is 4.6-5.6 per 100,000 people6 and nearly 9% of burn victims die.7 In an international burn study, 8% of the survivors suffered permanent disability.8
In Iran the cost of hospital admission has increased lately by an average of 606 $ per burn patient.9 The highest treatment costs for burn patients are incurred at initial admission, however these costs subsequently decrease. In various studies in the country, the average duration of hospitalization was reported to range from 8 to 16.7 days.10,11 The results of a study conducted in 12 Iranian universities indicate that the extent of burn rate among the rural population of Iran is higher than among the urban population.12 Due to their lower possibility of access to treatment facilities, mortality rate resulting from burns is higher among rural patients than urban patients.13
Second and third-degree burns are the most common type of burn.14 Ninety-eight percent of burns occur unintentionally.12 While heat burns caused by flames, hot liquids and hot objects are the most common type of burns, chemical burns are the least common4 in all studies. The most common cause of burns in hospital and deathbased studies was related to direct contact with flame.14 It is noteworthy that burns caused by electric shock and chemical substances are more common among men in the workplace.15
The extent and severity of TBSA burned are the most important predictors of death in burn patients. 4 Average TBSA was generally over 60% in cases that resulted in death, and lower than 30% in non-fatal cases in Iran.12 From 2010 to 2014, the LA50 index dropped from 9% to 3.48% among patients in the Sina Hospital.4
There are 15 specialized burn centres in Iran, one of which is Sina Hospital in East Azerbaijan Province in the northwest of Iran, which provides burn care services for an approximate population of 3,724,620.14 This hospital is one of the largest referral centres in the north-western region of Iran.
The aim of this study was to determine lethality in this centre by calculating the survival rate and some of the factors affecting mortality among burn victims in East Azerbaijan province, Iran.
Methods
This cross-sectional study surveyed all cases of acute burns occurring over one year from April 1, 2016 to the end of March 2016. A total of 1666 patients were admitted to hospital. All patients from different age groups and both genders with acute burns that resulted in admission or referral within 48 hours from another centre where they had not received any specialized care were included in the present study. Chronic burns, people treated as outpatients, patients who were referred for reconstructive services from other treatment centres, as well as 48 patients who did not meet our inclusion criteria were excluded from the study.
Demographic characteristics of patients such as age, sex, cause of burns, type of burns, length of stay (LOS) in the hospital, total body surface area (TBSA), anatomic distribution of burn, mortality rate, and final status of patients at the time of discharge from hospital (recovery, death) were among the variables studied.
In addition, LA50 of patients in each age group was calculated by determining the relationship between total body surface area and mortality rate.
Injury-related data were collected based on the classifications determined in the International Classification of Diseases (ICD-10). Injured site of the body and nature of the injury, Chapter XIX of ICD-10, was followed. External causes of morbidity and mortality of burns were reported based on chapter XX.
Data analysis
Central indices were reported with mean (standard deviation) or median (intra-quartile range). Normal distribution of continuous variables was measured by the Shapiro-Wilk test. The difference between the groups was calculated by independent t-test or Wilcoxon rank-sum two-sample. Pvalues less than 0.05, or Interval Confidence that did not include one hypothesis, were considered as statistically significant. The variables were studied in two models: univariable and multivariate models were entered into the final model with the Enter method. The preconditions for Cox regression include censorship assumptions (the censorship of the subjects is random and not related to the event being investigated) and constancy of relative risk (constancy of relative risk over time in the groups to be compared), which were investigated and established. Statistical analysis was performed by SPSS software version 21 together with the statistical software Stata version 14 (STATA Corp, College Station, TX, USA).
Results
The mean age of the injured persons was 30.38 (19.80), confidence range of average age was 29.42-31.33, and the minimum and the maximum age were 24 months and 96 years, respectively.
During this study, a total of 1618 acute burns were recorded. Eight hundred and fifty-four burns occurred in men and the ratio of burn in men compared to women was 10.05. The mean hospitalization time was 9.04 (9.80) days, the median admission was 7 days, and the percentiles 25 and percentiles 75 were 4-1, respectively. The total mortality rate was 6.84% and these values were 3.18% in the under 16 age group, 7.98% in the 16 to 44 age group, 7.11% in the 44-64 age group, and 12.04% in the over 64 age group. These findings suggest a meaningful relationship between age group and mortality rate: that is to say, age seems to be a negative confounder that might increase mortality rate.
