Abstract
OBJECTIVES:
To determine whether treating depression decreases mortality from various chronic medical conditions.
DESIGN:
Long-term follow-up of multisite-practice randomized controlled trial (Prevention of Suicide in Primary Care Elderly: Collaborative Trial).
SETTING:
Twenty primary care practices randomized to intervention or usual care.
PARTICIPANTS:
Individuals aged 60 and older identified through depression screening of random patients (N = 1,226).
INTERVENTION:
For 2 years, a depression care manager worked with primary care physicians in intervention practices to provide algorithm-based care for depression.
MEASUREMENTS:
Mortality risk based on a median follow-up of 98 months (range 0.8–116.4 months) through 2008; chronic medical conditions ascertained through self-report.
RESULTS:
For heart disease, persons with major depression were at greater risk of death, whether in usual-care or intervention practices. Older adults with major depression and diabetes mellitus in practices randomized to the intervention condition (hazard ratio = 0.47, 95% confidence interval = 0.24–0.91) were less likely to die. For other medical conditions, the point estimates for risk of death in persons with major depression were all in the direction of indicating lower risk in intervention practices but did not reach statistical significance.
CONCLUSION:
Older adults with depression and medical comorbidity pose a significant clinical and public health challenge. Evidence was found of a statistically significant intervention effect on mortality for diabetes mellitus in persons with major depression.
Keywords: depression, medical comorbidity, primary care, randomized clinical trial
Depression and chronic medical conditions are commonly encountered in primary care settings. It has been mechanisms such as inflammation and poor self-care and poor adherence to treatment regimens.2 recommended that people with medical comorbidity be considered a distinct population with many common clinical features.1 The association between depression and outcomes of chronic medical conditions includes biological Although some randomized trials of depression interventions have reported on mortality outcomes, most notably focused on heart disease, few studies have examined whether treating depression decreases mortality in various chronic medical conditions.
The Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) was a multisite effectiveness trial designed to assess the effect of the use of care management on reducing major risk factors for suicide in late life, primarily depression.3 Depression care management has been shown to be effective in a range of primary care practices that serve people with diverse sociodemo-graphic and clinical characteristics.3–5 In older adults with major depression, the intervention was associated with improvement in depressive symptoms, remission, and suicidal ideation.3 Specifically, a significantly larger proportion of intervention participants with major depression responded to treatment, defined as a 50% or greater decrease in symptoms (e.g., from 42.7% to 29.1% at 4 months). Remission, defined as achieving symptom reduction below a predetermined threshold, was more common in participants with major depression in intervention practices (e.g., from 40.0% to 22.5% at 4 months). The beneficial effects on depression remission persisted at 24 months, with 45.4% with major depression in intervention practices in remission (vs 31.5% in usual care).6
It was previously reported that overall mortality was lower in the intervention practices of PROSPECT,7 but it is natural to ask whether persons with specific medical conditions were more or less likely to benefit from the depression management program. The opportunity that PROSPECT afforded to compare mortality in persons with specific medical conditions in intervention practices with that of those in usual care was taken. Subgroup analysis defined according to medical condition must be interpreted with caution,8 but doing so does address an important clinical question: Does a depression management program improve mortality in older adults with specific medical conditions in primary care? Because of the diverse mechanisms linking depression with medical comorbidity, the primary hypothesis was that the intervention would have an effect regardless of the specific medical condition.
METHODS
Study Sample
PROSPECT was a cluster-randomized controlled trial comparing a primary care–based intervention with usual care to improve outcomes of depression.3,9,10 Individuals aged 60 and older who gave oral consent were screened for enrollment using the Centers for Epidemiologic Studies Depression Scale (CES-D). All who scored higher than 20 on the CES-D were invited to participate in the study, as well as a 5% random sample of individuals with lower scores including those without depression.11 This study received approval from the institutional review boards at all collaborating universities and independent review at the National Center for Health Statistics.
Usual Care and Intervention Conditions
Practices randomized to usual care received educational sessions for primary care physicians and notification of the depression status of participants. Physicians received no specific recommendations regarding individual participants (except for psychiatric emergencies). Practices randomized to the intervention condition received educational sessions for primary care physicians, education of participants’ families, and a depression care manager who worked within the practice.
Clinical Assessment of Depression
Trained research assistants used the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) to diagnose major depressive disorder. Clinically significant minor depression was defined as meeting DSM-IV criteria for minor depression with four depressive symptoms, a Hamilton Depression Rating Scale score of 10 or higher, and duration of symptoms of 4 weeks or longer.12 A Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) was conducted for all participants. Participants who did not meet criteria for depression continued to be followed. Physicians received written notification of the depression status of participants based on the SCID assessment.
Assessment of Medical Conditions
Self-report of medical conditions was based on the Charlson Comorbidity Index,13 supplemented by questions about common disabling conditions of late life. Heart disease was defined as reporting any of five conditions: myocardial infarction, heart failure, angina pectoris, angioplasty or coronary artery bypass surgery, and atrial fibrillation. High blood pressure, peripheral vascular disease, stroke, diabetes mellitus, cancer, and chronic pulmonary disease were considered separately.
Covariates Under Study
Sociodemographic characteristics were assessed using standard questions regarding age, sex, self-identified ethnicity, level of education attainment, and marital status. Smoking status was based on report of smoking within 6 months of the interview. The Mini-Mental State Examination was used to assess orientation to time and place, registration, memory, attention and concentration, praxis, and constructional and language capacity. Severity of depression was assessed using the 24-item Hamilton Depression Rating Scale. The presence of suicidal ideation was assessed using the Scale for Suicidal Ideation.
Ascertainment of Vital Status
Vital status was based on participant follow-up using the National Center for Health Statistics National Death Index.14 Written consent, including permission to obtain death certificate information, was obtained from each participant.
Analytical Strategy
Participant characteristics were compared according to baseline depression status (major depression or minor depression vs no depression) stratified according to groups defined according to practice randomization assignment (intervention condition or usual care) using linear and logistic regression with random effects to account for clustering of participants according to practice. The primary strategy was to compare persons with depression with persons without depression within strata defined according to medical condition. Doing so provides a benchmark for gauging the influence of unmeasured practice characteristics such as the interest and skill of the primary care physician, quality of care, and case-mix of patients in the practice. Survival time was modeled using Cox proportional hazards regression, adjusting standard errors for within-practice clustering.
To examine whether the intervention moderated the relationship between depression and mortality in the presence of medical conditions, a three-way interaction between medical condition, baseline depression status, and intervention assignment was introduced into the Cox model in addition to main effects and corresponding two-way interactions. Based on the above Cox three-way interaction model, hazard ratios (HRs) and corresponding confidence intervals (CIs) were stratified according to intervention condition. Separate models were estimated for each medical condition. Results are reported in terms of HRs and CIs. Final models included terms for characteristics identified according to their association (P < .05) with time to death: baseline age, sex, education, marital status, smoking status, cognition, suicidal ideation, and Charlson Comorbidity Index. There was no evidence of violation of the proportional hazards assumption.15 SAS version 9.4 (SAS Institute, Inc., Cary, NC) was used in these analyses.
RESULTS
Baseline Characteristics
The study sample consisted of 1,226 persons with a mean age of 72.8 7.4 (range 60–95). Baseline sociodemographic and clinical characteristics according to depression status and practice randomization group assignment are shown in Table 1.
Table 1.