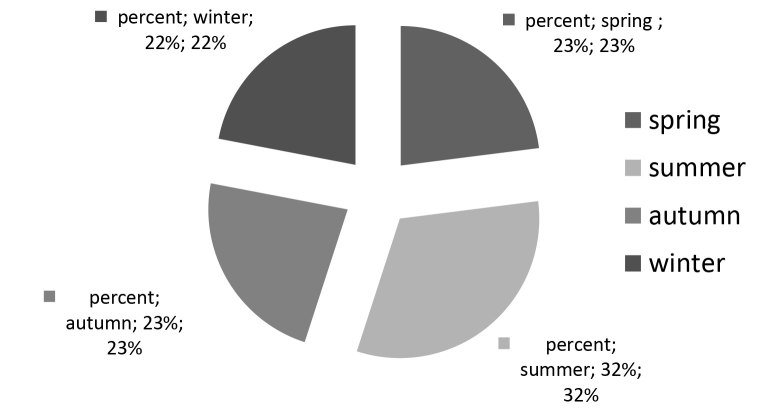
The majority of burns had occurred between 12.00-18.00 hours (37.58%) and 18.00-24.00 hours (32.23%). As Fig. 1 indicates, the majority of burn cases occurred during the warm season of the year, that is, in summer.
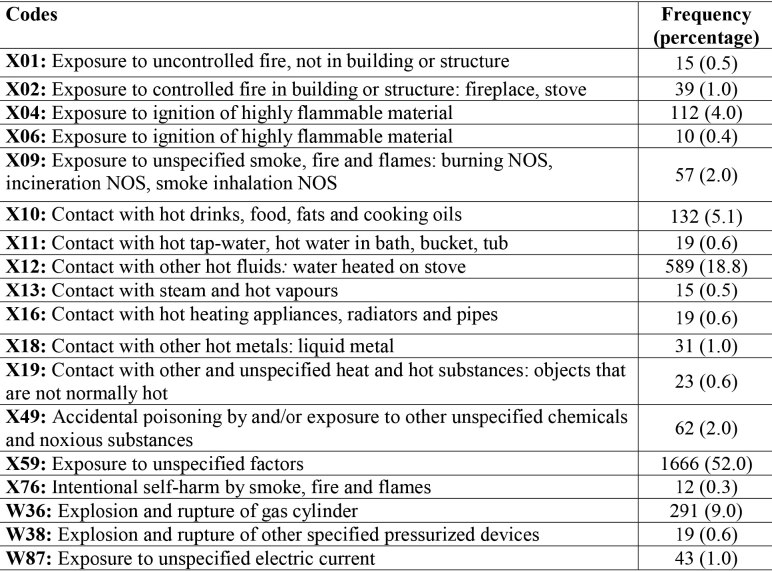
Apart from the X59 code which included exposure to unspecified factors, hot liquid burns (code X12) and gas cylinder explosion burns (code W36) were among the most common cases. (Table I).
Fig. 1. Diagram of burn cases recorded at the Sina Hospital, East Azerbaijan province (Iran), 2016, by season.
Table I. Chapter XX: external causes of morbidity and mortality in the Sina Hospital in East-Azerbaijan province (Iran), in 2016.