Baseline Sociodemographic and Clinical Characteristics According to Depression Status and Practice Randomization Group Assignment
| Characteristic | Intervention Practices |
Usual Care Practices |
||||
|---|---|---|---|---|---|---|
| Major Depression, n = 214 |
Major Depression, n = 106 |
Major Depression, n = 289 |
Major Depression, n = 182 |
Major Depression, n = 97 |
Major Depression, n = 338 |
|
| Sociodemographic | ||||||
| Age, mean ± SD | 70.3 ± 8.0 | 71.2 ± 7.5 | 71.7 ± 7.8 | 68.8 ± 7.5c | 71.8 ± 8.7 | 71.9 ± 7.7 |
| Female, n (%) | 149 (69.6) | 72 (67.8) | 194 (67.1) | 136 (74.7) | 72 (74.2) | 234 (69.2) |
| Ethnic minority, n (%)d | 63 (29.4) | 30 (28.3) | 82 (28.4) | 71 (39.0) | 32 (33.0) | 124 (36.7) |
| Education, mean ± sd | 12.3 ± 3.1b | 13.2 ± 3.4 | 13.1 ± 3.8 | 12.6 ± 3.4 | 13.0 ± 3.1 | 13.2 ± 3.8 |
| Married | 77 (36.0)a | 39 (36.8) | 124 (42.9) | 63 (34.6) | 41 (42.3) | 127 (37.6) |
| Current smoker, n (%) | 37 (17.3)a | 23 (21.7)b | 32 (11.1) | 41 (22.5)b | 12 (12.4) | 40 (11.8) |
| Medical comorbidity | ||||||
| Vascular conditions, n (%) | ||||||
| Heart disease | 95 (44.4)b | 31 (29.2) | 89 (30.8) | 70 (38.5) | 30 (30.9) | 105 (31.1) |
| High blood pressure | 141 (65.9) | 60 (56.6) | 186 (64.4) | 122 (67.0) | 69 (71.1) | 222 (65.7) |
| Peripheral vascular disease | 76 (35.5)b | 20 (18.9) | 65 (22.5) | 49 (26.9) | 28 (28.9) | 84 (24.9) |
| Stroke | 58 (27.1)c | 20 (18.9) | 33 (11.4) | 35 (19.2) | 20 (20.6) | 46 (13.6) |
| Nonvascular conditions, n (%) | ||||||
| Diabetes mellitus | 50 (23.4) | 20 (18.9) | 58 (20.1) | 39 (21.4) | 14 (14.4) | 79 (23.4) |
| Cancer | 27 (12.6) | 13 (12.3) | 31 (10.7) | 32 (17.6) | 13 (13.4) | 43 (12.7) |
| Chronic pulmonary disease | 62 (29.0)b | 19 (17.9) | 50 (17.3) | 55 (30.2)c | 18 (18.6) | 51 (15.1) |
| Charlson Comorbidity Index, mean ± SD | 3.4 ± 2.5b | 2.4 ± 2.3 | 2.3 ± 2.2 | 3.1 ± 2.3b | 2.6 ± 2.2a | 2.3 ± 2.1 |
| Cognition and depressione | ||||||
| Mini-Mental State Examination score, mean ± sdf | 27.4 ± 2.6 | 27.8 ± 2.1 | 27.5 ± 2.5 | 27.2 ± 2.6 | 27.6 ± 2.2 | 27.5 ± 2.4 |
| HDRS score, mean ± SDg | 21.1 ± 5.7c | 13.7 ± 3.2c | 5.0 ± 3.9 | 19.7 ± 5.5c | 13.4 ± 3.7c | 5.4 ± 4.4 |
| Scale for Suicidal Ideation score > 0h | 79 (36.9)c | 15 (14.2) | 19 (6.6) | 48 (26.4)c | 8 (8.2) | 28 (8.3) |
Data from Prevention of Suicide in Primary Care Elderly: Collaborative Trial (1999–2008).
SD = standard deviation.
P < .05
P < .01
P < .001 for comparison of participants with major or minor depression and those with no depression in intervention and usual care practices; all other comparisons with nondepressed group were not significant (P > .05).
Other than non-Hispanic white (n = 402; Hispanic n = 46, non-Hispanic black n = 333, Asian n = 9, other non-Hispanic n = 14).
Major depressive disorder defined as Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) major depression, in contrast to clinically significant minor depression (defined as having four DSM-IV depressive symptoms, Hamilton Depression Rating Scale (HDRS) score ≥10, and 4-week duration).
Range 0 to 30 (inclusion criteria limited range to 18–30), with higher scores indicating less cognitive impairment.
Range 0 to 76, with high scores indicating greater depressive symptoms.
Range 0 to 38, with high scores indicating greater suicidal ideation.