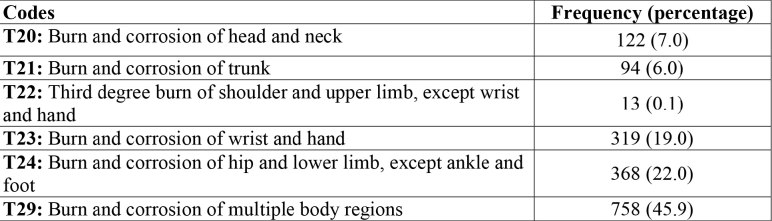
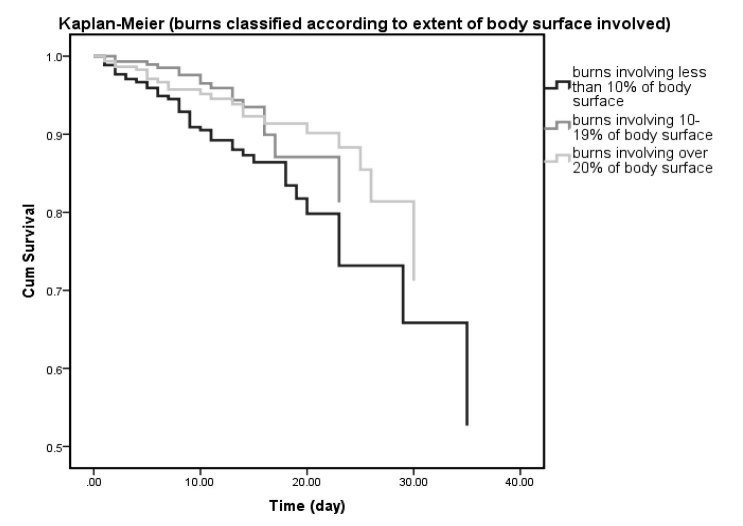
Based on Chapter XIX of ICD-10, burns on multiple body regions (45.9%) and pelvic and lower limb burns (22%) constituted the most common burns, as shown in Table II. In the TBSA index, compared to reference categories (burn extent of less than 50 percent), the categories 50-59, 60-69, 70-79, 80-89 and over 90 percent showed the lowest survival rate based on the Log-Rank test (Fig. 2).
Table II. Chapter XX: external causes of morbidity and mortality in the Sina Hospital in East-Azerbaijan province (Iran), in 2016.
Fig. 2. Comparison of survival rates based on the extent of burn among cases recorded at the Sina Hospital, East Azerbaijan province (Iran), 2016.
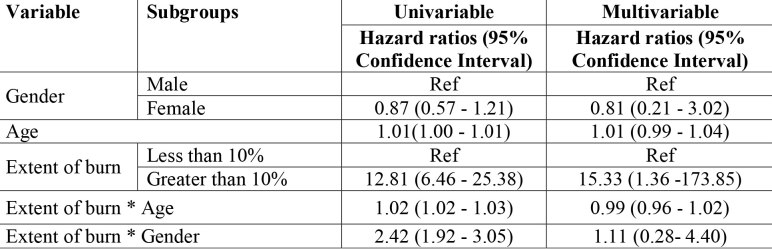
LA50 findings showed that the highest values for the age groups 16-44 and over 65 years old were 42.2% and 21.3%, respectively. Apparently this was lower compared to other age groups. Based on Table III, the assumption of Schoenfeld residuals test for proportional hazards (phtest) was met for all three variables in the multivariable model (p-value=0.532). Moreover, the variables were entered into the univariable model and the significant variables from the univariable model were entered into the multivariable model where the interaction variables were included in the model (i.e. full model). This model was selected as the final model. In order to compensate for sparse data and solve the problem, in the present regression models the extent of burns over 10 percent was combined; both univariable and multivariable models were significant. The hazard ratio for burns greater than 10% compared to the reference category i.e. burns less than 10%, was 15.33 fold, indicating that burn extent of over 10% has a much greater effect on risk of mortality than a burn extent of less than 10%.
Table III. Chapter XX: external causes of morbidity and mortality in the Sina Hospital in East-Azerbaijan province (Iran), in 2016.
Discussion
In Iran, the high prevalence of burns and deaths or resulting disabilities highlights burns to be a major public health problem which demands that country-wide epidemiological studies be carried out.16 The present study analyzed 1618 burn cases referred and admitted to the Sina Academic Burn Centre in the year 2016.