Mortality Risk of Major Depression in Intervention Versus Usual Care
The median follow-up time after baseline was 98 months (range 0.8–116.4 months), during which 405 participants died. Figure 1 shows the association between major depression and mortality, stratified according to intervention status and medical condition. Participants with different medical conditions with major depression in the intervention condition were compared with those in usual care. Older adults with major depression and diabetes mellitus were less likely to die when in practices randomized to the intervention condition (HR = 0.47, 95% CI = 0.24– 0.91), indicating that participants with diabetes mellitus and major depression were 53% less likely to die over follow-up if they had received the PROSPECT intervention. For other medical conditions, the point estimate for risk of death in persons with major depression were all in the direction of indicating lower risk but did not reach statistical significance.
Figure 1.
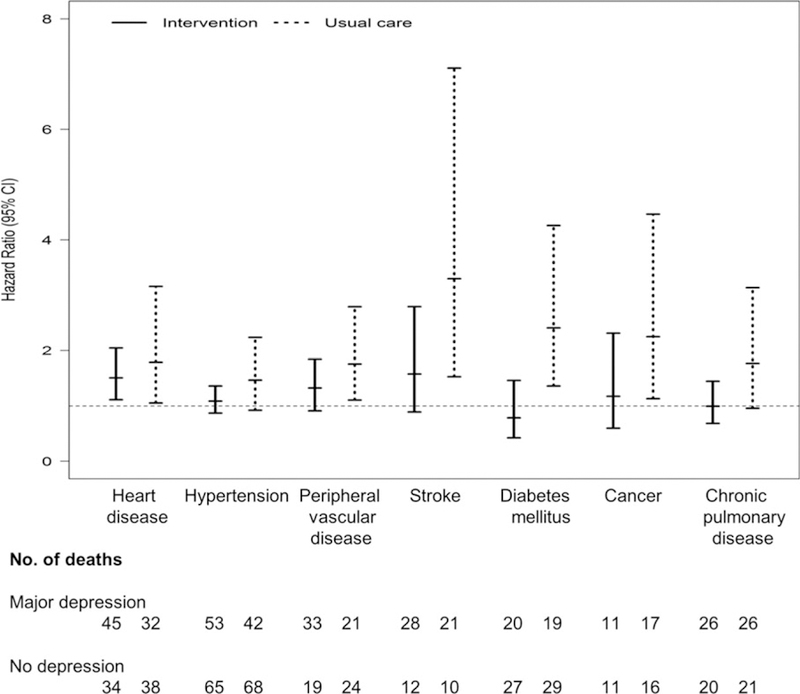
Mortality risk with major depression compared with no depression for each medical condition at baseline in intervention (dashed) and usual care (dotted) groups, adjusted hazard ratios and 95% confidence intervals (CIs). Data from Prevention of Suicide in Primary Care Elderly: Collaborative Trial (1999–2008).
Mortality Risk of Minor Depression in Intervention Versus Usual Care
Figure 2 shows the association between minor depression and mortality, stratified according to intervention status and medical condition. Participants in usual care with diabetes mellitus and minor depression were at greater risk of death (HR = 2.25, 95% CI = 1.12–4.53) than those without depression. In intervention practices, participants with diabetes mellitus and minor depression were no more likely to die than those without depression (HR = 1.40, 95% CI = 0.68–2.90). In usual care and intervention practices, participants with heart disease and minor depression were more likely to die than those without depression. For other conditions, minor depression did not confer greater risk of death. When participants with different medical conditions with minor depression in the intervention condition were compared with those in usual care, no statistically significant effects were observed.
Figure 2.