The average age of the patients with burn injuries was 30.38. The mean age of patients may vary with regard to the study group. For example, in Nepal working-age groups are between 15 and 60.17 In research by Kazemzadeh on 1717 pediatric patients the mean age was 4.11 ± 3.42 yrs,18 and in a study conducted in a major burn centre in Southern Iran, the mean age of admissions was 27.2±23.65 years.19 According to the findings of this study, the frequency of death in women and men was 35.9% and 18.4%, respectively; in other words, the ratio of burns in males to females was 1.05. In one population-based epidemiological study conducted in Tehran-Iran, the majority of non-fatal injuries happened among men.20 However in India21 men are more likely to be burned in the workplace and women at home, especially in the kitchen. In most of the previous studies carried out in Iran, the highest percentage of burns occurred in men. Burns resulting from work mostly occur in male rather than in female workers as men are more likely to be employed in outdoor workplaces.22
Burns in children mainly occur accidentally.18 The probability of intentional burns, especially self-immolation (97% in women), or burns caused during disputes, increases with age.20 Contact and exposure to burn factors might mostly occur in newly married young couples because of their insufficient experience and encounter with unsafe situations. The findings of the study showed that the ratio of burns in males to females was 1.05. In India,21 men are more likely to be burned in the workplace and women at home and in the kitchen. In most of the previous studies carried out in Iran, the highest percentage of burns occurred in men. Burns resulting from work mostly occur in male rather than female workers as men are more likely to be employed in outdoor workplaces.22 Sadeghi-Bazarghani et al.12 observed that intentional burns mostly occur in women and are also associated with a high mortality rate. For men, it seems that their greater risk-taking behaviour and their presence in hazardous environments are responsible for more burns.
Mortality rate was estimated with prospective studies rather than with cross-sectional ones. It is noteworthy that preventive measures and training courses on the emergency management of severe burns (EMSB) were effective in decreasing mortality rate for burn injuries and TBSA burned.4 In the present study, the total mortality rate was 6.84% while in a Dutch study carried out by Jan Dokter it was 3.2%. Patients who died during the study were often over 65 years old.23
Based on Cox regression analysis, TBSA>10% was one of the significant variables for mortality in patients. Multivariate analysis indicated that mortality rate increased with patient age. Moreover, the hazard ratio for burn extent, associated with burns greater than 10%, is 15.33, indicating that a burn extent of over 10% has a much greater effect on risk of mortality than a burn extent of less than 10%.
The findings of the present study agree with a study conducted in Tabriz where adolescence, illiteracy, unemployment, residing in rural areas, low socioeconomic status and percentage of TBSA burned were found to be effective factors in increasing mortality rate.4 On the other hand, improving the service during the course of cohort studies and a long study period were effective in reducing burn injuries.24 In the present study, multivariate analysis showed that mortality rate increases by one percent for each year, which shows a borderline significance (0.99 to 1.04). Although the interaction effect was significant between the age factor and TBSA in univariate analysis, the interference between TBSA and age was not significant in the final Cox model, although it was meaningful in single-variable analysis 0.99 (0.96 - 1.02).
Based on the findings of the present study, hot liquids followed by gas cylinder explosion were the most common causes of burn. In Nepal,17 flame burn was the main cause (66%), followed by scald (21.6%). Scald burn was more common in children. In a study conducted on children in Mexico, explosions of tankers and gas transmission lines and fire stations were reported to be the major causes of burn.25 In Zanjan, Iran, 53.6% of accidents occurred as a result of flame burns.26 Fluids and hot food were found to be the leading cause of burn among children under 10 years of age, whereas fuels and igniters were the main causes of burn among adolescents and older age groups.27
As regards the different parts of the body affected, the hip is the most burned area, involved in 45.9% of burn incidents, followed by thigh with 22% and wrist and hand with 19% (Chap. XIX of ICD-10). According to the log-rank test, the lowest survival rate was seen for this category compared to extent of burn less than 50%. In a study by Dokter, the main cause of death was the same as in the present study: multi-organ failure.23 LA50 findings revealed that the highest values were 42.2% and 21.3% for the over 16-44 years and over 65 years age groups, respectively, which were lower than values for other age groups. In another study conducted in Birjand, Iran, LA50 findings with 55% indicated that the nature of burn (deliberateness) (OR: 12.26 CI: 4.26-30.28), and burned body surface over 40% (OR: 31.65 CI: 13.71-73.06), as burn predicting factors, were associated with mortality.28 In the study by Dastgiri et al., patients with TBSA of more than 75% had a greater mortality rate. Burns on the head and neck, trunk and upper extremity increase the mortality risk.29 Cross-sectional studies do not compare with the efficacy of prospective studies in estimating mortality rate, and the present study is not an exception in this regard. Epidemiological studies of burns should not be restricted to studying limited groups such as children or elderly people.22
Limitations
It should be noted that mild burns treated in lower level burn centres on the basis of the country’s referral system or burns that were not referred to a hospital were not included in the present study.
Acknowledgments
Ethical issues.This study was approved by the Human Subjects Committee of Tabriz University of Medical Sciences. The study protocol was approved by the Tabriz Health Services Management Research Center in Tabriz University of Medical Sciences.
Data availability.Data on which this article was written may be available as innominate data upon request and approval from East Azerbaijan Province, the Tabriz Health Services Management Research Center in Tabriz University of Medical Sciences.
Conflict of interest.All authors declare that they have no conflict of interest.
Financial Disclosure.There were no sources of extra-institutional commercial findings.
Funding.None.
Acknowledgment.The authors would like to thank all personnel of the Sina Burn Hospital of Tabriz University of Medical Sciences for their cooperation.
References
- 1.Peck MD, Jeschke M. Epidemiology of burn injuries globally. Burns. 2011;37(7):1087–1274. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Arshi S, Sadeghi-Bazargani H, Mohammadi R, Ekman R. Prevention oriented epidemiologic study of accidental burns in rural areas of Ardabil, Iran. Burns. 2006;32(3):366–371. doi: 10.1016/j.burns.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 3.Seyed-Forootan K, Karimi H, Motevalian S, Momeni M. LA50 in burn injuries. Ann Burns Fire Disasters. 2016;29(1):14. [PMC free article] [PubMed] [Google Scholar]
- 4.Aghazadeh AM, Lotfi M, Ghahramanian A, Ahadi F. Lethal area 50 in patients with burn injuries in North West, Iran. J Caring Sci. 2018;7(1):53. doi: 10.15171/jcs.2018.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadeghi-Bazargani H, Maghsoudi H, Soudmand-Niri M, Ranjbar F, Mashadi-Abdollahi H. Stress disorder and PTSD after burn injuries: a prospective study of predictors of PTSD at Sina Burn Center, Iran. Neuropsych Dis Treat. 2011;7:425. doi: 10.2147/NDT.S23041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Othman N, Kendrick D. Epidemiology of burn injuries in the East Mediterranean Region: a systematic review. BMC Public Health. 2010;10(1):83. doi: 10.1186/1471-2458-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karimi H, Momeni M, Motevalian A, Bahar M. The burn registry program in Iran - First Report. Ann Burns Fire Dis. 2014;27(3):154. [PMC free article] [PubMed] [Google Scholar]
- 8.Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns. 2011;37(7):1087–1100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Ghaffari-fam S, Sarbazi E, Daemi A, Sarbazi MR. The epidemiological characteristics of motorcyclists associated injuries in road traffic accidents: a hospital-based study. Bull Emerg Trauma. 2016;4(4):223. [PMC free article] [PubMed] [Google Scholar]
- 10.Ghaffari-Fam S, Sarbazi E, Daemi A, Sarbazi M. Epidemiological and clinical characteristics of fall injuries in East Azerbaijan, Iran: a cross-sectional study. Bull Emerg Trauma. 2015;3(3):104. [PMC free article] [PubMed] [Google Scholar]
- 11.Salari-Lak S, Sadeghi-Bazargani H, Daemi A. Some epidemiological aspects of pedestrian injuries in road traffic injuries in the Imam Reza University Hospital, East Azerbaijan, Iran. Trauma Epidemiology Journal. 2016;1(1):1–7. [Google Scholar]
- 12.Sadeghi-Bazargani H, Mohammadi R. Epidemiology of burns in Iran during the last decade (2000–2010): review of literature and methodological considerations. Burns. 2012;38(3):319–329. doi: 10.1016/j.burns.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 13.Navarrete N, Rodriguez N. Epidemiologic characteristics of death by burn injury from 2000 to 2009 in Colombia, South America: a population-based study. Burns Trauma. 2016;4(1):8. doi: 10.1186/s41038-016-0033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maghsoudi H, Ghaffari A. Aetiology and outcome of elderly burn patients in Tabriz, Iran. Ann Burns Fire Disasters. 2009;22(3):115. [PMC free article] [PubMed] [Google Scholar]