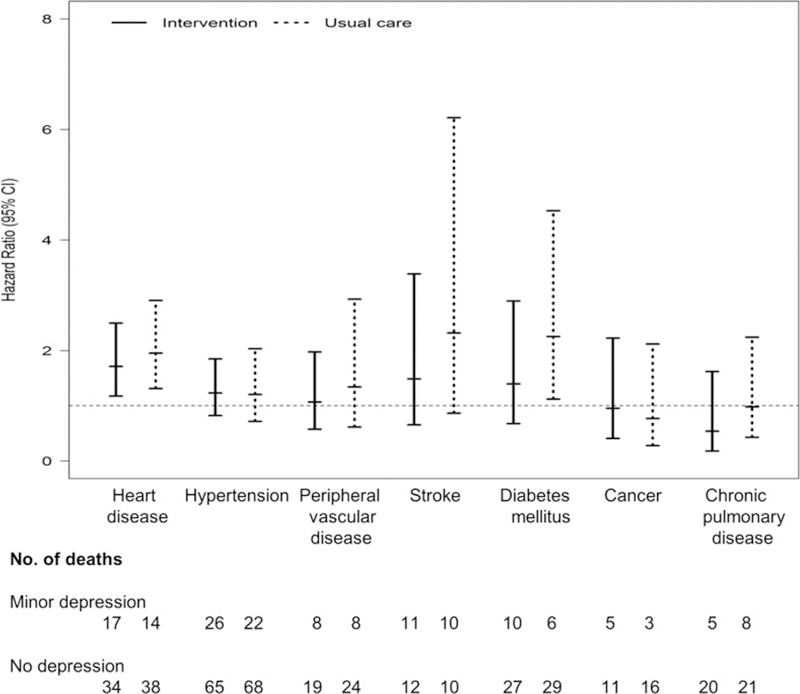
Mortality risk with minor depression compared with no depression for each medical condition at baseline in intervention (dashed) or usual care (dotted) group, adjusted hazard ratios and 95% confidence intervals (CIs). Data from Prevention of Suicide in Primary Care Elderly: Collaborative Trial (1999–2008).
DISCUSSION
Older adults with depression and medical comorbidity pose a significant clinical and public health challenge. The research question explored in this investigation concerned whether providing depression care management in primary care influenced mortality in the presence of several medical conditions. It was considered most appropriate to report findings for several medical conditions because primary care physicians must treat many conditions. In usual care, major depression was associated with greater risk of death for persons with heart disease, peripheral vascular disease, stroke, diabetes mellitus, and cancer. Participants in the intervention condition were not at greater risk of death from major depression for all conditions except heart disease. For diabetes mellitus, the intervention significantly modified the effect of major depression on death. It was not observed that minor depression conferred excess risk of death.
Before the findings are discussed, the results must be considered in the context of several important limitations. First, the diagnosis of chronic medical conditions was based on self-reports and was subject to imperfect recall and response bias. Information was not available on severity, duration, or treatment of specific medical conditions, so even within a condition, participants were likely to be heterogeneous. Small numbers preclude examining specific diagnoses (e.g., forms of heart disease or cancer). Estimates of association were reported adjusted for a validated index of medical comorbidity. Comparing the mortality of participants with depression with that of those without depression from the same sets of practices mitigates the influence of unmeasured characteristics at the practice level. The lower mortality of participants with major depression and specific medical comorbidities randomized to the intervention may be due to factors other than the specific effects of a depression management program. For example, it is not known whether primary care physicians in the intervention practices were more likely to see people with diabetes mellitus than those in the usual care practices. Third, subgroup analyses have limitations,8 but published criteria including subgroups defined according to risk, the known pathophysiological mechanisms linking depression and comorbidity, and the need for information about the role of medical comorbidity on treatment outcomes were used as a guide. This exploratory analysis was undertaken because there was evidence from a literature review of lower mortality related to depression treatment, with few studies having a randomized design.
For individuals with diabetes mellitus, depression has been specifically linked to prognostic variables such as micro- and macrovascular complications.16 Depression has been found to increase all-cause mortality even in the context of good glucose control.17 Although cohort studies document that depression is associated with greater risk of death in persons with diabetes mellitus,18–21 a previous report has been the only study to show that persons with diabetes mellitus and depression are half as likely to die over 5 years of follow-up in intervention practices as those in usual care.22 This exploratory analysis found evidence of a statistically significant intervention effect on mortality in persons with major depression, with trend toward an intervention effect for other conditions, except heart disease.