- 15.Maghsoudi H, Samnia N. Etiology and outcome of pediatric burns in Tabriz, Iran. Burns. 2005;31(6):721–725. doi: 10.1016/j.burns.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Sadeghi-Bazargani H, Samadirad B, Moslemi F. A decade of road traffic fatalities among the elderly in north-west Iran. BMC Public Health. 2018;18(1):111. doi: 10.1186/s12889-017-4976-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karki B, Rai SM, Nakarmi KK, Basnet SJ. Clinical epidemiology of acute burn injuries at Nepal Cleft and Burn Centre, Kathmandu, Nepal. Ann Plast Surg. 2018;80(3):S95–S97. doi: 10.1097/SAP.0000000000001270. [DOI] [PubMed] [Google Scholar]
- 18.Kazemzadeh J, Vaghardoost R, Dahmardehei M, Rabiepoor S. Retrospective epidemiological study of burn injuries in 1717 pediatric patients: 10 years analysis of hospital data in Iran. Iran J Public Health. 2018;47(4):584. [PMC free article] [PubMed] [Google Scholar]
- 19.Keshavarzi A, Kardeh S, Pourdavood A, Mohamadpour M, Dehghankhalili M. Determinants of the lethal area 50 index (LA50) in burn patients admitted to a tertiary referral burn center in Southern Iran. Bull Emerg Trauma, 2018;6(1):59. doi: 10.29252/beat-060109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hashemi E, Zangi M, Sadeghi-Bazargani H, Soares J. Population-based epidemiology of non-fatal injuries in Tehran, Iran. Health Promot Perspect. 2018;8(2):127. doi: 10.15171/hpp.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srivastava S, Kumari H, Singh A, Rai RK. Epidemiology and outcomes of electric burn injury: a study of 768 patients in a high volume tertiary care centre of North India. Int J Community Med Public Health. 2018;5(7):2786–2790. [Google Scholar]
- 22.Sadeghi-Bazargani H, Mohammadi R, Svanstrom L, Ekman R. Epidemiology of minor and moderate burns in rural Ardabil, Iran. Burns. 2010;36(6):933–937. doi: 10.1016/j.burns.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 23.Dokter J, Felix M, Krijnen P, Vloemans JF. Mortality and causes of death of Dutch burn patients during the period 2006–2011. Burns. 2015;41(2):235–240. doi: 10.1016/j.burns.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Åkerlund E, Huss FR, Sjöberg F. Burns in Sweden: an analysis of 24 538 cases during the period 1987–2004. Burns. 2007;33(1):31–36. doi: 10.1016/j.burns.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 25.Patel DD, Rosenberg L, Rosenberg M, Leal J. The epidemiology of burns in young children from Mexico treated at a US hospital. Burns. 2016;42(8):1825–1830. doi: 10.1016/j.burns.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 26.Ahmadi A, Mohammadi R, Stavrinos D, Almasi A, Schwebel DC. Self-immolation in Iran. J Burn Care Res. 2008;29(3):451–460. doi: 10.1097/BCR.0b013e31817112f1. [DOI] [PubMed] [Google Scholar]
- 27.Ghorbani F, Shiri M, Mortaqhy GM, Ansari P, Mohammadi F. Epidemiologic study of burn patients hospitalized in Mousavi Hospital, Zanjan 2010-2012. Preventive Care in Nursing and Midwifery Journal. 216;5(2):65–74. [Google Scholar]
- 28.Tabiee S, Nakhaee M. Epidemiology of burn patients in Emam Reza Hospital, Birjand, 1998–2002. Journal of Shahrekord University of Medical Sciences. 2004;6(1):43–51. [Google Scholar]
- 29.Dastgiri S, Kalankesh LR, Pourafkary N, Vahidi R, Mahmoodzadeh F. Incidence, survival pattern and prognosis of selfimmolation: a case study in Iran. J Public Health. 2006;14(1):2–6. [Google Scholar]