Few depression intervention studies of chronically ill individuals report mortality outcomes. For example, antidepressant treatment of individuals with chronic pulmonary disease and depression was associated with lower overall mortality after 2 years, although the study used claims data for depression diagnosis and did not randomized participants to antidepressants.23 Cancer progression does not seem to be related to depression, although depression increases the risk of death in persons with cancer.24
Enhancing Recovery in Coronary Heart Disease (ENRICHD), Sertraline Antidepressant Heart Attack Randomized Trial, and Myocardial INfarction and Depression —Intervention Trial did not find a benefit for the intervention on mortality for participants with heart disease, similar to the current findings. For all three of these trials, there was no difference in the primary medical end-point between the intervention and control arms. In ENRICHD, the largest of the three studies, enrolling 2,481 participants, 1,839 with depression, investigators found that taking a selective serotonin reuptake inhibitor was associated with lower risk of all-cause mortality,25 as was participation in group plus individual therapy,26 but these secondary analyses ignored randomization. In an observational cohort from Veterans Health Administration records of 4,037 individuals with depression after incident myocardial infarction, it was that participants who did not have 12 weeks or more of continuous antidepressant treatment at adequate doses were three times as likely to die as were persons who received adequate treatment.27 The study did not include clinical assessments of depression and did not randomize participants to treatment. Individuals who began adequate treatment may have differed from those who completed treatment in important factors that may be related to mortality.
It is necessary to understand more about the role of depression in cardiovascular disease, as well as the role of particular treatments for depression in cardiovascular disease. Overall, the current findings support the deleterious effect of depression in the context of cardiovascular disease on mortality, although major and minor depression conferred additional mortality risk for participants with heart disease regardless of whether they were in an intervention practice or usual care. The assumption that less depression will improve heart disease outcomes because the direction of association may be the other way around —better cardiovascular outcomes may result in remitted depression—has been questioned.28 It was argued that, although observational studies show that decreasing depression improves outcomes of cardiovascular disease, randomized trials have not shown benefit.
The Patient Protection and Affordable Care Act, signed into law in March 2010, provides new impetus for treating medical comorbidity and depression. Highlighted was the need for better communication between mental health and primary care, the inclusion of mental health management in the medical home model for diabetes mellitus and other conditions, and new models of integrated healthcare delivery. Integrated care is a promising development for management of complex older adults with comorbid conditions such as diabetes mellitus and depression.
ACKNOWLEDGMENTS
Financial support was received from the National Institute of Mental Health (HB: R21 MH094940, R34 MH085880; JJ: K23 MH100705; KM: K01 MH073903; MB: P30 MH085943; CR: P30 MH090333; JG: R01 MH065539) and American Heart Association (HB: Award #13GRNT17000021).
Sponsor’s Role: The mortality follow-up of PROSPECT participants was funded by the National Institute of Mental Health (NIMH) (PI: Joseph J. Gallo; R01 MH065539). Dr. Bogner was supported by Agency for Healthcare Research and Quality K18 HS23445-02, American Heart Association Award 13GRNT17000021, National Institute of Mental Health R21 MH094940 and R34 MH085880. Dr. Morales, Dr. Bruce, and Dr. Reynolds were supported by K01 MH073903, P30 MH085943, and P30 MH090333 by NIMH. The sponsors had no role in the design or conduct of the study; data collection, management, analysis, or interpretation; or preparation, review, or approval of manuscript.
Footnotes
Conflict of Interest: The authors have no financial or any other kind of conflicts of interest to declare.
REFERENCES
- 1.Druss B, Walker E. Mental Disorders and Medical Comorbidity. Research Synthesis Report No. 21 Princeton, NJ: The Robert Wood Johnson Foundation, 2011. [PubMed] [Google Scholar]
- 2.Penninx BW, Geerlings SW, Deeg DJ et al. Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry 1999;56: 889–895. [DOI] [PubMed] [Google Scholar]
- 3.Bruce ML, Ten Have TR, Reynolds CF III et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA 2004;291:1081–1091. [DOI] [PubMed] [Google Scholar]
- 4.Harpole LH, Stechuchak KM, Saur CD et al. Implementing a disease management intervention for depression in primary care: A random work sampling study. Gen Hosp Psychiatry 2003;25:238–245. [DOI] [PubMed] [Google Scholar]
- 5.Unützer J, Katon W, Callahan CM et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA 2002;288:2836–2845. [DOI] [PubMed] [Google Scholar]
- 6.Alexopoulos GS, Reynolds CF III, Bruce ML et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry 2009;166:882–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallo JJ, Morales KH, Bogner HR et al. Long term effect of depression care management on mortality in older adults: Follow-up of cluster randomized clinical trial in primary care. BMJ 2013;346:f2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.VanderWeele TJ, Knol MJ. Interpretation of subgroup analyses in randomized trials: Heterogeneity versus secondary interventions. Ann Intern Med 2011;154:680–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulsant BH, Alexopoulos GS, Reynolds CF III et al. Pharmacological treatment of depression in older primary care patients: The PROSPECT algorithm. Int J Geriatr Psychiatry 2001;16:585–592. [DOI] [PubMed] [Google Scholar]
- 10.Schulberg HC, Bryce C, Chism K et al. Managing late-life depression in primary care practice: A case study of the health specialist’s role. Int J Geriatr Psychiatry 2001;16:577–584. [DOI] [PubMed] [Google Scholar]
- 11.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas 1977;1:385–401. [Google Scholar]
- 12.Williams JW Jr, Barrett J, Oxman T et al. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. JAMA 2000;284:1519–1526. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 14.Doody MM, Hayes HM, Bilgrad R. Comparability of National Death Index Plus and standard procedures for determining causes of death in epidemiologic studies. Ann Epidemiol 2001;11:46–50. [DOI] [PubMed] [Google Scholar]
- 15.Allison PD. Survival Analysis Using SAS: A Practical Guide, 2nd Ed. Cary, NC: SAS Institute Inc, 2010. [Google Scholar]
- 16.de Groot M, Anderson R, Freedland KE et al. Association of depression and diabetes complications: A meta-analysis. Psychosom Med 2001;63: 619–630. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan MD, O’Connor P, Feeney P et al. Depression predicts all-cause mortality: Epidemiological evaluation from the ACCORD HRQL substudy. Diabetes Care 2012;35:1708–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Norris SL, Gregg EW et al. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol 2005;161:652–660. [DOI] [PubMed] [Google Scholar]
- 19.Katon WJ, Rutter C, Simon G et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 2005;28:2668–2672. [DOI] [PubMed] [Google Scholar]
- 20.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care 2003;26:2822–2828. [DOI] [PubMed] [Google Scholar]
- 21.Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care 2005;28:1339–1345. [DOI] [PubMed] [Google Scholar]
- 22.Bogner HR, Morales KH, Post EP et al. Depression, diabetes, and death: A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care 2007;30:3005–3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qian J, Simoni-Wastila L, Rattinger GB et al. Associations of depression diagnosis and antidepressant treatment with mortality among young and disabled Medicare beneficiaries with COPD. Gen Hosp Psychiatry 2013; 35:612–618. [DOI] [PubMed] [Google Scholar]
- 24.Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer 2009;115:5349–5361. [DOI] [PubMed] [Google Scholar]
- 25.Taylor CB, Youngblood ME, Catellier D et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005;62:792–798. [DOI] [PubMed] [Google Scholar]
- 26.Saab PG, Bang H, Williams RB et al. The impact of cognitive behavioral group training on event-free survival in patients with myocardial infarction: The ENRICHD experience. J Psychosom Res 2009;67:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scherrer JF, Chrusciel T, Garfield LD et al. Treatment-resistant and insufficiently treated depression and all-cause mortality following myocardial infarction. Br J Psychiatry 2012;200:137–142. [DOI] [PubMed] [Google Scholar]
- 28.Ziegelstein RC. Improving depression and reducing cardiac events: Which is the chicken and which is the egg? J Psychosom Res 2013;74:454–457. [DOI] [PubMed] [Google Scholar]


